Published online Mar 28, 2015. doi: 10.3748/wjg.v21.i12.3694
Peer-review started: July 18, 2014
First decision: August 15, 2014
Revised: September 3, 2014
Accepted: October 21, 2014
Article in press: October 21, 2014
Published online: March 28, 2015
Processing time: 256 Days and 4.2 Hours
AIM: To construct a meta-analysis in order to examine the relationship between cadherin-17 (CDH17) and gastric cancer (GC).
METHODS: Related articles were selected by searching the following English or Chinese electronic databases: CINAHL, MEDLINE, Science Citation Index, the Chinese Journal Full-Text, and the Weipu Journal. Newcastle-Ottawa Scale (NOS) criteria were used to ensure consistency in reviewing and reporting results. Statistical analyses were conducted with Version 12.0 STATA statistical software.
RESULTS: Ultimately, 11 articles, with a total of 2,120 GC patients, were found to be eligible for study inclusion. In comparisons of GC patients by TNM stage (III-IV vs I-II: OR = 2.35, 95%CI: 1.15-4.825, P = 0.019), histologic grade (3-4 vs 1-2: OR = 3.48, 95%CI: 1.36-8.92, P = 0.009), invasion grade (T3-4 vs T1-2: OR = 2.86; 95%CI: 1.69-4.83; P = 0.000), and lymph node metastasis (positive vs negative: OR = 2.64; 95%CI: 1.33-5.27; P = 0.006), it was found that CDH17 showed more positive expressions in each of the more severe cases. Country-stratified analyses from all four experimental subgroups showed that high CDH17 expression levels may be related to GC among Chinese and Korean populations (all P < 0.05), with the exception of the invasion grade T3-4 vs T1-2 comparison, where the relation only held among the Chinese population (OR = 2.86, 95%CI: 1.69-4.83, P = 0.000).
CONCLUSION: Collectively, the data reflects the capacity of CDH17 in tumor proliferation and metastasis among GC patients.
Core tip: This meta-analysis conducted in order to examine the relationship between cadherin-17 (CDH17) and gastric cancer (GC), with the data reflecting the capacity of CDH17 in tumor proliferation and metastasis in GC patients.
- Citation: Long ZW, Zhou ML, Fu JW, Chu XQ, Wang YN. Association between cadherin-17 expression and pathological characteristics of gastric cancer: A meta-analysis. World J Gastroenterol 2015; 21(12): 3694-3705
- URL: https://www.wjgnet.com/1007-9327/full/v21/i12/3694.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i12.3694
Gastric cancer (GC) is a malignant disease arising from gastric tissue. More than 90% of GCs are adenocarcinomas, with the remainder being lymphomas or emerging from gastrointestinal stromal tissue (sarcomas)[1]. GC is the fourth most common cancer in the world and the second leading cause of cancer-related death globally[2]. Although the last decade has witnessed a dramatic decrease in the prevalence of GC in some developed countries, approximately one million newly diagnosed cases, along with 800000 GC-related deaths, occur each year worldwide[3]. In fact, it has been reported that two-thirds of GC cases occur in developing countries, with particularly high incidences in areas such as Japan, China, Central America, and South America[4]. Generally, gastric carcinogenesis is a multifactorial process involving the participation of both environmental and epigenetic factors[1,5]. A variety of factors that are related to the occurrence and progression of GC have been confirmed, including Helicobacter pylori infection, low fruit intake, consumption of foods high in salt, smoking, and consumption of preserved foods and nitrites[4,6,7]. Recently, adhesion molecules such as cadherin-17 (CDH17), which is reported to be implicated in tumor invasion and metastasis, have been shown to be correlated with GC pathogenesis[8].
CDH17, also known as liver-intestine cadherin or human peptide transporter-1, consists of seven homologous repeated domains, and while it belongs to the cadherin superfamily responsible for intercellular conjunction, its structure is distinct from that of classic cadherin family members[9]. CDH17 possesses the ability to modulate Ca2+-dependent homophilic cell-cell adhesion without depending on cytoskeleton interaction, suggesting that it may play a central role in tumor metastasis[10,11]. In addition, CDH17 has been shown to both act as a peptide transporter and participate in the development of the embryonic gastrointestinal tract[12]. In recent studies, CDH17 expression was observed to be upregulated in GC patients, implying that CDH17 expression is related to GC development[5,9]. In general, CDH17 is expressed on the basolateral surface of enterocytes and goblet cells in the small and large intestines in a selective manner, and is seldom detected in the healthy adult stomach or liver[10,13]. Cadherins, including CDH17, are single-pass transmembrane proteins that function mainly in cell-cell adhesion and may be implicated in tumorigenesis[14]. It has been reported that CDH17 knockdown may result in the inactivation of Wnt signaling, which could in turn inhibit the activity of cancer cell invasion[12]. More importantly, there is evidence indicating that loss of CDH17 may lead to an increased expression of placental growth factor and metal-responsive transcription factor-1, which is believed to increase tumor aggression, thus modulating angiogenesis in human carcinoma[15]. Additionally, by activating the NFκB signaling pathway, CDH17 can also induce lymph node (LN) metastasis, as well as the formation of tumors in GC[16]. With this in mind, it is possible that CDH17 expression may be involved in the pathogenesis and progression of GC. Several clinical studies have documented that high expression levels of CDH17 were positively connected with histological stage, tumor invasion, and LN metastasis of GC, revealing that CDH17 expression might be a valuable indicator for predicting the progression and prognosis of GC[8,17]. However, other researchers have failed to find evidence to support the correlation of CDH17 expression with pathological characteristics of GC[5,9]. With such an inconsistency in previous reported findings in mind, we performed the current meta-analysis with the available data in order to clarify the connection between CDH17 expression and the pathological features of GC.
The following computerized bibliographic databases were reviewed, without restrictions with respect to language or data collection, to identify relevant articles relating to the association of CDH17 expression and GC susceptibility: PubMed, Embase, CINAHL, Science Citation Index, the Cochrane Library, Current Contents Index, Chinese Biomedical, the Chinese Journal Full-Text, and the Weipu Journal. The search terms “stomach neoplasms” or “gastric cancer” or “stomach cancer” or “gastric neoplasms” or “gastric carcinomas” or “stomach carcinomas” or “carcinoma ventriculi” or “stomach neoplasms” and “CDH17 protein, human” or “CDH17” or “liver-intestine-cadherin” or “cadherin-17” were entered in the databases searches as medical subject heading terms and text words, within a highly sensitive search strategy. Manual searches were used to screen other eligible studies.
After reading the abstract, full texts were retrieved and assessed for their suitability based on the following inclusion criteria: (1) clinical studies had to examine the association between CDH17 expression and the pathological features of GC within a human population; (2) tumor specimens were drawn from all patients confirmed to have GC via histological examination, and the pathological staging for each GC sample was classified in accordance with the TNM system[18]; (3) the article must be published in a peer-reviewed journal and provide original data; and (4) the article must supply sufficient information on CDH17 expression. The major exclusion criteria were: (1) article did not satisfy the inclusion criteria designed in the current study; (2) studies turned out to be abstracts, reviews, case report, letters, meta-analyses, or proceedings; (3) duplication publications or studies with overlapping data; and (4) subgroup analysis of the included trials.
A standard reporting form was used to extract data from each included study, with the collected descriptive information including: first author surname and initials, year of submission, country, racial descent, study design, number of cases and controls, demographic variables, CDH17 detection method, CDH17 expression, and confirmation of diagnosis. Two reviewers independently assessed the methodological quality of the included trials using the Newcastle-Ottawa Scale (NOS) criteria to ensure consistency in reviewing and reporting results[19]. Three aspects were considered in the NOS criteria: (1) subject selection: 0-4; (2) subject comparability: 0-2; and (3) clinical outcome: 0-3. NOS scores range from 0 to 9; a score ≥ 7 indicated that the study was of good quality. Disagreement on the inclusion of a single study was settled either by discussion or after consultation with a third investigator.
The association between CDH17 expression and the pathological features of GC was estimated by the odds ratio (OR) and a 95% confidence interval. We used Cochran’s Q-statistic (P < 0.05 was considered significant) and I2 tests to quantify heterogeneity[20]. In order to calculate the pooled ORs, fixed/random effects models were used; a random effects model was applied in the event of significant heterogeneity (P < 0.05 or I2 test exhibited > 50%), while ORs were pooled via the fixed-effects model[21,22]. In the event of significant heterogeneity, subgroup analysis was performed to find potential explanatory variables for the differences. In addition, we employed sensitivity analyses to evaluate whether a single study had the weight to impact the overall estimate. The effect of publication bias was determined via Egger’s linear regression test (P < 0.05 was considered significant), which can be used to evaluate funnel plot asymmetry; an asymmetric plot reveals possible publication bias[23,24]. Statistical analyses were conducted with STATA statistical software (Version 12.0, Stata Corporation, College Station, TX, United States).
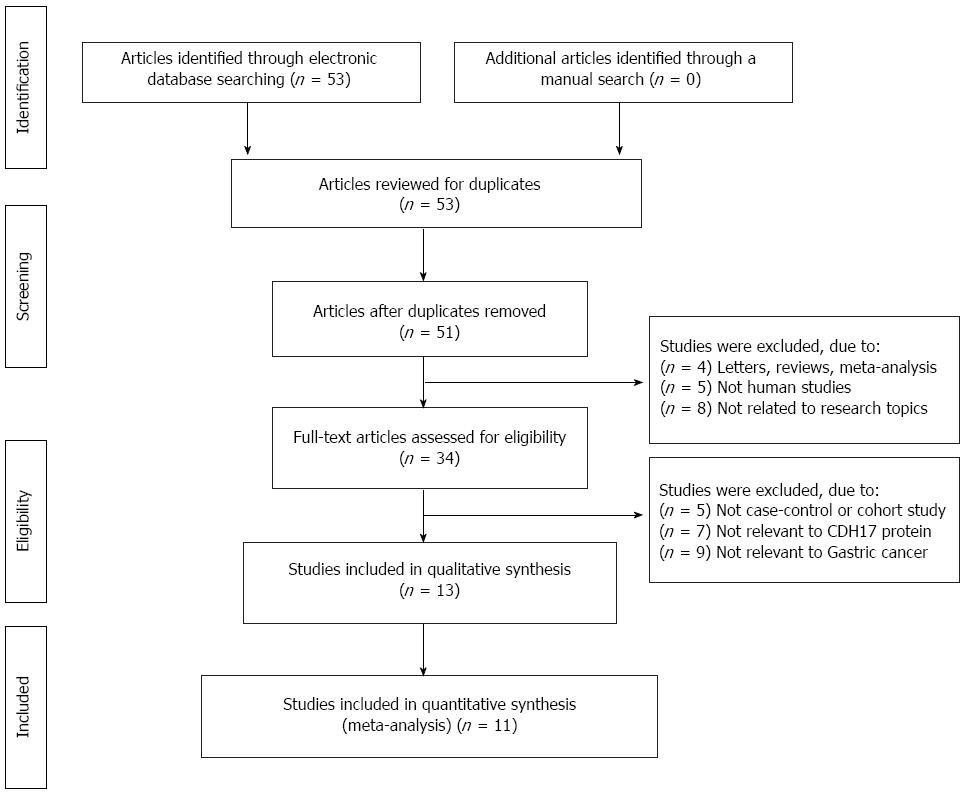
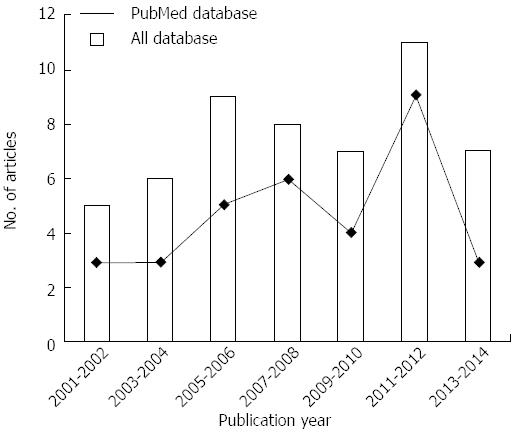
Figure 1 shows the flow chart of identified publications and the main reason for exclusion. Initially, 53 potential articles emerged from the electronic databases. Of the 53 articles, 2 studies were duplicates and thus removed. After title/abstract screening, 17 irrelevant studies were also removed. A further 21 studies were excluded after detailed readings during full text assessment, thereby leaving 13 remaining studies for qualitative analysis. Based on this analysis, 2 additional studies were removed. This left 11 case-controlled studies published between 2007 and 2014 for the meta-analysis[5,8,9,17,25-31] (Figure 2).
The 13 include studies consisted of 2,120 total GC patients with sample sizes ranging from 46 to 440. Sample sizes > 200 were considered “large”. Of the 11 included studies, only one operated within a Caucasian population [United States (Lee HJ)]; the remaining 10 studies were conducted in Asian populations [China (Lin Z, Qiu HB, Wang J, Wang B, Liu SQ, Xu XY, Ge J, and Tian MM), Japan (Sakamoto N), and Korea (Park SS)]. Two studies (Lee HJ and Sakamoto N) did not provide gender information, while six studies (Wang J, Sakamoto N, Wang B, Liu SQ, Lee HJ, and Park SS) failed to obtain age information. There was only one non-Asian study, though it had a large sample size. The detection of CDH17 expression was divided into EnVision and non-EnVision groups (PV, LSAB, SP, and ABC). CDH17 expression in different pathological stages (TNM stage, histologic grade, invasive grade, and LN metastasis) and baseline characteristics for the 11 individual studies are summarized in Table 1.
| Ref. | Year | Country | Sample | Gender (M/F) | Age (yr) | Sample | Method | NOS score |
| Lin et al[17] | 2014 | China | 216 | 150/66 | 65 (32-84) | Tissue | EnVision | 8 |
| Qiu et al[9] | 2013 | China | 156 | 103/53 | 57 (27-78) | Tissue | EnVision | 7 |
| Wang et al[16] | 2012 | China | 191 | 117/74 | - | Tissue | Non-EnVision | 8 |
| Sakamoto et al[5] | 2012 | Japan | 152 | - | - | Tissue | Non-EnVision | 7 |
| Wang et al[30] | 2011 | China | 264 | 157/107 | - | Tissue | EnVision | 8 |
| Liu et al[29] | 2011 | China | 46 | 37/9 | - | Tissue | EnVision | 6 |
| Lee et al[28] | 2010 | United States | 440 | - | - | Tissue | Non-EnVision | 8 |
| Xu et al[27] | 2009 | China | 215 | 169/46 | 57 (24-82) | Tissue | Non-EnVision | 8 |
| Ge et al[35] | 2008 | China | 166 | 109/57 | 52.2 ± 10.2 | Tissue | EnVision | 7 |
| Tian et al[25] | 2007 | China | 66 | 32/34 | 53 (29-91) | Tissue | Non-EnVision | 6 |
| Park et al[8] | 2007 | South Korea | 208 | 135/73 | - | Tissue | Non-EnVision | 8 |
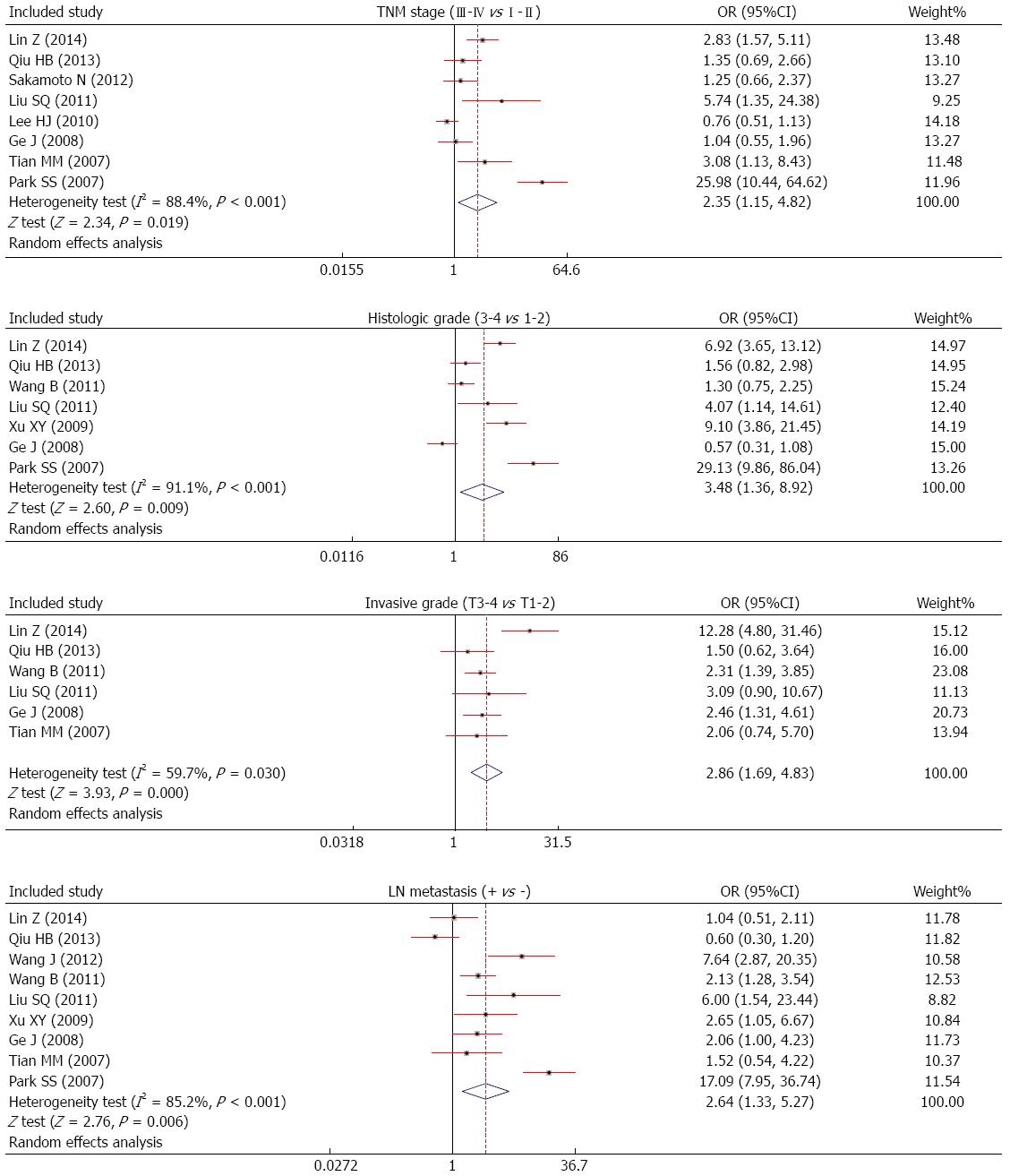
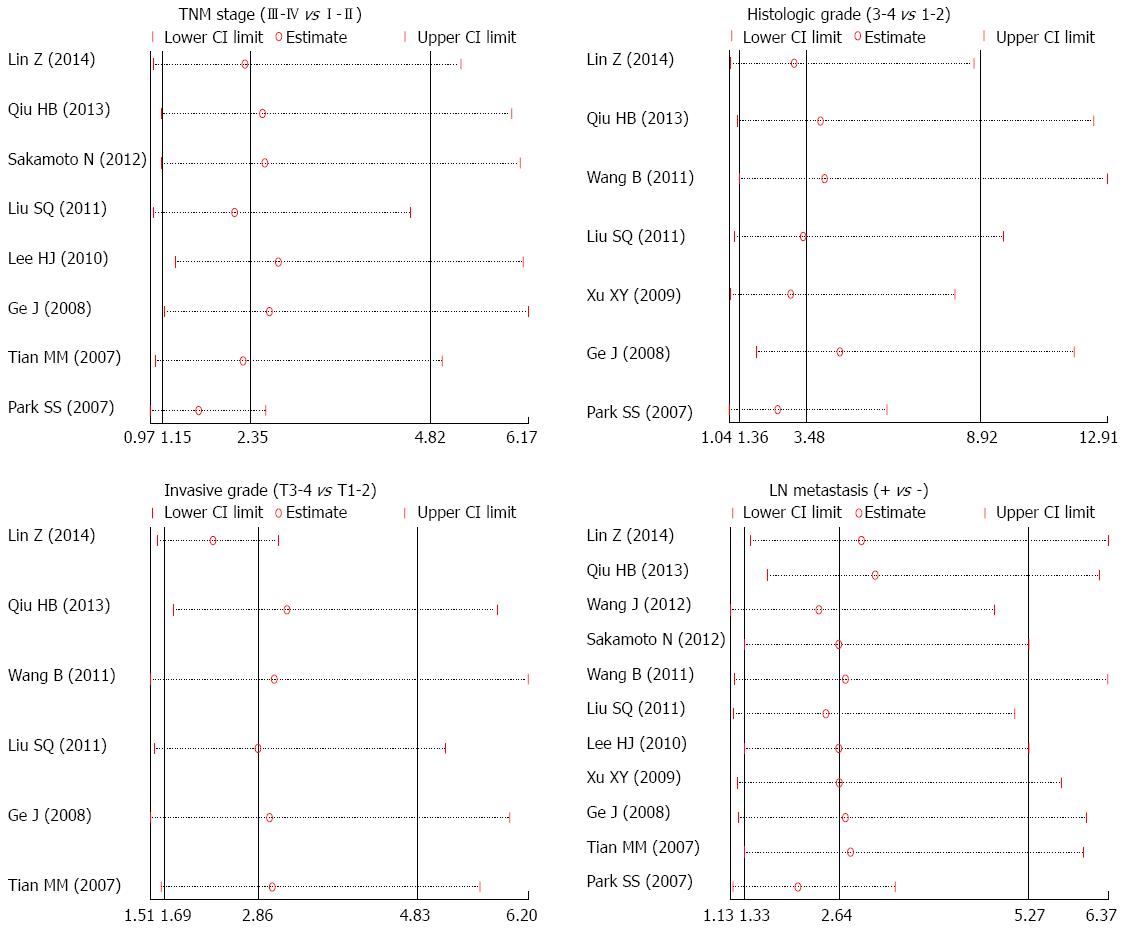
In the meta-analysis, the relationship between CDH17 expression and the pathological features of GC was assessed via the random effect model for observed heterogeneity (TNM III-IV vs I-II: I2 = 88.4%, P = 0.000; histologic grade 3-4 vs 1-2: I2 = 91.1%, P = 0.000; invasive grade: T3-4 vs T1-2: I2 = 59.7%, P = 0.030; LN metastasis: I2 = 85.2%, P = 0.000). Results showed that CDH17 exhibited more positive expression in patients with TNM III-IV staging GC than in those with III-IV staging GC based on the ORs from the combined results of all the included studies (OR = 2.35; 95%CI: 1.15-4.82; P = 0.019). We also examined the role of CDH17 expression in the histologic grade of GC progression, and found that GC tissues from histologic grades 3-4 had higher CDH17 expression than those with histologic grades 1-2 (OR = 3.48; 95%CI: 1.36-8.92; P = 0.009). As for the invasive grade, we found that CDH17 expression was significantly higher in GC tumors with an invasion depth of T3-4 when compared with the T1-2 (OR = 2.86; 95%CI: 1.69-4.83; P = 0.000). Meanwhile, GC tissues with LN metastases had higher CDH17 expression than those with no detectable LN metastases (OR = 2.64; 95%CI: 1.33-5.27; P = 0.006) (Figure 3).
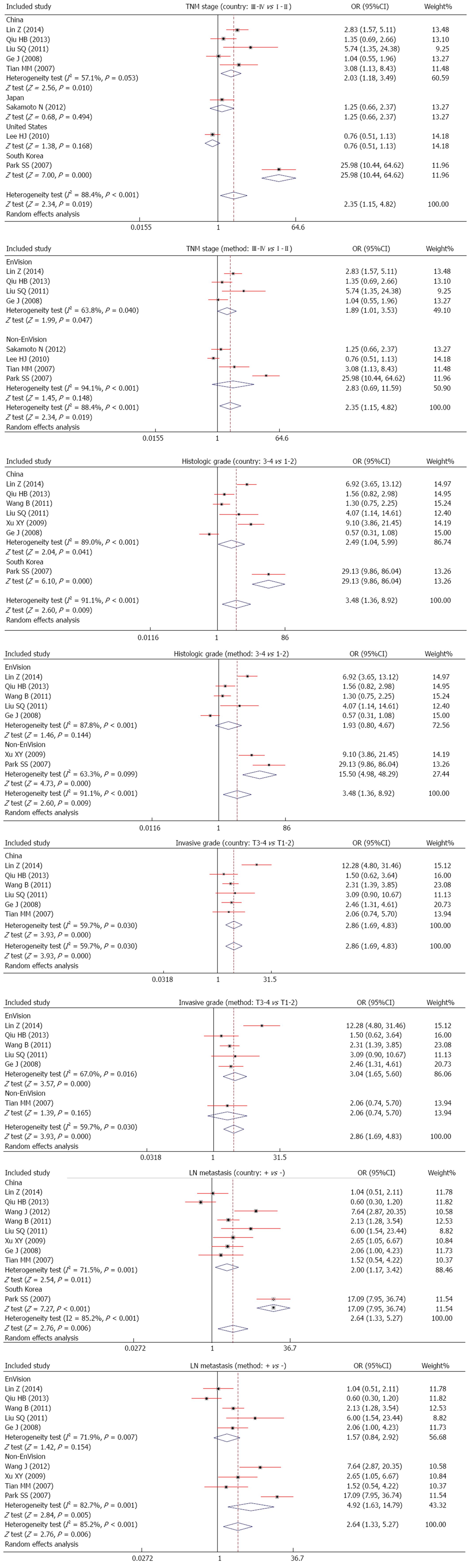
Since heterogeneity was found, the relationship between CDH17 expression and the pathological features of GC were evaluated for subgroups of different explanatory variables. We found that CDH17 expression occurred more frequently in TNM III-IV staging GC than those with I-II staging GC in the China (OR = 2.03; 95%CI: 1.18-3.49; P = 0.010) and Korea subgroups (OR = 25.98; 95%CI: 10.44-64.62; P = 0.000), but not in the Japan (OR = 1.25; 95%CI: 0.66-2.37; P = 0.494) or United States subgroups (OR = 0.76; 95%CI: 0.51-1.13; P = 0.168). In addition, we found positive associations between CDH17 expression and histologic grade of GC in the China (OR = 2.49; 95%CI: 1.04-5.99; P = 0.041) and Korea subgroups (OR = 29.13; 95%CI: 9.86-86.04; P = 0.000). Significant differences in CDH17 expression were also observed between samples with T3-4 grade GC and T1-2 grade GC in the China subgroup (OR = 2.86; 95%CI: 1.69-4.83; P = 0.000). In addition, the results showed significant difference in CDH17 expression between LN metastasis-positive samples and LN metastasis-negative GC samples in both the China (OR = 2.00; 95%CI: 1.17-3.42; P = 0.011) and Korea subgroups (OR = 17.09; 95%CI: 7.95-36.74; P = 0.000).
In the method-classified subgroup analysis, we revealed significant differences in CDH17 expression in GC patients with TNM stage III-IV when compared with those with TNM stage I-II in the EnVision subgroup (OR = 1.89; 95%CI: 1.01-3.53; P = 0.047), but not in the non-EnVision subgroup (OR = 2.83; 95%CI: 0.69-11.59; P = 0.148). Meanwhile, evidence suggested that GC patients with overexpressed CDH17 were associated with a higher histologic grade in the non-EnVision subgroup (OR = 15.50; 95%CI: 4.98-48.29; P = 0.000), but not in the EnVision subgroup (OR = 1.93; 95%CI: 0.80-4.67; P = 0.144). Additionally, the results also indicated that CDH17 expression occurred more frequently in GC patients with a higher invasive grade in the EnVision subgroup (OR = 3.04; 95%CI: 1.65-5.60; P = 0.000), but a similar association was not found in the non-EnVision subgroup (OR = 2.06; 95%CI: 0.74-5.70; P = 0.165). Furthermore, we observed increased CDH17 expression in GC patients with LN-positive metastasis relative to those with LN-negative metastasis in the non-EnVision subgroup (OR = 4.92; 95%CI: 1.63-14.79; P = 0.005), but not in the EnVision subgroup (OR = 1.57; 95%CI: 0.84-2.92; P = 0.154) (Figure 4).
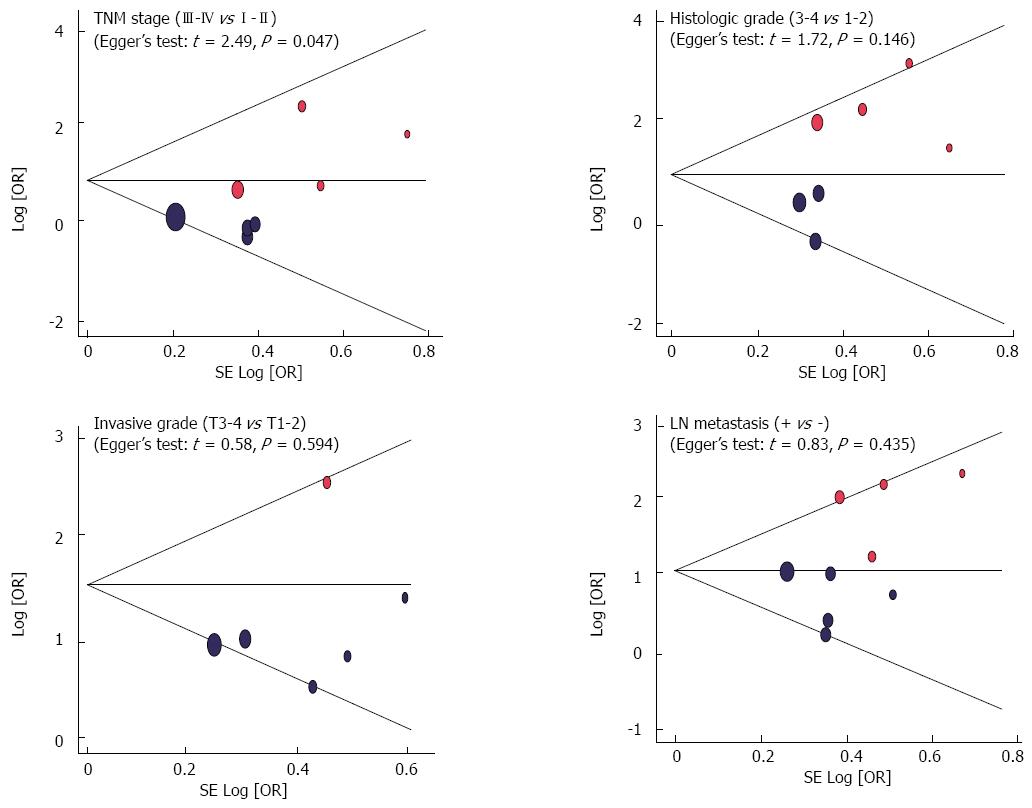
Sensitivity analyses were performed, with the results showing that no single study had the weight to impact the overall estimate of the association between CDH17 expression and the pathological features of GC (Figure 5). We did not observe any obvious asymmetry from the shapes of the funnel plots, and the Egger’s regression test suggested the absence of publication bias, with the exception of the association between CDH17 expression and TNM stage (t = 2.49; P = 0.047); thus, no significant publication bias was detected in the association of CDH17 expression with histologic grade (t = 1.72; P = 0.146), invasive grade (t = 0.58; P = 0.594), or LN metastasis (t = 0.83; P = 0.435) in our systematic reviews (Figure 6).
In this meta-analysis, the relationship between high CDH17 expression and pathological features of GC was observed. From the results, we can conclude there is a significant connection between CDH17 and TNM stages, histologic grade, invasive grade, and LN metastasis of GC. Single-pass transmembrane cadherins are a type of cell adhesion molecule that can regulate adhesion to adjacent cells depending on Ca2+, thereby contributing to homophilic cell adhesion and tumor development[32]. CDH17, a member of the cadherin superfamily that is expressed exclusively on enterocyte basolateral surfaces and intestine goblet cells (but not liver or stomach cells), differs from classic cadherins in structure and function[33]. Different from classic cadherins such as E-, P-, and N-cadherins, CDH17 consists of seven cadherin type repeats without the His-Ala-Val motif of the N-terminal domain, has only 20 amino acid residues for its CDH17 cytoplasmic portion, has a short COOH-terminal for possible cell adhesion function, and displays no homology to classical cadherins which have the highly conserved 150-160 amino acid residues[8]. The independent adhesion function from the cytoskeletal anchorage of CDH17 has no connection with catenins, actins, or other cytoplasmic components; this is vastly different from classical cadherins, suggesting a complementary classical cadherin adhesion function[34]. It has been reported that the high expression of CDH17, as opposed to the low levels of other classical cadherins, is related to gastric cancer, colorectal cancer, liver cancer, pancreatic cancer, and cholangiocarcinoma, suggesting that CDH17 might play an important part in tumor progression[33]. A series of studies have shown that the high expression of CDH17 is linked with the stage of the tumor, histological grade, invasive depth of the tumor, and lymph node metastasis of GC[5,31]. The reason for high CDH17 expression levels in this capacity may be related to the activation of the NFκB signaling pathway, which impacts processes such as p50/p65 heterodimer regulation of the transcription of responsive genes and differentiation of lymphatic endothelium into VEGFs. Relatedly, increased nuclear translocation of p65 in GC has a close relationship with tumor invasion depth and tumor metastases[16]. Another mechanism may involve the Wnt/β-catenin pathway. It was found that the knockdown of CDH17 had the ability to decrease phosphorylation of GSK-3b and β-catenin related with the reduction transactivation activity of TCF/LEF, thus decreasing the expression of cyclin-D1, which is of great importance in promoting cell proliferation and inhibiting cell apoptosis[9,35]. Furthermore, CDH17 over-expression can activate the Ras/Raf/MEK/ERK MAPK signaling pathway, which may regulate cell proliferation, apoptosis, metabolism, and differentiation, which are all processes important in tumor biology[17]. From the above analysis, we may draw the conclusion that the high expression of CDH17 is largely related to the pathological features of GC through three signaling pathways in the cells: the NFκB signaling pathway, the Wnt/β-catenin pathway, and the Ras/Raf/MEK/ERK MAPK signaling pathway. In agreement with our conclusion, Ge et al[26] also found that the expression of CDH17 may play an important part in the development of GC, suggesting a suitable marker for the prognosis of GC.
Given the fact that several factors may affect the linkage between CDH17 expression and pathological features of GC patients, a stratified analysis based on country and detection method was conducted. From the country-stratified analysis, we found no obvious influence in either Chinese or Korean populations in TNM stages, histologic grade, invasive grade, or LN metastasis of GC. In Japan and the United States, however, the relationship was not as obvious. This can be explained by the differences in the environmental backgrounds and gene pools of these different populations. In conclusion, our results are partly in accordance with previous studies that hold that high expression of CDH17 has a typical connection with the pathological features of GC patients.
Our study does have some limitations that merit additional investigation. Firstly, our study is observational research that is cross-sectionally designed. Secondly, the sample sizes in more than half of the total involved articles were relatively small, and the number of patients in some groups was low. In particular, the small patient numbers in the stratified analyses of country and method may detract from the study results. Thirdly, there was a difference in the high/low cut-off values of CDH17 expression levels in the various included studies. The different cut-off values of CDH17 between studies may influence the final results and be responsible for a few inconclusive outcomes. Finally, the existence of heterogeneity may also harm the integrity of results. A large number of the included studies were designed with small sample sizes, six studies lacked complete gender and age information, and the CDH17 expression detection methods were different from each other (EnVision, PV, LSAB, SP, and ABC). In this regard, differences in age, sex, and detection methods may be largely responsible for heterogeneity. Additionally, there was only one non-Asian study, and although it had a large sample size, this might have influenced the scope of our results. Considering the limitations listed above, the results, as well as the analysis, must be interpreted with caution.
In conclusion, the present study identified that CDH17 is an actual oncogene that plays an important role in cell proliferation, tumor growth, invasion, and metastasis in GC. This data may present a novel therapeutic approach in treating GC by targeting CDH17. Our conclusions, however, need to be confirmed due to the aforementioned limitations, via a combination of more and larger sample size publications, which use a consistent definition for cut-off values.
Cadherin-17 (CDH17) was detected to be overexpressed in gastric cancer (GC) and related to tumor incurrence and recurrence, invasion and metastasis, advanced tumor stage, and poor survival in GC patients. To date, the cellular function and signaling mechanisms of CDH17 in GC remain inconsistent.
The cellular function and signaling mechanisms of CDH17 in GC remain inconsistent.
The present study identified that CDH17 is an actual oncogene that plays an important role in cell proliferation, tumor growth, invasion, and metastasis in GC.
These data may present a novel therapeutic approach against GC by targeting CDH17.
Odds ratio (OR) and a 95% confidence interval (95%CI) were used to evaluate specified relationships. The Cochran’s Q-statistic and I2 test were used to evaluate potential heterogeneity among studies.
The review is well written and deals with an important topic. This study found that the cadherin 17 protein is associated with the growth and metastasis of gastric cancer, suggesting a potential of targeted therapy against the protein. The analysis is interesting and important.
| 1. | Brenner H, Rothenbacher D, Arndt V. Epidemiology of stomach cancer. Methods Mol Biol. 2009;472:467-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 374] [Cited by in RCA: 415] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 2. | Tan IB, Ivanova T, Lim KH, Ong CW, Deng N, Lee J, Tan SH, Wu J, Lee MH, Ooi CH. Intrinsic subtypes of gastric cancer, based on gene expression pattern, predict survival and respond differently to chemotherapy. Gastroenterology. 2011;141:476-85, 485.e1-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 273] [Cited by in RCA: 279] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 3. | Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23762] [Cited by in RCA: 25604] [Article Influence: 1706.9] [Reference Citation Analysis (10)] |
| 4. | Singh SR. Gastric cancer stem cells: a novel therapeutic target. Cancer Lett. 2013;338:110-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 77] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 5. | Sakamoto N, Oue N, Sentani K, Anami K, Uraoka N, Naito Y, Oo HZ, Hinoi T, Ohdan H, Yanagihara K. Liver-intestine cadherin induction by epidermal growth factor receptor is associated with intestinal differentiation of gastric cancer. Cancer Sci. 2012;103:1744-1750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Rathbone M, Rathbone B. Helicobacter pylori and gastric cancer. Recent Results Cancer Res. 2011;185:83-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Gomceli I, Demiriz B, Tez M. Gastric carcinogenesis. World J Gastroenterol. 2012;18:5164-5170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 28] [Reference Citation Analysis (0)] |
| 8. | Park SS, Kang SH, Park JM, Kim JH, Oh SC, Lee JH, Chae YS, Kim SJ, Kim CS, Mok YJ. Expression of liver-intestine cadherin and its correlation with lymph node metastasis in gastric cancer: can it predict N stage preoperatively? Ann Surg Oncol. 2007;14:94-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Qiu HB, Zhang LY, Ren C, Zeng ZL, Wu WJ, Luo HY, Zhou ZW, Xu RH. Targeting CDH17 suppresses tumor progression in gastric cancer by downregulating Wnt/β-catenin signaling. PLoS One. 2013;8:e56959. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Gessner R, Tauber R. Intestinal cell adhesion molecules. Liver-intestine cadherin. Ann N Y Acad Sci. 2000;915:136-143. [PubMed] |
| 11. | Ito R, Oue N, Yoshida K, Kunimitsu K, Nakayama H, Nakachi K, Yasui W. Clinicopathological significant and prognostic influence of cadherin-17 expression in gastric cancer. Virchows Arch. 2005;447:717-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Liu LX, Lee NP, Chan VW, Xue W, Zender L, Zhang C, Mao M, Dai H, Wang XL, Xu MZ. Targeting cadherin-17 inactivates Wnt signaling and inhibits tumor growth in liver carcinoma. Hepatology. 2009;50:1453-1463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 102] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 13. | Boo YJ, Park JM, Kim J, Chae YS, Min BW, Um JW, Moon HY. L1 expression as a marker for poor prognosis, tumor progression, and short survival in patients with colorectal cancer. Ann Surg Oncol. 2007;14:1703-1711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 95] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Hirohashi S, Kanai Y. Cell adhesion system and human cancer morphogenesis. Cancer Sci. 2003;94:575-581. [PubMed] |
| 15. | Takamura M, Yamagiwa S, Wakai T, Tamura Y, Kamimura H, Kato T, Tsuchiya A, Matsuda Y, Shirai Y, Ichida T. Loss of liver-intestine cadherin in human intrahepatic cholangiocarcinoma promotes angiogenesis by up-regulating metal-responsive transcription factor-1 and placental growth factor. Int J Oncol. 2010;36:245-254. [PubMed] |
| 16. | Wang J, Kang WM, Yu JC, Liu YQ, Meng QB, Cao ZJ. Cadherin-17 induces tumorigenesis and lymphatic metastasis in gastric cancer through activation of NFκB signaling pathway. Cancer Biol Ther. 2013;14:262-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Lin Z, Zhang C, Zhang M, Xu D, Fang Y, Zhou Z, Chen X, Qin N, Zhang X. Targeting cadherin-17 inactivates Ras/Raf/MEK/ERK signaling and inhibits cell proliferation in gastric cancer. PLoS One. 2014;9:e85296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17:1471-1474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5537] [Cited by in RCA: 6607] [Article Influence: 412.9] [Reference Citation Analysis (0)] |
| 19. | Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8858] [Cited by in RCA: 13578] [Article Influence: 848.6] [Reference Citation Analysis (1)] |
| 20. | Zintzaras E, Ioannidis JP. HEGESMA: genome search meta-analysis and heterogeneity testing. Bioinformatics. 2005;21:3672-3673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 348] [Cited by in RCA: 364] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 21. | Zintzaras E, Ioannidis JP. Heterogeneity testing in meta-analysis of genome searches. Genet Epidemiol. 2005;28:123-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 495] [Cited by in RCA: 559] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 22. | Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539-1558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21630] [Cited by in RCA: 27009] [Article Influence: 1125.4] [Reference Citation Analysis (0)] |
| 23. | Song F, Gilbody S. Bias in meta-analysis detected by a simple, graphical test. Increase in studies of publication bias coincided with increasing use of meta-analysis. BMJ. 1998;316:471. [PubMed] |
| 24. | Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of two methods to detect publication bias in meta-analysis. JAMA. 2006;295:676-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1326] [Cited by in RCA: 1622] [Article Influence: 81.1] [Reference Citation Analysis (1)] |
| 25. | Tian MM, Zhao AL, Li ZW, Li JY. Phenotypic classification of gastric signet ring cell carcinoma and its relationship with clinicopathologic parameters and prognosis. World J Gastroenterol. 2007;13:3189-3198. [PubMed] |
| 26. | Ge J, Chen Z, Wu S, Yuan W, Hu B, Chen Z. A clinicopathological study on the expression of cadherin-17 and caudal-related homeobox transcription factor (CDX2) in human gastric carcinoma. Clin Oncol (R Coll Radiol). 2008;20:275-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Xu XY, Hu NZ, Shi H. Expression of E-cadherin and LI-cadherin in human gastric carcinoma and prognostic significance. Anhui Yike Daxue Xuebao. 2009;44:495-499. |
| 28. | Lee HJ, Nam KT, Park HS, Kim MA, Lafleur BJ, Aburatani H, Yang HK, Kim WH, Goldenring JR. Gene expression profiling of metaplastic lineages identifies CDH17 as a prognostic marker in early stage gastric cancer. Gastroenterology. 2010;139:213-25.e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 127] [Cited by in RCA: 133] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 29. | Liu SQ, Niu JH, Lv Y, Mu LT, Wang TX, Xin GH. The significance protein expression of CDX-2 and LI-cadherin in gastric cancer and benign lesions. Zhongguo Puwai Jichu Yu Linchuang Zazhi. 2011;18:936-941. |
| 30. | Wang B, Zhou CZ, Tang HM, Wang Q, Wen YG, Yu ZH. Expression of liver-intestine cadherin in gastric cancer and its relationship with prognosis. Zhonghua Shiyan Waike Zazhi. 2011;28:714-716. |
| 31. | Wang J, Yu JC, Kang WM, Wang WZ, Liu YQ, Gu P. The predictive effect of cadherin-17 on lymph node micrometastasis in pN0 gastric cancer. Ann Surg Oncol. 2012;19:1529-1534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 32. | Dong WG, Yu QF, Xu Y, Fan LF. Li-cadherin is inversely correlated with galectin-3 expression in gastric cancer. Dig Dis Sci. 2008;53:1811-1817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 33. | Zhang J, Liu QS, Dong WG. Blockade of proliferation and migration of gastric cancer via targeting CDH17 with an artificial microRNA. Med Oncol. 2011;28:494-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 34. | Liu QS, Zhang J, Liu M, Dong WG. Lentiviral-mediated miRNA against liver-intestine cadherin suppresses tumor growth and invasiveness of human gastric cancer. Cancer Sci. 2010;101:1807-1812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 35. | van Roy F. Beyond E-cadherin: roles of other cadherin superfamily members in cancer. Nat Rev Cancer. 2014;14:121-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 328] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Abdel-Salam OME, Shimizu Y, Velayos B S- Editor: Yu J L- Editor: Rutherford A E- Editor: Zhang DN