Published online Feb 7, 2008. doi: 10.3748/wjg.14.812
Revised: December 3, 2007
Published online: February 7, 2008
Tuberous sclerosis complex (TSC) is a dominantly inherited disorder which characterized by the growth of hamartomatous in multiple organs. Unlike the common development of renal angiomyolipoma, hepatic angiomyolipoma rarely occur in patients with TSC. We report here a patient with hepatic angiomyolipomas and concurrent hepatocellular carcinoma in TSC. This represents the first reported case in English literature. In this patient, multiple hepatic angiomyolipomas were diagnosed with recognition of their fat components and typical clinical settings. Hepatocellular carcinoma in the left liver lobe was definitely diagnosed by US guided biopsy. In such clinical settings, fat containing lesions in liver can be reasonably treated as angiomyolipomas, but non fat containing lesions must be differentiated from hepatocellular carcinoma, imaging guided biopsy can be adopted to confirm the diagnosis.
- Citation: Yang B, Chen WH, Shi PZ, Xiang JJ, Xu RJ, Liu JH. Coincidence of hepatocelluar carcinoma and hepatic angiomyolipomas in tuberous sclerosis complex: A case report. World J Gastroenterol 2008; 14(5): 812-814
- URL: https://www.wjgnet.com/1007-9327/full/v14/i5/812.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.812
Tuberous sclerosis complex (TSC) is a dominantly inherited disorder with a prevalence of 1/6000 to 1/9000 in general population[12]. In patients with TSC, the incidence of renal angiomyolipoma has been reported in up to 80%, but hepatic angiomyolipoma has been less reported[34]. We recently encountered a patient with pathologic proved coincident hepatocellular carcinoma and hepatic angiomyolipomas in TSC. To our knowledge, there is no reported case of hepatic angiomyolipomas with concomitant hepatocellular carcinoma in TSC in English literature. We present here the imaging findings of this case, and discuss the diagnosis and it's practical significance.
A 51 years old woman was admitted in our hospital because of intrahepatic nodules found incidentally by abdominal ultrasonography (US) on general health examination. Her past medical history showed a right nephrectomy for renal angiomyolipomas 16 years prior to this admission. Physical examination revealed multiple miliary russet papilla on her face and several periungual fibroma. A palpable mass was touched with mild knock pain in the left flank. Laboratory analysis showed normal liver function, hepatitis B surface antigen (HBsAg) was positive. Concentration of serum alpha fetoprotein (αFP) was 7694 &mgr;g/mL (normal, < 20 &mgr;g/mL). Urine routine test and renal function were normal.
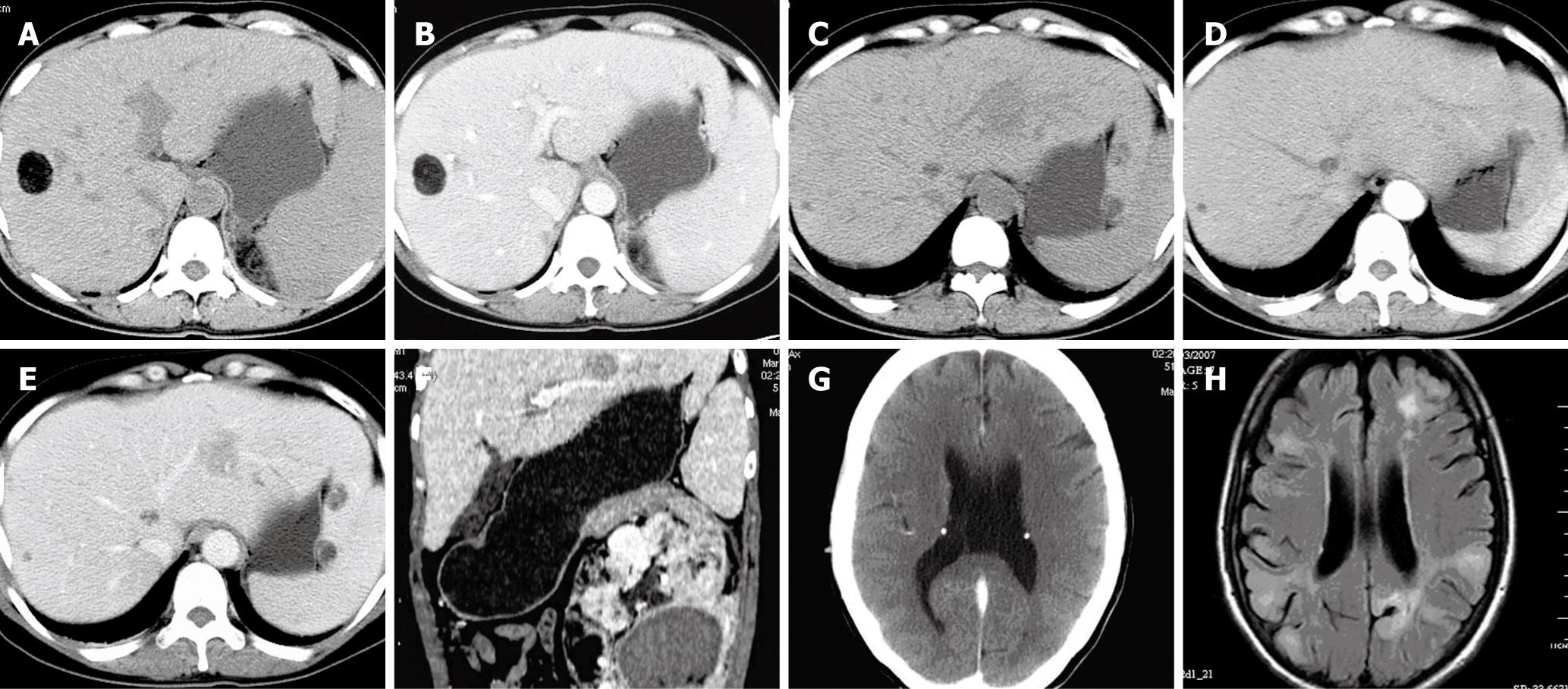
Abdominal US revealed multiple well-circumscribed nodules of various size with homogeneous hyperechoic nodules in the liver, and a hypoechoic nodule in the left liver lobe was noted. Plain helical CT scan showed multiple round well-defined nodules with variable fatty density in the liver (Figure 1A). After administration of intravenous contrast material, the non-fat components of these lesions were enhanced heterogeneously (Figure 1B). Apart from those fat containing lesions, the precontrast CT scan demonstrated a poor defined hypodensity mass with no fat component situated in the left liver lobe (Figure 1C). On dynamic contrast enhanced CT, it presented as nearly homogeneous isodensity in the arterial phase, hypodensity with dotted vessel in the portal venous phase in comparison with the surrounding liver (Figure 1D and E). On coronal reconstruction images, it was adjacent to the left portal vein. Left giant renal heterogeneous mass with fatty density and hemorrhage was found meanwhile (Figure 1F). Based on the abdominal imaging findings and the history of right nephrectomy for renal angiomyolipoma, TSC with multiple organs involved was suggested. Then cerebral CT scan was applied immediately after enhanced abdominal CT scan. Cerebral CT scan demonstrated symmetrical subependymal calcified tuber (Figure 1G). MRI showed multiple cortical tubers with high signal intensity in the bilateral hemisphere, linear and irregular spherical high signal areas from periventricular to subcortical regions in the left occipital and frontal lobes on T2WI and FLAIR sequence (Figure 1H). According to the typical clinical information and imaging findings, TSC with multiple organs involved, multiple angiomyolipomas in liver and left kidney was first considered. But the possibility of concurrent hepatocellular carcinoma can’t be excluded in this patient because of the remarkable increasing concentration of serum alpha fetoprotein (7694 &mgr;g/mL).
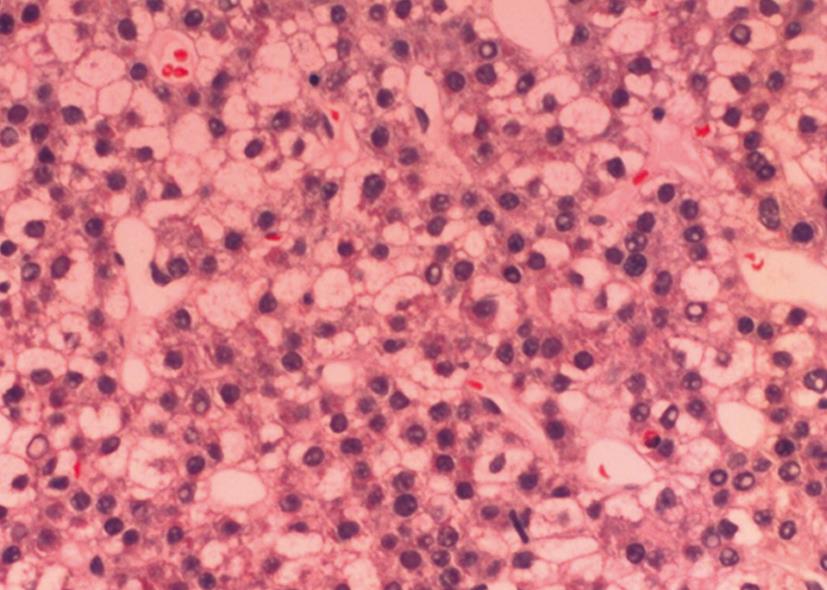
Ultrasound-guided biopsy of the mass with no fat component in the left liver lobe with 18-gauge needle was performed. Histopathological examination of the specimen showed heptocellular carcinoma. Neoplastic cells with eosinophilic cytoplasm were arranged in solid pattern, and inconspicuous sinusoid-like or slit-like blood vessels were noted (Figure 2). Immunohistochemical study showed AFP+, CD34+, HbsAg and HMB45 were negative.
The patient refused to undergo liver resection; ultrasound-guided radiofrequency ablation was performed. CT scan showed complete ablation of the heptocellular carcinoma, and she was uneventful during one year follow up.
TSC is an autosomal dominant disorder involving multiple organs[12]. The mutation of two tumor suppressor genes (TSC1 and TSC2) could account for the pathogenesis of hamartomatous in tuberous sclerosis[5]. In recent literature, hepatic angiomyolipoma has been reported in up to 13%-21% of patients with TSC, especially in female patients with bilateral diffuse renal angiomyolipomas[6]. However, coexistence of hepatocellular carcinoma and hepatic angiomyolipoma is extremely rare [7]. To our knowledge, no report of coincident hepatocellular carcinoma and hepatic angiomyolipomas in TSC exist in English literature.
Angiomyolipoma is a rare benign, non-encapsulated mesenchymal tumor consisting of vessels, smooth muscle and adipose tissue[3]. Hepatic angiomyolipoma is often asymptomatic and found incidentally on imaging studies[6]. In the setting of tuberous sclerosis, hepatic angimyolipomas are often accompanied by bilateral renal angiomyolipomas. Imaging studies play a key role in the diagnosis of hepatic angimyolipoma. On ultrasonography, hepatic angiomyolipomas often presented as multiple well defined, round hyperechoic nodules. Plain CT scan showed them as multiple hypodensity nodules with variable amounts of fatty density. After administration of intravenous contrast material, the non-fat components of these lesions were enhanced heterogeneously. The imaging findings of hepatic angiomyolipoma are similar to those of renal angiomyolipoma. The diagnosis of hepatic angiomyolipoma is often made on recognition of its fat component[6–9].
However, nearly 50% hepatic angiomyolipomas may present as solid mass with least or no fat-component[10]. Plain CT scan usually shows it as well circumscribed, hypodensity nodules. On dynamic contrast CT, it is often heterogeneous hyperdense in the arterial phase, hypodense with prominent central vessel in the portal venous phase. The enhancement pattern of hepatic angiomyolipoma is similar to that of hepatocellular carcinoma, so it's difficult to be differentiated from hepatocellular carcinoma[9–11]. However, no case of concurrent hepatocellular carcinoma and hepatic angiomyolipoma in TSC has been previously reported in the literature. It has even been reported that non-fatty hepatic lesions in TSC can be regarded as hepatic angimyolipomas[611]. In our patient, the imaging findings of multiple hepatic angiomyolpomas with fat component were in accordance with previously reported. The diagnosis of TSC with multiple organs involved was definitely based on the revised clinical diagnostic criteria[1]. But hepatocellular carcinoma can not be excluded in this patient, because the solid mass in the left liver lobe was presented as poor defined and hypovascular, and no fatty density can be found in it on the dynamic contrast enhanced CT. The imaging findings of the solid mass were not in accordance with those of hepatic angiomyolipomas without fat components. In addition, the markedly increasing concentration of serum alpha-fetoprotein strongly suggested the existence of hepatocellular carcinoma. This was confirmed with ultrasound guided biopsy of the solid mass with no fat component in the left liver lobe. Our case suggests that non-fatty hepatic lesions in TSC can’t be regarded as angiomyolipomas arbitrarily, they must be differentiated from hepatocellular carcinoma, because the natural history of hepatic angiomyolipoma is benign, and it needn’t surgery, except for suffer of complications[12], but hepatocellular carcinoma should be removed surgically.
In conclusion, awareness of coincident hepatocellular carcinoma and hepatic angiomyolipomas in TSC is important. When intrahepatic mass with no fat component be found in such clinical setting, the possibility of concomitant hepatocellular carcinoma and hepatic angiomyolipoma should be considered. Imaging studies and laboratory tests can help in the differentiated diagnosis. Imaging guided biopsy can be adopted to confirm the diagnosis.
| 1. | Roach ES, Gomez MR, Northrup H. Tuberous sclerosis complex consensus conference: revised clinical diagnostic criteria. J Child Neurol. 1998;13:624-628. |
| 2. | Maria BL, Deidrick KM, Roach ES, Gutmann DH. Tuberous sclerosis complex: pathogenesis, diagnosis, strategies, therapies, and future research directions. J Child Neurol. 2004;19:632-642. |
| 3. | Casper KA, Donnelly LF, Chen B, Bissler JJ. Tuberous sclerosis complex: renal imaging findings. Radiology. 2002;225:451-456. |
| 4. | Carmody E, Yeung E, McLoughlin M. Angiomyolipomas of the liver in tuberous sclerosis. Abdom Imaging. 1994;19:537-539. |
| 5. | Cheadle JP, Reeve MP, Sampson JR, Kwiatkowski DJ. Molecular genetic advances in tuberous sclerosis. Hum Genet. 2000;107:97-114. |
| 6. | Fricke BL, Donnelly LF, Casper KA, Bissler JJ. Frequency and imaging appearance of hepatic angiomyolipomas in pediatric and adult patients with tuberous sclerosis. AJR Am J Roentgenol. 2004;182:1027-1030. |
| 7. | Chang YC, Tsai HM, Chow NH. Hepatic angiomyolipoma with concomitant hepatocellular carcinomas. Hepatogastroenterology. 2001;48:253-255. |
| 8. | Arslan A, Ciftci E, Cetin A, Selcuk H, Demirci A. Tuberous sclerosis: ultrasound, CT and MRI features of two cases with multiple organ involvement. Australas Radiol. 1998;42:379-382. |
| 9. | Prasad SR, Wang H, Rosas H, Menias CO, Narra VR, Middleton WD, Heiken JP. Fat-containing lesions of the liver: radiologic-pathologic correlation. Radiographics. 2005;25:321-331. |
| 10. | Tsui WM, Colombari R, Portmann BC, Bonetti F, Thung SN, Ferrell LD, Nakanuma Y, Snover DC, Bioulac-Sage P, Dhillon AP. Hepatic angiomyolipoma: a clinicopathologic study of 30 cases and delineation of unusual morphologic variants. Am J Surg Pathol. 1999;23:34-48. |
| 11. | Yoshimura H, Murakami T, Kim T, Nakamura H, Hirabuki N, Sakon M, Wakasa K, Inoue Y. Angiomyolipoma of the liver with least amount of fat component: imaging features of CT, MR, and angiography. Abdom Imaging. 2002;27:184-187. |
| 12. | Guidi G, Catalano O, Rotondo A. Spontaneous rupture of a hepatic angiomyolipoma: CT findings and literature review. Eur Radiol. 1997;7:335-337. |