Published online Mar 7, 2017. doi: 10.3748/wjg.v23.i9.1637
Peer-review started: November 25, 2016
First decision: January 10, 2017
Revised: January 22, 2017
Accepted: February 7, 2017
Article in press: February 8, 2017
Published online: March 7, 2017
Processing time: 101 Days and 2.9 Hours
To assess the efficacy and safety of fibrin sealant for closure of mucosal penetration at the cardia during peroral endoscopic myotomy (POEM).
Twenty-four patients who underwent POEM and experienced mucosal injury of the cardia during the procedure were retrospectively identified. Of the 24 patients, 21 had mucosal penetration and 3 had only slight mucosal damage without penetration. The 21 patients with mucosal penetration received fibrin sealant for closure at the site of penetration. Penetration-related characteristics, treatment, and recovery were reviewed for all 21 patients to assess the efficacy and safety of fibrin sealant for closure of mucosal penetration at the cardia. Clinical data, including general characteristics, procedure-related parameters, Eckardt scores, lower esophageal sphincter pressures (LESP), and esophagogastroduodenoscopy (EGD) results, were analyzed to determine their influence on treatment success after mucosal penetration during POEM.
All 21 patients had a solitary mucosal penetration in the cardia (12 in esophageal region of the cardia, 9 in the stomach region of the cardia, and 1 in both the esophageal and stomach regions). Twelve had a hole-like penetration and 9 had a linear penetration. For those with a hole-like penetration, the mean size was 0.14 cm2 (0.02-0.32 cm2). For those with a linear penetration, the median size was 0.37 cm (0.10-1.00 cm). Closure of the mucosal penetration using fibrin sealant was performed successfully in all 21 patients (two patients required 5 mL fibrin sealant, and the remaining 19 patients required 2.5 mL). Two patients had a nasogastric tube placed for five days after POEM; the remaining 19 patients were kept fasting for 3 d. All 21 patients were discharged after a median of 5 d (range: 5-7 d) postoperatively. During a median 42 mo (range: 9-62 mo) follow-up, all 21 patients with a mucosal penetration successfully healed without the occurrence of infection, ulcer, or esophagitis. Furthermore, the median LESP decreased from 31.9 mmHg (range: 21.9-67.1 mmHg) preoperatively to 20.3 mmHg (range: 6.0-41.0 mmHg) postoperatively (P < 0.05). The median preoperative and postoperative Eckardt scores were 5.0 (range; 4-10) and 1.0 (range: 0-4), respectively (P < 0.05). Of the 21 patients with mucosal penetration, symptom remission, which is defined as a postoperative Eckardt score ≤ 3, was achieved in 20 patients (95.2%) indicating that mucosal penetration did not influence the success of POEM treatment if closed successfully using fibrin sealant.
Fibrin sealant is safe and effective for closure of mucosal penetration during POEM. Mucosal penetrations do not appear to influence the treatment success of POEM if closed successfully using fibrin sealant. Additional studies regarding the feasibility, efficacy, and safety of fibrin sealant for closure of larger mucosal penetrations is warranted.
Core tip: Mucosal penetration is one of the most dangerous adverse events during peroral endoscopic myotomy (POEM). We first reported the feasibility of fibrin sealant for closure of mucosal penetration at the cardia in two cases in 2012. However, there remains a lack of evidence about the treatment response to fibrin sealant for mucosal penetration in a cohort of patients who experienced this complication. Thus, we retrospective identified and analyzed the cases for 21 patients who experienced a mucosal penetration and received fibrin sealant for penetration closure during POEM, providing further support for the efficacy and safety of fibrin sealant for penetration closure. Moreover, instructions regarding the usage of fibrin sealant for penetration closure were provided for endoscopists who might be worried about mucosal penetrations during POEM.
- Citation: Zhang WG, Linghu EQ, Li HK. Fibrin sealant for closure of mucosal penetration at the cardia during peroral endoscopic myotomy: A retrospective study at a single center. World J Gastroenterol 2017; 23(9): 1637-1644
- URL: https://www.wjgnet.com/1007-9327/full/v23/i9/1637.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i9.1637
Peroral endoscopic myotomy (POEM) is an effective and safe procedure for achalasia, and is becoming one of the first-line therapies to treat achalasia[1-4]. However, some major perioperative adverse events after POEM have been reported; mucosal penetration is one of the most dangerous adverse events[1,2,5,6]. Mucosal penetration has been reported to occur in 4.2%-17.3% of POEM procedures[1,2,5,7]. Different studies have reported on different treatment strategies, including observation without special treatment, sealing of the penetration injury by hemostatic clips, and closing the penetration defect using fibrin sealant[8,9]. Mucosal penetration usually occurs at the cardia, where a myotomy is performed during POEM. We previously reported the usage of fibrin sealant for mucosal penetration at the cardia in two cases in 2012[7]. However, long-term outcomes with a larger population are needed to further assess this treatment strategy. To the best of our knowledge, there is still no evidence regarding the treatment response to fibrin sealant for mucosal penetration during POEM in a larger cohort. The purpose of the present study was to evaluate the efficacy and safety of fibrin sealant for closure of mucosal penetration at the cardia during POEM.
Twenty-four patients who underwent POEM and experienced mucosal injury of the cardia during the procedure between November 2010 and February 2016 were identified and collected. Of these, 21 had mucosal penetration and 3 had only minor mucosal damage without penetration. All 21 patients with a penetrating injury received fibrin sealant for closure of the mucosal penetration; these 21 patients were included in the analysis.
Prior to undergoing POEM, all patients had undergone esophagogastroduodenoscopy (EGD), high-resolution manometry (HRM), and had their symptoms evaluated using Eckardt scores to confirm a diagnosis of achalasia.
Patients were admitted and fasted for 48 h before POEM. Patients underwent EGD prior to POEM to ensure that there was no residual food in the esophageal lumen. During the procedure, patients were kept in a supine position with the right shoulder elevated, and general anesthesia was administered with continuous monitoring of electrocardiography (ECG), respirations, blood pressure, and oxygen saturation.
An additional cap attached at the top of the gastroscopy was required. With the outside cap diameter (12.0 mm) as reference, the penetration size was estimated. Then, POEM was performed. First, a submucosal injection was performed with methylene blue saline solution (1:10000), and a mucosal incision was made at the right posterior esophageal wall approximately 6-10 cm from the gastroesophageal junction (GEJ). Then, a submucosal tunnel was established, passing over the GEJ to approximately 2-3 cm into the proximal stomach. The myotomy started 2 cm distal to the incision and extended 2-3 cm into the stomach. After complete hemostasis and ensuring that an endoscope could easily pass the cardia, the mucosal incision was sutured with hemostatic clips.
In the present study, four different types of myotomy were performed, including inner circular muscle myotomy, full-thickness myotomy, glasses-style anti-reflux myotomy, and progressive full-thickness myotomy.
Glasses-style anti-reflux myotomy retains about 1 cm of longitudinal muscle at the level of the dentate line after incision of the inner circular muscle, and makes selective incision of the longitudinal muscle right above and below the dentate line. The retained 1 cm of longitudinal muscle is expected to achieve the best result to prevent reflux after POEM.
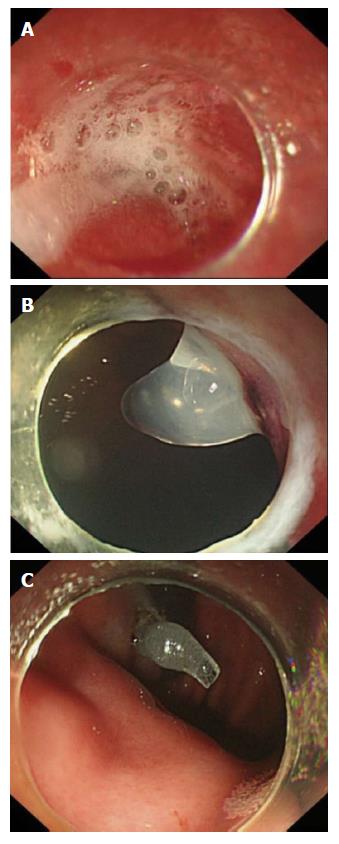
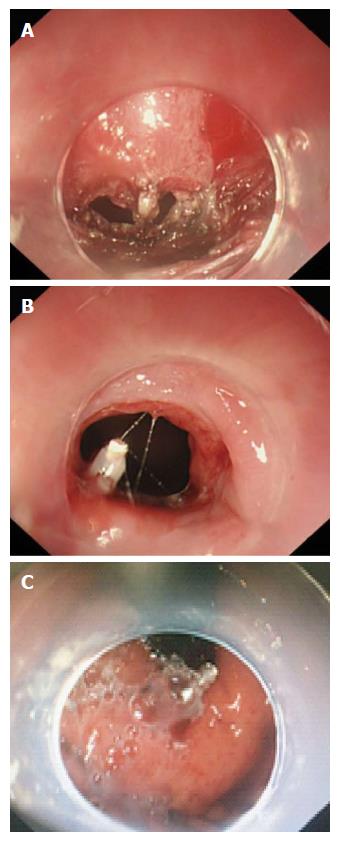
Once mucosal penetration occurred during the POEM procedure, fibrin sealant was sprayed into the penetrating injury in the submucosal tunnel under direct endoscopic visualization to ensure that the fibrin sealant fully covered the defect (Figure 1). The amount of fibrin sealant consumed was based on the size of the defect. For large penetrations, which were difficult to close only using fibrin sealant, a hemostatic clip was used to make a preliminary clipping that approximated the edges of the defect; then, fibrin sealant was sprayed to fully cover the penetration defect (Figure 2).
X-ray or chest and abdomen computed tomography (CT) was routinely performed postoperatively to evaluate for gas-related complications immediately after POEM. Delayed hemorrhage, pulmonary infection, and other complications were also monitored under EGD after the procedure. Evaluation of tunnel infection or penetration-raised esophagitis also occurs during the postoperative EGD examination, especially if the mucosa was penetrated during the procedure. After fasting for 3 d postoperatively, a liquid diet was followed for 1 d, then a soft diet. A regular diet was resumed 1 mo after POEM. Postoperative medications, including double-dose proton pump inhibitor (PPI) and antibiotics, were prescribed; PPI was required for at least 4 wk.
Patients were scheduled for a follow-up visit at 3 mo, 6 mo, 1 year, and 2 years after POEM. EGD, high-resolution manometry, and 24-h esophageal pH monitoring were required at the follow-up to assess the healing of the mucosal penetration or the entry incision, lower esophageal sphincter pressures, and postoperative esophagitis, respectively. For patients who experienced mucosal penetration during POEM, two additional follow-ups at one week and six weeks postoperatively were added. Postoperative complications and Eckardt scores for each patient were recorded via the telephone. Treatment success was defined as Eckardt scores no greater than 3.
All statistical analyses were performed using SPSS software version 17.0. Variables are expressed as mean or median. Paired-samples Student's t-test or Wilcoxon matched-pairs signed-ranks test was used to estimate the treatment outcomes of POEM. All reported P-values are two-tailed; P-values of < 0.05 were considered statistically significant.
As shown in Table 1, the study cohort consisted of 9 men and 12 women, aged 15 to 64 years (mean, 38.0 years). Among the 21 patients with mucosal penetration, the median duration of symptoms was 26.0 mo (range, 10-360 mo). Three patients had a previous Botox injection, and one had a previous bouginage. According to the Chicago classification, 2 patients were classified as type I , 18 as type II, and 1 as type III. All 21 patients successfully underwent POEM with a median operative time of 58.9 min (range, 20.0-141.0 min). The mean length of the submucosal tunnel and myotomy was 11.7 cm (range, 7-18 cm) and 5.6 cm (range, 3-10 cm), respectively.
| Patient characteristics | |
| Sex, female/male (n) | 12/9 |
| Age (yr), mean (range) | 38.0 (15-64) |
| Symptom duration (mo), median (range) | 26.0 (10-360) |
| Previous treatment (n) | |
| Botox injection | 3 |
| Bouginage | 1 |
| Chicago classification (n) | |
| Type I | 2 |
| Type II | 18 |
| Type III | 1 |
| Procedure-related parameters | |
| Procedure time (min.), median (range) | 58.9 (20.0-141.0) |
| Tunnel length (cm), mean (range) | 11.7 (7-18) |
| Myotomy length (cm), mean (range) | 5.6 (3-10) |
| Myotomy type (n) | |
| Inner circular muscle myotomy | 10 |
| Full-thickness myotomy | 1 |
| Glasses-style anti-reflux myotomy | 1 |
| Progressive full-thickness myotomy | 9 |
With regards to myotomy type, 10 patients received an inner circular muscle myotomy, 9 had a progressive full-thickness myotomy, 1 had a full-thickness myotomy, and 1 had a glasses-style anti-reflux myotomy.
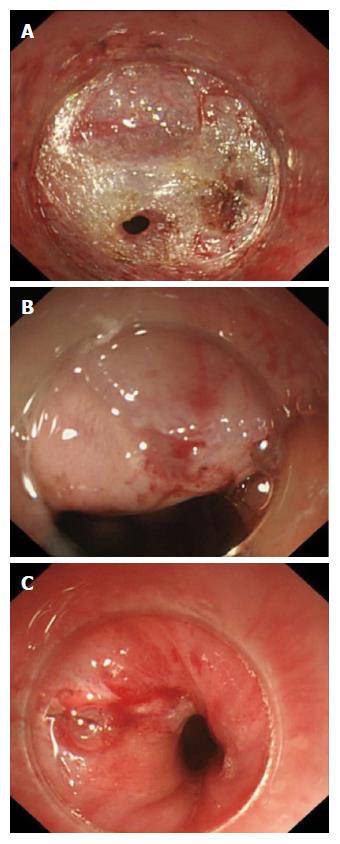
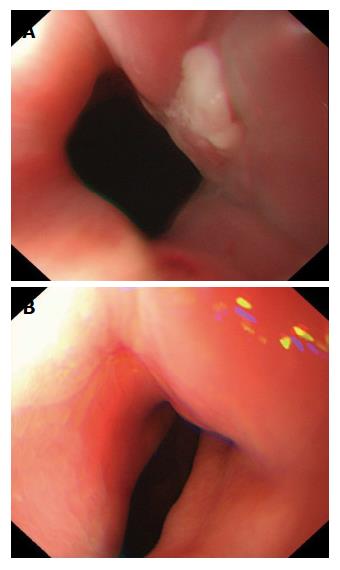
As shown in Table 2, all 21 patients had a solitary mucosal penetration in the cardia (12 in the esophageal region of cardia, 9 in the stomach region of cardia, and 1 in both the esophageal and stomach regions). Twelve patients had a hole-like penetration, while 9 had a linear penetration (Figure 3). Among those with a hole-like penetration, the mean size was 0.14 cm2 (range, 0.02-0.32 cm2). For the linear penetrations, the median size was 0.37 cm (range, 0.10-1.00 cm). Closure of mucosal penetration using fibrin sealant was performed successfully in all 21 patients. Two cases, one of which was a relatively longer linear penetration (1.0 cm), consumed 5 mL of fibrin sealant. Only 2.5 mL of sealant was required for the remaining 19 cases. One case had a 0.8 cm × 0.4 cm hole-like penetration that was difficult to close using only fibrin sealant; thus, one hemostatic clip was used to make a preliminary closure of the penetration, and fibrin sealant was then sprayed to fully cover the mucosal defect. The first two patients to experience mucosal penetration had a nasogastric tube placed for 5 d after POEM; the remaining 19 patients were kept fasting for 3 d. The mucosal penetrations had an appearance on EGD at one week postoperatively as shown in Figure 4A and an appearance at 6 wk as shown in Figure 4B. All 21 patients were discharged after a median of 5 d (range, 5-7 d) postoperatively. During a median 42 mo (range, 9-62 mo) follow-up, all 21 mucosal penetrations successfully healed without the occurrence of penetration-raised tunnel-infection, ulcer, esophagitis, mediastinal leak, or peritoneal leak. Detailed data of the 21 patients with mucosal penetrations are shown in Table 3.
| Penetration shape, n (%) | |
| Hole-like penetration | 12 (57.1) |
| Linear penetration | 9 (42.9) |
| Penetration location | |
| Esophageal part of cardia | 12 (61.9) |
| Stomach part of cardia | 8 (38.1) |
| Both esophageal and stomach parts of cardia | 1 (4.8) |
| Penetration size | |
| Hole like penetration (cm2), mean (range) | 0.14 (0.02-0.32) |
| Linear penetration (cm), median (range) | 0.37 (0.10-1.00) |
| Consumed fibrin sealant amount (n) | |
| 5.0 mL | 3 |
| 2.5 mL | 18 |
| Postoperative treatment | |
| Placement of nasogastric tube (n) | 2 |
| Postoperative stay (d), median (range) | 5 (5-7) |
| Number | Shape | Location | Estimated size (cm/cm2) | Postoperative treatment | Postoperative stay (d) | Amount of consumed fibrin sealant (mL) | Postoperative complaint |
| 1 | Hole like | GOC | 0.4 × 0.4 | NG tube | 7 | 5 | Slight abdominal pain |
| 2 | Hole like | GOC | 0.4 × 0.5 | NG tube | 7 | 2.5 | Normal |
| 3 | Hole like | GOC | 0.3 × 0.2 | Fasting | 7 | 2.5 | Normal |
| 4 | Linear | EOC | 0.3 | Fasting | 7 | 2.5 | Normal |
| 5 | Hole like | EOC | 0.4 × 0.3 | Fasting | 7 | 2.5 | Normal |
| 6 | Linear | EOC | 0.3 | Fasting | 6 | 2.5 | Normal |
| 7 | Linear | EOC | 0.1 | Fasting | 6 | 2.5 | Normal |
| 8 | Linear | GOC | 0.4 | Fasting | 6 | 2.5 | Normal |
| 9 | Linear | GOC | 0.4 | Fasting | 6 | 2.5 | Normal |
| 10 | Hole like | EOC | 0.3 × 0.2 | Fasting | 5 | 2.5 | Normal |
| 11 | Linear | EOC | 0.2 | Fasting | 5 | 2.5 | Normal |
| 12 | Hole like | EOC | 0.2 × 0.2 | Fasting | 5 | 2.5 | Normal |
| 13 | Linear | BOC | 1.0 | Fasting | 5 | 5 | Normal |
| 14 | Hole like | EOC | 0.8 × 0.4 | Fasting | 5 | 2.5 (one hemostatic clip) | Normal |
| 15 | Linear | EOC | 0.3 | Fasting | 5 | 2.5 | Normal |
| 16 | Hole like | GOC | 0.5 × 0.5 | Fasting | 5 | 2.5 | Normal |
| 17 | Hole like | EOC | 0.4 × 0.4 | Fasting | 5 | 2.5 | Normal |
| 18 | Hole like | GOC | 0.3 × 0.3 | Fasting | 5 | 2.5 | Normal |
| 19 | Hole like | EOC | 0.4 × 0.4 | Fasting | 5 | 2.5 | Normal |
| 20 | Linear | GOC | 0.3 | Fasting | 5 | 2.5 | Normal |
| 21 | Hole like | EOC | 0.1 × 0.2 | Fasting | 5 | 2.5 | Normal |
Symptom remission, which was defined as postoperative Eckardt score ≤ 3,was achieved in 20 patients (95.2%) during a median of 42 mo (range, 9-62 mo) follow-up (Table 4). The median preoperative and postoperative Eckardt score were 5.0 (range, 4-10) and 1.0 (range, 0-4), respectively (P < 0.05). A total of 15 patients had HRM both before and after treatment; 6 patients did not undergo post-operative HRM due to procedure-related discomfort or for other personal reasons. The median lower esophageal sphincter (LES) pressure decreased from 31.9 mmHg (range, 21.9-67.1 mmHg) preoperatively to 20.3 mmHg (range, 6.0-41.0 mmHg) postoperatively (P < 0.05), indicating a statistically significant decrease after POEM. All the treatment outcomes, mentioned above, indicated that mucosal penetration did not influence the treatment success of POEM if the defect was closed successfully using fibrin sealant.
| Follow-up period (mo), median (range) | 42.0 (9-62) |
| Symptom relief | |
| Eckardt score, median (range) | |
| Pre-treatment | 5.0 (4-10) |
| Post-treatment | 1.0 (0-4) |
| Pre/post-treatment difference value | 4.8 (1-9) |
| Treatment success (Eckardt score ≤ 3), n (%) | 20 (95.2) |
| Manometry outcomes | |
| Manometry follow-up rate, n (%) | 15 (71.4) |
| LESP (mmHg), median (range) | |
| Pre-treatment | 31.9 (21.9-67.1) |
| Post-treatment | 20.3 (6.0-41.0) |
| Pre/post-treatment difference value | 14.1 (9.6-35.2) |
| Post-POEM esophagitis on EGD | |
| LA-A | 1 |
| LA-B | 2 |
| Overall, n (%) | 3 (14.3) |
| Gas-related complications, n | |
| Pneumothorax | 1 |
| Pneumoperitoneum | 1 |
| Pneumomediastinum | 1 |
| Overall | 3 |
In terms of complications, 3 patients had post-POEM esophagitis on EGD; 2 were classified as Los Angeles classification B and one as Los Angeles classification A. Moreover, another 3 patients had gas-related complications: 1 experienced pneumothorax, 1 experienced pneumoperitoneum, and 1 experienced pneumomediastinum.
Esophageal achalasia is an esophageal motility disorder of unknown cause and is characterized by failure of the LES to relax and impaired peristalsis of the esophageal body[10]. Conventional therapies for achalasia include pharmacological therapy, endoscopic balloon dilation, and Heller-Dor surgery. With recent advances in endoscopic treatment techniques and devices, Inoue et al[9] have developed peroral endoscopic myotomy, in which the myotomy is performed through a submucosal tunnel. Excellent long-term outcomes after POEM have been reported[1,2], and POEM is expected to become a first-line therapy for achalasia requiring surgical intervention. However, some major perioperative adverse events from POEM have also been reported, with mucosal penetration being one of the most dangerous adverse events[1,2,5,6]. Mucosal penetration during POEM occurs at a rate ranging from 4.2%-17.3% depending on the study[1,2,5,7]. Treatment for this complication has varied, with some patients undergoing observation without special treatment, being sealed by multiple clips or an endoscopic suture device (OverStitch™ Endoscopic Suturing System; Apollo Endosurgery Austin, Texas), or being treated with the defect being closed using fibrin sealant[11-15]. Closure using hemostatic clips is not an ideal method. Once target mucosa is clipped, adjacent mucosa has the tendency to spontaneously split, making it hard to completely seal the penetration. Using endoscopic suture with the OverStitch system is usually considered when the mucosal penetration is large and difficult to close using conventional clips.
We first reported the usage of fibrin sealant for closure of mucosal penetration at the cardia in two cases in 2012[7]. The present study further supports the efficacy and safety of fibrin sealant for closure of mucosal penetration, including long-term follow-up in a larger population (21 patients). The biggest risk of mucosal penetration is that the fluids from the stomach or the esophagus could flow into the submucosal tunnel or the mediastinum and cause tunnel-infection, ulceration, esophagitis, mediastinal leak, or peritoneal leak[15,16]. In our study, all 21 mucosal penetrations healed successfully without tunnel-infection, ulceration, esophagitis, mediastinal leak, or peritoneal leak occurring. Of note, all 21 mucosal penetrations in the present study occurred at the cardia; one explanation for this might be that the small operating space and abundant submucosal vessels that demand repeated electrocoagulation during the POEM procedure make the mucosa in this area vulnerable. We presented the healing process of the mucosa after being closed using fibrin sealant (Figure 4). During a median 42 mo (range, 9-62 mo) follow-up, all patients had completely healed.
The required amount of fibrin sealant to adequately cover the mucosal injury was based on the size of the penetration; the endoscopist must ensure that the penetration is fully covered. In this cohort, we utilized 5 mL of fibrin sealant in the first patient with penetration because of lack of experience using this technique. Another patient who had a longer linear penetration (1.0 cm) consumed 5 mL fibrin sealant. The remaining 19 cases only required 2.5 mL. Of note, for penetration injuries that create larger defects, which are difficult to close using only fibrin sealant, it is suggested that one or two hemostatic clips be used to make a preliminary clipping that approximates the edges of the mucosal defect before then using fibrin sealant to fully cover the hole. Nasogastric tubes were placed postoperatively in the first two cases with penetration, again due to lack of experience with patient recovery from this technique. However, the remaining 19 cases did not require a nasogastric tube and had excellent healing results, suggesting that the postoperative placement of a nasogastric tube is not necessary in cases with a relatively small penetration.
The treatment outcomes of POEM for the 21 patients with mucosal penetration were excellent, with a 95.2% treatment success (Eckardt score ≤ 3), a 14.3% rate of gas-related complications, and a 14.3% rate of post-POEM esophagitis, indicating that mucosal penetration did not influence the treatment success of POEM if closed successfully using fibrin sealant.
Given that the sizes of the mucosal penetrations in this study were all relatively small, it is not clear whether the defects could have been observed and would have closed spontaneously. Therefore, a prospective randomized controlled trial comparing observation without special treatment to treatment with fibrin sealant is warranted. In previous studies evaluating intraoperative mucosal penetration during POEM, the injured mucosa could be closed only by prolonged fasting in those who received inner circular muscle myotomy. In the present study, 10 patients had an inner circular muscle myotomy, 1 had a full-thickness myotomy, 1 had a glasses-style anti-reflux myotomy, and 9 had a progressive full-thickness myotomy. Further research is needed to determine if the injured mucosa was more likely to close spontaneously in those who received inner circular muscle myotomy than in those who received a full-thickness myotomy. Our study is not without limitations. One limitation was that the submucosal defects in our study were all relatively small, so we cannot draw conclusions regarding the feasibility, efficacy, and safety of fibrin sealant in closing large mucosal penetrations. Additionally, with a small sample size of only 21 patients, we were not able to stratify our results to draw conclusions regarding the required amount of fibrin sealant based on the penetration size. Another limitation is that this was a single center study, suggesting that our results may not be representative of findings in other hospitals. However, to the best of our knowledge, this is the largest published study regarding the treatment response to fibrin sealant for mucosal penetration during POEM, incorporating data from 21 patients. The present study also provides instruction regarding the usage of fibrin sealant for penetration closure for endoscopists, which may be especially helpful for those who are unfamiliar with the technique or who might be worried about mucosal penetrations during POEM.
In conclusion, the use of fibrin sealant to close mucosal penetration during POEM is safe and effective. Mucosal penetrations do not appear to influence the treatment success of POEM if closed successfully using fibrin sealant. However, further research regarding the feasibility, efficacy, and safety of fibrin sealant for closing larger mucosal penetrations is warranted.
Peroral endoscopic myotomy (POEM) has been proved to be an effective and safe procedure for achalasia. However, mucosal penetration has been reported to be one of the most dangerous adverse events during POEM.
The treatments for the injured mucosa include observation without special treatment, sealed by multiple clips hemostatic clips, endoscopic suture device (OverStitch™ Endoscopic Suturing System; Apollo Endosurgery Austin, Texas) or closed using fibrin sealant. Fibrin sealant seems to be effective and safe for the penetration closure and the authors have reported a case in 2012. However, there is still no evidence regarding the treatment response to fibrin sealant for mucosal penetration during POEM in a larger cohort.
To the best of our knowledge, this is the largest published study regarding the treatment response to fibrin sealant for mucosal penetration during POEM, incorporating data from 21 patients.
The present study provided an instruction about the usage of fibrin sealant for penetration closure for endoscopists, especially for novices, who might be worried about the mucosal penetrations during POEM.
POEM: Peroral endoscopic myotomy, a recently developed endoscopic therapeutic technique, was performed for achalasia. peroral endoscopic myotomy.
This is an interesting, retrospective study from one center, on fibrin sealant for closure of cardia mucosal penetration during POEM.
| 1. | Familiari P, Gigante G, Marchese M, Boskoski I, Tringali A, Perri V, Costamagna G. Peroral Endoscopic Myotomy for Esophageal Achalasia: Outcomes of the First 100 Patients With Short-term Follow-up. Ann Surg. 2016;263:82-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 115] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 2. | Shiwaku H, Inoue H, Yamashita K, Ohmiya T, Beppu R, Nakashima R, Takeno S, Sasaki T, Nimura S, Yamashita Y. Peroral endoscopic myotomy for esophageal achalasia: outcomes of the first over 100 patients with short-term follow-up. Surg Endosc. 2016;30:4817-4826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Von Renteln D, Fuchs KH, Fockens P, Bauerfeind P, Vassiliou MC, Werner YB, Fried G, Breithaupt W, Heinrich H, Bredenoord AJ. Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology. 2013;145:309-311.e1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 265] [Cited by in RCA: 251] [Article Influence: 19.3] [Reference Citation Analysis (1)] |
| 4. | Yao S, Linghu E. Peroral endoscopic myotomy can improve esophageal motility in patients with achalasia from a large sample self-control research (66 patients). PLoS One. 2015;10:e0125942. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Zhang XC, Li QL, Xu MD, Chen SY, Zhong YS, Zhang YQ, Chen WF, Ma LL, Qin WZ, Hu JW. Major perioperative adverse events of peroral endoscopic myotomy: a systematic 5-year analysis. Endoscopy. 2016;48:967-978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 100] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 6. | Stavropoulos SN, Modayil RJ, Friedel D, Savides T. The International Per Oral Endoscopic Myotomy Survey (IPOEMS): a snapshot of the global POEM experience. Surg Endosc. 2013;27:3322-3338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 206] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 7. | Li H, Linghu E, Wang X. Fibrin sealant for closure of mucosal penetration at the cardia during peroral endoscopic myotomy (POEM). Endoscopy. 2012;44 Suppl 2 UCTN:E215-E216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Swanström LL, Rieder E, Dunst CM. A stepwise approach and early clinical experience in peroral endoscopic myotomy for the treatment of achalasia and esophageal motility disorders. J Am Coll Surg. 2011;213:751-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 111] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 9. | Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1168] [Cited by in RCA: 1282] [Article Influence: 80.1] [Reference Citation Analysis (1)] |
| 10. | Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet. 2014;383:83-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 390] [Cited by in RCA: 445] [Article Influence: 37.1] [Reference Citation Analysis (0)] |
| 11. | Onimaru M, Inoue H, Ikeda H, Yoshida A, Santi EG, Sato H, Ito H, Maselli R, Kudo SE. Peroral endoscopic myotomy is a viable option for failed surgical esophagocardiomyotomy instead of redo surgical Heller myotomy: a single center prospective study. J Am Coll Surg. 2013;217:598-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 127] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 12. | Inoue H, Tianle KM, Ikeda H, Hosoya T, Onimaru M, Yoshida A, Minami H, Kudo SE. Peroral endoscopic myotomy for esophageal achalasia: technique, indication, and outcomes. Thorac Surg Clin. 2011;21:519-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 131] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 13. | Modayil R, Friedel D, Stavropoulos SN. Endoscopic suture repair of a large mucosal perforation during peroral endoscopic myotomy for treatment of achalasia. Gastrointest Endosc. 2014;80:1169-1170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Minami H, Inoue H, Haji A, Isomoto H, Urabe S, Hashiguchi K, Matsushima K, Akazawa Y, Yamaguchi N, Ohnita K. Per-oral endoscopic myotomy: emerging indications and evolving techniques. Dig Endosc. 2015;27:175-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 15. | Eleftheriadis N, Inoue H, Ikeda H, Onimaru M, Maselli R, Santi G. Submucosal tunnel endoscopy: Peroral endoscopic myotomy and peroral endoscopic tumor resection. World J Gastrointest Endosc. 2016;8:86-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 39] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Patel K, Abbassi-Ghadi N, Markar S, Kumar S, Jethwa P, Zaninotto G. Peroral endoscopic myotomy for the treatment of esophageal achalasia: systematic review and pooled analysis. Dis Esophagus. 2016;29:807-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 93] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Eleftheriadis NP S- Editor: Qi Y L- Editor: A E- Editor: Liu WX