Published online Sep 28, 2025. doi: 10.3748/wjg.v31.i36.110583
Revised: July 15, 2025
Accepted: August 27, 2025
Published online: September 28, 2025
Processing time: 101 Days and 0.2 Hours
Although gastroscopy is a commonly used diagnostic and therapeutic technique, postoperative gastrointestinal dysfunction is prone to occur. Traditional Chinese medicine theory suggests that postoperative gastrointestinal disorders are related to spleen and stomach weakness. This study hypothesizes that the combination of acupoint application at the Ziwu Liuzhu acupoint and percutaneous acupoint electrical stimulation can promote postoperative gastrointestinal function recovery and alleviate stress reactions.
To investigate the effects of acupoint application of Ziwu Liuzhu combined with percutaneous acupoint electrical stimulation on postoperative gastrointestinal function recovery and stress response in patients undergoing gastrointestinal endoscopy surgery.
A total of 120 patients who underwent gastroscopy surgery were selected and treated between October 2024 and January 2025. This study used a stratified block randomization method, and then allocated groups using computer-generated random number sequences (SAS 9.4 software). The groups were divided into two groups: A control group of 60 patients who received routine postoperative intervention measures, and an observation group of 60 patients who received acupuncture point application combined with transcutaneous acupoint electrical stimulation therapy. The therapeutic effects were compared after 3 days of treatment.
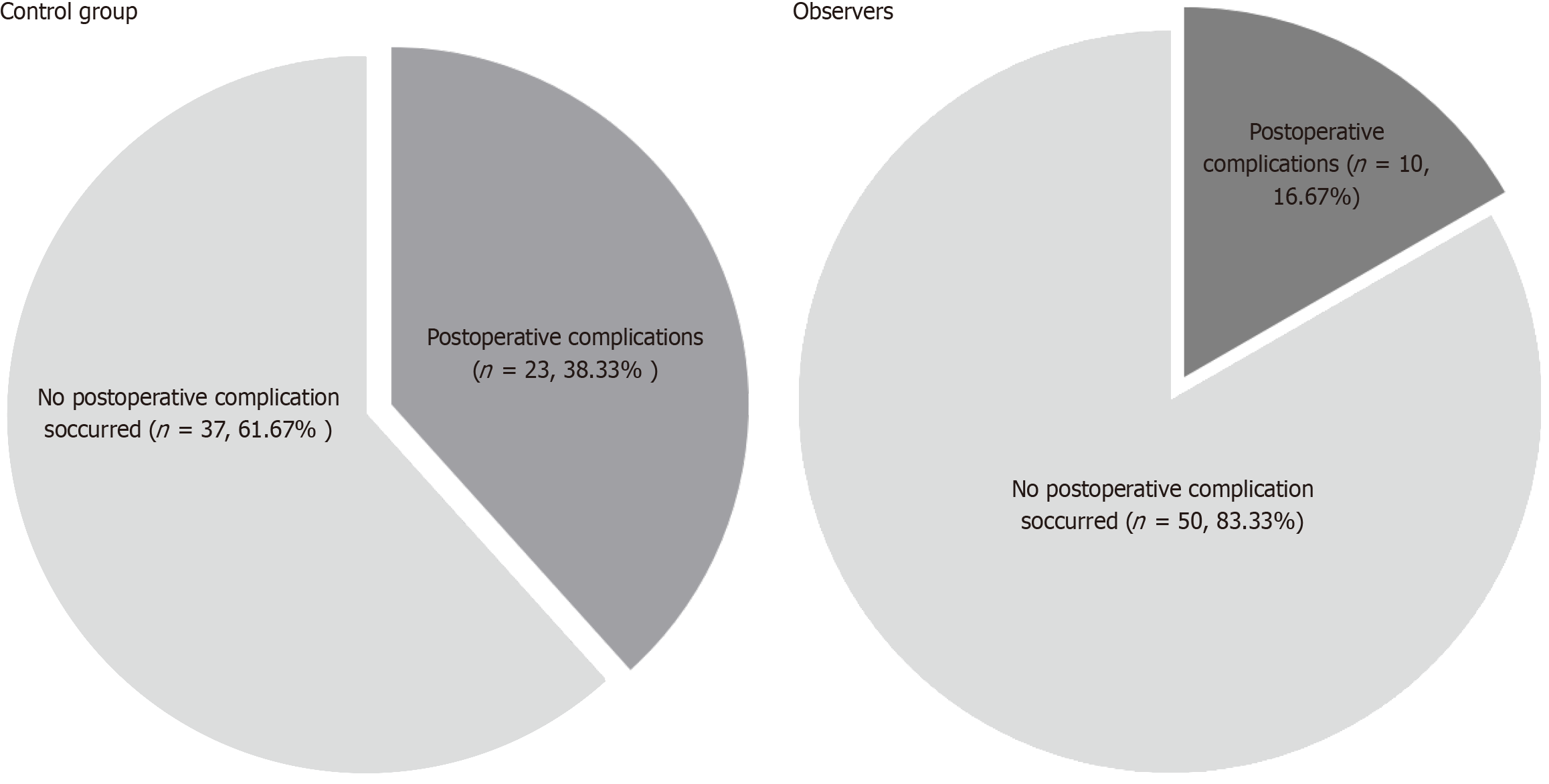
The mean time of first defecation was 3.20 ± 1.04 days, the mean first eating time was 2.55 ± 0.72 days, and the mean length of hospital stay was 5.57 ± 0.09 days (P < 0.05) after treatment. Gastrin levels were found to be (161.15 ± 16.75) pg/mL, norepinephrine (125.53 ± 17.78) pg/mL, cortisol (142.16 ± 19.55) μg/L, aldosterone (51.14 ± 5.39) pg/mL demonstrated superiority in comparison to the control group (P < 0.05). Conversely, the observation group exhibited superior outcomes, with an 93.33% success rate as opposed to the control group's 75.00%, and an overall satisfaction rate of 91.67% as compared to the control group's 68.33%. Moreover, the postoperative complication rate in the observation group was 16.67%, significantly lower than the 38.33% rate observed in the control group (P < 0.05).
The combination of percutaneous acupoint electrical stimulation in gastroscopy patients has been demonstrated to be both highly safe and effective. The benefits of this approach include the promotion of postoperative gastrointestinal function, the reduction of stress response, the attainment of optimal results, and the enhancement of patient satisfaction.
Core Tip: The article focuses on the application effect of Meridian flow injection acupoint application combined with transcutaneous acupoint electrical stimulation (TAES) in patients undergoing gastroenteroscopic surgery. When compared with conventional postoperative interventions, it was found that Meridian flow injection acupoint application combined with TAES could significantly shorten the time to first bowel movement, feeding time and hospital stay, improve gastrointestinal hormone levels, reduce stress response, improve patient satisfaction and reduce the incidence of complications. The trial confirmed the safety and efficacy of this combination therapy.
- Citation: Hong X, Wu XY, Xu QL. Application of Meridian flow injection acupoint application combined with transcutaneous electrical acupoint stimulation in patients undergoing gastroenteroscopy. World J Gastroenterol 2025; 31(36): 110583
- URL: https://www.wjgnet.com/1007-9327/full/v31/i36/110583.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i36.110583
Gastroenteroscopy is a diagnostic and therapeutic technology that is frequently employed in clinical practice. Despite the remarkable efficacy of this technology, as evidenced by the increasing volume of related research[1], scholars have identified several postoperative complications in patients who have undergone gastroenteroscopy surgery. These include vomiting, nausea, abdominal distension, anorexia, delayed defecation, and the disappearance or weakening of intestinal sounds. The symptoms described herein result in transient motor dysfunction of the gastrointestinal tract, prolonged hospitalisation and an adverse effect on prognosis. Thus, the current focus of research is on the promotion of recovery of gastrointestinal tract function after surgery[2].
Conventional Western medicine has been demonstrated to alleviate symptoms, but the overall efficacy of this approach is not optimal. From the perspective of Chinese medicine, postoperative gastrointestinal disorders are classified as 'intestinal paralysis' or 'intestinal knot', primarily resulting from deficiencies in the spleen and stomach, innate endowment insufficiency, gastrointestinal chemotaxis and disharmony, and flatulence[3]. The theoretical foundation of traditional Chinese medicine (TCM) is predicated on the holistic concept that the various internal organs interact with one another, frequently through the utilisation of specific TCM technologies, with the objective of regulating the gastrointestinal tract, peristalsis, qi, and blood circulation[4].
Acupressure is a simple, non-invasive, cost-effective Chinese medicine technology that can promote the operation of qi and blood, harmonise the functions of the internal organs, and help the spleen and stomach return to normal physiological function[5]. Meridian flow injection acupoint application is a novel application theory that has emerged in recent years. The Meridian flow note is an explanation of the human body's life phenomenon from the perspective of time. It provides an explanation of the twelve Meridians and blood flow. Stimulating the Meridians and blood flow in a specific manner is the most vigorous form of acupuncture. This can improve the operation of the Meridians and achieve the purpose of activating them and regulating the internal organs[6]. Transcutaneous electrical acupoint stimulation (TEAS) and electroacupuncture, which bears similarity to electroacupuncture in terms of mechanism, yet differs in that it combines acupuncture points with nerve electrical stimulation, has been shown to be a more straightforward procedure that is also safe and non-invasive. In addition, it exhibits minimal physiological interference and a number of other advantages. It has been demonstrated that this method can regulate the stability of the internal environment and reduce the inflammatory response, thus aligning with the characteristics of the two-way regulation[7]. However, at present, clinical reports on Meridian flow injection acupoint placement combined with transcutaneous acupoint electrical stimulation are relatively few, and the effect is still in the exploratory stage. The present study built upon this foundation, undertaking a detailed analysis of the benefits afforded by this combination, and its impact on the postoperative recovery of patients subjected to gastroenteroscopic surgery. The objective of this analysis was to furnish a scientific foundation for the prospective enhancement of treatment protocols.
Through previous pre-experiments, the difference in first defecation time between the two groups was 0.8 days (3.98 ± 1.12 days vs 3.20 ± 1.04 days). The test power was set (1 - β) = 0.8, and the significance level α = 0.05 (two-sided test). The sample size of two independent samples t-test was estimated through PASS 15 software. The calculation showed that 54 cases were needed in each group to detect the difference between the groups. After considering the 10% dropout rate, 120 cases (60 cases in each group) were finally included. This sample size ensured detection of a medium effect size of 0.7 SD (Cohen's d = 0.7), meeting the minimum important difference criterion for clinical research. Based on this, a total of 120 patients who underwent gastroenteroscopy between October 2024 and January 2025 were selected for this study, of whom 65 were male and 55 were female, with a mean age of (56.13 ± 12.64) years, an average body weight of (59.86 ± 6.33) kg, an average operative time of (54.64 ± 5.83) minutes, and a diagnosis of: Gastric lesions in 76 cases, and colorectal lesions in 27 cases, and oesophageal lesions in 17 cases. They were divided into 2 groups according to the random number table method. This study adopted a stratified block randomization method, and then allocated groups through a computer-generated random number sequence (SAS 9.4 software) and divided them into 2 groups. The random allocation plan was generated by an independent statistician and sealed in an opaque envelope. A third-party nurse opened the envelope immediately after surgery to determine the grouping to ensure that the allocation was concealed. The study complied with the ethical review of the Declaration of Helsinki, approved by Zhejiang Provincial People's Hospital Ethics Review 2024 Research, No. 235.
Inclusion criteria: (1) Age 18-70 years; (2) Benign polypoid changes, precancerous lesions or carcinoma in situ in the gastrointestinal tract confirmed by examination; (3) Surgeries were performed under intravenous general anaesthesia or tracheal intubation general anaesthesia and anaesthesia criteria of American Society of Anaesthesiologists grade I-III; (4) No history of gastrointestinal surgery; and (5) No communication barriers and informed consent.
Exclusion criteria: (1) Have taken medications that affect gastrointestinal motility; (2) Skin infection, breakage, redness of acupuncture points; (3) Those with combined coagulation disorders, neurological diseases, severe cardiovascular diseases or implanted pacemakers; (4) Those with a history of gastrointestinal surgery or other gastrointestinal diseases; (5) Those with opioid addiction or dependence; and (6) Those who are pregnant or breastfeeding, or those with combined psychiatric disorders.
The control group would undergo the conventional postoperative intervention. In the context of tracheal general anaesthesia, the urinary catheter was removed either six hours or the following day after the operation. Moreover, patients were encouraged to move around as soon as possible. For patients undergoing transoral small enteroscopy and gastric mucosal dissection surgery for early gastric cancer, it is necessary to prolong the retention time of the gastric tube, usually 1-3 days. The bleeding situation must be observed and the patient must be kept fasting for 48-72 hours. Following the resumption of diet, a gradual transition from fluid to solid food is required. Commencing from the first postoperative day, acupoint plastering was administered to Shenque, Zhongkou, Tianshu, and Shusanli, with the group formula comprising Qingpi, Houpu, and raw rhubarb, which were proportionally modulated. The formula was then transformed into a medicinal ointment, with the addition of Huangjiu, and administered four times per day for three consecutive days. This was accompanied by clockwise abdominal massage, two times per day, with each session comprising 20-30 Laps. Observation group in the control group on the basis of joint Meridian flow injection acupoints paste treatment, according to the Meridian flow injection points, opening and closing time, formula preparation: Qingpi, thick park, raw rhubarb according to the ratio of 2:2:1 grinding, plus yellow wine modulation into a thick paste, each paste contains 0.3 g/cm², made of 3 cm × 3 cm paste. Hour selection basis: According to the theory of Meridian flow injection, the spleen Meridian seasonal hour for the Si time (9:00-11:00), this time the spleen Meridian qi and blood is the most prosperous, stimulate the Shenque (Ren vein), in the epigastric (stomach collection point), the center of the sky (intestinal collection point), foot Sanli (joint point) can maximize “cultivate the earth to generate gold” effect. Stomach Meridian seasonal time for the hour (7:00-9:00), double hour stimulation in line with the “spleen rise stomach fall” physiological characteristics, combined with bilateral foot Sanli percutaneous acupoint electrical stimulation, the use of QX265-type therapeutic instrument, bilateral foot Sanli input symmetrical biphasic square wave, frequency 2/100 Hz alternating, the current intensity from 1 mA incremental to the patient's tolerance threshold (an average of 3.5 ± 0.8 mA), each time! Each treatment consisted of 5 minutes of basic stimulation + 25 minutes of rhythmic modulation, the treatment time was 30 minutes. the current was gradually transitioned from weak to strong, until the patient felt an obvious sense of tremor in the local area, and the treatment was continuous for 3 days.
The following three observation indicators were considered: (1) A comparison of the two groups in terms of the time taken for intestinal sound recovery, the time of first defecation, the time of first food intake, and the duration of hospitalization; (2) A comparison of the two groups in terms of gastrointestinal hormone index levels, measured before treatment, after treatment after three days, and after the extraction of 5 mL of blood from the elbow vein in a fasting state (8 a.m.), with gastrin detection; (3) In order to compare the two groups of satisfaction, the utilisation of this hospital's homemade questionnaire was employed. The investigation focused on the patient's treatment effect, service attitude and other satisfaction. The following scale was used to measure satisfaction: Very satisfied (100 points), satisfied (80-99 points), general (60-79 points), dissatisfied (0-60 points). The total satisfaction rate was calculated as the sum of the very satisfied and satisfied rates; (4) Prior to and three days following the treatment, 3 mL of elbow vein blood from the examinees in a fasting state (8 a.m.) was drawn. The norepinephrine, cortisol and aldosterone levels were then tested; and (5) The incidence of postoperative complications were compared between the two groups.
An excellent rate was defined as an excellent rate in conjunction with a good rate. Postoperative outcomes are categorised as follows: (1) Excellent: Return of normal bowel sounds within one day of surgery, with no complications, fever or discomfort after resumption of eating or drinking; (2) Good: Defecation within two days of resumption of eating after surgery, mild abdominal distension, weakened bowel sounds, reflux and acid reflux symptoms after eating or drinking, which can be alleviated by bedside activities or self-massage of the abdomen, and low-grade fever; and (3) Poor: Postoperative complications, including but not limited to hyperthermia, bleeding, and perforation, as well as bowel sounds of 0-2 beats per minute, still require fasting, gastrointestinal decompression, and abdominal distension is obvious after drinking water or no bowel movement after resumption of food for > 2 days[8].
The statistical analysis of the data was conducted using SPSS 22.0 software. The count data were expressed as a percentage [n (%)] and the χ2 test was employed. The measurement data were expressed as (mean ± SD) and an independent sample t-test was used to analyse these. A P value of < 0.05 indicated a statistically significant difference.
The results of the study revealed no statistically significant differences between the two groups with regard to gender, age, weight, operation time, and disease diagnosis (P > 0.05; Table 1).
| Group | n | Gender | Age (years) | Weight (kg) | Operation time (minute) | Disease diagnosis | ||||
| Male | Female | Gastric lesions | Colorectal lesions | Esophageal lesions | ||||||
| Observation group | 60 | 37 (61.67) | 23 (38.33) | 56.93 ± 11.88 | 59.98 ± 6.35 | 54.85 ± 6.66 | 36 (60.00) | 13 (21.67) | 11 (18.33) | |
| Control group | 60 | 28 (46.67) | 32 (53.33) | 55.85 ± 12.89 | 59.70 ± 6.38 | 55.42 ± 5.41 | 40 (66.67) | 14 (23.33) | 6 (10.00) | |
| χ2/t | - | 2.719 | 0.479 | 0.244 | 0.512 | 1.718 | ||||
| P value | - | 0.099 | 0.633 | 0.808 | 0.610 | 0.424 | ||||
There was no statistically significant difference between the two groups with respect to the time of recovery of bowel sounds and the time of first defecation (P > 0.05). Furthermore, the first bowel movement, first feeding time and hospitalisation time of the observation group were shorter than that of the control group (P < 0.05; Table 2).
| Group | n | Recovery of bowel sounds | The time of first defecation | The first bowel movement | First feeding time | Hospitalisation time |
| Observation group | 60 | 1.55 ± 0.57 | 1.87 ± 0.50 | 3.20 ± 1.04 | 2.55 ± 0.72 | 5.57 ± 0.89 |
| Control group | 60 | 1.65 ± 0.52 | 1.93 ± 0.36 | 3.98 ± 1.27 | 2.96 ± 0.82 | 6.30 ± 1.45 |
| t | - | 1.013 | 0.833 | 3.701 | 2.894 | 3.333 |
| P value | - | 0.313 | 0.406 | 0.001 | 0.005 | 0.001 |
Prior to the commencement of treatment, no statistically significant disparities in gastrin levels were observed between the two groups (P > 0.05). However, subsequent to the treatment, the observation group exhibited a more pronounced improvement in gastrin levels in comparison to the control group (P < 0.05; Table 3).
| Group | n | Gastrin (pg/mL) | |
| Before treatment | After 3 days of treatment | ||
| Observers | 60 | 241.65 ± 25.61 | 161.15 ± 16.75 |
| Control group | 60 | 240.86 ± 26.84 | 205.33 ± 18.64 |
| t | - | 0.165 | 13.655 |
| P value | - | 0.869 | < 0.001 |
The excellent rate of the observation group was found to be higher than that of the control group (P < 0.05; Table 4).
| Group | n | Excellent | Good | Poor | Excellent rate |
| Observation group | 60 | 40 (66.67) | 16 (26.67) | 4 (6.67) | 56 (93.33) |
| Control group | 60 | 30 (50.00) | 15 (25.00) | 15 (25.00) | 45 (75.00) |
| χ2 | - | 7.566 | |||
| P value | - | 0.006 |
The total satisfaction rate of patients in the observation group was higher than that of the control group (P < 0.05; Table 5).
| Group | n | Very satisfied | Satisfied | Generally dissatisfied | Unsatisfied | Overall satisfaction rate |
| Observation group | 60 | 32 (53.33) | 23 (38.33) | 5 (8.33) | 0 (0.00) | 55 (91.67) |
| Control group | 60 | 25 (41.67) | 16 (26.67) | 18 (30) | 1 (1.67) | 41 (68.33) |
| χ2 | - | 10.208 | ||||
| P value | - | 0.001 |
Prior to treatment, there was no statistically significant difference in stress reaction levels between the two groups (P > 0.05). Subsequent to treatment, the norepinephrine, cortisol and aldosterone levels of the observations made in the observation group were lower than those of the control group on the 3rd day after treatment (P > 0.05; Table 6).
| Group | n | Norepinephrine (pg/mL) | Cortisol (μg/L) | Aldosterone (pg/mL) | |||
| Before treatment | After 3 days of treatment | Before treatment | After 3 days of treatment | Before treatment | After 3 days of treatment | ||
| Observation group | 60 | 256.64 ± 23.32 | 125.53 ± 17.78 | 275.32 ± 32.65 | 142.16 ± 19.55 | 68.64 ± 9.61 | 51.14 ± 5.39 |
| Control group | 60 | 256.79 ± 23.41 | 176.33 ± 19.85 | 275.76 ± 32.48 | 196.08 ± 17.44 | 68.71 ± 9.22 | 68.83 ± 4.47 |
| t | - | 0.035 | 14.766 | 0.074 | 15.942 | 0.041 | 19.569 |
| P value | - | 0.972 | < 0.001 | 0.941 | < 0.001 | 0.968 | < 0.001 |
In the observation group, there were 4 cases of fever, 5 cases of abdominal distension and nausea, 0 cases of perforation, and 1 case of haemorrhage in the postoperative period, totalling 16.67% (10/60); in the control group, there were 8 cases of fever, 10 cases of abdominal distension and nausea, 2 cases of perforation (including intraoperative), and 3 cases of haemorrhage in the postoperative period, totalling 38.33% (23/60). There was a statistical difference between the two groups comparing postoperative complications (χ2 = 7.064, P = 0.008; Figure 1).
Gastroenteroscopy is indicated for a wide range of abdominal diseases and has become the preferred option for a wide range of such diseases as the surgical modality continues to be refined and improved. Despite the notable efficacy of this approach, post-surgical signs of gastrointestinal dysfunction have been observed in some patients[9]. The rationale behind this is that gastroenteroscopic surgery necessitates the utilisation of intra-abdominal pressure machinery, which leads to a reduction in the patient's gastric blood flow and compression of the capillary bed of the gastrointestinal tract. This, in turn, results in oedema and stasis within the gastrointestinal tract, thereby inhibiting gastrointestinal motility. Concurrently, intraoperative absorption of carbon dioxide from the peritoneum will excite the sympathetic nerves of the body, producing hypercapnia and acidosis. These, in turn, inhibit the excitation of neurons in the gastrointestinal plexus and gastrointestinal motility. Prolonged pneumoperitoneum has been demonstrated to exert a pull on and stimulate the vagus nerve endings, thereby altering the vagus nerve tone and exerting an effect on gastrointestinal function. It is imperative to address this issue promptly to ensure optimal postoperative recovery for the patient. A primary focus should be placed on the recovery of the patient's postoperative gastrointestinal function[10,11].
In the context of TCM, postoperative gastrointestinal impairment falls within the diagnostic category of 'depression' and 'abdominal pain'. These symptoms can arise due to a variety of factors, including spleen dysfunction and the reversal of yin and yang. The liver's loss of excretion, and the lack of ascension of clear Yang, result in loss of moistening. This, in turn, leads to weakness of the spleen and stomach, and abdominal organ qi rebellion. These factors contribute to abnormalities in the function of the stomach and intestines[12,13]. This has been demonstrated to result in gastrointestinal disorders, including dyspepsia, abdominal pain, abdominal distension and other gastrointestinal symptoms. As the etiology of abdominal pain is multifactorial, the operation of Meridian qi is disrupted in a variety of ways, and the disrupted Meridian qi should be adjusted according to the theory of the correspondence between heaven and man[14]. Abdominal pain is located in the intestinal tract. The disease is prolonged and the kidneys are affected. The onset of the disease is mostly related to the liver and spleen, and also associated with the brain and heart. There is no unified identification and typing, but the liver depression and spleen deficiency type is common.
The results of this study showed that gastrin improved in both groups after treatment compared with the pre-intervention period in the same group, which may be related to the enhancement of the release of acetylcholine and vasoactive intestinal peptide from the mesenteric plexus of the enteric nervous system induced by electroacupuncture stimulation[15]. Meanwhile, the findings of this study demonstrated that the observation group exhibited reduced defecation time, time to eat, and hospitalisation time when compared to the control group. Additionally, the excellent rate observed in the observation group surpassed that of the control group, and the improvement in gastrin levels was more pronounced in the third day following treatment. The present study indicates that the combination of Meridian flow injection acupoint application with transcutaneous acupoint electrical stimulation (TAES) has a significant advantage in improving gastrointestinal function in the postoperative period. This is beneficial to the regulation of gastrointestinal function and contributes to recovery[16], there appears to be a high level of consistency. Trace something to its cause, on the one hand, from the analysis of modern medical mechanisms, the efficacy of TEAS may be realized through dual neural-humoral regulation. Transcutaneous electrical stimulation regulates neuronal activity in the dorsal nucleus of the vagus nerve by activating the Aδ and C class afferent fibers in the area of the foot-sanli acupoints, and the signals are uploaded to the nucleus of the solitary tract via the dorsal horn of the spinal cord. The rationale behind this phenomenon pertains to the manifestation of Meridian flow injection acupoint application in the original points of the twelve Meridians and the five acupoints. The selection of acupoints for acupuncture is undertaken under the condition of time, in accordance with the law of cyclical opening and closing. The selection of acupoints that are full of qi and blood and open as a grouping serves to regulate the endocrine secretion of the body and the autonomic nervous system activity. The application of acupoints to the main acupoints of Shenque, Zhongkou, Tianshu, and Shusanli facilitates direct application of the medication to the acupoints, thereby preserving the more effective components of the medication and preventing decomposition and destruction of the medication components by digestive fluids, digestive enzymes, and the liver during internal administration[17]. Conversely, traditional medicine is predicated on the premise that the body's Meridian qi is characterised by unevenness. It is further postulated that Meridian damage is the primary causative agent of gastrointestinal dysfunction. Consequently, therapeutic interventions are theorised to be most efficacious when directed towards the dredging of Meridian qi and blood. Transcutaneous electrical acupoint stimulation has been demonstrated to enhance gastrointestinal blood perfusion, activate blood circulation, and prevent gastrointestinal dysfunction caused by ischemia and hypoxia by stimulating the corresponding acupoints. The foot Sanli, Tianshu, Zhongshu and Shenque points have been identified as the primary acupuncture points for the treatment of gastrointestinal dysfunction. Of these, the Shenque point is located within the Ren vein, and its function is believed to be the regulation of the intestines, the strengthening of the spleen and the stomach. It is widely accepted that both Tianshu and Zhongshu points are associated with the Ren vein. The primary function of the Ren vein is believed to be the warming of the middle and the tonification of emptiness. It is also understood to harmonise with the stomach and strengthen the spleen, as well as to dredge the liver to nourish the stomach and eliminate the stagnation of food and digestion. Foot Sanli is associated with the foot Yangming stomach Meridian, which is believed to have the function of tonifying the middle and benefiting the qi, supporting the correctness of the body to expel evil spirits, dredging the Meridian and regulating the spleen and stomach. When evaluated from the standpoint of contemporary medical theory, the application of Meridian flow injection acupoint application has been shown to induce a softening of the pylorus, regulate the functional state of gastrointestinal smooth muscle, reduce the tension of pyloric smooth muscle, enhance gastric dynamics, and promote gastric emptying[18,19]. TAES has been demonstrated to elicit excitatory responses in the vagus nerve, which in turn regulates gastrointestinal secretion function, enhances gastric tone, promotes gastrointestinal smooth muscle excitation, accelerates gastrointestinal peristalsis, alleviates gastrointestinal injuries, and facilitates exhaustion, thereby restoring gastrointestinal function[20].
As demonstrated in some studies, surgery, as a potent stressor, instigates the body's stress response, stimulates the excitation of the sympathetic nervous system, releases norepinephrine, and elevates aldosterone, thereby exerting a certain impact on postoperative recovery. While analyzing the present results, both groups showed better improvement in postoperative stress response after treatment than before intervention in the same group, which was consistent with the mechanism that electrical stimulation activates the solitary tract nucleus-medullary vagal complex pathway and inhibits excessive activation of the hypothalamic-pituitary-adrenal axis. The improvement of norepinephrine, cortisol, and aldosterone in the observation group was better than that in the control group 3 days after treatment. According to the principles of TCM, the application of Meridian flow injection acupoint application can promote the flow of qi and blood, regulate the function of internal organs, and thus improve the stress state of the organism by conforming to the physiological rhythm of qi and blood circulation in the human body. This process involves the stimulation of local acupoints and Meridian conduction. Acupoint application can regulate the nutritional balance of the organism and affect the excitatory parasympathetic function. The application of acupoints has been demonstrated to regulate the nutritional balance of the body, affect the excitation of parasympathetic nerves and inhibit nerve excitation[21]. TAES has been demonstrated to be a viable therapeutic modality for the management of stress-related pathologies. This approach involves the application of specific electric currents to acupoints, with the objective of attenuating sympathetic over-excitation and regulating the excitability of the nervous system. TAES has been shown to reduce the levels of stress hormones such as aldosterone, cortisol, and other stress-related bioactive substances, thereby contributing to a diminished stress response. The analysis of the satisfaction situation indicates that the overall satisfaction of the observation group was higher than that of the control group. This finding suggests that Meridian flow injection acupoint application combined with TAES is more conducive to the regulation of intestinal motility. It is hypothesised that this results in a change in the activity of the plexus of the intestinal nervous system, accelerating intestinal peristalsis and restoring gastrointestinal function. Consequently, the desired outcomes are achieved and patient satisfaction is enhanced.
In summary, Meridian flow injection acupoint taping combined with TAES is more able to play a synergistic role, and is used in gastroenteroscopy patients with significant effects, effectively promoting gastrointestinal mucosal damage repair, improving gastric dynamics, reducing the traumatic stress response, and improving the clinical efficacy. However, there are some shortcomings in this study. Firstly, as a single-center study, the sample size was only 120 cases and the follow-up period was only 3d, so the short-term observation may cover up the delayed changes of stress hormones, which could not fully reflect the long-term efficacy; secondly, there was no separate acupressure or transcutaneous electrical stimulation group for control, so the long-term effect has not yet been demonstrated, which needs to be explored through more high-quality studies in the future.
| 1. | Chuah JS, Tan JH, Bujang MA, Chan KK, Kosai NR. Transcutaneous electric nerve stimulation of acupuncture points improves tolerance in adults undergoing diagnostic upper gastrointestinal endoscopy: a single-center, double-blinded, randomized controlled trial. Surg Endosc. 2024;38:3279-3287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 2. | Xu JH, Tan HL, Zhang LN, Zhou ZG, Yuan L, Kong LX, Song MQ, Qi LJ, Ji XY. Transcutaneous Electrical Acupoint Stimulation Combined with Moderate Sedation of Remimazolam Tosilate in Gastrointestinal Endoscopy: A Prospective, Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Pain Ther. 2024;13:919-936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Diep C, Karibe H, Goddard G, Phan Y, Shubov A. Acupuncture and Transcutaneous Electrical Acupoint Stimulation Do Not Suppress Gag Reflex. Med Acupunct. 2021;33:353-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (1)] |
| 4. | Ali ZA, Eladl HM, Abdelbasset WK, Eid MM, Mosa HE, Elsayeh SM. Inhalation injury in adult males: Evaluation of the short-term efficacy of transcutaneous electrical acupoint stimulation on pulmonary functions and diaphragmatic mobility after burn: A double-blind randomized controlled study. Burns. 2022;48:1933-1939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 5. | Li Y, Wang M, Shi Z, Wang X, Niu Y. Application of midnight-noon ebb-flow combined with five-element music therapy in continuous nursing of patients with chronic wounds. J Eval Clin Pract. 2025;31:e14216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Lu C, Li GL, Deng DH, Bao WL, Wang Y, Zhang AQ. Transcutaneous Electrical Acupoint Stimulation Combined with Warm Acupuncture for Breast Cancer Related Upper Limb Lymphedema: A Retrospective Cohort Study. Chin J Integr Med. 2023;29:534-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | Ren G, Yang L. The effect of TCM triple rehabilitation and ear acupoint bean pressing on laparoscopic surgery for gastric cancer. Medicine (Baltimore). 2024;103:e39423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Nojkov B, Burnett C, Watts L, Yin J, Ali K, Zhao T, Gong S, Miller C, Habrowski M, Chey WD, Chen JDZ. The impact of transcutaneous electrical acustimulation (TEA) on rectal distension-induced pain in patients with irritable bowel syndrome (IBS)-A study to determine the optimal TEA delivery modalities and effects on rectal sensation and autonomic function. Neurogastroenterol Motil. 2024;36:e14799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 9. | Zhou YD, Yang SR, Wang YY, Lu W, Chen L, Liang FX. [Effect of electroacupuncture at different acupoint combination on intestinal inflammatory response and intestinal flora in obese rats]. Zhongguo Zhen Jiu. 2022;42:1145-1152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Lyu Z, Tian S, Bao G, Huang R, Gong L, Zhou J, Kong X, Zhang W, Ran R, Nie N, Liu Y, Ji C, Liu S, Shao X, Kai G, Lin X, Fang J, Liang Y. Transcutaneous electrical acupoint stimulation for cancer-related pain management in patients receiving chronic opioid therapy: a randomized clinical trial. Support Care Cancer. 2023;32:16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 11. | Mattioli LB, Frosini M, Corazza I, Fiorino S, Zippi M, Micucci M, Budriesi R. Long COVID-19 gastrointestinal related disorders and traditional Chinese medicine: A network target-based approach. Phytother Res. 2024;38:2323-2346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Li H, Du C, Lu L, Hu X, Xu H, Li N, Liu H, Wen Q. Transcutaneous electrical acupoint stimulation combined with electroacupuncture promotes rapid recovery after abdominal surgery: Study protocol for a randomized controlled trial. Front Public Health. 2022;10:1017375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (1)] |
| 13. | Yeom M, Ahn S, Hahm DH, Jang SY, Jang SH, Park SY, Jang JH, Park J, Oh JY, Lee IS, Kim K, Kwon SK, Park HJ. Acupuncture ameliorates atopic dermatitis by modulating gut barrier function in a gut microbiota-dependent manner in mice. J Integr Med. 2024;22:600-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 14. | Meng D, Mao Y, Song QM, Yan CC, Zhao QY, Yang M, Xiang G, Song Y. Efficacy and Safety of Transcutaneous Electrical Acupoint Stimulation (TEAS) for Postoperative Pain in Laparoscopy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Evid Based Complement Alternat Med. 2022;2022:9922879. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 15. | Ao L, Shi J, Bai Y, Zhang S, Gan J. Effects of transcutaneous electrical acupoint stimulation on perioperative immune function and postoperative analgesia in patients undergoing radical mastectomy: A randomized controlled trial. Exp Ther Med. 2021;21:184. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 16. | Su NJ, Huang CY, Li JS, Huang ZP, Zhang B, Wang SL, Pan BQ, Zhao CM, Zhang XQ, Liu FH. Letrozole + Ziwu Liuzhu Transcutaneous Electrical Acupoint Stimulation Improves Ovulation-Induced Pregnancy Rate in Obese Women with Polycystic Ovary Syndrome: A Prospective Cohort Study. Med Acupunct. 2023;35:334-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Li X, Liu S, Liu H, Zhu JJ. Acupuncture for gastrointestinal diseases. Anat Rec (Hoboken). 2023;306:2997-3005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 18. | Chang XL, Liu XM, An LX, Zheng JY, Zhang K. Effects of transcutaneous electrical acupoint stimulation (TEAS) on postoperative pain in patients undergoing gastric and esophageal ESD surgery: a study protocol for a prospective randomized controlled trial. BMC Complement Med Ther. 2023;23:253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 19. | Wei H, Huang JS, Zhao F, Xie ZQ, Xia ZY, Gan JH. Transcutaneous Electrical Acupoint Stimulation Improves Postoperative Cognitive Function in Senior Patients Undergoing Video-Assisted Thoracoscopic Surgery: A Randomized Controlled Trial. Chin J Integr Med. 2022;28:730-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 20. | Xu J, Lu Z, Zhang H, Shen Y, Zhao H. Analysis on Acupoint Selection and Combination for Amyotrophic Lateral Sclerosis Treated with Acupuncture Based on Data Mining. Evid Based Complement Alternat Med. 2022;2022:6541600. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Liu LY, Su Y, Wang RR, Lai YY, Huang L, Li YT, Tao XY, Su MH, Zheng XY, Huang SC, Wu YN, Yu SY, Liang FR, Yang J. Transcutaneous electrical acupoint stimulation benefits postoperative pain relief of oocyte retrieval: A randomized controlled trial. J Integr Med. 2024;22:32-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/