©The Author(s) 2026.
World J Gastroenterol. Jan 21, 2026; 32(3): 113452
Published online Jan 21, 2026. doi: 10.3748/wjg.v32.i3.113452
Published online Jan 21, 2026. doi: 10.3748/wjg.v32.i3.113452
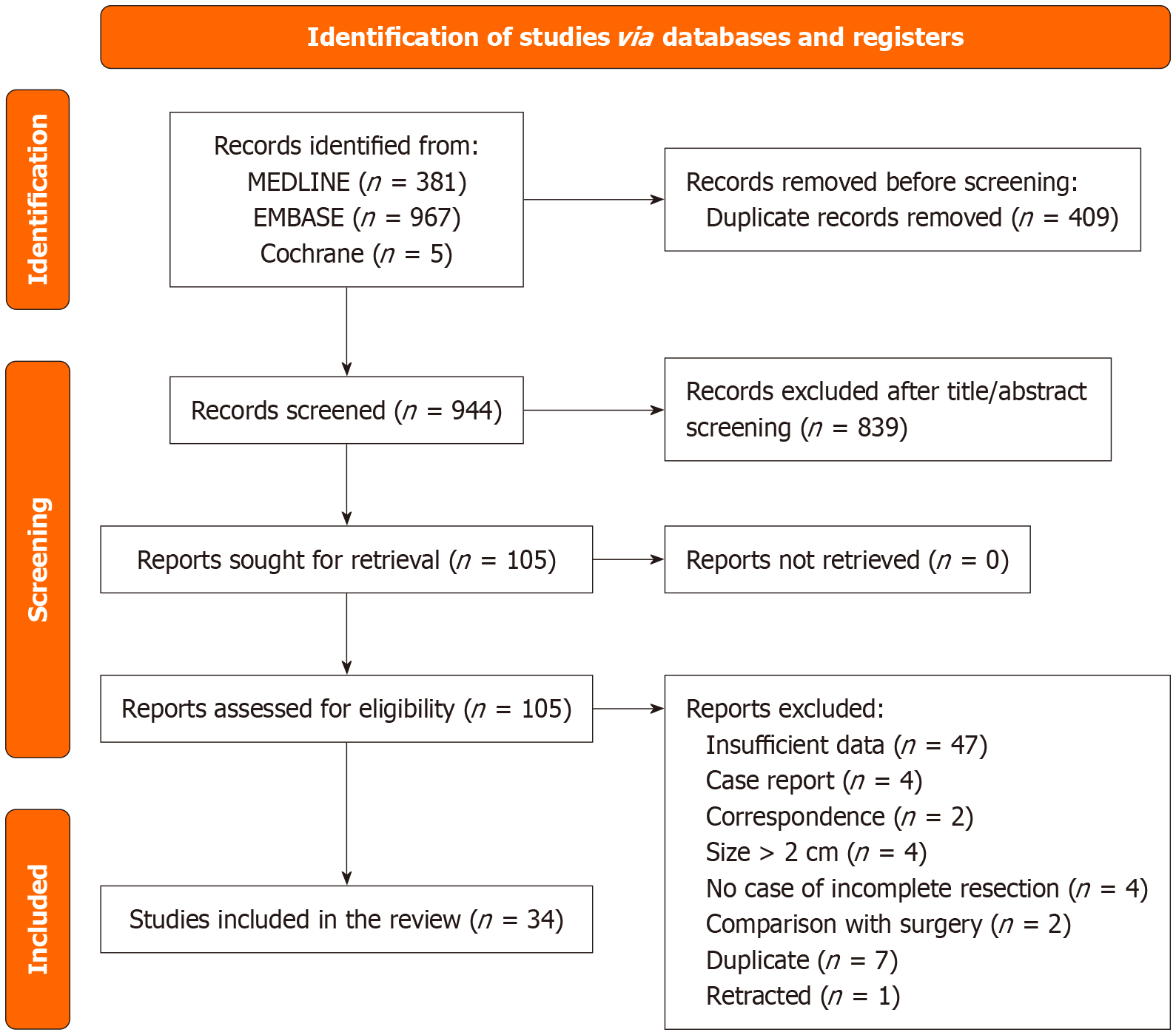
Figure 1 Preferred reporting items for systematic reviews and meta-analyses 2020 study selection flow diagram.
The flow diagram illustrates the study selection process according to the preferred reporting items for systematic reviews and meta-analyses 2020 guidelines. The number of records identified (n = 1353), screened (n = 944), and excluded (with reasons) are shown. The systematic review and meta-analysis included 34 studies.
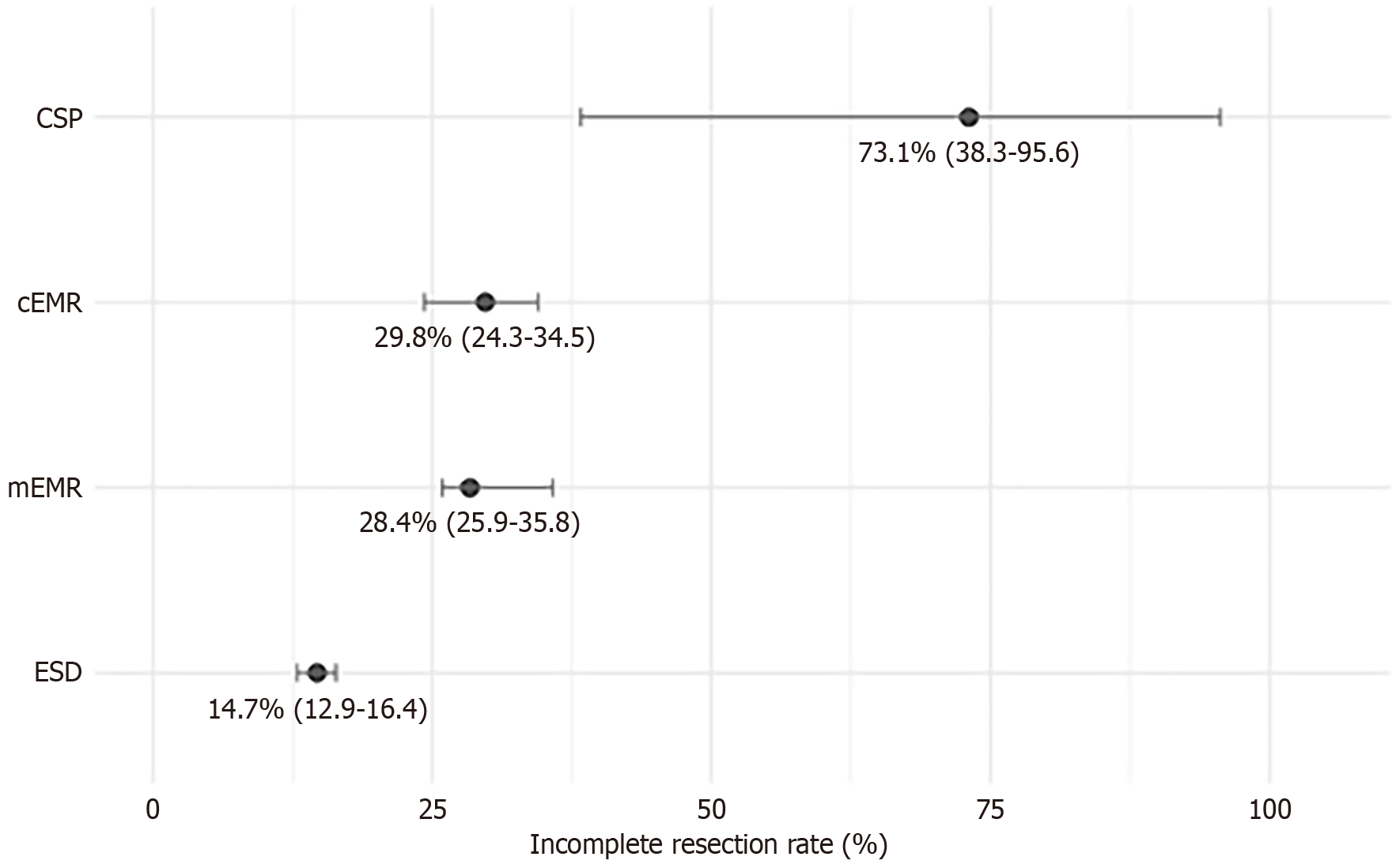
Figure 2 Incomplete resection rate by initial resection method.
The forest plot shows pooled incomplete resection rates across different primary endoscopic techniques based on 17 studies[19,20,24,27,28,30,33,34,37,40-42,46-50]. Cold snare polypectomy exhibited the highest rate (73.1%), whereas endoscopic submucosal dissection had the lowest rate (14.7%). Conventional endoscopic mucosal resection and modified endoscopic mucosal resection had intermediate incomplete resection rates. This figure emphasizes the impact of the resection technique on histological completeness. CSP: Cold snare polypectomy; cEMR: Conventional endoscopic mucosal resection; mEMR: Modified endoscopic mucosal resection; ESD: Endoscopic submucosal dissection.
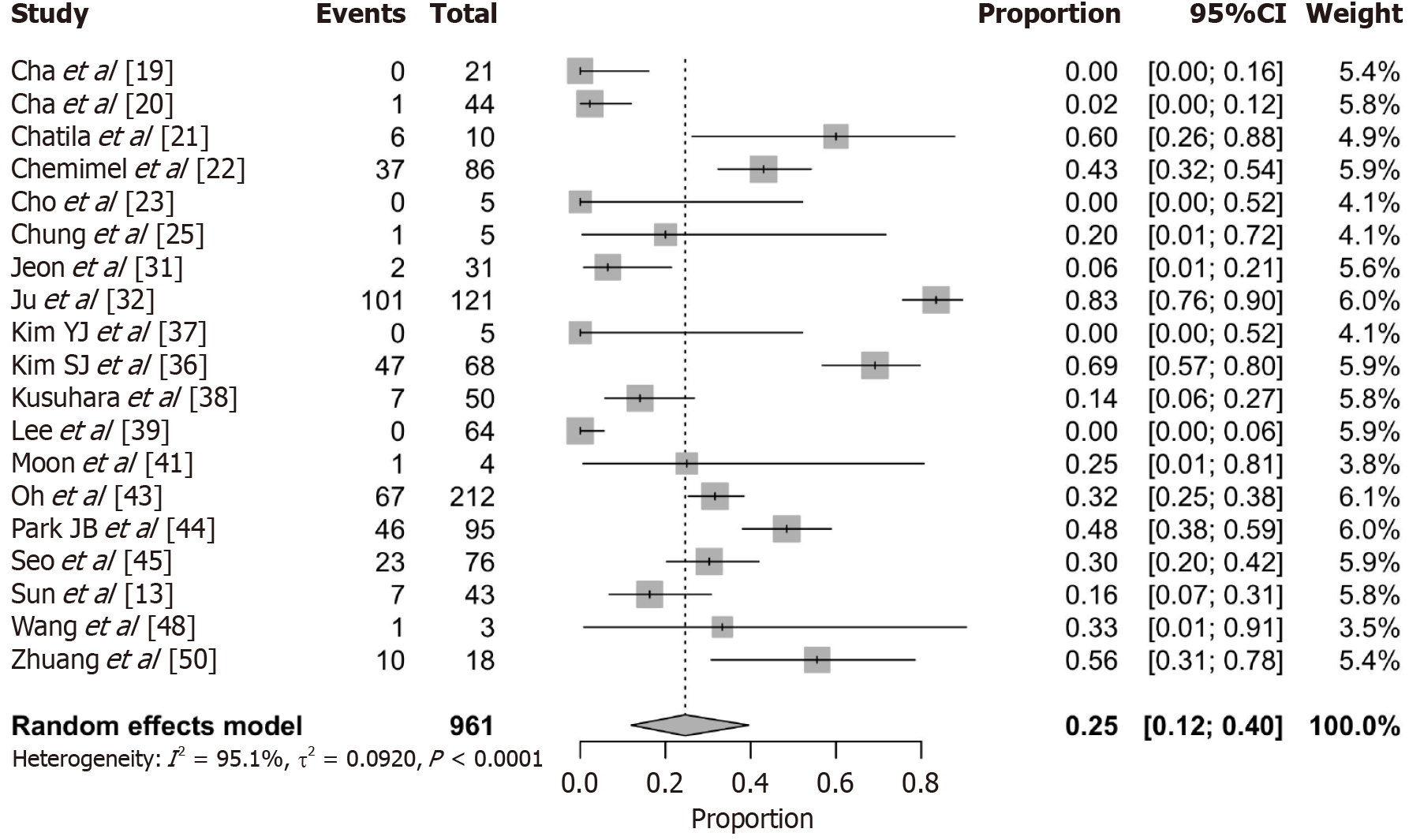
Figure 3 Residual tumor rate following salvage treatment.
The forest plot shows the pooled residual lesion rate after salvage treatment in patients with incompletely resected rectal neuroendocrine tumors based on a single-arm meta-analysis of 19 studies. The pooled rate was 25.0% (95% confidence interval: 12.0%-40.0%). This indicates that a substantial proportion of patients may harbor remnant tumors despite additional intervention. CI: Confidence interval.
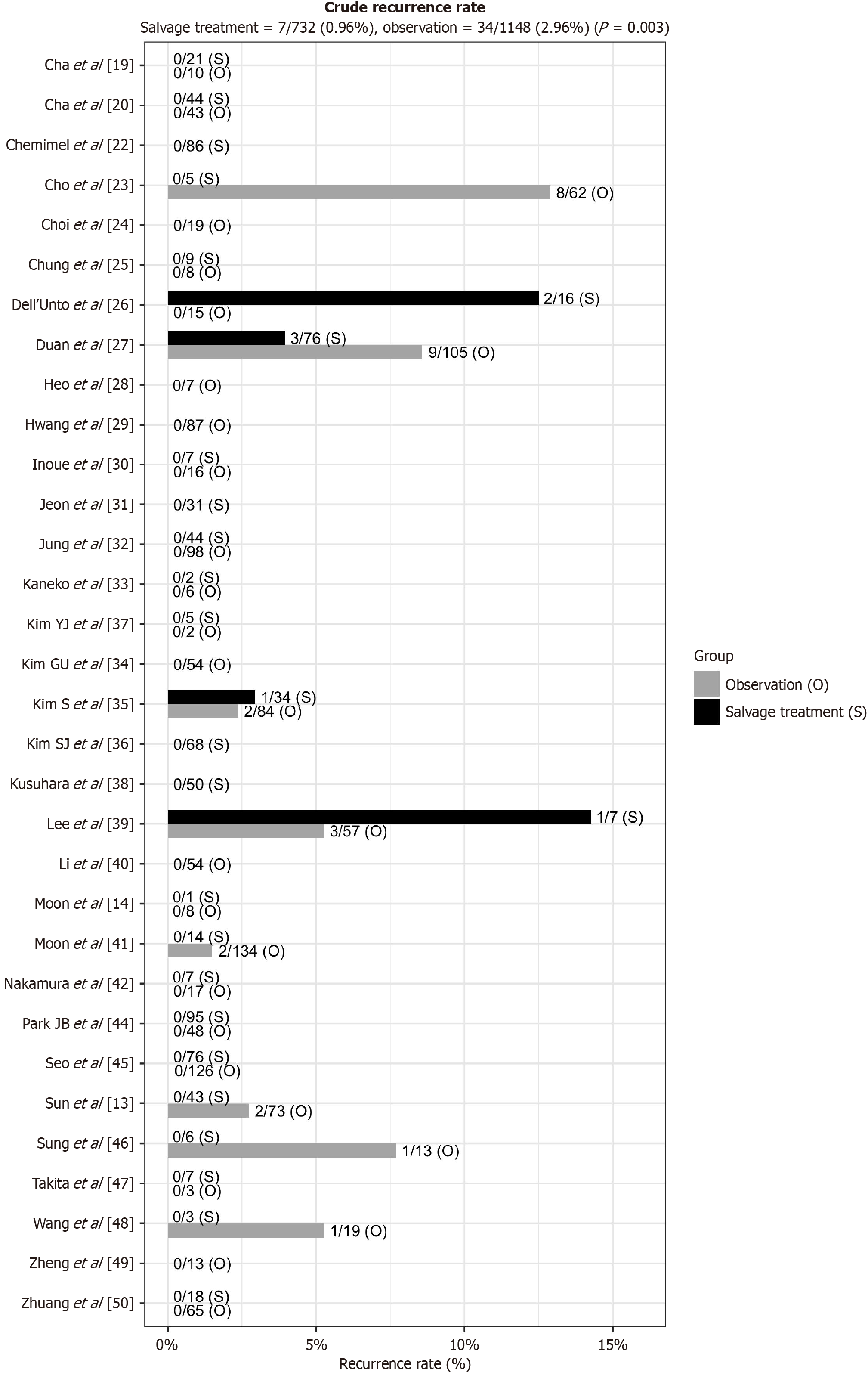
Figure 4 Crude recurrence rates: Salvage treatment vs observation.
The bar plot summarizes the crude recurrence rates from 31 studies by treatment group. Recurrence occurred in 0.96% of the patients receiving salvage treatment (7/776) and 2.96% of those managed with observation (34/1246), showing a statistically significant difference (P = 0.003) in favor of salvage treatment. O: Observation; S: Salvage treatment.
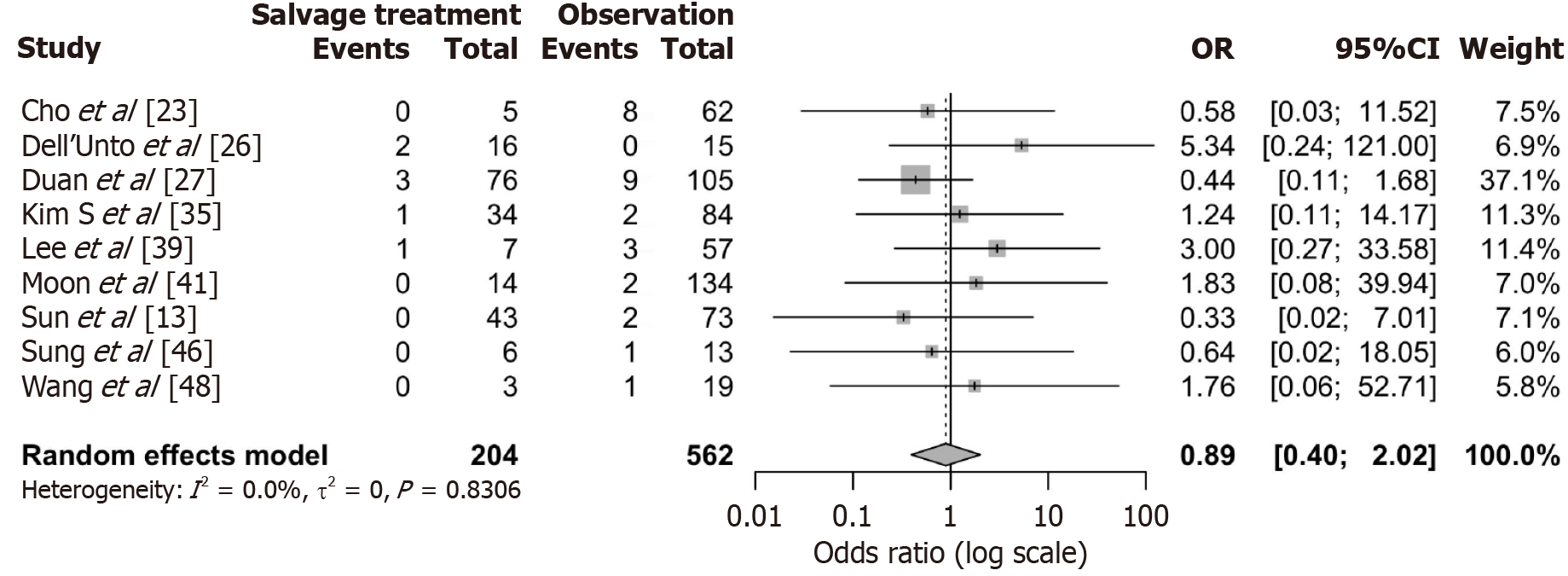
Figure 5 Meta-analysis of recurrence risk: Salvage treatment vs observation.
The forest plot compares the recurrence risk between salvage treatment and observation based on nine studies reporting events in both groups. The pooled odds ratio was 0.89 (95% confidence interval: 0.40-2.02), with no statistical significance and negligible heterogeneity (I2 = 0%), suggesting inconclusive comparative effectiveness. OR: Odds ratio; CI: Confidence interval.
- Citation: Kim JH, Lee JW, Kim HJ, Hong SM, Park SJ. Is salvage treatment necessary after incomplete resection of rectal neuroendocrine tumors: A systematic review and meta-analysis. World J Gastroenterol 2026; 32(3): 113452
- URL: https://www.wjgnet.com/1007-9327/full/v32/i3/113452.htm
- DOI: https://dx.doi.org/10.3748/wjg.v32.i3.113452