Published online Jul 21, 2007. doi: 10.3748/wjg.v13.i27.3776
Revised: March 23, 2007
Accepted: March 31, 2007
Published online: July 21, 2007
Bronchoesophageal fistulas are usually diagnosed in the neonatal period. As such, the condition is rare in adults. We present a case of a congenital bronchoesophageal fistula in a 62-year-old man with the complaint of severe bouts of cough and choking after swallowing liquid. His workup included a barium esophagogram that revealed a fistula between the esophagus and a right lower lobe bronchus. The diagnosis should be considered in certain individuals with suggestive symptomatology and unexplained respiratory pathology. The fistula was divided and resected, The patient had an uneventful recovery.
- Citation: Su L, Wei XQ, Zhi XY, Xu QS, Ma T. Congenital bronchoesophageal fistula in an adult: A case report. World J Gastroenterol 2007; 13(27): 3776-3777
- URL: https://www.wjgnet.com/1007-9327/full/v13/i27/3776.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i27.3776
Congenital bronchoesophageal fistula (BEF) is usually associated with esophageal atresia and is readily diagnosed in infancy. But if it is not associated with esophageal atresia, it may persist until adulthood. We present a case of a 62-year-old man with congenital BEF. The patient was treated surgically, with ligation and resection of the fistula. The patient had an uneventful recovery and tolerated a regular diet without coughing at the time of his discharge.
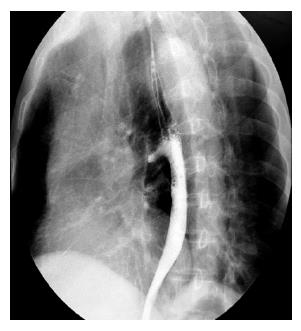
A 62-year-old man was admitted to our hospital with the complaint of severe bouts of cough and choking after swallowing liquid. The patient had done well until 6 mo prior to the admission. The increased symptoms of cough developed. Laryngoscopy showed normal motion of the vocal cords. Bronchofiberscopy revealed no abnormalities. Esophagoscopy showed a depressed lesion that looked as if it was papilla or a dimple without inflammation at a distance of 30 cm from the incisors in the middle intrathoracic esophagus, but the fistula opening was invisible. The barium esophagram demonstrated a fistulous connection between the esophagus and a right lower lobe bronchus (Figure 1). He had no significant medical or surgical history and did not smoke or drink alcohol. His physical exam was unremarkable, as was his admission chest radiograpy, abdominal films, and results of laboratory tests.
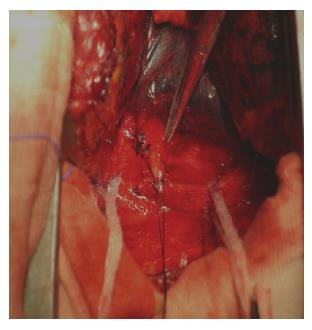
The patient underwent a right posterior lateral thoracostomy. The fistula was identified between the middle intrathoracic esophagus and the right intermediate bronchi. The diameter of the fistula in the patient was 8 mm, with a length of 2.40 cm (Figure 2). There was no evidence of inflammation or adherent lymph nodes around the fistula. The tract was divided and resected, and covered with fibrin glue. Pathological examination of the resected specimen revealed that the fistula was lined by benign squamous epithelium with the muscularis mucosa, and there was no evidence of malignancy, infection, or chronic inflammation. The postoperative course was uneventful. No cough and dysphagia after swallowing liquid in the 7th day after operation.
Congenital BEF or tracheoesophageal fistula (TEF) were first reported by Negus in 1929[1]. These congenital fistulas are still rare in adults[2-5]. Diagnosis can be difficult because of the nonspecific nature of the symptoms. Benign bronchoesophageal fistulas can remain undiagnosed for years. Bouts of coughing when swallowing liquids (Ohno’s sign) are reported to be pathognomonic for this condition and present in 65% of cases[3,4]. The duration of symptoms has been reported to vary from 6 mo to 50 years before diagnosis[2,4,6,7]. One review reported a patient’s condition diagnosed at the age of 83[2]. The congenital nature of the fistula is suggested by the absence of adherent lymph nodes[2] and past or present surrounding inflammation[4], by the presence of a mucosa and definitive muscularis mucosa within the fistulous tract[5], and by the patient’s history[8]. Conventional barium esophagography is considered to be the most sensitive test for diagnosing tracheoesophageal or bronchoesophageal fistula[4-7,9,10]. Esophagoscopy and bronchoscopy may not always demonstrate the fistulous orifice, but these procedures may help us chose modus operandi[2,4,6,7]. CT scanning may be utilized to rule out the presence of a neoplasm and adenopathy and to define the extent of coexisting pulmonary disease, which may need resection[5,7,11].
Braimbridge and Keith[8] classified congenital bronchoesophageal fistulas into four types. In typeI, a fistula is associated with an esophageal diverticulum. Type II consists of a short tract running directly from the esophagus to the bronchus. The type III fistula communicates between the esophagus and a cyst in the lung lobe, and type IV involves a fistula between the esophagus and a sequestered pulmonary segment. Type II is the most prevalent and comprises almost 90% of all cases in some series[2]. Our patient had a simple type II fistula.
The insidious nature of such a fistula may become life threatening, with repeated infection leading to pneumonia, bronchiectasis and abscess formation[5,7,12]. Despite the benign nature of this anomaly, if left untreated, it may lead to fatal complications.
For most cases of fistula formation, surgical management via thoracotomy is the traditional treatment[2,4-7]. The fistula is exposed and divided, and both the defects in the bronchus and the esophagus are repaired with interposition of viable tissue(e.g., pleural or muscular flap) between the suture lines[4,7,10,12]. Pulmonary resection is often needed in patients with coexistent pulmonary disease. The prognosis after surgical repair is excellent. Obliteration of the esophageal orifice with silver nitrate or biological glue is reserved for the patient who cannot tolerate thoracotomy.
Congenital BEF is a rare anomaly in adults. Barium swallow was the most useful diagnostic test. Once a bronchoesophageal fistula is recognized, surgery is the treatment of choice.
| 1. | Azoulay D, Regnard JF, Magdeleinat P, Diamond T, Rojas-Miranda A, Levasseur P. Congenital respiratory-esophageal fistula in the adult. Report of nine cases and review of the literature. J Thorac Cardiovasc Surg. 1992;104:381-384. [PubMed] |
| 2. | Risher WH, Arensman RM, Ochsner JL. Congenital bronchoesophageal fistula. Ann Thorac Surg. 1990;49:500-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Linnane BM, Canny G. Congenital broncho-esophageal fistula: A case report. Respir Med. 2006;100:1855-1857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Kim JH, Park KH, Sung SW, Rho JR. Congenital bronchoesophageal fistulas in adult patients. Ann Thorac Surg. 1995;60:151-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Rämö OJ, Salo JA, Mattila SP. Congenital bronchoesophageal fistula in the adult. Ann Thorac Surg. 1995;59:887-889; discussion 890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Hendry P, Crepeau A, Beatty D. Benign bronchoesophageal fistulas. J Thorac Cardiovasc Surg. 1985;90:789-791. [PubMed] |
| 7. | Aguiló R, Minguella J, Jimeno J, Puig S, Galeras JA, Gayete A, Sánchez-Ortega JM. Congenital bronchoesophageal fistula in an adult woman. J Thorac Cardiovasc Surg. 2006;131:916-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Braimbridge MV, Keith HI. Oesophago-bronchial fistula in the adult. Thorax. 1965;20:226-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 74] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Chiu HH, Chen CM, Mo LR, Chao TJ. Gastrointestinal: Tuberculous bronchoesophageal fistula. J Gastroenterol Hepatol. 2006;21:1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Ford MA, Mueller PS, Morgenthaler TI. Bronchoesophageal fistula due to broncholithiasis: a case series. Respir Med. 2005;99:830-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Nagata K, Kamio Y, Ichikawa T, Kadokura M, Kitami A, Endo S, Inoue H, Kudo SE. Congenital tracheoesophageal fistula successfully diagnosed by CT esophagography. World J Gastroenterol. 2006;12:1476-1478. [PubMed] |
| 12. | Zach MS, Eber E. Adult outcome of congenital lower respiratory tract malformations. Thorax. 2001;56:65-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 42] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
S- Editor Liu Y L- Editor Ma JY E- Editor Lu W