Published online Nov 28, 2013. doi: 10.3748/wjg.v19.i44.8042
Revised: August 14, 2013
Accepted: August 20, 2013
Published online: November 28, 2013
Processing time: 195 Days and 12.4 Hours
AIM: To study the prognosis (recurrence and mortality) of patients with ischemic colitis (IC).
METHODS: This study was conducted in four Spanish hospitals, participants in the Ischemic Colitis in Spain study We analyzed prospectively 135 consecutive patients who met criteria for definitive or probable IC according to Brandt criteria, and follow up these patients during the next five years, retrospectively. Long-term results (recurrence and mortality) were evaluated retrospectively after a median interval of 62 mo (range 54-75 mo).
RESULTS: Estimated IC recurrence rates were 2.9%, 5.1%, 8.1% and 9.7% at years 1, 2, 3 and 5 years, respectively. Five-year survival was 69% (93 of 135) and 24% (10 of 42 patients) died for causes related to the IC. Among these 10 patients, 8 died in their first episode at hospital (4 had gangrenous colitis and 4 fulminant colitis) and 2 due to recurrence.
CONCLUSION: The five-year recurrence rate of IC was low. On the other hand, mortality during follow-up was high and was not associated with ischemic colitis.
Core tip: The prognosis of patients with ischemic colitis is unknown. In this study we observed that recurrence rate of ischemic colitis was low (9.7% at 5 years). However, the mortality was high (31% at 5 years) and the only factor associated with mortality was age.
- Citation: Cosme A, Montoro M, Santolaria S, Sanchez-Puertolas AB, Ponce M, Durán M, Cabriada JL, Borda N, Sarasqueta C, Bujanda L. Prognosis and follow-up of 135 patients with ischemic colitis over a five-year period. World J Gastroenterol 2013; 19(44): 8042-8046
- URL: https://www.wjgnet.com/1007-9327/full/v19/i44/8042.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i44.8042
Ischemic colitis (IC) has been estimated to account for approximately 3 in 1000 of all admissions to tertiary hospitals[1]. In a recent prospective study conducted in 24 spanish hospitals, IC was the reason for 1.28 per 1000 hospital admissions[2]. According to the literature, the incidence in the general population is of 4.5-9.9 cases per 105 people/year and of 44 per 105 people/year for those above 40 years of age[3]. Many cases of IC (reversible forms) are ignored and undiagnosed.
The number of comorbid disorders (≥ 5)[4], location in the right colon[5], and certain clinical onset (gangrenous colitis and/or fulminant pancolitis)[2] are known to be associated with poor prognosis of the disease. However, only a few number of studies, have analysed the long-term prognosis of these patients. The objective of this study was to assess the prognosis (recurrence and mortality) of our patients with IC after first hospital admission.
We assessed the long-term recurrence and mortality of patients in four hospitals participating in the Ischemic Colitis in Spain (CIE) study (San Jorge Hospital in Huesca, Donostia Hospital in San Sebastian, La Fe Hospital in Valencia and Galdakao Hospital in Bizkaia). The CIE study is a prospective multicentre study which consecutively included all patients with diagnosis of IC between March 2005 and December 2006[2].
For our study, patients follow-up was continued until June 2011. Data were obtained retrospectively from the outpatient clinic (gastroenterology and/or surgery) or by telephone using a questionnaire given to the patient and/or their families. The mean follow-up period was 62 mo (54-75 mo).
Patients were categorized as having definitive, probable, or possible IC according to the Brandt criteria[6-8]. The clinical pattern and outcome for each patient was categorised according to Brandt and Boley classification[6]: (1) reversible colopathy; (2) transient colitis; (3) chronic segmental IC; (4) gangrenous colitis; or (5) fulminant universal colitis.
The Ethics Committee of the Clinic Hospital of Barcelona approved the study protocol on 9 June 2005. All patients gave their written consent. The initial study protocol included, in all cases, a colonoscopy before the patient was released from the hospital. A second colonoscopy was not performed in asymptomatic patients and those with reversible colopathy or transient colitis, as these subclasses of disease heal spontaneously.
To compare differences between the groups, the Fisher test was used for qualitative variables and the Student’s t-test for quantitative variables. Differences were considered to be significant when P values were below 0.05.
A total of 135 patients with who met IC criteria were included in the study. The diagnosis of IC was definitive in 74% and probable in 26% of these cases. The average age of our cohort was 73 ± 10 years with a range of 17-90 years, and 50% of them were women. Of the 135 patients included in the study, 51 (38%) were classified with reversible colopathy; 29 (21%) transient colitis; 42 (31%) chronic segmental IC; 9 (7%) gangrenous colitis, and 4 (3%) fulminant universal colitis.
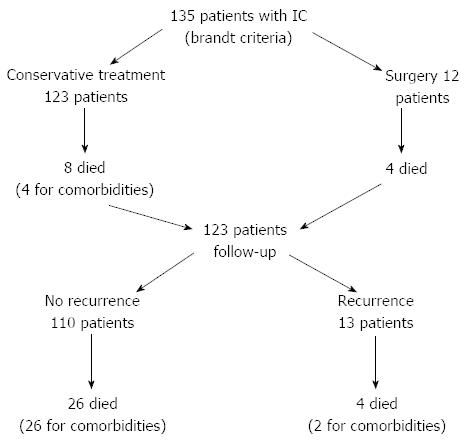
A total of 16 (12%) of the 135 patients had an unfavourable outcome namely death and/or the need for surgery. In the first episode at hospital, 12 patients (8.8%) died, 8 due to IC and 4 due to comorbidities after the acute episode had been solved (1-2 mo after) (Figure 1). Among the 8 who died from IC (3 fulminant universal colitis and 1 gangrenous colitis operated with a subtotal colectomy, and 1 fulminant universal colitis and 3 gangrenous colitis non-operated) the outcome reflected the severity of disease: gangrenous colitis (4/9, 44.4%) and fulminant pancolitis (4/4, 100%).
IC recurred during the follow-up period in 13 (9.7%) of the 123 patients (Tables 1 and 2). Patients with IC recurrence had a similar clinical onset at the first episode at hospital and at relapse. All these patients had colitis not gangrenous and had more frequently vomiting and abdominal pain in the first episode. These were non-grangrenous forms of colitis and located mainly in the left colon. Recurrence occurred in 4, 3, 4, 2 cases through the first, second, third and five year of follow-up, respectively.
| No recurrence (n = 110) | Recurrence(n = 13) | P value | |
| Men/women | 56/54 | 6/7 | 0.8 |
| Age ≥ 65 yr | 91 (83) | 12 (92) | 0.7 |
| Age ≥ 80 yr | 32 (29) | 4 (31) | 1 |
| Hypertension | 66 (60) | 10 (77) | 0.4 |
| Patients under NSAID treatments | 32 (29) | 5 (38) | 0.5 |
| ≥ 3 comorbidities diseases1 | 43 (39) | 4 (31) | 0.8 |
| Location | |||
| Pancolitis | 4 (3) | 0 (0) | 1 |
| ≥ 2 locations | 45 (41) | 5 (38) | 1 |
| Caecum | 6 (5) | 1 (8) | 0.5 |
| Ascending colon | 7 (6) | 1 (8) | 0.6 |
| Hepatic flexure | 8 (7) | 1 (8) | 1 |
| Transverse colon | 8 (7) | 1 (8) | 1 |
| Splenic colon | 23 (21) | 3 (23) | 1 |
| Descending colon | 45 (41) | 2 (15) | 0.08 |
| Sigmoid colon | 74 (67) | 11 (85) | 0.0001 |
| Rectum | 17 (15) | 1 (8) | 0.7 |
| Clinical presentations | |||
| Non-gangrenous | 98 (89) | 13 (100) | 0.8 |
| Gangrenous | 8 (7) | 0 (0) | 0.6 |
| Fulminant | 4 (3) | 0 (0) | 1 |
Considering the course of the 123 patients, 30 (24.3%) of them died within 5 years, 28 due to comorbidities and only 2 due to recurrence and complications of the IC. The only factor that was associated increased mortality was age (72.5 ± 11 years vs 78.6 years; P < 0.001). There were no differences by sex, nonsteroidal anti-inflammatory drugs (NSAIDs) intake or recurrence of colitis. Patients who died had more frequently hypertension 38.8% vs 22.4% (P = 0.06). Among the 2 patients who died of recurrent IC, one, had reversible colitis, two months after stent insertion for chronic mesenteric ischemia, and the other had chronic segmental colitis, after 24 mo of mesenteric angina. The overall five-year survival was 69% (93 of 135 patients).
The patients with chronic segmental IC were followed-up for six months with periodic colonoscopies and/or barium enemas. Of the 42 patients, 30 remained asymptomatic; 6 (14%) developed a stenosis; 3 (7%) had continuing or recurrent bloody diarrhoea and 1 (2%) suffered from persistent or chronic diarrhoea with protein-losing colopathy and serum albumin levels < 2.8 g/L. After six months none of these patients reported complications.
IC is the most common form of intestinal ischemia[9]. It is predominantly observed in elderly patients with varying comorbidities, though younger individuals may also be affected. The mean incidence of autopsy-verified fatal IC has been estimated to be 1.7/105 person years, rising to 23/105 person years in octogenarians[10]. In our study, the average age was 73 years, and clinical onset of IC was observed equally frequent in both women and men.
Clinical presentation in ischemic colitis varies, depending of the severity and extent of the disease. In general, the first symptoms of IC are haematochezia and acute abdominal pain[2,11-14]. Any part of the colon may be affected in IC although the left colon is the predominant location in approximately 75%-85% of patients[12-14]. Splenic flexure is involved in nearly one-quarter of patients[15-17], and isolated right colon ischemia (IRCI) in about 10%-26% of cases[6,17]. Right-sided colonic ischemia tends to be more severe: about 60% of patients require surgery (four or five times more than with colitis in other areas). In our cohort, of the 10 patients with the right colon involved, 6 (5 with gangrenous colitis) required surgery.
It has been estimated that about 20% of patients with acute IC will require surgery with an associated mortality rate of up to 60%[18-21]. In our study, 12 (9%) of the 135 patients underwent surgery, 3 with universal fulminant colitis, 6 with gangrenous colitis, 2 with chronic segmental colitis and 1 with transient colitis. The gangrenous and fulminant universal colitis are associated with poorer prognosis than non-gangrenous forms of IC. Global mortality of IC is of 8%-10%. Gangrenous forms mortality usually reaches 30% and universal colitis is near 100%.
The rate of the recurrence of IC has been reported to be 10%-16% within five years[11,22]. To assess the recurrence, we evaluated the long-term outcomes in our patients (54-75 mo). Thirteen patients had recurrent symptoms. Two of them, one presented chronic segmental colitis and another with transient colitis did not have sigmoid colon involved. There were no statistically significant differences between the clinical presentation of IC and the involvement of different segments of the left colon. The estimated cumulative recurrence rates at years, 1, 2, 3 and 4/5 were 2.9%, 5.1%, 8.1% and 9.7%, respectively.
Some authors[23,24] have recommended that the following studies should be carried out on a prospective basis to assess potential etiologic factors that may increase the likelihood of recurrence: hypercoagulability workup, tests for connective tissue disorders, echocardiogram and holter, and magnetic resonance angiography. In this way, we may be able to detect structural heart diseases, fibromuscular dysplasia and other conditions that may predispose individuals for IC or to recurrence.
The question of whether patients should receive prophylactic treatment for recurrent IC after discharge from the hospital is important. Currently, our efforts should be addressed to control those factors that may contribute to develop IC such as intake of NSAID[25,26] and vasoactive drugs and arterial hypertension.
The limitations of this study are those of a retrospective analysis but prospective follow-up patients. The data collection was made by telephone or at the out-patient clinic and colonoscopy was undertaken only if symptoms were consistent with IC.
In summary, IC is associated with age and occurrence on the right-side markedly increases the risk of severe disease that requires surgery or leads to death. The mortality rate of IC is still high and the recurrence increases with time. In our sample, mortality due to IC at the first admission was 5.9% and 7.4% five years later. The overall rates of mortality, including comorbidities were 8.8% and 31.1% respectively.
CIBERehd is funded by the Instituto de Salud Carlos III.
Ischemic colitis (IC) is the most common form of intestinal ischemia. IC is predominantly observed in elderly patients with varying comorbidities, although younger individuals may also be affected. IC was the reason for 1.28 per 1000 hospital admissions.
Few studies have assessed the long-term prognosis of these patients.
IC is associated with age and occurrence on the right-side markedly increases the risk of severe disease that requires surgery or leads to death. The mortality rate of IC is still high and the recurrence increases with time. In our study, mortality due to IC at the first admission was 5.9% and 7.4% five years later. The overall rates of mortality, including comorbidities were 8.8% and 31.1% respectively.
Patients with ischemic colitis should be monitored continuously to prevent decompensation during follow-up.
It is a clinical series of IC. It is well written.
| 1. | Sotiriadis J, Brandt LJ, Behin DS, Southern WN. Ischemic colitis has a worse prognosis when isolated to the right side of the colon. Am J Gastroenterol. 2007;102:2247-2252. [PubMed] |
| 2. | Montoro MA, Brandt LJ, Santolaria S, Gomollon F, Sánchez Puértolas B, Vera J, Bujanda L, Cosme A, Cabriada JL, Durán M. Clinical patterns and outcomes of ischaemic colitis: results of the Working Group for the Study of Ischaemic Colitis in Spain (CIE study). Scand J Gastroenterol. 2011;46:236-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 96] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 3. | Higgins PD, Davis KJ, Laine L. Systematic review: the epidemiology of ischaemic colitis. Aliment Pharmacol Ther. 2004;19:729-738. [PubMed] |
| 4. | Reissfelder C, Sweiti H, Antolovic D, Rahbari NN, Hofer S, Büchler MW, Weitz J, Koch M. Ischemic colitis: who will survive? Surgery. 2011;149:585-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Brandt LJ, Feuerstadt P, Blaszka MC. Anatomic patterns, patient characteristics, and clinical outcomes in ischemic colitis: a study of 313 cases supported by histology. Am J Gastroenterol. 2010;105:2245-2252; quiz 2253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 127] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 6. | Brandt LJ, Boley SJ. Colonic ischemia. Surg Clin North Am. 1992;72:203-229. [PubMed] |
| 7. | Brandt LJ. Intestinal ischemia. 8th ed. Sleisenger & Fordtran’s. Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. Philadelphia: Elsevier 2006; 2563-2586. |
| 8. | Balthazar EJ, Yen BC, Gordon RB. Ischemic colitis: CT evaluation of 54 cases. Radiology. 1999;211:381-388. [PubMed] |
| 9. | Brandt LJ, Boley SJ. AGA technical review on intestinal ischemia. American Gastrointestinal Association. Gastroenterology. 2000;118:954-968. [PubMed] |
| 10. | Acosta S, Ogren M, Sternby NH, Bergqvist D, Björck M. Fatal colonic ischemia: A population-based study. Scand J Gastroenterol. 2006;41:1312-1319. [PubMed] |
| 11. | Scharff JR, Longo WE, Vartanian SM, Jacobs DL, Bahadursingh AN, Kaminski DL. Ischemic colitis: spectrum of disease and outcome. Surgery. 2003;134:624-629; discussion 629-630;. [PubMed] |
| 12. | Longstreth GF, Yao JF. Epidemiology, clinical features, high-risk factors, and outcome of acute large bowel ischemia. Clin Gastroenterol Hepatol. 2009;7:1075-1080.e1-2; quiz 1023. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 78] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 13. | Añón R, Boscá MM, Sanchiz V, Tosca J, Almela P, Amorós C, Benages A. Factors predicting poor prognosis in ischemic colitis. World J Gastroenterol. 2006;12:4875-4878. [PubMed] |
| 14. | Zou X, Cao J, Yao Y, Liu W, Chen L. Endoscopic findings and clinicopathologic characteristics of ischemic colitis: a report of 85 cases. Dig Dis Sci. 2009;54:2009-2015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 75] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 15. | Elder K, Lashner BA, Al Solaiman F. Clinical approach to colonic ischemia. Cleve Clin J Med. 2009;76:401-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 70] [Article Influence: 4.1] [Reference Citation Analysis (1)] |
| 16. | Taourel P, Aufort S, Merigeaud S, Doyon FC, Hoquet MD, Delabrousse E. Imaging of ischemic colitis. Radiol Clin North Am. 2008;46:909-924, vi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Grubel P, LaMont TH. Colonic ischemia. Available from: http://www.uptodate.com/contents/colonic-ischemia. |
| 18. | Longo WE, Ballantyne GH, Gusberg RJ. Ischemic colitis: patterns and prognosis. Dis Colon Rectum. 1992;35:726-730. [PubMed] |
| 19. | Antolovic D, Koch M, Hinz U, Schöttler D, Schmidt T, Heger U, Schmidt J, Büchler MW, Weitz J. Ischemic colitis: analysis of risk factors for postoperative mortality. Langenbecks Arch Surg. 2008;393:507-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Guttormson NL, Bubrick MP. Mortality from ischemic colitis. Dis Colon Rectum. 1989;32:469-472. [PubMed] |
| 21. | Guivarc'h M, Roullet-Audy JC, Mosnier H, Boché O. [Ischemic colitis. A surgical series of 88 cases]. J Chir (Paris). 1997;134:103-108. [PubMed] |
| 22. | Glauser PM, Wermuth P, Cathomas G, Kuhnt E, Käser SA, Maurer CA. Ischemic colitis: clinical presentation, localization in relation to risk factors, and long-term results. World J Surg. 2011;35:2549-2554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 23. | Koutroubakis IE, Sfiridaki A, Theodoropoulou A, Kouroumalis EA. Role of acquired and hereditary thrombotic risk factors in colon ischemia of ambulatory patients. Gastroenterology. 2001;121:561-565. [PubMed] |
| 24. | Hourmand-Ollivier I, Bouin M, Saloux E, Morello R, Rousselot P, Piquet MA, Dao T, Verwaerde JC. Cardiac sources of embolism should be routinely screened in ischemic colitis. Am J Gastroenterol. 2003;98:1573-1577. [PubMed] |
| 25. | Santolaria S, De Sousa M, Morlans L, Toribio B, Hurtado G, Montoro M. Risk factors for colonic ischemia. A case-control study. Gut. 2007;A303. |
| 26. | Thiéfin G, Beaugerie L. Toxic effects of nonsteroidal antiinflammatory drugs on the small bowel, colon, and rectum. Joint Bone Spine. 2005;72:286-294. [PubMed] |
P- Reviewers: Bao BY, Morris DL, Qin JM S- Editor: Wen LL L- Editor: A E- Editor: Liu XM