Published online Apr 7, 2007. doi: 10.3748/wjg.v13.i13.2002
Revised: February 15, 2006
Accepted: March 5, 2007
Published online: April 7, 2007
Acute colonic pseudo-obstruction is a poorly understood syndrome, characterized by the signs, symptoms and radiological pattern of a large bowel obstruction without evidence for a mechanical obstruction. We report a case of a 2-year old boy who presented with progressive abdominal distention, vomiting and abdominal pain on postoperative d 3. Plain abdominal Χ-ray showed markedly dilated large bowel. Mechanical colonic obstruction was ruled out with hypaque enema. Ogilvie’s syndrome was suspected. The patient received treatment with oral erythromycin which had an immediate beneficial effect. During the 6 mo follow-up, no recurrences of symptoms were observed. We provide a safe and effective therapy for Ogilvie’s syndrome in pediatric individuals.
- Citation: Jiang DP, Li ZZ, Guan SY, Zhang YB. Treatment of pediatric Ogilvie’s syndrome with low-dose erythromycin: A case report. World J Gastroenterol 2007; 13(13): 2002-2003
- URL: https://www.wjgnet.com/1007-9327/full/v13/i13/2002.htm
- DOI: https://dx.doi.org/10.3748/wjg.v13.i13.2002
Acute colonic pseudo-obstruction (ACPO), also known as Ogilvie’s syndrome, is a disorder characterized by massive dilation of the colon in the absence of mechanical obstruction. William H Ogilvie first observed and reported this rare ileus[1]. It typically occurs in patients with serious illnesses, trauma, burns, surgery and infection. Most cases of it recover after conservative management, but the patient with distended abdomen is at risk of developing cecal perforation, peritonitis and nutritional depletion[2]. We present here the successful treatment of Ogilvie’s syndrome with low-dose erythromycin in a child.
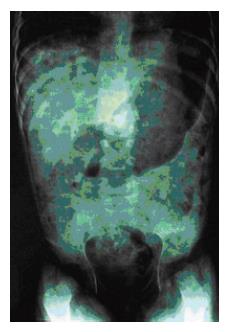
A 2-year old boy was admitted with diagnosis of tuberculosis located at the first lumbar vertebra. After removal of tuberculous foci an acellular bone was fixed. The procedure was performed under general anesthesia and the operation was successful. On postoperative d 3 the patient developed progressive abdominal distention, vomiting and abdominal pain. Physical examination showed that he had a temperature of 37.9°C, a regular pulse of 118 beats/min and poor nutrition. His abdomen was distended and tympanitic to percussion but soft with no tenderness, rebound or guarding. Bowel sounds were present. Laboratory findings were as follows: 10.7 × 109/L white blood cells, 267 × 109/L platelets, 108 g/L hemoglobin, 34 IU/L alanine aminotransferase, 4.3 mmol/L K+, 140 mmol/L Na+, 2.4 mmol/L Ca2, 0.92 mmol/L Mg2+. Plain abdominal Χ-ray showed markedly dilated large bowel (Figure 1). Mechanical colonic obstruction was ruled out with hypaque enema. The diagnosis of Ogilvie’s syndrome was established according to the clinical and radiographic findings.
The patient was treated with intravenous benzyl penicillin, nasogastric decompression and intravenous fluids. Drugs affecting colonic motility were discontinued. When the patient did not respond to 30 h of conservative therapy, nasogastric tube was occluded and oral erythromycin (50 mg four times a day) was started. Within 36 h, the patient began to pass flatus and large volumes of stool with rapid resolution of his abdominal distention. Further radiography and physical examination showed resolution of the colonic pseudo-obstruction. Erythromycin was continued for 3 d with no recurrence of colonic dilation. He recovered with no complication and was discharged in excellent condition. During the 6 mo follow-up, he was well with no gastrointestinal symptoms.
Ogilvie’s syndrome is a severe form of colonic ileus without evidence for mechanical obstruction[3]. Although Ogilvie’s syndrome has been extensively described in the literature, the precise mechanisms underlying acute pseudo-obstruction are still controversial[4]. It often arises in patients with severe infections, retroperitoneal hemorrhage during spinal or pelvic surgery, trauma, burns and narcotic administration[2]. Spinal surgery might contribute to the pathogenesis of the syndrome in our patient. Nausea, vomiting, abdominal pain and abdominal distension are the most common features of Ogilvie’s syndrome. Its diagnosis is sometimes delayed in children, so that many patients are still not properly treated and have a significant mortality[4].
In most cases, conservative management consisting of nasogastric decompression, intravenous fluid, and correction of electrolyte abnormalities can resolve ileus. If unsuccessful, the patient is at risk of developing perforation and colonoscopic decompression is indicated. This method fails in approximately 12%-27% of patients and has a recurrence rate of 18%-33%[5]. It is necessary to find a safe and effective therapy for Ogilvie’s syndrome.
Erythromycin, a macrolide antibiotic, is known to stimulate gastric and small bowel motor activity by binding to the motilin receptor and inducing smooth muscle contraction through a nifedipine-sensitive mechanism[6,7]. However, the short half-life of erythromycin and the rapid onset of tachyphylaxis hamper its broad application in treatment of Ogilvie’s syndrome. There are only a few reports on the efficacy of erythromycin in Ogilvie’s syndrome in adults[8,9]. No recurrence has been observed in these described cases. Neostigmine, an acetyl-cholinesterase inhibitor, has emerged as an effective pharmacyologic alternative for pseudo-obstruction[2]. However, patients eligible for neostigmine must have their potentially mechanical obstruction ruled out. Neostigmine should not be used if a recently sealed-off duodenal or colonic perforation is unplugged by strong peristalsis. The side-effects of cholinesterase inhibitors include salivation, nausea, vomiting, abdominal pain, bradycardia, hypotension and bronchospasm. During the infusion of neostigmine, patients should undergo cardiac monitoring, and atropine should be available. Finally, severely impaired renal function prolongs the elimination of neostigmine.
In conclusion, this report introduces the first successful treatment of Ogilvie’s syndrome with low-dose erythro-mycin in a child. It may be a safe and effective therapy for children with this disorder.
| 1. | Ogilvie WH. William Heneage Ogilvie 1887-1971. Large-intestine colic due to sympathetic deprivation. A new clinical syndrome. Dis Colon Rectum. 1987;30:984-987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 21] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Gmora S, Poenaru D, Tsai E. Neostigmine for the treatment of pediatric acute colonic pseudo-obstruction. J Pediatr Surg. 2002;37:E28. [PubMed] |
| 3. | Singh S, Nadgir A, Bryan RM. Post-cesarean section acute colonic pseudo-obstruction with spontaneous perforation. Int J Gynaecol Obstet. 2005;89:144-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | De Giorgio R, Barbara G, Stanghellini V, Tonini M, Vasina V, Cola B, Corinaldesi R, Biagi G, De Ponti F. Review article: the pharmacological treatment of acute colonic pseudo-obstruction. Aliment Pharmacol Ther. 2001;15:1717-1727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 66] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Saunders MD, Cappell MS. Endoscopic management of acute colonic pseudo-obstruction. Endoscopy. 2005;37:760-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Curry JI, Lander TD, Stringer MD. Review article: erythromycin as a prokinetic agent in infants and children. Aliment Pharmacol Ther. 2001;15:595-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 35] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Costalos C, Gounaris A, Varhalama E, Kokori F, Alexiou N, Kolovou E. Erythromycin as a prokinetic agent in preterm infants. J Pediatr Gastroenterol Nutr. 2002;34:23-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (1)] |
| 8. | Armstrong DN, Ballantyne GH, Modlin IM. Erythromycin for reflex ileus in Ogilvie's syndrome. Lancet. 1991;337:378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 30] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Rovira A, López A, Cambray C, Gimeno C. Acute colonic pseudo-obstruction (Ogilvie's syndrome) treated with erythromycin. Intensive Care Med. 1997;23:798. [PubMed] |
S- Editor Liu Y L- Editor Wang XL E- Editor Che YB