Published online Feb 7, 2006. doi: 10.3748/wjg.v12.i5.822
Revised: August 1, 2005
Accepted: August 3, 2005
Published online: February 7, 2006
We report a rare case of a patient who survived for 5 years after undergoing a medial pancreatectomy for invasive ductal carcinoma originating from the body of the pancreas. A 63-year-old woman was diagnosed as a small cancer of the pancreatic body, and surgery was performed. Even though the tumor was a carcinoma, its small size prompted us to perform a medial pancreatectomy with regional lymph nodes dissection. Additional chemoradiation was performed and, five years after surgery, the patient is well with no signs of recurrence. Medial pancreatectomy for invasive ductal carcinoma has not ever been reported. Furthermore, long-term survival after a lumpectomy for invasive ductal carcinoma has never been reported in the literatures. The current case suggests that long-term survival in patients with invasive ductal carcinoma of the pancreas may be associated with the pathological or biological features of pancreatic carcinoma.
- Citation: Abe H, Tsuneyama K, Tsukada K, Makuuchi M. Five-year survival following a medial pancreatectomy for an invasive ductal carcinoma from the body of the pancreas. World J Gastroenterol 2006; 12(5): 822-824
- URL: https://www.wjgnet.com/1007-9327/full/v12/i5/822.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i5.822
Invasive ductal carcinomas that originate from the body or tail of the pancreas are often unresectable because of unfortunate delays in tumor diagnosis. Most institutions continue to report resection rates for standard surgical procedures and 3-year or 5-year survival rates of no more than 20%[1]. Medial pancreatectomy is a segmental pancreatectomy for the treatment of benign lesions in the neck and body of the pancreas[2]. We report the extremely rare case of a patient who survived for 5 years after undergoing a medial pancreatectomy for invasive ductal carcinoma originating from the body of the pancreas.
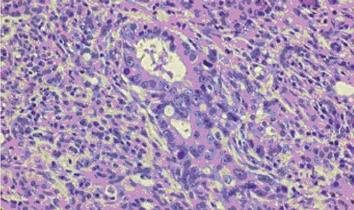
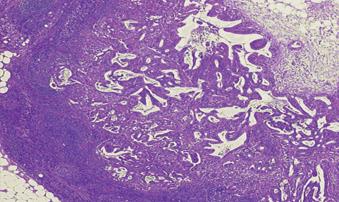
A 63-year-old woman was admitted to our hospital for an evaluation of a dilatation in her main pancreatic duct. She had been diagnosed as having diabetes mellitus at the age of 53 years. Blood sugar control prompted her previous doctor to perform an abdominal computed tomography examination, which showed an apparent dilatation of the main pancreatic duct in the body and tail of the pancreas. Neither contrast-enhanced computed tomography, magnetic resonance imaging nor endoscopic ultrasonography revealed the cause of the dilatation, however, magnetic resonance cholangiopancreaography showed that the main pancreatic duct with beaded dilatation suddenly became occluded in the body of the pancreas. A clinical diagnosis of non-detectable, small cancer of the pancreatic body was made, and surgery was performed. An intraoperative ultrasonography examination depicted a round hypoechoic mass, measuring 1.0 cm in diameter, in the body of the pancreas. No infiltration to the vessels or metastatic lesions was detected. Even though the tumor was a carcinoma, its small size prompted us not to perform a Whipple procedure or a left pancreatectomy. Instead, a medial pancreatectomy, 4 cm along the long pancreatic axis, and an independent dissection of the lymph nodes around the common hepatic artery and proximal splenic artery were performed. The tail of the pancreas was anastomosed using a Roux loop. The tumor was histologically diagnosed as a well-differentiated adenocarcinoma, with a maximum diameter of 1.0 cm (Figure 1); one peripancreatic lymph node containing a metastasis was observed (Figure 2). When examined under low magnification, lymphocyte aggregation around the cancer stroma was observed, immunohistochemically, the tissue stained positive for both CD4 and CD8. The patient’s postoperative course was uneventful; adjuvant chemoradiation was performed for 4 wk. The external-beam radiation doses were delivered using conventional fractionation: 2 Gy, 5 fractions a week. Concomitant chemotherapy was also performed on the first and fifth days of every week (10mg CDDP, 1KE OK432). In addition, she received a 120-h continuous infusion of 625 mg of 5-fluorouracil per week during the radiotherapy. The patient is well with no signs of recurrence five years after surgery.
Many surgeons perform extended radical surgeries, including an extended lymphadenectomy and retroperitoneal soft-tissue clearance, for various stages of pancreatic cancer; however, a survival benefit has not been demonstrated[3]. Even after a curative Whipple resection is performed, adjuvant treatments like radiotherapy and 5-FU treatment are often performed in the USA. So, Jeekel stated that a Whipple procedure was inadequate for pancreatic head cancer and regarded this procedure to be a lumpectomy rather than a curative procedure[4]. A medial pancreatectomy for invasive ductal carcinoma should also be regarded as a lumpectomy.
The main problem associated with performing a medial pancreatectomy is the need for careful patient selection[2]. In the present case, a very small tumor was visualized in the neck or right margin of the body of the pancreas. Preoperatively, evidence suggesting an invasive ductal carcinoma was minimal. The involvement of the main pancreatic duct enabled us to avoid enucleation. In conventional pancreatectomies, a pancreaticoduodenectomy or a near-total left pancreatectomy may be required. To avoid postoperative or late complications from a major pancreatic resection, we performed a medial pancreatectomy and independent lymph-node dissection in the present case. Medial pancreatectomy for invasive ductal carcinoma has not ever been reported. Furthermore, long-term survival after a lumpectomy for invasive ductal carcinoma has never been reported in the literatures, to the best our knowledge.
Large multivariate analyses of resected pancreatic adenocarcinoma have proven that lymph node metastasis serve as prognostic features, however, Fortner et al [5] reported that the presence of lymph node metastasis did not significantly influence survival after regional pancreatectomies for various stages of pancreatic cancer. In tumor biology, the existence of carcinoma cells in a lymph node is regarded as indicating metastatic invasion through the lymphatic ducts out of primary organ. In the present case, the peripancreatic lymph-node metastasis did not preclude long-term survival. Thus, long-term survival may not be precluded by the presence of lymph node metastasis, otherwise, extended radical surgery can not contribute to the treatment of metastatic invasion through the lymphatic ducts. The prognosis of patients with invasive ductal carcinoma of the pancreas who have survived for 5 years may be the same, regardless of whether an extended radical surgery or a lumpectomy is performed.
Many patients with even stage I diseases have recurrences after resection. Fortner et al [5] reported in 1996 that the 5-year survival rate after a regional pancreatectomy was 33% in 12 patients with ductal adenocarcinoma of the pancreatic head, in whom the tumor measured 2.5 cm or less in diameter. Some patients with advanced diseases, however, have survived longer than 5 years after their initial treatment. The pathological and biological features of the 5-year survivors varied.[6] In the present case, peritumoral lymphocyte aggregation was observed, and CD4 + and CD8 + T cells were noted using immnohistochemistry. Fukunaga et al [7] reported that the presence of CD4 + and CD8 + T cells in pancreatic adenocarcinoma serves as a good indicator of a favorable outcome after surgical treatment.
In summary, we report a patient with invasive ductal carcinoma from the body of the pancreas that survived for more than five years after undergoing a medial pancreatectomy. The current case suggests that complete surgical extirpation of early-stage carcinomas of the pancreas accompanied with adjuvant therapy can be long-term survival may be associated with the pathological or biological features of pancreatic carcinoma.
| 1. | Ozawa F, Friess H, Künzli B, Shrikhande SV, Otani T, Makuuchi M, Büchler MW. Treatment of pancreatic cancer: the role of surgery. Dig Dis. 2001;19:47-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Rotman N, Sastre B, Fagniez PL. Medial pancreatectomy for tumors of the neck of the pancreas. Surgery. 1993;113:532-535. [PubMed] |
| 3. | Pedrazzoli S, DiCarlo V, Dionigi R, Mosca F, Pederzoli P, Pasquali C, Klöppel G, Dhaene K, Michelassi F. Standard versus extended lymphadenectomy associated with pancreatoduodenectomy in the surgical treatment of adenocarcinoma of the head of the pancreas: a multicenter, prospective, randomized study. Lymphadenectomy Study Group. Ann Surg. 1998;228:508-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 519] [Cited by in RCA: 576] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 4. | Jeekel J. Adjuvant or neoadjuvant therapy for pancreatic carcinoma. Digestion. 1997;58:533-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Fortner JG, Klimstra DS, Senie RT, Maclean BJ. Tumor size is the primary prognosticator for pancreatic cancer after regional pancreatectomy. Ann Surg. 1996;223:147-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 163] [Article Influence: 5.4] [Reference Citation Analysis (1)] |
| 6. | Conlon KC, Klimstra DS, Brennan MF. Long-term survival after curative resection for pancreatic ductal adenocarcinoma. Clinicopathologic analysis of 5-year survivors. Ann Surg. 1996;223:273-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 539] [Cited by in RCA: 548] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 7. | Fukunaga A, Miyamoto M, Cho Y, Murakami S, Kawarada Y, Oshikiri T, Kato K, Kurokawa T, Suzuoki M, Nakakubo Y. CD8+ tumor-infiltrating lymphocytes together with CD4+ tumor-infiltrating lymphocytes and dendritic cells improve the prognosis of patients with pancreatic adenocarcinoma. Pancreas. 2004;28:e26-e31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 368] [Cited by in RCA: 418] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
S- Editor Guo SY L- Editor Elsevier HK E- Editor Cao L