Published online Dec 28, 2006. doi: 10.3748/wjg.v12.i48.7869
Revised: September 28, 2006
Accepted: November 27, 2006
Published online: December 28, 2006
AIM: To assess CT manifestations and its diagnostic value for lymphoma in the abdominal lymph nodes (LALN).
METHODS: CT findings in 52 cases of LALN proved by surgery or biopsy, including Hodgkin’s disease (HD) in 16 cases and non-Hodgkin’s lymphoma (NHL) in 36 cases, were retrospectively analyzed.
RESULTS: (1) CT manifestations based on distribution of the lesions of LALN: Solitary mass type was found in 10 cases, including solitary, round, uniform-density, enlarged lymph nodes in 3 cases; and multiple, enlarged lymph nodes fusing into singular lobular mass in 7 cases. Thirty-four cases of multiple-nodular type showed multiple, round, enlarged lymph nodes with uniform density and clear margins. Vessels-embedded signs, including mesenteric vessels, renal vessels, abdominal aorta or inferior vena cava, were seen in 6 cases, and duodenum-embedded signs were seen in 2 cases. Eight cases of diffuse type showed characteristic “cobblestone signs”. (2) CT manifestations correlated with pathological type: CT manifestations of 12 cases of HD were different from those of 40 cases of NHL in distribution, size, quantity and fused lesion of enlarged lymph nodes. (3) Twenty-eight cases of 52 patients were accompanied with extra-nodal lymphoma in the abdomen, especially gastrointestinal lymphoma, which had characteristic CT findings. (4) In follow-up examinations, CT images showed uniform, heterogeneous or rim enhancement in 15 cases, and occasional calcifications accompanied with reduction of the lesion size and quantity in 12 cases, whereas the lesions disappeared in 3 cases after treatment.
CONCLUSION: CT images show many characteristic manifestations valuable for qualitative diagnosis of LALN, and it is also helpful for pathological classification of LALN and therapeutic evaluation in follow-up of patients.
- Citation: Yu RS, Zhang WM, Liu YQ. CT diagnosis of 52 patients with lymphoma in abdominal lymph nodes. World J Gastroenterol 2006; 12(48): 7869-7873
- URL: https://www.wjgnet.com/1007-9327/full/v12/i48/7869.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i48.7869
Abdominal lymphoma is clinically not uncommon and lymphoma in the abdominal lymph nodes (LALN) is most frequently encountered[1]. Though it may be part of a systemic lymphoma, single onset of LALN is not rare. LALN can be divided into Hodgkin’s disease (HD) and non-Hodgkin’s lymphoma (NHL). HD is seldom seen in China[2-3] and mostly occurs in middle-aged and young people. The number of NHL patients is larger than that of HD with a diffuse distribution in age. In addition, AIDS patients are more susceptible to NHL[4].
CT is useful for diagnosis[1-2,5-14] and staging[15-21] of abdominal lymphomas. For evaluation of lymph node involvement, the sensitivity of contrast-enhanced CT is 88%, and specificity is 86%. For evaluation of organ involvement, the sensitivity of contrast-enhanced CT is 50%, and specificity is 90%[15]. To our knowledge, however, CT classification of LALN has not been reported in previous documents. We reviewed retrospectively CT findings of 52 patients with LALN confirmed by pathology and histology from 2000 to 2005 in our hospital, and analyzed its value in diagnosis, pathological classification and therapeutic assessment of LALN.
Of the 52 LALN patients, 29 were males and 23 females, with age ranging from 18 to 77 years (mean, 43.4 years), including Hodgkin’s disease (HD, age range 18-59 years, mean 34.6 years) in 12 cases and non-Hodgkin’s lymphoma (NHL, age range 20-77 years, mean 47.3 years) in 40 cases. The diagnosis was confirmed by surgery (20 cases) and lymph node biopsy (32 cases) including peripheral lymph nodes (19 cases) and abdominal lymph nodes (13 cases). The duration of symptoms ranged from 1 to 18 mo. All the patients had evident improvement in clinical symptoms and signs, and reduction in size of the lesions or disappearance of the lesions after chemotherapy and radiotherapy.
Twenty patients were performed with a Somatom HiQ CT machine (Siemens Medical Systems, Forchheim, Germany) and 32 patients were performed with a 4-detector row CT machine (Volume Zoom, Siemens Medical Systems, Forchheim, Germany). All patients were in routine fasting states. Some patients were given 1000-1500 mL of diluted iodinated contrast medium (10 g/L meglumine diatrizoate) orally 60-90 min before scanning. Scan scope ranged from the dome of diaphragm to symphysis pubica. All patients were examined with plain scanning at first and then examined using Ultravist (Schering, Berlin, Germany) 80 mL for enhanced scanning, with a section thickness of 10 mm and internal of 10 mm (Somatom HiQ CT machine) or 1.5 mm section thickness, a pitch of 1.25, 5 mm reconstruction interval (4-detector row CT machine).
Solitary mass type: Ten cases of solitary mass type of LALN were located in the retroperitoneum, mesenterium and lesser omentum. Of them, 3 cases on CT plain scanning showed solitary, round, enlarged lymph nodes of uniform-density with diameters of 3.2-5.8 cm. The lesions had rim enhancement in one case and slight homogeneous enhancement in 2 cases on enhanced CT. The other 7 cases showed multiple enlarged lymph nodes fusing into lobular masses with diameters of 7.8-18 cm and clear margins, of which 5 cases showed uniform density and 2 cases showed heterogeneous density on plain CT. Enhanced CT showed slight uniform enhancement in 4 cases, and heterogeneous enhancement in 3 cases. Of the all cases, the mesenteric vessels, abdominal aorta and inferior vena cava were embedded (vessels-embedded signs) in 3 cases (Figure 1).
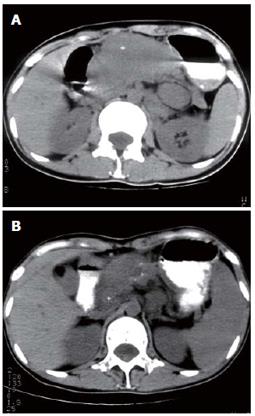
Multiple nodular type: Thirty-four cases were of multiple nodular type of LALN, which referred to regional distribution of lymph nodes. CT showed multiple, round, enlarged lymph nodes with clear margins and uniform density in the abdomen (Figure 2). Most enlarged lymph nodes were over 1.0 cm in diameter with exception of 2 cases of less than 1.0 cm, which located in the mesenterium. Among the 34 cases, 29 showed slight uniform enhancement, and 5 appeared slight uniform enhancement accompanied with rim enhancement after contrast administration. Nineteen cases revealed a fusion of lesions of different degrees and 6 cases showed embedding of vessels (vessels-embedded signs), including the mesenteric vessels (3 cases) (Figure 3), renal vessels (3 cases), abdominal aorta (2 cases) and inferior vena cava (1 case), and 2 cases showed embedding of the horizontal segment of the duodenum (duodenum-embedded signs).
Diffuse type: The diffuse type of LALN involved the whole distribution areas of abdominal lymph nodes, mainly in the mesenteric and retroperitoneal regions in eight cases. CT revealed diffuse, round, non-confluent, enlarged lymph nodes with homogeneous density and clear margins, forming the characteristic “cobblestone signs” named by us. All the enlarged lymph nodes were slightly homogeneously enhanced after contrast administration (Figure 4).
HD: Twelve cases of HD included solitary mass type and diffuse type in one case each (8.3%, respectively), and multiple nodular type in 10 cases (83.4%). The enlarged lymph nodes were mainly distributed in the lesser omentum and retroperitoneal region adjacent to the abdominal aorta (Figures 2 and 5) and inferior vena cava. All the enlarged lymph nodes showed homogeneous enhancement except one rim enhancement after contrast administration. Among the 12 cases, only one case (8.3%) involved the mesenteric lymph nodes, which showed scattered distribution of lesions and a small number of lymph node involvement with less than 2.0 cm in size. Two cases (16.7%) had confluence of lesions and 7 cases (58.3%) showed involvement of other abdominal organs (Figure 5).
NHL: Forty cases of NHL included solitary mass type (9 cases, 22.5%), multiple-nodular type (24 cases, 60%) and diffuse type (7 cases, 17.5%) (Figure 4). All the abdominal lymph nodes were involved, including 18 cases (45%) of mesenteric involvement. Among the 40 cases, 24 (60%) showed a fusion of the enlarged lymph nodes of different degrees, appearing as lobular masses (Figures 1 and 6); 4 exhibited embedding of vessels (Figures 1 and 3) and 2 had involvement of the intestine. Twenty-one cases (52.5%) were accompanied with involvement of other abdominal organs.
In follow-up, CT was performed in 15 cases of LALN after chemo-radiotherapy, of which abdominal enlarged lymph nodes completely disappeared in 3 cases. The lesion size was reduced by different degrees in 12 cases, including 9 cases with homogeneous density and 3 cases with heterogeneous density, and one case with flecked calcification (Figure 6).
Of the 52 cases of LALN, 28 involved other abdominal organs. Among the 28 cases, intestinal tract lymphomas (13 cases) showed notable circular thickening of the intestinal wall (25-38 mm, Figure 7) in 9 cases, including 2 cases with distinct dilation of intestinal cavity and one case with coexistence of narrowing and dilation of intestinal cavity, resulting in incomplete intestinal obstruction. The other 4 cases of intestinal lymphomas developed lobular masses with uneven margins in intestinal cavity. The CT manifestations of hepatic (7 cases) and splenic (6 cases) lymphomas were solitary or multiple nodular, low-density lesions (Figure 5). Ten cases of gastric lymphomas appeared notable circular thickening of gastric wall (22-33 mm). Renal lymphomas and adrenal gland lymphomas (2 cases each) were characterized by bilateral masses of both kidneys and adrenal glands. Involvement of the peritoneum and omentum (2 cases) resulted in a large amount of ascites (Figures 1 and 2) and omental cakes.
CT plays an important role in the diagnosis and staging of abdominal lymphomas. Based on the CT features of LALN, we classified LALN into solitary mass type, multiple-nodular type and diffuse type.
Solitary mass type of LALN included singular enlarged lymph nodes and fusion of multiple enlarged lymph nodes (most cases). CT featured a huge round mass or a lobular homogeneous density mass with uniform enhancement.
Multiple-nodular type of LALN, the most frequently seen, was characterized by enlarged lymph nodes with regional distribution. Parts of enlarged lymph nodes were fused together and formed a huge mass. CT showed uniform density lesions with mild homogenous enhancement. Sometimes coexistence of mild homogenous enhancement and rim enhancement was also observed, but fully rim enhancement of all lesions was rarely seen.
All the lesions of solitary mass or multiple-nodular type had clear margins. The vessels such as mesenteric vessels, renal vessels, abdominal aorta, and inferior vena cava could be imbedded by the fused multiple enlarged lymph nodes forming the unique “vascular-imbedded signs”[5,6], which were commonly seen in multiple-nodular type. The “duodenal-imbedded signs”, named by us and found in multiple-nodular type, could be induced by LALN due to rich lymphoid tissues in the horizontal segment of the duodenum, which was different from intestinal lymphomas in CT manifestations. The former was marked by narrowing of the intestinal cavity surrounded by the fusion of multiple small nodular lesions with a streak appearance and the latter was manifested as circular thickening of intestinal wall and sometimes complicated with intestinal distension. Therefore, “intestinal-imbedded signs” have an important value for the diagnosis of LALN, although this was not reported in previous documents.
The CT features of diffuse type were diffuse but non-confluent enlarged lymph nodes in the mesenteric and retroperitoneal region with uniform density and cobblestone appearance, named as “cobblestone signs”. It has an important value for the diagnosis of diffuse type of LALN because it has not been seen in other diseases. Moreover, the retroperitoneal lymph nodes below the level of lumbar 2-3 vertebrae were frequently involved (HD 94%, NHL 89%, respectively), which is of great importance in the differential diagnosis with tuberculous lymph nodes [1,6].
The above classification of CT manifestations into 3 types in LALN can not only help in the radiographic diagnosis of LALN but also guide the clinical management of LALN, e.g. the scope of radiotherapy.
LALN is frequently associated with abdominal extra-nodular lymphomas, and about 54% patients had gastrointestinal tract involvement[4]. This is of significance in the diagnosis of LALN, particularly lymphomas of the gastrointestinal tract, which have a high morbidity and show characteristic circular thickening of gastrointestinal wall with notable distension of intestinal cavity on CT. More than half of the patients in this series were associated with gastrointestinal lymphomas. In addition, the association with other solid organ lymphomas such as the liver and spleen is also helpful for the diagnosis. The peritoneum and omentum are seldom involved by LALN[7-11]. There were 2 cases in this series and CT showed a large amount of ascites and omental cakes.
CT findings of HD are different from those of NHL. According to the literature and this report[6,14], we summarize the differences as follows: The enlarged lymph nodes of HD are rarely seen in the mesentery, less than 5%[14], 8.3% in this paper, with a small number of small lesions distributed dispersedly. The confluence of enlarged lymph nodes of HD is seldom seen (16.7%), which mainly occurs in multiple-nodular type (60%). NHL has a wide distribution including all sites of abdominal lymph nodes, and the mesentery is frequently involved (45%). The fusion of enlarged lymph nodes is common (60%), showing vessel-imbedded signs, intestinal-imbedded signs and cobblestone signs. NHL is seen not only in the multiple-nodular type (60%), but also in nearly all of the diffuse type and solitary type (22.5%, 17.5%, respectively).
The CT manifestations of LALN before radio-chemotherapy are different from those of LALN after treatment[22], including reductions in extent of lesions and changes in internal nodal characteristics. The CT features of LALN after treatment are characterized by the reduction in the number of enlarged lymph nodes and the shrinkage of lesions. Though most enlarged lymph nodes remain uniform density on CT, an evident increase in heterogeneous or rim enhancement of lesions may occur due to intra-nodular necrosis after treatment and calcifications of lesions may occur in individual cases[5]. The results of this series revealed that 20% lesions disappeared after radio-chemotherapy and most of these occurred in multiple-nodular type with relative concentration of enlarged lymph nodes. Therefore, CT is valuable for the evaluation of therapeutic efficacy of radio-chemotherapy and helps guide the following treatment.
Lymph node tuberculosis: Lymph node tuberculosis may be easily confused with lymphomas and should be considered emphatically. Lesions of lymph node tuberculosis are relatively concentrated (non-hematogenous disseminated type) and the mesenteric lymph nodes are commonly involved. CT shows rim or multilocular enhancement of enlarged lymph nodes, and sometimes with intra-nodular calcifications. This disease is often associated with tuberculous peritonitis, which has characteristic signs of omental cakes, smudged mesentery signs and high-density ascites. LALN is relatively disperse and the mesenteric lymph nodes are not commonly involved in HD. CT shows homogenous enhancement of lymph node enlargement with fewer calcifications (only 0.84%) in untreated cases[12-13] and peritoneal and omental lymphomatosis is not often seen. In addition, rim enhancement of enlarged lymph nodes of LALN (including before and after radio-chemotherapy) on CT is different from that of lymph node tuberculosis. The lesions of LALN with clear margins and multilocular enhancement are not often found.
Metastatic tumor: The occurrence of abdominal lymph node metastasis usually follows the development of a primary tumor. The enlarged lymph nodes are located near the primary lesion, showing heterogeneous or rim enhancement due to necrosis of lymph nodes, with frequent occurrence of ascites. Neither tuberculous lymph nodes nor metastatic lymphadenopathy has blood vessel-imbedded signs, intestinal-imbedded signs, or cobblestone signs.
In summary, LALN has three kinds of CT manifesta-tions and each kind has some unique features valuable for qualitative diagnosis of LALN. CT is also helpful for the pathological classification of LALN and the therapeutic evaluation in follow-up.
| 1. | Yang ZG, Min PQ, Sone S, He ZY, Liao ZY, Zhou XP, Yang GQ, Silverman PM. Tuberculosis versus lymphomas in the abdominal lymph nodes: evaluation with contrast-enhanced CT. AJR Am J Roentgenol. 1999;172:619-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 59] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Wu N, Liu Y, Lin D, Chen Y, Shi M. [Abdominal and pelvic lymph nodes in non-Hodgkin lymphoma: the nodal distribution in Chinese patients]. Zhonghua Zhongliu Zazhi. 2002;24:580-584. [PubMed] |
| 4. | Radin DR, Esplin JA, Levine AM, Ralls PW. AIDS-related non-Hodgkin's lymphoma: abdominal CT findings in 112 patients. AJR Am J Roentgenol. 1993;160:1133-1139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 55] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Zhou KR. CT of the Abdomen. 1th ed. Shanghai: Shanghai Medical University publisher 1993; 274-278. |
| 6. | Young ZG, Wen PQ, Liao ZY, He ZY, Zhou XP, Yang HX. CT features and anatomic distribution of malignant lymphoma in abdominal lymph nodes involvement. Zhonghua Fangshe Zazie. 1996;30:727-731. |
| 7. | Goodman P, Raval B. Omental cakes in American Burkitt lymphoma. Computed tomography demonstration. Clin Imaging. 1989;13:117-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Horger M, Müller-Schimpfle M, Yirkin I, Wehrmann M, Claussen CD. Extensive peritoneal and omental lymphomatosis with raised CA 125 mimicking carcinomatosis: CT and intraoperative findings. Br J Radiol. 2004;77:71-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Sheth S, Horton KM, Garland MR, Fishman EK. Mesenteric neoplasms: CT appearances of primary and secondary tumors and differential diagnosis. Radiographics. 2003;23:457-73; quiz 535-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 106] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 10. | Fishman EK, Kuhlman JE, Jones RJ. CT of lymphoma: spectrum of disease. Radiographics. 1991;11:647-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 74] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Lynch MA, Cho KC, Jeffrey RB Jr, Alterman DD, Federle MP. CT of peritoneal lymphomatosis. AJR Am J Roentgenol. 1988;151:713-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Apter S, Avigdor A, Gayer G, Portnoy O, Zissin R, Hertz M. Calcification in lymphoma occurring before therapy: CT features and clinical correlation. AJR Am J Roentgenol. 2002;178:935-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Laufer L, Barki Y, Schulman H, Bernstein T, Niv A, Yaniv I. Calcification in an untreated case of Burkitt's lymphoma: radiographic, ultrasound and CT diagnosis. Pediatr Radiol. 1994;24:180-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Huang YR, Yan QH, Shi ML, Guan ZZ. Modern diagnosis and treatment of malignant lymphoma. 1th ed. Zhengzhou: Zhengzhou Henan Medical University Publisher 1997; 70-72. |
| 15. | Schaefer NG, Hany TF, Taverna C, Seifert B, Stumpe KD, von Schulthess GK, Goerres GW. Non-Hodgkin lymphoma and Hodgkin disease: coregistered FDG PET and CT at staging and restaging--do we need contrast-enhanced CT. Radiology. 2004;232:823-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 225] [Article Influence: 10.2] [Reference Citation Analysis (1)] |
| 16. | Oh YK, Ha CS, Samuels BI, Cabanillas F, Hess MA, Cox JD. Stages I-III follicular lymphoma: role of CT of the abdomen and pelvis in follow-up studies. Radiology. 1999;210:483-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Strijk SP, Boetes C, Rosenbusch G, Ruijs JH. Lymphography and abdominal computed tomography in staging Hodgkin's disease. Rofo. 1987;146:312-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Huang YR. [Value of abdominal CT scan in the staging of malignant lymphoma]. Zhonghua Zhongliu Zazhi. 1986;8:389-391. [PubMed] |
| 19. | Neumann CH, Robert NJ, Canellos G, Rosenthal D. Computed tomography of the abdomen and pelvis in non-Hodgkin lymphoma. J Comput Assist Tomogr. 1983;7:846-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Jung G, Heindel W, von Bergwelt-Baildon M, Bredenfeld H, Gossmann A, Zähringer M, Tesch H. Abdominal lymphoma staging: is MR imaging with T2-weighted turbo-spin-echo sequence a diagnostic alternative to contrast-enhanced spiral CT. J Comput Assist Tomogr. 2000;24:783-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Jing BS. Diagnostic imaging of abdominal and pelvic lymph nodes in lymphoma. Radiol Clin North Am. 1990;28:801-831. [PubMed] |
S- Editor Wang J L- Editor Zhu LH E- Editor Ma WH