Published online Dec 21, 2005. doi: 10.3748/wjg.v11.i47.7545
Revised: June 18, 2005
Accepted: June 21, 2005
Published online: December 21, 2005
A 53-year-old man with a history of blood transfusion at the age of 20 was admitted to our hospital because of liver dysfunction. He had bronchial asthma when he was 18 years old, which naturally resolved within 2 years. However, his bronchial asthma recurred at the age of 45 and was treated with oral theophylline. He was diagnosed as having chronic hepatitis C based on the histological and clinical findings, and then interferon (IFN) therapy was administered. The frequency of bronchial asthma attack was gradually decreasing after IFN therapy with marked improvement of hypereosinophilia. He achieved sustained viral response (SVR) and his bronchial asthma did not worsen even after the cessation of IFN. Hepatitis C virus (HCV) infection and IFN therapy were considered in the remission of asthma in this case. HCV infection could be the cause of bronchial asthma, especially in patients with late appearance of asthma.
- Citation: Yamamoto N, Murata K, Nakano T. Remission of bronchial asthma after viral clearance in chronic hepatitis C. World J Gastroenterol 2005; 11(47): 7545-7546
- URL: https://www.wjgnet.com/1007-9327/full/v11/i47/7545.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i47.7545
Hepatitis C virus (HCV) infection is sometimes associated with extrahepatic diseases, such as cryoglobulinemia[1,2] and lichen planus[2,3]. These extrahepatic diseases are considered as part of immune responses against HCV. We have presented a case of chronic hepatitis C with bronchial asthma which improved after interferon (IFN) therapy.
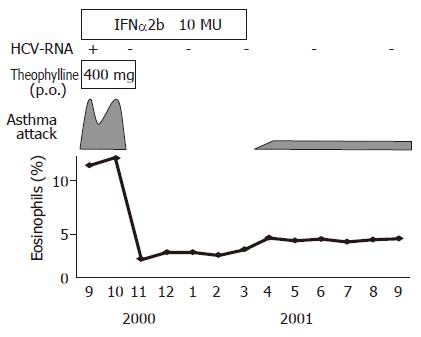
A 53-year-old man with a history of blood transfusion at the age of 20 was admitted to our hospital because of liver dysfunction. He had bronchial asthma when he was 18 years old, which naturally resolved within 2 years. However, his bronchial asthma recurred at the age of 45 and has been treated with oral theophylline. Asthma occurred 5-10 times a week before IFN therapy which needed inhalation of β2 stimulators in addition to daily treatment of theophylline therapy. They were all minor attacks and the patient was easily relieved after a few inhalations of β2 stimulators. On admission, physical examinations revealed mild wheezing at bilateral lung fields, but no hepatosplenomegaly was observed. Laboratory findings were as follows; white blood cell counts: 5 500/mm3 (eosinophils 11.2%); platelet counts: 169 000/mm3, alanine aminotransferase (ALT): 171 IU/L; and aspartate aminotransferase (AST): 81 IU/L, albumin: 42 g/L. HCV-RNA (Genotype 1b, 500 KIU/mL) was positive, but HBsAg, anti-HBc and anti nuclear antibody were all negative. IgE level was within the normal limit (55 IU/mL) and immune complex was negative (Table 1). Abdominal ultrasonography showed chronic liver injury. Liver biopsy revealed moderate portal inflammation and fibrous expansion (A2F2). Based on these findings, he was diagnosed as having chronic hepatitis C. IFN-α2b (10 MU daily for 2 wk, followed by 10 MU thrice a week for another 22 wk) was started on September 2000 with careful observation because asthma exacerbation during IFN therapy was reported[4]. Surprisingly, the frequency of asthma attack was gradually decreasing after IFN therapy with marked improvement of hypereosinophilia (Figure 1). Furthermore, during IFN therapy, asthma attack never recurred even after the cessation of daily theophylline. HCV-RNA became negative after IFN therapy and he achieved sustained virological response (SVR). After the cessation of IFN therapy, he needed inhalation of β2 stimulators for asthma occasionally. However, he did not require theophylline or steroid any more since the frequency of attack per month was well reduced and the degree of asthma attack was very mild. Interestingly, the eosinophil counts slightly increased after the cessation of IFN, but remained within the normal level (Figure 1).
| Peripheral blood | Coagulation test | ||
| WBC | 5 500/μL (Eo:11.2%) | PT | 149 % |
| RBC | 456× 104 /μL | HPT | 139 % |
| Hb | 14.7 g/dL | Biochemistry | |
| Hct | 43.6 % | TP | 7.0 g/dL |
| Plt | 16.9×104/mm3 | Alb | 4.2 g/dL |
| Serological study | T-Bi | 0.6 mg/dL | |
| IgG | 1236 mg/dL | AST | 81 IU/L |
| IgA | 240 mg/dL | ALT | 171 IU/L |
| IgM | 41 mg/dL | LDH | 203 IU/L |
| CH50 | 55 U/mL | ALP | 298 IU/L |
| Cryoglobulin | - | γGTP | 65 IU/L |
| Immune complex | - | T.chol | 176 mg/dL |
| Virology | Amy | 104 IU/L | |
| HCV genotype | Ib | BUN | 11.1 mg/dL |
| HCV RNA | 500KIU/mL | Cre | 0.8 mg/dL |
Chronic HCV infection can be associated with various immune mediated extrahepatic manifestations, including porphyria cutanea tarda[1,2], membranoproliferative glomerulonephritis[1,2], oral lichen planus[2,3], mixed cryoglobulinemias[1,2], vitiligo[2], B-cell non-Hodgkin lymphoma[2], etc. The response of bronchodilator against asthma was significantly better in the IFN responder group than in the IFN non-responder group[5]. Remission of asthma after the clearance of HCV by IFN therapy in our case could be considered from two points of view. Cytotoxic T cells induced by chronic HCV infection might be a trigger for the development of airway inflammation in patients with bronchial asthma[5] since latent viral infections may be an important cofactor causing airway inflammation[6]. In patients with chronic hepatitis C, the responses of inhaled corticosteroid therapy[5] or bronchodilator for bronchial asthma are impaired, which are recovered in IFN responders[5]. Peripheral B-cell markers such as CD81 and CD5 are correlated with HCV viral load and autoimmunity[7]. The response of antiviral therapy is correlated with the downregulation of these markers. These observations suggest that immune responses by HCV, including cytokines from lymphocytes, may contribute to chronic airway inflammation, and the clearance of HCV by IFN may improve it. The other cause is IFN itself. Injected IFN or released IFN induced by cytotoxic T cells against HCV may improve bronchial asthma by suppressing the chronic airway inflammation since IFN-γ acts as Th1 paracrine inflammatory cytokine. On the contrary, IFN-γ producing T cells may induce the migration of Th2 cells to the airways and IFN may worsen bronchial asthma[8]. Furthermore, IFN increases histamine release from basophilic cells, which is an important trigger for asthma attack[9]. The effect of IFN on bronchial asthma is still controversial.
This is, to our knowledge, the first case in which bronchial asthma improved after the clearance of HCV by IFN. HCV infection could be the cause of bronchial asthma, especially in patients with late onset of asthma.
| 1. | Gumber SC, Chopra S. Hepatitis C: a multifaceted disease. Review of extrahepatic manifestations. Ann Intern Med. 1995;123:615-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 299] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 2. | El-Serag HB, Hampel H, Yeh C, Rabeneck L. Extrahepatic manifestations of hepatitis C among United States male veterans. Hepatology. 2002;36:1439-1445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 115] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Pilli M, Penna A, Zerbini A, Vescovi P, Manfredi M, Negro F, Carrozzo M, Mori C, Giuberti T, Ferrari C. Oral lichen planus pathogenesis: A role for the HCV-specific cellular immune response. Hepatology. 2002;36:1446-1452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Bini EJ, Weinshel EH. Severe exacerbation of asthma: a new side effect of interferon-alpha in patients with asthma and chronic hepatitis C. Mayo Clin Proc. 1999;74:367-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Kanazawa H, Mamoto T, Hirata K, Yoshikawa J. Interferon therapy induces the improvement of lung function by inhaled corticosteroid therapy in asthmatic patients with chronic hepatitis C virus infection: a preliminary study. Chest. 2003;123:600-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Keicho N, Elliott WM, Hogg JC, Hayashi S. Adenovirus E1A upregulates interleukin-8 expression induced by endotoxin in pulmonary epithelial cells. Am J Physiol. 1997;272:L1046-L1052. [PubMed] |
| 7. | Zuckerman E, Kessel A, Slobodin G, Sabo E, Yeshurun D, Toubi E. Antiviral treatment down-regulates peripheral B-cell CD81 expression and CD5 expansion in chronic hepatitis C virus infection. J Virol. 2003;77:10432-10436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Krouwels FH, Hol BE, Bruinier B, Lutter R, Jansen HM, Out TA. Cytokine production by T-cell clones from bronchoalveolar lavage fluid of patients with asthma and healthy subjects. Eur Respir J Suppl. 1996;22:95s-103s. [PubMed] |
| 9. | Krasnowska M, Małolepszy J, Liebhart E, Inglot AD. Inhaled natural human interferon alpha induces bronchospastic reactions in asthmatics. Arch Immunol Ther Exp (Warsz). 1992;40:75-78. [PubMed] |
Science Editor Ma JY and Guo SY Language Editor Elsevier HK