Published online Jun 21, 2021. doi: 10.3748/wjg.v27.i23.3142
Peer-review started: March 17, 2021
First decision: April 5, 2021
Revised: April 15, 2021
Accepted: May 21, 2021
Article in press: May 21, 2021
Published online: June 21, 2021
Processing time: 92 Days and 11.6 Hours
Patients with chronic pancreatitis often experience severe, unrelenting abdominal pain, which can significantly impact their quality of life. Pain control, therefore, remains central to the overall management of chronic pancreatitis. Most of the strategies aimed at treating the pain of chronic pancreatitis are based on expert opinion and vary from one institution to another, as there are no uniform guidelines to direct a stepwise approach towards achieving this goal. In this editorial, we comment on best practice strategies targeted towards pain control in chronic pancreatitis, specifically highlighting the use of opioid medications in this patient population. We discuss various safe and efficacious prescription monitoring practices in this article.
Core Tip: Pain management in chronic pancreatitis is complex; collaboration with local pain specialists maybe necessary to provide optimal care.
- Citation: Shah I, Sheth SG, Kothari DJ. Pain management in chronic pancreatitis incorporating safe opioid practices: Challenge accepted. World J Gastroenterol 2021; 27(23): 3142-3147
- URL: https://www.wjgnet.com/1007-9327/full/v27/i23/3142.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i23.3142
Chronic pancreatitis (CP) is a fibro-inflammatory disorder characterized by irrever
With abdominal pain being the predominant symptom, pain management is central to the treatment of CP. Lifestyle modifications such as alcohol and tobacco cessation along with frequent consumption of small meals remain the first-line treatment for CP[7,8]. Efficacy of pancreatic enzymes has been debated based on results from multiple randomized controlled clinical trials, and the current consensus is that uncoated preparations containing large amounts of pancreatic enzymes can be used for pain control in selected patients, in addition to treating symptoms of pancreatic insufficiency[2,9]. Similarly, some studies have shown that antioxidants with or without other analgesics could be beneficial in treating pain via suppression of oxidative stress which would reduce pancreatic inflammation[10,11].
Several experts have recommended following the World Health Organization (WHO) pain relief ladder while choosing the appropriate analgesic in CP[2,3,5,12]. Acetaminophen continues to remain the analgesic of choice. This is followed by neuromodulators such as gabapentin, pregabalin and tricyclic antidepressants. Antispasmodics and muscle relaxants such as baclofen and hyoscyamine have also been used as adjunctive therapies. Oftentimes, endoscopic intervention with sphincterotomy and stent placement is employed in patients with distal pancreatic duct obstruction. Surgical techniques aimed at ductal decompression or parenchymal resection or both, albeit limited by their invasive nature, are often employed in patients who have pain that is refractory to other treatment measures. In the United States, total pancreatectomy with islet auto transplantation has shown promising results, although there have been mixed results on long term diabetes control and insulin dependence[13-16]. Denervation techniques such as celiac plexus blocks are also used when other treatments fail[17]. Use of neurostimulation techniques such as spinal cord stimulation and transcranial magnetic stimulation have shown promising results, although rarely employed in standard practice owing to paucity of literature[18,19]. When these strategies fail, providers are often left with opioids for pain management although there is limited published literature outlining their use in patients with CP. Knowing about the devastating nature of the current opioid epidemic that has been prevalent for more than 25 years, it is important to have a mindful and cautious approach while effectively using opioids to treat pain in such patients[20,21].
Opioid use disorder (OUD) has evolved into a major health emergency over the last few years, contributing to more than 600000 deaths just in the United States, man
With the increased use of opioids, there remains a high level of concern among gastroenterologists and other providers for the risk of opioid dependence and abuse along with increased healthcare utilization. In CP, opioid use has limited data and uniform guidelines are lacking to direct prescription practices, which can lead to further apprehension and confusion among providers when deciding upon an ideal approach. Although the WHO pain relief ladder has been recommended by some experts while choosing an appropriate analgesic in patients with CP, it should be noted that this stepwise approach was originally designed for achieving pain control primarily in cancer patients, and the feasibility of its use has not been studied in CP[2,12]. Absence of a uniform stepwise approach towards analgesic use in CP, may further result in irregular and scattered methods of opioid prescription among various providers, further adding to opioid overuse and associated adverse outcomes.
Curbing the overuse of opioids and regulating a streamlined opioid-prescription system, is a critical task for providers caring for patients with chronic pancreatitis. There is a need for treatment approaches that are successful in minimizing pain while minimizing the risk of developing OUD. Several pain societies have developed prescription guidelines for patients with non-cancer pain and thus it is important to partner with experienced pain clinics who can provide appropriate attention to patients requiring narcotic therapy[28-31].
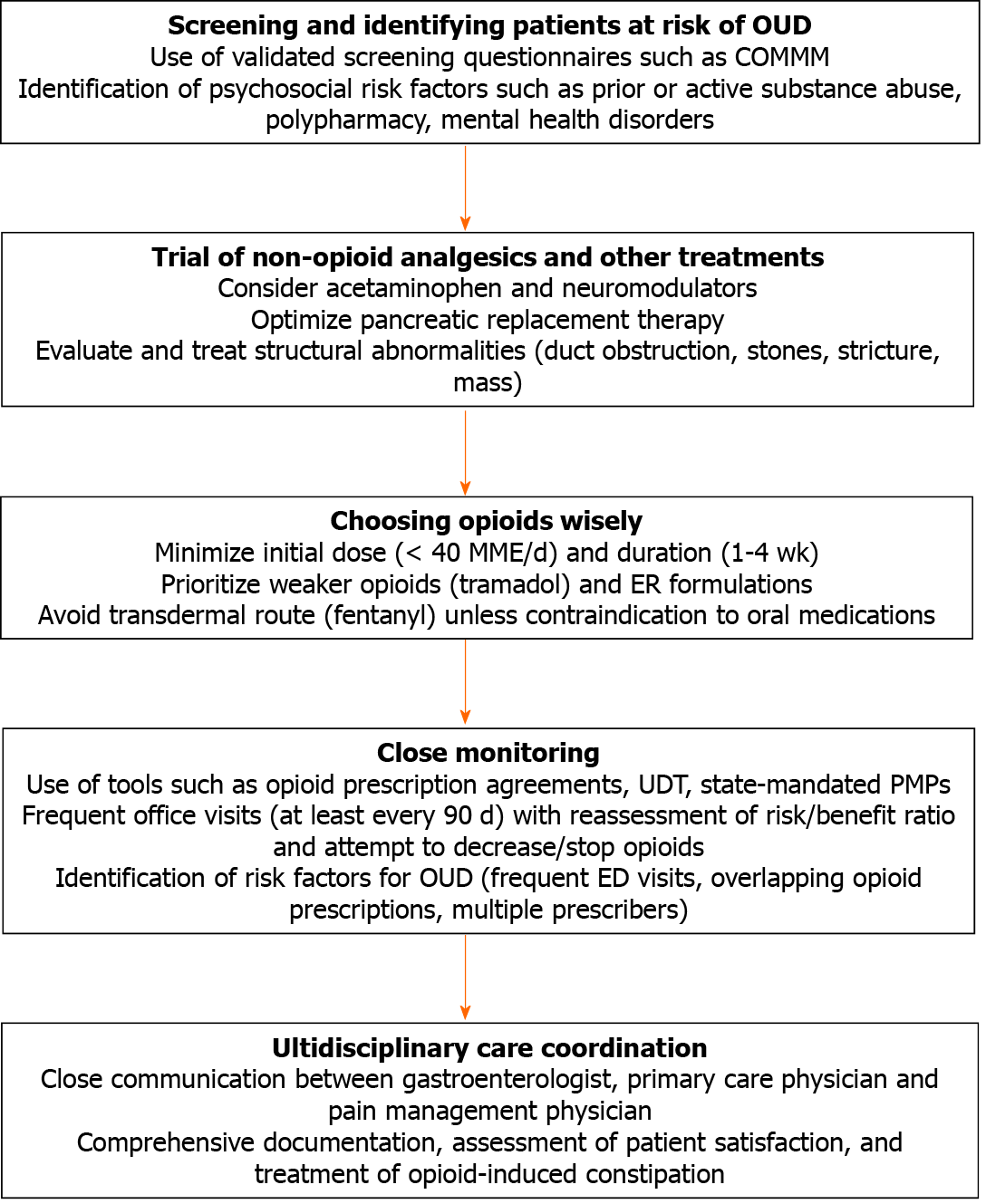
Selection of patients who would benefit from opioid therapy and predicting their risk of misuse potential should be carefully executed. Several validated screening tools for OUD can be used for this purpose including the Current Opioid Misuse Measure, which has been studied in nonalcoholic CP[32-35]. Clinicians should be vigilant for commonly encountered psychosocial risk factors that may be associated with a higher risk of abuse potential such as active or prior concurrent substance abuse, alcohol use, polypharmacy with sedating medications such as benzodiazepines, mental health disorders, etc.[36]. Since CP patients could often have comorbid substance abuse disorder, close attention should be paid to either completely avoiding or at least minimizing opioid prescriptions in patients with these risk factors[35,36].
While there is limited data on the opioid prescription guidelines in patients with CP, most experts recommend a one-to-four-week course of low dose opioids (less than 40 morphine milliequivalents) before committing to a long-term opioid therapy for patients with non-cancer pain. This is because higher doses of more than 60 to 90 morphine milliequivalents have been associated with increased risk of dependence and adverse outcomes[30,31,37]. Furthermore, there is a dearth of evidence to suggest better efficacy and safety profile of any one opioid over another[30]. Priority should be given to weaker opioids such as tramadol and extended-release formulations should be avoided due to their higher risk of overdose[30,37]. Transdermal opioids such as fentanyl should only considered when patients are unable to tolerate oral medications [30].
Prior to initiating long term opioid therapy, it is important to extensively educate the patient about its abuse potential and its associated consequences. Many states have mandated opioid treatment agreements that should be signed by both the prescriber and the patient and renewed on a regular basis[38-40]. Once long-term opioid therapy has been initiated, it is important to closely monitor for opioid misuse via various physician-based and state-mandated tools. Frequent office visits should be scheduled, no less than once in every 90 d[41]. During each visit, via means of a comprehensive history taking and physical exam, an assessment should carefully made to determine need for continuing opioid therapy. If continuing opioid therapy is deemed necessary, an attempt should be made to assess if the opioid dose can be progressively reduced to the minimum effective dose. Additionally, many experts recommend urine drug testing (UDT) prior to starting opioids and eventually for regular monitoring in an effort to curb opioid misuse[28,30]. The United States has mandated prescription monitoring programs (PMP) to track controlled prescriptions which is an efficient tool that can be regularly used by providers to reduce misuse of opioids and other controlled substances[28,30,31,37]. Close attention can thus be paid to patients with frequent emergency room visits who may be receiving multiple overlapping prescriptions of short course opioids. At any point, if lack of response, adverse events or opioid misuse are encountered, opioids may need to be discontinued[37]. Our approach is summarized in Figure 1.
Abdominal pain is the central symptom for most patients with CP resulting in high healthcare utilization. While several non-opioid therapies exist, unfortunately patients remain symptomatic and thus opioids may be necessary to treat ongoing abdominal pain. With the ongoing opioid epidemic and elevated risk of OUD, several strategies should be incorporated while using opioids for the treatment of pain in patients with CP. These include robust screening measures to predetermine the risk of OUD, safe prescription practices using tools such as UDT and PMP, close clinical follow up and frequent reassessment to assess the need for continuing opioids. Finally, a multidisciplinary approach and coordination with pain management physicians is recommended to adequately cater to each patient’s individual needs. Further studies and guidelines are needed to address opioid use in CP.
| 1. | Machicado JD, Dudekula A, Tang G, Xu H, Wu BU, Forsmark CE, Yadav D. Period prevalence of chronic pancreatitis diagnosis from 2001-2013 in the commercially insured population of the United States. Pancreatology. 2019;19:813-818. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 2. | Drewes AM, Bouwense SAW, Campbell CM, Ceyhan GO, Delhaye M, Demir IE, Garg PK, van Goor H, Halloran C, Isaji S, Neoptolemos JP, Olesen SS, Palermo T, Pasricha PJ, Sheel A, Shimosegawa T, Szigethy E, Whitcomb DC, Yadav D; Working group for the International (IAP – APA – JPS – EPC) Consensus Guidelines for Chronic Pancreatitis. Guidelines for the understanding and management of pain in chronic pancreatitis. Pancreatology. 2017;17:720-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 213] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 3. | Whitcomb DC, Shimosegawa T, Chari ST, Forsmark CE, Frulloni L, Garg P, Hegyi P, Hirooka Y, Irisawa A, Ishikawa T, Isaji S, Lerch MM, Levy P, Masamune A, Wilcox CM, Windsor J, Yadav D, Sheel A, Neoptolemos JP; Working Group for the International (IAP – APA – JPS – EPC) Consensus Guidelines for Chronic Pancreatitis. International consensus statements on early chronic Pancreatitis. Recommendations from the working group for the international consensus guidelines for chronic pancreatitis in collaboration with The International Association of Pancreatology, American Pancreatic Association, Japan Pancreas Society, PancreasFest Working Group and European Pancreatic Club. Pancreatology. 2018;18:516-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 118] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 4. | Drewes AM, Olesen AE, Farmer AD, Szigethy E, Rebours V, Olesen SS. Gastrointestinal pain. Nat Rev Dis Primers. 2020;6:1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 198] [Article Influence: 33.0] [Reference Citation Analysis (0)] |
| 5. | Beyer G, Habtezion A, Werner J, Lerch MM, Mayerle J. Chronic pancreatitis. Lancet. 2020;396:499-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 356] [Article Influence: 59.3] [Reference Citation Analysis (1)] |
| 6. | Löhr JM, Dominguez-Munoz E, Rosendahl J, Besselink M, Mayerle J, Lerch MM, Haas S, Akisik F, Kartalis N, Iglesias-Garcia J, Keller J, Boermeester M, Werner J, Dumonceau JM, Fockens P, Drewes A, Ceyhan G, Lindkvist B, Drenth J, Ewald N, Hardt P, de Madaria E, Witt H, Schneider A, Manfredi R, Brøndum FJ, Rudolf S, Bollen T, Bruno M; HaPanEU/UEG Working Group. United European Gastroenterology evidence-based guidelines for the diagnosis and therapy of chronic pancreatitis (HaPanEU). United European Gastroenterol J. 2017;5:153-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 521] [Cited by in RCA: 450] [Article Influence: 50.0] [Reference Citation Analysis (0)] |
| 7. | Singhvi A, Yadav D. Myths and realities about alcohol and smoking in chronic pancreatitis. Curr Opin Gastroenterol. 2018;34:355-361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 8. | Edderkaoui M, Thrower E. Smoking and Pancreatic Disease. J Cancer Ther. 2013;4:34-40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Warshaw AL, Banks PA, Fernández-Del Castillo C. AGA technical review: treatment of pain in chronic pancreatitis. Gastroenterology. 1998;115:765-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 182] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 10. | Zhou D, Wang W, Cheng X, Wei J, Zheng S. Antioxidant therapy for patients with chronic pancreatitis: A systematic review and meta-analysis. Clin Nutr. 2015;34:627-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Talukdar R, Lakhtakia S, Nageshwar Reddy D, Rao GV, Pradeep R, Banerjee R, Gupta R, Ramchandani M, Tandan M, Murthy HV. Ameliorating effect of antioxidants and pregabalin combination in pain recurrence after ductal clearance in chronic pancreatitis: Results of a randomized, double blind, placebo-controlled trial. J Gastroenterol Hepatol. 2016;31:1654-1662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | Jadad AR, Browman GP. The WHO analgesic ladder for cancer pain management. Stepping up the quality of its evaluation. JAMA. 1995;274:1870-1873. [PubMed] |
| 13. | Kesseli SJ, Smith KA, Gardner TB. Total pancreatectomy with islet autologous transplantation: the cure for chronic pancreatitis? Clin Transl Gastroenterol. 2015;6:e73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Bellin MD, Abu-El-Haija M, Morgan K, Adams D, Beilman GJ, Chinnakotla S, Conwell DL, Dunn TB, Freeman ML, Gardner T, Kirchner VA, Lara LF, Long-Simpson L, Nathan JD, Naziruddin B, Nyman JA, Pruett TL, Schwarzenberg SJ, Singh VK, Smith K, Steel JL, Wijkstrom M, Witkowski P, Hodges JS; POST study consortium. A multicenter study of total pancreatectomy with islet autotransplantation (TPIAT): POST (Prospective Observational Study of TPIAT). Pancreatology. 2018;18:286-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 59] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 15. | Gardner TB, Smith KD. Total Pancreatectomy and Islet Autotransplant in the Treatment of Chronic Pancreatitis: Tread Very, Very Carefully. Am J Gastroenterol. 2018;113:322-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Bellin MD, Whitcomb DC, Abberbock J, Sherman S, Sandhu BS, Gardner TB, Anderson MA, Lewis MD, Alkaade S, Singh VK, Baillie J, Banks PA, Conwell D, Cote GA, Guda NM, Muniraj T, Tang G, Brand RE, Gelrud A, Amann ST, Forsmark CE, Wilcox CM, Slivka A, Yadav D. Patient and Disease Characteristics Associated With the Presence of Diabetes Mellitus in Adults With Chronic Pancreatitis in the United States. Am J Gastroenterol. 2017;112:1457-1465. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 117] [Cited by in RCA: 95] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 17. | Sachdev AH, Gress FG. Celiac Plexus Block and Neurolysis: A Review. Gastrointest Endosc Clin N Am. 2018;28:579-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 18. | Kapural L, Cywinski JB, Sparks DA. Spinal cord stimulation for visceral pain from chronic pancreatitis. Neuromodulation. 2011;14:423-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 19. | Fregni F, Potvin K, Dasilva D, Wang X, Lenkinski RE, Freedman SD, Pascual-Leone A. Clinical effects and brain metabolic correlates in non-invasive cortical neuromodulation for visceral pain. Eur J Pain. 2011;15:53-60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 72] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 20. | Singh VK, Yadav D, Garg PK. Diagnosis and Management of Chronic Pancreatitis: A Review. JAMA. 2019;322:2422-2434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 341] [Article Influence: 48.7] [Reference Citation Analysis (2)] |
| 21. | Stoicea N, Costa A, Periel L, Uribe A, Weaver T, Bergese SD. Current perspectives on the opioid crisis in the US healthcare system: A comprehensive literature review. Medicine (Baltimore). 2019;98:e15425. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 127] [Cited by in RCA: 134] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 22. | Gostin LO, Hodge JG Jr, Noe SA. Reframing the Opioid Epidemic as a National Emergency. JAMA. 2017;318:1539-1540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 181] [Article Influence: 20.1] [Reference Citation Analysis (1)] |
| 23. | Szigethy E, Knisely M, Drossman D. Opioid misuse in gastroenterology and non-opioid management of abdominal pain. Nat Rev Gastroenterol Hepatol. 2018;15:168-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 94] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 24. | Cross RK, Wilson KT, Binion DG. Narcotic use in patients with Crohn's disease. Am J Gastroenterol. 2005;100:2225-2229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 98] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 25. | Nusrat S, Yadav D, Bielefeldt K. Pain and opioid use in chronic pancreatitis. Pancreas. 2012;41:264-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 26. | Ahmed A, Yakah W, Freedman SD, Kothari DJ, Sheth SG. Evaluation of Opioid Use in Acute Pancreatitis in Absence of Chronic Pancreatitis: Absence of Opioid Dependence an Important Feature. Am J Med. 2020;133:1209-1218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 27. | Bilal M, Chatila A, Siddiqui MT, Al-Hanayneh M, Shah AR, Desai M, Wadhwa V, Parupudi S, Casey BW, Krishnan K, Hernandez-Barco YG. Rising Prevalence of Opioid Use Disorder and Predictors for Opioid Use Disorder Among Hospitalized Patients With Chronic Pancreatitis. Pancreas. 2019;48:1386-1392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 28. | Manchikanti L, Abdi S, Atluri S, Balog CC, Benyamin RM, Boswell MV, Brown KR, Bruel BM, Bryce DA, Burks PA, Burton AW, Calodney AK, Caraway DL, Cash KA, Christo PJ, Damron KS, Datta S, Deer TR, Diwan S, Eriator I, Falco FJ, Fellows B, Geffert S, Gharibo CG, Glaser SE, Grider JS, Hameed H, Hameed M, Hansen H, Harned ME, Hayek SM, Helm S 2nd, Hirsch JA, Janata JW, Kaye AD, Kaye AM, Kloth DS, Koyyalagunta D, Lee M, Malla Y, Manchikanti KN, McManus CD, Pampati V, Parr AT, Pasupuleti R, Patel VB, Sehgal N, Silverman SM, Singh V, Smith HS, Snook LT, Solanki DR, Tracy DH, Vallejo R, Wargo BW; American Society of Interventional Pain Physicians. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part 2--guidance. Pain Physician. 2012;15:S67-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 29. | Chou R, Fanciullo GJ, Fine PG, Adler JA, Ballantyne JC, Davies P, Donovan MI, Fishbain DA, Foley KM, Fudin J, Gilson AM, Kelter A, Mauskop A, O'Connor PG, Passik SD, Pasternak GW, Portenoy RK, Rich BA, Roberts RG, Todd KH, Miaskowski C; American Pain Society-American Academy of Pain Medicine Opioids Guidelines Panel. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10:113-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1400] [Cited by in RCA: 1487] [Article Influence: 87.5] [Reference Citation Analysis (0)] |
| 30. | Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain--United States, 2016. JAMA. 2016;315:1624-1645. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3080] [Cited by in RCA: 2989] [Article Influence: 298.9] [Reference Citation Analysis (1)] |
| 31. | Black E, Khor KE, Demirkol A. Responsible Prescribing of Opioids for Chronic Non-Cancer Pain: A Scoping Review. Pharmacy (Basel). 2020;8:150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Butler SF, Budman SH, Fernandez K, Jamison RN. Validation of a screener and opioid assessment measure for patients with chronic pain. Pain. 2004;112:65-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 248] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 33. | Cheatle MD, Compton PA, Dhingra L, Wasser TE, O'Brien CP. Development of the Revised Opioid Risk Tool to Predict Opioid Use Disorder in Patients with Chronic Nonmalignant Pain. J Pain. 2019;20:842-851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 79] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 34. | Butler SF, Budman SH, Fernandez KC, Houle B, Benoit C, Katz N, Jamison RN. Development and validation of the Current Opioid Misuse Measure. Pain. 2007;130:144-156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 515] [Cited by in RCA: 493] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 35. | Barth KS, Balliet W, Pelic CM, Madan A, Malcolm R, Adams D, Morgan K, Owczarski S, Borckardt JJ. Screening for current opioid misuse and associated risk factors among patients with chronic nonalcoholic pancreatitis pain. Pain Med. 2014;15:1359-1364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 36. | Vowles KE, Witkiewitz K, Pielech M, Edwards KA, McEntee ML, Bailey RW, Bolling L, Sullivan MD. Alcohol and Opioid Use in Chronic Pain: A Cross-Sectional Examination of Differences in Functioning Based on Misuse Status. J Pain. 2018;19:1181-1188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 37. | Manchikanti L, Kaye AM, Knezevic NN, McAnally H, Slavin K, Trescot AM, Blank S, Pampati V, Abdi S, Grider JS, Kaye AD, Manchikanti KN, Cordner H, Gharibo CG, Harned ME, Albers SL, Atluri S, Aydin SM, Bakshi S, Barkin RL, Benyamin RM, Boswell MV, Buenaventura RM, Calodney AK, Cedeno DL, Datta S, Deer TR, Fellows B, Galan V, Grami V, Hansen H, Helm Ii S, Justiz R, Koyyalagunta D, Malla Y, Navani A, Nouri KH, Pasupuleti R, Sehgal N, Silverman SM, Simopoulos TT, Singh V, Solanki DR, Staats PS, Vallejo R, Wargo BW, Watanabe A, Hirsch JA. Responsible, Safe, and Effective Prescription of Opioids for Chronic Non-Cancer Pain: American Society of Interventional Pain Physicians (ASIPP) Guidelines. Pain Physician. 2017;20:S3-S92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 257] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 38. | Straub M, Pashkova AA. Controlled Substance Agreements and Other Best Opioid Prescription Practices. Otolaryngol Clin North Am. 2020;53:877-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 39. | Kraus CN, Baldwin AT, Curro FA, McAllister RG Jr. Clinical implications of patient-provider agreements in opioid prescribing. Curr Drug Saf. 2015;10:159-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 40. | McAuliffe Staehler TM, Palombi LC. Beneficial opioid management strategies: A review of the evidence for the use of opioid treatment agreements. Subst Abus. 2020;41:208-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 41. | Kaye AD, Jones MR, Kaye AM, Ripoll JG, Galan V, Beakley BD, Calixto F, Bolden JL, Urman RD, Manchikanti L. Prescription Opioid Abuse in Chronic Pain: An Updated Review of Opioid Abuse Predictors and Strategies to Curb Opioid Abuse: Part 1. Pain Physician. 2017;20:S93-S109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 79] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: American Gastroenterological Association; American Society for Gastrointestinal Endoscopy; and American College of Gastroenterology.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bataga SM, Ewers A, Xu ZL S-Editor: Liu M L-Editor: A P-Editor: Ma YJ