©The Author(s) 2026.
World J Gastroenterol. Jan 28, 2026; 32(4): 112635
Published online Jan 28, 2026. doi: 10.3748/wjg.v32.i4.112635
Published online Jan 28, 2026. doi: 10.3748/wjg.v32.i4.112635
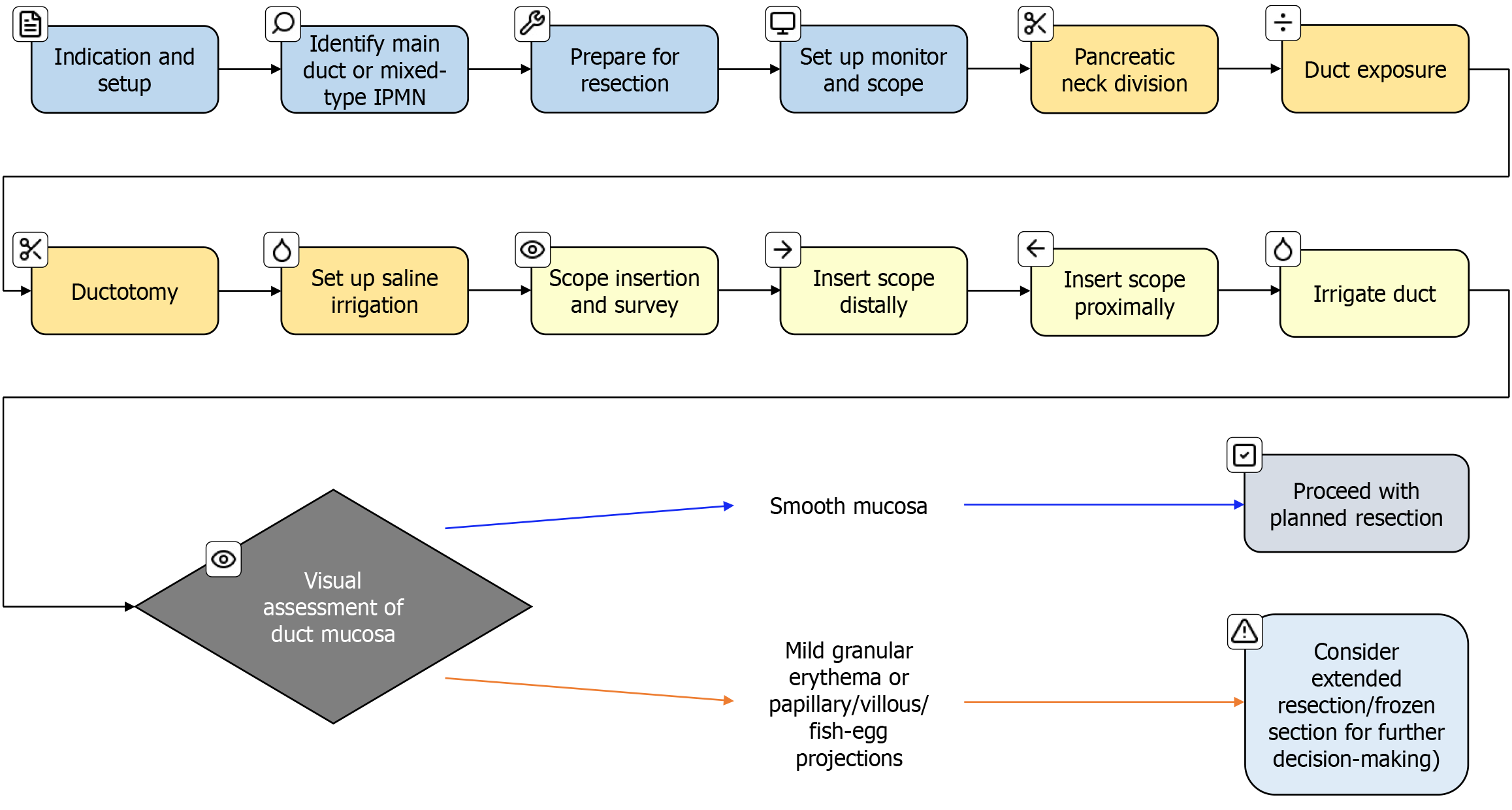
Figure 1 Workflow for resection of main-duct or mixed-type intraductal papillary mucinous neoplasm.
IPMN: Intraductal papillary mucinous neoplasms.
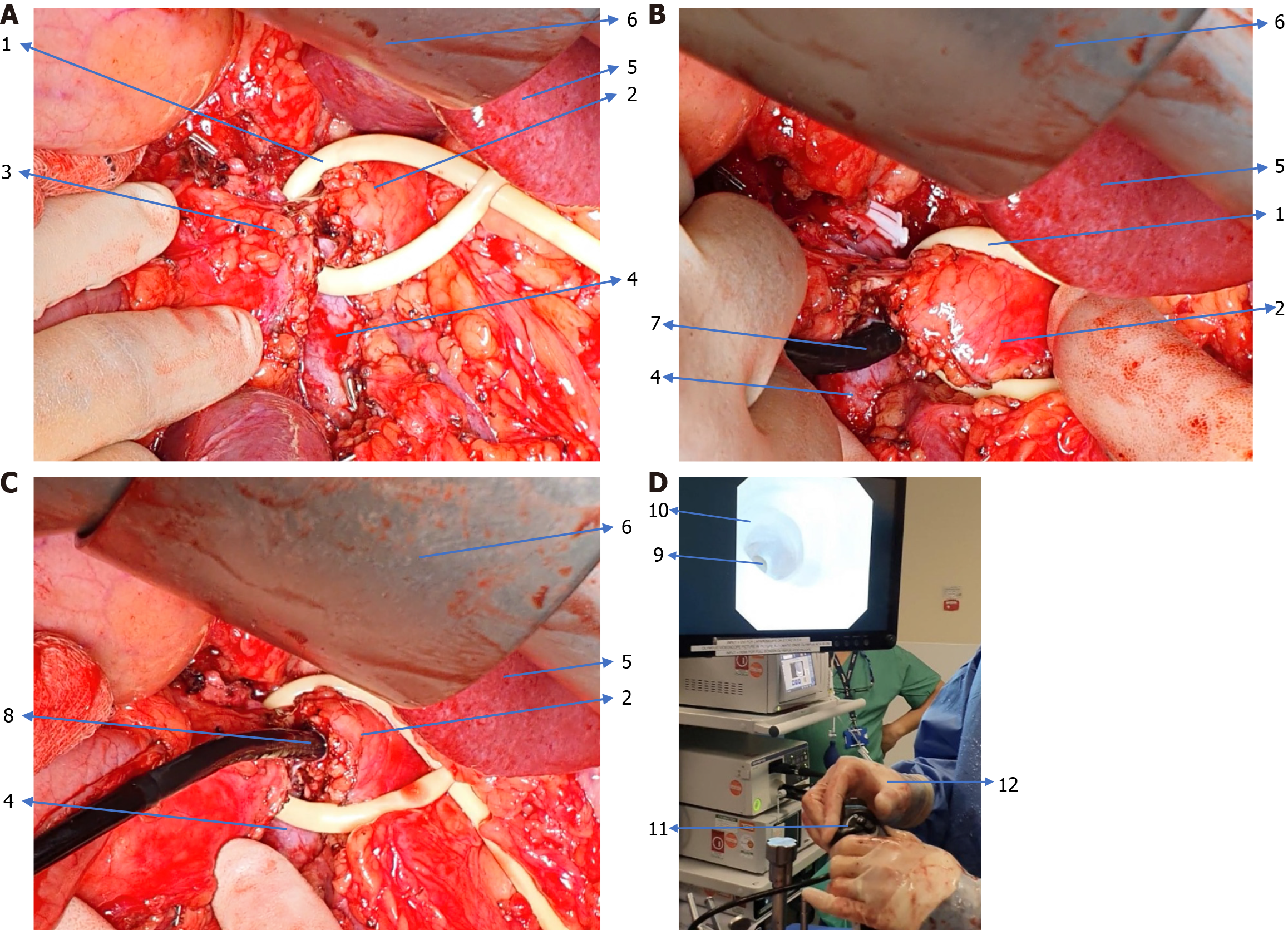
Figure 2 Intraoperative pancreatoscopy.
A: Isolation of the main pancreatic duct; B: Scope insertion into the main pancreatic duct; C: Scope lying within the main pancreatic duct handled by the surgeon; D: On-screen pancreatoscopic view with choledochoscope stack. 1: Sling isolating the neck of the pancreas and main pancreatic duct; 2: Body and tail of the pancreas; 3: Head of the pancreas; 4: Superior mesenteric vein; 5: Liver; 6: Retractor; 7: Choledochoscope; 8: Choledochoscope inserted into main pancreatic duct; 9: Inside view of main pancreatic duct; 10: Pancreatic duct lumen; 11: Choledochoscope used for pancreatoscopy; 12: Operating surgeon handling scope.
- Citation: Abusharar M, Barritt C, Mavroeidis VK, Aroori S. Role of pancreatoscopy in the management of suspected and confirmed intraductal papillary mucinous neoplasm of the pancreas. World J Gastroenterol 2026; 32(4): 112635
- URL: https://www.wjgnet.com/1007-9327/full/v32/i4/112635.htm
- DOI: https://dx.doi.org/10.3748/wjg.v32.i4.112635