Published online Jun 28, 2025. doi: 10.3748/wjg.v31.i24.104907
Revised: April 14, 2025
Accepted: June 3, 2025
Published online: June 28, 2025
Processing time: 169 Days and 15.3 Hours
Various approaches to laparoscopic anatomic liver resection have been described. In this paper, the authors present a technique that utilizes the ventral avascular areas above the inferior vena cava. While many liver surgeons partially adopt this elements of this method, few employ it to the full extent outlined here. Main
Core Tip: Different approaches to laparoscopic anatomic liver resection have been described. The authors describe an approach using the ventral avascular areas above the inferior vena cava, which requires a skillful laparoscopic surgeon. However, concerns over margin positivity and tumor recurrence remain, and follow up studies are necessary to validate the approach.
- Citation: Sonbare DJ. Approaches to laparoscopic anatomic liver resection: Does one size fit all? World J Gastroenterol 2025; 31(24): 104907
- URL: https://www.wjgnet.com/1007-9327/full/v31/i24/104907.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i24.104907
I found the article by Huang et al[1] on laparoscopic liver resection (LLR) utilizing the ventral avascular area both infor
The authors describe a ventral approach performed early in the operation, involving dissection directly over the inferior vena cava (IVC) within the avascular plane. This technique is not commonly used, as bleeding from IVC is typically poorly tolerated during liver resection. The authors identify an avascular dissection plane similar to that used in the hanging maneuver, which is usually performed after devascularizing the short hepatic veins (SHVs) on the side of resection. However, in this article, the authors propose accessing the ventral avascular plane after achieving inflow control, but without outflow control. Most liver surgeons tend to adopt elements of this approach, though rarely to the full extent described. Maintaining low central venous pressure anesthesia is crucial, as shown in the operative images with collapsed hepatic veins. This helps decrease intra-abdominal pressure, reducing blood loss and preserving respira
The authors present the case of a 50-year-old male with hepatocellular carcinoma who underwent a segment VII resection using a conventional approach. He experienced intra-operative blood loss from SHVs. However, the video demonstrates that the SHVs were accessed from the ventral aspect rather than the typical right-sided approach. Most surgeons would ligate the SHV via the lateral approach during a segment VII resection, typically after mobilizing the right lobe due to risk of bleeding. Furthermore, the images suggest that some tumors were resected with minimal tumor margins. In such cases, it is advisable to maintain at least a 1 cm margin around the tumor and to avoid exposing the tumor surface.
This approach has definite advantages when the patient’s body mass index (BMI) is low, the tumor is small (or large but embedded in the liver parenchyma), and the overlying liver parenchyma is not excessively bulky or heavy. In patients with a high BMI, it can be difficult to clearly visualize the ventral area early during the operation. However, in such cases, following the natural course of the Glissonean pedicle may be more advantageous. Therefore, this approach may not be suitable when other essential criteria for LLR are not met. Another limitation of this method is that because it does not follow classical partitioning, there is a risk of residual tumor or tumor metastasis. A follow-up study of patients who have undergone the procedure would be valuable in assessing the risks of tumor recurrence and dissemination.
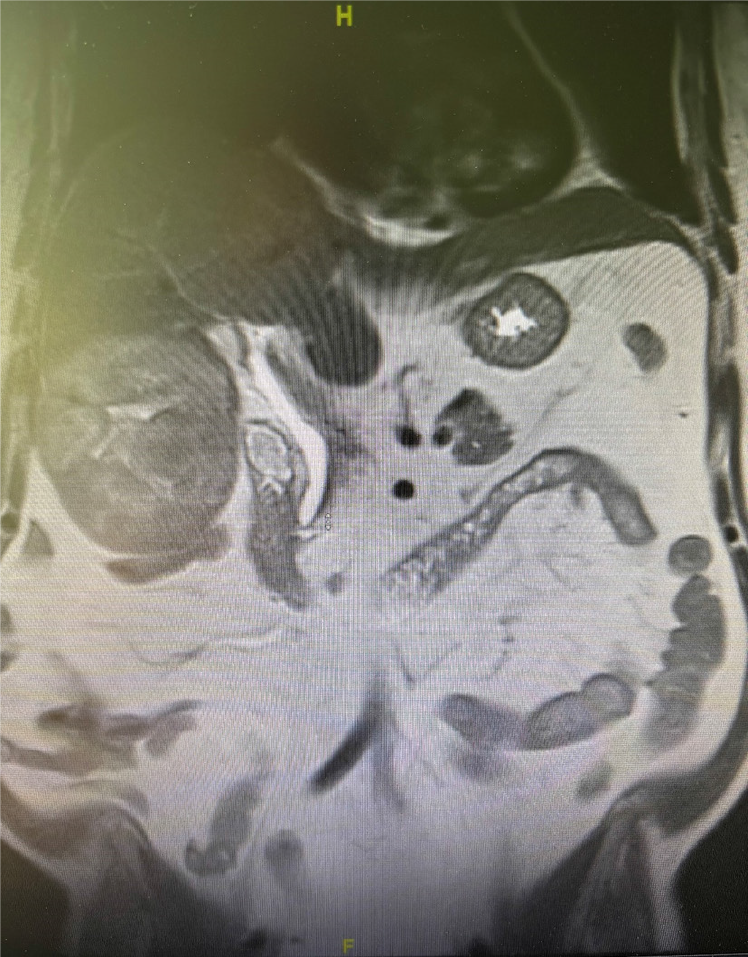
I have had a personal experience with a patient on whom I used this approach and failed. The patient was a 66 year-old male with no features of chronic liver disease. He was diagnosed with a right lobe hepatocellular carcinoma that was 9.3 cm × 8.6 cm. The tumor was partly exophytic and involved liver segment 5 and part of segment 6 (Figure 1).
The tumor was located near the right anterior and right posterior portal pedicle. Laparoscopic intra-operative ul
Despite the drawbacks, the ventral approach clearly offers advantages in cases of tumors involving the IVC or the right adrenal gland. This article demonstrates the expertise of the surgeons who completed these procedures laparoscopically using this novel approach without compromising the oncological outcomes of the patients.
I thank Susannah Faith Clarke for the English language corrections.
| 1. | Huang K, Chen Z, Xiao H, Hu HY, Chen XY, Du CY, Lan X. Laparoscopic liver resection utilizing the ventral avascular area of the inferior vena cava: A retrospective cohort study. World J Gastroenterol. 2025;31:100750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 2. | Endo T, Morise Z, Katsuno H, Kikuchi K, Matsuo K, Asano Y, Horiguchi A. Caudal Approach to Laparoscopic Liver Resection-Conceptual Benefits for Repeated Multimodal Treatment for Hepatocellular Carcinoma and Extended Right Posterior Sectionectomy in the Left Lateral Position. Front Oncol. 2022;12:950283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Morise Z. Laparoscopic liver resection for posterosuperior tumors using caudal approach and postural changes: A new technical approach. World J Gastroenterol. 2016;22:10267-10274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 30] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Hasegawa Y, Nitta H, Takahara T, Katagiri H, Kanno S, Umemura A, Sasaki A. Anterior approach for pure laparoscopic donor right hepatectomy. Surg Endosc. 2020;34:4677-4678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Kim JH, Ryu DH, Jang LC, Choi JW. Lateral approach liver hanging maneuver in laparoscopic anatomical liver resections. Surg Endosc. 2016;30:3611-3617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/