Published online Oct 7, 2025. doi: 10.3748/wjg.v31.i37.110269
Revised: June 27, 2025
Accepted: August 22, 2025
Published online: October 7, 2025
Processing time: 114 Days and 10.3 Hours
Data suggest that elderly patients may have a lower risk of complications after endoscopic retrograde cholangiopancreatography (ERCP), especially post-ERCP pancreatitis (PEP).
To validate these findings in a large, real-world clinical setting.
Clinical, epidemiological, and procedural data collected from a prospectively maintained database were gathered over a 20-year period (2001-2021) from consecutive patients undergoing their first ERCP. Patients were grouped based on age: < 80 years and ≥ 80 years.
A total of 3147 patients were included in the study, with 70.3% < 80 years old and 28.7% ≥ 80 years. The most common indication for ERCP was biliary colic with or without elevated liver enzymes (39.6%). Periampullary diverticula were more frequently observed in elderly patients (P < 0.001). Successful cannulation of the common bile duct was achieved in 96.1% of cases and did not differ significantly between age groups (P = 0.148). Complete common bile duct clearance during the first ERCP was accomplished in 90.1%, and stone size was the only independent predictor of success. Use of antiplatelet or anticoagulant therapy was independently associated with intraprocedural bleeding (odds ratio [OR] = 1.333; P = 0.03 and OR = 1.275; P = 0.041, respectively). Overall, post-ERCP complications occurred in 6% of cases, with similar rates between elderly and younger patients. The most common complication was PEP. The incidences of clinical bleeding and PEP did not differ significantly between groups (P = 0.290 and P = 0.128, respectively). Clinical bleeding was independently associated with anticoagulant use and intraprocedural bleeding.
Our findings highlight that elderly patients do not experience higher complication rates or lower success rates with ERCP, supporting the procedure’s safety and efficacy in this population.
Core Tip: Data suggest that endoscopic retrograde cholangiopancreatography (ERCP) is just as effective in elderly patients as in younger ones and is associated with a lower rate of complications, including post-ERCP pancreatitis. Based on our experience, ERCP in elderly patients is generally as safe and effective as in younger patients. However, when complications do occur, they tend to be more challenging to manage. Additionally, factors such as the use of antiplatelet and anticoagulant medications, the presence of periampullary diverticula, and larger stones, more frequently observed among elderly patients, may pose additional risks, especially for bleeding, and may influence procedural success.
- Citation: Voulgaris TA, Tribonias G, Papanikolaou IS, Karamanolis GP, Vezakis IA, Louta A, Varvarelis OP, Chardalias L, Polydorou A, Vezakis A. Endoscopic retrograde cholangiopancreatography in elderly patients: Is age just a number or something more? World J Gastroenterol 2025; 31(37): 110269
- URL: https://www.wjgnet.com/1007-9327/full/v31/i37/110269.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i37.110269
Endoscopic retrograde cholangiopancreatography (ERCP) is currently an invaluable therapeutic procedure indicated for a variety of biliary and pancreatic conditions[1]. In recent years, improvements in training, accumulated endoscopist experience, and advances in techniques and modalities have led to an exceptionally high success rate. Nonetheless, ERCP remains imperfect[2,3]. It is also associated with a risk of peri- and post-procedural adverse events, which are not negligible and can sometimes be severe, even resulting in death. The most common complications include post-ERCP pancreatitis (PEP), bleeding, cholangitis, and perforation. Despite guidelines recommending prophylactic measures to mitigate these risks, such adverse events cannot be entirely avoided[4,5]. In Greece, as in many parts of Europe, recent data indicate that the average life expectancy exceeds 80 years[6]. Consequently, endoscopists are increasingly performing ERCPs in elderly patients, who are often characterized by higher frailty, polypharmacy, and more complex medical histories[7,8].
Some recent evidence suggests that elderly patients may even have a lower risk of complications following ERCP, particularly PEP[9,10]. This protective effect of aging appears to persist in patients over 65 years old, according to an older meta-analysis[11]. However, the success rate of ERCP does not seem to be affected by age; even in patients over 80 or 90 years, success rates generally exceed 90%[12,13].
Interestingly, a recent study involving patients over 90 concluded that, although complication rates such as PEP did not differ between frail and non-frail elders, frail patients had a significantly higher mortality risk and healthcare burden[14]. Similarly, a meta-analysis of studies including patients over 90 years old failed to demonstrate significant differences in ERCP success or adverse event rates compared to younger patients; however, the risk of bleeding and procedure-related mortality was notably higher in nonagenarians[15].
Research on the success rates and complications of ERCP in patients over 80 is limited and often involves small sample sizes. Furthermore, many studies do not apply a consistent age cutoff; some define elderly as 80 years old, while others use 90. As previously noted, the average life expectancy in Europe, and particularly in Greece, is close to 80 years. Data focusing on patients over 65 are more plentiful. Therefore, the main objective of our study was to evaluate the safety and efficacy of ERCP in a large, real-world cohort of patients aged 80 years and older. We specifically examined those undergoing their first ERCP and compared their outcomes to a younger control group, utilizing a prospectively maintained database.
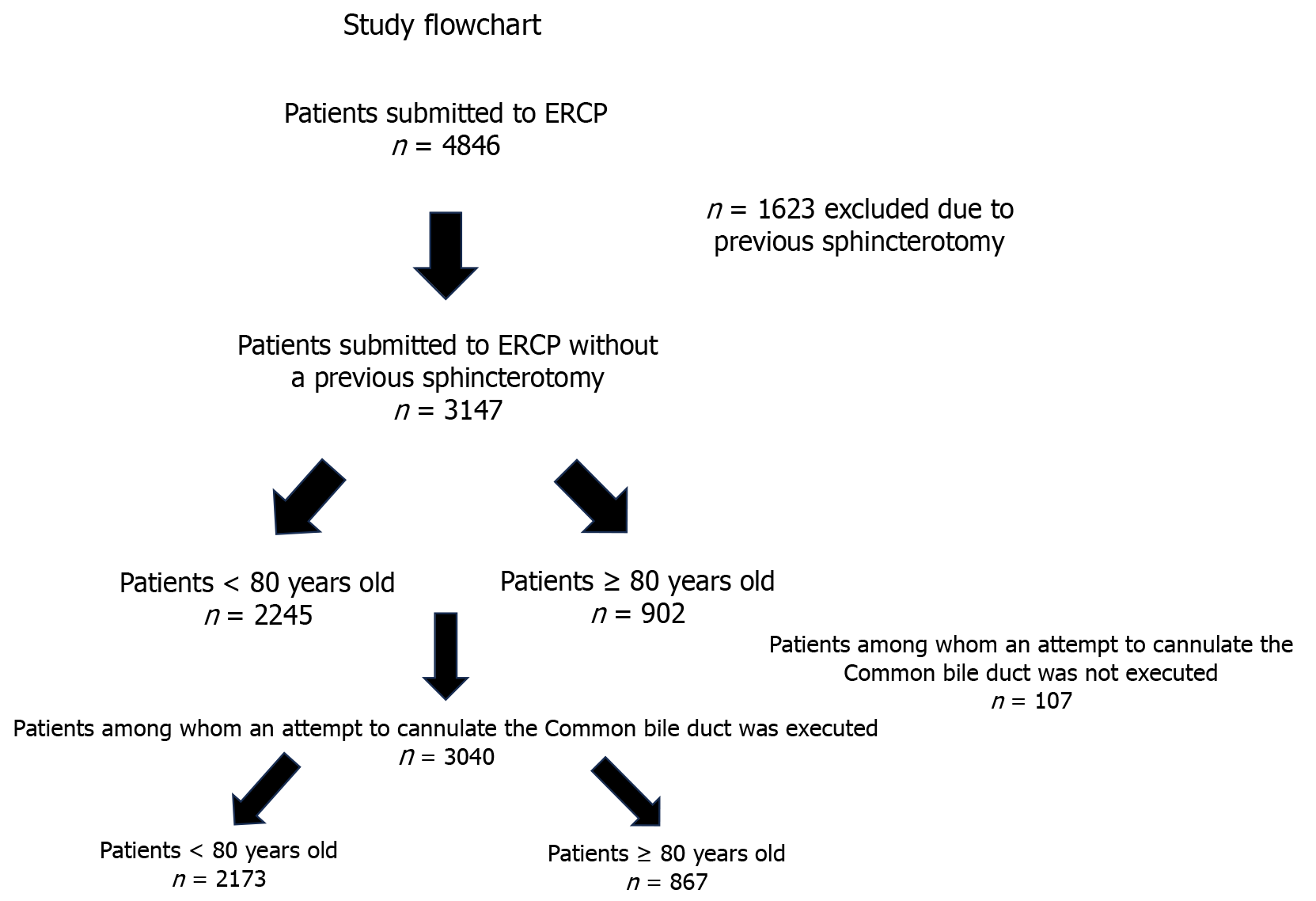
This is a real-world clinical practice study based on consecutive ERCP procedures performed at two hepatopancreatobiliary reference centers in Athens, Greece: Tzaneio General Hospital and Aretaeion Hospital. All procedures were conducted by a senior endoscopist or by fellows supervised by the same senior endoscopist. The study population included patients over 17 years of age who underwent ERCP over a 20-year period (2001-2021). A total of 4846 patients received ERCP during this period. After excluding patients with previous sphincterotomy, 3147 patients undergoing their first ERCP were included. Patients were categorized based on age (< 80 or ≥ 80 years; Figure 1).
All information was recorded prospectively in a predefined form, standardized for all patients throughout the 20-year study period. Epidemiological, clinical, laboratory, radiological, therapeutic data, as well as post-ERCP follow-up information, were collected from a maintained database in 2024 and analyzed retrospectively.
ERCP procedure cannulation of the common bile duct (CBD) was attempted using a sphincterotome with a guidewire. No contrast was injected into the pancreatic duct unless indicated. Patients underwent needle-knife (NK) precut after 5-10 minutes of failed cannulation attempts or after 5-10 unsuccessful attempts. The interval and number of attempts decreased over time during the study. Once cannulation was achieved, endoscopic sphincterotomy was performed based on clinical indication. Fluoroscopy was routinely used at the end of each procedure to exclude retroperitoneal gas. No prophylactic medications as non-steroidal anti-inflammatory drugs (NSAIDs) or pancreatic stents were applied to prevent pancreatitis, though all patients received intravenous (IV) fluids before and for 4-6 hours post-ERCP, initially 1 L of normal saline, or Ringer’s lactate in the last 10 years, depending on cardiac function and clinician judgment. All patients received prophylactic IV antibiotics preoperatively (cefuroxime, ciprofloxacin, or piperacillin/tazobactam), tailored according to allergies and prior hospitalizations.
Antiplatelet and anticoagulant drug use was documented. Until 2010 both aspirin and clopidogrel were discontinued 5 days before ERCP performance while warfarin was also ceased 5 days before ERCP, with bridging therapy with low molecular heparin administered based on attending physician’s judgement. For all patients on anticoagulants, international normalized ratio was measured before the procedure and was not performed if international normalized ratio was not < 1.5. After 2010, aspirin was not routinely stopped before the procedure, and with the introduction of direct oral anticoagulants, the last dose was administered at least 48-72 hours before the procedure.
The sedation protocol evolved over the years. Initially, it consisted of administering 1-2 mg midazolam ± 0.50 μg fentanyl bolus IV, according to endoscopist judgment, followed by titrated propofol dosing (minimum: 20 mg; maximum: 800 mg). Pulse rate, oxygen saturation, and blood pressure were continuously monitored during the procedure.
Definitions of individual complications followed Cotton et al[5]. Pancreatitis was defined as an increase in serum amylase > 3 times the normal value, combined with new or worsening abdominal pain, more than 24 hours after ERCP[4]. Hyperamylasemia in the absence of pain persisting more than 6 hours post-ERCP was considered non-clinically significant. Hyperamylasemia was documented in case of serum amylase increase > 3 times the upper normal value. Perforation was considered clinically significant if treatment was escalated during or after ERCP with contrast leakage, presence of subcutaneous emphysema, or patient distress. Intraprocedural bleeding was defined as bleeding during sphincterotomy, while clinical bleeding was observed after the procedure. Peritoneal guidewire insertion or contrast injection without retroperitoneal gas was not classified as perforation. Cholangitis and cholecystitis were diagnosed according to Tokyo criteria[16,17]. Complication severity was graded: Mild (2-3 days of hospitalization), moderate (4-10 days), and severe (> 10 days). Procedures requiring intervention (endoscopic, percutaneous, or surgical) or intensive care admission were considered severe.
Data were analyzed using SPSS version 27 (IBM SPSS Statistics, Chicago, IL, United States). Variables were expressed as frequencies, means ± SD, or medians with interquartile ranges, as appropriate. Continuous variables were compared using Student’s t-test (for normal distributions, assessed by skewness and kurtosis since our sample is large enough) or the Mann-Whitney U test (for non-normal distributions). Categorical variables were compared with χ² or Fisher’s exact tests. Associations between variables were assessed with Spearman’s correlation coefficient. Multivariate linear and logistic regression models identified independent predictors. Only variables with P < 0.10 in univariate analysis were entered into multivariate models. Goodness of fit was assessed by the Hosmer-Lemeshow test. Two-sided P < 0.05 was considered statistically significant. Since this was a post hoc analysis of de-identified, previously collected data, ethical approval was deemed not required.
In total 3147 patients were included. Fifty-one percent were female. Of these, 2245 (70.3%) were < 80 years old and 902 (28.7%) were ≥ 80 years old (elders). Female sex was more common among the elders (P = 0.044). Antiplatelet drugs and anticoagulants were received significantly more frequently among elders (P < 0.001 for both). American Society of Anesthesiologists (ASA) score differed between groups: Patients ≥ 80 years were less likely to have an ASA score of 1 and more likely to have an ASA score of 3. The major indication for ERCP was biliary colic with or without jaundice and/or elevated liver enzymes (39.6%) and was the most frequent indication in both age groups. It was more common among non-elders (41% vs 36.3%), whereas cholangitis was more common among elders (20.4% vs 9.0%; P < 0.001). Prior gastrectomy was more frequent among elders, while prior hepatobiliary surgery was more common among non-elders (P = 0.040 and P = 0.008, respectively). Periampullary diverticula (PAD) occurred more often in elderly patients (P < 0.001). The rate of papillary abnormalities (inflamed papilla, impacted stone, or adenoma) did not differ between groups. Specifics for epidemiological data and ERCP indications are given in Table 1.
| Total cohort | < 80 age old (n = 2245) | ≥ 80 (n = 902) | P value | |
| Sex (male/female) | 1541 (49)/1606 (51) | 1125 (49.9)/1120 (50.1) | 416 (46.1)/486 (53.9) | 0.044 |
| Age [mean ± SD (min-max)] (years old) | 68 ± 16 (17-101) (skewness: -0.892 and kurtosis: 0.282) | 62 ± 15 (17-79) | 85 ± 4 (80-101) | |
| ASA score | < 0.001 | |||
| 1 | 540 (17.2) | 533 (23.7) | 7 (0.8) | |
| 2 | 1611 (51.2) | 1228 (54.7) | 383 (42.5) | |
| 3 | 984 (31.3) | 480 (21.4) | 504 (55.9) | |
| 4 | 12 (0.4) | 4 (0.2) | 8 (0.9) | |
| Antiplatelet use | 242 (7.7) | 141/2245 (6.3) | 101/902 (11.2) | < 0.001 |
| Anticoagulant use | 181 (5.8) | 95/2245 (4.2) | 86/902 (9.5) | < 0.001 |
| Indication | < 0.001 | |||
| Cholangitis | 386 (12.3) | 202 (9.0) | 184 (20.4) | |
| Obstructive jaundice | 910 (28.9) | 658 (29.3) | 252 (27.9) | |
| Biliary colic | 1247 (39.6) | 920 (41.0) | 327 (36.3) | |
| Pancreatitis | 315 (10) | 226 (10.1) | 89 (9.9) | |
| Bile leak | 139 (4.4) | 120 (5.3) | 19 (2.1) | |
| Asymptomatic choledocholithiasis | 150 (4.8) | 119 (5.3) | 31 (3.4) | |
| Previous gastrectomy | 76/3147 (2.4) | 46/2245 (2.0) | 30/902 (3.3) | 0.040 |
| Previous hepatobiliary operation | 970/3147 (30.8) | 723/2245 (32.2) | 247/902 (27.4) | 0.008 |
| Periampullary diverticula (among patients in whom Vater ampulla was reached) | 617/3085 (20) | 374/2205 (17.0) | 243/880 (27.6) | < 0.001 |
| Papilla abnormalities (inflamed, impacted stone or adenoma) | 501/3040 (16.5) | 368/2173 (16.9) | 133/867 (15.3) | 0.304 |
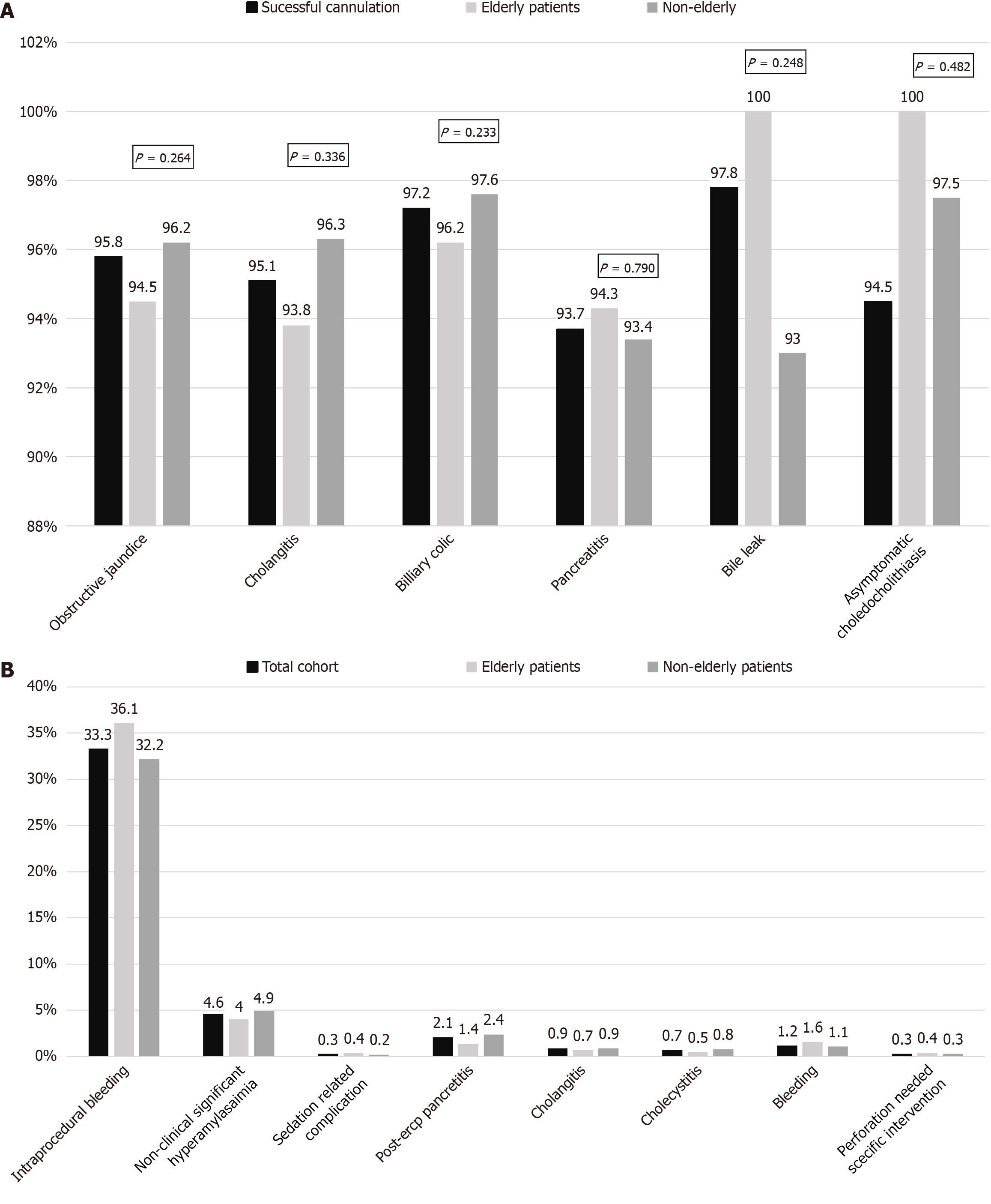
Inability to locate or reach the ampulla was observed in 107 patients (3.4%) and did not differ among the elders or not (P = 0.348). Among the remaining 3040 patients in whom at least one attempt to cannulate the CBD was performed, cannulation was successful in 96.1% and did not differ between age groups (P = 0.148). No differences in cannulation rate were observed across age groups for different ERCP indications (Figure 2A). Five or more attempts to cannulate were equally performed in the two groups (P = 0.291); use of NK sphincterotomy was also similar (P = 0.480). Elderly patients had lower rates of pancreatic duct catheterization and lower rates of subsequent normal cholangiogram (P = 0.012 and P < 0.001, respectively; Table 2).
| Total cohort | < 80 age old | ≥ 80 | P value | |
| Inability to locate or reach the ampulla | 107/3147 (3.4) | 72/2245 (3.2) | 35/902 (3.9) | 0.384 |
| Successful cannulation | 2291/3040 (96.1) | 2095/2173 (96.4) | 823/867 (95.3) | 0.148 |
| Attempts to cannulate | 0.291 | |||
| < 5 | 1296/3040 (42.6) | 913/2173 (42) | 383/867 (44.2) | |
| ≥ 5 | 1744/3040 (57.4) | 1260/2173 (58) | 484/867 (55.8) | |
| Needle-knife use | 0.480 | |||
| Yes | 1136/3040 (37.4) | 821/2173 (37.8) | 315/867(36.3) | |
| No | 1904/3040 (62.6) | 1352/2173 (62.2) | 552/867 (62.7) | |
| Catheterization of the pancreatic duct | 0.012 | |||
| Yes | 1095/3040 (36.0) | 813/2173 (37.4) | 282/867 (32.5) | |
| No | 1945/3040 (64.0) | 1360/2173 (62.6) | 585/867 (67.5) | |
| Stricture in the cholangiogram | 0.063 | |||
| Yes | 701/3040 (23.1) | 521/2173 (24.0) | 180/867 (20.8) | |
| No | 2339/3040 (76.9) | 1652/2173 (76.0) | 687/867 (79.2) | |
| Normal common bile duct in the cholangiogram | 210/2921 (7.2) | 171/2095 (8.2) | 39/826 (4.7) | < 0.001 |
Among patients in whom an attempt to cannulate the CBD was performed, the indication for ERCP generally did not influence cannulation success rates. However, a difference was observed when comparing specific patient groups: Those with pancreatitis had lower success rates, while patients with bile leaks experienced the highest success rates. This difference was statistically significant (P = 0.038). Additionally, cannulation rates were decreased in the presence of PAD (553/592, 93.4% vs 2368/2448, 96.7% if no PAD; P < 0.001), when five or more attempts were required to cannulate (1631/1744, 93.5% vs 1290/1296, 99.5% if < five attempts; P < 0.005), after cannulation of the pancreatic duct (1031/1095, 94.2% vs 1890/1945, 97.2% with no pancreatic duct cannulation; P < 0.001), or when NK was used (1027/1136, 90.4% vs 1895/1904, 99.5% when NK not used; P < 0.001). On the other hand, cannulation success was not correlated with sex (males: 1416/1483, 95.5% vs females: 1505/1557, 96.7%; P = 0.111) or the presence of an abnormal papilla (inflamed, impacted stone, or adenoma) (abnormal: 489/501, 97.6% vs 2432/2539, 95.8% when normal; P = 0.058). Irrespective of age group, patients in whom cannulation was unsuccessful were older (mean age of patients with successful cannulation: 68 ± 16 years old vs unsuccessful: 72 ± 15 years old; P = 0.020).
In patients with PAD, five or more cannulation attempts were less common (300/592, 50.7% vs 1444/2448, 59.0% when no PAD was observed; P < 0.001), and NK use was also less common (157/592, 26.5% vs 979/2448; P < 0.001). The rate of pancreatic duct catheterization did not differ (208/592, 35.1% vs 887/2448, 36.2%; P = 0.634). In the multivariate logistic regression analysis concerning factors affecting successful cannulation, age (odds ratio [OR] = 1.011, 95% confidence interval [CI]: 0.997-1.025; P = 0.111) and papillary abnormalities (OR = 0.945, 95%CI: 0.008-1.431; P = 0.868) were not associated with cannulation failure. By contrast, PAD was independently associated with cannulation failure (OR = 1.678, 95%CI: 1.504-1.686; P < 0.001). Other independent predictors of cannulation failure included NK use (OR = 1.929, 95%CI: 0.854-1.965; P < 0.001), five or more cannulation attempts (OR = 1.696, 95%CI: 1.247-1.877; P = 0.010), and pancreatic duct catheterization (OR = 1.390, 95%CI: 1.102-1.586; P = 0.012).
Among 1943 patients, in whom an attempt to clear the CBD of stones, sludge, or stone fragments was attempted, complete CBD clearance during the first ERCP was observed in 1751/1943 (90.1%) and was observed more frequently among non-elders (1242/1360, 91.3% vs 509/583, 87.3%; P = 0.008). Although stones > 15 mm were observed more frequently among the elders (84/583, 14.3% vs 74/1360, 5.5%; P < 0.001). In the multivariate analysis, however, age group (P = 0.967) was not correlated with complete CBD clearance, but the existence of stones > 15 mm was (OR = 1.942, 95%CI: 1.915-1.960; P < 0.001).
Among 642 patients having a stricture on cholangiography suggesting mainly malignancy, overall successful stent placement was observed in 97.5% (626/642) and the rate of successful stent placement did not differ between the two age groups (elders: 98.8% vs non-elders 97.0%; P = 0.259). A metallic stent was placed in 152 (24.3%) (114 uncovered and 38 partially covered) and plastic stents in 474 (75.7%) (straight plastic stents in 378 and pigtail in 89 patients while in 7 both a straight and a pigtail stent were inserted).
In 4.6% (145/3147), a non-clinically significant hyperamylasemia without the existence of abdominal pain after the first 6 hours following the exam was noticed. This rate did not differ among the two age groups (P = 0.347).
Intraprocedural bleeding was observed in 1048 patients (33.3%) and was more frequent among elders (36.1% vs 32.2%; P = 0.033) and also among antiplatelet (43.4% vs 32.5%; P < 0.001) or anticoagulant users (42.0% vs 32.8%; P = 0.012). Moreover, intraprocedural bleeding was more common in the presence of a PAD (37.9% vs 32.9%; P = 0.020), when five or more attempts were made to cannulate the CBD (37.6% vs 30.2%; P < 0.001), and when NK was used (41.5% vs 30.2%; P < 0.001), but was not correlated with sex (P = 0.734).
In the multivariate analysis, antiplatelets (OR = 1.323, 95%CI: 1.117-1.485; P = 0.005), anticoagulants (OR = 1.275, 95%CI: 0.997-1.463; P = 0.049), PAD (OR = 1.354, 95%CI: 1.119-1.638; P = 0.002), and NK use (OR = 1.610, 95%CI: 1.338-1.937; P < 0.001) were all significantly correlated with intraprocedural bleeding; age group and five or more attempts to cannulate the CBD were not (P = 0.132 and P = 0.263, respectively). Intraprocedural bleeding was initially successfully treated during ERCP performance in all patients, though recurrence of bleeding post-ERCP was observed in 28/1012 (2.7%) patients with intraprocedural bleeding and did not differ between elders and non-elders (2.8% vs 2.6%; P = 1.000). The most commonly used technique for endoscopic hemostasis during the procedure was subepithelial adrenaline injection (609/1012; 60.2%), while bleeding stopped spontaneously in 315 patients (31.1%). In 6 patients (0.1%), a metal stent was placed.
When excluding non-clinically significant hyperamylasemia and intraprocedural bleeding, ERCP-related complications occurred in 6.0% of cases and did not differ between the two age groups (elders: 54/902, 6.0% vs non-elders: 135/2245, 6.0%; P = 1.000). The majority of complications were graded as mild (122/189, 64.6% in the total cohort), with 44/189 (23.3%) classified as moderate and 23/189 (12.2%) as severe. Severe complications tended to occur more frequently among the elderly (10/902, 1.1%) compared to non-elders (13/2245, 0.6%; P = 0.092). Moreover, severe complications were more common in patients with an ASA score ≥ 3 (14/996, 1.4%) vs those with lower scores (9/2151; P = 0.004). The most frequently observed complication was pancreatitis (2.1%), occurring equally in elders and non-elders (P = 0.129). Rates of complications in the total cohort and within each group are presented in Figure 2B.
PEP was observed in 66 of 3147 patients (2.1%) and did not differ significantly between elders and non-elders, despite a numerically higher rate among non-elders (2.4% vs 1.4%; P = 0.129). A normal CBD (among 2921 patients who had a cholangiogram), five or more attempts to cannulate (among 3040 patients who attempted cannulation), and the use of a NK (among 3040 patients who attempted cannulation) were all associated with increased rates of PEP, as confirmed in multivariate logistic regression analysis (Hosmer and Lemeshow test; P = 0.916). Conversely, sex, an ASA score ≥ 3, obstructive jaundice as an indication for ERCP, the presence of periampullary diverticulum (PAD), successful cannulation, and CBD stenting were not significantly associated with PEP.
Cannulation of the pancreatic duct in general was correlated with PEP in univariate analysis but not in multivariate analysis. The rate of pancreatitis was higher when the pancreatic duct was catheterized two or more times, although this difference was marginally non-significant statistically (5.4% vs 2.5%; P = 0.062). However, more than one cannulation attempt of the pancreatic duct was not independently associated with PEP in the multivariate analysis (P = 0.156; OR = 1.432; 95%CI: 0.760-1.740). Table 3 summarizes these findings. Irrespective of age groups, younger age was identified as an independent risk factor for PEP. In univariate analysis, the mean age of patients who developed pancreatitis was 63 ± 17 years vs 68 ± 17 years in those who did not (P = 0.004). Multivariate logistic regression confirmed this, with an OR of 1.019 (95%CI: 1.005-1.032; P = 0.036).
| Pancreatitis development, n (%) | P value, univariate (χ2 test or Fisher’s exact test, as appropriate) | P value, multivariate binary logistic regression analysis | Multivariate binary logistic regression analysis, objective risk (95%CI) | |
| Elderly patients | 11/910 (1.4) | 0.129 | ||
| Non-elderly patients | 53/2245 (2.4) | |||
| Sex | 0.135 | 0.114 | 1.498 (0.907-2.475) | |
| Male | 26/1541 (1.7) | |||
| Female | 40/1606 (2.5) | |||
| ASA | 0.183 | |||
| 1-2 | 49/2151 (2.3) | |||
| 3-4 | 17/996 (1.7) | |||
| Normal common bile duct | 0.023 | 0.037 | 1.808 (1.091-1.959) | |
| Yes | 10/210 (4.8) | |||
| No | 54/2711 (2.0) | |||
| Attempts in order to cannulate | < 0.001 | 0.018 | 2.015 (1.129-3.596) | |
| < 5 | 12/1296 (0.9) | |||
| ≥ 5 | 54/1744 (3.1) | |||
| Needle knife use | < 0.001 | 0.018 | 2.381 (1.159-4.891) | |
| Yes | 41/1136 (3.6) | |||
| No | 25/1904 (1.3) | |||
| Successful cannulation | 0.708 | |||
| Yes | 64/2921 (2.2) | |||
| No | 2/119 (1.7) | |||
| Common bile duct stenting | 0.239 | |||
| Yes | 27/1034 (2.6) | |||
| No | 39/2006 (1.9) | |||
| Catheterization of the pancreatic duct | 0.026 | 0.280 | 1.320 (0.797-2186) | |
| Yes | 32/1100 (2.9) | |||
| No | 34/2047 (1.7) | |||
| Periampulary diverticula | 0.876 | |||
| Yes | 12/592 (2.0) | |||
| No | 54/2448 (2.2) |
Cholangitis was observed in a total of 27/3147 (0.9%) patients and the rate did not differ significantly between the elder and non-elder groups (P = 0.529). Post-ERCP cholangitis was more frequently observed in patients with stent placement (18/1034, 1.7% vs 9/2113, 0.4%; P < 0.001), patients with obstructive jaundice (16/910, 1.8% vs 11/2237, 0.5%; P = 0.001), and patients with a stricture in the cholangiogram (14/701, 2.0% vs 13/2446, 0.5%; P < 0.001). It was also more common among men (19/1541, 1.2% vs 8/1606, 0.5%; P = 0.032). In multivariate logistic regression analysis, none of these factors was independently associated with the development of cholangitis; however, male sex (OR = 1.542, 95%CI: 0.993-1.809; P = 0.052) and stent placement (OR = 2.473, 95%CI: 0.855-7.154; P = 0.095) showed tendencies toward significance. The P values for obstructive jaundice and stricture at cholangiogram were 0.303 and 0.674, respectively.
Excluding patients with a history of cholecystectomy, cholecystitis was observed in a total of 15/2184 (0.7%) patients, and the rate did not significantly differ between the elder and non-elder groups (P = 0.574). Post-ERCP cholecystitis was more frequently observed in patients who had a stent placed (8/721, 1.1% vs 7/1463, 0.7%), although this difference did not reach statistical significance (P = 0.102). When focusing on stent type, patients with fully covered metal stents showed a higher, though not statistically significant, rate of post-ERCP cholecystitis (0.7% vs 1.5%; P = 0.248). Patients with obstructive jaundice as the indication for ERCP were significantly more prone to develop post-ERCP cholecystitis (9/742, 1.2% vs 6/1442, 0.4%; P = 0.033) compared to patients with other indications such as cholangitis, pancreatitis, biliary colic, or asymptomatic choledocholithiasis.
Retroperitoneal perforation was observed in 31 patients (1%), with treatment escalation, either metallic stent placement (n = 6) or surgery, performed in 11 cases (0.3%). In the remaining 20 patients, conservative treatment was applied. Although perforation was more common among elder patients (1.4% vs 0.8%), this difference was not statistically significant (P = 0.111). There was no significant difference between the two groups regarding perforations requiring treatment escalation (0.4% vs 0.3%; P = 0.997). Additionally, retroperitoneal perforation was more frequent among patients with an ASA score ≥ 3, though this was not statistically significant (13/996, 1.3% vs 18/2151, 0.8%; P = 0.149).
Perforations requiring treatment were not correlated with the presence of PAD (0.2% vs 0.4%; P = 0.704) or with five or more attempts to cannulate (0.5% vs 0.2% with fewer than five attempts; P = 0.131). However, the use of a NK was associated with a higher perforation rate (0.7% vs 0.2%; P = 0.024). No deaths were directly attributable to retroperitoneal perforation, although 1 patient with perforation died due to sepsis related to a bile leak.
Post-intervention bleeding was observed in 39 of 3147 patients (1.2%) and was significantly more common in patients with initially arrested intraprocedural bleeding (28/1048; 2.7%) compared to those without such bleeding (11/2099; 0.5%; P < 0.001). Post-ERCP bleeding did not differ significantly between the two age groups (P = 0.372) and was not associated with antiplatelet use (P = 0.544), the presence of PAD (P = 1.000), or NK use (P = 0.320). However, it was more common among anticoagulant users (6.7% vs 0.9%; P < 0.001). Additionally, clinical bleeding tended to be more frequent among patients with an ASA score ≥ 3 (17/996; 1.7%) compared to those with lower scores (22/2151; 1.0%), although this difference was not statistically significant (P = 0.077).
Multivariate regression analysis confirmed (Hosmer and Lemeshow test; P = 0.851) that both initial intraprocedural bleeding and anticoagulant use were independently associated with post-ERCP bleeding, while ASA score ≥ 3 was not (OR = 0.981; 95%CI: 0.480-2.004; P = 0.978). Specifically, anticoagulant use was associated with a higher risk (OR = 4.842; 95%CI: 2.390-9.810; P < 0.001), whereas initial intraprocedural bleeding was also significantly associated (OR = 1.855; 95%CI: 1.705-1.928; P < 0.001).
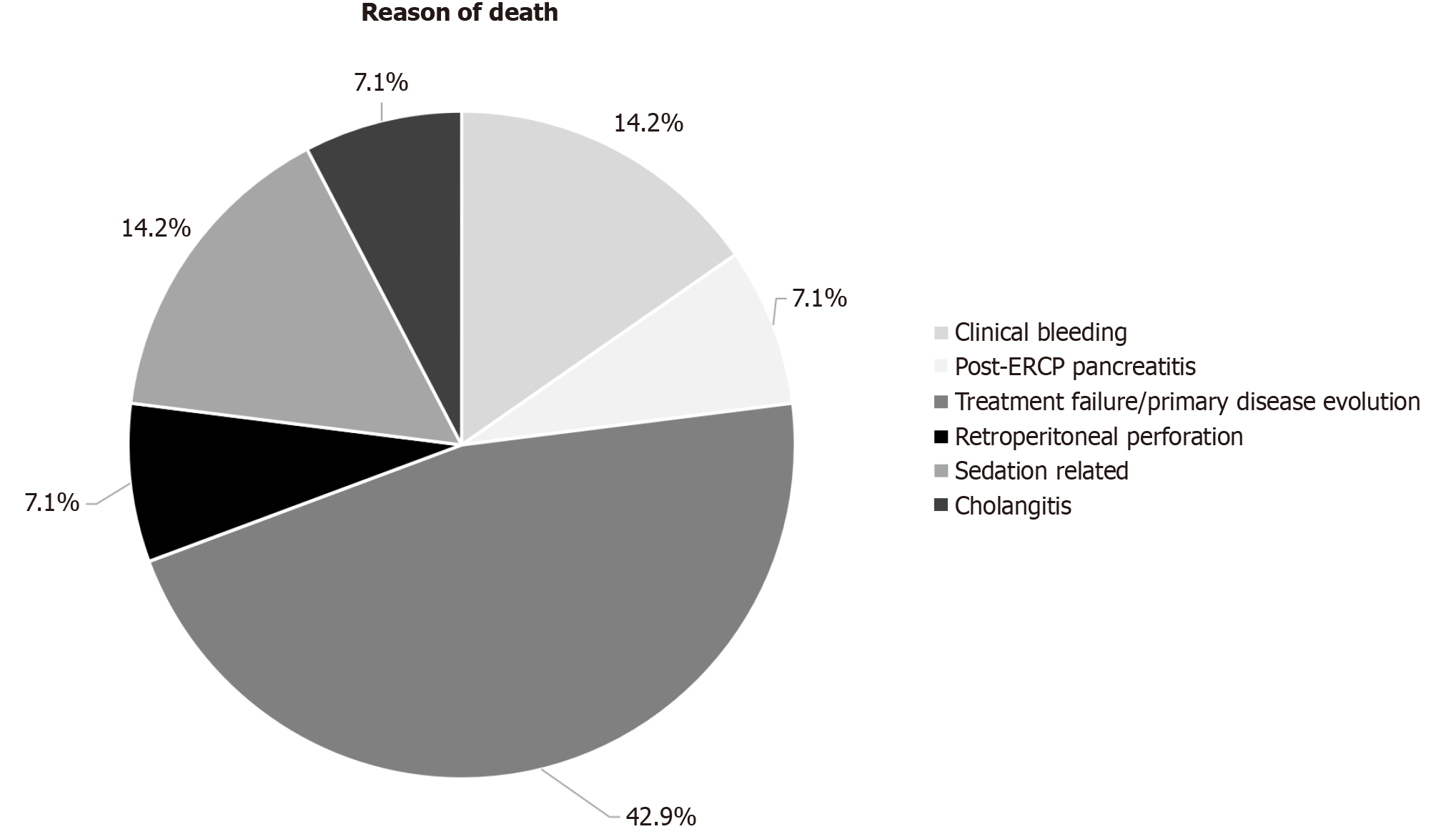
A total of 14 patients (0.4%) died, with no significant difference in mortality among elders (0.8% vs 0.3%; P = 0.077). Mortality was more frequent in patients with an ASA score ≥ 3 (10/996; 1.0%) compared to those with lower scores (2/2151; 0.1%; P < 0.001). The median time from ERCP to death was 5 days (range: 1 to 14 days). Six deaths (43%) were related to procedure complications, including one case of cholecystitis, one perforation, one case of acute necrotizing pancreatitis in a septic patient already diagnosed with pancreatitis and elevated bilirubin levels, two cases of clinical bleeding, and one case of cholangitis. Six additional deaths were due to disease progression or treatment failure, and two deaths resulted from cardiovascular causes, specifically, acute deterioration of pre-existing heart failure and cardiac arrest during the procedure, attributed to ERCP sedation (Figure 3).
To the best of our knowledge, excluding meta-analyses, our study comprises the largest cohort of elderly patients undergoing their first ERCP, focusing on the safety and efficacy of the procedure. We have once again shown that ERCP-related complication rates are similar across age groups and that procedural efficacy remains comparable. Our data indicate an overall complication rate of 6%, which aligns with the range reported by previous large-scale studies[18-20]. Importantly, this complication rate did not differ significantly between elderly and non-elderly patients, supporting prior findings in patients over 80 years old[21,22]. For example, Kanamori et al[23] reported a similar 30-day post-ERCP complication rate of 7.2%, with no significant difference between patients younger and older than 80, except for a higher cardiopulmonary complication rate in the elderly[23]. Conversely, Galeazzi et al[12] observed a higher overall complication rate, 13.2% in patients under 80 and 10% in those over 80, without statistically significant differences between the groups[12].
Our study also provided evidence that, although the overall complication rate does not differ significantly with age, elderly patients tend to experience a slightly higher incidence of severe complications that require prolonged hospitalization. Specifically, 1% of elderly patients vs 0.4% of younger patients experienced such events. Most prior studies either did not report complication severity or documented very low rates of severe complications, often without adequately assessing length of hospital stay[21,22]. Ergin et al[24] found that hospitalized patients over 65 stayed on average one day longer (4 days vs 3 days), although this difference was not statistically significant, and data specifically for patients over 80 were limited[24]. In our study, while the trend toward increased length of stay among elderly patients did not reach statistical significance, it should not be overlooked, as it may reflect the intrinsic frailty often observed in older individuals. Most importantly, our data show that severe complications and mortality are more common among patients with an ASA score ≥ 3. Supporting this, a prior study of nonagenarians who underwent ERCP concluded that frail individuals had a longer median hospital stay (6.7 days vs 5.5 days)[14]. Therefore, even though overall complication rates are similar across age groups, managing post-ERCP complications in this vulnerable population can be more challenging due to frailty and comorbidities.
Previously published data, mostly from smaller studies, show no significant difference in mortality between elderly and younger patients[21-24]. Our findings echo this, with no statistically significant difference in mortality, although a numerical trend was noted. Meta-analyses suggest increased mortality in patients over 80 and 90 years old[11,15], but given that ERCP-related mortality in our cohort was very low (0.3%), detecting meaningful differences would require very large sample sizes.
One of the main concerns for endoscopists performing ERCP is the development of PEP, which remains the most common complication[25]. For this reason, guidelines from major endoscopic societies strongly emphasize strategies to prevent PEP[4,5]. Contrary to some previous reports, our study did not demonstrate a lower rate of PEP among elderly patients[9,22]. The idea of a lower PEP rate in elderly patients is not universally supported, as other studies have found no significant difference between older and younger patients[23,24,26]. It is important to note that, in our multivariate analysis, younger age was an independent predictor of PEP. Therefore, the slight numerical increase in PEP observed among elderly patients (2.4% vs 1.4%; P = 0.129) was not considered significant. Supporting this, when dividing our cohort using an age cutoff of 65 years, the rate of PEP was significantly lower in patients over 65 (1.6% vs 3.1%; P = 0.003). Notably, the original study proposing a reduced PEP rate in elderly patients also used the same age cutoff of 65 years[26].
Interestingly, our observed PEP rate of 2.4% in the elderly is lower than rates reported in previous studies and was achieved even without routine prophylaxis with NSAIDs or pancreatic stents, which are commonly used elsewhere. This rate falls within the range previously reported for elderly populations[23,24,26,27]. Some hypotheses suggest that increased pancreatic atrophy, fibrosis, or reduced pancreatic enzyme secretion with age might explain reduced PEP rates in the elderly, but this was not confirmed in our age group comparisons[11]. Because this is a retrospective cohort study and we did not include data on pathophysiological changes among elderly vs non-elderly patients, we cannot provide an evidence-based explanation for discrepancies in PEP rates observed across different studies.
Several studies have identified independent risk factors for PEP, including difficult cannulation (e.g., five or more attempts), the use of NK sphincterotomy, and a normal CBD caliber, which are consistent with European Society of Gastrointestinal Endoscopy (ESGE) guidelines on ERCP-related adverse events[4]. Although a female predominance was numerically observed in our cohort, sex was not an independent predictor of PEP, nor was multiple cannulation of the pancreatic duct associated with increased risk. Unfortunately, data regarding prior episodes of pancreatitis were not documented, limiting our ability to evaluate this factor.
Regarding bleeding, our analysis yielded different findings for intraprocedural and post-procedure bleeding. Intraprocedural bleeding, which was successfully controlled in all cases, was significantly more frequent among elderly patients. Conversely, post-ERCP bleeding, responsible for the death of two patients, did not significantly differ between age groups. Once again, multivariate analysis demonstrated that age was not an independent predictor of intraprocedural bleeding; instead, use of antiplatelet and anticoagulant medications, the presence of PAD, and NK sphincterotomy were significant factors. The increased bleeding rates observed in elderly patients may be attributable to higher usage of antiplatelet and anticoagulant therapies and a greater prevalence of PAD in this group, findings supported by prior studies[21,23]. Clinicians should remain particularly vigilant when managing elderly patients on these medications or with PAD, as the risk of intraprocedural bleeding is heightened, necessitating preparedness for prompt intervention.
Regarding post-procedural clinical bleeding, our results were consistent with prior reports, with no significant differences observed between patients over 80 and younger patients[10,14,23]. Importantly, we confirmed that the use of anticoagulants, but not antiplatelet agents, and intraprocedural bleeding are independently associated with post-ERCP bleeding, as outlined in ESGE guidelines[4]. Clinicians should be particularly vigilant for post-ERCP bleeding in patients who experience intraprocedural bleeding and should follow guidelines on the management of anticoagulant and antiplatelet therapies prior to ERCP[28].
Our findings are consistent with previous studies indicating no significant difference in the rates of perforation, post-ERCP cholangitis, and cholecystitis among patients over 80[10,14,21,23]. However, we observed a numerically higher rate of post-ERCP cholangitis and, most notably, cholecystitis in patients who received biliary stents, although no significant differences were found when comparing fully covered metallic stents to other types such as plastic pigtail, straight, or uncovered metallic stents. This aligns with recent reports, including a study by Khan et al[29]. Importantly, the rate of post-ERCP cholecystitis associated with fully covered metallic stents in our cohort (1.5%) closely matches the rate reported by Khan et al[29], highlighting the importance of clinician awareness when managing patients with such stents and in situ gallbladder.
Regarding procedural efficacy, our data indicate that successful cannulation rates are similar between elderly and younger patients, consistent with previous studies[12,16,21,22,30]. This may partly be explained by the fact that, despite the increased use of antiplatelet and anticoagulant therapies among elderly patients, our technique, particularly NK sphincterotomy, remained effective. Additionally, although diverticula were more common among elderly patients, they did not significantly impact overall cannulation success. However, in multivariate analysis, the presence of PAD was an independent predictor of unsuccessful cannulation, corroborating previous research suggesting that diverticula can complicate CBD access[30-32]. Meta-analyses have yielded conflicting results: One published in 2019 suggested that PAD decreases cannulation success[33], while another in 2020 found no such correlation[34]. More recently, a meta-analysis concluded that diverticula can affect cannulation success, although this effect was predominantly observed in studies published before 2015[35]. This variation over time likely reflects advancements in ERCP techniques, such as the increased utilization of NK sphincterotomy. Since our cohort includes procedures from up to 20 years ago, these temporal changes may have influenced our findings. For example, although not part of our primary analysis, successful cannulation in patients with PAD was achieved in 88.9% of cases before 2015 and increased to 91.1% after 2015, though this difference was not statistically significant (P = 0.248). Additionally, a recent study suggests that larger diverticula may impact ERCP outcomes, although not all diverticula are detrimental[36]. Unfortunately, in our study, diverticula size was not documented in the standardized data collection, limiting our ability to assess this factor.
Regarding CBD clearance in patients undergoing ERCP for bile duct stones, our data showed that a higher proportion of elderly patients did not achieve complete CBD clearance during their initial ERCP. This aligns with previous findings indicating that the complete stone clearance rate is significantly lower in patients over 80 years old (92.4% vs 99.0%; P < 0.01)[37]. However, our multivariate analysis demonstrated that age itself was not an independent factor; rather, stone size influenced CBD clearance. Larger stones tend to be more difficult to extract, and prior research has confirmed this association[38,39]. Since our results indicate that elderly patients more frequently have stones larger than 15 mm, this naturally explains the lower rates of complete CBD clearance during the first ERCP in this group. Conversely, no significant difference was observed in the success of biliary stent placement between age groups.
In summary, the overall efficacy of initial ERCP, whether aiming for complete CBD clearance or stent placement, is primarily affected by anatomical factors such as the presence of PAD (which are more common in the elderly) or by larger stone size in older patients, rather than by age itself. Endoscopists should consider these age-related anatomical and pathological factors when planning and performing procedures in older patients to optimize outcomes.
This study reflects the experience of a single endoscopist, with all procedures either performed or supervised by one senior clinician. Consequently, our findings may have limited generalizability and could be affected by selection bias. Additionally, as a retrospective analysis, all ERCPs were performed prior to the study’s initiation. Nonetheless, the data were prospectively collected over the years and recorded in a standardized, predefined form, ensuring consistency in data collection.
Certain factors were not initially documented in our data collection forms and could not be analyzed, for example, prior history of pancreatitis, the size of PAD, cannulation of the cystic duct, or the nature of strictures (malignant vs benign or intermediate). Furthermore, detailed assessment of complication severity, beyond hospitalization duration or the need for intervention (endoscopic, percutaneous, or surgical), was limited by these constraints. Since the prophylactic use of NSAIDs or pancreatic stents for PEP prevention is not part of our current practice, we could not evaluate their impact. Similarly, tools used in other studies to assess patient frailty, such as the Elixhauser or Charlson comorbidity indices, were not employed in our analysis. These limitations should be kept in mind when interpreting our results. Finally, no adverse device-related events were explicitly recorded in our dataset. To our knowledge, such events were not documented separately during the observation period, so we cannot provide specific insights regarding device-related complications.
Our study, which includes the largest dataset of patients over 80 years old published to date over the past 20 years, provides reassuring evidence that gastroenterologists and endoscopists can, and should, offer ERCP to elderly patients who need it, “age is just a number”. Being 80 or even 90 years old does not inherently increase the risk of ERCP failure or complications. This is particularly relevant because biliary and pancreatic conditions, such as choledocholithiasis, cholangitis, and pancreaticobiliary tumors causing obstruction, are common in older adults. ERCP often provides definitive therapy, such as stone removal or stenting, which can be life-saving or greatly improve quality of life. Current guidelines from professional societies (American Society for Gastrointestinal Endoscopy, ESGE) do not contraindicate ERCP based on age and cite evidence supporting its safety in the elderly.
Our findings further support that ERCP can be performed safely in older patients, with success and complication rates similar to those seen in younger populations. However, factors like frailty, polypharmacy, and comorbidities, characteristic of many elderly patients, may increase the risk of prolonged hospitalization if complications arise, as reflected by the higher rate of severe complications among patients with elevated ASA scores in our cohort. Endoscopists and clinicians should recognize that while the efficacy of ERCP is not diminished by age, managing potential complications requires heightened vigilance and preparedness.
The data from our study, alongside other research, reinforce current guidelines on ERCP safety and suggest a shift toward evaluating individual patient risk based on biological age, specifically frailty and comorbidities, rather than chronological age alone. Future guidelines could incorporate frailty assessment tools into risk stratification algorithms to better identify patients at higher risk of adverse events. Larger, prospective studies examining the utility of specific frailty measures, such as the Elixhauser or Charlson comorbidity indices, and evaluating the impact of prophylactic strategies in frail patients are necessary to advance guideline development and improve clinical decision-making.
| 1. | Adler DG, Baron TH, Davila RE, Egan J, Hirota WK, Leighton JA, Qureshi W, Rajan E, Zuckerman MJ, Fanelli R, Wheeler-Harbaugh J, Faigel DO; Standards of Practice Committee of American Society for Gastrointestinal Endoscopy. ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas. Gastrointest Endosc. 2005;62:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 291] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 2. | Domagk D, Oppong KW, Aabakken L, Czakó L, Gyökeres T, Manes G, Meier P, Poley JW, Ponchon T, Tringali A, Bellisario C, Minozzi S, Senore C, Bennett C, Bretthauer M, Hassan C, Kaminski MF, Dinis-Ribeiro M, Rees CJ, Spada C, Valori R, Bisschops R, Rutter MD. Performance measures for ERCP and endoscopic ultrasound: a European Society of Gastrointestinal Endoscopy (ESGE) Quality Improvement Initiative. Endoscopy. 2018;50:1116-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 76] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 3. | ASGE Standards of Practice Committee; Chandrasekhara V, Khashab MA, Muthusamy VR, Acosta RD, Agrawal D, Bruining DH, Eloubeidi MA, Fanelli RD, Faulx AL, Gurudu SR, Kothari S, Lightdale JR, Qumseya BJ, Shaukat A, Wang A, Wani SB, Yang J, DeWitt JM. Adverse events associated with ERCP. Gastrointest Endosc. 2017;85:32-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 591] [Article Influence: 65.7] [Reference Citation Analysis (0)] |
| 4. | Dumonceau JM, Kapral C, Aabakken L, Papanikolaou IS, Tringali A, Vanbiervliet G, Beyna T, Dinis-Ribeiro M, Hritz I, Mariani A, Paspatis G, Radaelli F, Lakhtakia S, Veitch AM, van Hooft JE. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2020;52:127-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 707] [Cited by in RCA: 591] [Article Influence: 98.5] [Reference Citation Analysis (1)] |
| 5. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1890] [Cited by in RCA: 2086] [Article Influence: 59.6] [Reference Citation Analysis (2)] |
| 6. | GBD 2021 Europe Life Expectancy Collaborators. Changing life expectancy in European countries 1990-2021: a subanalysis of causes and risk factors from the Global Burden of Disease Study 2021. Lancet Public Health. 2025;10:e172-e188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 22] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 7. | Santos-Eggimann B, Cuénoud P, Spagnoli J, Junod J. Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. J Gerontol A Biol Sci Med Sci. 2009;64:675-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 557] [Cited by in RCA: 634] [Article Influence: 37.3] [Reference Citation Analysis (0)] |
| 8. | Pazan F, Wehling M. Polypharmacy in older adults: a narrative review of definitions, epidemiology and consequences. Eur Geriatr Med. 2021;12:443-452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 274] [Article Influence: 54.8] [Reference Citation Analysis (0)] |
| 9. | Baykan AR, Cerrah S, Çiftel S, Karahan B, Özdemir Y. Safety of endoscopic retrograde cholangiopancreatography (ERCP) in patients aged 85 years and older: A single center experience. Turk J Surg. 2021;37:162-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Finkelmeier F, Tal A, Ajouaou M, Filmann N, Zeuzem S, Waidmann O, Albert J. ERCP in elderly patients: increased risk of sedation adverse events but low frequency of post-ERCP pancreatitis. Gastrointest Endosc. 2015;82:1051-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 11. | Day LW, Lin L, Somsouk M. Adverse events in older patients undergoing ERCP: a systematic review and meta-analysis. Endosc Int Open. 2014;2:E28-E36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 12. | Galeazzi M, Mazzola P, Valcarcel B, Bellelli G, Dinelli M, Pasinetti GM, Annoni G. Endoscopic retrograde cholangiopancreatography in the elderly: results of a retrospective study and a geriatricians' point of view. BMC Gastroenterol. 2018;18:38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 13. | Colmenero Gargari AE, Melgar Somoza FE, Vera J, Micames CG. ERCP in patients over 90 years old: Safety and efficacy comparison with a younger cohort. Endosc Int Open. 2023;11:E893-E898. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 14. | Basida SD, Dahiya DS, Yousaf MN, Basida B, Pinnam BSM, Gangwani MK, Ali H, Singh S, Shah YR, Ahluwalia D, Shah MP, Chandan S, Sharma NR, Thakkar S. Impact of frailty on endoscopic retrograde cholangiopancreatography outcomes in nonagenarians: A United States national experience. World J Gastrointest Endosc. 2024;16:148-156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 15. | Iqbal U, Anwar H, Khan MA, Weissman S, Kothari ST, Kothari TH, Confer BD, Khara HS. Safety and Efficacy of Endoscopic Retrograde Cholangiopancreatography in Nonagenarians: A Systematic Review and Meta-Analysis. Dig Dis Sci. 2022;67:1352-1361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Kiriyama S, Kozaka K, Takada T, Strasberg SM, Pitt HA, Gabata T, Hata J, Liau KH, Miura F, Horiguchi A, Liu KH, Su CH, Wada K, Jagannath P, Itoi T, Gouma DJ, Mori Y, Mukai S, Giménez ME, Huang WS, Kim MH, Okamoto K, Belli G, Dervenis C, Chan ACW, Lau WY, Endo I, Gomi H, Yoshida M, Mayumi T, Baron TH, de Santibañes E, Teoh AYB, Hwang TL, Ker CG, Chen MF, Han HS, Yoon YS, Choi IS, Yoon DS, Higuchi R, Kitano S, Inomata M, Deziel DJ, Jonas E, Hirata K, Sumiyama Y, Inui K, Yamamoto M. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25:17-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 468] [Cited by in RCA: 487] [Article Influence: 60.9] [Reference Citation Analysis (0)] |
| 17. | Yokoe M, Hata J, Takada T, Strasberg SM, Asbun HJ, Wakabayashi G, Kozaka K, Endo I, Deziel DJ, Miura F, Okamoto K, Hwang TL, Huang WS, Ker CG, Chen MF, Han HS, Yoon YS, Choi IS, Yoon DS, Noguchi Y, Shikata S, Ukai T, Higuchi R, Gabata T, Mori Y, Iwashita Y, Hibi T, Jagannath P, Jonas E, Liau KH, Dervenis C, Gouma DJ, Cherqui D, Belli G, Garden OJ, Giménez ME, de Santibañes E, Suzuki K, Umezawa A, Supe AN, Pitt HA, Singh H, Chan ACW, Lau WY, Teoh AYB, Honda G, Sugioka A, Asai K, Gomi H, Itoi T, Kiriyama S, Yoshida M, Mayumi T, Matsumura N, Tokumura H, Kitano S, Hirata K, Inui K, Sumiyama Y, Yamamoto M. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25:41-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 769] [Cited by in RCA: 782] [Article Influence: 97.8] [Reference Citation Analysis (0)] |
| 18. | Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, Pilotto A, Forlano R. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007;102:1781-1788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 669] [Cited by in RCA: 802] [Article Influence: 42.2] [Reference Citation Analysis (0)] |
| 19. | Fujita K, Yazumi S, Matsumoto H, Asada M, Nebiki H, Matsumoto K, Maruo T, Takenaka M, Tomoda T, Onoyama T, Kurita A, Ueki T, Katayama T, Kawamura T, Kawamoto H; Bilio-pancreatic Study Group of West Japan. Multicenter prospective cohort study of adverse events associated with biliary endoscopic retrograde cholangiopancreatography: Incidence of adverse events and preventive measures for post-endoscopic retrograde cholangiopancreatography pancreatitis. Dig Endosc. 2022;34:1198-1204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 20. | Dahale AS, Gupta M, Saxena P, Kumar A, Sonika U, Kumar M, Srivastava S, Sachdeva S, Sharma BC, Puri AS, Dalal A. Endoscopic retrograde cholangiopancreaticography-related complications - Experience from tertiary care teaching centre over half a decade. J Minim Access Surg. 2022;18:526-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 21. | Han SJ, Lee TH, Kang BI, Choi HJ, Lee YN, Cha SW, Moon JH, Cho YD, Park SH, Kim SJ. Efficacy and Safety of Therapeutic Endoscopic Retrograde Cholangiopancreatography in the Elderly Over 80 Years. Dig Dis Sci. 2016;61:2094-2101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Fritz E, Kirchgatterer A, Hubner D, Aschl G, Hinterreiter M, Stadler B, Knoflach P. ERCP is safe and effective in patients 80 years of age and older compared with younger patients. Gastrointest Endosc. 2006;64:899-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 81] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 23. | Kanamori A, Kiriyama S, Tanikawa M, Hisanaga Y, Toyoda H, Tada T, Kitabatake S, Kaneoka Y, Maeda A, Kumada T. Long- and short-term outcomes of ERCP for bile duct stones in patients over 80 years old compared to younger patients: a propensity score analysis. Endosc Int Open. 2016;4:E83-E90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Ergin E, Oruç N, Ersöz G, Tekeşin O, Özütemiz Ö. Prognosis and risk factors of ERCP pancreatitis in elderly. Sci Rep. 2021;11:15930. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 25. | Frank CD, Adler DG. Post-ERCP pancreatitis and its prevention. Nat Clin Pract Gastroenterol Hepatol. 2006;3:680-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Deans GT, Sedman P, Martin DF, Royston CM, Leow CK, Thomas WE, Brough WA. Are complications of endoscopic sphincterotomy age related? Gut. 1997;41:545-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Köklü S, Parlak E, Yüksel O, Sahin B. Endoscopic retrograde cholangiopancreatography in the elderly: a prospective and comparative study. Age Ageing. 2005;34:572-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 28. | Veitch AM, Radaelli F, Alikhan R, Dumonceau JM, Eaton D, Jerrome J, Lester W, Nylander D, Thoufeeq M, Vanbiervliet G, Wilkinson JR, Van Hooft JE. Endoscopy in patients on antiplatelet or anticoagulant therapy: British Society of Gastroenterology (BSG) and European Society of Gastrointestinal Endoscopy (ESGE) guideline update. Gut. 2021;70:1611-1628. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 129] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 29. | Khan R, Osman H, Lee S, Chen YI, Singh A, Hookey L, Arya N, Causada Calo N, Grover SC, Tepox-Padrón A, Bass S, Cole M, Lei Y, Li S, Mohamed R, Turbide C, Koury HF, Chau M, Howarth M, Cartwright S, Heitman SJ, Forbes N. Post-ERCP cholecystitis: Incidence, characteristics, and outcomes from a prospective multicenter biliary endoscopy registry. Gastrointest Endosc. 2024;99:633-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 30. | Yang JH, Li W, Si XK, Zhang JX, Cao YJ. Efficacy and Safety of Therapeutic ERCP in the Elderly: A Single Center Experience. Surg Laparosc Endosc Percutan Tech. 2018;28:e44-e48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 31. | Tohda G, Ohtani M, Dochin M. Efficacy and safety of emergency endoscopic retrograde cholangiopancreatography for acute cholangitis in the elderly. World J Gastroenterol. 2016;22:8382-8388. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 31] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 32. | Karaahmet F, Kekilli M. The presence of periampullary diverticulum increased the complications of endoscopic retrograde cholangiopancreatography. Eur J Gastroenterol Hepatol. 2018;30:1009-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 33. | Jayaraj M, Mohan BP, Dhindsa BS, Mashiana HS, Radhakrishnan G, Dhir V, Trindade AJ, Adler DG. Periampullary Diverticula and ERCP Outcomes: A Systematic Review and Meta-Analysis. Dig Dis Sci. 2019;64:1364-1376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 34. | Mu P, Yue P, Li F, Lin Y, Liu Y, Meng W, Zhou W, Li X. Does periampullary diverticulum affect ERCP cannulation and post-procedure complications? an up-to-date meta-analysis. Turk J Gastroenterol. 2020;31:193-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 35. | Xie XX, Li X, Chen YH, Geng C, Wang CH. Impact of periampullary diverticula on the rates of successful cannulation and ERCP complications: An up-to-date systematic review and meta-analysis. J Dig Dis. 2024;25:573-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 36. | Cagir Y, Durak MB, Simsek C, Yuksel I. Effect of periampullary diverticulum morphology on ERCP cannulation and clinical results. Scand J Gastroenterol. 2025;60:292-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 37. | Obana T, Fujita N, Noda Y, Kobayashi G, Ito K, Horaguchi J, Koshita S, Kanno Y, Yamashita Y, Kato Y, Ogawa T. Efficacy and safety of therapeutic ERCP for the elderly with choledocholithiasis: comparison with younger patients. Intern Med. 2010;49:1935-1941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 38. | Wongkanong C, Patumanond J, Ratanachu-Ek T, Junrungsee S, Tantraworasin A. Common bile duct stone-related parameters and their potential prognostic values for stone extraction requiring endoscopic papillary large balloon dilation. JGH Open. 2023;7:16-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 39. | Wongkanong C, Patumanond J, Ratanachu-Ek T, Junrungsee S, Tantraworasin A. Development of clinical prediction rule for the requirement of endoscopic papillary large balloon dilation (EPLBD) on endoscopic CBD stone clearance. PLoS One. 2023;18:e0282899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/