Published online May 28, 2021. doi: 10.3748/wjg.v27.i20.2630
Peer-review started: January 24, 2021
First decision: March 7, 2021
Revised: March 15, 2021
Accepted: April 22, 2021
Article in press: April 22, 2021
Published online: May 28, 2021
Processing time: 115 Days and 10.6 Hours
The incidence and prevalence of inflammatory bowel disease (IBD) vary between regions but have risen globally in recent decades. A lack of data from developing nations limits the understanding of IBD epidemiology.
To perform a follow-up review of IBD epidemiology in the Tuzla Canton of Bosnia-Herzegovina during a 10-year period (2009-2019).
We prospectively evaluated the hospital records of both IBD inpatients and outpatients residing in Tuzla Canton for the specified period of time between January 1, 2009 and December 31, 2019. Since all our patients had undergone proximal and distal endoscopic evaluations at the hospital endoscopy unit, we used the hospital’s database as a primary data source, alongside an additional cross-relational search of the database. Both adult and pediatric patients were included in the study. Patients were grouped by IBD type, phenotype, age, and gender. Incidence rates were calculated with age standardization using the European standard population. Trends in incidence and prevalence were evaluated as a 3-year moving average and average annual percentage change rates.
During the 10-year follow-up period, 651 patients diagnosed with IBD were monitored (of whom 334, or 51.3%, were males, and 317, or 48.7%, were females). Of all the patients, 346 (53.1%) had been diagnosed with ulcerative colitis (UC), 292 (44.9%) with Crohn’s disease (CD), and 13 (2%) with indeterminate colitis (IC). We observed 440 newly diagnosed patients with IBD: 240 (54.5%) with UC, 190 (43.2%) with CD, and 10 (2.3%) with IC. The mean annual crude incidence rates were found to be 9.01/100000 population for IBD [95% confidence interval (CI): 8.17-9.85], with 4.91/100000 (95%CI: 4.29-5.54) for UC and 3.89/100000 (95%CI: 3.34-4.44) for CD. Calculated IBD prevalence in 2019 was 146.64/100000 (95%CI: 128.09-165.19), with 77.94/100000 (95%CI: 68.08-87.70) for UC and 65.77/100000 (95%CI: 54.45-74.1) for CD. The average annual IBD percentage change was 0.79% (95%CI: 0.60-0.88), with -2.82% (95%CI: -2.67 to -2.97) for UC and 6.92% (95%CI: 6.64-7.20) for CD. During the study period, 24,509 distal endoscopic procedures were performed. The incidence of IBD was 3.16/100 examinations (95%CI: 2.86-3.45) or 1.72/100 examinations (95%CI: 1.5-1.94) for UC and 1.36/100 examinations (95%CI: 1.17-1.56) for CD.
Trends in the incidence and prevalence of IBD in Tuzla Canton are similar to Eastern European averages, although there are significant epidemiological differences within geographically close and demographically similar areas.
Core Tip: The greatest gap in knowledge about the epidemiological picture of inflammatory bowel disease relates to developing countries, such as those in Eastern Europe. The heterogeneity between the results among the few available epidemiological studies concerning Eastern Europe is intriguing. Therefore, we aimed to perform a follow-up review of inflammatory bowel disease epidemiology in the Tuzla Canton of Bosnia-Herzegovina during a 10-year period (2009-2019).
- Citation: Tulumović E, Salkić N, Tulumović D. Inflammatory bowel disease in Tuzla Canton, Bosnia-Herzegovina: A prospective 10-year follow-up. World J Gastroenterol 2021; 27(20): 2630-2642
- URL: https://www.wjgnet.com/1007-9327/full/v27/i20/2630.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i20.2630
Inflammatory bowel disease (IBD) is a group of diseases sharing characteristics of chronic and relapsing-remitting immune activation and inflammation within the gastrointestinal tract; this group shares several clinical and epidemiological character-istics[1].
Traditionally, a higher incidence of IBD is found in developed and industrialized countries. Recent reports indicate a stabilization of the incidence in most Western European countries, with the highest reported incidence in Netherlands [ulcerative colitis (UC) 17.2/100.000 inhabitants; Crohn’s disease (CD) 10.5/100.000 inhabitants] and North American countries, with the highest reported incidence in Nova Scotia, Canada (UC 23.14/100.000 inhabitants; CD 23.82/100.000 inhabitants), and suggest an increase in northern European countries[2-4]. On the other hand, there is a trend of increasing incidence in areas with traditionally lower incidence rates, such as the countries of Eastern Europe[2].
The heterogeneity of results among the few available epidemiological studies concerning Eastern Europe is intriguing[5-11]. It is apparent that the epidemiological picture of the region needs to be investigated if we are to further our understanding of the nature of IBD. Building on the results of previous studies conducted in Tuzla Canton[10,11], this study aimed to contribute to understanding the epidemiological picture of IBD in the region of Southeastern Europe by evaluating the epidemiological characteristics of IBD in the Tuzla Canton of Bosnia-Herzegovina over a follow-up period of 10 years (2009-2019).
We prospectively evaluated both IBD inpatients and outpatients residing in Tuzla Canton in northeast Bosnia-Herzegovina between January 1, 2009 and December 31, 2019 at the Department of Gastroenterology and Hepatology, University Clinical Center Tuzla. Both adult and pediatric patients were included in the study.
Tuzla Canton is one of ten cantons of the Federation of Bosnia-Herzegovina, the one of two entities in Bosnia-Herzegovina. As the most populous region with 12.5% of the nation’s population, Tuzla Canton is also an industrial center. The population in the study area is homogenous in terms of ethnicity and genetic background.
Since all our patients had undergone proximal and distal endoscopic evaluations at the hospital endoscopy unit, we used the hospital’s database as a primary data source, alongside an additional cross-relational search of the database. The study included only patients with a definitive diagnosis, based on widely accepted diagnostic criteria consisting of history data, clinical examinations, laboratory tests, radiology, endoscopy, and histology[12,13]; those with an uncertain diagnosis or without permanent residency in Tuzla Canton were excluded from the study.
Patients were grouped by IBD type, phenotype, age, and gender. As UC is cate-gorized according to endoscopic findings relating to the disease localization, it was divided into proctitis, left-sided colitis, and extensive colitis[12]. CD was categorized according to the Montreal classification[13]. Indeterminate colitis (IC) was diagnosed in those patients for whom endoscopic, radiological, and pathohistological evaluations could not confirm either of the two main forms of IBD[1].
Statistical analyses were performed with SPSS software, version 26 (SPSS, IBM, United States). Calculations of disease incidence were performed based on the 2013 census and data from the Statistical Office of the Federation of Bosnia-Herzegovina.
Descriptive statistical parameters were used to determine the basic characteristics of the study population. The year of diagnosis was used to calculate incidence. Incidence and prevalence calculations were performed using census data from the Statistical Office of the Federation of Bosnia-Herzegovina. Ninety-five percent confidence intervals (95%CIs) for the incidence rate were calculated assuming a Poisson distribution of cases.
Crude annual incidence rates for both genders were calculated based on the number of diagnosed patients and the number of inhabitants, while the average incidence rate during the observed period was calculated based on the number of years of the study. Incidence rates were standardized using standard European age groups for each of the standardized age groups[14].
Morbidity trends from 2009 to 2019 were determined by moving 3-year averages with 95%CI and by calculating annual average percentage change. The annual incidence of new cases detected per 100 distal endoscopic procedures and colonoscopies was estimated. Trends in incidence and prevalence were estimated using a linear regression model, where applicable. Prevalence estimates during the observed period were produced based on the total number of detected cases and the number of inhabitants.
The statistical level of 95% (P < 0.05) was considered significant for all statistical tests. The statistic review of the study was performed by a biomedical statistician.
From January 1, 2009 to December 31, 2019, 651 patients diagnosed with IBD were monitored (of whom 334, or 51.3%, were males, and 317, or 48.7%, were females). Of these, 346 (53.1%) had been diagnosed with UC, 292 (44.9%) with CD, and the remaining 13 (2%) with IC.
In total, 440 new IBD patients were diagnosed: 240 (54.5%) with UC, 190 (43.2%) with CD, and 10 (2.3%) with IC. Among the newly diagnosed cases, 230 (52.3%) were males, and 210 (47.7%) were females.
The mean age (± SD) of all monitored patients was 46.2 ± 16.6 years, with a median of 47 years (25th and 75th percentiles: 33 and 58 years). The mean age (± SD) of newly diagnosed patients was 45.26 ± 17.38 years, with a median age of 47 years (25th and 75th percentiles: 30 and 59 years). The mean age of newly diagnosed patients with UC was 48.16 ± 16.31 years, with a median age of 50 years (25th and 75th percentiles: 35 and 60 years), among whom the youngest patient was 15 and the oldest, 81 years old. The mean age of newly diagnosed patients with CD was 41.18 ± 18.01 years, with a median age of 40 years (25th and 75th percentiles: 26 and 55 years), among whom the youngest patient was 8 and the oldest, 80 years old. In total, 27 (6.1%) newly diagnosed patients younger than 19 years of age were registered. UC was diagnosed in five of these (18.5%), while CD was diagnosed in the remaining 22 (81.5%).
There were slightly more males among the newly diagnosed patients than women, with a ratio of 52.3% to 47.7%. Males were more likely to suffer from both major forms of IBD. Of the new cases of UC diagnosed, 124 were male (51.7%) and 116 (48.3%) were female (a ratio of 1.07:1). In total, 102 new cases of CD among the male population were registered (53.7%) and 88 (46.3%) new cases among the female population (a ratio of 1.16:1). Among the ten new cases of IC, the gender distribution was equal.
In general, no statistically significant difference in age was observed between genders at the time of diagnosis. The mean age (± SD) among male patients was 45.22 ± 18.01 (8-81) years, while the mean age of female patients was 45.3 ± 16.7 (11-80) years (t = 0.046, d.f. = 438, P = 0.964). A statistically significant difference in age between genders was observed among the patients diagnosed with UC. Males were older, with a mean age of 50.98 ± 18.12 (17-81) years, compared to females, with a mean age of 45.15 ± 16.05 (15-79) years (t = 2.805, d.f. = 238, P = 0.005). The same observation was true for IC.
Among the patients diagnosed with CD, a statistically significant difference between genders was observed in terms of age at the time of diagnosis, and females were older than males. Therefore, the average age of males was 37.53 ± 17.47 (8-76) years, while the average age of females was 45.41 ± 17.79 (11-80) years (t = 3, d.f. = 188, P = 0.002).
The mean annual crude incidence of IBD during the study period was 9.01/100000 inhabitants (95%CI: 8.17-9.85), with an incidence of 9.64/100000 inhabitants (95%CI: 8.5-10.78) in the male population and 8.41/100000 inhabitants (95%CI: 7.16-9.65) in the female population. The age-standardized mean annual incidence was 8.9/100000 inhabitants (95%CI: 8.07-9.72). In general, the ratio between the incidence of individual forms (UC:CD:IC) of the disease during the study was 54.55%:43.18%:2.27%.
The mean crude annual incidence of UC was 4.91/100000 inhabitants per year (95%CI: 4.29-5.54), with an incidence of 5.16/100000 (95%CI: 4.25-6.07) among males, and 4.68/100000 (95%CI: 3.83-5.53) among females. The age-standardized incidence for the observed period was 4.9/100000 inhabitants per year (95%CI: 4.3-5.54). The average annual incidence during the last 5 years of the study (2015-2019) was 4.91/100000 inhabitants (95%CI: 4-5.83).
The mean crude annual incidence of CD was 3.89/100000 inhabitants (95%CI: 3.34-4.44), with a prevalence of 4.28/100000 (95%CI: 3.54-5.01) for males and 3.52/100000 (95%CI: 2.69-4.35) for females. The age-standardized incidence for the observed period was 3.76/100000 inhabitants (95%CI: 3.22-4.29). The average annual incidence for the last 5 years of the study was 4.05/100000 inhabitants (95%CI: 3.22-4.89).
The mean crude annual incidence of IC was 0.2/100000 inhabitants (95%CI: 0.08-0.33).
The mean crude annual incidence of IBD in the pediatric and adolescent population was 2.49/100000 inhabitants (95%CI: 1.55-3.43), with 0.46/100000 inhabitants (95%CI: 0.06-0.87) for UC and 2.03/100000 inhabitants (95%CI: 1.26-2.79) for CD.
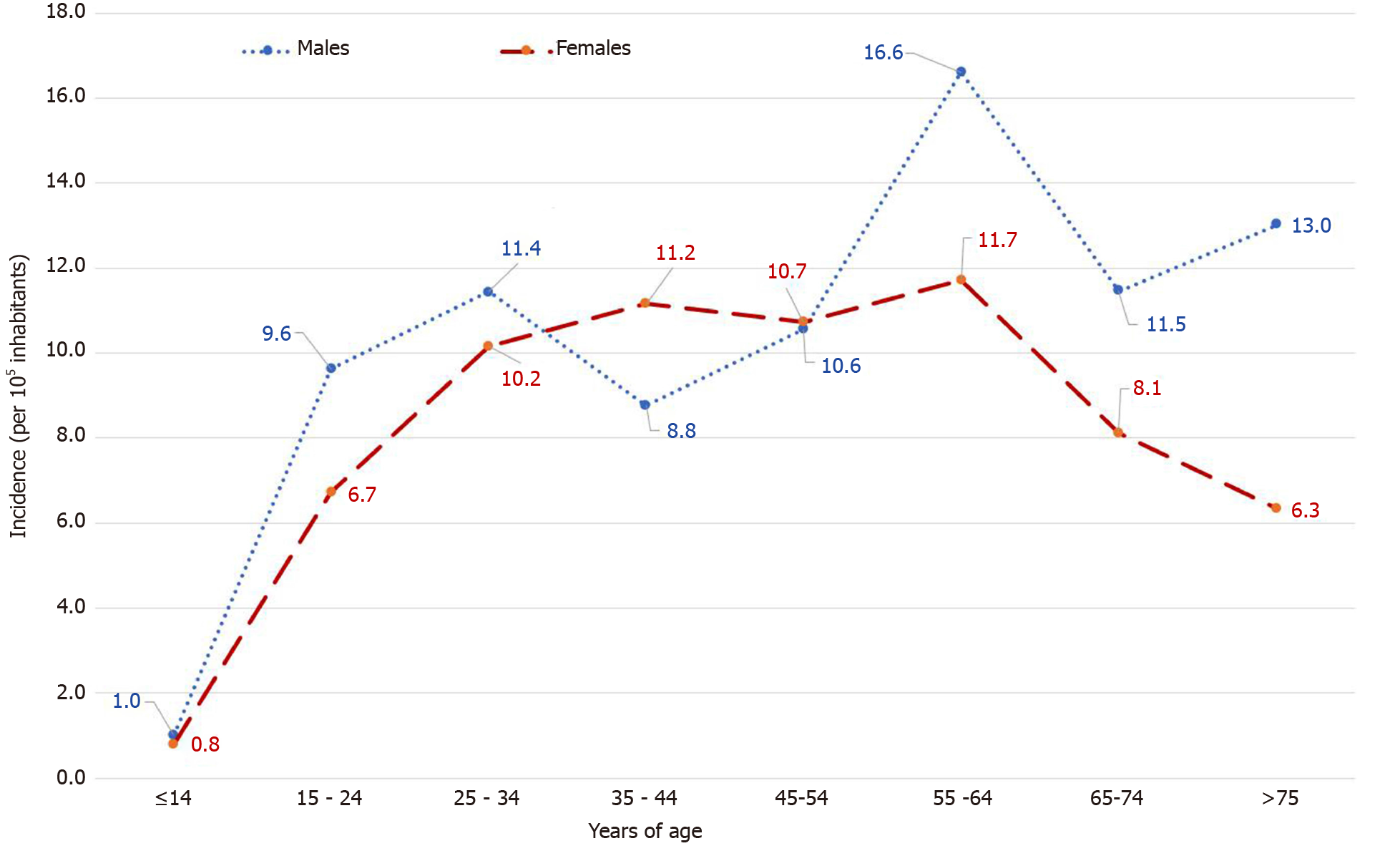
Figure 1 presents the mean crude annual incidence of IBD clustered by age and gender. Overall, the highest incidence of IBD occurred in three age groups in the male population: Patients between 55 and 64 years (14/100000 inhabitants), between 25 and 34 years (10.8/100000 inhabitants), and between 45 and 54 years (10.6/100000 inhabitants).
In general, a higher incidence was recorded both in the younger female age groups and in the older male age groups among patients diagnosed with UC. The highest incidence was recorded among males aged between 55 and 64 (11.2/100000 inhabitants) and in the age group between 55 and 64 years among the female population, which was 6.9/100000 inhabitants.
The highest incidence of CD was recorded among age groups in the male population comprising patients between 15 and 34 years: 7/100000 inhabitants. Among the female population, the disease was most often diagnosed in patients between 45 and 54 years of age, which amounts to 5.4/100000 inhabitants.
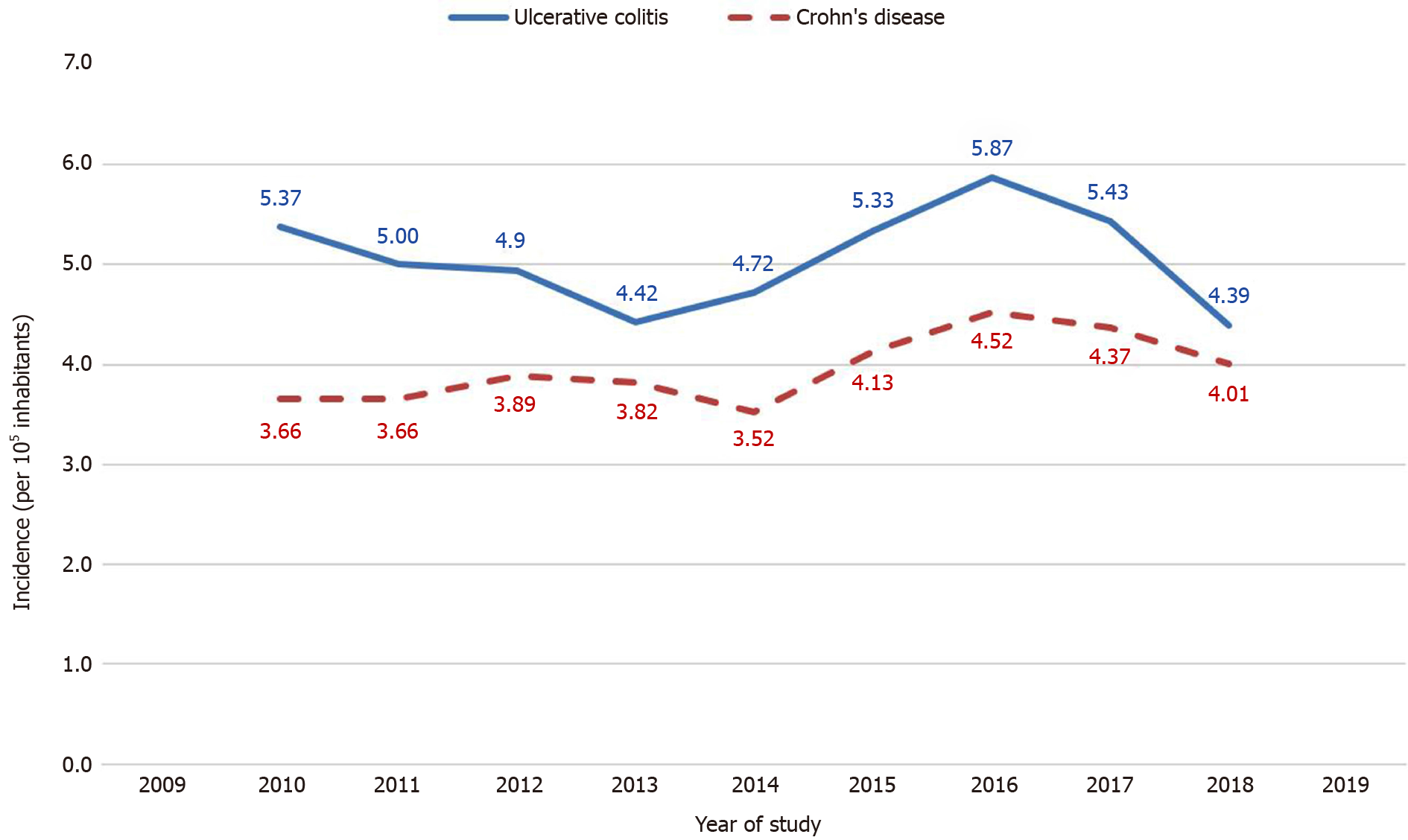
Based on the 3-year average incidence rate, which is presented in Figure 2, the incidence of both major forms of IBD occurred fairly uniformly throughout the study. The average annual incidence percentage variation was 0.79% (95%CI: 0.60-0.88) or -2.82% (95%CI: -2.67 - -2.97) for UC and 6.92% (95%CI: 6.64-7.20) for CD. Summarizing the above, we concluded that the UC incidence trend is stable; however, the same cannot be concluded for CD, where the incidence trend is increasing (Figure 2).
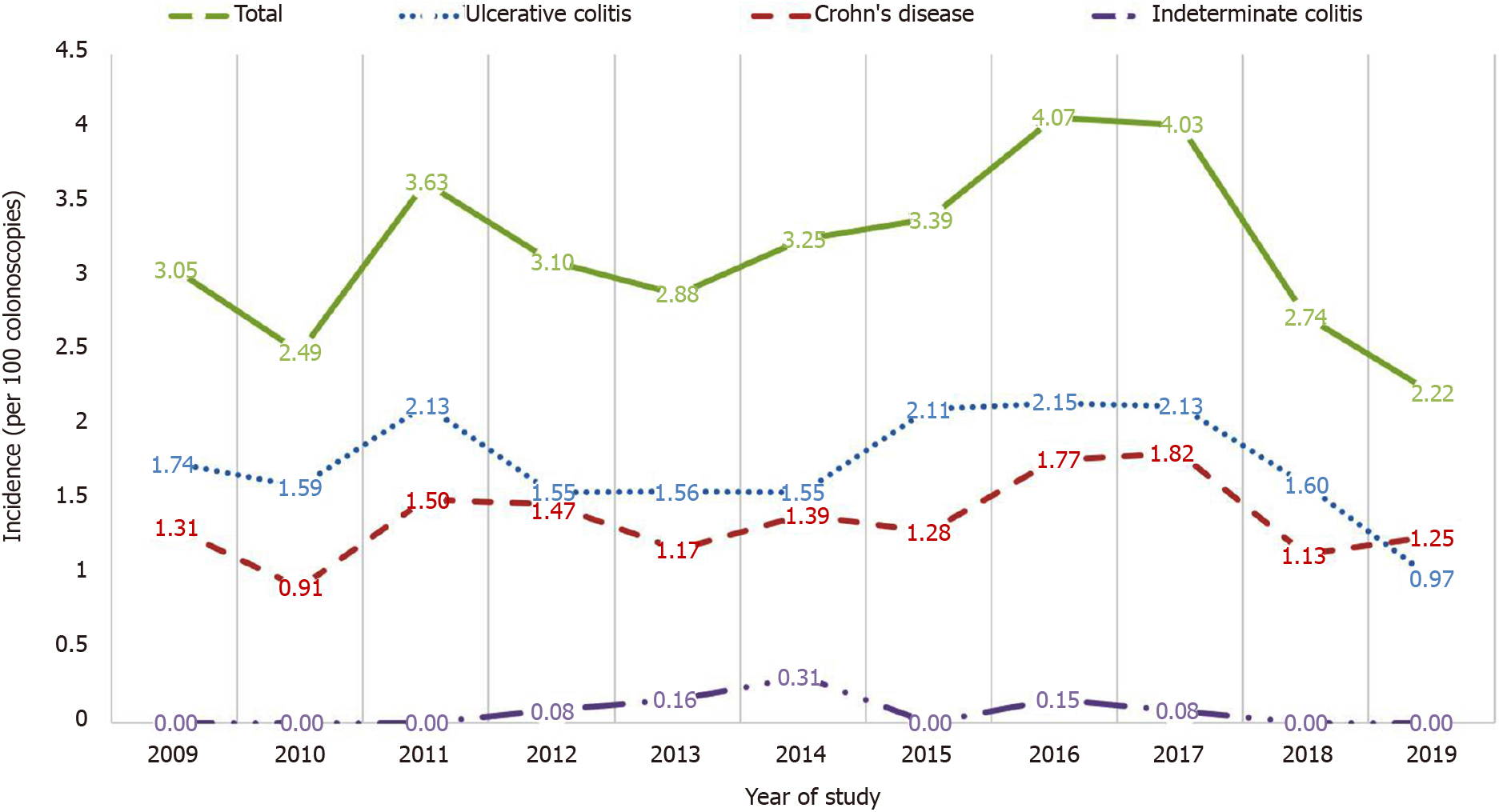
During the study period, 24509 distal endoscopic procedures were performed (an average of 2228 per year). Figure 3 shows the trend of incidence per 100 colonoscopies. Any patient suspected of having IBD underwent a detailed endoscopic evaluation in the form of a gastroscopy and colonoscopy with—if the disease phenotype allowed—intubation of the terminal ileum. The incidence of IBD was 3.16/100 examinations (95%CI: 2.86-3.45) or 1.72/100 examinations (95%CI: 1.5-1.94) for UC and 1.36/100 examinations (95%CI: 1.17-1.56) for CD.
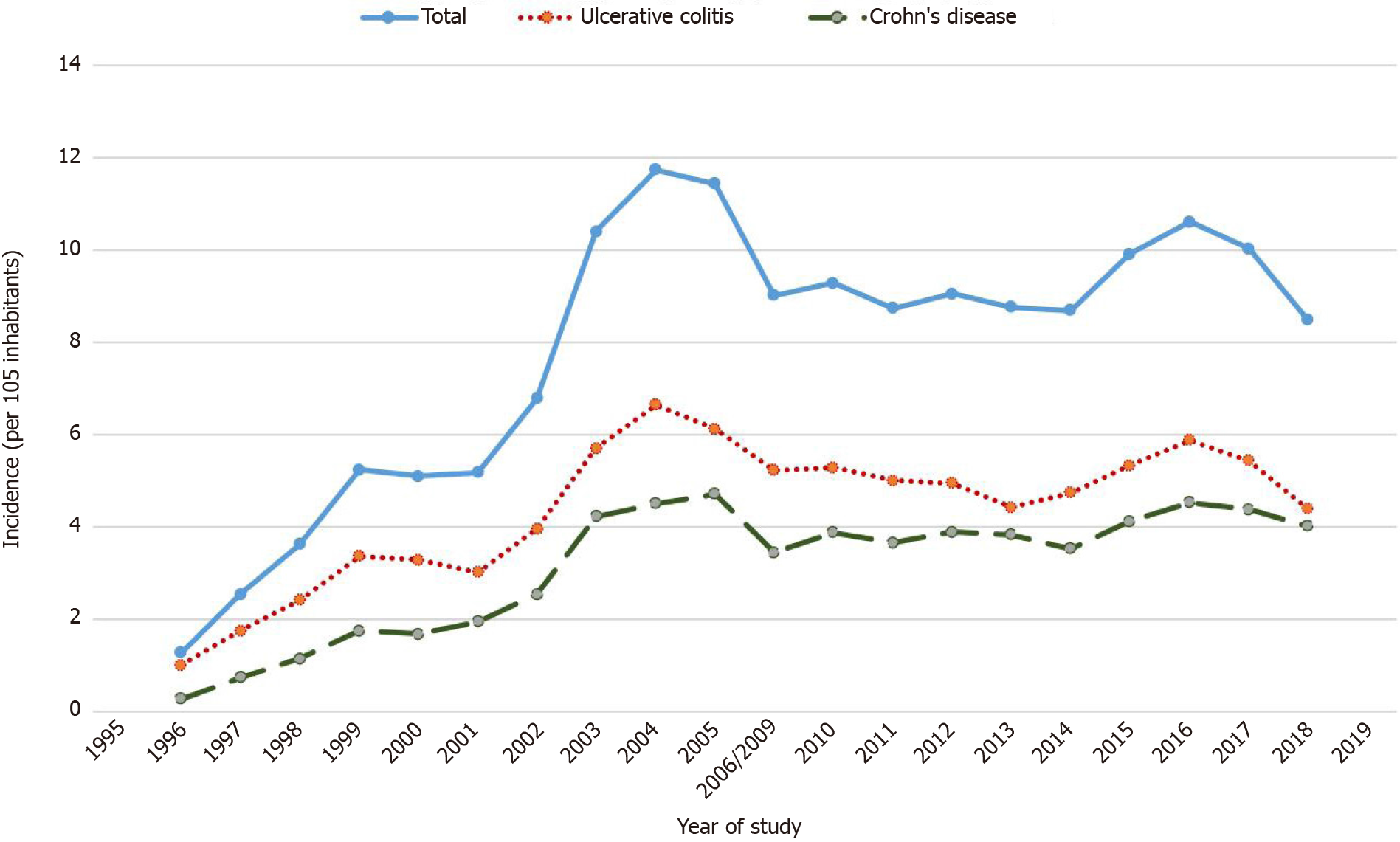
A summarized review of the 3-year average incidence rate reported in previous studies[10,11] and a recent study is presented in Figure 4. Data from the last year of the previous study (2006) and the first year of our study (2009) were used to fill in for missing years by averaging the values of these 2 years.
In the last year of the study, the prevalence of IBD was 147.44/100000 inhabitants (95%CI: 136.1-158.8): 154.48/100000 inhabitants (95%CI: 137.8-171.1) in the male population and 140.73/100000 inhabitants (95%CI: 125.2-156.2) in the female population. The age-standardized prevalence was 147.3/100000 inhabitants (95%CI: 136-158.7).
The types of individual forms of IBD according to the Montreal classification at diagnosis are presented in Tables 1 and 2. In eight (0.12%) patients, a change in the previously made diagnosis was recorded.
| Males | Females | Total | |
| Proctitis, n (%) | 32 (13.3) | 37 (15.4) | 69 (28.7) |
| Left-sided colitis, n (%) | 68 (28.3) | 64 (26.7) | 132 (55) |
| Extensive colitis, n (%) | 24 (10) | 15 (6.3) | 39 (16.3) |
| n (%) | |
| Age | |
| A1 | 13 (6.8) |
| A2 | 117 (61.6) |
| A3 | 60 (31.6) |
| Location | |
| L1 | 79 (41.5) |
| L2 | 52 (27.4) |
| L3 | 59 (31.1) |
| Behaviour | |
| B1 | 124 (65.3) |
| B2 | 49 (25.8) |
| B3 | 17 (8.9) |
| Perianal disease | |
| Present | 12 (6.3) |
| Absent | 178 (93.7) |
Among 651 patients, 49 (7.53%) required surgical treatment. In total, 8 (2.31%) patients treated for UC and 41 (14%) treated for CD underwent surgical treatment due to complications. The most common indication was lumen stenosis, which occurred in 23 (46.94%) patients. Multiple surgical treatments were performed in four (8.16%) patients. Comorbidities, primarily gastroenterological and autoimmune diseases, were also monitored during the study. Primary sclerosing cholangitis was diagnosed in four (1.37%) patients treated for CD and one (0.03%) treated for UC. Primary biliary cirrhosis, followed by liver transplantation, was noted in one (0.15%) patient. Autoimmune hepatitis was diagnosed in two (0.3%) patients, one of whom was treated for UC and the other for CD. Familial adenomatous polyposis or ankylosing spondylitis were diagnosed in two patients. Malignant colon disease occurred in five (0.76%) patients, four of whom were treated for UC (1.16%) and one for CD (0.03%). Fatal outcome occurred in six (0.9%) patients. Two patients died due to the consequences of malignant colon disease, two immediately after demanding surgical procedures, while one patient died due to the consequences of toxic megacolon accompanied by massive pulmonary embolism.
Until recently, scholars have considered IBD to be a group of diseases of developed Western societies. Recent research into the global epidemiological situation confirms a stabilization of the IBD incidence in these areas, with far higher prevalence than in less developed societies, such as in Eastern Europe[4]. The GBD (Global Burden of Disease) study observed the highest age-standardized prevalence in societies with the highest socio-demographic index (SDI)[15]. The study found the highest prevalence in the region of North America (422/100000 inhabitants) and Western Europe, especially the United Kingdom (449.6/100000 inhabitants). Bosnia-Herzegovina is currently classified as a country with a high middle SDI; according to the study, the values of age-standardized prevalence do not differ significantly compared to regions and countries of a similar standard.
When it comes to neighbouring countries, the GBD study ranked Bosnia-Herzegovina among countries with an estimated age-standardized prevalence between 100 and 120/100000 inhabitants, which is still slightly lower than the results of our research. Among the former Yugoslavian republics, neighbouring Croatia and Slovenia lead, with an estimated prevalence of between 180 and 200/100000 inhabitants[15]. These amounts do not apply to Hungary; since the 1970s, several extensive studies have shown that Hungary hosts the highest incidence of IBD in Eastern Europe[16,17].
Our study recorded the highest prevalence among males over the age of 75, which is similar to the GBD study results. The highest prevalence among the female population in our study occurred among slightly younger age groups (44-54 years) than those globally[15].
Paralysis of the healthcare system caused by the war in our country at the end of the last century required a longer recovery, which is certainly reflected in the volume of diagnostic tests and the results of scientific research. When compared with incidence rates from 1995-2006[10,11], a stable trend can be seen in IBD incidence over the study’s 10-year period. According to a study by Salkic et al[11] of the period between 1995 and 2006, an average of 397 colonoscopies per year were performed, which is 3.2 times fewer than the average number of diagnostic procedures performed annually during our study. The frequency of diagnosing UC per 100 colonoscopies performed during the previous study was 3.2 times higher than now; CD was diagnosed 2.2 times more often according to the given number of procedures performed.
The incidence rate among developing countries and regions such as Eastern Europe can be seen to have significantly increased when compared to previous reports[4]. Earlier studies from developing regions have shown an increase in the incidence of CD compared to UC[18], which was (based on the average percentile annual variation) also found to be the case in our study. Conducted in 2010 among 22 European countries, the ECCO-EpiCom cohort study[3] compared epidemiological differences between diseases in both Western and Eastern Europe, presenting the clearest and most concise epidemiological picture of IBD in Eastern Europe. It showed that the annual crude incidence of IBD in Eastern Europe was half that in Western Europe, with an average of 8.1/100000 inhabitants. The incidence of UC was 4.6/100000 inhabitants in 2010, while the incidence of CD was 3.3/100000 inhabitants, which are fairly uniform results, compared to the results presented in our study.
When it comes to the area of Southeastern Europe, the epidemiological situation is—except for Greece, Croatia, and Bosnia-Herzegovina[5-11] — poorly researched or unknown. Epidemiological studies among the pediatric population have been performed only in Slovenia[8]. The incidence calculated during our study period is somewhat lower compared to that in this region. A 10-year study (2000-2010) of both major forms of IBD in Zadar county has found a trend of increasing incidence, similar to previous studies from the Tuzla Canton[5,6,10,11]. The other recent Croatian study (conducted in Split-Dalmatia county), on the other hand, observed a decline in UC incidence and stabilization of CD incidence[7]. With the results of our study showing stabilization of UC incidence alongside an increasing trend in CD incidence, we came to the conclusion that there are significant epidemiological differences within geographically close and demographically similar areas.
The population of Tuzla Canton is generally older than it was during the previous studies, which ultimately affected the results in terms of the epidemiological situation. Although the canton’s population is still younger than the average European population, the patients involved in the study are generally older than the patients analysed in the ECCO-EpiCom study[3]. Despalatović et al[7] reported the highest incidence of UC within the 18-30 and 51-60 age groups. Their results are similar to ours and the results from a previous study from Tuzla Canton[11]. One can consider age structure to be a bimodal distribution of incidence. Similarities in the findings of these two studies can also be seen in relation to CD incidence, with the results showing a higher incidence of CD among the younger population[7,10].
When it comes to the pediatric and adolescent population, our study recorded a significantly lower incidence of IBD than research conducted in Croatia, Slovenia, and most of European countries[5,8,19], probably due to a relatively small number of colonoscopies performed in the pediatric and adolescent population in our center.
The main forms of IBD are characterized by a relapsing and remitting course, with a tendency to change localization and phenotype over time, although the results among studies are inconsistent[20-23]. The trend of localization change over time is more pronounced in UC than in CD. We registered a change in the localization of CD in 3.53% of patients during our study, which is significantly lower than those of the studies of Louis et al[21] and Lo et al[20]. Phenotype change was recorded in 16.47% of patients, which is close to the result of Lo et al[20] but drastically lower than that of Louis et al[21]’s study, which observed a change in phenotype in 45.9% of patients. Considering the new modalities of CD treatment—primarily in terms of the introduction of anti-TNF therapy—the reduction in phenotype change frequency is unsurprising. Modification of the early diagnosis was observed far less frequently than in the IBSEN study[24], in which the diagnosis of 9% of patients changed over time.
In comparison with an earlier study by Salkic et al[11], we observed a significantly higher incidence of proctitis at the expense of left-sided colitis. Given the significantly greater number of endoscopic procedures, our observation might have resulted from earlier detection of the disease. Interestingly, both studies detected the same incidence of extensive colitis, which was diagnosed in 16.3% of patients. The results of our study are close to the Eastern European average, with a higher incidence of left-sided colitis but a lower incidence of proctitis and extensive colitis. The localization and phenotype of CD do not differ significantly between Eastern and Western Europe. Except for a somewhat more frequent incidence of colic and stenotic types of CD, the results of our study do not differ significantly from the (Eastern) European average. The results of our study showed a higher incidence of the ileocolic form among the younger population, while the colic form was found to affect the older population more frequently (results which are analogous to previous studies)[25,26].
Despite the fact that patients with IBD develop a significantly higher risk of malignancy over time compared to the rest of the population[27], the results of our study show that a large number of newly diagnosed cases (128, or 37%, cases newly diagnosed with UC) undergo endoscopic examination less than two times. Similar results were obtained by Vienne et al[28] during a 7-year multicenter study in France: As many as 54% of patients with extensive colitis underwent endoscopic examination only once.
Etiological factors related to the onset or worsening of the course of the disease are numerous. IBD is mostly associated with industrialization, urbanization, and the Western way of life[2,4]. Tuzla Canton is the industrial and electric power center of Bosnia-Herzegovina, with coal as the primary raw material used for electricity production. Considering that the University Clinical Center Tuzla is the largest medical center in northeastern Bosnia-Herzegovina, it is not unrealistic to expect that the region suffers one of the highest IBD incidence rates in the country.
Population-based study in Bosnia-Herzegovina estimates that nearly half of all adults consume tobacco products on a daily basis[29]. Given the fact that tobacco consumption in public places in Bosnia-Herzegovina is not legally restricted, even a larger proportion of the population is exposed to tobacco smoke. The number of breastfeeding mothers in Bosnia-Herzegovina is far below the European average[30], which is alarming if the benefits of breastfeeding as a protective factor against the development of IBD are taken into account[31].
The design of our study was conceived according to a follow-up of patients over a 10-year period. Given the lack of an adequate information system from 2006 to 2009, 2009 was accepted as satisfactory for our study’s beginning point. Our study is retrospective-prospective in nature, based on respondents evaluated and treated at the University Clinical Center Tuzla, which is the only clinical center in the region and is a meeting place for all IBD-treated patients in the region and beyond. Given that the largest gap in the epidemiological picture of IBD relates to regions and developing countries[32] that include Bosnia-Herzegovina, we believe that our study (along with earlier reports[10,11]) can serve as a template for understanding the epidemiological picture in developing countries. In future, a multicenter study of the territory of Bosnia-Herzegovina and the countries of Southeastern Europe would greatly help us to understand this issue.
Conducted in a clinical center, this was a hospital study and, as such, has its limitations. The University Clinical Center Tuzla was the only institution capable of providing a comprehensive evaluation of patients with IBD in Tuzla Canton. Additionally, since all patients undergoing any form of IBD treatment must have a written recommendation for treatment in order to obtain reimbursement for the costs, any IBD patient from Tuzla Canton must eventually be evaluated in our center. We therefore feel safe in our assumption that despite it being single-hospital-based, our study is a confident representation of the epidemiological status of IBD in our region.
The need to conduct the study was made apparent by previous research conducted on this topic during the 11-year period from 1995 to 2006. Given the already mentioned technical limitations, the study did not follow the period from the end of 2006 to 2009. However, by monitoring prevalence, we can conclude that the incidence data throughout this period are close to data from the end of the previous study and from the beginning of our study.
The epidemiological image of IBD in Tuzla Canton is similar to the Eastern European average. Stagnation of the incidence of UC was registered, as well as an increase in the incidence of CD during the observed period. The prevalence of both major forms of IBD tends to increase. The incidence and prevalence of IC are similar to those of the Eastern European and the world average. The highest incidence of UC is observed in slightly older age groups, comparable to the average in Eastern Europe and the rest of the world. The highest incidence of CD is observed among younger age groups, between the second and fourth decades of life, as it follows Eastern European and world trends. Gender distribution among newly diagnosed patients during the study was approximately the same, with a slightly higher incidence among the males for all three most common forms of the disease. The results of the study did not show significant deviations according to the clinical and endoscopic characteristics of the disease compared to the European average.
Recent epidemiological studies conducted in Southeastern Europe show increasing incidence of inflammatory bowel diseases (IBD) in areas previously characterized as low-incidence areas. However, the results are still heterogenous as studies were conducted in areas heterogenous in terms of ethnicity, genetics background and lifestyle.
The region of Eastern Europe, especially Balkan region, is poorly described in terms of epidemiology of inflammatory bowel disease. This obvious gap in our understanding of IBD epidemiology in this region of Europe was previously partially described, and this study represents a continuation of one of the longest continuous surveys in Europe at all with nearly 25 years of epidemiological data.
The authors sought to publish an epidemiological evaluation of IBD through a detailed 10-year follow-up of the clinical and epidemiological characteristics of the major forms of the disease.
The study evaluated both IBD inpatients and outpatients residing in Tuzla Canton, and is single-hospital-based. Descriptive statistical parameters were used to determine basic characteristics of the study population. Incidence and prevalence calculations were performed using census data from the Statistical Office of the Federation of Bosnia-Herzegovina. The statistical level of 95% (P < 0.05) was considered significant for all statistical tests.
We observed 440 newly diagnosed patients with IBD: 240 (54.5%) with ulcerative colitis (UC), 190 (43.2%) with Crohn’s disease (CD), and 10 (2.3%) with indeterminate colitis (IC). The mean annual crude incidence rates were found to be 9.01/100000 population for IBD [95% confidence interval (CI): 8.17-9.85], with 4.91/100000 (95%CI: 4.29-5.54) for UC and 3.89/100000 (95%CI: 3.34-4.44) for CD. Calculated IBD prevalence in 2019 was 146.64/100000 (95%CI: 128.09-165.19), with 77.94/100000 (95%CI: 68.08-87.70) for UC and 65.77/100000 (95%CI: 54.45-74.1) for CD. The average annual IBD percentage change was 0.79% (95%CI: 0.60-0.88), with -2.82% (95%CI: -2.67 - -2.97) for UC and 6.92% (95%CI: 6.64-7.20) for CD.
We conclude that our region of Europe has a relatively stable incidence of UC (5/100000) and CD (4/100000), which is in line with previous predictions that IBD incidence in Eastern Europe is approximately half of the incidence in Western Europe. Whether this is the result of lower ascertainment or there are other factors included remains to be seen in future research.
The most important factor for future research is why the incidence is lower in Eastern Europe. There are numerous factors to be considered, which include environmental, genetic, and sociological peculiarities of the region and its population. All of these factors should be taken in consideration during the design of future research.
The authors would like to thank the staff of the Endoscopy Unit and the Department of gastroenterology and hepatology, University Clinical Center Tuzla for their valuable contribution and technical help.
| 1. | Feldman M, Friedman LS, Brandt LJ. Sleisenger and Fordtran's gastrointestinal and liver disease: Pathophysiology/diagnosis/management. 10th ed. Philadelphia, PA: Saunders/Elsevier, 2016: 115-116. |
| 2. | Loftus EV Jr. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology. 2004;126:1504-1517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2085] [Cited by in RCA: 2174] [Article Influence: 98.8] [Reference Citation Analysis (2)] |
| 3. | Burisch J, Pedersen N, Čuković-Čavka S, Brinar M, Kaimakliotis I, Duricova D, Shonová O, Vind I, Avnstrøm S, Thorsgaard N, Andersen V, Krabbe S, Dahlerup JF, Salupere R, Nielsen KR, Olsen J, Manninen P, Collin P, Tsianos EV, Katsanos KH, Ladefoged K, Lakatos L, Björnsson E, Ragnarsson G, Bailey Y, Odes S, Schwartz D, Martinato M, Lupinacci G, Milla M, De Padova A, D'Incà R, Beltrami M, Kupcinskas L, Kiudelis G, Turcan S, Tighineanu O, Mihu I, Magro F, Barros LF, Goldis A, Lazar D, Belousova E, Nikulina I, Hernandez V, Martinez-Ares D, Almer S, Zhulina Y, Halfvarson J, Arebi N, Sebastian S, Lakatos PL, Langholz E, Munkholm P; EpiCom-group. East-West gradient in the incidence of inflammatory bowel disease in Europe: the ECCO-EpiCom inception cohort. Gut. 2014;63:588-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 297] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 4. | Ng SC, Shi HY, Hamidi N, Underwood FE, Tang W, Benchimol EI, Panaccione R, Ghosh S, Wu JCY, Chan FKL, Sung JJY, Kaplan GG. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390:2769-2778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2677] [Cited by in RCA: 4493] [Article Influence: 499.2] [Reference Citation Analysis (111)] |
| 5. | Sincić BM, Vucelić B, Persić M, Brncić N, Erzen DJ, Radaković B, Mićović V, Stimac D. Incidence of inflammatory bowel disease in Primorsko-goranska County, Croatia, 2000-2004: A prospective population-based study. Scand J Gastroenterol. 2006;41:437-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 70] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Klarin I, Majnarić L, Jovanović Z, Nakić D, Vcev I, Vcev A. Epidemiology and clinical presentation of inflammatory bowel disease in Zadar County, Croatia. Coll Antropol. 2013;37:1161-1170. [PubMed] |
| 7. | Despalatović BR, Bratanić A, Radić M, Jurišić Z, Tonkić A. Epidemiological trends of inflammatory bowel disease (IBD) in Split-Dalmatia County, Croatia from 2006 to 2014. Eur J Intern Med. 2017;46:e17-e19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Urlep D, Blagus R, Orel R. Incidence Trends and Geographical Variability of Pediatric Inflammatory Bowel Disease in Slovenia: A Nationwide Study. Biomed Res Int. 2015;2015:921730. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Malakos Z, Saridi M, Latsou D, Katsanos K, Bakasis AD, Albani E, Christodoulou D. Increasing Incidence of Crohn’s Disease in Epirus, Greece: A 30-Year Prospective Study from a Referral Center. [cited 5 May 2020]. In: Ecronicon [Internet]. Available from: https://www.ecronicon.com/ecgds/pdf/ECGDS-05-00211.pdf. |
| 10. | Pavlovic-Calic N, Salkic NN, Gegic A, Smajic M, Alibegovic E. Crohn's disease in Tuzla region of Bosnia and Herzegovina: a 12-year study (1995-2006). Int J Colorectal Dis. 2008;23:957-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Salkic NN, Pavlovic-Calic N, Gegic A, Jovanovic P, Basic M. Ulcerative colitis in the Tuzla region of Bosnia and Herzegovina between 1995 and 2006: epidemiological and clinical characteristics. Eur J Gastroenterol Hepatol. 2010;22:346-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Stange EF, Travis SP, Vermeire S, Reinisch W, Geboes K, Barakauskiene A, Feakins R, Fléjou JF, Herfarth H, Hommes DW, Kupcinskas L, Lakatos PL, Mantzaris GJ, Schreiber S, Villanacci V, Warren BF; European Crohn's and Colitis Organisation (ECCO). European evidence-based Consensus on the diagnosis and management of ulcerative colitis: Definitions and diagnosis. J Crohns Colitis. 2008;2:1-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 399] [Cited by in RCA: 379] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 13. | Silverberg MS, Satsangi J, Ahmad T, Arnott ID, Bernstein CN, Brant SR, Caprilli R, Colombel JF, Gasche C, Geboes K, Jewell DP, Karban A, Loftus EV Jr, Peña AS, Riddell RH, Sachar DB, Schreiber S, Steinhart AH, Targan SR, Vermeire S, Warren BF. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005;19 Suppl A:5A-36A. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2148] [Cited by in RCA: 2430] [Article Influence: 202.5] [Reference Citation Analysis (1)] |
| 14. | Pace M, Lanzieri G, Glickman M, Županič T. Revision of the European Standard Population: report of Eurostat's task force. Publications O_ce of the European Union. 2013. [cited 21 June 2020]. In: ec.europa.eu [Internet]. Available from: https://ec.europa.eu/eurostat/documents/3859598/5926869/KS-RA-13-028-EN.PDF/e713fa79-1add-44e8-b23d-5e8fa09b3f8f. |
| 15. | GBD 2017 Inflammatory Bowel Disease Collaborators. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5:17-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1466] [Cited by in RCA: 1630] [Article Influence: 271.7] [Reference Citation Analysis (0)] |
| 16. | Lakatos L, Kiss LS, David G, Pandur T, Erdelyi Z, Mester G, Balogh M, Szipocs I, Molnar C, Komaromi E, Lakatos PL. Incidence, disease phenotype at diagnosis, and early disease course in inflammatory bowel diseases in Western Hungary, 2002-2006. Inflamm Bowel Dis. 2011;17:2558-2565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 136] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 17. | Kurti Z, Vegh Z, Golovics PA, Fadgyas-Freyler P, Gecse KB, Gonczi L, Gimesi-Orszagh J, Lovasz BD, Lakatos PL. Nationwide prevalence and drug treatment practices of inflammatory bowel diseases in Hungary: A population-based study based on the National Health Insurance Fund database. Dig Liver Dis. 2016;48:1302-1307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 18. | Cosnes J, Gower-Rousseau C, Seksik P, Cortot A. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011;140:1785-1794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1390] [Cited by in RCA: 1601] [Article Influence: 106.7] [Reference Citation Analysis (3)] |
| 19. | Sýkora J, Pomahačová R, Kreslová M, Cvalínová D, Štych P, Schwarz J. Current global trends in the incidence of pediatric-onset inflammatory bowel disease. World J Gastroenterol. 2018;24:2741-2763. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 271] [Cited by in RCA: 285] [Article Influence: 35.6] [Reference Citation Analysis (6)] |
| 20. | Lo B, Vester-Andersen MK, Vind I, Prosberg M, Dubinsky M, Siegel CA, Bendtsen F, Burisch J. Changes in Disease Behaviour and Location in Patients With Crohn's Disease After Seven Years of Follow-Up: A Danish Population-based Inception Cohort. J Crohns Colitis. 2018;12:265-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 21. | Louis E, Collard A, Oger AF, Degroote E, Aboul Nasr El Yafi FA, Belaiche J. Behaviour of Crohn's disease according to the Vienna classification: changing pattern over the course of the disease. Gut. 2001;49:777-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 684] [Cited by in RCA: 715] [Article Influence: 28.6] [Reference Citation Analysis (1)] |
| 22. | Lovasz BD, Lakatos L, Horvath A, Szita I, Pandur T, Mandel M, Vegh Z, Golovics PA, Mester G, Balogh M, Molnar C, Komaromi E, Kiss LS, Lakatos PL. Evolution of disease phenotype in adult and pediatric onset Crohn's disease in a population-based cohort. World J Gastroenterol. 2013;19:2217-2226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 56] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 23. | Vester-Andersen MK, Prosberg MV, Jess T, Andersson M, Bengtsson BG, Blixt T, Munkholm P, Bendtsen F, Vind I. Disease course and surgery rates in inflammatory bowel disease: a population-based, 7-year follow-up study in the era of immunomodulating therapy. Am J Gastroenterol. 2014;109:705-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 137] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 24. | Henriksen M, Jahnsen J, Lygren I, Sauar J, Schulz T, Stray N, Vatn MH, Moum B; Ibsen Study Group. Change of diagnosis during the first five years after onset of inflammatory bowel disease: results of a prospective follow-up study (the IBSEN Study). Scand J Gastroenterol. 2006;41:1037-1043. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 84] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 25. | Castro M, Papadatou B, Baldassare M, Balli F, Barabino A, Barbera C, Barca S, Barera G, Bascietto F, Berni Canani R, Calacoci M, Campanozzi A, Castellucci G, Catassi C, Colombo M, Covoni MR, Cucchiara S, D'Altilia MR, De Angelis GL, De Virgilis S, Di Ciommo V, Fontana M, Guariso G, Knafelz D, Lambertini A, Licciardi S, Lionetti P, Liotta L, Lombardi G, Maestri L, Martelossi S, Mastella G, Oderda G, Perini R, Pesce F, Ravelli A, Roggero P, Romano C, Rotolo N, Rutigliano V, Scotta S, Sferlazzas C, Staiano A, Ventura A, Zaniboni MG. Inflammatory bowel disease in children and adolescents in Italy: data from the pediatric national IBD register (1996-2003). Inflamm Bowel Dis. 2008;14:1246-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 73] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 26. | Charpentier C, Salleron J, Savoye G, Fumery M, Merle V, Laberenne JE, Vasseur F, Dupas JL, Cortot A, Dauchet L, Peyrin-Biroulet L, Lerebours E, Colombel JF, Gower-Rousseau C. Natural history of elderly-onset inflammatory bowel disease: a population-based cohort study. Gut. 2014;63:423-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 266] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 27. | Axelrad JE, Lichtiger S, Yajnik V. Inflammatory bowel disease and cancer: The role of inflammation, immunosuppression, and cancer treatment. World J Gastroenterol. 2016;22:4794-4801. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 285] [Cited by in RCA: 355] [Article Influence: 35.5] [Reference Citation Analysis (4)] |
| 28. | Vienne A, Simon T, Cosnes J, Baudry C, Bouhnik Y, Soulé JC, Chaussade S, Marteau P, Jian R, Delchier JC, Coffin B, Admane H, Carrat F, Drouet E, Beaugerie L. Low prevalence of colonoscopic surveillance of inflammatory bowel disease patients with longstanding extensive colitis: a clinical practice survey nested in the CESAME cohort. Aliment Pharmacol Ther. 2011;34:188-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 29. | Gligorić D, Petković S, Pepić A, Ateljević J, Vukojević B. The elasticity of tobacco products in BiH – macrodata analysis. Tob Prev Cessation. 2019;5:A97. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 30. | Šumanović-Glamuzina D. Breastfeeding practice in Bosnia and Herzegovina. J Pediatr Neonat Individual Med. 2013;2:55-62. [DOI] [Full Text] |
| 31. | Xu L, Lochhead P, Ko Y, Claggett B, Leong RW, Ananthakrishnan AN. Systematic review with meta-analysis: breastfeeding and the risk of Crohn's disease and ulcerative colitis. Aliment Pharmacol Ther. 2017;46:780-789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 177] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 32. | Kaplan GG, Ng SC. Understanding and Preventing the Global Increase of Inflammatory Bowel Disease. Gastroenterology 2017; 152: 313-321. e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 566] [Cited by in RCA: 871] [Article Influence: 96.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Bosnia and Herzegovina
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Luo HS, Rawat K, Zhu YF S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Liu JH