Published online Jul 14, 2016. doi: 10.3748/wjg.v22.i26.5971
Peer-review started: March 22, 2016
First decision: May 30, 2016
Revised: June 3, 2016
Accepted: June 28, 2016
Article in press: June 28, 2016
Published online: July 14, 2016
Processing time: 109 Days and 10.9 Hours
Pancreatic cancer (PaCa) has the highest death rate and incidence is increasing. Poor prognosis is due to late diagnosis and early metastatic spread, which is ascribed to a minor population of so called cancer stem cells (CSC) within the mass of the primary tumor. CSC are defined by biological features, which they share with adult stem cells like longevity, rare cell division, the capacity for self renewal, differentiation, drug resistance and the requirement for a niche. CSC can also be identified by sets of markers, which for pancreatic CSC (Pa-CSC) include CD44v6, c-Met, Tspan8, alpha6beta4, CXCR4, CD133, EpCAM and claudin7. The functional relevance of CSC markers is still disputed. We hypothesize that Pa-CSC markers play a decisive role in tumor progression. This is fostered by the location in glycolipid-enriched membrane domains, which function as signaling platform and support connectivity of the individual Pa-CSC markers. Outside-in signaling supports apoptosis resistance, stem cell gene expression and tumor suppressor gene repression as well as miRNA transcription and silencing. Pa-CSC markers also contribute to motility and invasiveness. By ligand binding host cells are triggered towards creating a milieu supporting Pa-CSC maintenance. Furthermore, CSC markers contribute to the generation, loading and delivery of exosomes, whereby CSC gain the capacity for a cell-cell contact independent crosstalk with the host and neighboring non-CSC. This allows Pa-CSC exosomes (TEX) to reprogram neighboring non-CSC towards epithelial mesenchymal transition and to stimulate host cells towards preparing a niche for metastasizing tumor cells. Finally, TEX communicate with the matrix to support tumor cell motility, invasion and homing. We will discuss the possibility that CSC markers are the initial trigger for these processes and what is the special contribution of CSC-TEX.
Core tip: Cancer progression relies on a small population of cancer stem cells (CSC), characterized by longevity, self renewal, drug resistance and requirement of a niche. In addition, CSC abundantly deliver exosomes (TEX) allowing CSC a long distance communication. At the descriptive level, CSC are characterized by a set of so called CSC markers. We here discuss for pancreatic cancer that the CSC markers CD44v6, c-Met, Tspan8, alpha6beta4, EpCAM, claudin7, CXCR4 and prominin1 can in a concerted activity account for all CSC features. This includes CSC TEX activity due to the engagement of CSC markers in TEX biogenesis and enrichment in TEX.
- Citation: Heiler S, Wang Z, Zöller M. Pancreatic cancer stem cell markers and exosomes - the incentive push. World J Gastroenterol 2016; 22(26): 5971-6007
- URL: https://www.wjgnet.com/1007-9327/full/v22/i26/5971.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i26.5971
Pancreatic cancer (PaCa) has a dismal prognosis due to late diagnosis and early metastatic spread. Thus, there is an urgent need for improving diagnosis and for a better understanding of the mechanisms underlying PaCa progression. We briefly outline the state of the art in concern about diagnosis with emphasis on tumor exosomes (TEX) as a promising diagnostic tool and proceed to introduce cancer stem cells (CSC) including the processes of epithelial mesenchymal transition (EMT) and premetastatic niche formation. After introducing exosomes, we outline the functional activity of Pa-CSC markers and how they contribute to the dismal prognosis of PaCa.
PaCa still holds the highest mortality rate, which is due to late diagnosis, early metastatic spread and drug and chemoresistance[1]. Though the survival rate of patients with a tumor of < 1 cm is close to 100% and about 50% fo patients with a tumor of < 2 cm survive, the 5-year survival rate for locally advanced PaCa is 9% and for metastatic PaCa 2%[2], which is very demanding for approaching early diagnosis[3-9].
Imaging advices (computed tomography, endoscopic ultrasound, emission tomography and combined computed tomography/positron emission tomography) are well established for therapy control. These new imaging advices have strongly improved PaCa detection, yet are still suboptimal for early detection[3]. Therefore, imaging is frequently combined with additional serum biomarkers. The most common marker, carbohydrate-associated antigen 19-9 (CA19-9) is helpful in response monitoring and in taking a decision on resectability, but shows insufficient sensitivity and specificity for early PaCa detection[10]. Thus, the search for additional biomarkers is still ongoing[11]. To name a few, mucin 1 (Muc-1), which is also detected in other malignancies, showed a minor improvement compared to CA19-9[12]. It is suggested to be suited for early stage detection[13]. DJ-1 (Parkinsonism associated deglycase) and combinations of regenerating family member 1β, syncoilin, anterior gradient 2 with CA19-9 improve sensitivity and specificity[14,15]. A serum proteome analysis of patients with PaCa showed significant upregulation of 40 proteins. Several of these proteins revealed disease associations to TP53[16,17]. In addition, upregulation of galectin-1, gelsolin, lumican, 14-3-3σ, cathepsin D, cofilin, moesin and plectin were described in PaCa patients. Gelsolin and lumican were suggested as markers to differentiate PaCa from chronic pancreatitis (CP)[18-20]. The search for early serum PaCa markers also includes genetic and epigenetic markers[21-23]. DNA methylation of basonuclin and ADAM metalloproteinase with thrombospondin type 1 motif 1 (ADAMTS1) in serum indicate prognostic valence[24]. Recovery of hypermethylated TNFR superfamily member 10c, and apoptotic chromatin condensation inducer 1[25] and of long noncoding (lnc) RNA metastasis associated lung adenomcarcinoma transcript 1 are predictors of poor survival[26]. Recovery of miR-21, miR-210, miR-155 and miR-196a in the serum allows differentiating PaCa patients from healthy donors. Recovery of these miRNA correlates with PaCa progression[27]. When combining the evaluation of CA19-9, miR-155, miR-181a/b and miR-196a stage I PaCa could be detected and differentiated from CP[28]. Serum miR-20a, miR-21, miR-24, miR-25, miR-99a, miR-185 and miR-191 allowed to differentiate PaCa from CP patients and healthy donors[29]. A panel of 10 free serum miRNA indicated discrimination between tumor stages[30]. A statistical meta-analysis confirmed free serum miRNA as a diagnostic tool in PaCa. However, none of these miRNA are selective for PaCa[31]. Recently, TEX in serum, which allow concomitantly evaluating PaCa-promoted genetic, epigenetic, lipidomic and proteomic alterations[23], received increased interest. A first report based on mutations in KRAS and TP53 revealed promising results[32]. Another study reports on the recovery of miR-17-5p and miR-21 in serum TEX. Recovery of miR-17-5p and miR-21 in serum exosomes differs between PaCa and CP patients and correlates with tumor progression[33]. The finding that glypican-1+ can be detected with 100% specificity and 100% sensitivity in serum TEX of PaCa patients attracted much attention. Notably, this included reliable detection of PanIN (pancreatic cancer in situ). Furthermore, the level of glypican-1+ TEX correlated with tumor burden and survival time. A mouse model with specific KRAS mutations promoting spontaneous PaCa development, confirmed recovery of glypican-1+ TEX at the stage of intraepithelial lesions[34]. We were concerned about the recovery of Pa-CSC protein markers (CD44v6, Tspan8, EpCAM, β4 integrin) in serum TEX. Additionally, microarray screenings of PaCa serum and tumor line derived TEX suggested a panel of miR-1246, miR-4644, miR-3976, miR-4306 to be suited for PaCa diagnosis. Two findings should be mentioned. TEX-enclosed miRNA is recovered at a significantly higher level than free serum miRNA. Second, we recommend to evaluate both protein and miRNA markers, which improved sensitivity (100%) and specificity (80%)[35].
These few studies on serum TEX require large scale controls. Yet, results so far appear promising for the long awaited early diagnosis of PaCa, where late diagnosis of PaCa becomes particularly vicious due to the early spread of PaCa[36]. To shed light on the unexpected power of TEX, we introduce CSC including the process of epithelial mesenchymal transition (EMT) and the establishment of a premetastatic niche in advance of reasoning on the suggested linkage between Pa-CSC markers, TEX and tumor progression.
The propensity to metastasize relies on the small subpopulation of CSC, named according to several joint features with embryonic and adult SC[37]. CSC are long lived, can self renew and differentiate, slowly progress through the cell cycle, are radiation and drug resistant and account for primary tumor growth and metastatic spread[38]. CSC and ESC share several signaling pathways, particularly over-expression of Oct4 (POU class5 homeobox1), Nanog (Nanog homeobox) and avian myelocytomatosis viral oncogene homolog (c-Myc)[39] and signaling via Notch, Wnt and Hedgehog[40], frequently initiating activation of the Ras-Raf-MAPK and PI3K-Akt pathway[41].
The metastatic cascade of epithelial tumors is initiated through EMT[42,43]. EMT essentially depends on CSC[44,45]. The hallmarks of EMT are loss of cell-cell adhesion, via E-cadherin downregulation and gain in motility by remodeling of the cytoskeleton and formation of new cell-substrate contacts supported by intermediate filament proteins like vimentin[43]. Initiation of the EMT program depends on a multitude of signals received from the environment that activate a corresponding array of intracellular signaling cascades[46-48], which force expression of EMT transcription factors Twist, Snail, Slug, Zeb1 and others[49]. Transforming growth factor (TGF)β is the major EMT inducer[50], which signals through its receptors phosphorylating SMAD2 and SMAD3 that bind to SMAD4, the complex translocating to the nucleus[50,51]. Wnt signals activate β-catenin that support Snail, but also vimentin transcription[52-54]. Activation of the EMT program through receptor tyrosine kinase (RTK) ligands like HGF, EGF, FGF and PDGF (hepatocyte-, epidermal, -fibroblast, -platelet-derived growth factor), appears to be content dependent[55-57].
EMT is initiated by downregulation of E-cadherin at the transcriptional and posttranscriptional level. EMT transcription factors are recruited to the E-cadherin promoter and repress transcription[58]. Histone modifying enzymes cooperate in E-cadherin promoter repression. This includes polycomb group proteins, which form polycomb repressive complexes silencing transcription via modifying histones and recruiting additional repressors[59]. Another important factor is Bmi1 that is upregulated in CSC and supposed to facilitate the EMT phenotype. Bmi1 downregulates Pten, which leads to activation of the PI3K/Akt pathway and posttranslational stabilization of Snail[60]. Furthermore, Twist can bind to the Bmi1 promoter and upregulate its expression[61]. Histone deacetylases are also engaged in E-cadherin silencing. They are either recruited by Snail[62] or by Twist directly associated with the histone deacetylase complex[63]. MiRNA presents the second major epigenetic mechanism engaged in the EMT process. In most instances miRNA binds to the untranslated region of their target genes, which prohibits target gene translation[64]. The engagement of miRNA in EMT was first described for the miR-200 family. This family comprises miR-200a/b/c, miR-141 and miR-429. Decreased expression of the miR-200 family is accompanied by enhanced Zeb1 and Zeb2 expression[65]. Additional miRNAs regulating EMT transcription factors are miR-29b, miR-30a, miR-205[66-68]. Other EMT targets of miRNAs are E-cadherin (miR-9), N-cadherin (miR-194), Nestin and Star1 (miR-661), pulmonary adenoma resistance 3 (miR-491-5p), which is engaged in tight junction (TJ) distortion and p120 (catenin δ1) (miR-197)[69-73]. Notably, some miRNA concomitantly regulate CSC and EMT. miR-200c becomes activated via p53, which binds to the miRNA promoter. As a consequence tumorigenicity and metastasis are suppressed[74,75]. Also, by depletion of miR-21 the number of CSC decreases and EMT is reverted[76]. In this context, it is important to remember that in epithelial cancer the process of EMT is transient[77]. In line with this, the epithelial phenotype can be restored by a double-negative feedback loop, between Zeb, Snail1 and Gata3 and miR34a or miR-200[78,79]. A similar feedback loop was described for miR-203 and Snail1[80].
There is some debate, whether non-CSC by turning into the mesenchymal phenotype acquire CSC features or whether CSC transfer the required messages towards non-CSC[44]. These options may not be mutually exclusive, taking the vision that CSC initiate the EMT phenotype in non-CSC, either by activating relevant signaling cascades by direct cell contact or via TEX, which could account for both binding initiated activation of signaling cascades and transfer of genetic and epigenetic information. The latter option has been most convincing demonstrated for the preparation of the premetastatic niche by CSC TEX.
CSC share with embryonic and adult SC dependence on a crosstalk with a special surrounding, called niche[81,82]. Adult SC and CSC niches, which are important to maintain stemness, consist of epithelial and mesenchymal cells and extracellular substrates[83]. An important contributor in the CSC niche are cancer-associated fibroblasts (CAF). CAF provide HGF, interleukin (IL)6, PDGFβ, prostaglandins (PG) and proteases, which jointly remodel the extracellular matrix (ECM)[84,85]. Other important players are mesenchymal stem cells (MSC)[86], which cooperate with CAF and macrophages (M)[87]. MSC are stimulated by tumor cell-derived IL1 to secrete PGE2, which operates in an autocrine manner promoting cytokine secretion and induces β-catenin signaling. These signaling cascades promote CSC conversion of adjacent non-CSC tumor cells[88]. Stroma cell-derived tumor necrosis factor (TNF)α and IL6 sustain TGFβ production and attract MSC to produce CSC supportive CXCL7[89]. Tumor-derived growth factors stimulate resident fibroblasts to secrete fibronectin promoting CSC attachment. Stromal fibroblasts- and CAF-derived CXCL12 (stroma-derived factor 1, SDF1) attracts CXCR4 expressing hematopoietic, endothelial cell progenitors and CSC[90]. c-Met becomes involved via HGF expressing MSC and β-catenin that together with the Tcf/Lef (lymphoid enhancer binding factor 1) complex translocates to the nucleus and initiate transcription of cell cycle related genes like cyclin D1 and c-Myc[91]. Activated integrin-linked kinase (ILK) further supports nuclear translocation of β-catenin, where ILK activation is promoted by matrix-bound β1 integrins and costimulatory signals from the environment[92]. Finally, there is evidence that niche maintenance is supported by a mutual exchange of miRNA between CIC and niche cells[93-95]. Thus, SC actively recruit and activate those cells that in a feedback support their survival.
CSC also shape a niche for metastasizing tumor cells in selective organs in advance of tumor cell arrival, known as premetastatic niche. Tumor-derived growth factors stimulate resident fibroblasts to secrete fibronectin, which promotes attachment of hematopoietic progenitors expressing VEGF receptor (R)1 and α4. In addition, stromal fibroblasts-derived CXCL12 attracts CXCR4 expressing hematopoietic progenitors and CSC[96]. Meanwhile it is well established that TEX are the central actors in establishing a premetastatic niche in epithelial cancer[97-99] including PaCa[100,101].
Taken together, CSC maintenance depends on a crosstalk with the surrounding matrix and nearby as well as distant cells. There is strong evidence that TEX are the major player in this crosstalks.
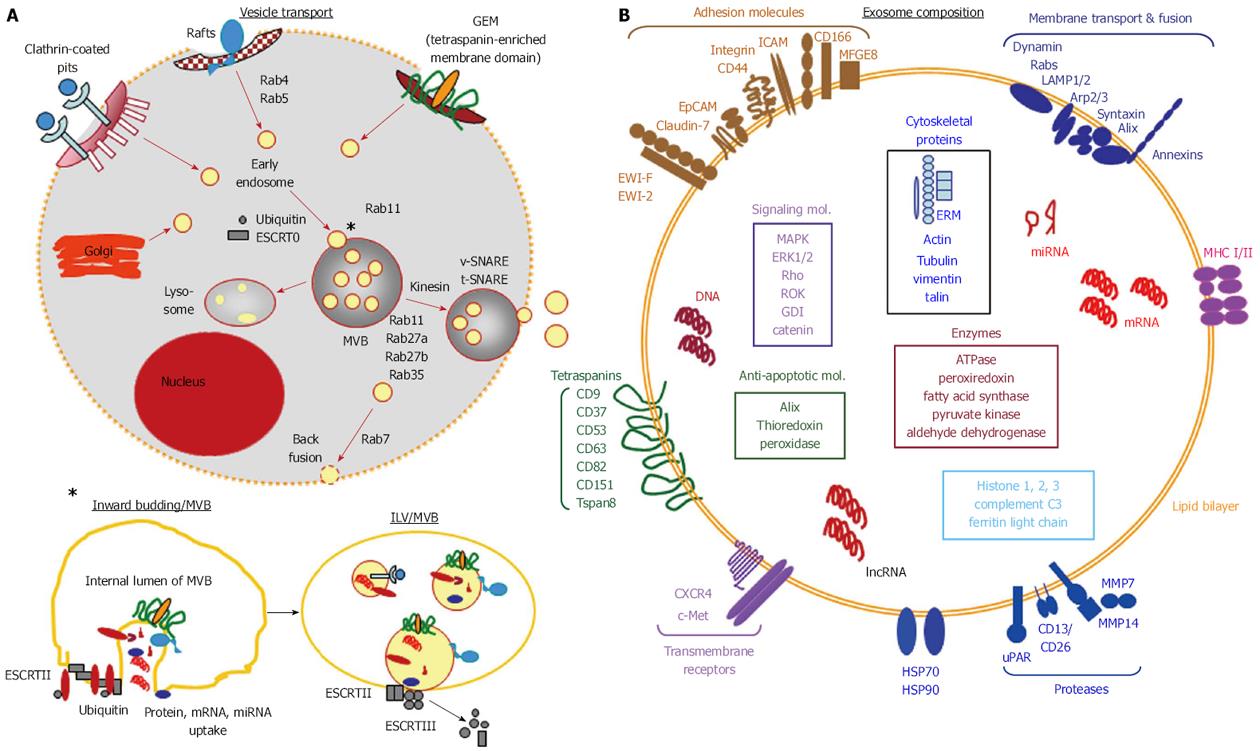
Exosomes are small 40-100 nm vesicles. They are delivered by many cells and abundantly by tumor cells[102]. Exosomes biogenesis is initiated by the formation of early endosomes that become integrated as intraluminal vesicles (ILV) into multivesicular bodies (MVB). MVB can fuse with lysosomes for protein degradation. Alternatively, MVB fuse with the plasma membrane and release their ILV, which are termed exosomes[103].
MVBs are assembled from early endosomes sorted from the trans-Golgi network or from internalized membranes, where the endosomal sorting complex required for transport (ESCRT) plays an important role in vesicle traffic and loading. The ESCRT complex is composed of the subcomplexes ESCRT I, II and III[104]. Tsg (tumor susceptibility gene)101 in the ESCRT complex I binds ubiquitinated proteins and recruits ESCRT II. ESCRT II or Alix (ALG-2-interacting protein X) recruits ESCRT III. ESCRT III recruits a deubiquitinating enzyme that removes the ubiquitin tag from the cargo proteins prior to sorting into MVB[105]. Finally, the ATPase vacuolar protein sorting 4 (Vsp4) dissociates the ESCRT III complex from the membrane. Additional essential partners in ESCRT-dependent exosome biogenesis are syndecans and transmembrane heparan sulfates, which interact with syntenin. Syntenin cooperates with CD63 and Alix[106]. Alternatively, cell membrane integrated tetraspanins and other proteins residing in glycolipid-enriched microdomains (GEM)[107] become incorporated into MVB, which is a sequel of the physical properties of GEM being prone for internalization[108]. Indeed, tetraspanins are essential for exosome generation as demonstrated by defective exosome secretion in CD9 knockout mice[109]. A third pathway proceeds via proteolipids (PLP). In cholesterol and ceramide-rich compartments, the PLP colocalize with flotilin and glycosylphosphatidylinositol. Exosome biogenesis via PLP depends on ceramide production by neutral sphinomyelinase-2. Sphingosine-1-phosphatase and diaglycerol (DAG) are engaged in cargo sorting[110].
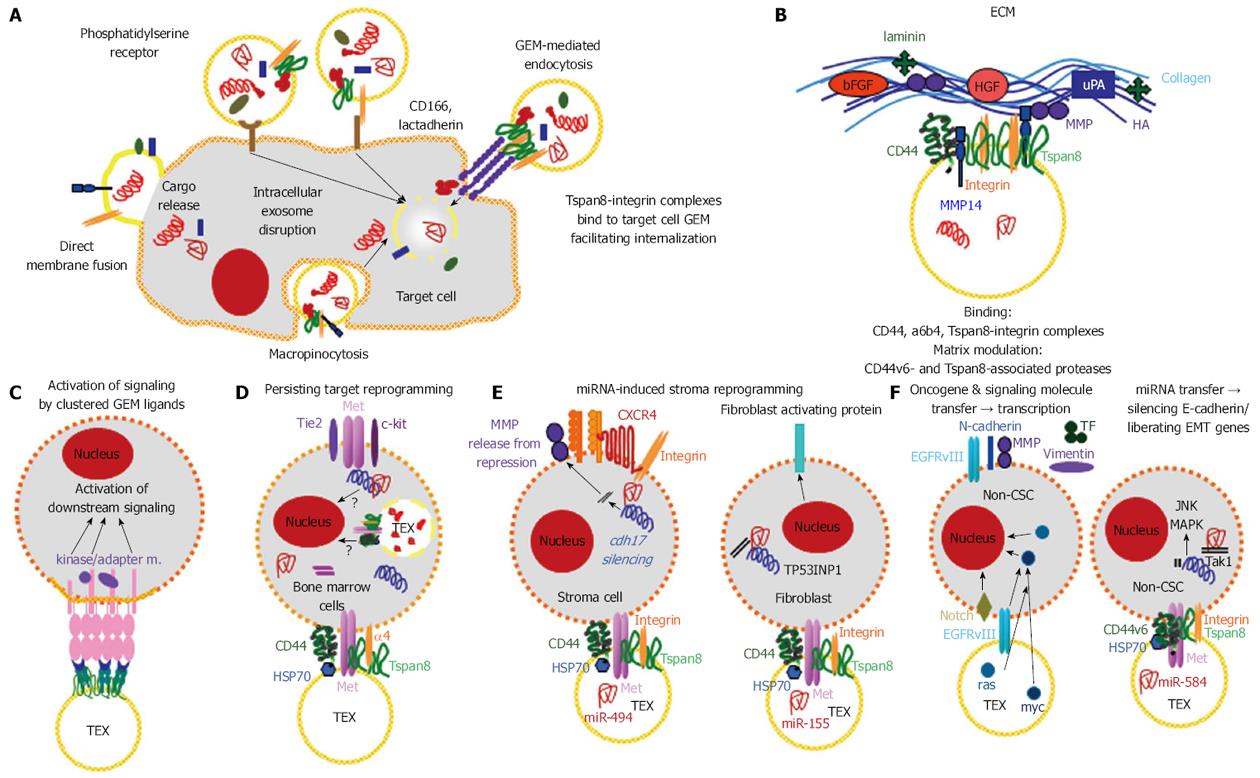
Early endosomes hike through the cytoplasm in advance of being released as exosomes. Rab proteins, a subfamily of small GTPases, associate via geranylgeranyl modifications with membranes, regulate vesicle budding, tethering and fusion. Rab4 and rab5 mostly are recovered on early endosomes, rab11 is engaged in juxtanuclear recycling endosome traffic, rab7 and rab9 are recovered in late endosome and MVB. Rab35 and rab11 are engaged in endocytic recycling. Rab proteins regulate vesicle traffic via the interaction with actin and microtubules. Rab11 recruits myosin and dynein, moving of late endosomes along microtubules being dynein-dependent. Docking on the plasma membrane via kinesin is regulated by rab25. Rab GTPase activating proteins (GAP) and Rab27b are engaged in exosome release, where SNARE proteins (soluble-N-ethylmaleimide-sensitive fusion protein-attachment protein receptors) (v-SNARE) pair with SNARE-binding partners (t-SNARE) on vesicles[111]. Finally, during the invagination of early endosomes into MVB, the exosome cytoplasm receives its cargo (Figure 1A).
Exosomes are composed of a lipid bilayer containing transmembrane proteins. The small plasma contains proteins, mRNA, non-coding RNA and DNA. The potential cargo is estimated to approximately 100 proteins and 10000 nucleotides[102]. The origin of the early endosomes determines the membrane lipid and protein composition of exosomes. Loading of the small plasma is a non-random, selective process that is not yet fully clarified.
As reviewed[112], exosomes contain phosphatidylcholine, phosphatidylethanolamine, phosphatidylinositol, prostaglandins, and lysobisphosphatidic acid and are enriched in sphingomyelin, cholesterol, GM3, and phosphatidylserine[113]. Phosphatidic acid, diglycerides, and ceramides, lipid second messengers are involved in exosome biogenesis, where proteins of the ESCRT machinery interact with various lipids or lipid-related enzymes. Vps4 interacts with an oxysterol binding protein[114] making a link with cholesterol metabolism. In fact, lipids in general, and more specifically sterols and fatty acids play a key role in Golgi/endosome/vacuole sorting[115]. Furthermore, the high content of sphingomyelin, cholesterol and GM3 increase overall rigidity and stability[116,117]. Phosphatidylserine facilitates exosome fusion and fission[118] and lysobisphosphatidic acid is involved in intracellular fusion and budding[119]. Packaging of miRNA into exosomes requires the neutral sphingomyelinase2[120].
Exosomes contain approximately 7000 proteins[121,122]. Constitutive exosomal proteins are structural vesicle components and proteins involved in vesicle biogenesis and trafficking. For GEM-derived exosomes, including tetraspanin networks, higher order oligomerization is important[123]. There is strong evidence that exosomes derived from tetraspanin-enriched microdomains contain the unchanged membrane complex including attached cytoplasmic components[124], which may account for GEM-derived exosomes in general. In raft-derived exosomes ceramide forming sphingolipids play an important role in exosome loading[125]. Otherwise, mono-ubiquitination, acylation or myristoylation are known to facilitate sorting of proteins into exosomes[126,127].
Tetraspanins are the most abundant exosome component[107]. They are enriched 7-124 fold in exosomes compared to the parental cells[128]. Additional abundantly recovered exosome components are adhesion molecules, proteases, MHC molecules, heat shock proteins (HSP), TSG101, Alix, annexins, cytoskeleton proteins (actins, cofilin-1, ezrin/radixin/moesin, profilin-1, tubulins), metabolic enzymes, cytosolic signal transduction molecules and ribosomal proteins. Some of these constitutive exosomal proteins are recruited via their association with proteins engaged in exosome biogenesis, which is well explored for tetraspanin-associated integrins and proteases[129,130], HSP-associated transferrin receptor and cytosolic proteins associated with transmembrane proteins or attached to the inner membrane of invagination prone GEM[131]. Cell type-specific exosomal proteins are most comprehensively explored for cancer/CSC-TEX. Melanoma TEX contain MART1, epithelial cancer cell-derived TEX contain EpCAM and gastrointestinal cancer derived TEX contain cld7, glioblastoma TEX contain EGFRVIII and TEX of docetaxel-resistant prostate cancer cells contain multidrug resistance gene 1[132-134]. TEX also contain c-Met, mutant KRAS and tissue factor[132,135,136]. Notably, all CSC markers are recovered in TEX[137,138].
Exosomes also contain mRNA, rRNA, tRNA, miRNA, lncRNA, mitochondrial DNA and short DNA sequences of retrotransposons[139-141], protected from degradation by the double lipid membrane[142,143]. RNA and DNA sorting into exosomes required further elaboration. Annexin-2 recruits specific RNAs by binding [144]. A zip code in the 3’-UTR guides miRNA recruitment. It is facilitated by coupling of the RNA-induced silencing complex (RISC) to sorting complex components. GW182 containing GW bodies promote continuous assembly/disassembly of membrane-associated miRNA-loaded RISC. Finally, a specific EXO motif (GGAG) controls miRNA loading by binding to the heterogeneous ribonucleoprotein A2B1 (hnRNPA2B1), where sumoylated hnRNPA2B1 binds to an RNA transport signal (RTS or A2RE) in the 3′UTR containing the EXOmotifs[145]. The mechanisms for selective recruitment of lncRNA into exosomes remains to be explored[146].
Though next-generation sequencing can be expected to shortly unravel exosomal DNA, coding and noncoding RNA[147], microarray analysis already provided some valuable information, particularly on exosomal miRNA. MiRNA constitutes only 1%-3% of the human genome, but due to multiple targets, miRNA control about 30% of the coding genes. With perfect base pairing, mRNA is cleaved by Argonaut (AGO), upon imperfect binding, translation is repressed[148]. Knowledge on miRNA greatly fostered progress in oncology. Selected miRNA could be linked to prognosis, disease progression, recurrence and metastasis[149]. miRNA plays an important role in EMT[150], maintenance of CSC[151], tumor invasion, migration and angiogenesis[152]. Most studies being not specifically concerned about TEX CSC miRNA, two publications should be mentioned that described selective TEX miRNA recovery in a subtype of CD44+ breast cancer cells[153] as well as a report on CD133+ melanoma TEX that revealed 49 miRNA not detected in TEX from the parental cells, 20 of these selectively recruited miRNA displaying cancer related function[154]. lncRNA makes up approximately 3% of the exosomal RNA. It also is transferred into host cells. Deep sequencing results are awaited for a profound evaluation on clinical relevance[155] (Figure 1B).
Taken together, CSC/metastasizing tumor cells display SC features, which becomes most prominent during EMT and the establishment of and crosstalk with CSC niches including the premetastatic niche, supposed to be promoted by TEX. Thus, the question arose on the specific equipment of CSC that provides the base of these activities. Besides their functional characterization, CSC are defined by protein marker panels, which are frequently used for CSC/CSC-TEX isolation[119-122]. Functional importance of these CSC markers only recently received attention. We hypothesize that CSC markers are the major players including the assembly of CSC-TEX.
Prominent Pa-CSC markers are CD44v6, c-Met, Tspan8, α6β4, CXCR4, EpCAM and prominin-1 (CD133)[35,156-162], most of which are also recovered in other gastrointestinal CSC. Importantly, these markers were demonstrated to be of functional relevance and to cooperate.
CD44v6 is a CSC marker in PaCa and colorectal adenocarcinoma (CoCa)[35,162-166]. Its functional engagement was repeatedly demonstrated by the impact of CD44v6 overexpression and targeted deletion on metastasis formation[100,167-169].
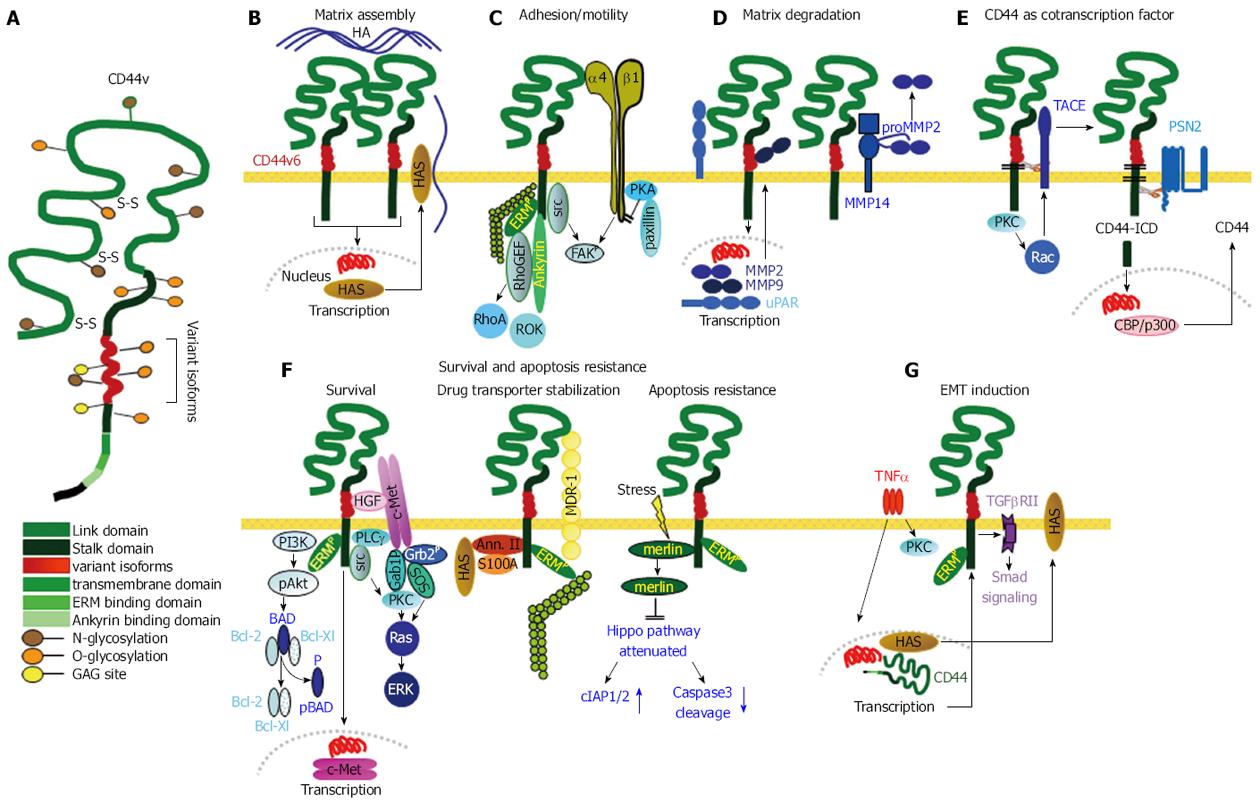
CD44v6 is a splice variant of CD44, an abundantly expressed adhesion molecule and the prime receptor for hyaluronan (HA)[170], the globular N-terminal region also binds collagen, laminin, fibronectin (FN) and selectins[171-173]. CD44v6 contains additional binding sites for the chemokine osteopontin (OPN)[174,175], HGF and VEGF[176,177] (Figure 2A). Via chemokine binding , CD44v6 becomes engaged in motility. OPN is chemotactic and haptotactic and as such important for cell recruitment[178] and motility. Thus, p53koCD44ko mice develop primary tumors at a comparable rate to p53ko mice, but p53koCD44ko tumors do not metastasize[165,179]. CD44v6 has binding sites for cytokines. Via bound cytokines, CD44v6 takes over a coordinating role in RTK activation[180,181], which is detailed below for the cooperation with c-Met. The cytoplasmic tail of CD44 plays an important role in signal transduction. It contains binding sites for the cytoskeletal proteins ezrin, radixin, moesin (ERM) and ankyrin. Ankyrin mediates contact with spectrin and is involved in adhesion and motility[182]. ERM proteins are engaged in regulating migration, cell shape and protein resorting in the plasma membrane[183]. The N-terminus of activated ERM proteins binds to CD44 and the C-terminus binds to F-actin, linking CD44 to the actin cytoskeleton[184]. The binding of CD44 to cytoskeletal linker proteins influences signaling pathways downstream of CD44, which expands the range of CD44-mediated functions. Finally, CD44 can be cleaved by ADAMs and MMP-14[185]. After ectodomain cleavage, CD44 becomes accessible to the presenilin/γ-secretase complex, which triggers intramembrane CD44 cleavage, setting free the CD44 intracellular domain (CD44-ICD). CD44-ICD acts as a co-transcription factor that potentiates beside others CD44, MMP9, MMP3 and HIF2α transcription[186-188]. The last point to mention is of central importance for the functional activity of CD44v6 as a CSC marker. CD44v6 O-glycosylation, the transmembrane region and the cytoplasmic tail affect the membrane subdomain localization, where recruitment into GEM[189] promotes the interaction of CD44 with extracellular ligands and the association with other transmembrane and cytoplasmic molecules[190]. These associations are most crucial for the activity of CD44 in signal transduction, migration, apoptosis resistance, premetastatic niche preparation[191,192] and the cooperation with additional Pa-CSC markers[98], one example being the recruitment of CXCR4 into GEM upon ligand binding, where it associates with CD44[193,194].
Another CD44 feature of special importance for CSC migration is the cooperativity with proteases. CD44 concentrates MMPs at the cell surface and CD44 aggregation via HA binding further facilitates MMP binding[187]. By the interaction with HA the production of uPAR, MMP2 and MMP9 is stimulated[195]. Furthermore, the CD44-ICD binds to a MMP9 promoter response element actively supporting MMP9 transcription[187]. ProMMP2 and proMMP9 become activated through CD44v-associated MMP14. Cell-bound MMPs being protected from their inhibitors, this allows for ECM degradation forming space for invading tumor cells[196]. In addition, TGFβ activation through CD44-associated MMP9, promotes angiogenesis and invasion and several mechanisms of TGFβ-promoted apoptosis become silenced[197,198] (Figure 2B-G).
Finally, as recently reviewed, CD44/CD44v6 and CD44/CD44v regulates miRNA engaged in metastasis[180,199]. First to note, the CD44 3’-UTR binds several miRNA (miR-328, miR-491, miR-671, miR-512-3p) such that collagen 1 and FN are released from repression[200]. Furthermore, upon activation Oct4-Sox2-Nanog are recruited to CD44v3 and translocate into the nucleus, where they initiate miR-302 transcription, which suppresses epigenetic regulators and increases expression of cIAP-1, cIAP-2 and XIAP strengthening drug resistance[201]. We described abundant recovery of miR-494 and miR-542-3p in TEX from a CD44v6+ rat PaCa that promoted cadherin-17 downregulation accompanied by MMP release from repression[202]. These sporadic findings will become consolidated by deep sequencing. Nonetheless, they provide first support for the engagement of CD44/CD44v6 in CSC activities also via miRNA.
Another Pa-CSC marker is the RTK c-Met[156,203], which contribution relies at least in part on its cooperativity with CD44v6. c-Met becomes activated by binding its ligand HGF. As CD44v6 bind HGF, c-Met comes into proximity of CD44v6, which contributes to c-Met activation. c-Met is a transmembrane heterodimer[204]. Upon ligand binding the intracellular tyrosine kinase domain becomes activated through tyrosine phosphorylation in the carboxyterminal end providing docking sites for adaptor and intracellular kinases[205]. The major adaptor protein is Grb2, prominent downstream signaling cascades are MAPK, PI3K/Akt and via these two pathways src, STAT3, nuclear factor κB (NFκB), FAK and β-catenin[206]. CD44v6-initiated c-Met phosphorylation requires the cytoplasmic tail of CD44 and the interaction with ERM proteins for activation of the Ras-MAPK pathway[204], the PI3K-Akt pathway and Wnt/β-catenin signaling[207,208]. In addition, CD44v6 regulates c-Met transcription[100,209]. Similar observations account for the cooperation of CD44v6 with insulin-like growth factor-1- and PDGFR[209,210]. Major cellular responses of c-Met activation include migration, invasion, stemness maintenance, apoptosis resistance and EMT. c-Met can directly interact with E-cadherin, which drives nuclear accumulation of β-catenin and leads to disruption of cell-cell adhesion[211,212].
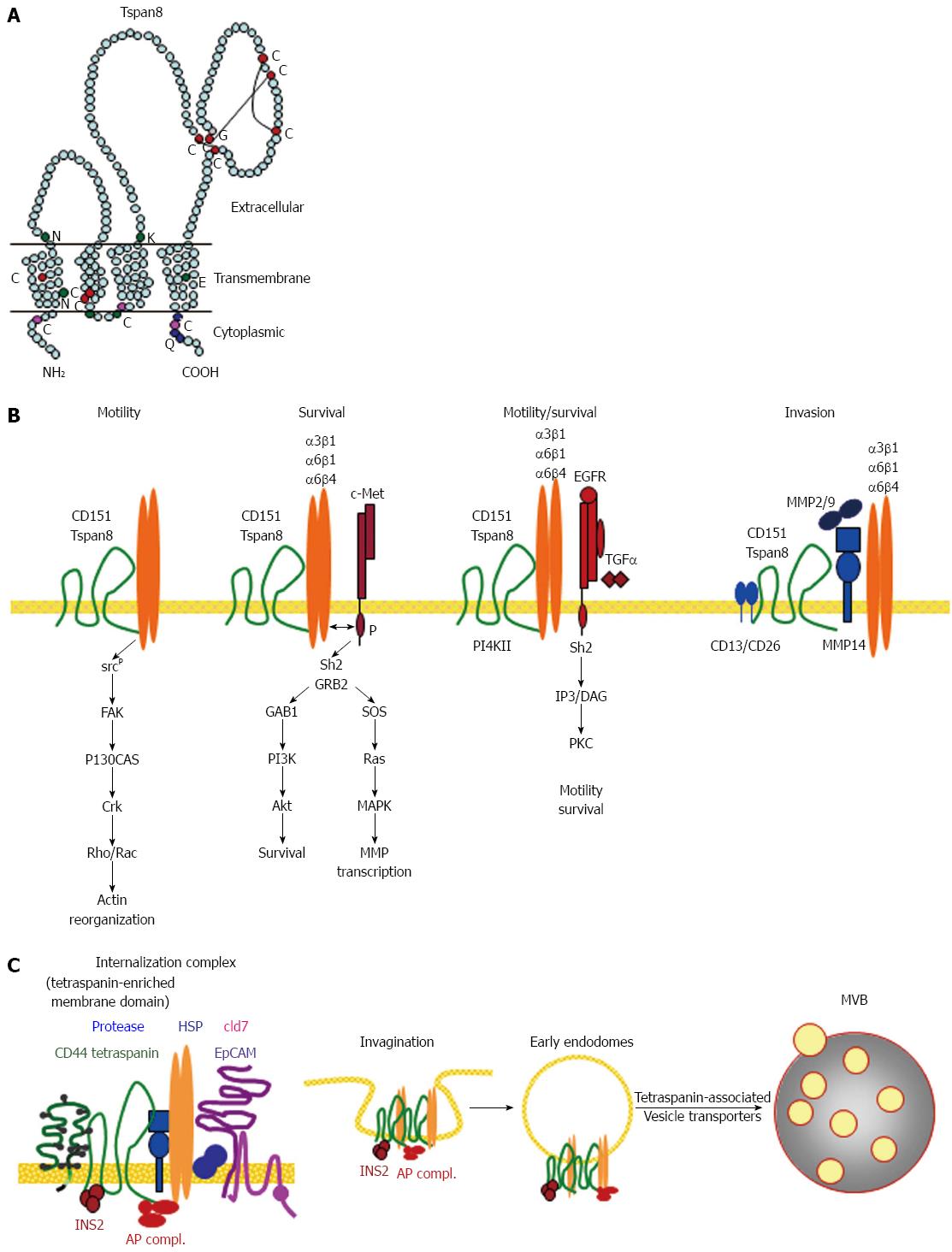
Tetraspanins are a family of small proteins passing the membrane 4 times[213]. Two family members, CD151 and Tspan8 are associated with tumor progression[107,214,215]. For Tspan8 this accounts particularly for gastrointestinal cancer[216-226], where we provided evidence that Tspan8 is enriched in Pa-CSC[35,130,162]. What qualifies Tspan8 as a functionally relevant CSC marker?
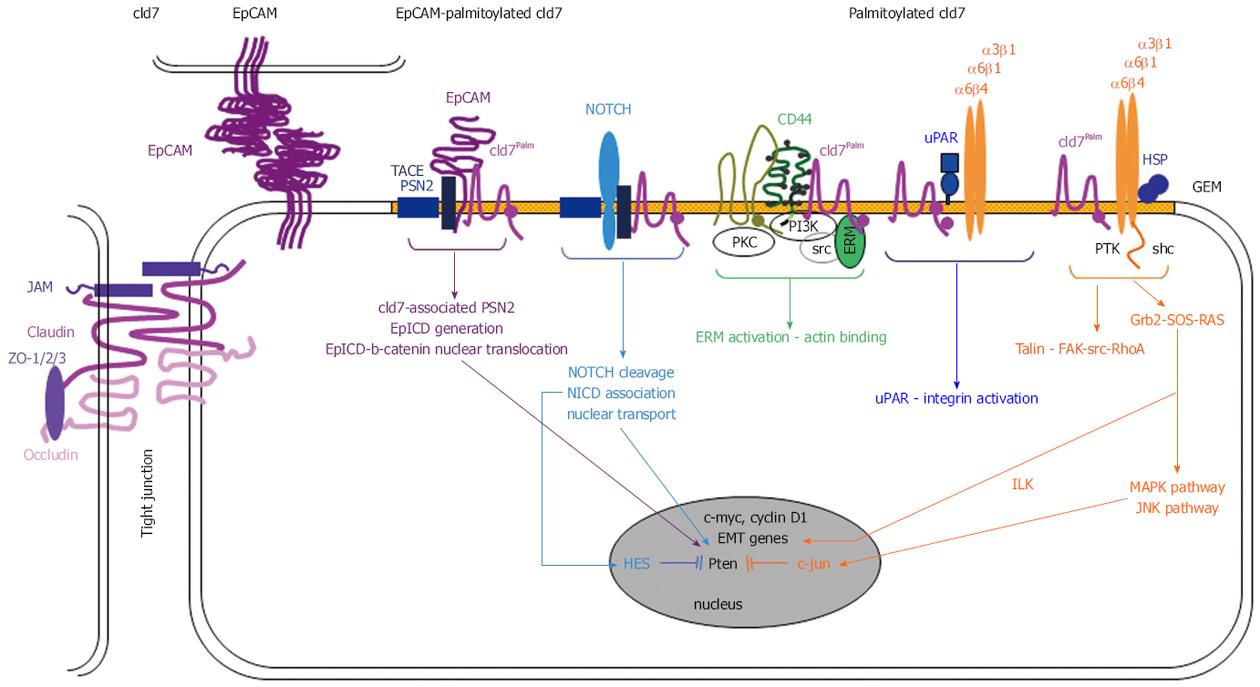
Tetraspanin cross the membrane 4 times with the short N- and C-terminal tails being located in the cytoplasm. Tetraspanins have a small extracellular loop between transmembrane region 1 and 2 and a large extracellular loop between transmembrane regions 3 and 4. The large extracellular loop contains highly conserved cyteines that provide the essential signature of tetraspanins differentiating them from other 4-span molecules. The large extracellular loop accounts for dimerization and for interactions with non-tetraspanin partner molecules. Polar residues in the transmembrane regions stabilize the tertiary structures[227-230]. Palmitoylation is required for initiating tetraspanin-tetraspanin web formation, protects from degradation and provides a link to cholesterol and gangliosides, which supports the formation of GEM[231-236]. Some tetraspanins avail on a tyrosine-based sorting motif that promotes internalization. Yet, internalization can also proceed via associated molecules with a sorting motif[237-239] (Figure 3A).
With few exceptions, tetraspanins have no direct ligands. Instead, they form complexes by interacting between themselves and a large variety of transmembrane and cytosolic proteins[240]. The most prominent tetraspanin partners are integrins[241,242], for Tspan8 particularly α3β1, α6β1 and α6β4[243-245], but α4β1 and α5β1 also associate with Tspan8[246,247]. Proteases are an additional class of functionally important tetraspanin partners[248], Tspan8 associating with the dipeptidase CD26, MMP14, TACE (ADAM17), MMP2 and 9[130,226,245,246,249]. Tetraspanins associate with growth factor receptors[250,251], G protein coupled receptors (GPCR) and their intracellular associated heterotrimeric G-proteins[252] as demonstrated for the relaxin receptor in prostate cancer[253] Prominent cytosolic signal transduction molecules co-immunoprecipitating with tetraspanins are protein kinase C (PKC), a type II phosphatidylinositol 4 kinase (PI4KII) and phospholipase Cγ (PLCγ)[254-256], these associations being also relevant for Tspan8[243,257]. Most important for the activity of Tspan8 as Pa-CSC marker are the associations with α6β4, CD44v6 and EpCAM[243-245,258,259].
Besides providing a signaling platform, tetraspanin complex location in GEM facilitate vesicular fusion and/or fission[107,260-262], which is supported by a tyrosine-based sorting motif of tetraspanins or associated proteins[263].
Taking into account the reversibility of palmitoylation and the instability of membrane microdomains, it can be expected that tetraspanin activities vary considerably depending on the activation state of the cell. The fact that tetraspanins act via laterally associated molecules and only exceptionally via ligand binding, promotes their large array of functions. Nonetheless, there is a common theme. Tetraspanins promote adhesion, spreading, motility, cable formation, invasion, membrane microdomain internalization and vesicle formation. These activities rely on integrin compartmentalization, internalization, modulation of integrin signaling and integrin biosynthesis[241,242,264]. Invasiveness depends on the association with proteases or could proceed through modulating MMP transcription and secretion[245,248]. The involvement of tetraspanins in fusion events has been convincingly demonstrated by the failure of egg-sperm fusion in CD9 and CD81 knockout mice[265], the involvement in cell-virus and cell-parasite interactions[266,267] and their morphogenic features[268,269].
Tspan8 shares most of these activities with other tetraspanins[107]. In gastric cancer Tspan8 promotes metastasis via activation of the MAPK pathway[223]. It contributes in particular via its strong association with α6β4, which is only seen upon α6β4 activation by ligand binding. The Tspan8-α6β4 association strikingly increases tumor cell motility and is accompanied by ezrin, paxillin, src, FAK, and rac/ras activation[245]. Dysregulated adhesion and motility also account for colorectal cancer metastasis[216]. Invasion is supported by the association with TACE, MMP2 and MMP9 and a weak association with MMP14, which could be indirect via the association with CD44v6[245]. In esophageal cancer, too, cooperativity between Tspan8 and ADAM12m promotes metastases[226]. We consider the engagement in EMT gene transcription via its association with β-catenin[130] and Notch[270], also described for CD44[271] and EpCAM/cld7-associated EpCAM[272,273] and the cooperativity with CD44v6, α6β4 and the EpCAM-cld7 complex[98,266] as most important for the contribution of Tspan8 to the CSC phenotype of PaCa (Figure 3B). The contribution of Tspan8 to exosome generation (Figure 3C) and, as outlined below to targeting[107], adds to the central importance of Tspan8 in Pa-CSC.
As mentioned, one of the Tspan8 partners is the α6β4 integrin, the linkage between α6β4 and the tetraspanins CD151 and Tspan8 being repeatedly reported[264,274,275] and ample evidence is provided for the engagement of α6β4 in PaCa progression[130,243,276-280].
The α6β4 integrin is unique in structure and subcellular localization. Distinct to other β chains, the cytoplasmic domain of β4 is over 1000 amino acids long. Towards the C terminus it contains two pairs of type III fibronectin-like modules, which contain tyrosine phosphorylation and proteolytic cleavage sites. Furthermore in the resting state α6β4 is located in hemidesmosomes anchoring epithelial cells via laminin binding to the basement membrane, indicating its interaction with keratin filaments opposing the actin filament association of other integrin β chains[281]. However, upon stimulation, e.g., by wounding, stress and in tumor cells, hemidesmosomes become disassembled and α6β4 is driven into GEM, preferentially in F-actin protrusions[207,264,282-284]. Palmitoylation of the β4 chain support the GEM localization and β4 initiated signal transduction[285,286]. Upon disassembly of hemidesmosomes, the β4 cytoplasmic domain becomes phosphorylated preferentially via PKCα[287,288]. Phosphorylated α6β4 binding to laminin activates both PI3K and ras homolog family member A (RhoA) small GTPases[280,289,290]. Alternatively to laminin binding, α6β4 activation can be initiated by cooperation with growth factor receptors including ErbB-1,2,3 and c-Met[207,290-296], which promotes activation of PI3K, Akt, MAPK, and Rho small GTPases pathways[207,289,297-299].
α6β4 affects cell survival and angiogenesis[244,289,297,300,301] and was reported to alter expression of > 500 genes[302]. Its dominating activity relies in promoting tumor cell invasiveness[130,274,278,279,290], which fits well to its association with tetraspanins in GEM. Notably, there is evidence for engagement in stemness[35,130,162,303-306]. In PaCa it is predominantly associated with Tspan8 and expression is upregulated in Pa-CSC[35,162]. The impact of this association may gain further weight by the joint recovery in PaCa TEX[130,204].
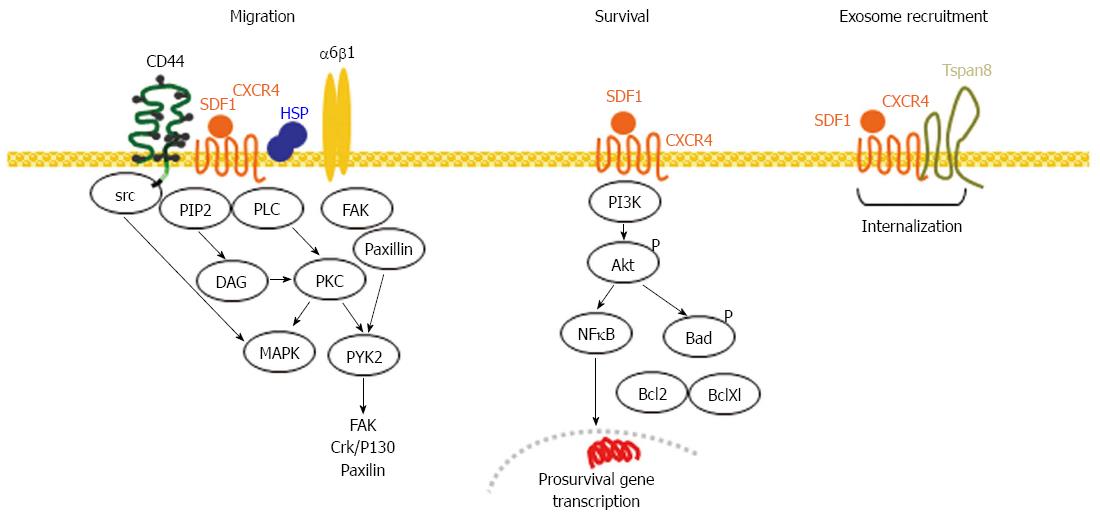
CXCR4 is a G protein-coupled chemokine receptor[307], upregulated in CSC, particularly migrating CSC[308] including metastatic PaCa and lung cancer cells with CSC-like properties, which show upregulated CXCR4 and CD133 expression[309,310]. CXCR4 is suggested to contribute to tumor growth, angiogenesis, therapy resistance[90,311-313] and to have a strong impact on metastasis including the recruitment to specific sites such as the bone marrow[314]. In 85% of PaCa CXCR4 expression is increased and was identified as an independent factor for poor prognosis[162,315,316].
After stromal-derived factor (SDF)1 binding CXCR4 and possibly extracellular HSP90 colocalize to lipid rafts, which facilitate together with HSP90 signal transduction[317]. Activated CXCR4 increases intracellular calcium levels and induces a phosphorylation cascade, which is terminated by CXCR4 internalization[318]. After chemokine binding the heterotrimeric G protein is activated and dissociates in GTP-bound α and βγ subunits. Cell motility is regulated by several phosphorylation cascades, which include src and Akt as the central node. Akt phosphorylates several downstream targets that reorganize actin fibers. The βγ subunit activates PLCβ and PI3K. PLCβ cleaves PIP2 in IP3 and DAG, where IP3 induces the release of Ca from intracellular stores. DAG together with Ca activates PKC and MAPK. PI3K activation leads to activation of focal adhesion components and cytoskeletal proteins contributing to reorganization of the actin cytoskeleton. Actin polymerization is stabilized by HSP90, which promotes the formation of filipodia and directed cell migration[319]. Activated PI3K additionally activates via Akt the mitochondrial antiapoptotic signaling pathway[320]. Activated Akt also contributes to β-catenin stabilization and gene transcription[321]. Signaling through Gαi is linked to transcription through PI3K/Akt, NFκB, mitogen-activated protein kinase kinase 1/2 and leads to activation of the Ras and Rac/Rho pathways[322]. Ligand binding induced dimerization results in G-protein-independent signaling with activation of the JAK/Stat pathway[323], which might be accompanied by polarization[324]. Finally, CD44 binding to human epidermal growth factor receptor 2 (HER2) supports CXCR4 expression in gastric cancer by suppressing transcription of miR-139, which targets CXCR4[325].
There are several reports on the association of CXCR4 with tetraspanins in hematological malignancies[326,327], where the GEM located complex cointernalizes and is recovered in TEX[328]. We recovered CXCR4 and Tspan8 in PaCa TEX[35,130] and CXCR4 expressing TEX from a metastatic CoCa line promote metastasis formation of poorly metastatic lines. The authors speculate that this is due to recruiting CXCR4+ stroma cells to create a metastasis-permissive environment[329].
In brief, CXCR4 increases the motility of metastasizing CSC. Recruitment into GEM facilitates cooperativity with addition GEM-located CSC markers as well as internalization and recovery in TEX (Figure 4).
EpCAM (EpC) is a prominent CSC-marker in colorectal, pancreatic, liver and breast cancer[330-332], but information is limited, whether EpC fulfills CSC-related tasks[333-336]. In gastrointestinal cancer evidence was provided that CSC activity of EpCAM requires support by claudin 7 (cld7)[259,273,337-341].
EpC is a tetramer forming transmembrane molecules, which mediates homophilic cell-cell adhesion[342]. This weak homophilic binding is only seen in E-Cadherin cells due to EpC interfering with E-cadherin via disrupting the link between β-catenin and F-actin[343]. Due to a response element to the Wnt downstream effector Tcf4 it fosters Wnt signaling responses[52,344]. However, EpC can also act as a Wnt derepressor via sustaining Lrp6 (LDL receptor related protein 6) retention[345]. EpC also can control motility via down-regulation of PKC[346] and by regulating MMP7 expression[347,348]. These activities are promoted by the cytoplasmic tail of EpCAM (EpICD), which forms a complex with β-catenin, FHL2 (four-and-half-LIM-only) and Lef-1. The complex relocates to the nucleus, initiating, c-myc, cyclinA and E transcription[349]. The finding that EpC cross-linking triggers TACE (TNFα converting enzyme), which cuts the extracellular domain such that the membrane-anchored intracellular domain becomes accessible to PSN2 (presenilin 2 N-terminal fragment), which cleaves the intracellular peptide, EpICD, opened a new window towards the activity of EpC as a CSC marker[11]. EpICD also initiates transcription of additional reprogramming genes like Oct4 and Nanog, which is accompanied by EMT with upregulation of vimentin, Snail, Slug and downregulation of E-cadherin in a murine colon cancer and a human hepatoma line[350]. This study did not take into account the expression of cld7. However, hepatocyte progenitors express, besides EpC, cld7[351] and in CoCa and PaCa, EpC associates with cld7[235]. Under physiological conditions, too, the EpC-cld7 association is vital, an EpCko mouse dying within one week after birth due to intestine destruction, which relies on the missing association of EpC with cld7[352]. These findings pointed towards a concerted activity of EpC and cld7 in tumor progression, which was confirmed by a cld7kd and an EpCkd in a metastasizing line. Both knockdowns sufficed to wave metastatic growth[341].
Claudins, four-pass transmembrane proteins, were first described as TJ components that are engaged in sealing, formation of ion channels and organization of paracellular small organic solute flux[353-355]. The importance of clds, including cld7, was repeatedly demonstrated by targeted deletion. A cld7ko is lethal within 10 d after birth due to intestine destruction[356]. The authors speculate that gut destruction is promoted by a missing association with integrins and upregulation of MMPs. An intestine-specific conditional cld7ko mouse revealed a specific enhancement of paracellular small organic solute flux across the TJ including a major bacterial product that initiates colonic inflammation[357].
However, claudins are also found outside of TJ[358-362]. Claudins are PKA, PKC and myosin light chain kinase targets[363-367]. Importantly, cld phosphorylation can prohibit integration into tight junctions with the consequence of loss of epithelial cell polarization[368-370]. Cld7 also has palmitoylation sites[36,356,371] and palmitoylated cld7 is excluded from TJ[371], but partitioned into GEM, where it is associated with monomeric EpCAM[273,341,372]. As already mentioned, GEM harbor palmitoylated proteins and act as a scaffold for signal transduction and reorganization of the cytoskeleton[373-376]. GEM-located, palmitoylated cld7 promotes tumor progression by supporting motility and invasion. This was confirmed in PaCa and CoCa for the EpC-cld7 complex, which promotes motility and invasion[259,341,372] as well as drug resistance that is initiated by downregulation of Pten[341]. There is additional evidence for a shift towards EMT gene expression[273], palmitoylated cld7 contributing to the generation of EpICD[371], facilitated by the GEM location of TACE and PSN2. Further supporting the cld7-EpC complex functioning as a CSC marker, triple negative breast cancer cells are cld7-, but cld7-associated rab25 is expressed in breast-CSC[377-379]. Finally, outlined above, GEM are prone for internalization and recruitment into exosomes, which facilitate the metastatic process[380], where we experienced that cld7 actively contributes to the vesicle transport via associating with vesicle transporters. In CoCA and Pa-CSC the EpC-cld7 complex is recovered in TEX[273,361].
Taken together, cld7 and palmitoylated cld7 apparently account for distinct, non-overlapping activities such that dependent on the cellular context, the functional engagement in TJ or in GEM is dominating. Only GEM-located, palmitoylated cld7 displays CSC activity, where EpC contributes due to its association with GEM-located cld7. The main activity of this CSC marker complex builds on apoptosis resistance and EMT gene expression (Figure 5). A contribution of cld7 to TEX biogenesis might further strengthen the impact on CSC activity.
Prominin-1 (CD133) is a CSC marker in several cancer entities[381-384], including PaCa[156,308,385-390]. CD133 is a pentaspan protein[391,392]. It is suggested to be associated with the Notch pathway, which is accompanied by slow cell cycling and increased drug resistance[393,394] as well as Hedgehog signaling with an increased capacity of anchorage independent growth[395]. CD133 is also engaged in Akt, JNK, mTOR, MAPK and IL-8/CXCL1 signaling cascades[396]. These findings are well in line with CD133 supporting maintenance of stemness and point towards a possible engagement in EMT gene transcription. Furthermore, it is well documented that CD133 interacts with cholesterol and is concentrated in different types of membrane protrusions with different types of cytoskeletal bases, i.e., actin for microvilli and tubulin for cilia. These different membrane protrusions also appear to be released in at least two types of vesicles[396,397]. The smaller vesicles resembles exosomes containing all the constitutive exosomal proteins and the exosomal lipid profile. These exosomes, which also contain prometastatic proteins like CD44 and ADAMs, are taken up by tumor cells and bone marrow derived stroma cells, the transfer of CD133 being accompanied by increased invasiveness and metastatic potential[154]. Whether the second type of exosomes proceeds via the PLP pathway[110], which could be suggested by the interaction of CD133 with cholesterol, remains to be elaborated. Irrespective of their origin, CD133+ TEX are recovered in CoCa and PaCa[35,159,361].
Taken together, CD133 is engaged in multiple signaling pathways linked to metastasis and EMT. CD133 also is another Pa-CSC marker that is constitutively located in internalization-prone membrane domains and is recovered in TEX.
In brief, the dominating features of the Pa-CSC markers are their connectivity, their engagement in multiple signaling pathways and their location in internalization prone membrane domains, which accounts for the enriched recovery in TEX. By these characteristics, Pa-CSC markers are prone to contribute to motility, invasiveness and EMT. Via their enrichment in TEX they appear destinated for the crosstalk with the host and non-CSC.
There are different modes, whereby Pa-CSC markers can contribute to EMT, markers can be engaged in the regulation of EMT gene transcription factors, EMT gene related miRNA processing or can be targets of miRNA. Last, not least, they can be engaged in the transfer of EMT transcription factors or miRNA into TEX, where TEX could become the actual transporter of EMT. So far information on these topics are rather limited. One hindrance being the transient nature of EMT, which becomes aggravated by the definition of CSC as a population of cells, enriched but not purified by a variety of distinct procedures. An additional hindrance relies on the evaluation of overall expression of CSC markers, which does not take into account that CSC markers are mostly recruited into GEM, where they can fulfill distinct or opposing functions compared to activities outside of GEM, like anchoring epithelial cells to the lamina basalis (α6β4) or contributing to epithelial cell sealing (cld7). Nonetheless, there are reports describing regulation of CSC markers by EMT genes and vice versa.
There are several reports on the engagement of CD44 in EMT gene regulation. In PaCa Snail-1 is a downstream target of CD44. Snail regulates MMP14 expression, which supports invasion[398]. Another EMT transcription factor linked to CD44 is Zeb1. There is a self reinforcing feedback loop as Zeb1 and CD44 mutually sustain their expression. Notably, this study also describes an inverse linkage to CD44v expression, which is due to Zeb1 suppressing transcription of the epithelial splicing regulatory protein 1 (ESRP1)[399]. An excess of HA production also drives EMT, accompanied by upregulation of TGFβ and induction of Snail and Twist. Accordingly, inhibition of TGFβ-Snail signaling or Twist silencing abrogated the entrance into a stem cell state[400]. Furthermore, STAT3 is physically linked to CD44 and NFκB. This initiates the activation the catalytic subunit of telomerase (hTERT), which functions as a transcription cofactor in EMT[401]. Overexpression of Notch-1 induces CD44 and EpC expression and increases the formation of PaCa sphere formation, accompanied by the induction of the EMT markers Zeb1 and Hes-1[402]. In thyroid Ca, CD44-ICD binds to CREB, which promotes cyclinD1 transcription[403] and in hepatocellular CA, a CD44/TM4SF5 (tetraspanin L six family member 5) association leads to activation of src, STAT3, Twist1 and Bmi1, supporting establishing the CSC phenotype and EMT[404]. In CoCa the CD44-HA ligation initiates src activation, which supports Snail activation that represses the stemness inhibitor miR-203[405]. Finally, GEM-located CD44 becomes internalized and migrates together with acetylated STAT3 to the nucleus. Nuclear CD44 binds to the promoters of several genes including c-myc and Twist1, promoting the EMT shift[406].
The tetraspanin TM4SF5 also is involved in EMT induction. TGFβ1-mediated Smad activation causes TM4SF5 expression, EMT and EGFR pathway activation. The finding that inhibition of EGFR activity abolished EMT suggests a link between Smad and the EGFR in TM4SF5 expression. In fact, inhibition of Smad or the epidermal growth factor receptor (EGFR) blocked TM4SF5 expression and EMT[407]. In human hepatocellular carcinoma cell lines TM4SF5 expression correlates with enhanced p27Kip1 (cyclin-dependent kinase inhibitor 1B) expression and cytosolic stabilization. Cells acquire an elongated phenotype, which relates to RhoA inactivation and loss of E-cadherin expression is accompanied by EMT[408]. In glioma, KITENIN (VANGL planar cell polarity protein 1), a tetraspanin partner, induces expression of the EMT markers N-cadherin, Zeb1, Zeb2, Snail and Slug and expression of the CSC markers CD133, aldehyde dehydrogenase 1 and ephrin receptor B1[409]. Signaling through TIMP-1 (metallopeptidase inhibitor 1) induces in breast cancer in dependence of CD63 Twist1 expression, where a knockdown of Twist1 rescues E-cadherin expression[410]. In PaCa, upregulation of Notch-1 depends on Tspan8, similar effects being not induced by CD151[130]. Instead, in mammary progenitor cells CD151 accounts for nuclear distribution of Slug and represses mammary branching morphogenesis[306], whereas in ovarian cancer the CD151-α3β1 complex represses Slug-mediated EMT and Wnt signaling[411]. Similar, highest level of CD63 in melanoma revealed a significant resistance to undergo an EMT program[412].
The CSC marker CXCR4, too, was described to contribute to EMT. Constitutively active CXCR4, but not wild type CXCR4 induces EMT in mammary carcinoma cells, characterized by upregulation of Zeb1, upregulation of cadherin 11, p120 isoform switching, activation of ERK1/2 and MMP2, but loss of E-cadherin. In 3-dimensional cultures, wt CXCR4 also suffices promoting EMT, which is accompanied by CXCR2, CXCR7, CXCL1, CXCL8, CCL2, IL6 and GMCSF expression. Inhibition of CXCR4 together with MAPK1 or PI3K reversed the EMT phenotype[413]. UHRF1 (ubiquitin-like, with PHD and RING finger domains 1) plays a crucial role in DNA CpG methylation, chromatin remodeling and gene expression. Downregulation of UHRF1 induces Zeb1 and Snail expression accompanied by decreased E-cadherin and increased N-cadherin and vimentin expression. The authors speculate that activation of the CXCR4 signaling pathway is of central importance[414].
EpC is well accepted as a CSC marker, but reports on its contribution to EMT are opposing. One study with breast cancer cells reports on the contribution of EpC in TGFβ1-induced EMT. TGFβ1 treatment induced EpC expression, which promoted EMT and cell migration. EpC overexpression further enhanced TGFβ1-induced EMT. TGFβ1 treatment induces JNK phosphorylation that promoted increased Jun and Fos expression suggesting an important role of EpC in the induction of EMT via JNK signaling[415]. Opposing findings were reported for prostate cancer, where EpC was repressed upon induction of EMT. miR-200c and miR-205 are two inducers of MET (mesenchymal-epithelial transition). Re-induction of the epithelial phenotype through miR-200c and miR-205 was accompanied by EpC reexpression[416]. Instead, we reported on unaltered EpC and increased cld7 expression in PaCa and CoCa spheres/holoclones and migrating tumor cells[341]. Recruitment of monomeric EpC into GEM via palmitoylated cld7 and EpC cleavage could well account for EpC initiating pronounced EMT induction[273,371]. Furthermore, we and other groups reported on upregulation of GEM-located palmitoylated cld7 in CSC and a pronounced release of the EpC-cld7 complex into TEX[273,361], which promote Snail, Slug and Twist expression[273]. Opposing findings have also been reported, where a knockdown of cld7 induced EMT. A cld7 signature gene profile revealed highly upregulated Rab25, a CoCa suppressor and regulator of polarized cell trafficking in cld7 overexpressing cells. Rab25 silencing counteracted the effects of cld7 expression and increased p-src and Erk1/2 expression[417]. The study did not take into account the engagement of rab25 in vesicle traffic. Further elaborating the recruitment of the EpC-cld7 complex into GEM and exosomes may clarify these seemingly opposing findings.
Finally, CD133 overexpression induces “stemness” properties in PaCa cells and EMT. EMT induction and increased invasiveness are mediated by NFκB activation[418].
Thus, CD44v6, c-Met, Tspan8, α6β4, CXCR4 and CD133 are engaged in promoting EMT. We and others provided evidence for a contribution of an EpC-cld7 complex in EMT. However, this topic is still controversial.
There is abundant information on altered miRNA profiles in cancer, including CSC and tumor cells in EMT. For more detailed information on miRNA in PaCa excellent reviews are available, besides others in[137,419-422]. Thus, we will mention only a few publications referring explicitly to the mutual impact of CSC markers on miRNA and vice versa.
HA-activated CD44 binds Twist, which supports transcription of miR-10b, which blocks the tumor suppressor HOXD10 allowing for RhoA and ROK activation with consequences on organization of the cytoskeleton/tumor cell motility as well as apoptosis resistance via activation of the PI3K/Akt pathway. Activated CD44 also binds to Nanog, which together with Stat3 translocates to the nucleus and initiates miR-21 transcription, which downregulates the tumor suppressor PDCD4 and promotes expression of survival proteins[423]. HA-activated CD44v3 interacts with Oct4, Sox2 and Nanog, stimulating miR-302 expression, which leads to downregulation of epigenetic regulators and activation of survival proteins[424]. CD44-bound HER2 induces histone deacetylation accounting for transcriptional repression of miR-139, which targets CXCR4, the finding providing a link between upregulated expression of CD44 and CXCR4 in gastrointestinal CSC[325]. Notch-1-induced increased miR-21 and decreased miR-200b, miR-200c, let-7a, let-7b and let-7c expression is accompanied by upregulation of the CSC surface markers CD44 and EpC[402]. Up-regulated miR-155 significantly increases the population of CSCs as well as EMT in liver cancer cells via silencing TP53INP1 (tumor protein p53 inducible nuclear protein 1), changes being initiated by TGFβ1 that indirectly regulates TP53INP1 via induction of miR-155[425]. miR-34a induces MET via down-regulation of Snail by binding to the Snail 3’-UTR, which is accompanied by down-regulation of Bmi1, CD44, CD133, olfactomedin and c-myc. Conversely, Snail and Zeb1 bind to E-boxes in the miR-34a/b/c promoters, which represses miR-34a and miR-34b/c expression. Thus, inactivation of miR-34a/b/c, which is frequent in cancer, can shift the equilibrium of these reciprocal regulations towards EMT[78]. Sonic hedgehog signaling also becomes engaged in EMT by downregulation of miR-200b and let-7c with concomitant upregulation of CSC markers[426]. In CoCa, miR-142-3p targets CD133, Lgr5 (leucine-rich repeat containing G protein-coupled receptor 5) and ABCG2, where Oct4 suppresses miR-142-3, expression being particularly low in CSC-enriched spheres[427]. In PaCa miR-34 is lost in the population of CSC, which is accompanied by Notch and Bcl2 pathway activation, transcription of miR-34 being regulated by p53[428]. However, it should be mentioned that most of these studies were oriented towards therapy and evaluated in first instance the regulation of EMT transcription factors, their reduction expectedly correlating with CSC marker expression, which excludes in several instances a statement on a direct impact of these miRNA on CSC marker expression. A miRNA analysis of rat and human PaCa with downregulation of the CSC markers CD44v6, EpC, cld7 and Tspan8[35,202] confirmed low level miR-34a recovery in CD44v6-competent PaCa and upregulated expression in CD44v6kd PaCa, which is in line with miR-34a targeting CD44[429]. Furthermore, miR-103 transcription is more than two-fold increased in TEX from CD44v6-competent compared to CD44v6-deficient cells. As c-Met supports miR-103 transcription[430], the finding indicates that via CD44v6 c-Met also becomes engaged in miRNA transcription and/or posttranscriptional regulation. Finally, CD44v6-related changes are mostly reflected in the TEX miRNA profile such that miRNA reduced in CD44v6kd cells is also lower in TEX from CD44v6kd than CD44v6-competent cells[202]. Tspan8 and cld7 exerted a pronounced effect mostly on miRNA known to be engaged in EMT gene expression. The functional relevance remains to be explored.
In brief, there is evidence for an impact of CSC markers on miRNA expression/repression. miRNA also affects CSC marker expression directly or via EMT genes and involved signaling pathways. Still, we are far from having a precise overview of these interlinked networks.
We already outlined the engagement of Pa-CSC markers in TEX biogenesis, where GEM located Tspan8 plays a decisive role in early endosome formation[124,129]. CD44v6, α6β4, the EpC-cld7 complex and partly CD133 are co-recruited due to enrichment in these tetraspanin-dominated microdomains. According to unpublished findings, palmitoylated cld7 is actively engaged in early endosome traffic towards MVB and the release of ILV as exosomes. Fittingly, Tspan8, α6β4, CD44v6, cld7 and CD133 are enriched in TEX compared to Pa-CSC[162]. Comparative analyses of miRNA in TEX derived from Pa-CSC marker-expressing vs -depleted cells confirmed enriched recovery of EMT-related miRNA in Pa-CSC TEX and indicated an additional loss, respectively, enrichment of several miRNA related to the metastatic process, which still requires elaboration of the routing into TEX[202]. Similar findings were reported at the proteome level by the group of Rak. TEX from A431 cells that were driven into EMT exhibit profound qualitative differences in their proteome compared to TEX from the parental cells, but also differed from the A431-EMT cells with 30 proteins related to growth, signaling and motility being uniquely recruited into A431-EMT-derived TEX. The authors propose that changes in the cellular differentiation status translate into unique qualitative rearrangements in the cargo of TEX[431]. Along this line, the oncoprotein latent membrane protein 1 (LMP1) recruits HIF1α into TEX of nasopharyngeal carcinoma. TEX HIF1α remains function-competent in recipient cells, LMP1+ and HIF1a+ TEX initiating EMT with reverting the expression of E- and N-cadherins in TEX target cells[432].
The power of exosomes relies on their ubiquitous presence, their particular protein, mRNA, ncRNA and DNA profile and their most efficient binding and/or transfer in target cells. Information on the latter aspect, though a prerequisite for clinical translation, is still limited.
Binding of PaCa TEX to the extracellular matrix (ECM) varies with the adhesion molecule profile of the exosomes. Thus, high CD44 expression is accompanied by HA binding and high α6β4 expression by laminin (LN) 332 binding, the findings being confirmed by antibody blocking[433]. Myeloma cell line- and myeloma patient-derived TEX revealed fibronectin as key heparan sulfate-binding ligand and mediator of TEX-cell interactions, where removal of heparan sulfate from TEX dramatically inhibiting TEX-target cell interactions. The authors describe a dual role of heparan sulfate in TEX-cell interaction. TEX heparan sulfate captures FN. Concomitantly it acts as a FN receptor on target cells[434]. Live-cell imaging also revealed a critical role of FN and integrin cargo sorting into TEX, which promoted persisting cell motility[435]. In line with the latter report, there is abundant evidence for the engagement of integrins in exosome binding. During reticulocyte maturation, integrin α4β1 is recruited into exosomes, which bind to FN. The interaction depends on divalent cations and is inhibited by an α4-specific antibody, the authors speculating on functional activity of exosomal α4β1 by binding to endothelial cells through CD54[436]. B cell exosomes also interact with the ECM and fibroblasts viaβ1 and β2 integrins, antibody blocking studies confirming engagement in adhesion to collagen-I and FN and to activated fibroblasts via TNFα[437]. TEX of a PaCa transiently interfered with leukocyte migration. This is due to TEX occupying the migration-promoting receptors CD44, α4, CD62L and CD54[438]. T cells, too, recruit dendritic cell (DC) exosomes not via the T cell receptor complex, but via leukocyte function-associated antigen-1 (LFA1)[439]. Most impressive has been the elucidation that TEX integrin profiles account for the organ preference of metastasis initiated by formation of a premetastatic niche. A proteome analysis revealed distinct integrin expression patterns in subpopulations of TEX. Notably, exosomal integrins α6β4 and α6β1 were associated with lung metastasis, whereas exosomal integrin αvβ5 was linked to liver metastasis. A blockade of α6β4 or αvβ5 decreased TEX uptake, as well as lung, respectively, liver metastasis. Furthermore, TEX from mouse and human tumors are preferentially taken up by resident cells at their predicted metastatic destination, i.e., TEX of tumors metastaizing to the lung are taken up by lung fibroblasts and epithelial cells, TEX of tumors that metastasize to the liver are captured by Kupffer cells and TEX from tumors metastasizing to the brain are recovered in brain endothelial cells (EC). Finally, TEX integrins displayed functional activity, activating Src phosphorylation and pro-inflammatory S100 gene expression after uptake by resident cells[440]. These studies confirmed and expanded our previous work that described distinct TEX integrins to target e.g., EC, fibroblasts or bone marrow cells, where the selectivity of TEX uptake is guided or, at least, facilitated by the engagement of protein complexes at the exosome and the target cell membranes[441]. In fact, only defined tetraspanin-integrin complexes are taken up by selected target cells. Importantly, TEX uptake proceeds via binding to internalization prone microdomains[129]. The constitutively high expression of GEM-located tetraspanins and the multitude of associated molecules, with a preference for integrins[107], favors our suggestion. Besides supporting the selectivity of binding and uptake, the engagement of complexes of TEX receptors and target cell ligands favors induction of signal transduction as e.g., known for T cell activation, which requires engagement of the T cell receptor and accessory molecules that interact with MHC and costimulatory molecules on DC[442]. So far we supported our hypothesis by elaborating that TEX expressing Tspan8 and α4β1 preferentially target EC and promote EC and EC progenitor activation[247], where exosomes from Tspan8 and α4 transfected fibroblasts exhibited a comparable target cell selectivity[129]. Instead, PaCa TEX expressing Tspan8 and α6β4 preferentially bind and are taken up by lymph node stroma cells and lung fibroblasts[130], lymph nodes and lung being the exclusive metastatic sites for this PaCa[443].
Taken together, for GEM-derived TEX there is strong evidence for preferential uptake by corresponding, internalization prone membrane microdomains. Furthermore, the work by the Lyden group depicting TEX integrins accounting for metastasis organ preference[440] and our work on the engagement of tetraspanin-integrin complexes facilitating selective targeting[129,130,247,443] provides a solid base for defining GEM-derived TEX target structures. Comparable studies for TEX uptake via phosphatidylserine receptors, by phagocytosis, macropinocytosis and membrane fusion[444-449] are still awaited (Figure 6A).
In advance of reviewing the impact of Pa-CSC markers on angiogenesis and the premetastatic niche, we want to refer to excellent reviews that elaborate the impact of TEX on tumorigenicity[98,450], tumor growth related thrombosis[451-453], hematopoiesis[199,454,455] and mature leukocytes, including all components of the immune system[456-463], where particularly the Pa-CSC TEX markers CXCR4, CD44v6 and c-Met may play a role.
There is ample evidence on the engagement of TEX in angiogenesis. It was first described for TEX of a non-metastatic rat pancreatic cancer that induced overshooting angiogenesis resulting in a lethal consumption coagulopathy[464]. TEX were preferentially taken up by EC and EC progenitors, binding and uptake requiring a Tspan8-α4β1 complex. Notably, by exchange of α4β1 by α6β4, TEX did not bind to EC and overshooting angiogenesis was prevented[246]. Uptake of Tspan8-α4β1 TEX by EC resulted in upregulation of tissue factor, VEGFR1, CXCL5, CCR1 and HMOX1 as well as of Tpan8 and CD31. Depending on the culture condition, progenitor cells could also be driven into smooth muscle cell differentiation[250]. We are not aware on further studies on Pa-CSC TEX markers in angiogenesis. Therefore, and as TEX-induced angiogenesis meanwhile is described in nearly all tumor entities, we refer to some reviews on TEX-initiated signal transduction in EC as well as on the engagement of transferred miRNA[152,465-467]. However, we want to mention that to our knowledge, the first report on exosomes induced angiogenesis referred to platelet-derived exosomes[468], which we interpret as an additional evidence that CSC take over physiological programs including the use of exosomes.
Paving the way for metastasizing tumor cells: Exosomes are rich in function-competent proteases. Exosome proteases can modulate the exosome protein profile, the ECM and/or target cells. Besides others, MMP2, 7, 9, 14, ADAM10, 15, 17, ADAMTS1, 13 and several dipeptidases were recovered in TEX[469,470]. These TEX proteases can modulate the TEX protein profile, which includes the Pa-CSC markers CD44, shedded by ADAM10, MMP14 and MMP9[471-473], and EpC, shedded by ADAM14[474]. Besides this internal regulation of CD44v6 and EpC expression in TEX, frequently accompanied by release of the ICD, which in turn promotes transcription of genes promoting tumorigenicity and metastasis[187,349,350], the association of TEX CD44v6 and Tspan8 with proteases severely affects the host matrix. The modulated matrix, in turn, facilitates metastasizing tumor cell migration towards the metastatic organ.
HA is the most abundant ECM protein, with TEX binding via CD44[170,475]. Notably, TEX also contain HAS and Hyal and were described to be HA-coated. The authors speculate that TEX serve as special vehicle for HA, where exosomal HA itself or associated molecules could create an environment supporting cancer cell invasion and metastasis[476]. In concern about the contribution of CD44v6, we noted in some, but not all tested TEX of PaCa-CD44v6kd lines a reduction in HAS3 and upregulated expression of Hyal1. In addition, CD44v6-competent, but not CD44v6-deficient TEX-modulated HA promotes tumor cell migration[100].
CD44 regulates expression and cooperates with several proteases[195,196,477], where MMP2, MMP3, MMP7, MMP9, MMP14 as well as ADAM10 and ADAM17 are recovered in PaCa TEX and MMP9, MMP14 and ADAM17 are strongly downregulated in TEX of CD44v6kd lines[433]. These proteases coimmunoprecipitate with CD44v6 in PaCa-TEX, indicating their recruitment into TEX via associated CD44v6[433]. CD44v6-competent PaCa TEX degrade coll I, coll IV, FN, LN111 and, less pronounced LN332, matrix degradation by PaCa TEX being accompanied by pronounced tumor cell migration and invasion[433]. Similar findings were reported for MMP14, where the authors suggest that coll IV, which is not a MMP14 target, becomes degraded by MMP14-activated proMMP-2[470]. Finally, host matrix degradation by CD44v6-competent TEX is accompanied by activation of proliferation and survival signals[433]. This is likely due to liberation of growth factors, chemokines and additional proteases from the degraded matrix as well as by cleavage of additional targets by the TEX proteases[207,478].
Tspan8 also associates with proteases, particularly MMP9 and TACE[245] and Tspan8-associated proteases are recovered in PaCa TEX, where they degrade the host matrix[130]. The efficacy of Tpan8-expressing TEX appears to exceed that of CD44v6+ TEX, which likely is due to the strong association of tetraspanins with integrins[241,242]. Thereby matrix protein binding becomes focalized, strengthening the efficacy of matrix degradation. This accounts in particular for LN332 degradation. Due to its association with TACE, Tspan8 also contributes to FN degradation[130]. Though we focused on the contribution of the Pa-CSC marker Tspan8 in matrix modulation, other TEX tetraspanin-protease complexes also contribute to host matrix modulation[130,460,479-484].
In brief (Figure 6B), TEX proteases modulate the ECM thereby creating a path for migrating PaCa cells and a milieu favoring tumor cell migration, angiogenesis and premetastatic niche establishment. The Pa-CSC markers CD44v6 and Tspan8 essentially contribute to the process of matrix modulation by TEX due to their engagement in protease transcription (CD44v6), TEX biogenesis (Tspan8) and their association with proteases in GEM (CD44v6 and Tspan8).
Preparing a niche: TEX uptake remodels recipient non-tumor cells towards driving tumor growth. After the first description of a premetastatic niche[96], the engagement of TEX soon became obvious, which we were the first to describe for a rat PaCa-CD44v6kd line that had lost the capacity of the parental line to metastasize, but regained metastatic capacity, when rats were pretreated with TEX of the parental line[100]. Similarly, renal CSC expressing the SC marker CD105 release TEX that trigger angiogenesis and greatly enhanced lung metastases. The CD105+ TEX are characterized by sets of mRNAs and microRNAs supporting angiogenesis and tumor progression[95]. Also melanoma TEX home to sentinel lymph nodes imposing molecular signals that support melanoma cell recruitment, extracellular matrix deposition, and vascular proliferation, thereby facilitating lymphatic metastasis[485]. A proteome analysis of CoCa TEX uncovered enrichment particularly of metastasis-promoting factors (c-Met, S100A8, S100A9, tenascinC), of signal transduction molecules (ephrinB2, jagged1, src, TRAF2 and NCK interacting kinase <TNIK>), and lipid raft/lipid raft-associated components (caveolin, flotilin1 and 2, CD133) in TEX derived from a metastatic line. An additional key finding was the recovery of EpC-cld7 and TNIK-rap2A complexes in TEX[132] (Figure 6C). The mode of TEX-induced premetastatic niche formation was also elaborated using TEX from a metastatic and a non-metastatic melanoma line. TEX from highly metastatic melanoma line increased the metastatic behavior of primary tumors by affecting bone marrow progenitors through c-Met. Melanoma-TEX reprogrammed bone marrow progenitors towards a provasculogenic phenotype defined by c-Kit, Tie2 and c-Met expression. Reduced c-Met expression in TEX diminished the pro-metastatic behavior of bone marrow cells. c-Met+/c-Kit+/Tie2+ bone marrow progenitors were also recovered in patients with metastatic melanoma. Premetastatic niche promoting TEX were high in α4, HSP and c-Met. The authors conclude that metastasizing melanoma TEX “home” to the bone marrow, where they reprogram bone marrow cells to support tumor growth and metastasis[486]. The pathway of persisting reprogramming remains to be elaborated. However, it is conceivable that TEX contain transcription factors inducing a differentiation switch in this non-differentiated cells. In a mouse model of PaCa that metastasizes to the liver, TEX induce liver premetastatic niche formation and increase liver metastatic burden. TEX uptake by Kupffer cells promoted TGFβ and FN secretion. The fibrotic microenvironment enhanced recruitment of bone marrow-derived macrophages. The authors report on high macrophage migration inhibitory factor (MIF) expression in PaCa TEX, where a MIF blockade prevented liver pre-metastatic niche formation and metastasis. High MIF expression in TEX was also seen at an early stage of PaCa growth in patients that developed liver metastasis[101]. Evidence for the transfer of c-Met and for TEX stimulated c-Met-signaling in target cells fits to the CD44v6-c-Met complex recovery in Pa-CSC TEX[202,433]. Activation of src also may well proceed via CD44v6-c-Met as well as via integrin tetraspanin complexes[130,207]. The high recovery of inflammatory HSP in TEX could be due to the association with Tspan8 and could strengthen the efficacy of the frequently described upregulation of chemokines and mostly immunosuppressive cytokines as well as of inflammatory complement components and S100 in Pa-CSC TEX[487-490]. However, for the latter set of molecules a link to Pa-CSC markers remains to be defined (Figure 6C and D).
The miRNA content of TEX from CD44v6kd, Tspan8kd and cld7kd cells differ from that of wt cell-derived TEX. Exploring the impact of CD44v6-linked miRNA transferred into stroma cells revealed 18 mRNA downregulation. From the total TEX miRNA, 60% could potentially be engaged in targeting these 18 mRNA. We focused on abundant miR-494, potentially targeting MAL and cdh17, and miR-542-3p, targeting cdh17 and TNF receptor associated factor 4 (TRAF4). MAL can contribute to differentiation and apical sorting[491] and cdh17 to tumor growth/Wnt signaling[492]; TRAF4 exerts morphogenetic functions[493]. Lymph node stroma transfection with these miRNAs was accompanied by down-regulation of the predicted target(s). Significant up-regulation of mRNA in exosome-treated LnStr pointed toward mRNA up-regulation through miRNA silencing regulatory mRNA. Cdh17 represses MMP2 and MMP9 expression[494] and down-regulation of cdh17 in miR-494 and miR-542-3p transfected stroma cells was accompanied by MMP2, MMP3 and MMP14 up-regulation[202]. In another study with PaCa TEX, the authors found down-regulation of exosomal miR-155 and miR-196a and upregulation of miR-17-5p, upregulation correlating with metastasis and advanced tumor stages[33]. Further controlling for the impact of miR-155 in PaCa TEX revealed normal fibroblasts to become converted into CAF after uptake of miR-155 containing TEX. TP53INP1 is a target of miR-155 in fibroblasts and TP53INP1 protein downregulation can contribute to fibroblasts activation[495] (Figure 6E).
Without question TEX account for preparing a niche for migrating tumor cells. In PaCa TEX, there is strong evidence for a direct engagement of CD44v6, c-Met, integrins and Tspan8-associated integrins. An active contribution of cld7, the EpCAM-cld7 complex, CD133 and CXCR4 remains to be explored. According to the current state of knowledge, binding-induced as well as uptake-initiated signal transduction and the transfer of miRNA cooperate in target cell modulation.
CSC TEX also modulate other tumor cells via protein, mRNA and miRNA transfer[496,497].
One of the first and most impressive reports on TEX-uptake being critical in tumor growth stimulation describes the intercellular transfer of the oncogenic receptor EGFRvIII via TEX to glioma cells, lacking this receptor, which causes transformation of indolent glioma cells[133]. The oncogenes Ras, Myc, SV40T also induce signaling and gene expression[136,140,498]. Amphiregulin is an EGFR ligand. Compared to recombinant protein, TEX-associated amphiregulin increases tumor invasiveness 5-fold. The finding strongly suggests the transfer of additional messages via TEX[499]. In lung cancer TEX miR-21 and miR-29a act a TLR ligand and function as agonist. This leads to NFκB activation and IL6 and TNFα secretion promoting metastasis[500]. A set of miRNA, including miR-584, miR-517c, are not detected in the donor cell, but are highly enriched in hepatocellular carcinoma TEX. A potential target of these miRNA is TGFβ activated kinase 1, which activates JNK and MAPK pathways and NFκB. In cocultures, these TEX miRNA promote anchorage-independent growth and apoptosis resistance[501]. Apoptosis resistance can also rely on the transfer of multidrug resistance (MDR)1[502], which is enriched in TEX[503].
Furthermore, after oncogenic H-Ras-induced EMT, the TEX profile significantly changes, including TGFβ, TNFα, IL6, TSG101, Akt, ILK1, β-catenin, hepatoma-derived growth factor, casein kinase II, annexinA2, α3 integrin, caveolin and MMPs, the authors pointing out that the protein content of EMT TEX likely can induce EMT in recipient cells[473]. TEX also contain EBV-derived LMP1, which modulates together with HIF1α EMT marker expression in recipient cells[504]. TEX from human CSC-enriched CoCa lines can induce EMT in the CSC-depleted population. There is a strong induction of Notch, N-cadherin becomes upregulated and E-cadherin downregulated[273]. In a rat PaCa, CSC TEX promote Notch and Snail transcription depending on the presence of Tspan8[130] (Figure 6F). Still being at the descriptive level, it is obvious that CSC TEX can confer CSC features towards non-CSC including EMT, where TEX components work in concert.
Thus, Pa-CSC TEX markers are essential components for TEX targeting and account for selective responses, e.g., via src activation. For other responses, including the impact of miRNA, a contribution of Pa-CSC markers to the recruitment into TEX was repeatedly demonstrated. Though information on the contribution of exosomal Pa-CSC markers on target cell activation/reprogramming is still limited, available data convincingly demonstrate the engagement of Pa-CSC markers in TEX assembly, binding and message transfer.
CSC markers have long been considered as a tool for CSC enrichment and diagnosis. We here demonstrate for the Pa-CSC markers CD44v6, c-Met, Tspan8, α6β4, EpCAM, cld7, CXCR4 and CD133 that these markers contribute in maintaining CSC features essential for tumor persistence and progression. These Pa-CSC markers are required to (1) maintain the CSC status by their engagement in signal transduction, transcription including miRNA and repression of tumor suppressor genes; (2) establish a stem cell niche including a premetastatic niche by affecting via ligand binding target cell activation and message transfer; (3) support EMT by gene transcription and/or silencing; and (4) tumor cell migration and invasion via associated integrins and proteases.
The power of these markers relies on their residence in GEM, which allows for concerted activity and the engagement in TEX biogenesis and delivery. The CSC marker panel being maintained in TEX guarantees CSC to prepare the host for their maintenance at distant sites.
| 1. | Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9215] [Cited by in RCA: 9875] [Article Influence: 759.6] [Reference Citation Analysis (5)] |
| 2. | Wang Z, Lai ST, Xie L, Zhao JD, Ma NY, Zhu J, Ren ZG, Jiang GL. Metformin is associated with reduced risk of pancreatic cancer in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Res Clin Pract. 2014;106:19-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 130] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 3. | Wang XY, Yang F, Jin C, Fu DL. Utility of PET/CT in diagnosis, staging, assessment of resectability and metabolic response of pancreatic cancer. World J Gastroenterol. 2014;20:15580-15589. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 69] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (1)] |
| 4. | Urayama S. Pancreatic cancer early detection: expanding higher-risk group with clinical and metabolomics parameters. World J Gastroenterol. 2015;21:1707-1717. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 25] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Del Chiaro M, Segersvärd R, Lohr M, Verbeke C. Early detection and prevention of pancreatic cancer: is it really possible today? World J Gastroenterol. 2014;20:12118-12131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 95] [Cited by in RCA: 98] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 6. | Jenkinson C, Earl J, Ghaneh P, Halloran C, Carrato A, Greenhalf W, Neoptolemos J, Costello E. Biomarkers for early diagnosis of pancreatic cancer. Expert Rev Gastroenterol Hepatol. 2015;9:305-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Ansari D, Gustafsson A, Andersson R. Update on the management of pancreatic cancer: surgery is not enough. World J Gastroenterol. 2015;21:3157-3165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 138] [Cited by in RCA: 134] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 8. | Okano K, Suzuki Y. Strategies for early detection of resectable pancreatic cancer. World J Gastroenterol. 2014;20:11230-11240. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 32] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | He XY, Yuan YZ. Advances in pancreatic cancer research: moving towards early detection. World J Gastroenterol. 2014;20:11241-11248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 52] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 10. | Goonetilleke KS, Siriwardena AK. Systematic review of carbohydrate antigen (CA 19-9) as a biochemical marker in the diagnosis of pancreatic cancer. Eur J Surg Oncol. 2007;33:266-270. [PubMed] |
| 11. | Bussom S, Saif MW. Methods and rationale for the early detection of pancreatic cancer. Highlights from the “2010 ASCO Gastrointestinal Cancers Symposium”. Orlando, FL, USA. January 22-24, 2010. JOP. 2010;11:128-130. [PubMed] |
| 12. | Gold DV, Modrak DE, Ying Z, Cardillo TM, Sharkey RM, Goldenberg DM. New MUC1 serum immunoassay differentiates pancreatic cancer from pancreatitis. J Clin Oncol. 2006;24:252-258. [PubMed] |
| 13. | Canto MI, Goggins M, Yeo CJ, Griffin C, Axilbund JE, Brune K, Ali SZ, Jagannath S, Petersen GM, Fishman EK. Screening for pancreatic neoplasia in high-risk individuals: an EUS-based approach. Clin Gastroenterol Hepatol. 2004;2:606-621. [PubMed] |
| 14. | Chen Y, Kang M, Lu W, Guo Q, Zhang B, Xie Q, Wu Y. DJ-1, a novel biomarker and a selected target gene for overcoming chemoresistance in pancreatic cancer. J Cancer Res Clin Oncol. 2012;138:1463-1474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 15. | Makawita S, Dimitromanolakis A, Soosaipillai A, Soleas I, Chan A, Gallinger S, Haun RS, Blasutig IM, Diamandis EP. Validation of four candidate pancreatic cancer serological biomarkers that improve the performance of CA19.9. BMC Cancer. 2013;13:404. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 16. | Wingren C, Sandström A, Segersvärd R, Carlsson A, Andersson R, Löhr M, Borrebaeck CA. Identification of serum biomarker signatures associated with pancreatic cancer. Cancer Res. 2012;72:2481-2490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 84] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 17. | Ansari D, Andersson R, Bauden MP, Andersson B, Connolly JB, Welinder C, Sasor A, Marko-Varga G. Protein deep sequencing applied to biobank samples from patients with pancreatic cancer. J Cancer Res Clin Oncol. 2015;141:369-380. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 18. | Chen R, Yi EC, Donohoe S, Pan S, Eng J, Cooke K, Crispin DA, Lane Z, Goodlett DR, Bronner MP. Pancreatic cancer proteome: the proteins that underlie invasion, metastasis, and immunologic escape. Gastroenterology. 2005;129:1187-1197. [PubMed] |
| 19. | Lu Z, Hu L, Evers S, Chen J, Shen Y. Differential expression profiling of human pancreatic adenocarcinoma and healthy pancreatic tissue. Proteomics. 2004;4:3975-3988. [PubMed] |
| 20. | Shen J, Person MD, Zhu J, Abbruzzese JL, Li D. Protein expression profiles in pancreatic adenocarcinoma compared with normal pancreatic tissue and tissue affected by pancreatitis as detected by two-dimensional gel electrophoresis and mass spectrometry. Cancer Res. 2004;64:9018-9026. [PubMed] |
| 21. | Fukushige S, Horii A. Road to early detection of pancreatic cancer: Attempts to utilize epigenetic biomarkers. Cancer Lett. 2014;342:231-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 22. | Rachagani S, Macha MA, Heimann N, Seshacharyulu P, Haridas D, Chugh S, Batra SK. Clinical implications of miRNAs in the pathogenesis, diagnosis and therapy of pancreatic cancer. Adv Drug Deliv Rev. 2015;81:16-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 86] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 23. | Zöller M. Pancreatic cancer diagnosis by free and exosomal miRNA. World J Gastrointest Pathophysiol. 2013;4:74-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 59] [Cited by in RCA: 65] [Article Influence: 5.0] [Reference Citation Analysis (2)] |
| 24. | Yi JM, Guzzetta AA, Bailey VJ, Downing SR, Van Neste L, Chiappinelli KB, Keeley BP, Stark A, Herrera A, Wolfgang C. Novel methylation biomarker panel for the early detection of pancreatic cancer. Clin Cancer Res. 2013;19:6544-6555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 125] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 25. | Nagpal G, Sharma M, Kumar S, Chaudhary K, Gupta S, Gautam A, Raghava GP. PCMdb: pancreatic cancer methylation database. Sci Rep. 2014;4:4197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Jin K, Luo G, Xiao Z, Liu Z, Liu C, Ji S, Xu J, Liu L, Long J, Ni Q. Noncoding RNAs as potential biomarkers to predict the outcome in pancreatic cancer. Drug Des Devel Ther. 2015;9:1247-1255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 27. | Wang J, Chen J, Chang P, LeBlanc A, Li D, Abbruzzesse JL, Frazier ML, Killary AM, Sen S. MicroRNAs in plasma of pancreatic ductal adenocarcinoma patients as novel blood-based biomarkers of disease. Cancer Prev Res (Phila). 2009;2:807-813. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 434] [Cited by in RCA: 449] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 28. | Liu J, Gao J, Du Y, Li Z, Ren Y, Gu J, Wang X, Gong Y, Wang W, Kong X. Combination of plasma microRNAs with serum CA19-9 for early detection of pancreatic cancer. Int J Cancer. 2012;131:683-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 240] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 29. | Liu R, Chen X, Du Y, Yao W, Shen L, Wang C, Hu Z, Zhuang R, Ning G, Zhang C. Serum microRNA expression profile as a biomarker in the diagnosis and prognosis of pancreatic cancer. Clin Chem. 2012;58:610-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 318] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 30. | Schultz NA, Dehlendorff C, Jensen BV, Bjerregaard JK, Nielsen KR, Bojesen SE, Calatayud D, Nielsen SE, Yilmaz M, Holländer NH. MicroRNA biomarkers in whole blood for detection of pancreatic cancer. JAMA. 2014;311:392-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 348] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 31. | Wan C, Shen Y, Yang T, Wang T, Chen L, Wen F. Diagnostic value of microRNA for pancreatic cancer: a meta-analysis. Arch Med Sci. 2012;8:749-755. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 32. | Kahlert C, Melo SA, Protopopov A, Tang J, Seth S, Koch M, Zhang J, Weitz J, Chin L, Futreal A. Identification of double-stranded genomic DNA spanning all chromosomes with mutated KRAS and p53 DNA in the serum exosomes of patients with pancreatic cancer. J Biol Chem. 2014;289:3869-3875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 646] [Cited by in RCA: 801] [Article Influence: 66.8] [Reference Citation Analysis (0)] |
| 33. | Que R, Ding G, Chen J, Cao L. Analysis of serum exosomal microRNAs and clinicopathologic features of patients with pancreatic adenocarcinoma. World J Surg Oncol. 2013;11:219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 200] [Cited by in RCA: 224] [Article Influence: 17.2] [Reference Citation Analysis (1)] |
| 34. | Melo SA, Luecke LB, Kahlert C, Fernandez AF, Gammon ST, Kaye J, LeBleu VS, Mittendorf EA, Weitz J, Rahbari N. Glypican-1 identifies cancer exosomes and detects early pancreatic cancer. Nature. 2015;523:177-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2108] [Cited by in RCA: 2275] [Article Influence: 206.8] [Reference Citation Analysis (0)] |
| 35. | Madhavan B, Yue S, Galli U, Rana S, Gross W, Müller M, Giese NA, Kalthoff H, Becker T, Büchler MW. Combined evaluation of a panel of protein and miRNA serum-exosome biomarkers for pancreatic cancer diagnosis increases sensitivity and specificity. Int J Cancer. 2015;136:2616-2627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 396] [Article Influence: 33.0] [Reference Citation Analysis (0)] |
| 36. | Sohal DP, Walsh RM, Ramanathan RK, Khorana AA. Pancreatic adenocarcinoma: treating a systemic disease with systemic therapy. J Natl Cancer Inst. 2014;106:dju011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 134] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 37. | Greenow K, Clarke AR. Controlling the stem cell compartment and regeneration in vivo: the role of pluripotency pathways. Physiol Rev. 2012;92:75-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 38. | Sales KM, Winslet MC, Seifalian AM. Stem cells and cancer: an overview. Stem Cell Rev. 2007;3:249-255. [PubMed] |
| 39. | Tam WL, Weinberg RA. The epigenetics of epithelial-mesenchymal plasticity in cancer. Nat Med. 2013;19:1438-1449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 831] [Cited by in RCA: 949] [Article Influence: 73.0] [Reference Citation Analysis (0)] |
| 40. | Cerdan C, Bhatia M. Novel roles for Notch, Wnt and Hedgehog in hematopoesis derived from human pluripotent stem cells. Int J Dev Biol. 2010;54:955-963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 41. | Fossett N. Signal transduction pathways, intrinsic regulators, and the control of cell fate choice. Biochim Biophys Acta. 2013;1830:2375-2384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 42. | Brabletz T, Jung A, Spaderna S, Hlubek F, Kirchner T. Opinion: migrating cancer stem cells - an integrated concept of malignant tumour progression. Nat Rev Cancer. 2005;5:744-749. [PubMed] |
| 43. | Thiery JP, Acloque H, Huang RY, Nieto MA. Epithelial-mesenchymal transitions in development and disease. Cell. 2009;139:871-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6805] [Cited by in RCA: 7899] [Article Influence: 464.6] [Reference Citation Analysis (1)] |
| 44. | Mani SA, Guo W, Liao MJ, Eaton EN, Ayyanan A, Zhou AY, Brooks M, Reinhard F, Zhang CC, Shipitsin M. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell. 2008;133:704-715. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6972] [Cited by in RCA: 6910] [Article Influence: 383.9] [Reference Citation Analysis (0)] |
| 45. | Wang Z, Ali S, Banerjee S, Bao B, Li Y, Azmi AS, Korc M, Sarkar FH. Activated K-Ras and INK4a/Arf deficiency promote aggressiveness of pancreatic cancer by induction of EMT consistent with cancer stem cell phenotype. J Cell Physiol. 2013;228:556-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 46. | Biddle A, Mackenzie IC. Cancer stem cells and EMT in carcinoma. Cancer Metastasis Rev. 2012; Epub ahead of print. [PubMed] |
| 47. | Scheel C, Eaton EN, Li SH, Chaffer CL, Reinhardt F, Kah KJ, Bell G, Guo W, Rubin J, Richardson AL. Paracrine and autocrine signals induce and maintain mesenchymal and stem cell states in the breast. Cell. 2011;145:926-940. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 739] [Cited by in RCA: 723] [Article Influence: 48.2] [Reference Citation Analysis (0)] |
| 48. | Lamouille S, Xu J, Derynck R. Molecular mechanisms of epithelial-mesenchymal transition. Nat Rev Mol Cell Biol. 2014;15:178-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4715] [Cited by in RCA: 6470] [Article Influence: 539.2] [Reference Citation Analysis (0)] |
| 49. | Tania M, Khan MA, Fu J. Epithelial to mesenchymal transition inducing transcription factors and metastatic cancer. Tumour Biol. 2014;35:7335-7342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 213] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 50. | Moustakas A, Heldin P. TGFβ and matrix-regulated epithelial to mesenchymal transition. Biochim Biophys Acta. 2014;1840:2621-2634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 108] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 51. | Taylor MA, Parvani JG, Schiemann WP. The pathophysiology of epithelial-mesenchymal transition induced by transforming growth factor-beta in normal and malignant mammary epithelial cells. J Mammary Gland Biol Neoplasia. 2010;15:169-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 190] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 53. | Vermeulen L, De Sousa E Melo F, van der Heijden M, Cameron K, de Jong JH, Borovski T, Tuynman JB, Todaro M, Merz C, Rodermond H. Wnt activity defines colon cancer stem cells and is regulated by the microenvironment. Nat Cell Biol. 2010;12:468-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1301] [Cited by in RCA: 1468] [Article Influence: 91.8] [Reference Citation Analysis (1)] |
| 54. | Yook JI, Li XY, Ota I, Hu C, Kim HS, Kim NH, Cha SY, Ryu JK, Choi YJ, Kim J. A Wnt-Axin2-GSK3beta cascade regulates Snail1 activity in breast cancer cells. Nat Cell Biol. 2006;8:1398-1406. [PubMed] |
| 55. | Brabletz S, Bajdak K, Meidhof S, Burk U, Niedermann G, Firat E, Wellner U, Dimmler A, Faller G, Schubert J. The ZEB1/miR-200 feedback loop controls Notch signalling in cancer cells. EMBO J. 2011;30:770-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 304] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 56. | Thomson S, Petti F, Sujka-Kwok I, Mercado P, Bean J, Monaghan M, Seymour SL, Argast GM, Epstein DM, Haley JD. A systems view of epithelial-mesenchymal transition signaling states. Clin Exp Metastasis. 2011;28:137-155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 166] [Cited by in RCA: 178] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 57. | Hardy KM, Booth BW, Hendrix MJ, Salomon DS, Strizzi L. ErbB/EGF signaling and EMT in mammary development and breast cancer. J Mammary Gland Biol Neoplasia. 2010;15:191-199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 136] [Cited by in RCA: 136] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 58. | Peinado H, Olmeda D, Cano A. Snail, Zeb and bHLH factors in tumour progression: an alliance against the epithelial phenotype? Nat Rev Cancer. 2007;7:415-428. [PubMed] |
| 59. | Cedar H, Bergman Y. Linking DNA methylation and histone modification: patterns and paradigms. Nat Rev Genet. 2009;10:295-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1601] [Cited by in RCA: 1665] [Article Influence: 97.9] [Reference Citation Analysis (0)] |
| 60. | Song LB, Li J, Liao WT, Feng Y, Yu CP, Hu LJ, Kong QL, Xu LH, Zhang X, Liu WL. The polycomb group protein Bmi-1 represses the tumor suppressor PTEN and induces epithelial-mesenchymal transition in human nasopharyngeal epithelial cells. J Clin Invest. 2009;119:3626-3636. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 334] [Cited by in RCA: 349] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 61. | Martin A, Cano A. Tumorigenesis: Twist1 links EMT to self-renewal. Nat Cell Biol. 2010;12:924-925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 82] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 62. | von Burstin J, Eser S, Paul MC, Seidler B, Brandl M, Messer M, von Werder A, Schmidt A, Mages J, Pagel P. E-cadherin regulates metastasis of pancreatic cancer in vivo and is suppressed by a SNAIL/HDAC1/HDAC2 repressor complex. Gastroenterology. 2009;137:361-71, 371.e1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 289] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 63. | Fu J, Qin L, He T, Qin J, Hong J, Wong J, Liao L, Xu J. The TWIST/Mi2/NuRD protein complex and its essential role in cancer metastasis. Cell Res. 2011;21:275-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 226] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 64. | Scherr M, Eder M. Gene silencing by small regulatory RNAs in mammalian cells. Cell Cycle. 2007;6:444-449. [PubMed] |
| 65. | Gregory PA, Bert AG, Paterson EL, Barry SC, Tsykin A, Farshid G, Vadas MA, Khew-Goodall Y, Goodall GJ. The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat Cell Biol. 2008;10:593-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2843] [Cited by in RCA: 3115] [Article Influence: 173.1] [Reference Citation Analysis (0)] |
| 66. | Ru P, Steele R, Newhall P, Phillips NJ, Toth K, Ray RB. miRNA-29b suppresses prostate cancer metastasis by regulating epithelial-mesenchymal transition signaling. Mol Cancer Ther. 2012;11:1166-1173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 157] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 67. | Zhang J, Zhang H, Liu J, Tu X, Zang Y, Zhu J, Chen J, Dong L, Zhang J. miR-30 inhibits TGF-β1-induced epithelial-to-mesenchymal transition in hepatocyte by targeting Snail1. Biochem Biophys Res Commun. 2012;417:1100-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 128] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 68. | Gandellini P, Giannoni E, Casamichele A, Taddei ML, Callari M, Piovan C, Valdagni R, Pierotti MA, Zaffaroni N, Chiarugi P. miR-205 hinders the malignant interplay between prostate cancer cells and associated fibroblasts. Antioxid Redox Signal. 2014;20:1045-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 67] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 69. | Ma L, Young J, Prabhala H, Pan E, Mestdagh P, Muth D, Teruya-Feldstein J, Reinhardt F, Onder TT, Valastyan S. miR-9, a MYC/MYCN-activated microRNA, regulates E-cadherin and cancer metastasis. Nat Cell Biol. 2010;12:247-256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1073] [Cited by in RCA: 1086] [Article Influence: 67.9] [Reference Citation Analysis (15)] |
| 70. | Meng Z, Fu X, Chen X, Zeng S, Tian Y, Jove R, Xu R, Huang W. miR-194 is a marker of hepatic epithelial cells and suppresses metastasis of liver cancer cells in mice. Hepatology. 2010;52:2148-2157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 164] [Cited by in RCA: 178] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 71. | Vetter G, Saumet A, Moes M, Vallar L, Le Béchec A, Laurini C, Sabbah M, Arar K, Theillet C, Lecellier CH. miR-661 expression in SNAI1-induced epithelial to mesenchymal transition contributes to breast cancer cell invasion by targeting Nectin-1 and StarD10 messengers. Oncogene. 2010;29:4436-4448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 102] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 72. | Zhou Q, Fan J, Ding X, Peng W, Yu X, Chen Y, Nie J. TGF-{beta}-induced MiR-491-5p expression promotes Par-3 degradation in rat proximal tubular epithelial cells. J Biol Chem. 2010;285:40019-40027. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 73. | Hamada S, Satoh K, Miura S, Hirota M, Kanno A, Masamune A, Kikuta K, Kume K, Unno J, Egawa S. miR-197 induces epithelial-mesenchymal transition in pancreatic cancer cells by targeting p120 catenin. J Cell Physiol. 2013;228:1255-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 88] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 74. | Chang CJ, Chao CH, Xia W, Yang JY, Xiong Y, Li CW, Yu WH, Rehman SK, Hsu JL, Lee HH. p53 regulates epithelial-mesenchymal transition and stem cell properties through modulating miRNAs. Nat Cell Biol. 2011;13:317-323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 611] [Cited by in RCA: 618] [Article Influence: 41.2] [Reference Citation Analysis (0)] |
| 75. | Chen D, Zhang Y, Wang J, Chen J, Yang C, Cai K, Wang X, Shi F, Dou J. MicroRNA-200c overexpression inhibits tumorigenicity and metastasis of CD117+CD44+ ovarian cancer stem cells by regulating epithelial-mesenchymal transition. J Ovarian Res. 2013;6:50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 81] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 76. | Han M, Liu M, Wang Y, Chen X, Xu J, Sun Y, Zhao L, Qu H, Fan Y, Wu C. Antagonism of miR-21 reverses epithelial-mesenchymal transition and cancer stem cell phenotype through AKT/ERK1/2 inactivation by targeting PTEN. PLoS One. 2012;7:e39520. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 165] [Cited by in RCA: 198] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 77. | Tsai JH, Donaher JL, Murphy DA, Chau S, Yang J. Spatiotemporal regulation of epithelial-mesenchymal transition is essential for squamous cell carcinoma metastasis. Cancer Cell. 2012;22:725-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 784] [Cited by in RCA: 880] [Article Influence: 62.9] [Reference Citation Analysis (0)] |
| 78. | Siemens H, Jackstadt R, Hünten S, Kaller M, Menssen A, Götz U, Hermeking H. miR-34 and SNAIL form a double-negative feedback loop to regulate epithelial-mesenchymal transitions. Cell Cycle. 2011;10:4256-4271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 432] [Cited by in RCA: 486] [Article Influence: 32.4] [Reference Citation Analysis (0)] |
| 79. | Brabletz S, Brabletz T. The ZEB/miR-200 feedback loop--a motor of cellular plasticity in development and cancer? EMBO Rep. 2010;11:670-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 599] [Cited by in RCA: 670] [Article Influence: 41.9] [Reference Citation Analysis (0)] |
| 80. | Moes M, Le Béchec A, Crespo I, Laurini C, Halavatyi A, Vetter G, Del Sol A, Friederich E. A novel network integrating a miRNA-203/SNAI1 feedback loop which regulates epithelial to mesenchymal transition. PLoS One. 2012;7:e35440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 128] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 81. | Fuchs E, Tumbar T, Guasch G. Socializing with the neighbors: stem cells and their niche. Cell. 2004;116:769-778. [PubMed] |
| 82. | Li L, Neaves WB. Normal stem cells and cancer stem cells: the niche matters. Cancer Res. 2006;66:4553-4557. [PubMed] |
| 83. | Kuhn NZ, Tuan RS. Regulation of stemness and stem cell niche of mesenchymal stem cells: implications in tumorigenesis and metastasis. J Cell Physiol. 2010;222:268-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 187] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 84. | Borovski T, De Sousa E Melo F, Vermeulen L, Medema JP. Cancer stem cell niche: the place to be. Cancer Res. 2011;71:634-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 378] [Cited by in RCA: 396] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 85. | Cabarcas SM, Mathews LA, Farrar WL. The cancer stem cell niche--there goes the neighborhood? Int J Cancer. 2011;129:2315-2327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 197] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 86. | Méndez-Ferrer S, Michurina TV, Ferraro F, Mazloom AR, Macarthur BD, Lira SA, Scadden DT, Ma’ayan A, Enikolopov GN, Frenette PS. Mesenchymal and haematopoietic stem cells form a unique bone marrow niche. Nature. 2010;466:829-834. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2810] [Cited by in RCA: 2622] [Article Influence: 163.9] [Reference Citation Analysis (1)] |
| 87. | Winkler IG, Sims NA, Pettit AR, Barbier V, Nowlan B, Helwani F, Poulton IJ, van Rooijen N, Alexander KA, Raggatt LJ. Bone marrow macrophages maintain hematopoietic stem cell (HSC) niches and their depletion mobilizes HSCs. Blood. 2010;116:4815-4828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 584] [Cited by in RCA: 630] [Article Influence: 39.4] [Reference Citation Analysis (0)] |
| 88. | Li HJ, Reinhardt F, Herschman HR, Weinberg RA. Cancer-stimulated mesenchymal stem cells create a carcinoma stem cell niche via prostaglandin E2 signaling. Cancer Discov. 2012;2:840-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 298] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 89. | Wang R, Chadalavada K, Wilshire J, Kowalik U, Hovinga KE, Geber A, Fligelman B, Leversha M, Brennan C, Tabar V. Glioblastoma stem-like cells give rise to tumour endothelium. Nature. 2010;468:829-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 882] [Cited by in RCA: 919] [Article Influence: 57.4] [Reference Citation Analysis (0)] |
| 90. | Domanska UM, Kruizinga RC, Nagengast WB, Timmer-Bosscha H, Huls G, de Vries EG, Walenkamp AM. A review on CXCR4/CXCL12 axis in oncology: no place to hide. Eur J Cancer. 2013;49:219-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 410] [Cited by in RCA: 511] [Article Influence: 39.3] [Reference Citation Analysis (0)] |
| 91. | Gherardi E, Birchmeier W, Birchmeier C, Vande Woude G. Targeting MET in cancer: rationale and progress. Nat Rev Cancer. 2012;12:89-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1057] [Cited by in RCA: 1180] [Article Influence: 84.3] [Reference Citation Analysis (0)] |
| 92. | Jamieson C, Sharma M, Henderson BR. Wnt signaling from membrane to nucleus: β-catenin caught in a loop. Int J Biochem Cell Biol. 2012;44:847-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 77] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 93. | Ono M, Kosaka N, Tominaga N, Yoshioka Y, Takeshita F, Takahashi RU, Yoshida M, Tsuda H, Tamura K, Ochiya T. Exosomes from bone marrow mesenchymal stem cells contain a microRNA that promotes dormancy in metastatic breast cancer cells. Sci Signal. 2014;7:ra63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 441] [Cited by in RCA: 547] [Article Influence: 45.6] [Reference Citation Analysis (0)] |
| 94. | Nakano I, Garnier D, Minata M, Rak J. Extracellular vesicles in the biology of brain tumour stem cells--Implications for inter-cellular communication, therapy and biomarker development. Semin Cell Dev Biol. 2015;40:17-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 86] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 95. | Grange C, Tapparo M, Collino F, Vitillo L, Damasco C, Deregibus MC, Tetta C, Bussolati B, Camussi G. Microvesicles released from human renal cancer stem cells stimulate angiogenesis and formation of lung premetastatic niche. Cancer Res. 2011;71:5346-5356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 630] [Cited by in RCA: 709] [Article Influence: 47.3] [Reference Citation Analysis (0)] |
| 96. | Kaplan RN, Riba RD, Zacharoulis S, Bramley AH, Vincent L, Costa C, MacDonald DD, Jin DK, Shido K, Kerns SA. VEGFR1-positive haematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature. 2005;438:820-827. [PubMed] |
| 97. | Alderton GK. Metastasis. Exosomes drive premetastatic niche formation. Nat Rev Cancer. 2012;12:447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 75] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 98. | Thuma F, Zöller M. Outsmart tumor exosomes to steal the cancer initiating cell its niche. Semin Cancer Biol. 2014;28:39-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 99. | Suchorska WM, Lach MS. The role of exosomes in tumor progression and metastasis (Review). Oncol Rep. 2016;35:1237-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 102] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 100. | Jung T, Castellana D, Klingbeil P, Cuesta Hernández I, Vitacolonna M, Orlicky DJ, Roffler SR, Brodt P, Zöller M. CD44v6 dependence of premetastatic niche preparation by exosomes. Neoplasia. 2009;11:1093-1105. [PubMed] |
| 101. | Costa-Silva B, Aiello NM, Ocean AJ, Singh S, Zhang H, Thakur BK, Becker A, Hoshino A, Mark MT, Molina H. Pancreatic cancer exosomes initiate pre-metastatic niche formation in the liver. Nat Cell Biol. 2015;17:816-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1554] [Cited by in RCA: 2156] [Article Influence: 196.0] [Reference Citation Analysis (0)] |
| 102. | Vlassov AV, Magdaleno S, Setterquist R, Conrad R. Exosomes: current knowledge of their composition, biological functions, and diagnostic and therapeutic potentials. Biochim Biophys Acta. 2012;1820:940-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1267] [Cited by in RCA: 1511] [Article Influence: 107.9] [Reference Citation Analysis (0)] |
| 103. | Lo Cicero A, Stahl PD, Raposo G. Extracellular vesicles shuffling intercellular messages: for good or for bad. Curr Opin Cell Biol. 2015;35:69-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 394] [Article Influence: 35.8] [Reference Citation Analysis (0)] |
| 104. | Henne WM, Buchkovich NJ, Emr SD. The ESCRT pathway. Dev Cell. 2011;21:77-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 956] [Cited by in RCA: 1211] [Article Influence: 80.7] [Reference Citation Analysis (0)] |
| 105. | Colombo M, Moita C, van Niel G, Kowal J, Vigneron J, Benaroch P, Manel N, Moita LF, Théry C, Raposo G. Analysis of ESCRT functions in exosome biogenesis, composition and secretion highlights the heterogeneity of extracellular vesicles. J Cell Sci. 2013;126:5553-5565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 728] [Cited by in RCA: 906] [Article Influence: 69.7] [Reference Citation Analysis (0)] |
| 106. | Baietti MF, Zhang Z, Mortier E, Melchior A, Degeest G, Geeraerts A, Ivarsson Y, Depoortere F, Coomans C, Vermeiren E. Syndecan-syntenin-ALIX regulates the biogenesis of exosomes. Nat Cell Biol. 2012;14:677-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1084] [Cited by in RCA: 1444] [Article Influence: 103.1] [Reference Citation Analysis (0)] |
| 107. | Zöller M. Tetraspanins: push and pull in suppressing and promoting metastasis. Nat Rev Cancer. 2009;9:40-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 495] [Cited by in RCA: 536] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 108. | van Niel G, Charrin S, Simoes S, Romao M, Rochin L, Saftig P, Marks MS, Rubinstein E, Raposo G. The tetraspanin CD63 regulates ESCRT-independent and -dependent endosomal sorting during melanogenesis. Dev Cell. 2011;21:708-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 516] [Cited by in RCA: 750] [Article Influence: 50.0] [Reference Citation Analysis (0)] |
| 109. | Chairoungdua A, Smith DL, Pochard P, Hull M, Caplan MJ. Exosome release of β-catenin: a novel mechanism that antagonizes Wnt signaling. J Cell Biol. 2010;190:1079-1091. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 371] [Cited by in RCA: 463] [Article Influence: 28.9] [Reference Citation Analysis (0)] |
| 110. | Kajimoto T, Okada T, Miya S, Zhang L, Nakamura S. Ongoing activation of sphingosine 1-phosphate receptors mediates maturation of exosomal multivesicular endosomes. Nat Commun. 2013;4:2712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 256] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 111. | Kelly EE, Horgan CP, Goud B, McCaffrey MW. The Rab family of proteins: 25 years on. Biochem Soc Trans. 2012;40:1337-1347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 112. | Record M, Carayon K, Poirot M, Silvente-Poirot S. Exosomes as new vesicular lipid transporters involved in cell-cell communication and various pathophysiologies. Biochim Biophys Acta. 2014;1841:108-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 502] [Cited by in RCA: 635] [Article Influence: 48.8] [Reference Citation Analysis (0)] |
| 113. | Subra C, Grand D, Laulagnier K, Stella A, Lambeau G, Paillasse M, De Medina P, Monsarrat B, Perret B, Silvente-Poirot S. Exosomes account for vesicle-mediated transcellular transport of activatable phospholipases and prostaglandins. J Lipid Res. 2010;51:2105-2120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 425] [Cited by in RCA: 517] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 114. | Katzmann DJ, Odorizzi G, Emr SD. Receptor downregulation and multivesicular-body sorting. Nat Rev Mol Cell Biol. 2002;3:893-905. [PubMed] |
| 115. | Costanzo M, Baryshnikova A, Bellay J, Kim Y, Spear ED, Sevier CS, Ding H, Koh JL, Toufighi K, Mostafavi S. The genetic landscape of a cell. Science. 2010;327:425-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1783] [Cited by in RCA: 1644] [Article Influence: 102.8] [Reference Citation Analysis (0)] |
| 116. | Ramstedt B, Slotte JP. Membrane properties of sphingomyelins. FEBS Lett. 2002;531:33-37. [PubMed] |
| 117. | Allen TM, Austin GA, Chonn A, Lin L, Lee KC. Uptake of liposomes by cultured mouse bone marrow macrophages: influence of liposome composition and size. Biochim Biophys Acta. 1991;1061:56-64. [PubMed] |
| 118. | Chernomordik LV, Kozlov MM. Protein-lipid interplay in fusion and fission of biological membranes. Annu Rev Biochem. 2003;72:175-207. [PubMed] |
| 119. | Subra C, Laulagnier K, Perret B, Record M. Exosome lipidomics unravels lipid sorting at the level of multivesicular bodies. Biochimie. 2007;89:205-212. [PubMed] |
| 120. | Trajkovic K, Hsu C, Chiantia S, Rajendran L, Wenzel D, Wieland F, Schwille P, Brügger B, Simons M. Ceramide triggers budding of exosome vesicles into multivesicular endosomes. Science. 2008;319:1244-1247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2186] [Cited by in RCA: 2798] [Article Influence: 155.4] [Reference Citation Analysis (0)] |
| 121. | Schey KL, Luther JM, Rose KL. Proteomics characterization of exosome cargo. Methods. 2015;87:75-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 161] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 122. | Mathivanan S, Ji H, Simpson RJ. Exosomes: extracellular organelles important in intercellular communication. J Proteomics. 2010;73:1907-1920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1718] [Cited by in RCA: 1984] [Article Influence: 124.0] [Reference Citation Analysis (0)] |
| 123. | Shen B, Fang Y, Wu N, Gould SJ. Biogenesis of the posterior pole is mediated by the exosome/microvesicle protein-sorting pathway. J Biol Chem. 2011;286:44162-44176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 79] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 124. | Rana S, Claas C, Kretz CC, Nazarenko I, Zoeller M. Activation-induced internalization differs for the tetraspanins CD9 and Tspan8: Impact on tumor cell motility. Int J Biochem Cell Biol. 2011;43:106-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 125. | Guo BB, Bellingham SA, Hill AF. The neutral sphingomyelinase pathway regulates packaging of the prion protein into exosomes. J Biol Chem. 2015;290:3455-3467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 196] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 126. | Nabhan JF, Hu R, Oh RS, Cohen SN, Lu Q. Formation and release of arrestin domain-containing protein 1-mediated microvesicles (ARMMs) at plasma membrane by recruitment of TSG101 protein. Proc Natl Acad Sci USA. 2012;109:4146-4151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 416] [Cited by in RCA: 563] [Article Influence: 40.2] [Reference Citation Analysis (0)] |
| 127. | Shen B, Wu N, Yang JM, Gould SJ. Protein targeting to exosomes/microvesicles by plasma membrane anchors. J Biol Chem. 2011;286:14383-14395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 221] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 128. | Hoshino D, Kirkbride KC, Costello K, Clark ES, Sinha S, Grega-Larson N, Tyska MJ, Weaver AM. Exosome secretion is enhanced by invadopodia and drives invasive behavior. Cell Rep. 2013;5:1159-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 356] [Cited by in RCA: 442] [Article Influence: 34.0] [Reference Citation Analysis (0)] |
| 129. | Rana S, Yue S, Stadel D, Zöller M. Toward tailored exosomes: the exosomal tetraspanin web contributes to target cell selection. Int J Biochem Cell Biol. 2012;44:1574-1584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 555] [Cited by in RCA: 530] [Article Influence: 37.9] [Reference Citation Analysis (0)] |
| 130. | Yue S, Mu W, Erb U, Zöller M. The tetraspanins CD151 and Tspan8 are essential exosome components for the crosstalk between cancer initiating cells and their surrounding. Oncotarget. 2015;6:2366-2384. [PubMed] |
| 131. | Choi DS, Yang JS, Choi EJ, Jang SC, Park S, Kim OY, Hwang D, Kim KP, Kim YK, Kim S. The protein interaction network of extracellular vesicles derived from human colorectal cancer cells. J Proteome Res. 2012;11:1144-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 132. | Ji H, Greening DW, Barnes TW, Lim JW, Tauro BJ, Rai A, Xu R, Adda C, Mathivanan S, Zhao W. Proteome profiling of exosomes derived from human primary and metastatic colorectal cancer cells reveal differential expression of key metastatic factors and signal transduction components. Proteomics. 2013;13:1672-1686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 283] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 133. | Al-Nedawi K, Meehan B, Micallef J, Lhotak V, May L, Guha A, Rak J. Intercellular transfer of the oncogenic receptor EGFRvIII by microvesicles derived from tumour cells. Nat Cell Biol. 2008;10:619-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1347] [Cited by in RCA: 1578] [Article Influence: 87.7] [Reference Citation Analysis (0)] |
| 134. | Corcoran C, Rani S, O’Brien K, O’Neill A, Prencipe M, Sheikh R, Webb G, McDermott R, Watson W, Crown J. Docetaxel-resistance in prostate cancer: evaluating associated phenotypic changes and potential for resistance transfer via exosomes. PLoS One. 2012;7:e50999. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 300] [Cited by in RCA: 369] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 135. | Park JA, Sharif AS, Tschumperlin DJ, Lau L, Limbrey R, Howarth P, Drazen JM. Tissue factor-bearing exosome secretion from human mechanically stimulated bronchial epithelial cells in vitro and in vivo. J Allergy Clin Immunol. 2012;130:1375-1383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 92] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 136. | Demory Beckler M, Higginbotham JN, Franklin JL, Ham AJ, Halvey PJ, Imasuen IE, Whitwell C, Li M, Liebler DC, Coffey RJ. Proteomic analysis of exosomes from mutant KRAS colon cancer cells identifies intercellular transfer of mutant KRAS. Mol Cell Proteomics. 2013;12:343-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 356] [Cited by in RCA: 425] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
| 137. | Kumar D, Gupta D, Shankar S, Srivastava RK. Biomolecular characterization of exosomes released from cancer stem cells: Possible implications for biomarker and treatment of cancer. Oncotarget. 2015;6:3280-3291. [PubMed] |
| 138. | Zöller M. Exosomes in Cancer Disease. Methods Mol Biol. 2016;1381:111-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 139. | Gibbings DJ, Ciaudo C, Erhardt M, Voinnet O. Multivesicular bodies associate with components of miRNA effector complexes and modulate miRNA activity. Nat Cell Biol. 2009;11:1143-1149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 741] [Cited by in RCA: 798] [Article Influence: 46.9] [Reference Citation Analysis (0)] |
| 140. | Balaj L, Lessard R, Dai L, Cho YJ, Pomeroy SL, Breakefield XO, Skog J. Tumour microvesicles contain retrotransposon elements and amplified oncogene sequences. Nat Commun. 2011;2:180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 962] [Cited by in RCA: 954] [Article Influence: 63.6] [Reference Citation Analysis (0)] |
| 141. | Salido-Guadarrama I, Romero-Cordoba S, Peralta-Zaragoza O, Hidalgo-Miranda A, Rodríguez-Dorantes M. MicroRNAs transported by exosomes in body fluids as mediators of intercellular communication in cancer. Onco Targets Ther. 2014;7:1327-1338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 142. | Valadi H, Ekström K, Bossios A, Sjöstrand M, Lee JJ, Lötvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9:654-659. [PubMed] |
| 143. | Turchinovich A, Weiz L, Langheinz A, Burwinkel B. Characterization of extracellular circulating microRNA. Nucleic Acids Res. 2011;39:7223-7233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1356] [Cited by in RCA: 1553] [Article Influence: 103.5] [Reference Citation Analysis (0)] |
| 144. | Vedeler A, Hollås H, Grindheim AK, Raddum AM. Multiple roles of annexin A2 in post-transcriptional regulation of gene expression. Curr Protein Pept Sci. 2012;13:401-412. [PubMed] |
| 145. | Villarroya-Beltri C, Gutiérrez-Vázquez C, Sánchez-Cabo F, Pérez-Hernández D, Vázquez J, Martin-Cofreces N, Martinez-Herrera DJ, Pascual-Montano A, Mittelbrunn M, Sánchez-Madrid F. Sumoylated hnRNPA2B1 controls the sorting of miRNAs into exosomes through binding to specific motifs. Nat Commun. 2013;4:2980. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1165] [Cited by in RCA: 1581] [Article Influence: 131.8] [Reference Citation Analysis (0)] |
| 146. | Kogure T, Yan IK, Lin WL, Patel T. Extracellular Vesicle-Mediated Transfer of a Novel Long Noncoding RNA TUC339: A Mechanism of Intercellular Signaling in Human Hepatocellular Cancer. Genes Cancer. 2013;4:261-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 264] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 147. | Pinto R, De Summa S, Petriella D, Tudoran O, Danza K, Tommasi S. The value of new high-throughput technologies for diagnosis and prognosis in solid tumors. Cancer Biomark. 2014;14:103-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 148. | Iwakawa HO, Tomari Y. The Functions of MicroRNAs: mRNA Decay and Translational Repression. Trends Cell Biol. 2015;25:651-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 499] [Cited by in RCA: 574] [Article Influence: 52.2] [Reference Citation Analysis (0)] |
| 149. | Sato-Kuwabara Y, Melo SA, Soares FA, Calin GA. The fusion of two worlds: non-coding RNAs and extracellular vesicles--diagnostic and therapeutic implications (Review). Int J Oncol. 2015;46:17-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 151] [Cited by in RCA: 192] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 150. | Garg M. Targeting microRNAs in epithelial-to-mesenchymal transition-induced cancer stem cells: therapeutic approaches in cancer. Expert Opin Ther Targets. 2015;19:285-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 151. | Garofalo M, Croce CM. Role of microRNAs in maintaining cancer stem cells. Adv Drug Deliv Rev. 2015;81:53-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 94] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 152. | Katoh M. Therapeutics targeting angiogenesis: genetics and epigenetics, extracellular miRNAs and signaling networks (Review). Int J Mol Med. 2013;32:763-767. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 121] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 153. | Palma J, Yaddanapudi SC, Pigati L, Havens MA, Jeong S, Weiner GA, Weimer KM, Stern B, Hastings ML, Duelli DM. MicroRNAs are exported from malignant cells in customized particles. Nucleic Acids Res. 2012;40:9125-9138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 158] [Cited by in RCA: 184] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 154. | Rappa G, Mercapide J, Anzanello F, Pope RM, Lorico A. Biochemical and biological characterization of exosomes containing prominin-1/CD133. Mol Cancer. 2013;12:62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 96] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 155. | Silva A, Bullock M, Calin G. The Clinical Relevance of Long Non-Coding RNAs in Cancer. Cancers (Basel). 2015;7:2169-2182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 120] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 156. | Fitzgerald TL, McCubrey JA. Pancreatic cancer stem cells: association with cell surface markers, prognosis, resistance, metastasis and treatment. Adv Biol Regul. 2014;56:45-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 80] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 157. | Abel EV, Simeone DM. Biology and clinical applications of pancreatic cancer stem cells. Gastroenterology. 2013;144:1241-1248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 85] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 158. | Ohara Y, Oda T, Sugano M, Hashimoto S, Enomoto T, Yamada K, Akashi Y, Miyamoto R, Kobayashi A, Fukunaga K. Histological and prognostic importance of CD44(+) /CD24(+) /EpCAM(+) expression in clinical pancreatic cancer. Cancer Sci. 2013;104:1127-1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 60] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 159. | Hori Y. Prominin-1 (CD133) Reveals New Faces of Pancreatic Progenitor Cells and Cancer Stem Cells: Current Knowledge and Therapeutic Perspectives. Adv Exp Med Biol. 2013;777:185-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 160. | Balic A, Dorado J, Alonso-Gómez M, Heeschen C. Stem cells as the root of pancreatic ductal adenocarcinoma. Exp Cell Res. 2012;318:691-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 161. | Vaz AP, Ponnusamy MP, Seshacharyulu P, Batra SK. A concise review on the current understanding of pancreatic cancer stem cells. J Cancer Stem Cell Res. 2014;2:e1004. [PubMed] |
| 162. | Wang H, Rana S, Giese N, Büchler MW, Zöller M. Tspan8, CD44v6 and alpha6beta4 are biomarkers of migrating pancreatic cancer-initiating cells. Int J Cancer. 2013;133:416-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 70] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 163. | Li C, Wu JJ, Hynes M, Dosch J, Sarkar B, Welling TH, Pasca di Magliano M, Simeone DM. c-Met is a marker of pancreatic cancer stem cells and therapeutic target. Gastroenterology. 2011;141:2218-2227.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 292] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 164. | Saito S, Okabe H, Watanabe M, Ishimoto T, Iwatsuki M, Baba Y, Tanaka Y, Kurashige J, Miyamoto Y, Baba H. CD44v6 expression is related to mesenchymal phenotype and poor prognosis in patients with colorectal cancer. Oncol Rep. 2013;29:1570-1578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 68] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 165. | Todaro M, Gaggianesi M, Catalano V, Benfante A, Iovino F, Biffoni M, Apuzzo T, Sperduti I, Volpe S, Cocorullo G. CD44v6 is a marker of constitutive and reprogrammed cancer stem cells driving colon cancer metastasis. Cell Stem Cell. 2014;14:342-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 476] [Cited by in RCA: 589] [Article Influence: 49.1] [Reference Citation Analysis (0)] |
| 166. | Dalla Pozza E, Dando I, Biondani G, Brandi J, Costanzo C, Zoratti E, Fassan M, Boschi F, Melisi D, Cecconi D. Pancreatic ductal adenocarcinoma cell lines display a plastic ability to bidirectionally convert into cancer stem cells. Int J Oncol. 2015;46:1099-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 167. | Klingbeil P, Marhaba R, Jung T, Kirmse R, Ludwig T, Zöller M. CD44 variant isoforms promote metastasis formation by a tumor cell-matrix cross-talk that supports adhesion and apoptosis resistance. Mol Cancer Res. 2009;7:168-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 88] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 168. | Matzke-Ogi A, Jannasch K, Shatirishvili M, Fuchs B, Chiblak S, Morton J, Tawk B, Lindner T, Sansom O, Alves F. Inhibition of Tumor Growth and Metastasis in Pancreatic Cancer Models by Interference With CD44v6 Signaling. Gastroenterology. 2016;150:513-25.e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 86] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 169. | Chen K, Li Z, Jiang P, Zhang X, Zhang Y, Jiang Y, He Y, Li X. Co-expression of CD133, CD44v6 and human tissue factor is associated with metastasis and poor prognosis in pancreatic carcinoma. Oncol Rep. 2014;32:755-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 170. | Aruffo A, Stamenkovic I, Melnick M, Underhill CB, Seed B. CD44 is the principal cell surface receptor for hyaluronate. Cell. 1990;61:1303-1313. [PubMed] |
| 171. | Ishii S, Ford R, Thomas P, Nachman A, Steele G, Jessup JM. CD44 participates in the adhesion of human colorectal carcinoma cells to laminin and type IV collagen. Surg Oncol. 1993;2:255-264. [PubMed] |
| 172. | Jalkanen S, Jalkanen M. Lymphocyte CD44 binds the COOH-terminal heparin-binding domain of fibronectin. J Cell Biol. 1992;116:817-825. [PubMed] |
| 173. | Konstantopoulos K, Thomas SN. Cancer cells in transit: the vascular interactions of tumor cells. Annu Rev Biomed Eng. 2009;11:177-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 173] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 174. | Kim MS, Park MJ, Moon EJ, Kim SJ, Lee CH, Yoo H, Shin SH, Song ES, Lee SH. Hyaluronic acid induces osteopontin via the phosphatidylinositol 3-kinase/Akt pathway to enhance the motility of human glioma cells. Cancer Res. 2005;65:686-691. [PubMed] |
| 175. | Khan SA, Cook AC, Kappil M, Günthert U, Chambers AF, Tuck AB, Denhardt DT. Enhanced cell surface CD44 variant (v6, v9) expression by osteopontin in breast cancer epithelial cells facilitates tumor cell migration: novel post-transcriptional, post-translational regulation. Clin Exp Metastasis. 2005;22:663-673. [PubMed] |
| 176. | Tremmel M, Matzke A, Albrecht I, Laib AM, Olaku V, Ballmer-Hofer K, Christofori G, Héroult M, Augustin HG, Ponta H. A CD44v6 peptide reveals a role of CD44 in VEGFR-2 signaling and angiogenesis. Blood. 2009;114:5236-5244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 126] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 177. | Zöller M. CD44: can a cancer-initiating cell profit from an abundantly expressed molecule? Nat Rev Cancer. 2011;11:254-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 785] [Cited by in RCA: 886] [Article Influence: 59.1] [Reference Citation Analysis (0)] |
| 178. | Kollet O, Dar A, Shivtiel S, Kalinkovich A, Lapid K, Sztainberg Y, Tesio M, Samstein RM, Goichberg P, Spiegel A. Osteoclasts degrade endosteal components and promote mobilization of hematopoietic progenitor cells. Nat Med. 2006;12:657-664. [PubMed] |
| 179. | Weber GF, Bronson RT, Ilagan J, Cantor H, Schmits R, Mak TW. Absence of the CD44 gene prevents sarcoma metastasis. Cancer Res. 2002;62:2281-2286. [PubMed] |
| 180. | Williams K, Motiani K, Giridhar PV, Kasper S. CD44 integrates signaling in normal stem cell, cancer stem cell and (pre)metastatic niches. Exp Biol Med (Maywood). 2013;238:324-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 174] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 181. | Trusolino L, Bertotti A, Comoglio PM. MET signalling: principles and functions in development, organ regeneration and cancer. Nat Rev Mol Cell Biol. 2010;11:834-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 850] [Cited by in RCA: 987] [Article Influence: 61.7] [Reference Citation Analysis (1)] |
| 182. | Lokeshwar VB, Fregien N, Bourguignon LY. Ankyrin-binding domain of CD44(GP85) is required for the expression of hyaluronic acid-mediated adhesion function. J Cell Biol. 1994;126:1099-1109. [PubMed] |
| 183. | Fehon RG, McClatchey AI, Bretscher A. Organizing the cell cortex: the role of ERM proteins. Nat Rev Mol Cell Biol. 2010;11:276-287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 887] [Cited by in RCA: 852] [Article Influence: 53.3] [Reference Citation Analysis (0)] |
| 184. | Mori T, Kitano K, Terawaki S, Maesaki R, Fukami Y, Hakoshima T. Structural basis for CD44 recognition by ERM proteins. J Biol Chem. 2008;283:29602-29612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 106] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 185. | Nagano O, Saya H. Mechanism and biological significance of CD44 cleavage. Cancer Sci. 2004;95:930-935. [PubMed] |
| 186. | Okamoto I, Kawano Y, Murakami D, Sasayama T, Araki N, Miki T, Wong AJ, Saya H. Proteolytic release of CD44 intracellular domain and its role in the CD44 signaling pathway. J Cell Biol. 2001;155:755-762. [PubMed] |
| 187. | Miletti-González KE, Murphy K, Kumaran MN, Ravindranath AK, Wernyj RP, Kaur S, Miles GD, Lim E, Chan R, Chekmareva M. Identification of function for CD44 intracytoplasmic domain (CD44-ICD): modulation of matrix metalloproteinase 9 (MMP-9) transcription via novel promoter response element. J Biol Chem. 2012;287:18995-19007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 104] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 188. | Pietras A, Katz AM, Ekström EJ, Wee B, Halliday JJ, Pitter KL, Werbeck JL, Amankulor NM, Huse JT, Holland EC. Osteopontin-CD44 signaling in the glioma perivascular niche enhances cancer stem cell phenotypes and promotes aggressive tumor growth. Cell Stem Cell. 2014;14:357-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 335] [Cited by in RCA: 425] [Article Influence: 35.4] [Reference Citation Analysis (0)] |
| 189. | Oliferenko S, Paiha K, Harder T, Gerke V, Schwärzler C, Schwarz H, Beug H, Günthert U, Huber LA. Analysis of CD44-containing lipid rafts: Recruitment of annexin II and stabilization by the actin cytoskeleton. J Cell Biol. 1999;146:843-854. [PubMed] |
| 190. | Zarbock A, Ley K, McEver RP, Hidalgo A. Leukocyte ligands for endothelial selectins: specialized glycoconjugates that mediate rolling and signaling under flow. Blood. 2011;118:6743-6751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 433] [Article Influence: 28.9] [Reference Citation Analysis (0)] |
| 191. | Föger N, Marhaba R, Zöller M. Involvement of CD44 in cytoskeleton rearrangement and raft reorganization in T cells. J Cell Sci. 2001;114:1169-1178. [PubMed] |
| 192. | Róg T, Vattulainen I. Cholesterol, sphingolipids, and glycolipids: what do we know about their role in raft-like membranes? Chem Phys Lipids. 2014;184:82-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 157] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 193. | Lin ML, Lu YC, Chen HY, Lee CC, Chung JG, Chen SS. Suppressing the formation of lipid raft-associated Rac1/PI3K/Akt signaling complexes by curcumin inhibits SDF-1α-induced invasion of human esophageal carcinoma cells. Mol Carcinog. 2014;53:360-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 194. | Ratajczak MZ, Lee H, Wysoczynski M, Wan W, Marlicz W, Laughlin MJ, Kucia M, Janowska-Wieczorek A, Ratajczak J. Novel insight into stem cell mobilization-plasma sphingosine-1-phosphate is a major chemoattractant that directs the egress of hematopoietic stem progenitor cells from the bone marrow and its level in peripheral blood increases during mobilization due to activation of complement cascade/membrane attack complex. Leukemia. 2010;24:976-985. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 215] [Cited by in RCA: 215] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 195. | Desai B, Ma T, Zhu J, Chellaiah MA. Characterization of the expression of variant and standard CD44 in prostate cancer cells: identification of the possible molecular mechanism of CD44/MMP9 complex formation on the cell surface. J Cell Biochem. 2009;108:272-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 56] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 196. | Bourguignon LY, Gunja-Smith Z, Iida N, Zhu HB, Young LJ, Muller WJ, Cardiff RD. CD44v(3,8-10) is involved in cytoskeleton-mediated tumor cell migration and matrix metalloproteinase (MMP-9) association in metastatic breast cancer cells. J Cell Physiol. 1998;176:206-215. [PubMed] |
| 197. | Zarzynska JM. Two faces of TGF-beta1 in breast cancer. Mediators Inflamm. 2014;2014:141747. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 155] [Cited by in RCA: 177] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 198. | Takahashi E, Nagano O, Ishimoto T, Yae T, Suzuki Y, Shinoda T, Nakamura S, Niwa S, Ikeda S, Koga H. Tumor necrosis factor-alpha regulates transforming growth factor-beta-dependent epithelial-mesenchymal transition by promoting hyaluronan-CD44-moesin interaction. J Biol Chem. 2010;285:4060-4073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 138] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 199. | Zöller M. CD44, Hyaluronan, the Hematopoietic Stem Cell, and Leukemia-Initiating Cells. Front Immunol. 2015;6:235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 200. | Rutnam ZJ, Yang BB. The non-coding 3’ UTR of CD44 induces metastasis by regulating extracellular matrix functions. J Cell Sci. 2012;125:2075-2085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 201. | Bourguignon LY, Earle C, Wong G, Spevak CC, Krueger K. Stem cell marker (Nanog) and Stat-3 signaling promote MicroRNA-21 expression and chemoresistance in hyaluronan/CD44-activated head and neck squamous cell carcinoma cells. Oncogene. 2012;31:149-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 202] [Cited by in RCA: 210] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 202. | Rana S, Malinowska K, Zöller M. Exosomal tumor microRNA modulates premetastatic organ cells. Neoplasia. 2013;15:281-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 292] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 203. | Delitto D, Vertes-George E, Hughes SJ, Behrns KE, Trevino JG. c-Met signaling in the development of tumorigenesis and chemoresistance: potential applications in pancreatic cancer. World J Gastroenterol. 2014;20:8458-8470. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 49] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 204. | Orian-Rousseau V, Morrison H, Matzke A, Kastilan T, Pace G, Herrlich P, Ponta H. Hepatocyte growth factor-induced Ras activation requires ERM proteins linked to both CD44v6 and F-actin. Mol Biol Cell. 2007;18:76-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 152] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 205. | Maroun CR, Rowlands T. The Met receptor tyrosine kinase: a key player in oncogenesis and drug resistance. Pharmacol Ther. 2014;142:316-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 171] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 206. | Marano L, Chiari R, Fabozzi A, De Vita F, Boccardi V, Roviello G, Petrioli R, Marrelli D, Roviello F, Patriti A. c-Met targeting in advanced gastric cancer: An open challenge. Cancer Lett. 2015;365:30-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 207. | Jung T, Gross W, Zöller M. CD44v6 coordinates tumor matrix-triggered motility and apoptosis resistance. J Biol Chem. 2011;286:15862-15874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 66] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 208. | Ni J, Cozzi PJ, Hao JL, Beretov J, Chang L, Duan W, Shigdar S, Delprado WJ, Graham PH, Bucci J. CD44 variant 6 is associated with prostate cancer metastasis and chemo-/radioresistance. Prostate. 2014;74:602-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 125] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 209. | Hasenauer S, Malinger D, Koschut D, Pace G, Matzke A, von Au A, Orian-Rousseau V. Internalization of Met requires the co-receptor CD44v6 and its link to ERM proteins. PLoS One. 2013;8:e62357. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 210. | Dallas NA, Xia L, Fan F, Gray MJ, Gaur P, van Buren G, Samuel S, Kim MP, Lim SJ, Ellis LM. Chemoresistant colorectal cancer cells, the cancer stem cell phenotype, and increased sensitivity to insulin-like growth factor-I receptor inhibition. Cancer Res. 2009;69:1951-1957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 386] [Cited by in RCA: 458] [Article Influence: 26.9] [Reference Citation Analysis (0)] |
| 211. | Porsch H, Mehić M, Olofsson B, Heldin P, Heldin CH. Platelet-derived growth factor β-receptor, transforming growth factor β type I receptor, and CD44 protein modulate each other’s signaling and stability. J Biol Chem. 2014;289:19747-19757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 212. | Sakai K, Aoki S, Matsumoto K. Hepatocyte growth factor and Met in drug discovery. J Biochem. 2015;157:271-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 61] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 213. | Maecker HT, Todd SC, Levy S. The tetraspanin superfamily: molecular facilitators. FASEB J. 1997;11:428-442. [PubMed] |
| 214. | Hemler ME. Tetraspanin proteins promote multiple cancer stages. Nat Rev Cancer. 2014;14:49-60. [PubMed] |
| 215. | Wang HX, Li Q, Sharma C, Knoblich K, Hemler ME. Tetraspanin protein contributions to cancer. Biochem Soc Trans. 2011;39:547-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 63] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 216. | Guo Q, Xia B, Zhang F, Richardson MM, Li M, Zhang JS, Chen F, Zhang XA. Tetraspanin CO-029 inhibits colorectal cancer cell movement by deregulating cell-matrix and cell-cell adhesions. PLoS One. 2012;7:e38464. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 217. | Berthier-Vergnes O, Kharbili ME, de la Fouchardière A, Pointecouteau T, Verrando P, Wierinckx A, Lachuer J, Le Naour F, Lamartine J. Gene expression profiles of human melanoma cells with different invasive potential reveal TSPAN8 as a novel mediator of invasion. Br J Cancer. 2011;104:155-165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 218. | Sterk LM, Geuijen CA, van den Berg JG, Claessen N, Weening JJ, Sonnenberg A. Association of the tetraspanin CD151 with the laminin-binding integrins alpha3beta1, alpha6beta1, alpha6beta4 and alpha7beta1 in cells in culture and in vivo. J Cell Sci. 2002;115:1161-1173. [PubMed] |
| 219. | Liu L, He B, Liu WM, Zhou D, Cox JV, Zhang XA. Tetraspanin CD151 promotes cell migration by regulating integrin trafficking. J Biol Chem. 2007;282:31631-31642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 112] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 220. | Zijlstra A, Lewis J, Degryse B, Stuhlmann H, Quigley JP. The inhibition of tumor cell intravasation and subsequent metastasis via regulation of in vivo tumor cell motility by the tetraspanin CD151. Cancer Cell. 2008;13:221-234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 201] [Cited by in RCA: 195] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 221. | Hong IK, Jeoung DI, Ha KS, Kim YM, Lee H. Tetraspanin CD151 stimulates adhesion-dependent activation of Ras, Rac, and Cdc42 by facilitating molecular association between β1 integrins and small GTPases. J Biol Chem. 2012;287:32027-32039. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 222. | Yang XH, Mirchev R, Deng X, Yacono P, Yang HL, Golan DE, Hemler ME. CD151 restricts the α6 integrin diffusion mode. J Cell Sci. 2012;125:1478-1487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 223. | Wei L, Li Y, Suo Z. TSPAN8 promotes gastric cancer growth and metastasis via ERK MAPK pathway. Int J Clin Exp Med. 2015;8:8599-8607. [PubMed] |
| 224. | Kim TK, Park CS, Jeoung MH, Lee WR, Go NK, Choi JR, Lee TS, Shim H, Lee S. Generation of a human antibody that inhibits TSPAN8-mediated invasion of metastatic colorectal cancer cells. Biochem Biophys Res Commun. 2015;468:774-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 225. | Zhu H, Wu Y, Zheng W, Lu S. CO-029 is overexpressed in gastric cancer and mediates the effects of EGF on gastric cancer cell proliferation and invasion. Int J Mol Med. 2015;35:798-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 226. | Zhou Z, Ran YL, Hu H, Pan J, Li ZF, Chen LZ, Sun LC, Peng L, Zhao XL, Yu L. TM4SF3 promotes esophageal carcinoma metastasis via upregulating ADAM12m expression. Clin Exp Metastasis. 2008;25:537-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 227. | Hemler ME. Tetraspanin functions and associated microdomains. Nat Rev Mol Cell Biol. 2005;6:801-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 958] [Cited by in RCA: 1078] [Article Influence: 51.3] [Reference Citation Analysis (0)] |
| 228. | Levy S, Shoham T. Protein-protein interactions in the tetraspanin web. Physiology (Bethesda). 2005;20:218-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 175] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 229. | Stipp CS, Kolesnikova TV, Hemler ME. Functional domains in tetraspanin proteins. Trends Biochem Sci. 2003;28:106-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 367] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 230. | Seigneuret M. Complete predicted three-dimensional structure of the facilitator transmembrane protein and hepatitis C virus receptor CD81: conserved and variable structural domains in the tetraspanin superfamily. Biophys J. 2006;90:212-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 91] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 231. | Berditchevski F, Odintsova E, Sawada S, Gilbert E. Expression of the palmitoylation-deficient CD151 weakens the association of alpha 3 beta 1 integrin with the tetraspanin-enriched microdomains and affects integrin-dependent signaling. J Biol Chem. 2002;277:36991-37000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 173] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 232. | Delandre C, Penabaz TR, Passarelli AL, Chapes SK, Clem RJ. Mutation of juxtamembrane cysteines in the tetraspanin CD81 affects palmitoylation and alters interaction with other proteins at the cell surface. Exp Cell Res. 2009;315:1953-1963. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 233. | Sharma C, Yang XH, Hemler ME. DHHC2 affects palmitoylation, stability, and functions of tetraspanins CD9 and CD151. Mol Biol Cell. 2008;19:3415-3425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 234. | Todeschini AR, Dos Santos JN, Handa K, Hakomori SI. Ganglioside GM2/GM3 complex affixed on silica nanospheres strongly inhibits cell motility through CD82/cMet-mediated pathway. Proc Natl Acad Sci USA. 2008;105:1925-1930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 92] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 235. | Wang XQ, Yan Q, Sun P, Liu JW, Go L, McDaniel SM, Paller AS. Suppression of epidermal growth factor receptor signaling by protein kinase C-alpha activation requires CD82, caveolin-1, and ganglioside. Cancer Res. 2007;67:9986-9995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 78] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 236. | Delaguillaumie A, Harriague J, Kohanna S, Bismuth G, Rubinstein E, Seigneuret M, Conjeaud H. Tetraspanin CD82 controls the association of cholesterol-dependent microdomains with the actin cytoskeleton in T lymphocytes: relevance to co-stimulation. J Cell Sci. 2004;117:5269-5282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 74] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 237. | Escola JM, Kleijmeer MJ, Stoorvogel W, Griffith JM, Yoshie O, Geuze HJ. Selective enrichment of tetraspan proteins on the internal vesicles of multivesicular endosomes and on exosomes secreted by human B-lymphocytes. J Biol Chem. 1998;273:20121-20127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 902] [Cited by in RCA: 973] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 238. | Berditchevski F, Odintsova E. Tetraspanins as regulators of protein trafficking. Traffic. 2007;8:89-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 236] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 239. | Marks MS, Ohno H, Kirchnausen T, Bonracino JS. Protein sorting by tyrosine-based signals: adapting to the Ys and wherefores. Trends Cell Biol. 1997;7:124-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 257] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 240. | Charrin S, le Naour F, Silvie O, Milhiet PE, Boucheix C, Rubinstein E. Lateral organization of membrane proteins: tetraspanins spin their web. Biochem J. 2009;420:133-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 313] [Cited by in RCA: 346] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 241. | Berditchevski F. Complexes of tetraspanins with integrins: more than meets the eye. J Cell Sci. 2001;114:4143-4151. [PubMed] |
| 242. | Bassani S, Cingolani LA. Tetraspanins: Interactions and interplay with integrins. Int J Biochem Cell Biol. 2012;44:703-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 76] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 243. | Herlevsen M, Schmidt DS, Miyazaki K, Zöller M. The association of the tetraspanin D6.1A with the alpha6beta4 integrin supports cell motility and liver metastasis formation. J Cell Sci. 2003;116:4373-4390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 52] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 244. | Gesierich S, Paret C, Hildebrand D, Weitz J, Zgraggen K, Schmitz-Winnenthal FH, Horejsi V, Yoshie O, Herlyn D, Ashman LK. Colocalization of the tetraspanins, CO-029 and CD151, with integrins in human pancreatic adenocarcinoma: impact on cell motility. Clin Cancer Res. 2005;11:2840-2852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 97] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 245. | Yue S, Mu W, Zöller M. Tspan8 and CD151 promote metastasis by distinct mechanisms. Eur J Cancer. 2013;49:2934-2948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 246. | Gesierich S, Berezovskiy I, Ryschich E, Zöller M. Systemic induction of the angiogenesis switch by the tetraspanin D6.1A/CO-029. Cancer Res. 2006;66:7083-7094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 164] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 247. | Nazarenko I, Rana S, Baumann A, McAlear J, Hellwig A, Trendelenburg M, Lochnit G, Preissner KT, Zöller M. Cell surface tetraspanin Tspan8 contributes to molecular pathways of exosome-induced endothelial cell activation. Cancer Res. 2010;70:1668-1678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 573] [Cited by in RCA: 545] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 248. | Yáñez-Mó M, Gutiérrez-López MD, Cabañas C. Functional interplay between tetraspanins and proteases. Cell Mol Life Sci. 2011;68:3323-3335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 57] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 249. | Le Naour F, André M, Greco C, Billard M, Sordat B, Emile JF, Lanza F, Boucheix C, Rubinstein E. Profiling of the tetraspanin web of human colon cancer cells. Mol Cell Proteomics. 2006;5:845-857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 132] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 250. | Wang GP, Han XF. CD9 modulates proliferation of human glioblastoma cells via epidermal growth factor receptor signaling. Mol Med Rep. 2015;12:1381-1386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 251. | Sridhar SC, Miranti CK. Tetraspanin KAI1/CD82 suppresses invasion by inhibiting integrin-dependent crosstalk with c-Met receptor and Src kinases. Oncogene. 2006;25:2367-2378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 119] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 252. | Little KD, Hemler ME, Stipp CS. Dynamic regulation of a GPCR-tetraspanin-G protein complex on intact cells: central role of CD81 in facilitating GPR56-Galpha q/11 association. Mol Biol Cell. 2004;15:2375-2387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 158] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 253. | Feng S, Agoulnik IU, Truong A, Li Z, Creighton CJ, Kaftanovskaya EM, Pereira R, Han HD, Lopez-Berestein G, Klonisch T. Suppression of relaxin receptor RXFP1 decreases prostate cancer growth and metastasis. Endocr Relat Cancer. 2010;17:1021-1033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 61] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 254. | André M, Le Caer JP, Greco C, Planchon S, El Nemer W, Boucheix C, Rubinstein E, Chamot-Rooke J, Le Naour F. Proteomic analysis of the tetraspanin web using LC-ESI-MS/MS and MALDI-FTICR-MS. Proteomics. 2006;6:1437-1449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 75] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 255. | Zhang XA, Bontrager AL, Hemler ME. Transmembrane-4 superfamily proteins associate with activated protein kinase C (PKC) and link PKC to specific beta(1) integrins. J Biol Chem. 2001;276:25005-25013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 272] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 256. | Claas C, Stipp CS, Hemler ME. Evaluation of prototype transmembrane 4 superfamily protein complexes and their relation to lipid rafts. J Biol Chem. 2001;276:7974-7984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 246] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 257. | Claas C, Wahl J, Orlicky DJ, Karaduman H, Schnölzer M, Kempf T, Zöller M. The tetraspanin D6.1A and its molecular partners on rat carcinoma cells. Biochem J. 2005;389:99-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 40] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 258. | Le Naour F, André M, Boucheix C, Rubinstein E. Membrane microdomains and proteomics: lessons from tetraspanin microdomains and comparison with lipid rafts. Proteomics. 2006;6:6447-6454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 102] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 259. | Kuhn S, Koch M, Nübel T, Ladwein M, Antolovic D, Klingbeil P, Hildebrand D, Moldenhauer G, Langbein L, Franke WW. A complex of EpCAM, claudin-7, CD44 variant isoforms, and tetraspanins promotes colorectal cancer progression. Mol Cancer Res. 2007;5:553-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 199] [Article Influence: 10.5] [Reference Citation Analysis (2)] |
| 260. | Yáñez-Mó M, Barreiro O, Gordon-Alonso M, Sala-Valdés M, Sánchez-Madrid F. Tetraspanin-enriched microdomains: a functional unit in cell plasma membranes. Trends Cell Biol. 2009;19:434-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 421] [Cited by in RCA: 492] [Article Influence: 28.9] [Reference Citation Analysis (0)] |
| 261. | Hemler ME. Tetraspanin proteins mediate cellular penetration, invasion, and fusion events and define a novel type of membrane microdomain. Annu Rev Cell Dev Biol. 2003;19:397-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 607] [Cited by in RCA: 668] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
| 262. | Andreu Z, Yáñez-Mó M. Tetraspanins in extracellular vesicle formation and function. Front Immunol. 2014;5:442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 697] [Cited by in RCA: 1106] [Article Influence: 92.2] [Reference Citation Analysis (0)] |
| 263. | Scheffer KD, Gawlitza A, Spoden GA, Zhang XA, Lambert C, Berditchevski F, Florin L. Tetraspanin CD151 mediates papillomavirus type 16 endocytosis. J Virol. 2013;87:3435-3446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 121] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 264. | Stipp CS. Laminin-binding integrins and their tetraspanin partners as potential antimetastatic targets. Expert Rev Mol Med. 2010;12:e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 117] [Cited by in RCA: 138] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 265. | Klinovska K, Sebkova N, Dvorakova-Hortova K. Sperm-egg fusion: a molecular enigma of mammalian reproduction. Int J Mol Sci. 2014;15:10652-10668. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 266. | Monk PN, Partridge LJ. Tetraspanins: gateways for infection. Infect Disord Drug Targets. 2012;12:4-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 267. | Thali M. The roles of tetraspanins in HIV-1 replication. Curr Top Microbiol Immunol. 2009;339:85-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 268. | Zhang XA, Huang C. Tetraspanins and cell membrane tubular structures. Cell Mol Life Sci. 2012;69:2843-2852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 269. | Conley SM, Stuck MW, Naash MI. Structural and functional relationships between photoreceptor tetraspanins and other superfamily members. Cell Mol Life Sci. 2012;69:1035-1047. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 270. | Greco C, Bralet MP, Ailane N, Dubart-Kupperschmitt A, Rubinstein E, Le Naour F, Boucheix C. E-cadherin/p120-catenin and tetraspanin Co-029 cooperate for cell motility control in human colon carcinoma. Cancer Res. 2010;70:7674-7683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 271. | Apostolou P, Toloudi M, Ioannou E, Kourtidou E, Chatziioannou M, Kopic A, Komiotis D, Kiritsis C, Manta S, Papasotiriou I. Study of the interaction among Notch pathway receptors, correlation with stemness, as well as their interaction with CD44, dipeptidyl peptidase-IV, hepatocyte growth factor receptor and the SETMAR transferase, in colon cancer stem cells. J Recept Signal Transduct Res. 2013;33:353-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 272. | Palagani V, El Khatib M, Kossatz U, Bozko P, Müller MR, Manns MP, Krech T, Malek NP, Plentz RR. Epithelial mesenchymal transition and pancreatic tumor initiating CD44+/EpCAM+ cells are inhibited by γ-secretase inhibitor IX. PLoS One. 2012;7:e46514. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 273. | Philip R, Heiler S, Mu W, Büchler MW, Zöller M, Thuma F. Claudin-7 promotes the epithelial-mesenchymal transition in human colorectal cancer. Oncotarget. 2015;6:2046-2063. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 67] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 274. | Sadej R, Grudowska A, Turczyk L, Kordek R, Romanska HM. CD151 in cancer progression and metastasis: a complex scenario. Lab Invest. 2014;94:41-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 275. | Ashman L, Zöller M. Tetraspanin and metastasis. Tetraspanins. Berlin: Springer Verlag 2013; 257-298. |
| 276. | Cruz-Monserrate Z, O’Connor KL. Integrin alpha 6 beta 4 promotes migration, invasion through Tiam1 upregulation, and subsequent Rac activation. Neoplasia. 2008;10:408-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 62] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 277. | Cruz-Monserrate Z, Qiu S, Evers BM, O’Connor KL. Upregulation and redistribution of integrin alpha6beta4 expression occurs at an early stage in pancreatic adenocarcinoma progression. Mod Pathol. 2007;20:656-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 278. | Baril P, Gangeswaran R, Mahon PC, Caulee K, Kocher HM, Harada T, Zhu M, Kalthoff H, Crnogorac-Jurcevic T, Lemoine NR. Periostin promotes invasiveness and resistance of pancreatic cancer cells to hypoxia-induced cell death: role of the beta4 integrin and the PI3k pathway. Oncogene. 2007;26:2082-2094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 238] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 279. | Carpenter BL, Chen M, Knifley T, Davis KA, Harrison SM, Stewart RL, O’Connor KL. Integrin α6β4 Promotes Autocrine Epidermal Growth Factor Receptor (EGFR) Signaling to Stimulate Migration and Invasion toward Hepatocyte Growth Factor (HGF). J Biol Chem. 2015;290:27228-27238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 280. | Laval S, Laklai H, Fanjul M, Pucelle M, Laurell H, Billon-Galés A, Le Guellec S, Delisle MB, Sonnenberg A, Susini C. Dual roles of hemidesmosomal proteins in the pancreatic epithelium: the phosphoinositide 3-kinase decides. Oncogene. 2014;33:1934-1944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 281. | Giancotti FG. Signal transduction by the alpha 6 beta 4 integrin: charting the path between laminin binding and nuclear events. J Cell Sci. 1996;109:1165-1172. [PubMed] |
| 282. | Yang XH, Flores LM, Li Q, Zhou P, Xu F, Krop IE, Hemler ME. Disruption of laminin-integrin-CD151-focal adhesion kinase axis sensitizes breast cancer cells to ErbB2 antagonists. Cancer Res. 2010;70:2256-2263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 116] [Cited by in RCA: 112] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 283. | Lipscomb EA, Mercurio AM. Mobilization and activation of a signaling competent alpha6beta4integrin underlies its contribution to carcinoma progression. Cancer Metastasis Rev. 2005;24:413-423. [PubMed] |
| 284. | Gagnoux-Palacios L, Dans M, van’t Hof W, Mariotti A, Pepe A, Meneguzzi G, Resh MD, Giancotti FG. Compartmentalization of integrin alpha6beta4 signaling in lipid rafts. J Cell Biol. 2003;162:1189-1196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 99] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 285. | Yang X, Kovalenko OV, Tang W, Claas C, Stipp CS, Hemler ME. Palmitoylation supports assembly and function of integrin-tetraspanin complexes. J Cell Biol. 2004;167:1231-1240. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 170] [Cited by in RCA: 179] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 286. | Sharma C, Rabinovitz I, Hemler ME. Palmitoylation by DHHC3 is critical for the function, expression, and stability of integrin α6β4. Cell Mol Life Sci. 2012;69:2233-2244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 287. | Germain EC, Santos TM, Rabinovitz I. Phosphorylation of a novel site on the {beta}4 integrin at the trailing edge of migrating cells promotes hemidesmosome disassembly. Mol Biol Cell. 2009;20:56-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 288. | Frijns E, Sachs N, Kreft M, Wilhelmsen K, Sonnenberg A. EGF-induced MAPK signaling inhibits hemidesmosome formation through phosphorylation of the integrin {beta}4. J Biol Chem. 2010;285:37650-37662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 289. | O’Connor KL, Chen M, Towers LN. Integrin α6β4 cooperates with LPA signaling to stimulate Rac through AKAP-Lbc-mediated RhoA activation. Am J Physiol Cell Physiol. 2012;302:C605-C614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 290. | Stewart RL, O’Connor KL. Clinical significance of the integrin α6β4 in human malignancies. Lab Invest. 2015;95:976-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 181] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 291. | Wang H, Leavitt L, Ramaswamy R, Rapraeger AC. Interaction of syndecan and alpha6beta4 integrin cytoplasmic domains: regulation of ErbB2-mediated integrin activation. J Biol Chem. 2010;285:13569-13579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 57] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 292. | Chung J, Yoon SO, Lipscomb EA, Mercurio AM. The Met receptor and alpha 6 beta 4 integrin can function independently to promote carcinoma invasion. J Biol Chem. 2004;279:32287-32293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 293. | Wang H, Jin H, Beauvais DM, Rapraeger AC. Cytoplasmic domain interactions of syndecan-1 and syndecan-4 with α6β4 integrin mediate human epidermal growth factor receptor (HER1 and HER2)-dependent motility and survival. J Biol Chem. 2014;289:30318-30332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 294. | Folgiero V, Avetrani P, Bon G, Di Carlo SE, Fabi A, Nisticò C, Vici P, Melucci E, Buglioni S, Perracchio L. Induction of ErbB-3 expression by alpha6beta4 integrin contributes to tamoxifen resistance in ERbeta1-negative breast carcinomas. PLoS One. 2008;3:e1592. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 295. | Sugiyama H, Mizutani K, Kurita S, Okimoto N, Shimono Y, Takai Y. Interaction of Necl-4/CADM4 with ErbB3 and integrin α6 β4 and inhibition of ErbB2/ErbB3 signaling and hemidesmosome disassembly. Genes Cells. 2013;18:519-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 296. | Deng X, Li Q, Hoff J, Novak M, Yang H, Jin H, Erfani SF, Sharma C, Zhou P, Rabinovitz I. Integrin-associated CD151 drives ErbB2-evoked mammary tumor onset and metastasis. Neoplasia. 2012;14:678-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 69] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 297. | Lipscomb EA, Simpson KJ, Lyle SR, Ring JE, Dugan AS, Mercurio AM. The alpha6beta4 integrin maintains the survival of human breast carcinoma cells in vivo. Cancer Res. 2005;65:10970-10976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 74] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 298. | Faure E, Garrouste F, Parat F, Monferran S, Leloup L, Pommier G, Kovacic H, Lehmann M. P2Y2 receptor inhibits EGF-induced MAPK pathway to stabilise keratinocyte hemidesmosomes. J Cell Sci. 2012;125:4264-4277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 299. | Bhatia V, Mula RV, Weigel NL, Falzon M. Parathyroid hormone-related protein regulates cell survival pathways via integrin alpha6beta4-mediated activation of phosphatidylinositol 3-kinase/Akt signaling. Mol Cancer Res. 2009;7:1119-1131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 300. | Mercurio AM, Bachelder RE, Bates RC, Chung J. Autocrine signaling in carcinoma: VEGF and the alpha6beta4 integrin. Semin Cancer Biol. 2004;14:115-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 54] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 301. | Serini G, Valdembri D, Bussolino F. Integrins and angiogenesis: a sticky business. Exp Cell Res. 2006;312:651-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 151] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 302. | Chen M, Sinha M, Luxon BA, Bresnick AR, O’Connor KL. Integrin alpha6beta4 controls the expression of genes associated with cell motility, invasion, and metastasis, including S100A4/metastasin. J Biol Chem. 2009;284:1484-1494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 137] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 303. | Soung YH, Gil HJ, Clifford JL, Chung J. Role of α6β4 integrin in cell motility, invasion and metastasis of mammary tumors. Curr Protein Pept Sci. 2011;12:23-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 304. | Vieira AF, Ribeiro AS, Dionísio MR, Sousa B, Nobre AR, Albergaria A, Santiago-Gómez A, Mendes N, Gerhard R, Schmitt F. P-cadherin signals through the laminin receptor α6β4 integrin to induce stem cell and invasive properties in basal-like breast cancer cells. Oncotarget. 2014;5:679-692. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 305. | Wicha MS. B4 androgen ablation: attacking the prostate cancer stem cell. J Clin Invest. 2013;123:563-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 306. | Yin Y, Deng X, Liu Z, Baldwin LA, Lefringhouse J, Zhang J, Hoff JT, Erfani SF, Rucker EB, O’Connor K. CD151 represses mammary gland development by maintaining the niches of progenitor cells. Cell Cycle. 2014;13:2707-2722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 307. | Ramsey DM, McAlpine SR. Halting metastasis through CXCR4 inhibition. Bioorg Med Chem Lett. 2013;23:20-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 308. | Hermann PC, Huber SL, Herrler T, Aicher A, Ellwart JW, Guba M, Bruns CJ, Heeschen C. Distinct populations of cancer stem cells determine tumor growth and metastatic activity in human pancreatic cancer. Cell Stem Cell. 2007;1:313-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1987] [Cited by in RCA: 2163] [Article Influence: 113.8] [Reference Citation Analysis (0)] |
| 309. | Du H, Bennett D, Li L, Whitlock G, Guo Y, Collins R, Chen J, Bian Z, Hong LS, Feng S. Physical activity and sedentary leisure time and their associations with BMI, waist circumference, and percentage body fat in 0.5 million adults: the China Kadoorie Biobank study. Am J Clin Nutr. 2013;97:487-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 217] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 310. | Bertolini G, D’Amico L, Moro M, Landoni E, Perego P, Miceli R, Gatti L, Andriani F, Wong D, Caserini R. Microenvironment-Modulated Metastatic CD133+/CXCR4+/EpCAM- Lung Cancer-Initiating Cells Sustain Tumor Dissemination and Correlate with Poor Prognosis. Cancer Res. 2015;75:3636-3649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 86] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 311. | Nagasawa T. CXC chemokine ligand 12 (CXCL12) and its receptor CXCR4. J Mol Med (Berl). 2014;92:433-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 135] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 312. | Trautmann F, Cojoc M, Kurth I, Melin N, Bouchez LC, Dubrovska A, Peitzsch C. CXCR4 as biomarker for radioresistant cancer stem cells. Int J Radiat Biol. 2014;90:687-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 69] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 313. | Chatterjee S, Behnam Azad B, Nimmagadda S. The intricate role of CXCR4 in cancer. Adv Cancer Res. 2014;124:31-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 325] [Cited by in RCA: 516] [Article Influence: 46.9] [Reference Citation Analysis (0)] |
| 314. | Shi J, Wei Y, Xia J, Wang S, Wu J, Chen F, Huang G, Chen J. CXCL12-CXCR4 contributes to the implication of bone marrow in cancer metastasis. Future Oncol. 2014;10:749-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 315. | Maréchal R, Demetter P, Nagy N, Berton A, Decaestecker C, Polus M, Closset J, Devière J, Salmon I, Van Laethem JL. High expression of CXCR4 may predict poor survival in resected pancreatic adenocarcinoma. Br J Cancer. 2009;100:1444-1451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 124] [Cited by in RCA: 145] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 316. | Bachet JB, Maréchal R, Demetter P, Bonnetain F, Couvelard A, Svrcek M, Bardier-Dupas A, Hammel P, Sauvanet A, Louvet C. Contribution of CXCR4 and SMAD4 in predicting disease progression pattern and benefit from adjuvant chemotherapy in resected pancreatic adenocarcinoma. Ann Oncol. 2012;23:2327-2335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 317. | Chinni SR, Yamamoto H, Dong Z, Sabbota A, Bonfil RD, Cher ML. CXCL12/CXCR4 transactivates HER2 in lipid rafts of prostate cancer cells and promotes growth of metastatic deposits in bone. Mol Cancer Res. 2008;6:446-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 115] [Reference Citation Analysis (0)] |
| 318. | Ho TK, Shiwen X, Abraham D, Tsui J, Baker D. Stromal-Cell-Derived Factor-1 (SDF-1)/CXCL12 as Potential Target of Therapeutic Angiogenesis in Critical Leg Ischaemia. Cardiol Res Pract. 2012;2012:143209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 319. | Arjonen A, Kaukonen R, Ivaska J. Filopodia and adhesion in cancer cell motility. Cell Adh Migr. 2011;5:421-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 205] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 320. | Liao Y, Hung MC. Physiological regulation of Akt activity and stability. Am J Transl Res. 2010;2:19-42. [PubMed] |
| 321. | Mo W, Chen J, Patel A, Zhang L, Chau V, Li Y, Cho W, Lim K, Xu J, Lazar AJ. CXCR4/CXCL12 mediate autocrine cell- cycle progression in NF1-associated malignant peripheral nerve sheath tumors. Cell. 2013;152:1077-1090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 130] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 322. | Zoughlami Y, Voermans C, Brussen K, van Dort KA, Kootstra NA, Maussang D, Smit MJ, Hordijk PL, van Hennik PB. Regulation of CXCR4 conformation by the small GTPase Rac1: implications for HIV infection. Blood. 2012;119:2024-2032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 323. | Drury LJ, Ziarek JJ, Gravel S, Veldkamp CT, Takekoshi T, Hwang ST, Heveker N, Volkman BF, Dwinell MB. Monomeric and dimeric CXCL12 inhibit metastasis through distinct CXCR4 interactions and signaling pathways. Proc Natl Acad Sci USA. 2011;108:17655-17660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 182] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 324. | Sotillos S, Díaz-Meco MT, Moscat J, Castelli-Gair Hombría J. Polarized subcellular localization of Jak/STAT components is required for efficient signaling. Curr Biol. 2008;18:624-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 325. | Bao W, Fu HJ, Xie QS, Wang L, Zhang R, Guo ZY, Zhao J, Meng YL, Ren XL, Wang T. HER2 interacts with CD44 to up-regulate CXCR4 via epigenetic silencing of microRNA-139 in gastric cancer cells. Gastroenterology. 2011;141:2076-2087.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 131] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 326. | Arnaud MP, Vallée A, Robert G, Bonneau J, Leroy C, Varin-Blank N, Rio AG, Troadec MB, Galibert MD, Gandemer V. CD9, a key actor in the dissemination of lymphoblastic leukemia, modulating CXCR4-mediated migration via RAC1 signaling. Blood. 2015;126:1802-1812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 327. | Desterke C, Martinaud C, Guerton B, Pieri L, Bogani C, Clay D, Torossian F, Lataillade JJ, Hasselbach HC, Gisslinger H. Tetraspanin CD9 participates in dysmegakaryopoiesis and stromal interactions in primary myelofibrosis. Haematologica. 2015;100:757-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 328. | Zhang Y, Foudi A, Geay JF, Berthebaud M, Buet D, Jarrier P, Jalil A, Vainchenker W, Louache F. Intracellular localization and constitutive endocytosis of CXCR4 in human CD34+ hematopoietic progenitor cells. Stem Cells. 2004;22:1015-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 91] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 329. | Wang X, Ding X, Nan L, Wang Y, Wang J, Yan Z, Zhang W, Sun J, Zhu W, Ni B. Investigation of the roles of exosomes in colorectal cancer liver metastasis. Oncol Rep. 2015;33:2445-2453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 79] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 330. | Munz M, Baeuerle PA, Gires O. The emerging role of EpCAM in cancer and stem cell signaling. Cancer Res. 2009;69:5627-5629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 375] [Cited by in RCA: 424] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 331. | Marhaba R, Klingbeil P, Nuebel T, Nazarenko I, Buechler MW, Zoeller M. CD44 and EpCAM: cancer-initiating cell markers. Curr Mol Med. 2008;8:784-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 139] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 332. | Keysar SB, Jimeno A. More than markers: biological significance of cancer stem cell-defining molecules. Mol Cancer Ther. 2010;9:2450-2457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 161] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 333. | Patriarca C, Macchi RM, Marschner AK, Mellstedt H. Epithelial cell adhesion molecule expression (CD326) in cancer: a short review. Cancer Treat Rev. 2012;38:68-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 352] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 334. | Gires O. Lessons from common markers of tumor-initiating cells in solid cancers. Cell Mol Life Sci. 2011;68:4009-4022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 335. | Imrich S, Hachmeister M, Gires O. EpCAM and its potential role in tumor-initiating cells. Cell Adh Migr. 2012;6:30-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 152] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 336. | Dollé L, Theise ND, Schmelzer E, Boulter L, Gires O, van Grunsven LA. EpCAM and the biology of hepatic stem/progenitor cells. Am J Physiol Gastrointest Liver Physiol. 2015;308:G233-G250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 96] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 337. | Le Naour F, Zoller M. The tumor antigen EpCAM: tetraspanins and the tight junction protein claudin-7, new partners, new functions. Front Biosci. 2008;13:5847-5865. [PubMed] |
| 338. | Ladwein M, Pape UF, Schmidt DS, Schnölzer M, Fiedler S, Langbein L, Franke WW, Moldenhauer G, Zöller M. The cell-cell adhesion molecule EpCAM interacts directly with the tight junction protein claudin-7. Exp Cell Res. 2005;309:345-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 132] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 339. | Wu CJ, Mannan P, Lu M, Udey MC. Epithelial cell adhesion molecule (EpCAM) regulates claudin dynamics and tight junctions. J Biol Chem. 2013;288:12253-12268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 108] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 340. | Okada T, Nakamura T, Watanabe T, Onoda N, Ashida A, Okuyama R, Ito K. Coexpression of EpCAM, CD44 variant isoforms and claudin-7 in anaplastic thyroid carcinoma. PLoS One. 2014;9:e94487. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 341. | Thuma F, Zöller M. EpCAM-associated claudin-7 supports lymphatic spread and drug resistance in rat pancreatic cancer. Int J Cancer. 2013;133:855-866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 342. | Balzar M, Briaire-de Bruijn IH, Rees-Bakker HA, Prins FA, Helfrich W, de Leij L, Riethmüller G, Alberti S, Warnaar SO, Fleuren GJ. Epidermal growth factor-like repeats mediate lateral and reciprocal interactions of Ep-CAM molecules in homophilic adhesions. Mol Cell Biol. 2001;21:2570-2580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 146] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 343. | Winter MJ, Nagelkerken B, Mertens AE, Rees-Bakker HA, Briaire-de Bruijn IH, Litvinov SV. Expression of Ep-CAM shifts the state of cadherin-mediated adhesions from strong to weak. Exp Cell Res. 2003;285:50-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 110] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 344. | Yamashita T, Budhu A, Forgues M, Wang XW. Activation of hepatic stem cell marker EpCAM by Wnt-beta-catenin signaling in hepatocellular carcinoma. Cancer Res. 2007;67:10831-10839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 368] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 345. | Lu H, Ma J, Yang Y, Shi W, Luo L. EpCAM is an endoderm-specific Wnt derepressor that licenses hepatic development. Dev Cell. 2013;24:543-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 130] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 346. | Maghzal N, Vogt E, Reintsch W, Fraser JS, Fagotto F. The tumor-associated EpCAM regulates morphogenetic movements through intracellular signaling. J Cell Biol. 2010;191:645-659. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 55] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 347. | Denzel S, Mack B, Eggert C, Massoner P, Stöcklein N, Kemming D, Harréus U, Gires O. MMP7 is a target of the tumour-associated antigen EpCAM. Int J Exp Pathol. 2012;93:341-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 348. | Sankpal NV, Willman MW, Fleming TP, Mayfield JD, Gillanders WE. Transcriptional repression of epithelial cell adhesion molecule contributes to p53 control of breast cancer invasion. Cancer Res. 2009;69:753-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 75] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 349. | Maetzel D, Denzel S, Mack B, Canis M, Went P, Benk M, Kieu C, Papior P, Baeuerle PA, Munz M. Nuclear signalling by tumour-associated antigen EpCAM. Nat Cell Biol. 2009;11:162-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 490] [Cited by in RCA: 557] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 350. | Lin CW, Liao MY, Lin WW, Wang YP, Lu TY, Wu HC. Epithelial cell adhesion molecule regulates tumor initiation and tumorigenesis via activating reprogramming factors and epithelial-mesenchymal transition gene expression in colon cancer. J Biol Chem. 2012;287:39449-39459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 92] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 351. | Yovchev MI, Grozdanov PN, Zhou H, Racherla H, Guha C, Dabeva MD. Identification of adult hepatic progenitor cells capable of repopulating injured rat liver. Hepatology. 2008;47:636-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 196] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 352. | Lei Z, Maeda T, Tamura A, Nakamura T, Yamazaki Y, Shiratori H, Yashiro K, Tsukita S, Hamada H. EpCAM contributes to formation of functional tight junction in the intestinal epithelium by recruiting claudin proteins. Dev Biol. 2012;371:136-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 120] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 353. | Schneeberger EE, Lynch RD. The tight junction: a multifunctional complex. Am J Physiol Cell Physiol. 2004;286:C1213-C1228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1008] [Cited by in RCA: 1050] [Article Influence: 47.7] [Reference Citation Analysis (0)] |
| 354. | Lal-Nag M, Morin PJ. The claudins. Genome Biol. 2009;10:235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 225] [Cited by in RCA: 278] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 355. | Krug SM, Schulzke JD, Fromm M. Tight junction, selective permeability, and related diseases. Semin Cell Dev Biol. 2014;36:166-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 238] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 356. | Ding L, Lu Z, Foreman O, Tatum R, Lu Q, Renegar R, Cao J, Chen YH. Inflammation and disruption of the mucosal architecture in claudin-7-deficient mice. Gastroenterology. 2012;142:305-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 180] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 357. | Tanaka H, Takechi M, Kiyonari H, Shioi G, Tamura A, Tsukita S. Intestinal deletion of Claudin-7 enhances paracellular organic solute flux and initiates colonic inflammation in mice. Gut. 2015;64:1529-1538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 147] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 358. | Van Itallie CM, Anderson JM. Claudin interactions in and out of the tight junction. Tissue Barriers. 2013;1:e25247. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 121] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 359. | Findley MK, Koval M. Regulation and roles for claudin-family tight junction proteins. IUBMB Life. 2009;61:431-437. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 161] [Cited by in RCA: 166] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 360. | Gonzalez-Mariscal L, Namorado Mdel C, Martin D, Sierra G, Reyes JL. The tight junction proteins claudin-7 and -8 display a different subcellular localization at Henle’s loops and collecting ducts of rabbit kidney. Nephrol Dial Transplant. 2006;21:2391-2398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 361. | Tauro BJ, Greening DW, Mathias RA, Mathivanan S, Ji H, Simpson RJ. Two distinct populations of exosomes are released from LIM1863 colon carcinoma cell-derived organoids. Mol Cell Proteomics. 2013;12:587-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 332] [Cited by in RCA: 362] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 362. | Lu Z, Kim do H, Fan J, Lu Q, Verbanac K, Ding L, Renegar R, Chen YH. A non-tight junction function of claudin-7-Interaction with integrin signaling in suppressing lung cancer cell proliferation and detachment. Mol Cancer. 2015;14:120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 70] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 363. | D’Souza T, Agarwal R, Morin PJ. Phosphorylation of claudin-3 at threonine 192 by cAMP-dependent protein kinase regulates tight junction barrier function in ovarian cancer cells. J Biol Chem. 2005;280:26233-26240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 171] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 364. | French AD, Fiori JL, Camilli TC, Leotlela PD, O’Connell MP, Frank BP, Subaran S, Indig FE, Taub DD, Weeraratna AT. PKC and PKA phosphorylation affect the subcellular localization of claudin-1 in melanoma cells. Int J Med Sci. 2009;6:93-101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 95] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 365. | Chen C, Wang P, Su Q, Wang S, Wang F. Myosin light chain kinase mediates intestinal barrier disruption following burn injury. PLoS One. 2012;7:e34946. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 366. | Nishida M, Yoshida M, Nishiumi S, Furuse M, Azuma T. Claudin-2 regulates colorectal inflammation via myosin light chain kinase-dependent signaling. Dig Dis Sci. 2013;58:1546-1559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 367. | Ikari A, Ito M, Okude C, Sawada H, Harada H, Degawa M, Sakai H, Takahashi T, Sugatani J, Miwa M. Claudin-16 is directly phosphorylated by protein kinase A independently of a vasodilator-stimulated phosphoprotein-mediated pathway. J Cell Physiol. 2008;214:221-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 368. | Li X, Akhtar S, Choudhry MA. Alteration in intestine tight junction protein phosphorylation and apoptosis is associated with increase in IL-18 levels following alcohol intoxication and burn injury. Biochim Biophys Acta. 2012;1822:196-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 73] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 369. | Shen L. Tight junctions on the move: molecular mechanisms for epithelial barrier regulation. Ann N Y Acad Sci. 2012;1258:9-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 160] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 370. | Sjö A, Magnusson KE, Peterson KH. Protein kinase C activation has distinct effects on the localization, phosphorylation and detergent solubility of the claudin protein family in tight and leaky epithelial cells. J Membr Biol. 2010;236:181-189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 371. | Heiler S, Mu W, Zöller M, Thuma F. The importance of claudin-7 palmitoylation on membrane subdomain localization and metastasis-promoting activities. Cell Commun Signal. 2015;13:29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 372. | Nübel T, Preobraschenski J, Tuncay H, Weiss T, Kuhn S, Ladwein M, Langbein L, Zöller M. Claudin-7 regulates EpCAM-mediated functions in tumor progression. Mol Cancer Res. 2009;7:285-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 100] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 373. | Levental I, Grzybek M, Simons K. Greasing their way: lipid modifications determine protein association with membrane rafts. Biochemistry. 2010;49:6305-6316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 324] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 374. | Stepanek O, Draber P, Horejsi V. Palmitoylated transmembrane adaptor proteins in leukocyte signaling. Cell Signal. 2014;26:895-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 375. | Head BP, Patel HH, Insel PA. Interaction of membrane/lipid rafts with the cytoskeleton: impact on signaling and function: membrane/lipid rafts, mediators of cytoskeletal arrangement and cell signaling. Biochim Biophys Acta. 2014;1838:532-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 343] [Cited by in RCA: 413] [Article Influence: 31.8] [Reference Citation Analysis (10)] |
| 376. | Mollinedo F, Gajate C. Lipid rafts as major platforms for signaling regulation in cancer. Adv Biol Regul. 2015;57:130-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 247] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 377. | Thiel KW, Carpenter G. ErbB-4 and TNF-alpha converting enzyme localization to membrane microdomains. Biochem Biophys Res Commun. 2006;350:629-633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 378. | Vetrivel KS, Cheng H, Kim SH, Chen Y, Barnes NY, Parent AT, Sisodia SS, Thinakaran G. Spatial segregation of gamma-secretase and substrates in distinct membrane domains. J Biol Chem. 2005;280:25892-25900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 180] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 379. | Cheng JM, Volk L, Janaki DK, Vyakaranam S, Ran S, Rao KA. Tumor suppressor function of Rab25 in triple-negative breast cancer. Int J Cancer. 2010;126:2799-2812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 380. | Nicolson GL. Cell membrane fluid-mosaic structure and cancer metastasis. Cancer Res. 2015;75:1169-1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 381. | Ren F, Sheng WQ, Du X. CD133: a cancer stem cells marker, is used in colorectal cancers. World J Gastroenterol. 2013;19:2603-2611. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 106] [Cited by in RCA: 135] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 382. | Grosse-Gehling P, Fargeas CA, Dittfeld C, Garbe Y, Alison MR, Corbeil D, Kunz-Schughart LA. CD133 as a biomarker for putative cancer stem cells in solid tumours: limitations, problems and challenges. J Pathol. 2013;229:355-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 220] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 383. | Yiming L, Yunshan G, Bo M, Yu Z, Tao W, Gengfang L, Dexian F, Shiqian C, Jianli J, Juan T. CD133 overexpression correlates with clinicopathological features of gastric cancer patients and its impact on survival: a systematic review and meta-analysis. Oncotarget. 2015;6:42019-42027. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 384. | Wu Y, Wu PY. CD133 as a marker for cancer stem cells: progresses and concerns. Stem Cells Dev. 2009;18:1127-1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 231] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 385. | Li X, Zhao H, Gu J, Zheng L. Prognostic value of cancer stem cell marker CD133 expression in pancreatic ductal adenocarcinoma (PDAC): a systematic review and meta-analysis. Int J Clin Exp Pathol. 2015;8:12084-12092. [PubMed] |
| 386. | Xu L. Cancer stem cell in the progression and therapy of pancreatic cancer. Front Biosci (Landmark Ed). 2013;18:795-802. [PubMed] |
| 387. | Zhu H, Wang D, Zhang L, Xie X, Wu Y, Liu Y, Shao G, Su Z. Upregulation of autophagy by hypoxia-inducible factor-1α promotes EMT and metastatic ability of CD133+ pancreatic cancer stem-like cells during intermittent hypoxia. Oncol Rep. 2014;32:935-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 108] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 388. | Hou YC, Chao YJ, Tung HL, Wang HC, Shan YS. Coexpression of CD44-positive/CD133-positive cancer stem cells and CD204-positive tumor-associated macrophages is a predictor of survival in pancreatic ductal adenocarcinoma. Cancer. 2014;120:2766-2777. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 84] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 389. | Banerjee S, Nomura A, Sangwan V, Chugh R, Dudeja V, Vickers SM, Saluja A. CD133+ tumor initiating cells in a syngenic murine model of pancreatic cancer respond to Minnelide. Clin Cancer Res. 2014;20:2388-2399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 390. | Olempska M, Eisenach PA, Ammerpohl O, Ungefroren H, Fandrich F, Kalthoff H. Detection of tumor stem cell markers in pancreatic carcinoma cell lines. Hepatobiliary Pancreat Dis Int. 2007;6:92-97. [PubMed] |
| 391. | Yin AH, Miraglia S, Zanjani ED, Almeida-Porada G, Ogawa M, Leary AG, Olweus J, Kearney J, Buck DW. AC133, a novel marker for human hematopoietic stem and progenitor cells. Blood. 1997;90:5002-5012. [PubMed] |
| 392. | Weigmann A, Corbeil D, Hellwig A, Huttner WB. Prominin, a novel microvilli-specific polytopic membrane protein of the apical surface of epithelial cells, is targeted to plasmalemmal protrusions of non-epithelial cells. Proc Natl Acad Sci USA. 1997;94:12425-12430. [PubMed] |
| 393. | Liu J, Mao Z, Huang J, Xie S, Liu T, Mao Z. Blocking the NOTCH pathway can inhibit the growth of CD133-positive A549 cells and sensitize to chemotherapy. Biochem Biophys Res Commun. 2014;444:670-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 394. | Liu YP, Yang CJ, Huang MS, Yeh CT, Wu AT, Lee YC, Lai TC, Lee CH, Hsiao YW, Lu J. Cisplatin selects for multidrug-resistant CD133+ cells in lung adenocarcinoma by activating Notch signaling. Cancer Res. 2013;73:406-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 176] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 395. | Jeng KS, Sheen IS, Jeng WJ, Yu MC, Hsiau HI, Chang FY, Tsai HH. Activation of the sonic hedgehog signaling pathway occurs in the CD133 positive cells of mouse liver cancer Hepa 1-6 cells. Onco Targets Ther. 2013;6:1047-1055. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 396. | Ma S. Biology and clinical implications of CD133(+) liver cancer stem cells. Exp Cell Res. 2013;319:126-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 77] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 397. | Fargeas CA, Karbanová J, Jászai J, Corbeil D. CD133 and membrane microdomains: old facets for future hypotheses. World J Gastroenterol. 2011;17:4149-4152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 398. | Jiang W, Zhang Y, Kane KT, Collins MA, Simeone DM, di Magliano MP, Nguyen KT. CD44 regulates pancreatic cancer invasion through MT1-MMP. Mol Cancer Res. 2015;13:9-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 399. | Preca BT, Bajdak K, Mock K, Sundararajan V, Pfannstiel J, Maurer J, Wellner U, Hopt UT, Brummer T, Brabletz S. A self-enforcing CD44s/ZEB1 feedback loop maintains EMT and stemness properties in cancer cells. Int J Cancer. 2015;137:2566-2577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 150] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 400. | Chanmee T, Ontong P, Mochizuki N, Kongtawelert P, Konno K, Itano N. Excessive hyaluronan production promotes acquisition of cancer stem cell signatures through the coordinated regulation of Twist and the transforming growth factor β (TGF-β)-Snail signaling axis. J Biol Chem. 2014;289:26038-26056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 81] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 401. | Chung SS, Aroh C, Vadgama JV. Constitutive activation of STAT3 signaling regulates hTERT and promotes stem cell-like traits in human breast cancer cells. PLoS One. 2013;8:e83971. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 90] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 402. | Bao B, Wang Z, Ali S, Kong D, Li Y, Ahmad A, Banerjee S, Azmi AS, Miele L, Sarkar FH. Notch-1 induces epithelial-mesenchymal transition consistent with cancer stem cell phenotype in pancreatic cancer cells. Cancer Lett. 2011;307:26-36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 227] [Cited by in RCA: 239] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 403. | De Falco V, Tamburrino A, Ventre S, Castellone MD, Malek M, Manié SN, Santoro M. CD44 proteolysis increases CREB phosphorylation and sustains proliferation of thyroid cancer cells. Cancer Res. 2012;72:1449-1458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 404. | Lee D, Na J, Ryu J, Kim HJ, Nam SH, Kang M, Jung JW, Lee MS, Song HE, Choi J. Interaction of tetraspan(in) TM4SF5 with CD44 promotes self-renewal and circulating capacities of hepatocarcinoma cells. Hepatology. 2015;61:1978-1997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 405. | Ju SY, Chiou SH, Su Y. Maintenance of the stemness in CD44(+) HCT-15 and HCT-116 human colon cancer cells requires miR-203 suppression. Stem Cell Res. 2014;12:86-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 80] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 406. | Su YJ, Lai HM, Chang YW, Chen GY, Lee JL. Direct reprogramming of stem cell properties in colon cancer cells by CD44. EMBO J. 2011;30:3186-3199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 151] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 407. | Kang M, Choi S, Jeong SJ, Lee SA, Kwak TK, Kim H, Jung O, Lee MS, Ko Y, Ryu J. Cross-talk between TGFβ1 and EGFR signalling pathways induces TM4SF5 expression and epithelial-mesenchymal transition. Biochem J. 2012;443:691-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 408. | Lee SA, Lee SY, Cho IH, Oh MA, Kang ES, Kim YB, Seo WD, Choi S, Nam JO, Tamamori-Adachi M. Tetraspanin TM4SF5 mediates loss of contact inhibition through epithelial-mesenchymal transition in human hepatocarcinoma. J Clin Invest. 2008;118:1354-1366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 102] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 409. | Lee KH, Ahn EJ, Oh SJ, Kim O, Joo YE, Bae JA, Yoon S, Ryu HH, Jung S, Kim KK. KITENIN promotes glioma invasiveness and progression, associated with the induction of EMT and stemness markers. Oncotarget. 2015;6:3240-3253. [PubMed] |
| 410. | D’Angelo RC, Liu XW, Najy AJ, Jung YS, Won J, Chai KX, Fridman R, Kim HR. TIMP-1 via TWIST1 induces EMT phenotypes in human breast epithelial cells. Mol Cancer Res. 2014;12:1324-1333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 411. | Baldwin LA, Hoff JT, Lefringhouse J, Zhang M, Jia C, Liu Z, Erfani S, Jin H, Xu M, She QB. CD151-α3β1 integrin complexes suppress ovarian tumor growth by repressing slug-mediated EMT and canonical Wnt signaling. Oncotarget. 2014;5:12203-12217. [PubMed] |
| 412. | Lupia A, Peppicelli S, Witort E, Bianchini F, Carloni V, Pimpinelli N, Urso C, Borgognoni L, Capaccioli S, Calorini L. CD63 tetraspanin is a negative driver of epithelial-to-mesenchymal transition in human melanoma cells. J Invest Dermatol. 2014;134:2947-2956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 413. | Sobolik T, Su YJ, Wells S, Ayers GD, Cook RS, Richmond A. CXCR4 drives the metastatic phenotype in breast cancer through induction of CXCR2 and activation of MEK and PI3K pathways. Mol Biol Cell. 2014;25:566-582. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 414. | Jung YD, Shim JW, Park SJ, Choi SH, Yang K, Heo K, Park MT. Downregulation of UHRF1 promotes EMT via inducing CXCR4 in human cancer cells. Int J Oncol. 2015;46:1232-1242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 415. | Gao J, Yan Q, Wang J, Liu S, Yang X. Epithelial-to-mesenchymal transition induced by TGF-β1 is mediated by AP1-dependent EpCAM expression in MCF-7 cells. J Cell Physiol. 2015;230:775-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 51] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 416. | Massoner P, Thomm T, Mack B, Untergasser G, Martowicz A, Bobowski K, Klocker H, Gires O, Puhr M. EpCAM is overexpressed in local and metastatic prostate cancer, suppressed by chemotherapy and modulated by MET-associated miRNA-200c/205. Br J Cancer. 2014;111:955-964. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 90] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 417. | Bhat AA, Pope JL, Smith JJ, Ahmad R, Chen X, Washington MK, Beauchamp RD, Singh AB, Dhawan P. Claudin-7 expression induces mesenchymal to epithelial transformation (MET) to inhibit colon tumorigenesis. Oncogene. 2015;34:4570-4580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 71] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 418. | Nomura A, Banerjee S, Chugh R, Dudeja V, Yamamoto M, Vickers SM, Saluja AK. CD133 initiates tumors, induces epithelial-mesenchymal transition and increases metastasis in pancreatic cancer. Oncotarget. 2015;6:8313-8322. [PubMed] |
| 419. | Yu Z, Pestell TG, Lisanti MP, Pestell RG. Cancer stem cells. Int J Biochem Cell Biol. 2012;44:2144-2151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 396] [Cited by in RCA: 518] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 420. | Mimeault M, Batra SK. Molecular biomarkers of cancer stem/progenitor cells associated with progression, metastases, and treatment resistance of aggressive cancers. Cancer Epidemiol Biomarkers Prev. 2014;23:234-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 421. | Zaravinos A. The Regulatory Role of MicroRNAs in EMT and Cancer. J Oncol. 2015;2015:865816. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 190] [Cited by in RCA: 226] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 422. | Hu Y, Tang H. MicroRNAs regulate the epithelial to mesenchymal transition (EMT) in cancer progression. Microrna. 2014;3:108-117. [PubMed] |
| 423. | Bourguignon LY. Hyaluronan-CD44 interaction promotes microRNA signaling and RhoGTPase activation leading to tumor progression. Small GTPases. 2012;3:53-59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 424. | Bourguignon LY, Wong G, Earle C, Chen L. Hyaluronan-CD44v3 interaction with Oct4-Sox2-Nanog promotes miR-302 expression leading to self-renewal, clonal formation, and cisplatin resistance in cancer stem cells from head and neck squamous cell carcinoma. J Biol Chem. 2012;287:32800-32824. [PubMed] |
| 425. | Liu F, Kong X, Lv L, Gao J. TGF-β1 acts through miR-155 to down-regulate TP53INP1 in promoting epithelial-mesenchymal transition and cancer stem cell phenotypes. Cancer Lett. 2015;359:288-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 426. | Ahmad A, Maitah MY, Ginnebaugh KR, Li Y, Bao B, Gadgeel SM, Sarkar FH. Inhibition of Hedgehog signaling sensitizes NSCLC cells to standard therapies through modulation of EMT-regulating miRNAs. J Hematol Oncol. 2013;6:77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 125] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 427. | Shen WW, Zeng Z, Zhu WX, Fu GH. MiR-142-3p functions as a tumor suppressor by targeting CD133, ABCG2, and Lgr5 in colon cancer cells. J Mol Med (Berl). 2013;91:989-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 114] [Article Influence: 8.8] [Reference Citation Analysis (1)] |
| 428. | Ji Q, Hao X, Zhang M, Tang W, Yang M, Li L, Xiang D, Desano JT, Bommer GT, Fan D. MicroRNA miR-34 inhibits human pancreatic cancer tumor-initiating cells. PLoS One. 2009;4:e6816. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 532] [Cited by in RCA: 547] [Article Influence: 32.2] [Reference Citation Analysis (0)] |
| 429. | Liu C, Kelnar K, Liu B, Chen X, Calhoun-Davis T, Li H, Patrawala L, Yan H, Jeter C, Honorio S. The microRNA miR-34a inhibits prostate cancer stem cells and metastasis by directly repressing CD44. Nat Med. 2011;17:211-215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1145] [Cited by in RCA: 1139] [Article Influence: 75.9] [Reference Citation Analysis (0)] |
| 430. | Garofalo M, Romano G, Di Leva G, Nuovo G, Jeon YJ, Ngankeu A, Sun J, Lovat F, Alder H, Condorelli G. EGFR and MET receptor tyrosine kinase-altered microRNA expression induces tumorigenesis and gefitinib resistance in lung cancers. Nat Med. 2012;18:74-82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 300] [Cited by in RCA: 314] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 431. | Garnier D, Magnus N, Meehan B, Kislinger T, Rak J. Qualitative changes in the proteome of extracellular vesicles accompanying cancer cell transition to mesenchymal state. Exp Cell Res. 2013;319:2747-2757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 67] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 432. | Aga M, Bentz GL, Raffa S, Torrisi MR, Kondo S, Wakisaka N, Yoshizaki T, Pagano JS, Shackelford J. Exosomal HIF1α supports invasive potential of nasopharyngeal carcinoma-associated LMP1-positive exosomes. Oncogene. 2014;33:4613-4622. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 214] [Cited by in RCA: 284] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 433. | Mu W, Rana S, Zöller M. Host matrix modulation by tumor exosomes promotes motility and invasiveness. Neoplasia. 2013;15:875-887. [PubMed] |
| 434. | Purushothaman A, Bandari SK, Liu J, Mobley JA, Brown EE, Sanderson RD. Fibronectin on the Surface of Myeloma Cell-derived Exosomes Mediates Exosome-Cell Interactions. J Biol Chem. 2016;291:1652-1663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 249] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 435. | Sung BH, Ketova T, Hoshino D, Zijlstra A, Weaver AM. Directional cell movement through tissues is controlled by exosome secretion. Nat Commun. 2015;6:7164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 485] [Cited by in RCA: 477] [Article Influence: 43.4] [Reference Citation Analysis (0)] |
| 436. | Rieu S, Géminard C, Rabesandratana H, Sainte-Marie J, Vidal M. Exosomes released during reticulocyte maturation bind to fibronectin via integrin alpha4beta1. Eur J Biochem. 2000;267:583-590. [PubMed] |
| 437. | Clayton A, Turkes A, Dewitt S, Steadman R, Mason MD, Hallett MB. Adhesion and signaling by B cell-derived exosomes: the role of integrins. FASEB J. 2004;18:977-979. [PubMed] |
| 438. | Zech D, Rana S, Büchler MW, Zöller M. Tumor-exosomes and leukocyte activation: an ambivalent crosstalk. Cell Commun Signal. 2012;10:37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 128] [Cited by in RCA: 187] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 439. | Nolte-’t Hoen EN, Buschow SI, Anderton SM, Stoorvogel W, Wauben MH. Activated T cells recruit exosomes secreted by dendritic cells via LFA-1. Blood. 2009;113:1977-1981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 335] [Cited by in RCA: 341] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 440. | Hoshino A, Costa-Silva B, Shen TL, Rodrigues G, Hashimoto A, Tesic Mark M, Molina H, Kohsaka S, Di Giannatale A, Ceder S. Tumour exosome integrins determine organotropic metastasis. Nature. 2015;527:329-335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2697] [Cited by in RCA: 3960] [Article Influence: 360.0] [Reference Citation Analysis (0)] |
| 441. | Rana S, Zöller M. Exosome target cell selection and the importance of exosomal tetraspanins: a hypothesis. Biochem Soc Trans. 2011;39:559-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 186] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 442. | Van Gool SW, Vandenberghe P, de Boer M, Ceuppens JL. CD80, CD86 and CD40 provide accessory signals in a multiple-step T-cell activation model. Immunol Rev. 1996;153:47-83. [PubMed] |
| 443. | Matzku S, Komitowski D, Mildenberger M, Zöller M. Characterization of BSp73, a spontaneous rat tumor and its in vivo selected variants showing different metastasizing capacities. Invasion Metastasis. 1983;3:109-123. [PubMed] |
| 444. | Tian T, Wang Y, Wang H, Zhu Z, Xiao Z. Visualizing of the cellular uptake and intracellular trafficking of exosomes by live-cell microscopy. J Cell Biochem. 2010;111:488-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 370] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 445. | Mulcahy LA, Pink RC, Carter DR. Routes and mechanisms of extracellular vesicle uptake. J Extracell Vesicles. 2014;3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1298] [Cited by in RCA: 2139] [Article Influence: 178.3] [Reference Citation Analysis (0)] |
| 446. | Taylor MJ, Lampe M, Merrifield CJ. A feedback loop between dynamin and actin recruitment during clathrin-mediated endocytosis. PLoS Biol. 2012;10:e1001302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 111] [Cited by in RCA: 118] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 447. | Parton RG, Simons K. The multiple faces of caveolae. Nat Rev Mol Cell Biol. 2007;8:185-194. [PubMed] |
| 448. | Kerr MC, Teasdale RD. Defining macropinocytosis. Traffic. 2009;10:364-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 474] [Cited by in RCA: 531] [Article Influence: 31.2] [Reference Citation Analysis (0)] |
| 449. | Chernomordik LV, Kozlov MM. Mechanics of membrane fusion. Nat Struct Mol Biol. 2008;15:675-683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 876] [Cited by in RCA: 804] [Article Influence: 44.7] [Reference Citation Analysis (0)] |
| 450. | Ogorevc E, Kralj-Iglic V, Veranic P. The role of extracellular vesicles in phenotypic cancer transformation. Radiol Oncol. 2013;47:197-205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 71] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 451. | Belting M, Christianson HC. Role of exosomes and microvesicles in hypoxia-associated tumour development and cardiovascular disease. J Intern Med. 2015;278:251-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 452. | Aharon A, Brenner B. Microparticles, thrombosis and cancer. Best Pract Res Clin Haematol. 2009;22:61-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 84] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 453. | Rak J. Microparticles in cancer. Semin Thromb Hemost. 2010;36:888-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 219] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 454. | Ratajczak MZ, Kucia M, Jadczyk T, Greco NJ, Wojakowski W, Tendera M, Ratajczak J. Pivotal role of paracrine effects in stem cell therapies in regenerative medicine: can we translate stem cell-secreted paracrine factors and microvesicles into better therapeutic strategies? Leukemia. 2012;26:1166-1173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 265] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 455. | Chiarini F, Lonetti A, Evangelisti C, Buontempo F, Orsini E, Evangelisti C, Cappellini A, Neri LM, McCubrey JA, Martelli AM. Advances in understanding the acute lymphoblastic leukemia bone marrow microenvironment: From biology to therapeutic targeting. Biochim Biophys Acta. 2016;1863:449-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 106] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 456. | Filipazzi P, Bürdek M, Villa A, Rivoltini L, Huber V. Recent advances on the role of tumor exosomes in immunosuppression and disease progression. Semin Cancer Biol. 2012;22:342-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 236] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 457. | Kunigelis KE, Graner MW. The Dichotomy of Tumor Exosomes (TEX) in Cancer Immunity: Is It All in the ConTEXt? Vaccines (Basel). 2015;3:1019-1051. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 458. | Whiteside TL. Immune modulation of T-cell and NK (natural killer) cell activities by TEXs (tumour-derived exosomes). Biochem Soc Trans. 2013;41:245-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 323] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 459. | Greening DW, Gopal SK, Xu R, Simpson RJ, Chen W. Exosomes and their roles in immune regulation and cancer. Semin Cell Dev Biol. 2015;40:72-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 493] [Article Influence: 44.8] [Reference Citation Analysis (0)] |
| 460. | Bobrie A, Théry C. Exosomes and communication between tumours and the immune system: are all exosomes equal? Biochem Soc Trans. 2013;41:263-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 107] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 461. | Wieckowski E, Whiteside TL. Human tumor-derived vs dendritic cell-derived exosomes have distinct biologic roles and molecular profiles. Immunol Res. 2006;36:247-254. [PubMed] |
| 462. | Taylor DD, Gercel-Taylor C. Exosomes/microvesicles: mediators of cancer-associated immunosuppressive microenvironments. Semin Immunopathol. 2011;33:441-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 312] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 463. | Gehrmann U, Näslund TI, Hiltbrunner S, Larssen P, Gabrielsson S. Harnessing the exosome-induced immune response for cancer immunotherapy. Semin Cancer Biol. 2014;28:58-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 102] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 464. | Claas C, Seiter S, Claas A, Savelyeva L, Schwab M, Zöller M. Association between the rat homologue of CO-029, a metastasis-associated tetraspanin molecule and consumption coagulopathy. J Cell Biol. 1998;141:267-280. [PubMed] |
| 465. | Ribeiro MF, Zhu H, Millard RW, Fan GC. Exosomes Function in Pro- and Anti-Angiogenesis. Curr Angiogenes. 2013;2:54-59. [PubMed] |
| 466. | Finn NA, Searles CD. Intracellular and Extracellular miRNAs in Regulation of Angiogenesis Signaling. Curr Angiogenes. 2012;4:299-307. [PubMed] |
| 467. | Gai C, Carpanetto A, Deregibus MC, Camussi G. Extracellular vesicle-mediated modulation of angiogenesis. Histol Histopathol. 2016;31:379-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 468. | Janowska-Wieczorek A, Wysoczynski M, Kijowski J, Marquez-Curtis L, Machalinski B, Ratajczak J, Ratajczak MZ. Microvesicles derived from activated platelets induce metastasis and angiogenesis in lung cancer. Int J Cancer. 2005;113:752-760. [PubMed] |
| 469. | Shimoda M, Khokha R. Proteolytic factors in exosomes. Proteomics. 2013;13:1624-1636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 76] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 470. | Sevenich L, Joyce JA. Pericellular proteolysis in cancer. Genes Dev. 2014;28:2331-2347. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 131] [Cited by in RCA: 152] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 471. | Stoeck A, Keller S, Riedle S, Sanderson MP, Runz S, Le Naour F, Gutwein P, Ludwig A, Rubinstein E, Altevogt P. A role for exosomes in the constitutive and stimulus-induced ectodomain cleavage of L1 and CD44. Biochem J. 2006;393:609-618. [PubMed] |
| 472. | Nakamura H, Suenaga N, Taniwaki K, Matsuki H, Yonezawa K, Fujii M, Okada Y, Seiki M. Constitutive and induced CD44 shedding by ADAM-like proteases and membrane-type 1 matrix metalloproteinase. Cancer Res. 2004;64:876-882. [PubMed] |
| 473. | Chetty C, Vanamala SK, Gondi CS, Dinh DH, Gujrati M, Rao JS. MMP-9 induces CD44 cleavage and CD44 mediated cell migration in glioblastoma xenograft cells. Cell Signal. 2012;24:549-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 106] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 474. | Tsaktanis T, Kremling H, Pavšič M, von Stackelberg R, Mack B, Fukumori A, Steiner H, Vielmuth F, Spindler V, Huang Z. Cleavage and cell adhesion properties of human epithelial cell adhesion molecule (HEPCAM). J Biol Chem. 2015;290:24574-24591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 475. | Lokeshwar VB, Mirza S, Jordan A. Targeting hyaluronic acid family for cancer chemoprevention and therapy. Adv Cancer Res. 2014;123:35-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 117] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 476. | Rilla K, Siiskonen H, Tammi M, Tammi R. Hyaluronan-coated extracellular vesicles--a novel link between hyaluronan and cancer. Adv Cancer Res. 2014;123:121-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 71] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 477. | Seiki M. Membrane-type 1 matrix metalloproteinase: a key enzyme for tumor invasion. Cancer Lett. 2003;194:1-11. [PubMed] |
| 478. | Bauvois B. New facets of matrix metalloproteinases MMP-2 and MMP-9 as cell surface transducers: outside-in signaling and relationship to tumor progression. Biochim Biophys Acta. 2012;1825:29-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 260] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 479. | Ramteke A, Ting H, Agarwal C, Mateen S, Somasagara R, Hussain A, Graner M, Frederick B, Agarwal R, Deep G. Exosomes secreted under hypoxia enhance invasiveness and stemness of prostate cancer cells by targeting adherens junction molecules. Mol Carcinog. 2015;54:554-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 324] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 480. | Tauro BJ, Mathias RA, Greening DW, Gopal SK, Ji H, Kapp EA, Coleman BM, Hill AF, Kusebauch U, Hallows JL. Oncogenic H-ras reprograms Madin-Darby canine kidney (MDCK) cell-derived exosomal proteins following epithelial-mesenchymal transition. Mol Cell Proteomics. 2013;12:2148-2159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 162] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 481. | Mazurov D, Barbashova L, Filatov A. Tetraspanin protein CD9 interacts with metalloprotease CD10 and enhances its release via exosomes. FEBS J. 2013;280:1200-1213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 89] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 482. | Liu T, Mendes DE, Berkman CE. Functional prostate-specific membrane antigen is enriched in exosomes from prostate cancer cells. Int J Oncol. 2014;44:918-922. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 70] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 483. | Hakulinen J, Sankkila L, Sugiyama N, Lehti K, Keski-Oja J. Secretion of active membrane type 1 matrix metalloproteinase (MMP-14) into extracellular space in microvesicular exosomes. J Cell Biochem. 2008;105:1211-1218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 236] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 484. | Hendrix A, Westbroek W, Bracke M, De Wever O. An ex(o)citing machinery for invasive tumor growth. Cancer Res. 2010;70:9533-9537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 82] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 485. | Hood JL, San RS, Wickline SA. Exosomes released by melanoma cells prepare sentinel lymph nodes for tumor metastasis. Cancer Res. 2011;71:3792-3801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 719] [Cited by in RCA: 798] [Article Influence: 53.2] [Reference Citation Analysis (0)] |
| 486. | Peinado H, Alečković M, Lavotshkin S, Matei I, Costa-Silva B, Moreno-Bueno G, Hergueta-Redondo M, Williams C, García-Santos G, Ghajar C. Melanoma exosomes educate bone marrow progenitor cells toward a pro-metastatic phenotype through MET. Nat Med. 2012;18:883-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2866] [Cited by in RCA: 3003] [Article Influence: 214.5] [Reference Citation Analysis (0)] |
| 487. | Webber J, Yeung V, Clayton A. Extracellular vesicles as modulators of the cancer microenvironment. Semin Cell Dev Biol. 2015;40:27-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 128] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 488. | Altevogt P, Bretz NP, Ridinger J, Utikal J, Umansky V. Novel insights into exosome-induced, tumor-associated inflammation and immunomodulation. Semin Cancer Biol. 2014;28:51-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 489. | Whitehead B, Wu L, Hvam ML, Aslan H, Dong M, Dyrskjøt L, Ostenfeld MS, Moghimi SM, Howard KA. Tumour exosomes display differential mechanical and complement activation properties dependent on malignant state: implications in endothelial leakiness. J Extracell Vesicles. 2015;4:29685. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 84] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 490. | Fontana S, Saieva L, Taverna S, Alessandro R. Contribution of proteomics to understanding the role of tumor-derived exosomes in cancer progression: state of the art and new perspectives. Proteomics. 2013;13:1581-1594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 76] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 491. | Brandt DT, Xu J, Steinbeisser H, Grosse R. Regulation of myocardin-related transcriptional coactivators through cofactor interactions in differentiation and cancer. Cell Cycle. 2009;8:2523-2527. [PubMed] |
| 492. | Lee NP, Poon RT, Shek FH, Ng IO, Luk JM. Role of cadherin-17 in oncogenesis and potential therapeutic implications in hepatocellular carcinoma. Biochim Biophys Acta. 2010;1806:138-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 493. | Mathew SJ, Haubert D, Krönke M, Leptin M. Looking beyond death: a morphogenetic role for the TNF signalling pathway. J Cell Sci. 2009;122:1939-1946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 65] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 494. | Liu QS, Zhang J, Liu M, Dong WG. Lentiviral-mediated miRNA against liver-intestine cadherin suppresses tumor growth and invasiveness of human gastric cancer. Cancer Sci. 2010;101:1807-1812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 495. | Pang W, Su J, Wang Y, Feng H, Dai X, Yuan Y, Chen X, Yao W. Pancreatic cancer-secreted miR-155 implicates in the conversion from normal fibroblasts to cancer-associated fibroblasts. Cancer Sci. 2015;106:1362-1369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 155] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 496. | Ratajczak J, Miekus K, Kucia M, Zhang J, Reca R, Dvorak P, Ratajczak MZ. Embryonic stem cell-derived microvesicles reprogram hematopoietic progenitors: evidence for horizontal transfer of mRNA and protein delivery. Leukemia. 2006;20:847-856. [PubMed] |
| 497. | Pan Q, Ramakrishnaiah V, Henry S, Fouraschen S, de Ruiter PE, Kwekkeboom J, Tilanus HW, Janssen HL, van der Laan LJ. Hepatic cell-to-cell transmission of small silencing RNA can extend the therapeutic reach of RNA interference (RNAi). Gut. 2012;61:1330-1339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 136] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 498. | Verweij FJ, Middeldorp JM, Pegtel DM. Intracellular signaling controlled by the endosomal-exosomal pathway. Commun Integr Biol. 2012;5:88-93. [PubMed] |
| 499. | Higginbotham JN, Demory Beckler M, Gephart JD, Franklin JL, Bogatcheva G, Kremers GJ, Piston DW, Ayers GD, McConnell RE, Tyska MJ. Amphiregulin exosomes increase cancer cell invasion. Curr Biol. 2011;21:779-786. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 299] [Cited by in RCA: 285] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 500. | Yang M, Chen J, Su F, Yu B, Su F, Lin L, Liu Y, Huang JD, Song E. Microvesicles secreted by macrophages shuttle invasion-potentiating microRNAs into breast cancer cells. Mol Cancer. 2011;10:117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 491] [Cited by in RCA: 564] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 501. | Zhang Y, Liu D, Chen X, Li J, Li L, Bian Z, Sun F, Lu J, Yin Y, Cai X. Secreted monocytic miR-150 enhances targeted endothelial cell migration. Mol Cell. 2010;39:133-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 891] [Cited by in RCA: 975] [Article Influence: 60.9] [Reference Citation Analysis (0)] |
| 502. | Roninson IB. Molecular mechanism of multidrug resistance in tumor cells. Clin Physiol Biochem. 1987;5:140-151. [PubMed] |
| 503. | Bebawy M, Combes V, Lee E, Jaiswal R, Gong J, Bonhoure A, Grau GE. Membrane microparticles mediate transfer of P-glycoprotein to drug sensitive cancer cells. Leukemia. 2009;23:1643-1649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 264] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 504. | Aga M, Bradley JM, Wanchu R, Yang YF, Acott TS, Keller KE. Differential effects of caveolin-1 and -2 knockdown on aqueous outflow and altered extracellular matrix turnover in caveolin-silenced trabecular meshwork cells. Invest Ophthalmol Vis Sci. 2014;55:5497-5509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Invited manuscript
P- Reviewer: Jorg K, Ross JA S- Editor: Gong ZM L- Editor: A E- Editor: Ma S