Published online Dec 21, 2015. doi: 10.3748/wjg.v21.i47.13240
Peer-review started: April 9, 2015
First decision: June 19, 2015
Revised: August 27, 2015
Accepted: September 13, 2015
Article in press: September 14, 2015
Published online: December 21, 2015
Processing time: 251 Days and 3.7 Hours
AIM: To study histidine decarboxylase (HDC) expression in normal and neoplastic gastric neuroendocrine cells in relationship to the main histamine metabolite.
METHODS: Control tissues from fundus (n = 3) and corpus (n = 3) mucosa of six patients undergoing operations for gastric adenocarcinoma, biopsy and/or gastric surgical specimens from 64 patients with primary gastric neuroendocrine tumours (GNETs), as well as metastases from 22 of these patients, were investigated using conventional immunohistochemistry and double immunofluorescence with commercial antibodies vs vesicular monoamine transporter 2 (VMAT-2), HDC and ghrelin. The urinary excretion of the main histamine metabolite methylimidazoleacetic acid (U-MeImAA) was determined using high-performance liquid chromatography in 27 of the 64 patients.
RESULTS: In the gastric mucosa of the control tissues, co-localization studies identified neuroendocrine cells that showed immunoreactivity only to VMAT-2 and others with reactivity only to HDC. A third cell population co-expressed both antigens. There was no co-expression of HDC and ghrelin. Similar results were obtained in the foci of neuroendocrine cell hyperplasia associated with chronic atrophic gastritis type A and also in the tumours. The relative incidence of the three aforementioned markers varied in the tumours that were examined using conventional immunohistochemistry. All of these GNETs revealed both VMAT-2 and HDC immunoreactivity, and their metastases showed an immunohistochemical pattern and frequency similar to that of their primary tumours. In four patients, increased U-MeImAA excretion was detected, but only two of the patients exhibited related endocrine symptoms.
CONCLUSION: Human enterochromaffin-like cells appear to partially co-express VMAT-2 and HDC. Co-expression of VMAT-2 and HDC might be required for increased histamine production in patients with GNETs.
Core tip: It is suggested that only a fraction of vesicular monoamine transporter 2 (VMAT-2) immunoreactive neuroendocrine cells in human oxyntic mucosa co-express histidine decarboxylase (HDC), and vice versa, suggesting that the enterochromaffin-like (ECL) cells may not represent a homogeneous cell population when examined for HDC immunoreactivity. Co-expression of VMAT-2 and HDC might be important for giving rise to increased histamine production in patients with ECL cell neuroendocrine tumours. Furthermore, an increase of urinary excretion of the main histamine metabolite methylimidazoleacetic acid was not always associated with hormonal symptoms. This result could be attributed to the rate of histamine release. A sudden rapid release will cause a flush, whereas a slower release will not.
- Citation: Tsolakis AV, Grimelius L, Granerus G, Stridsberg M, Falkmer SE, Janson ET. Histidine decarboxylase and urinary methylimidazoleacetic acid in gastric neuroendocrine cells and tumours. World J Gastroenterol 2015; 21(47): 13240-13249
- URL: https://www.wjgnet.com/1007-9327/full/v21/i47/13240.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i47.13240
The enterochromaffin-like (ECL) cell is the most abundant neuroendocrine cell type of the gastric oxyntic mucosa and is generally considered to produce, store and secrete histamine[1]. This biogenic amine is formed by enzymatic decarboxylation of the amino acid histidine by histidine decarboxylase (HDC) and transported into secretory granules by proton-histamine counter transport via the vesicular monoamine transporter subtype 2 (VMAT-2)[2-4].
Recent studies have shown that only some ghrelin immunoreactive (IR) cells in the gastric mucosa express VMAT-2[5,6]. Thus, VMAT-2 does not seem specific for a homogeneous neuroendocrine cell type. However, VMAT-2 is suggested to be a specific marker for ECL cell neuroendocrine tumours (NETs) and is not expressed in ghrelinomas[6-12].
At present, histamine cannot be detected immunohistochemically in routine formalin-fixed tissue specimens by any commercially available antibody because its preservation requires a specific fixation procedure[13]. Because HDC is the specific enzyme for the production of histamine, its presence indicates synthesis of this amine and thus it can be used to visualize histamine-forming cells immunohistochemically[14].
Two immunohistochemical studies have examined human ECL cell NETs by means of both VMAT-2 and HDC antibodies[10,15]. In these tumours, some of the neoplastic parenchymal cells were IR to HDC, whereas the transporter had a wider distribution.
The production and release of histamine can be estimated by measuring the urinary excretion of the main and specific histamine metabolite methylimidazoleacetic acid (U-MeImAA)[16]. Patients with various types of ECL cell NETs occasionally have an increased excretion of U-MeImAA[17-21]. Some of these patients also suffer from the atypical carcinoid syndrome (ACS)[17-20].
The purpose of this study was to characterize normal gastric mucosa, foci of neuroendocrine cell hyperplasia associated with ECL cell NETs, and different types of gastric NETs with respect to the occurrence of HDC expression in relation to VMAT-2- and ghrelin-IR cells. Furthermore, the immunohistochemical expression of HDC in gastric NETs was compared to U-MeImAA levels and clinical symptoms.
Biopsy and/or gastric surgical specimens from 64 patients with primary gastric NETs, and metastases from 22 of these patients, were included in this study. Non-neoplastic oxyntic mucosa surrounding the tumours was also included with a view to examine the possible existence of foci of neuroendocrine cell hyperplasia. Based on clinico-pathological criteria, the tumours were classified as type I (n = 37), type II (n = 3) or type III (n = 10) ECL cell NETs, as non-ECL cell NET (n = 1), as ghrelinomas (n = 2), and as neuroendocrine carcinomas (NECs) (n = 11)[22]. The latter included four small-cell and seven large-cell type NECs. The cases of metastases that were examined included type I (n = 3), type II (n = 1) and type III (n = 7) ECL cell NETs, ghrelinomas (n = 2), and NECs (n = 9). The tumours were also classified according to the staging system based on TNM (Tables 1 and 2)[23]. One patient with type II ECL cell NET complained of flushes and another with type III developed ACS.
| Tumour type | n | TNM/stage | Age (yr), median (range) | M:F (ratio) | Tumour size (mm) | Localization |
| Type I ECL cell NETs | 37 | 65 (29-80) | 13:24 | 1-50 | Fundus, corpus | |
| 22 | T1N0M0/I | |||||
| 12 | T2N0M0/IIa | |||||
| 2 | T2N1M0/IIIb | |||||
| 1 | T2N1M1/IV | |||||
| Type II ECL cell NETs | 3 | 48 (47-49) | 1:2 | 0.5-25 | Fundus, corpus, antrum | |
| 2 | T1N0M0/I | |||||
| 1 | T2N1M0/IIa | |||||
| Type III ECL cell NETs | 10 | 62 (23-77) | 4:6 | 7-55 | Fundus, Corpus, antrum | |
| 1 | T1N0M0/I | |||||
| 3 | T2N1M0/IIIb | |||||
| 2 | T2N0M1/IV | |||||
| 2 | T2N1M1/IV | |||||
| 2 | T4N1M1/IV | |||||
| Non-ECL cell NET | 1 | T2N1M1/IV | 71 | 0:1 | 20 | Corpus, antrum |
| Ghrelinomas | 2 | T2N1M1/IV | 55 (47-63) | 2:0 | 35-40 | Corpus |
| NECs | 11 | 58 (39-77) | 8:3 | 30-100 | Fundus, corpus | |
| Small cell | 4 | |||||
| 2 | T2N0M0/IIa | |||||
| 1 | T3N1M1/IV | |||||
| 1 | T4N1M1/IV | |||||
| Large cell | 7 | T4N0M0/IIIa | ||||
| 1 | T2N1M1/IV | |||||
| 4 | T3N1M1/IV | |||||
| 1 | T4N1M1/IV | |||||
| 1 | ||||||
| Total number | 64 |
| Age/Gender | VMAT-2-IR tumour cells (primary) | HDC-IR tumour cells (primary) | HDC-IR tumour cells (metastases) | U-MeImAA(mmol/mol creatinine) | Diameter(mm) | TNM/stage |
| Type I ECL cell NETs (n = 15) | ||||||
| 47/F | > 90% | 0% | - | 1.6 | 2 | T1m,N0,M0/I |
| 52/M | > 90% | 0% | - | 1.6 | 10 | T1m,N0,M0/I |
| 55/F | > 90% | 0%D | - | 1.1 | 23 | T2,N0,M0/IIa |
| 61/F | > 90% | 0% | - | 1.3 | 2 | T1,N0,M0/I |
| 62/F | > 90% | 0% | - | 1.4 | 3 | T1m,N0,M0/I |
| 64/M | > 90% | 0% | - | 1.1 | 5 | T1m,N0,M0/I |
| 65/F | > 90% | 0% | - | 2.0 | 25 | T2,N0,M0/IIa |
| 72/F | > 90% | 0% | - | 1.1 | 5 | T1,N0,M0/I |
| 74/F | > 90% | 0%D | - | 1.7 | 2.2 | T1m,N0,M0/I |
| 78/F | > 90% | 0% | - | 1.8 | 4 | T1m,N0,M0/I |
| 79/F | > 90% | 0% | - | 2.4 | 1.5 | T1m,N0,M0/I |
| 80/M | > 90% | 0% | - | 1.5 | 7 | T1m,N0,M0/I |
| 54/F | > 90% | 1% | - | 1.5 | 5 | T1m,N0,M0/I |
| 71/F | > 90% | 1% | - | 1.8 | 15 | T2,N0,M0/IIa |
| 65/M | > 90% | 3%D | - | 1.6 | 12 | T2m,N0,M0/IIa |
| Type II ECL cell NET (n = 1) | ||||||
| 49/F | > 90% | 10%D, L | 40% | 9.01 | 3 | T1m,N0,M0/I |
| Type III ECL cell NETs (n = 6) | ||||||
| 44/F | > 90% | 0% | 0% | 1.6 | 22 | T2,N1,M0/IIIb |
| 60/M | > 90% | 0% | 0% | 1.4 | 11 | T2,N1,M0/IIIb |
| 60/F | > 90% | 0% | - | 2.4 | 7 | T1,N0,M0/I |
| 77/F | > 90% | 1% | 40% | 40.8 | 30 | T2,N0,M1/IV |
| 72/M | > 90% | 10% | 70% | 1.1 | 11 | T2,N1,M1/IV |
| 62/M | > 90% | 20% | 40% | 18.22 | 45 | T4,N1,M1/IV |
| Ghrelinoma (n = 1) | ||||||
| 47/M | 0% | 0% | 0% | 1.2 | 40 | T2,N1,M1/IV |
| NECs (n = 4) | ||||||
| 76/M | 0% | 0% | 0% | 1.6 | 30 | T2,N1,M1/IV |
| 69/M | 10% | 0% | 0% | 1.8 | 100 | T4,N1,M1/IV |
| 61/F | 60% | 15% | 15% | 2.9 | 100 | T4,N1,M1/IV |
| 58/M | 0% | 60% | 60% | 1.2 | 90 | T4,N0,M0/IIIa |
Control tissues were from the fundus (n = 3) and corpus (n = 3) mucosa of six patients undergoing operations for gastric adenocarcinoma. All of the specimens examined originated from macro- and microscopically normal gastric mucosa. The surgical specimens were located at least 3 cm from the neoplasm. In the tissue samples obtained from the gastric NETs, adjacent non-neoplastic mucosa was also used as an internal control.
All of the tissue samples were conventionally fixed in 10% buffered neutral formalin and routinely processed to paraffin wax. Consecutive sections, approx. 4 μm thick, were attached to positively charged glass slides (Superfrost® Plus; Menzel Gläser, Braunschweig, Germany).
The primary antibodies used were rabbit polyclonal antibodies vs VMAT-2 (AB1767, Chemicon International, Temecula, CA, United States, 1:400), vs human ghrelin (H-031-30, Phoenix Pharmaceuticals Inc., Belmont, CA, United States, 1:4800) and vs recombinant HDC raised in E. coli (B 260-1, Euro-Diagnostica, Malmö, Sweden, diluted 1:5000). The tissues were immunostained using a polymer-detection system (DakoCytomation, EnVision® + System-HRP, K4010 for primary rabbit) with diaminobenzidine as the chromogen. Before immunostaining, the sections were microwave treated for 2 min × 5 min at 750 W, using Tris buffer saline, pH 8.0, as a retrieval solution.
The density of the IR cells, expressed as the number of IR cells per one mm2 of mucosal area, was calculated using a square grid in one of the oculars. In small lesions with a tumour area of < 1 mm2, all of the neoplastic parenchymal cells were examined.
For immunofluorescence staining, the following primary antibodies were used: polyclonal rabbit anti-HDC (B 260-1, Euro-Diagnostica, Malmö, diluted 1:100 when the conventional indirect method was used and 1:800 with the streptavidin), polyclonal goat anti-VMAT-2 (C-20, sc-7721, Santa Cruz Biotechnology®, Santa Cruz, CA, 1:200), and polyclonal chicken anti-ghrelin (a-a 17-28, Y-031-44, Phoenix Pharmaceuticals, Belmont, CA, 1:800).
The sections were microwave treated as described above and then incubated overnight with a cocktail of two primary antibodies at 4 °C. Before application of the antibody cocktail, the sections were incubated with a mixture of non-immune sera from the animal species producing the secondary antibodies, diluted 1:10. The following secondary antisera were used: (1) tetramethyl rhodamine isothiocyanate (TRITC)-conjugated AffiniPure donkey anti-rabbit (711-025-152, Jackson ImmunoResearch Laboratories, 1:100) and biotinylated horse anti-goat (BA-9500, Vector Laboratories, 1:100) for the co-localization studies of HDC and VMAT-2; and (2) biotinylated goat anti- rabbit (BA-1000, Vector Laboratories, 1:100) and fluorescein isothiocyanate (FITC)-conjugated AffiniPure donkey anti-chicken (703-095-155, Jackson ImmunoResearch Laboratories, 1:100) for HDC and ghrelin. The incubation time for the secondary antisera was 30 min at room temperature. A further incubation was performed for 30 min at room temperature with a streptavidin-conjugated fluorophore. Streptavidin-FITC (SA-5001, Vector Laboratories) was used as a fluorophore for the first combination, and streptavidin-Texas Red (SA-5006, Vector Laboratories) was used for the second combination. Tests for inappropriate binding of the secondary antisera were performed as described previously[11]. TRITC and Texas Red fluorophores give rise to red fluorescence, and FITC gives rise to green fluorescence.
The sections were examined using a Zeiss Axioplan2 fluorescence microscope and photographed with an AxioCam HRm camera employing Axiovision imaging software and a 63X plan-apochromat objective. In the co-localization studies, the tissue specimens from normal fundus (n = 3) and corpus (n = 3) and from types I (n = 5), II (n = 1), and III (n = 2) ECL cell NETs, including their respective metastases (one lymph node metastasis from each type of ECL cell NET, respectively), were examined.
When the gastric fundus (n = 3) and corpus (n = 3) mucosal specimens were examined, photos were taken from randomly identified neuroendocrine cells with a view to investigate a possible co-expression of HDC- with VMAT-2- or ghrelin-IR cells. A total of 1000 cells were examined, including 750 cells (125 randomly chosen cells/specimen) that were HDC- and/or VMAT-2-IR and 250 cells (approximately 40 cells/specimen) that were ghrelin-IR.
The immunostained controls included omission of the primary antisera and replacement of the primary antibody by non-immune serum at the same dilution as the primary antibody in question and in the same diluent.
U-MeImAA was measured in 27 patients with various types of gastric NETs before obtaining biopsy samples or operation and before specific treatment (Table 2). A 24-h urine sample, collected while patients were on a histamine-restricted diet, was analysed for U-MeImAA[16]. All of the patients were instructed to avoid antihistamine medication and alcohol for at least 24 h prior to admission. U-MeImAA was determined using a HPLC assay with UV detection[24]. The reference range was 0.4-2.4 mmol/mol creatinine.
The research protocol was reviewed and approved by the local research ethics board at Uppsala University Hospital.
Multiple foci of neuroendocrine cell hyperplasia were observed adjacent to types I and II ECL cell NETs where VMAT-2-IR cells predominated followed by ghrelin-IR cells. In these foci, HDC-IR cells were few in number, but in occasional foci an inverse result occurred. The latter type of foci was observed in 14 cases of type I and two of type II ECL cell NETs (diffuse, linear and nodular hyperplasia patterns, in various combinations). Focally, diffuse HDC-IR cell hyperplasia was detected in the mucosa adjacent to the non-ECL cell NET. In the latter foci, no VMAT-2 cell hyperplasia was observed. No signs of neuroendocrine cell hyperplasia expressing HDC were observed in the peritumourous mucosa of the type III ECL cell NETs, the ghrelinomas and the NECs.
All the ECL cell NETs were VMAT-2-IR in more than 80% of the neoplastic parenchymal cells. In type I ECL cell NETs, ghrelin immunoreactivity varied from negative to the majority of the tumour cells. The two ghrelinomas examined expressed only ghrelin and did not display VMAT-2 immunoreactivity. The non-ECL cell NET examined contained a small fraction of VMAT-2- (approximately 3%) and ghrelin-IR cells (approximately 5%). Three of the NECs expressed VMAT-2 in more than half of the total number of the neoplastic cells. The remaining NECs were occasional- or non-IR for VMAT-2. None of the NECs examined expressed ghrelin.
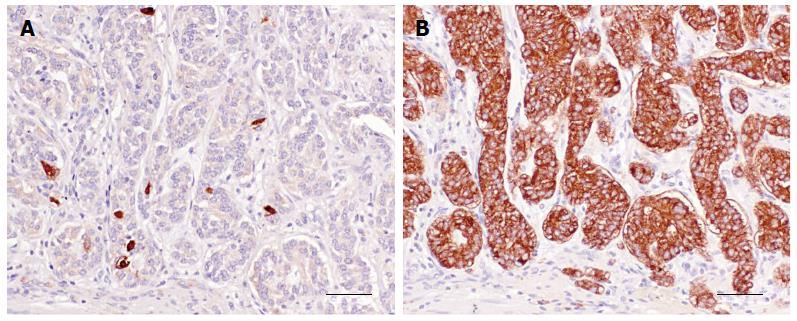
Sixteen of the 37 type I ECL cell NETs contained HDC-IR cells (< 5% in 15 cases, approximately 50% in one case) (Figure 1). In the cases with metastases, a similar distribution pattern and frequency of HDC-IR cells was seen both in the primary tumour and in its respective metastases.
Two of the three type II ECL cell NETs contained HDC-IR cells in a frequency varying from 1% to 10%. In the lymph node metastases present in one case, the relative incidence of HDC-IR cells was greater (up to 40%).
Four of the ten type III ECL cell NETs contained HDC-IR cells with a relative incidence between 1% and 30%. Their metastases usually expressed HDC more abundantly than in the primary tumours.
The non-ECL cell NET and the two ghrelinomas did not contain HDC-IR cells.
Three NECs contained HDC-IR tumour cells in approximately 15%, 20% and 60% of the neoplastic cell population. The first two above mentioned NECs revealed VMAT-2 immunoreactivity in approx. 60% of the tumour cells, whereas the latter case lacked such cells. Their metastases revealed an immunohistochemical pattern and frequency similar to that of the primary tumours.
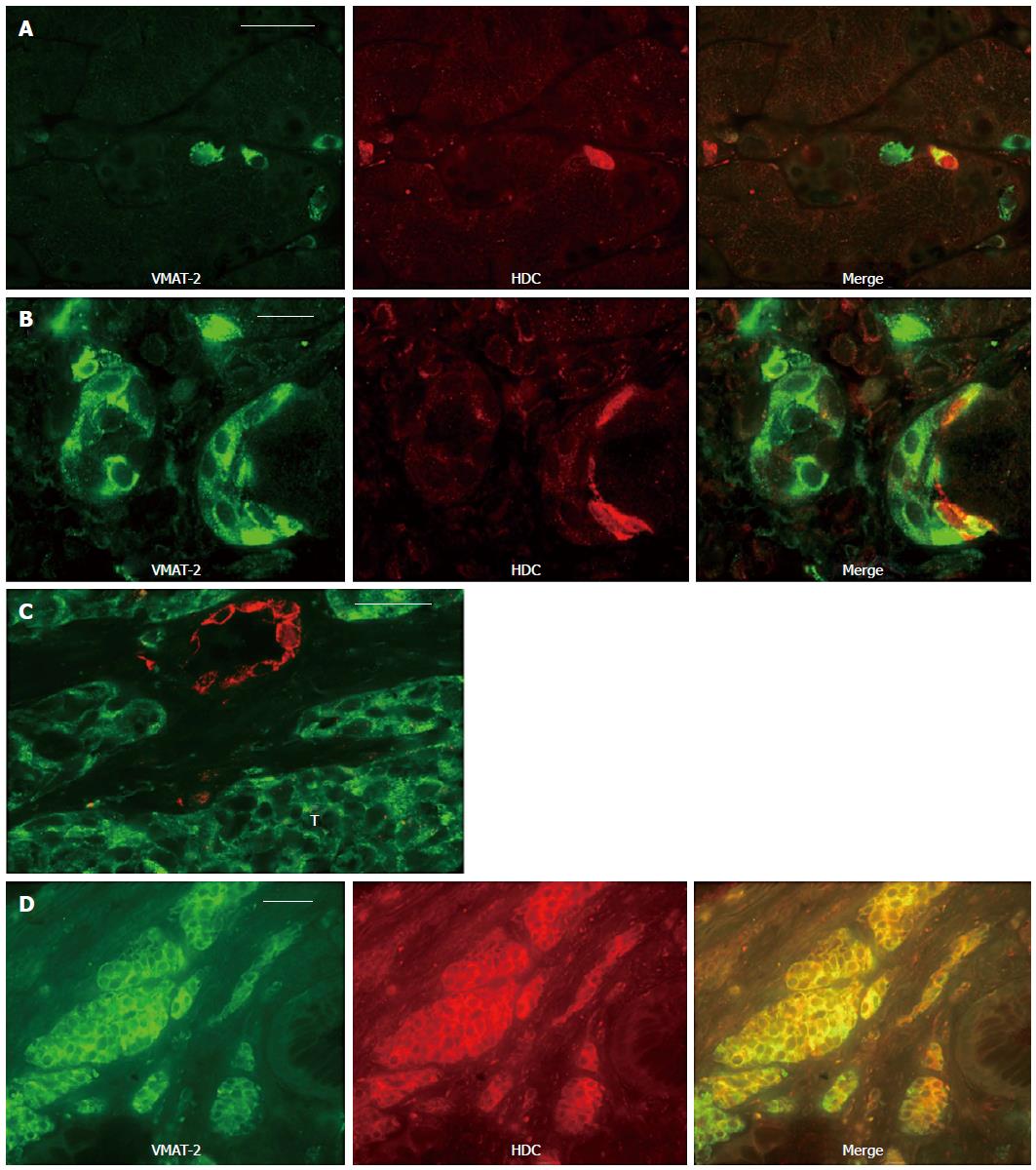
By using double immunofluorescence techniques, three patterns of immunoreactivity could be identified in the glands of the normal mucosa examined: (1) cells expressing only VMAT-2 (335/750 IR cells identified, approximately 45%); (2) only HDC (144/750 IR cells, approximately 19%); and (3) cells co-expressing both proteins (271/750 IR cells, approximately 36%) (Figure 2A). Ghrelin cells (n = 250) did not express HDC in the normal oxyntic mucosa.
In the foci of neuroendocrine cell hyperplasia in types I and II ECL cell NETs, VMAT-2-IR cells were predominant, but only a few of them co-expressed HDC (Figure 2B). In occasional foci of neuroendocrine cell hyperplasia, the HDC-IR cells were predominant, whereas VMAT-2-IR cells were few or absent (Figure 2C). In types I, II and III ECL cell NETs, most HDC-IR cells co-expressed VMAT-2 and occasional cells expressed only HDC (Figure 2D). However, the majority of the tumour cells were only VMAT-2-IR. The same finding was observed in the metastases of the type III ECL cell NETs examined. None of the neoplastic cells in types I, II and III ECL cell NETs or in the foci of neuroendocrine cell hyperplasia in the former two types of ECL cell NETs that showed ghrelin immunoreactivity were HDC-IR.
Immunoreactivity was not observed when the primary antibodies were omitted or replaced by non-immune serum. In double immunostaining, the omission of one of the primary antibodies, or its replacement by non-immune serum, gave an immunostaining pattern corresponding to that obtained with the remaining primary antibody. When both antibodies were omitted or replaced by the respective non-immune sera, the tissues were non-IR.
Four of 27 patients in whom U-MeImAA was determined had an increased excretion of the histamine metabolite (results summarized in Table 2). None of the patients with type I ECL cell NETs had increased U-MeImAA or clinical symptoms that might be related to increased histamine production, irrespective of the presence of HDC-IR tumour cells.
The U-MeImAA excretion was increased moderately in one patient with metastatic disease of type II ECL cell NET expressing VMAT-2 in virtually all neoplastic cells and HDC in 10% in the primary tumour and 40% in the respective lymph node metastasis. The patient suffered occasionally from flushes.
Two patients diagnosed with metastatic type III ECL cell NETs had increased and high levels of U-MeImAA. One of these patients developed ACS (the tumour cells were HDC-IR in 20% and 40% of the primary tumour and omentum metastasis, respectively), whereas the other patient did not report clinical symptoms related to increased histamine production (the primary tumour contained few HDC-IR cells, but the liver metastasis showed 40% HDC immunoreactivity). By contrast, one other patient with type III ECL cell NET, who had liver metastases and skin metastasis expressing HDC and VMAT-2, had U-MeImAA within the reference range.
One of the four investigated patients with NEC had a slightly elevated level of U-MeImAA without any clinical symptoms related to ACS (HDC immunoreactivity of approximately 15% of the neoplastic cells in both the primary tumour and the lymph node metastasis examined). The NEC patient with numerous HDC-IR cells in the primary tumour and in the adrenal metastasis (60%) had normal levels of the histamine metabolite in the urine. The tumour cells of that patient were non-IR for VMAT-2.
Human oxyntic mucosa contains four major types of neuroendocrine cells (ECL, ghrelin, serotonin and somatostatin cells), which have been described morphologically and functionally[25]. ECL cells are the most abundant type, and they produce histamine. The histamine-synthesizing ability of ECL cells is based on cytosolic HDC. Histamine might be transported by VMAT-2 into the secretory vesicles. The ghrelin-producing cells are the second most frequent cell type and have been reported to express VMAT-2[5]. However, these results differ from findings presented in a study where only approximately 2% of the ghrelin cell population expressed VMAT-2[11]. This disparity may be due to the differing techniques used to compare the two cell types. Our results were based on double immunofluorescence stainings, which enable visualization of a large number of cells, whereas the other results were achieved by means of immunoelectron microscopy and using immunostaining consecutive sections with the respective antibodies.
The current study showed that approximately one-third of the VMAT-2-IR cells in normal human gastric mucosa co-express HDC. Additionally, numerous HDC-IR cells in the oxyntic mucosa were non-IR for VMAT-2, implying that HDC is expressed in only a fraction of VMAT-2-IR cells. Thus, we show that there is by no means a complete co-existence between histamine expression visualized by HDC immunoreactivity and VMAT-2. In animal models it has been shown that a disappearance of HDC-IR cells occurs after 24 h of food deprivation[26]. Although our specimens were obtained during the operation from patients fasting overnight, it is less likely that the disparity between VMAT-2- and HDC-IR cells can be entirely attributed to down regulation of HDC because of food deprivation. Although VMAT-2 is well characterized, it cannot be excluded that other proteins or forms of VMAT-2 exist that were not identified by the chosen antibody. As previously reported for the fundus, ghrelin did not co-localize with HDC in the corpus mucosa[27].
In the foci of neuroendocrine cell hyperplasia, two different patterns appeared: a more common one identified primarily by VMAT-2 immunoreactivity and a less common one with predominantly HDC-IR cells. According to our co-localization studies in the former foci, only a few cells co-expressed HDC, whereas in the latter foci an inverse result occurred. It is well established that hypergastrinaemia causes ECL cell hyperplasia, which can transform into ECL cell NETs[28,29]. Biochemical studies have shown that the total mucosa content of HDC increases in patients with chronic atrophic gastritis type A[30]. However, remains unclear whether this increase in concentration depends on a higher frequency of HDC expressing cells or on an increase in HDC content in individual cells or both. It was expected that the increase in VMAT-2-IR cells would be accompanied by a similar increase in HDC-IR cells. However, only occasional foci with HDC-IR cell hyperplasia were identified in the atrophic mucosa. The HDC antibody used is well characterized, but we cannot exclude that HDC may undergo post-translational modifications and exist in forms not identified by the present antibody[10].
In agreement with previous studies, our results showed that all types of ECL cell NETs, as well their respective metastases, can express HDC-IR tumour cells in varying relative incidences[10,15]. Furthermore, according to our co-localization findings, occasional neoplastic cells displaying HDC immunoreactivity were non-IR for VMAT-2. This may be due to tumour de-differentiation or, more plausibly, because these neoplastic cells are derived from the HDC-IR cells that do not express VMAT-2.
Four of the 27 patients in whom U-MeImAA was determined had increased urinary excretion of this histamine metabolite. All of these patients had metastatic tumours that showed both HDC and VMAT-2 immunoreactivity. In other studies, it has been reported that even type I ECL cell NETs may be accompanied by increased U-MeImAA levels[19,21]. Our results indicate that only disseminated disease can give rise to increased U-MeImAA excretion, although disseminated disease does not invariably lead to increased U-MeImAA levels. It is likely that the tumour load, often high in type III ECL cell NETs, is decisive; however, the tumour load also has to be accompanied most likely by both HDC and VMAT-2 expression, as HDC expression alone does not invariably predict increased U-MeImAA excretion. Other factors involved in the production, transport and/or secretion of histamine that were not examined in the present study may also play an important role.
Furthermore, no apparent relationship was found between increased U-MeImAA excretion and the clinical symptoms of the respective patients. This could probably be attributed to the rate of histamine release. A sudden rapid release will cause a flush whereas a slower release will not. Additionally, an efficient local inactivation of histamine before it reaches the systemic circulation might explain the absence of symptoms even when large amounts of histamine are being released.
In conclusion, only a fraction of the VMAT-2-IR neuroendocrine cells in human oxyntic mucosa co-express HDC, and vice versa, suggesting that the ECL cells may not represent a homogeneous cell population when examined for HDC immunoreactivity. Co-expression of VMAT-2 and HDC might be substantial for giving rise to increased histamine production in patients with ECL cell NETs. Furthermore, an increase in U-MeImAA excretion is not always associated with hormonal symptoms.
Enterochromaffin-like (ECL) cells are the most abundant neuroendocrine cell type in the gastric mucosa, and they produce histamine. The histamine-synthesizing ability of ECL cells is based on cytosolic histidine decarboxylase (HDC). Histamine is transported by vesicular monoamine transporter subtype 2 (VMAT-2) into the secretory vesicles. The production and release of histamine can be estimated by measuring the urinary excretion of the main and specific histamine metabolite tele-methylimidazoleacetic acid (U-MeImAA). ECL cells can undergo malignant transformation to ECL cell neuroendocrine tumours (NETs)
Previous immunohistochemical studies have examined human ECL cell NETs by means of both VMAT-2 and HDC antibodies. In these tumours, some of the neoplastic parenchymal cells were immunoreactive to HDC, whereas the transporter had a wider distribution.
This study show that there is by no means a complete co-existence between histamine expression visualized by HDC immunoreactivity and VMAT-2, neither in the gastric mucosa nor in the foci of endocrine cell hyperplasia/ECL cell NETs. The results indicate that only disseminated disease can give rise to increased U-MeImAA excretion, although disseminated disease does not invariably lead to increased U-MeImAA levels. Furthermore, no apparent relationship was found between increased U-MeImAA excretion and the clinical symptoms of the respective patients.
The ECL cells may not represent a homogeneous cell population when examined for HDC immunoreactivity. Co-expression of VMAT-2 and HDC might be important for giving rise to increased histamine production in patients with ECL cell NETs. Furthermore, an increase in U-MeImAA excretion is not always associated with hormonal symptoms.
ECL cells use the enzyme HDC to produce histamine, which is transported by VMAT-2 from the cytoplasm into the secretory vesicles. The production and release of histamine can be estimated by measurement of the urinary excretion of the main and specific histamine metabolite U-MeImAA.
The paper is well written but the topic is extremely specific and it may be of limited interest for the most of journal readers.
| 1. | Bordi C, D’Adda T, Azzoni C, Ferraro G. Classification of gastric endocrine cells at the light and electron microscopical levels. Microsc Res Tech. 2000;48:258-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Viguera E, Trelles O, Urdiales JL, Matés JM, Sánchez-Jiménez F. Mammalian L-amino acid decarboxylases producing 1,4-diamines: analogies among differences. Trends Biochem Sci. 1994;19:318-319. [PubMed] |
| 3. | Dimaline R, Struthers J. Expression and regulation of a vesicular monoamine transporter in rat stomach: a putative histamine transporter. J Physiol. 1996;490:249-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 51] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Zhao CM, Jacobsson G, Chen D, Hâkanson R, Meister B. Exocytotic proteins in enterochromaffin-like (ECL) cells of the rat stomach. Cell Tissue Res. 1997;290:539-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Rindi G, Necchi V, Savio A, Torsello A, Zoli M, Locatelli V, Raimondo F, Cocchi D, Solcia E. Characterisation of gastric ghrelin cells in man and other mammals: studies in adult and fetal tissues. Histochem Cell Biol. 2002;117:511-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 144] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 6. | Tsolakis AV, Grimelius L, Stridsberg M, Falkmer SE, Waldum HL, Saras J, Janson ET. Obestatin/ghrelin cells in normal mucosa and endocrine tumours of the stomach. Eur J Endocrinol. 2009;160:941-949. [PubMed] |
| 7. | Eissele R, Anlauf M, Schäfer MK, Eiden LE, Arnold R, Weihe E. Expression of vesicular monoamine transporters in endocrine hyperplasia and endocrine tumors of the oxyntic stomach. Digestion. 1999;60:428-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Rindi G, Paolotti D, Fiocca R, Wiedenmann B, Henry JP, Solcia E. Vesicular monoamine transporter 2 as a marker of gastric enterochromaffin-like cell tumors. Virchows Arch. 2000;436:217-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 49] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Jakobsen AM, Andersson P, Saglik G, Andersson E, Kölby L, Erickson JD, Forssell-Aronsson E, Wängberg B, Ahlman H, Nilsson O. Differential expression of vesicular monoamine transporter (VMAT) 1 and 2 in gastrointestinal endocrine tumours. J Pathol. 2001;195:463-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 40] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Uccella S, Cerutti R, Vigetti D, Furlan D, Oldrini R, Carnevali I, Pelosi G, La Rosa S, Passi A, Capella C. Histidine decarboxylase, DOPA decarboxylase, and vesicular monoamine transporter 2 expression in neuroendocrine tumors: immunohistochemical study and gene expression analysis. J Histochem Cytochem. 2006;54:863-875. [PubMed] |
| 11. | Tsolakis AV, Stridsberg M, Grimelius L, Portela-Gomes GM, Falkmer SE, Waldum HL, Janson ET. Ghrelin immunoreactive cells in gastric endocrine tumors and their relation to plasma ghrelin concentration. J Clin Gastroenterol. 2008;42:381-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Tsolakis AV, Portela-Gomes GM, Stridsberg M, Grimelius L, Sundin A, Eriksson BK, Oberg KE, Janson ET. Malignant gastric ghrelinoma with hyperghrelinemia. J Clin Endocrinol Metab. 2004;89:3739-3744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 69] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 13. | Håkanson R, Böttcher G, Ekblad E, Panula P, Simonsson M, Dohlsten M, Hallberg T, Sundler F. Histamine in endocrine cells in the stomach. A survey of several species using a panel of histamine antibodies. Histochemistry. 1986;86:5-17. [PubMed] |
| 14. | Dartsch C, Chen D, Håkanson R, Persson L. Histidine decarboxylase in rat stomach ECL cells: relationship between enzyme activity and different molecular forms. Regul Pept. 1999;81:41-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Rindi G, Savio A, Torsello A, Zoli M, Locatelli V, Cocchi D, Paolotti D, Solcia E. Ghrelin expression in gut endocrine growths. Histochem Cell Biol. 2002;117:521-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Granerus G. Urinary excretion of histamine, methylhistamine and methylimidazoleacetic acids in man under standardized dietary conditions. Scand J Clin Lab Invest Suppl. 1968;104:59-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 47] [Article Influence: 0.8] [Reference Citation Analysis (2)] |
| 17. | Granerus G, Lindell SE, Waldenström J, Westling H, White T. Histamine metabolism in carcinoidosis. Lancet. 1966;1:1267-1268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Ahlman H, Dahlström A, Enerbäck L, Granérus G, Nilsson O, Persson S, Tisell LE. Two cases of gastric carcinoids: diagnostic and therapeutic aspects. World J Surg. 1988;12:356-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Ahlman H, Wängberg B, Nilsson O, Grimelius L, Granérus G, Modlin IM, Stenqvist O, Scherstén T. Aspects on diagnosis and treatment of the foregut carcinoid syndrome. Scand J Gastroenterol. 1992;27:459-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Ahlman H, Kölby L, Lundell L, Olbe L, Wängberg B, Granérus G, Grimelius L, Nilsson O. Clinical management of gastric carcinoid tumors. Digestion. 1994;55 Suppl 3:77-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 49] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Borch K, Ahrén B, Ahlman H, Falkmer S, Granérus G, Grimelius L. Gastric carcinoids: biologic behavior and prognosis after differentiated treatment in relation to type. Ann Surg. 2005;242:64-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 193] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 22. | Solcia E, Arnold R, Capella C, Klimstra DS, Klöppel G, Komminoth P, Rindi G. Neuroendocrine neoplasms of the stomach. WHO Classification of Tumours of the Digestive System. 4th ed. Lyon: World Health Organization 2010; 64-68. |
| 23. | Rindi G, Klöppel G, Alhman H, Caplin M, Couvelard A, de Herder WW, Erikssson B, Falchetti A, Falconi M, Komminoth P, Körner M, Lopes JM, McNicol AM, Nilsson O, Perren A, Scarpa A, Scoazec JY, Wiedenmann B; all other Frascati Consensus Conference participants; European Neuroendocrine Tumor Society (ENETS). TNM staging of foregut (neuro)endocrine tumors: a consensus proposal including a grading system. Virchows Arch. 2006;449:395-401. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1196] [Cited by in RCA: 1095] [Article Influence: 54.8] [Reference Citation Analysis (0)] |
| 24. | Granerus G, Lönnqvist B, Wass U. Determination of the histamine metabolite tele-methylimidazoleacetic acid and of creatinine in urine by the same HPLC system. Inflamm Res. 1999;48:75-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Solcia E, Rindi G, Buffa R, Fiocca R, Capella C. Gastric endocrine cells: types, function and growth. Regul Pept. 2000;93:31-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 54] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 26. | Torbergsen K, Wiksén H, Johansen K, Rahimipoor S, Falkmer UG, Zhao CM. Immunoreactivity of gastric ECL and A-like cells in fasted and fed rats and mice. Biotech Histochem. 2005;80:21-30. [PubMed] |
| 27. | Date Y, Kojima M, Hosoda H, Sawaguchi A, Mondal MS, Suganuma T, Matsukura S, Kangawa K, Nakazato M. Ghrelin, a novel growth hormone-releasing acylated peptide, is synthesized in a distinct endocrine cell type in the gastrointestinal tracts of rats and humans. Endocrinology. 2000;141:4255-4261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 919] [Cited by in RCA: 963] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 28. | Bordi C, D’Adda T, Azzoni C, Pilato FP, Caruana P. Hypergastrinemia and gastric enterochromaffin-like cells. Am J Surg Pathol. 1995;19 Suppl 1:S8-S19. [PubMed] |
| 29. | Thomas D, Tsolakis AV, Grozinsky-Glasberg S, Fraenkel M, Alexandraki K, Sougioultzis S, Gross DJ, Kaltsas G. Long-term follow-up of a large series of patients with type 1 gastric carcinoid tumors: data from a multicenter study. Eur J Endocrinol. 2013;168:185-193. [PubMed] |
| 30. | Cattan D, Roucayrol AM, Launay JM, Callebert J, Charasz N, Nurit Y, Belaiche J, Kalifat R. Circulating gastrin, endocrine cells, histamine content, and histidine decarboxylase activity in atrophic gastritis. Gastroenterology. 1989;97:586-596. [PubMed] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Cananzi FCM S- Editor: Yu J L- Editor: A E- Editor: Ma S