Published online Aug 28, 2014. doi: 10.3748/wjg.v20.i32.11439
Revised: March 11, 2014
Accepted: April 28, 2014
Published online: August 28, 2014
Processing time: 215 Days and 11.5 Hours
Percutaneous endoscopic gastrostomy (PEG) is a common practice for long-term nutrition of patients who are unable to take oral food. We report of an 85-year old man with a history of recurrent larynx carcinoma and hemicolectomy many years ago due to unknown reason. Laryngectomy was indicated. Preoperatively a PEG was inserted endoscopically after an abdominal ultrasonography without abnormal findings. Few months after PEG insertion, the patient was evaluated for diarrhea and insufficient feeding without signs of infection or peritonism. An upper endoscopy and computed tomography scan confirmed a buried bumper syndrome with migration of the PEG tube into the colon as a rare complication. He underwent successful colonoscopic removal of the internal bumper and closure of the colonic orifice of the fistula with the over-the-scope-clip system (OTSC). OTSC is an endoscopic device for treatment of bleeding, perforation, leak and fistula in the gastrointestinal tract. To the best of our knowledge, this is the first report of the use of OTSC for colonoscopic closure of a gastrocolocutaneous fistula due to a buried bumper syndrome with transcolonic PEG tube migration.
Core tip: We present a case of buried bumper syndrome with percutaneous endoscopic gastrostomy tube migration into the transverse colon that was treated endoscopically using the over-the-scope-clip (OTSC) system for closure. OTSC is a new endoscopic device for treatment of bleeding, perforations, leaks and fistulae in the gastrointestinal tract.
- Citation: Bertolini R, Meyenberger C, Sulz MC. First report of colonoscopic closure of a gastrocolocutaneous PEG migration with over-the-scope-clip-system. World J Gastroenterol 2014; 20(32): 11439-11442
- URL: https://www.wjgnet.com/1007-9327/full/v20/i32/11439.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i32.11439
Percutaneous endoscopic gastrostomy (PEG) tubes are widely used for long-term enteral nutrition for patients who are unable to take oral food, e.g., after head and neck surgery. PEG tube insertion is associated with some potential complications although it is generally considered to be safe[1].
The over-the-scope-clip (OTSC) system (Ovesco Endoscopy AG, Tübingen, Germany) is a new endoscopic device suitable to close perforations[2,3], post-surgical fistulae[3,4] or resection of submucosal tumors[5]. It can also be used as hemostatic tool in gastrointestinal bleeding[6] and for esophageal stent fixation[5]. To the best of our knowledge, in literature there are only case reports or small case series regarding the efficacy and safety[2-8], so far randomized controlled trials are not available.
A rare complication of PEG insertion is a secondary PEG migration from the stomach into the colon[1,9,10]. In our case the migrated PEG was removed via colonoscopy and the fistula was closed with an OTSC.
An 85-year-old man was hospitalized with a recurrent larynx carcinoma and pharyngotracheal fistula after radiotherapy and laser cordectomy. Laryngectomy was indicated. To avoid oral intake, a PEG was planned after an abdominal ultrasonography without abnormal findings. The patient had undergone a laparotomy with right-sided hemicolectomy many years ago. Based on the available records we could not find out the reason for that hemicolectomy.
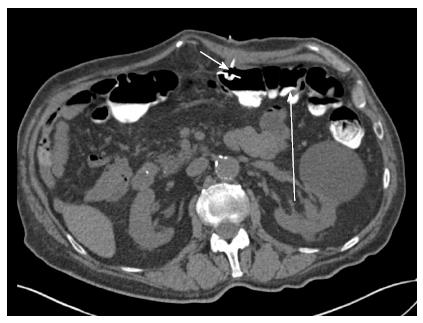
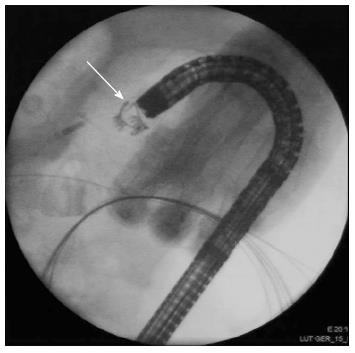
The endoscopic transillumination prior to gastric puncture was not easy to perform. A PEG tube (15 Charrière; Fresenius Kabi Deutschland GmbH, Bad Homburg, Germany) was inserted and the internal bumper placement could be confirmed endoscopically. After one week, peristomal putrid leakage as well as limited in and out movement was reported. The clinical examination revealed neither signs of peritonism nor relevant local infection. The tube could be flushed easily. A plain radiograph and an ultrasonography of the abdomen were normal. In order to prevent recurrent regurgitation two weeks after insertion, a jejunal extension was performed endoscopically, the internal bumper was still correctly placed. Five months later, again putrid leakage beside the PEG tube was observed and it was difficult to flush the gastric port whereas the jejunal port worked properly. Initially the tube could be moved toughly, but then easily, possibly due to a beginning buried bumper syndrome. Ten months after PEG tube insertion the patient was re-evaluated for therapy-refractory diarrhea and insufficient feeding. The upper endoscopy revealed a buried bumper syndrome. The internal bumper was covered with scarf tissue, only a small fistula was present. We carefully inserted an atraumatic guide wire into the gastrostomy tube without resistance, but it was not endoscopically visible. Computed tomography confirmed a buried bumper syndrome with displacement of the internal bumper into the transverse colon (Figure 1). A colonoscopy also revealed the internal bumper in the transverse colon, the colocutaneous fistula measured about 3-4 mm in diameter (Figure 2). The internal bumper was removed with a polypectomy snare (Figure 3). A 1TQ-160 gastroscope (Olympus, Tokyo, Japan) was re-inserted with the mounted and loaded OTSC device (size 12/6 mm type a 10 mm), that was released under suction (Figures 4 and 5). Despite air insufflation no air leaked through the skin. The patient underwent a new PEG and continued PEG feeding. Diarrhea stopped.
The OTSC system shows a great variety of treatment options in the upper and lower GI tract. OTSC application within the colon has been described as successful tool to close anastomotic dehiscence, post-surgical fistulae[4], colovesicular fistulae with diverticulosis, colocutaneous fistulae[2], endoscopic R1 resection of a adenocarcinoma of the sigma[3], perforation after polypectomy[6], endoscopic submucosal dissection[7] as well as acute perforation with gastrointestinal bleeding of the colonic wall one day after PEG[3].
To the best of our knowledge, this is the first report of the use of OTSC for colonoscopic closure of a gastrocolocutaneous fistula due to a buried bumper syndrome with transcolonic PEG tube migration. We decided to close the colonic fistula orifice after colonoscopic removal of the PEG tube because the colonic fistula orifice was greater than the gastric one and the tissue of the colonic wall was easy to suck. Recently, Murino et al[11] also reported a case of gastrocolic fistula secondary to transcolonic PEG tube migration. However, they used the OTSC to close the gastric orifice. Mönkemüller et al[12] successfully closed a gastrocolic fistula in a severely malnourished patient with an OTSC application at the gastrojejunal anastomosis after Billroth II.
After abdominal surgery, in our case laparotomy and right-sided hemicolectomy, the transverse colon can be displaced over the anterior gastric wall. In those settings, the colon can be injured and a gastrocolocutaneous fistula can occur during PEG placement. This potential complication of PEG tube insertion is very rare[1,9,10]. Transcolonic displacement of the PEG tube can present with diarrhea, fecal discharge or rarely without symptoms. Some patients need surgery due to peritonitis or abdominal sepsis[13]. However, a conservative procedure by removal of the tube or colonoscopic clip application can also be successful[14,15].
Some important issues need to be addressed to prevent this complication. Pre- and peri-interventional imaging examinations are essential for adequate prevention. In our case, we performed a pre-interventional abdominal ultrasonography, but this imaging modality is not adequately suitable to detect a colonic interposition. The most important issue is that gastric insufflation and transillumination should be adequate. In this case, transillumination was difficult to obtain. Furthermore, an abdominal fingerprint impression should indent the gastric wall, and a sudden escape of gas or stool using a pilot needle not visible endoscopically indicates the puncture of another structure[1]. Tominaga et al[9] recommend the use of a colonoscope to facilitate the colonic displacement after abdominal surgery.
In conclusion, we report the first use of OTSC for colonoscopic closure of a gastrocolocutaneous fistula due to a buried bumper syndrome with transcolonic PEG tube migration.
An 85-year-old man with a history of percutaneous endoscopic gastrostomy few months ago and right-sided hemicolectomy many years ago presented with diarrhea and insufficient feeding.
Neither signs of peritonism nor fever.
Infection, colitis, malabsorption syndrome, percutaneous endoscopic gastrostomy (PEG) migration, perforation.
Hemoglobin 100 g/L, white blood cell 5 g/L, C-reactive protein 53 mg/L.
Computed tomography confirmed buried bumper syndrome with displacement, localizing the position of the internal bumper in the transverse colon. No free fluid collection or gas intraabdominal.
Colonoscopy revealed the internal bumper within the transverse colon.
The PEG tube was removed with a polypectomy snare and the gastrocolocutaneus fistula was closed colonoscopically with an over-the-scope-clip (OVESCO Endoscopy AG, Tübingen, Germany).
Over-the-scope-clip is a new endoscopic device for closure of lesions in the GI tract.
This report used the over-the-scope-clip system for colonoscopic treatment of a gastrocolocutaneous fistula in a patient with buried bumper syndrome and secondary PEG migration. Important issues are discussed to prevent this very rare complication of PEG tube insertion.
This is an interesting case report that support the utilization of over-the-scope-clip system (OTSC) device for coloscopic closure of a gastrocolocutaneous fistula due to a buried bumper syndrome with transcolonic PEG tube migration. In my opinion this is a very original and useful application of OTSC device.
| 1. | Schrag SP, Sharma R, Jaik NP, Seamon MJ, Lukaszczyk JJ, Martin ND, Hoey BA, Stawicki SP. Complications related to percutaneous endoscopic gastrostomy (PEG) tubes. A comprehensive clinical review. J Gastrointestin Liver Dis. 2007;16:407-418. [PubMed] |
| 2. | Parodi A, Repici A, Pedroni A, Blanchi S, Conio M. Endoscopic management of GI perforations with a new over-the-scope clip device (with videos). Gastrointest Endosc. 2010;72:881-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 128] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 3. | Sandmann M, Heike M, Faehndrich M. Application of the OTSC system for the closure of fistulas, anastomosal leakages and perforations within the gastrointestinal tract. Z Gastroenterol. 2011;49:981-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Manta R, Manno M, Bertani H, Barbera C, Pigò F, Mirante V, Longinotti E, Bassotti G, Conigliaro R. Endoscopic treatment of gastrointestinal fistulas using an over-the-scope clip (OTSC) device: case series from a tertiary referral center. Endoscopy. 2011;43:545-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 100] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 5. | Mönkemüller K, Peter S, Toshniwal J, Popa D, Zabielski M, Stahl RD, Ramesh J, Wilcox CM. Multipurpose use of the ‘bear claw’ (over-the-scope-clip system) to treat endoluminal gastrointestinal disorders. Dig Endosc. 2014;26:350-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 6. | Kirschniak A, Kratt T, Stüker D, Braun A, Schurr MO, Königsrainer A. A new endoscopic over-the-scope clip system for treatment of lesions and bleeding in the GI tract: first clinical experiences. Gastrointest Endosc. 2007;66:162-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 252] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 7. | Nishiyama N, Mori H, Kobara H, Rafiq K, Fujihara S, Kobayashi M, Oryu M, Masaki T. Efficacy and safety of over-the-scope clip: including complications after endoscopic submucosal dissection. World J Gastroenterol. 2013;19:2752-2760. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 101] [Cited by in RCA: 111] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 8. | Weiland T, Fehlker M, Gottwald T, Schurr MO. Performance of the OTSC System in the endoscopic closure of iatrogenic gastrointestinal perforations: a systematic review. Surg Endosc. 2013;27:2258-2274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 117] [Article Influence: 9.0] [Reference Citation Analysis (1)] |
| 9. | Tominaga K, Saigusa Y, Ito S, Hirahata K, Nemoto Y, Maetani I. Percutaneous endoscopic gastrostomy with the aid of a colonoscope to avoid gastrocolic fistula formation. Endoscopy. 2007;39 Suppl 1:E112-E113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Yamazaki T, Sakai Y, Hatakeyama K, Hoshiyama Y. Colocutaneous fistula after percutaneous endoscopic gastrostomy in a remnant stomach. Surg Endosc. 1999;13:280-282. [PubMed] |
| 11. | Murino A, Despott EJ, Vaizey C, Bashir G, Hansmann A, Gupta A, Konieczko K, Fraser C. First report of endoscopic closure of a gastrocolic fistula using an over-the-scope clip system (with video). Gastrointest Endosc. 2012;75:893; discussion 894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Mönkemüller K, Peter S, Alkurdi B, Ramesh J, Popa D, Wilcox CM. Endoscopic closure of a gastrocolic fistula using the over-the-scope-clip-system. World J Gastrointest Endosc. 2013;5:402-406. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Ahmad J, Thomson S, McFall B, Scoffield J, Taylor M. Colonic injury following percutaneous endoscopic-guided gastrostomy insertion. BMJ Case Rep. 2010;2010:pii: bcr0520102976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Hwang JH, Kim HW, Kang DH, Choi CW, Park SB, Park TI, Jo WS, Cha DH. A case of endoscopic treatment for gastrocolocutaneous fistula as a complication of percutaneous endoscopic gastrostomy. Clin Endosc. 2012;45:95-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Lenzen H, Weismüller T, Bredt M, Bahr M. Education and imaging. Gastrointestinal: PEG feeding tube migration into the colon; a late manifestation. J Gastroenterol Hepatol. 2012;27:1254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
P- Reviewer: Kapischke M, Ranieri G, Tsimogiannis K S- Editor: Qi Y L- Editor: A E- Editor: Wang CH