©The Author(s) 2025.
World J Gastroenterol. Aug 21, 2025; 31(31): 109994
Published online Aug 21, 2025. doi: 10.3748/wjg.v31.i31.109994
Published online Aug 21, 2025. doi: 10.3748/wjg.v31.i31.109994
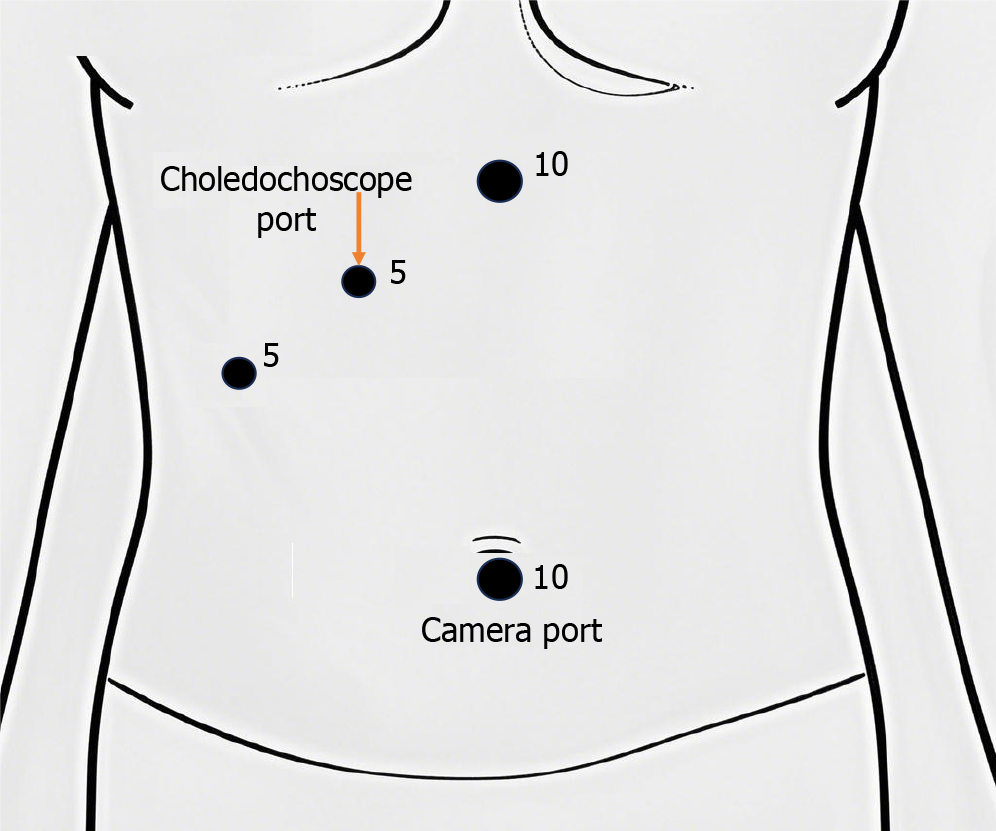
Figure 1 Trocar position.
A 1.5-2 cm infraumbilical incision was created to establish pneumoperitoneum at an intra-abdominal pressure of approximately 12 mmHg. A trocar, cannula, and laparoscope were inserted in sequence. Additional ports were introduced via puncture sites at the xiphoid process, 2 cm inferior to the right midclavicular line at the costal margin, and 2 cm below the right anterior axillary line at the costal margin.
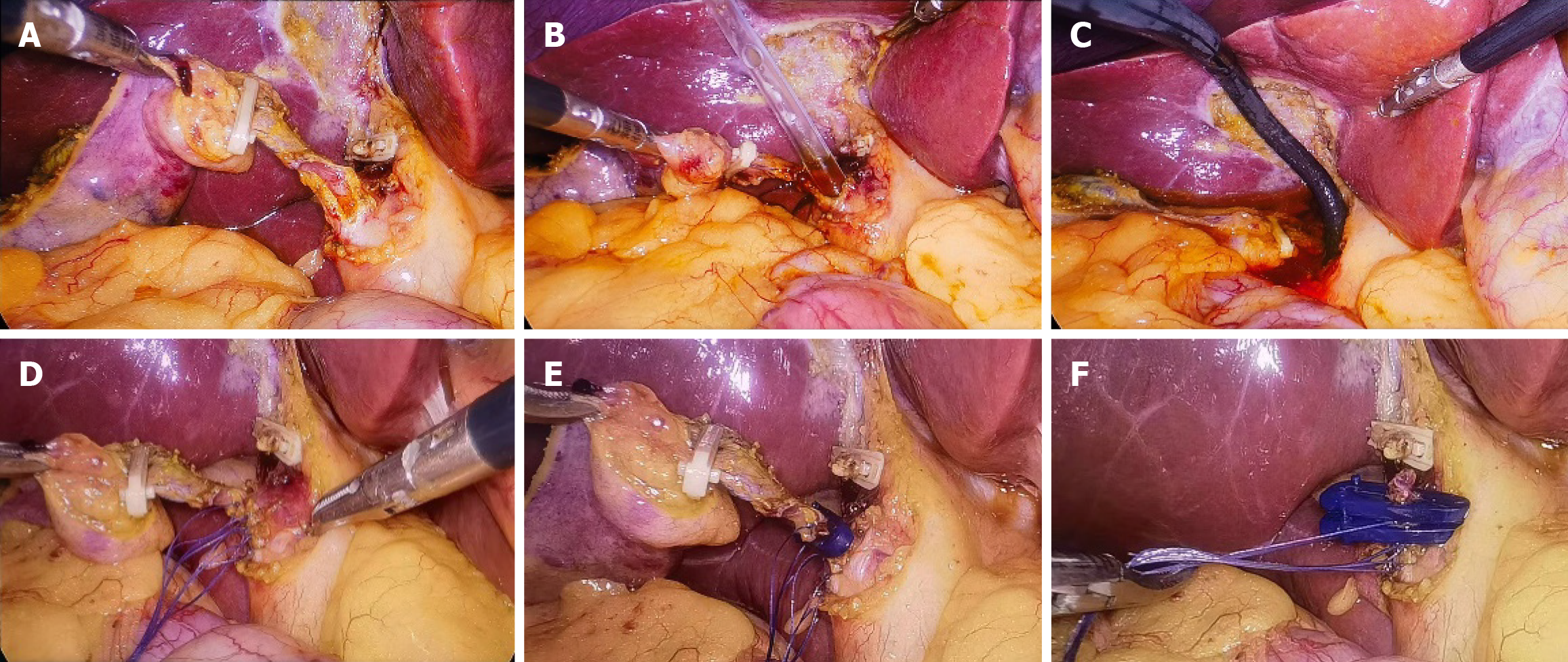
Figure 2 Surgical procedure.
A: Clip the cystic artery and the gallbladder-side of the cystic duct, make a transverse incision on the cystic duct 1-2 cm from the common bile duct, and extend a longitudinal incision from the transverse incision along the cystic duct to its junction with the common bile duct; B: Sequentially insert 6F, 8F, 10F, 12F, 14F, and 16F dilators through the incision to dilate the bile duct; C: Insert a choledochoscope through the cystic duct to explore the common bile duct and remove stones; D: Perform interrupted suture at the junction of the cystic duct and common bile duct with absorbable sutures; E: Clip the cystic duct with absorbable clips; F: Complete cholecystectomy.
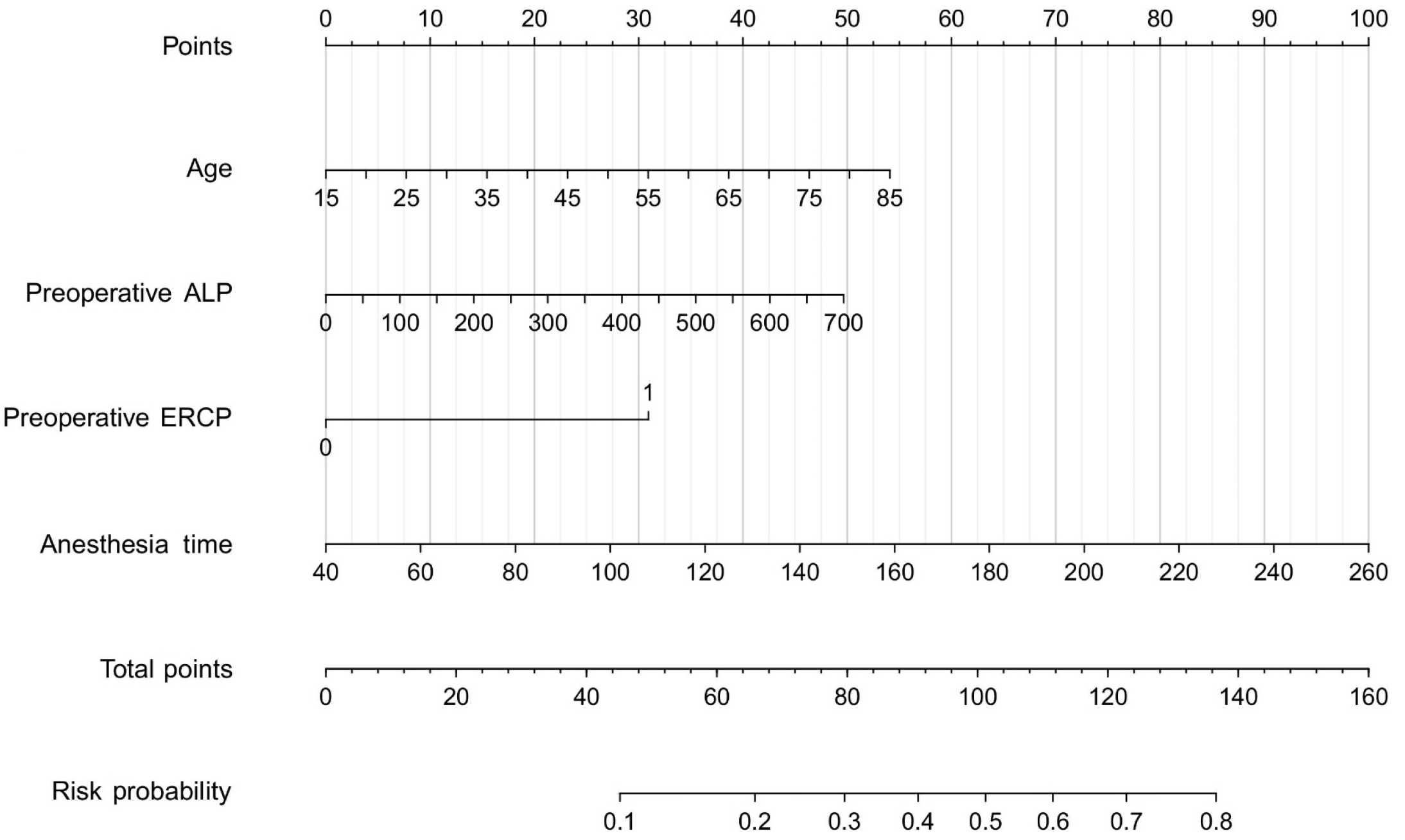
Figure 3 Nomogram for predicting the probability of achieving textbook outcome after laparoscopic transcystic common bile duct exploration.
ALP: Alkaline phosphatase; ERCP: Endoscopic retrograde cholangiopancreatography.
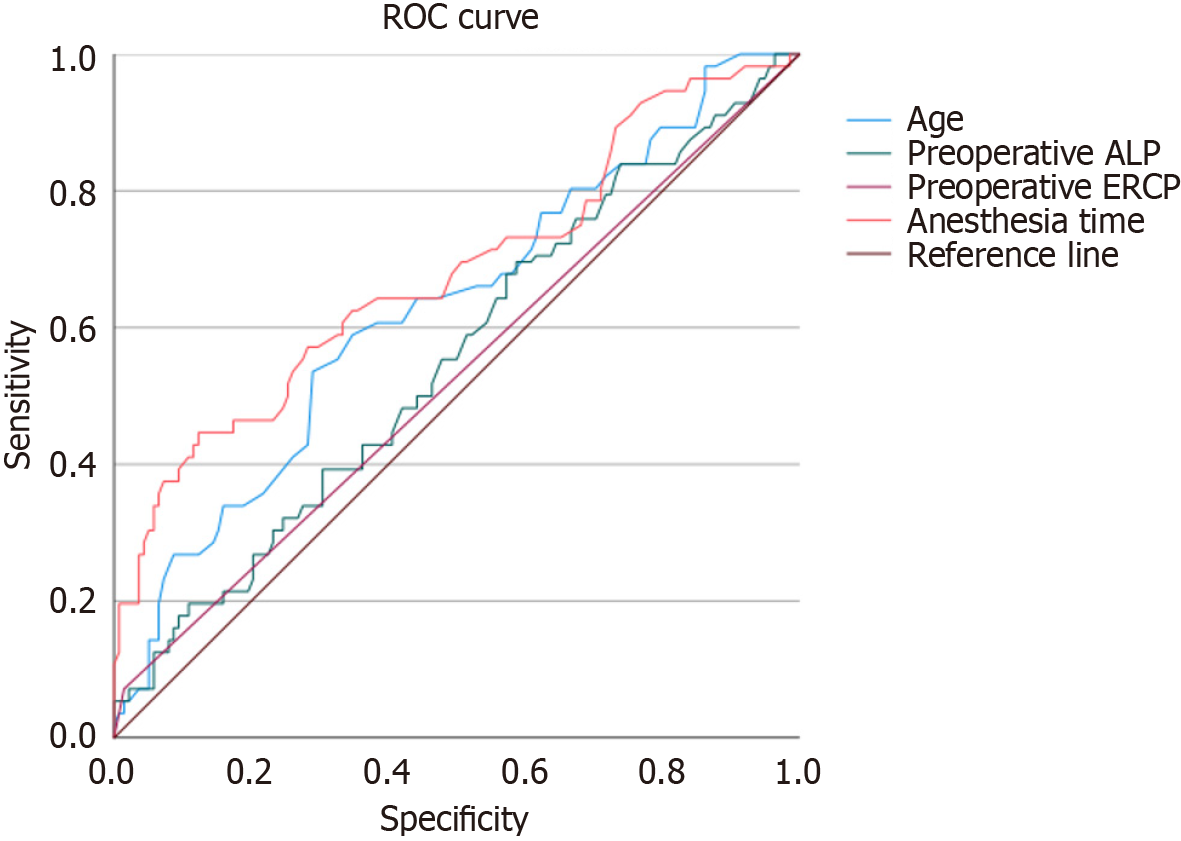
Figure 4 Receiver operating characteristic curve for risk factors associated with textbook outcome failure after laparoscopic transcystic common bile duct exploration.
ROC: Receiver operating characteristic; ALP: Alkaline phosphatase; ERCP: Endoscopic retrograde cholangiopancreatography.
- Citation: Zhu DS, Zhang Z, Huang XR, Zhang JZ, Zhang ZW, Guo XY, Zheng H, Guo T, Yu YH. Textbook outcome and associated risk factors in laparoscopic transcystic common bile duct exploration. World J Gastroenterol 2025; 31(31): 109994
- URL: https://www.wjgnet.com/1007-9327/full/v31/i31/109994.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i31.109994