©The Author(s) 2025.
World J Gastroenterol. Sep 7, 2025; 31(33): 109811
Published online Sep 7, 2025. doi: 10.3748/wjg.v31.i33.109811
Published online Sep 7, 2025. doi: 10.3748/wjg.v31.i33.109811
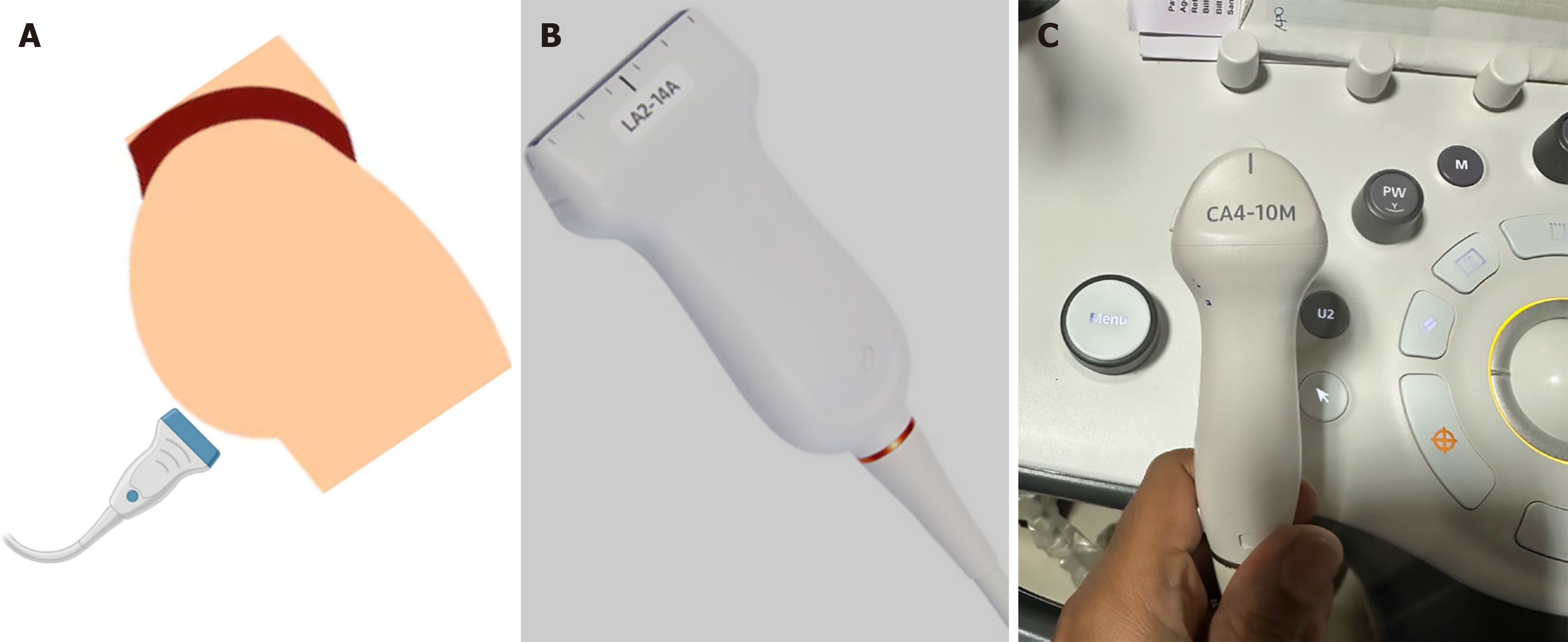
Figure 1 Transperineal ultrasound.
A: Schematic demonstrating transperineal ultrasound probe placement in the left lateral decubitus position; B: High-frequency linear probe (e.g., LA2-14A) for superficial structures and rectal wall imaging; C: Microconvex probe (CA4-10M), offering superior maneuverability within the perineal cleft.
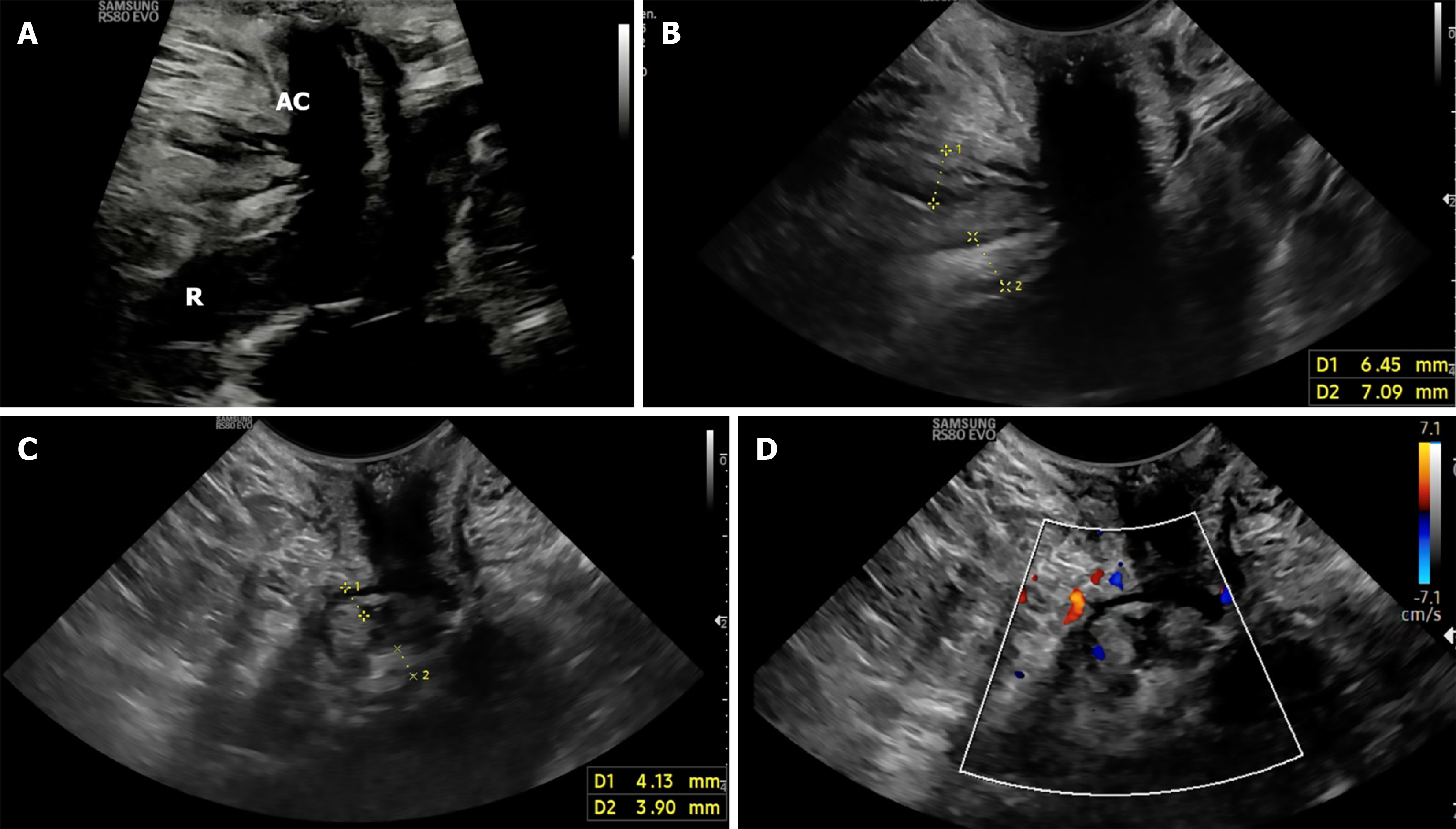
Figure 2 Perineal ultrasound for measuring rectal thickness using various probes.
A: Sagittal view on transperineal ultrasound with linear probe showing the anal canal and rectum; B: Axial image showing hypoechoic internal anal sphincter and hyperechoic external anal sphincter; C: Axial image showing rectal wall thickness; D: Doppler-enhanced axial view showing color flow within perianal structures (Modified Limberg scoring in progress). AC: Anal canal; R: Rectum.
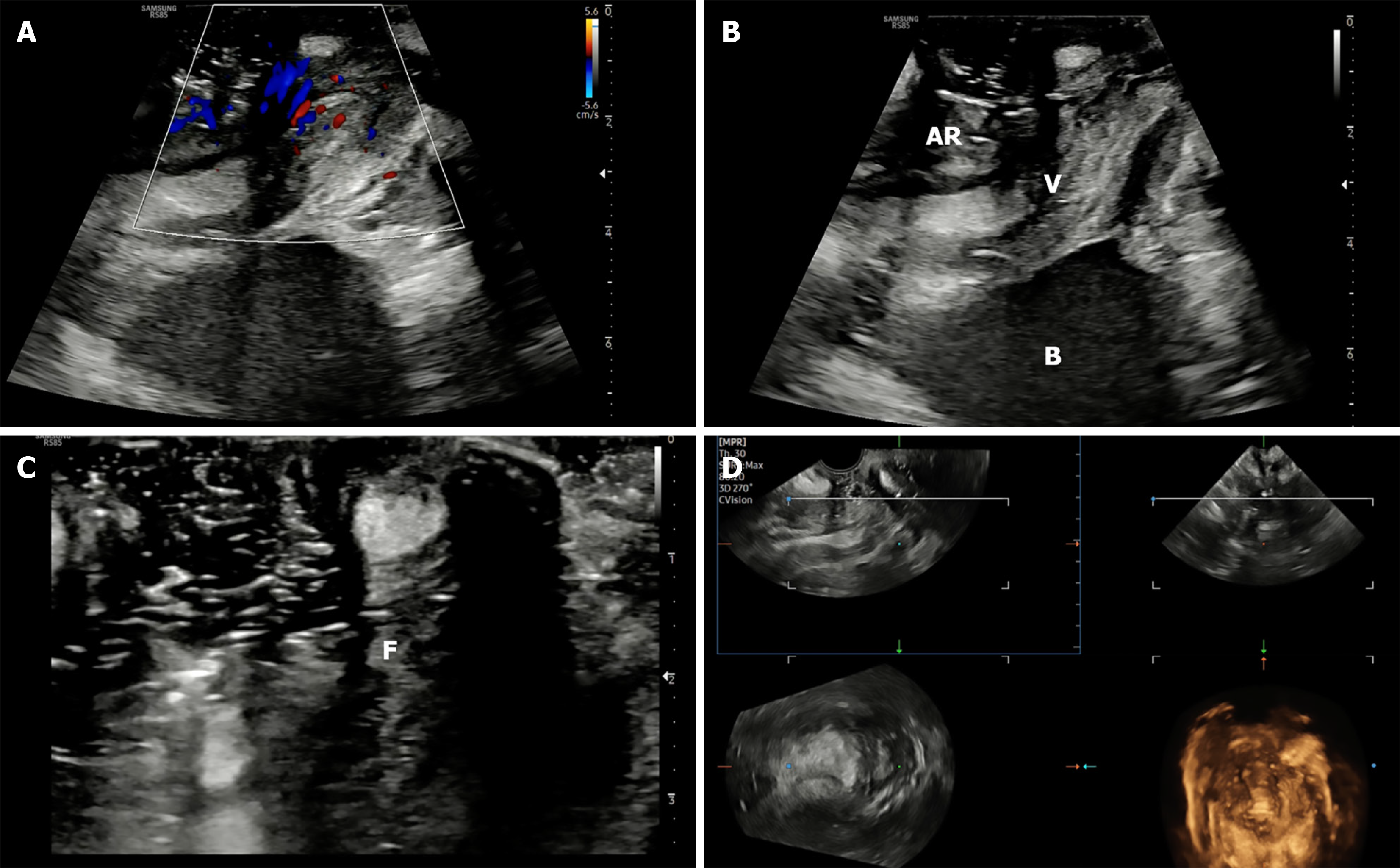
Figure 3 Perineal ultrasound in anovaginal fistula.
A: Sagittal view showing anterior anorectal anatomy including bladder and vagina; B: Doppler imaging depicting perianal vascularity suggestive of active inflammation; C: High-frequency linear probe image showing superficial anovaginal fistula, with air tracking inside fistula; D: Volumetric three-dimensional transperineal ultrasound reconstruction of fistula. AR: Anterior anorectal; B: Bladder; V: Vagina; F: Fistula.
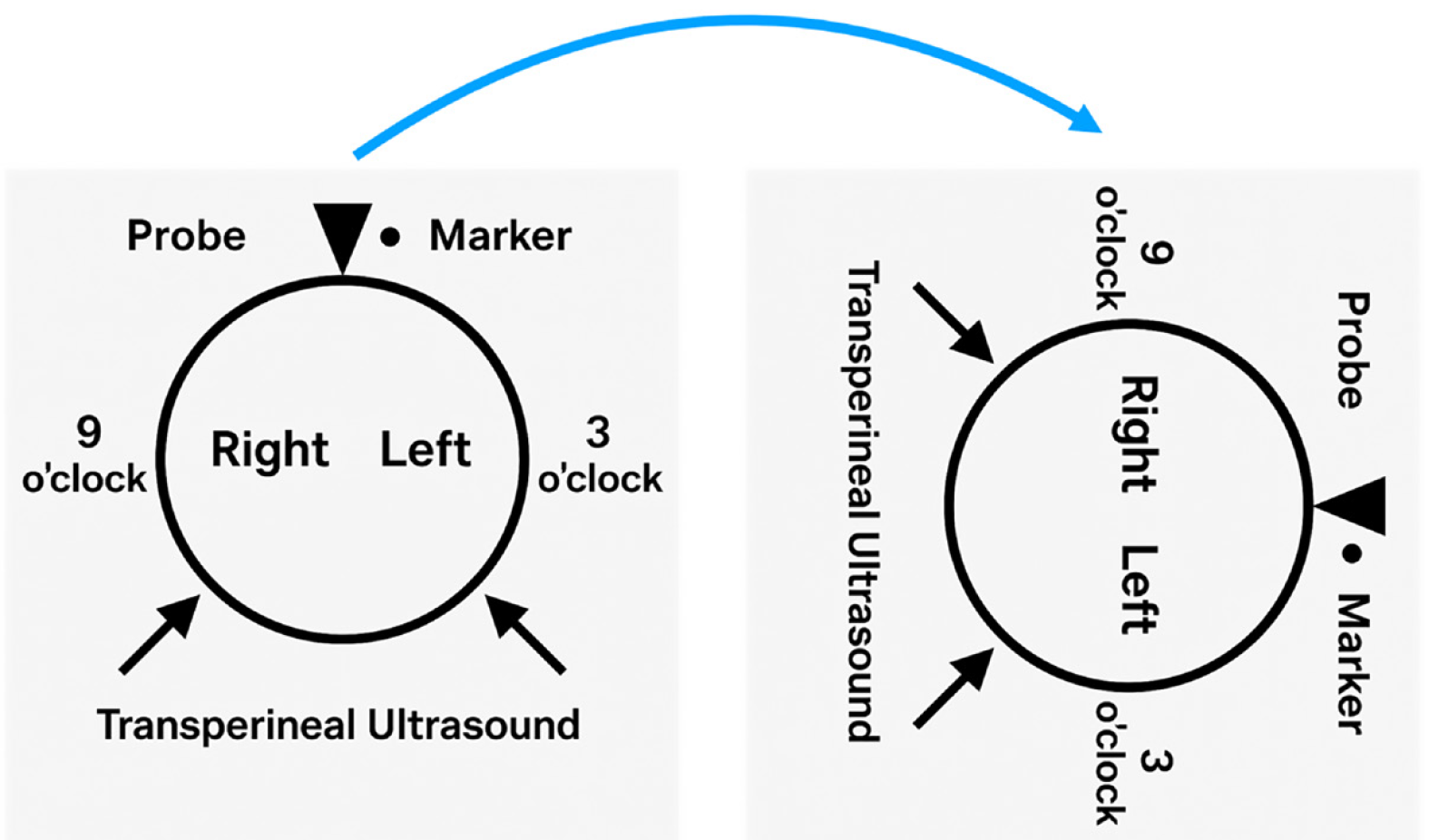
Figure 4 Clock-face orientation comparison for fistula reporting: Lithotomy position (left) vs transperineal ultrasound in left lateral decubitus (right).
In transperineal ultrasound, 12 o’clock is anterior (screen right), and 6 o’clock is posterior (screen left).
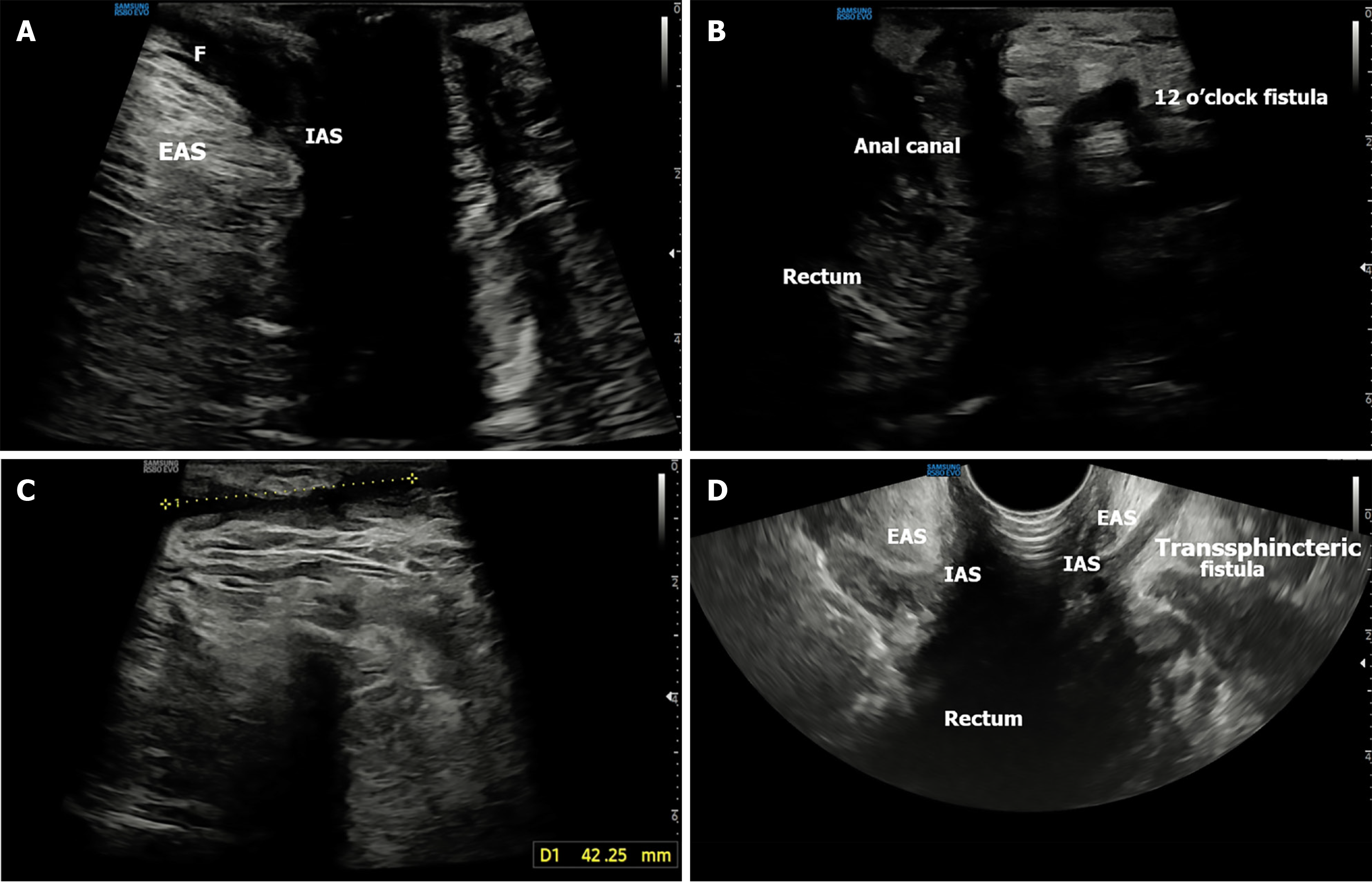
Figure 5 Inter- and trans- sphincteric fistula.
A: Transperineal ultrasound sagittal image showing intersphincteric fistula between internal anal sphncter and extenal anal sphicter (EAS); B: Transsphincteric fistula originating from anal canal and extending through EAS (12 o’clock); C: Axial view showing orientation of the long tract going anteriorly; D: Complex transsphincteric tract with anterior extension seen on transrectal ultrasound. F: Fistula; EAS: Extenal anal sphincter; IAS: Internal anal sphincter.
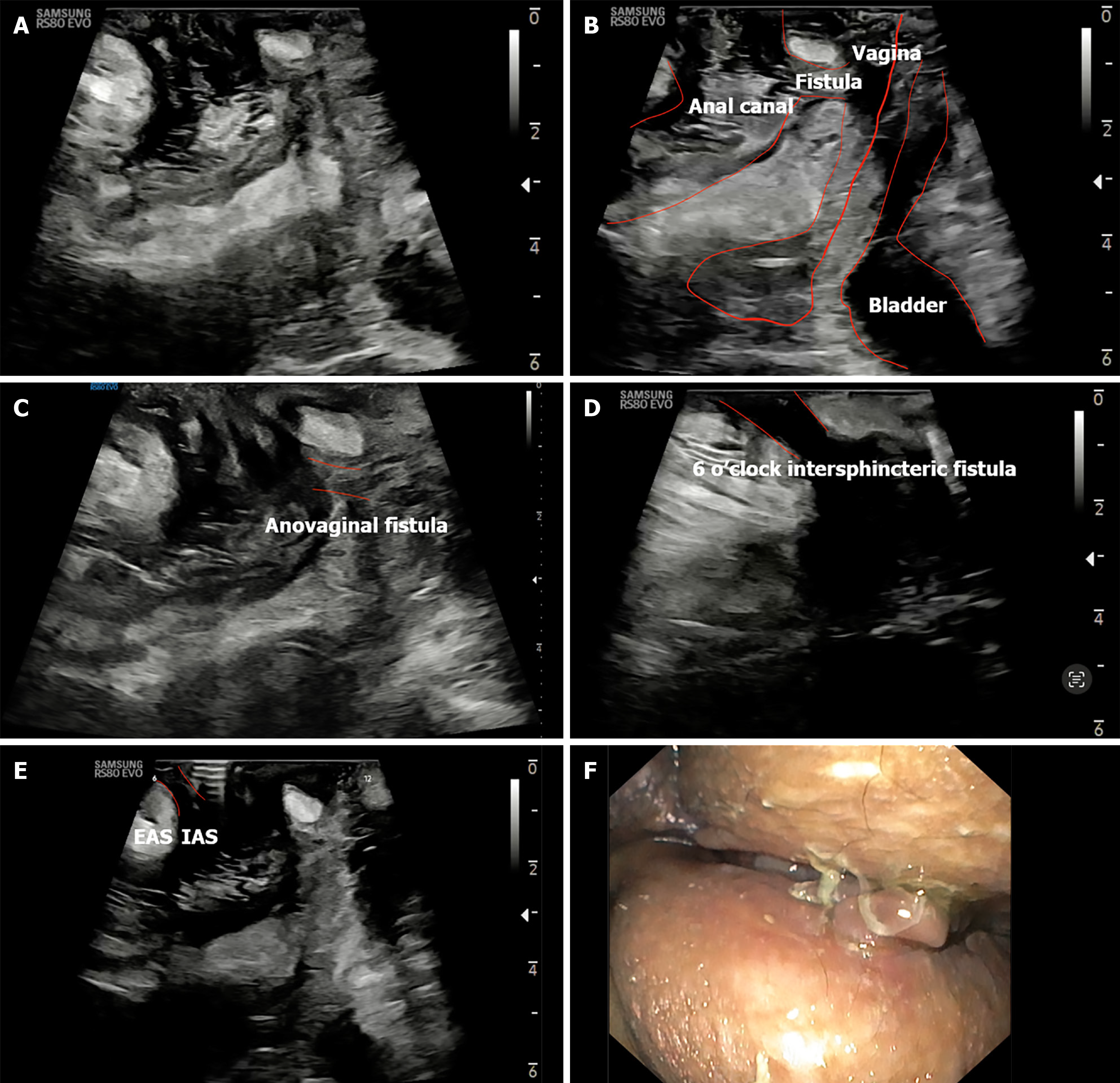
Figure 6 Rectovaginal fistula.
A: Intersphincteric fistula at 6 o’clock; B: Annotated image showing fistulous connection between rectum and vagina; C: Superficial anovaginal fistula; D and E: Transperineal ultrasound axial images demonstrating posterior intersphicteric fistulous extension; F: Endoscopic image of perineum. EAS: Extenal anal sphincter; IAS: Internal anal sphincter.
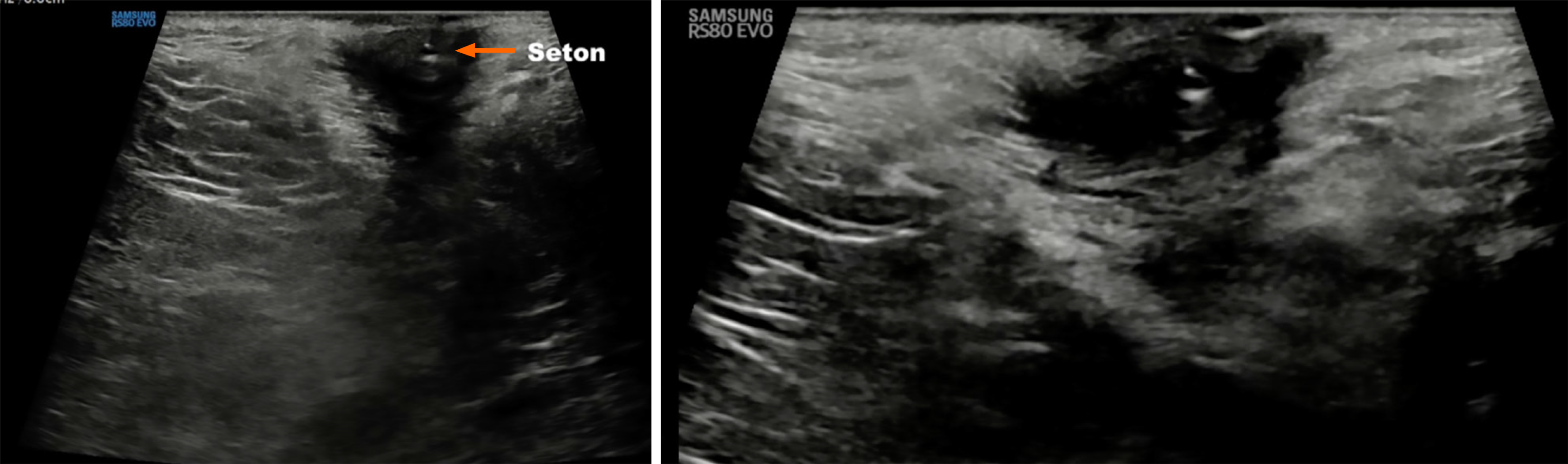
Figure 7 Seton on transperineal ultrasound.
Hyperechoic linear seton visualized within hypoechoic fistulous tract, indicating treated perianal disease under follow-up.
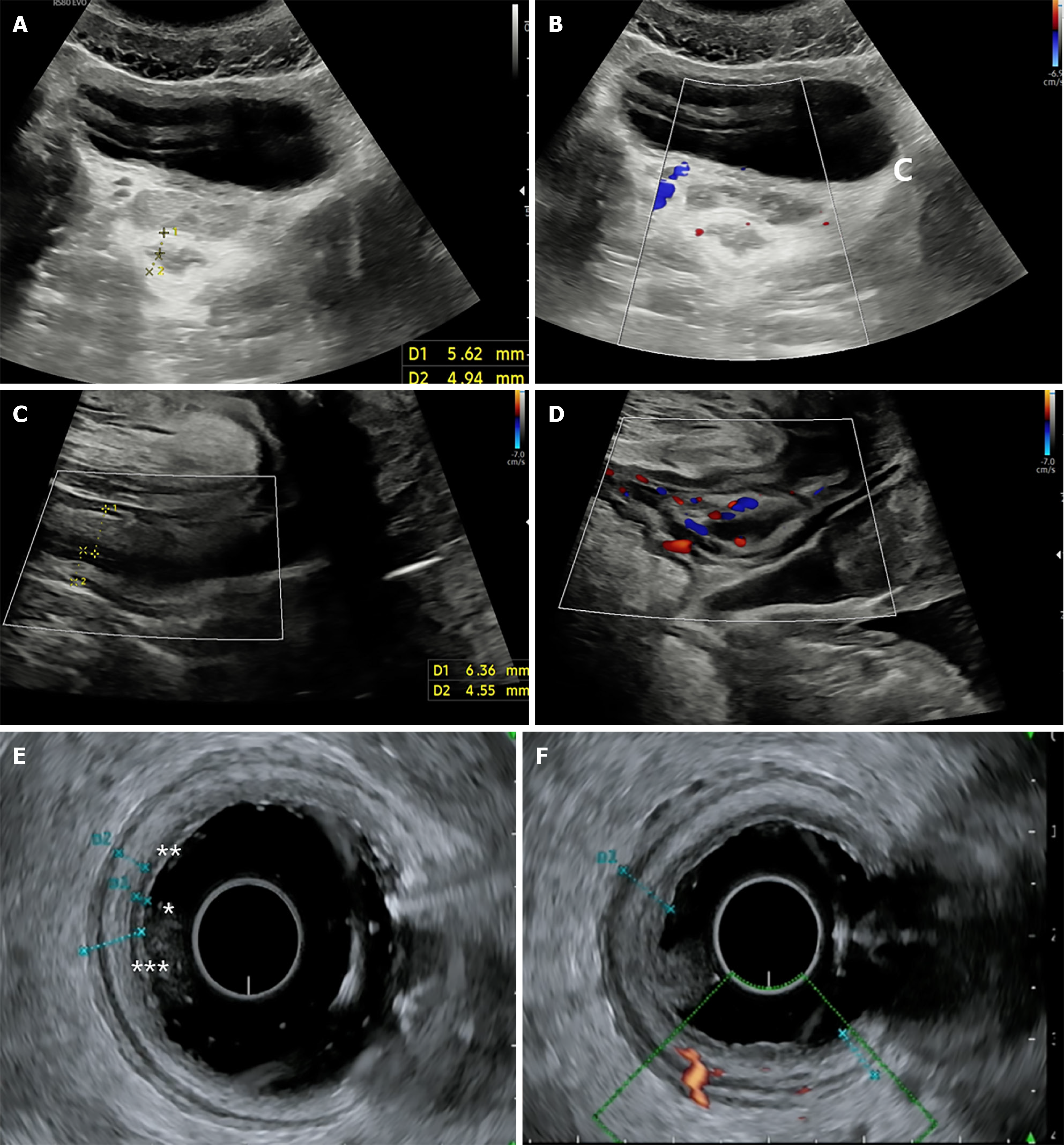
Figure 8 Transperineal ultrasound in ulcerative colitis.
A and B: Transabdominal ultrasound showing rectal wall thickness with Doppler signal; C: Transperineal ultrasound (TPUS) axial image assessing rectal inflammation (bowel wall thickness > 4 mm); D: TPUS Doppler showing modified Limberg score 2; E and F: Endoscopic ultrasound showing rectal mucosa and layered wall; Doppler overlay (F) confirms vascular activity.
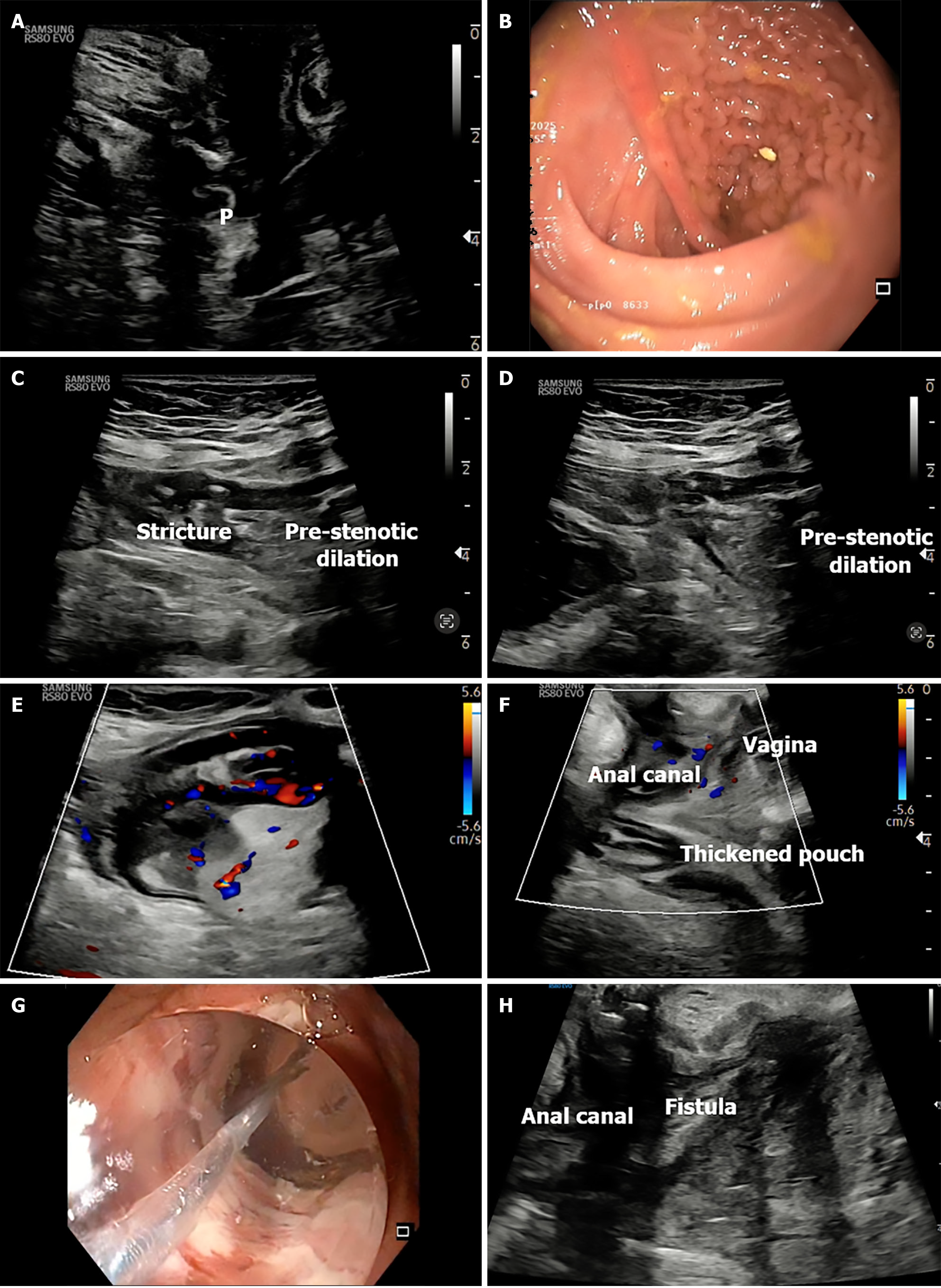
Figure 9 Transperineal ultrasound in ileal pouch.
A: Transperineal ultrasound (TPUS) image showing normal pouch wall; B: Endoscopic view of normal pouch mucosa; C and D: Transabdominal ultrasound showing prestenotic dilatation with stricture; E: Color Doppler showing increased vascularity in the pouch; F: TPUS sagittal image of thickened pouch with adjacent vagina; G: Endoscopic balloon dilation under image guidance; H: TPUS view of anorectum and vagina for assessing anovaginal fistula in in ileal pouch case. P: Pouch wall.
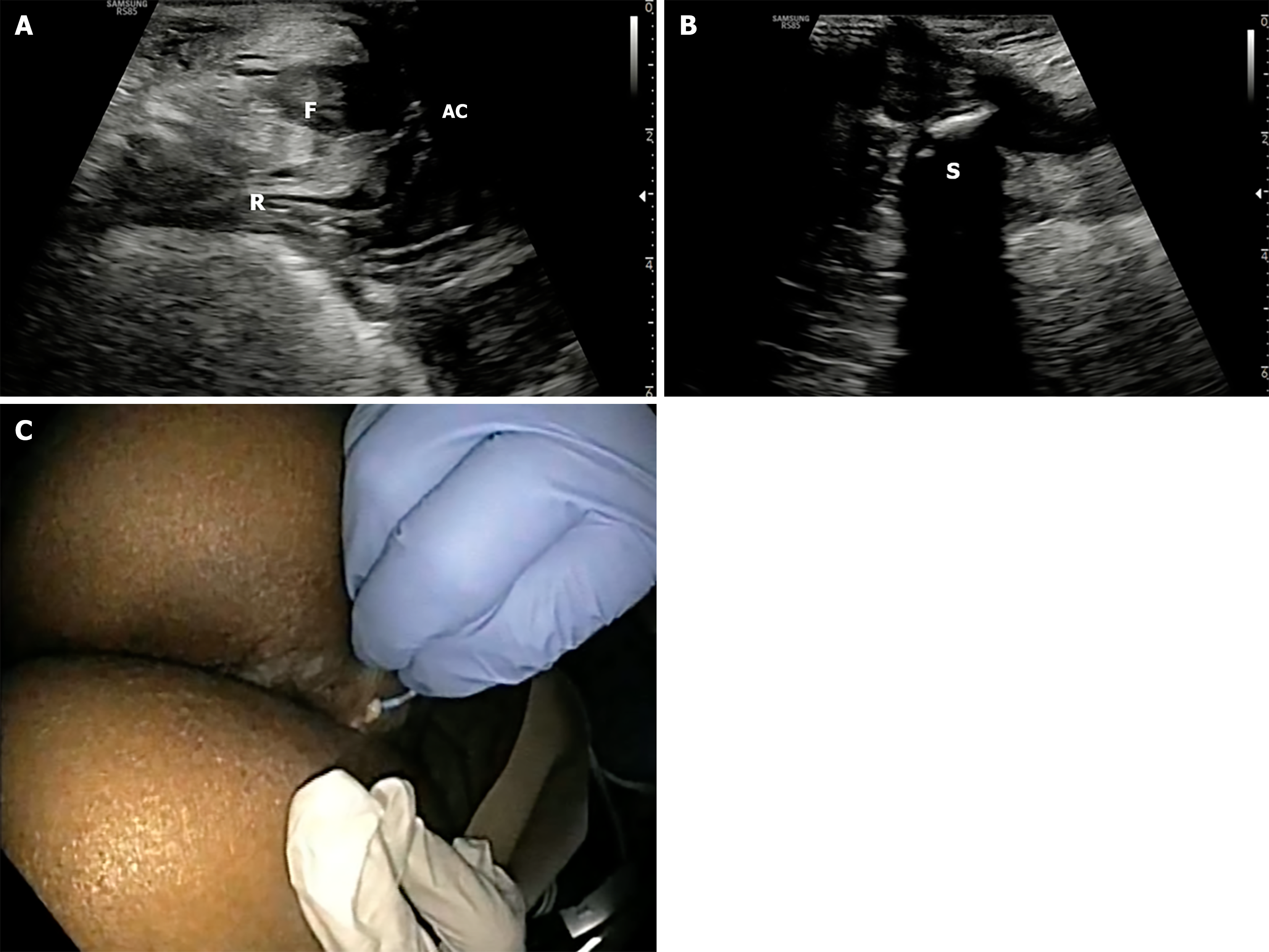
Figure 10 Transperineal ultrasound guided fistulotomy.
A: Transsphincteric fistula extending from anal canal, rectum; B: Fistula extending posteriorly to coccyx; C: Endoscopic fistulotomy done guided by pre-procedure transperineal ultrasound. F: Fistula; AC: Anal canal; R: Rectum; S: Sacrum.
- Citation: Pal P, Mateen MA, Pooja K, Gupta R, Tandan M, Reddy DN. Transperineal ultrasound: Role in inflammatory bowel disease management. World J Gastroenterol 2025; 31(33): 109811
- URL: https://www.wjgnet.com/1007-9327/full/v31/i33/109811.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i33.109811