©The Author(s) 2022.
World J Gastroenterol. Feb 21, 2022; 28(7): 704-714
Published online Feb 21, 2022. doi: 10.3748/wjg.v28.i7.704
Published online Feb 21, 2022. doi: 10.3748/wjg.v28.i7.704
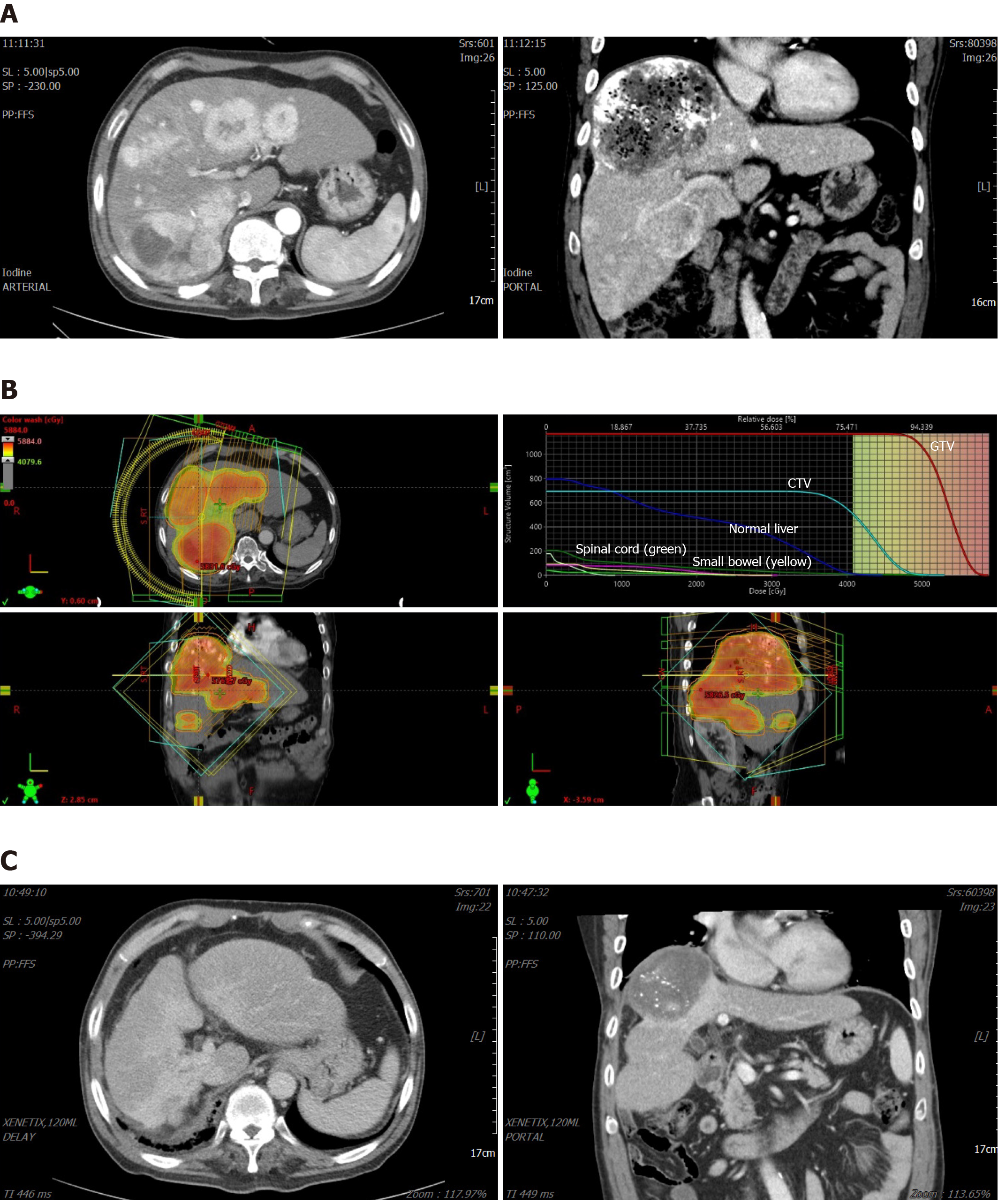
Figure 1 A case of a locally advanced hepatocellular carcinoma with portal thrombosis treated with radiotherapy.
A: Multiple tumors noted in right lobe and segment 4, with a large tumor in segment 8, and involving right portal vein thrombosis; B: A dose-distribution of external radiotherapy plan. We prescribed 53 Gy/20F to gross tumor volume (red color wash in upper-left figure) with at least 42 Gy/20F were delivered to clinical target volume (green color wash in upper-left figure). Quantitative dose-histogram for specific organs is generated (upper-right figure). We planned to save at least 70% of normal liver to be irradiated less than 30 Gy; C: One year after radiotherapy and three times of transarterial chemoembolization, tumors were remised without active enhancing lesions. Liver function was maintained at Child-Pugh score A. GTV: Gross tumor volume; CTV: Clinical target volume.
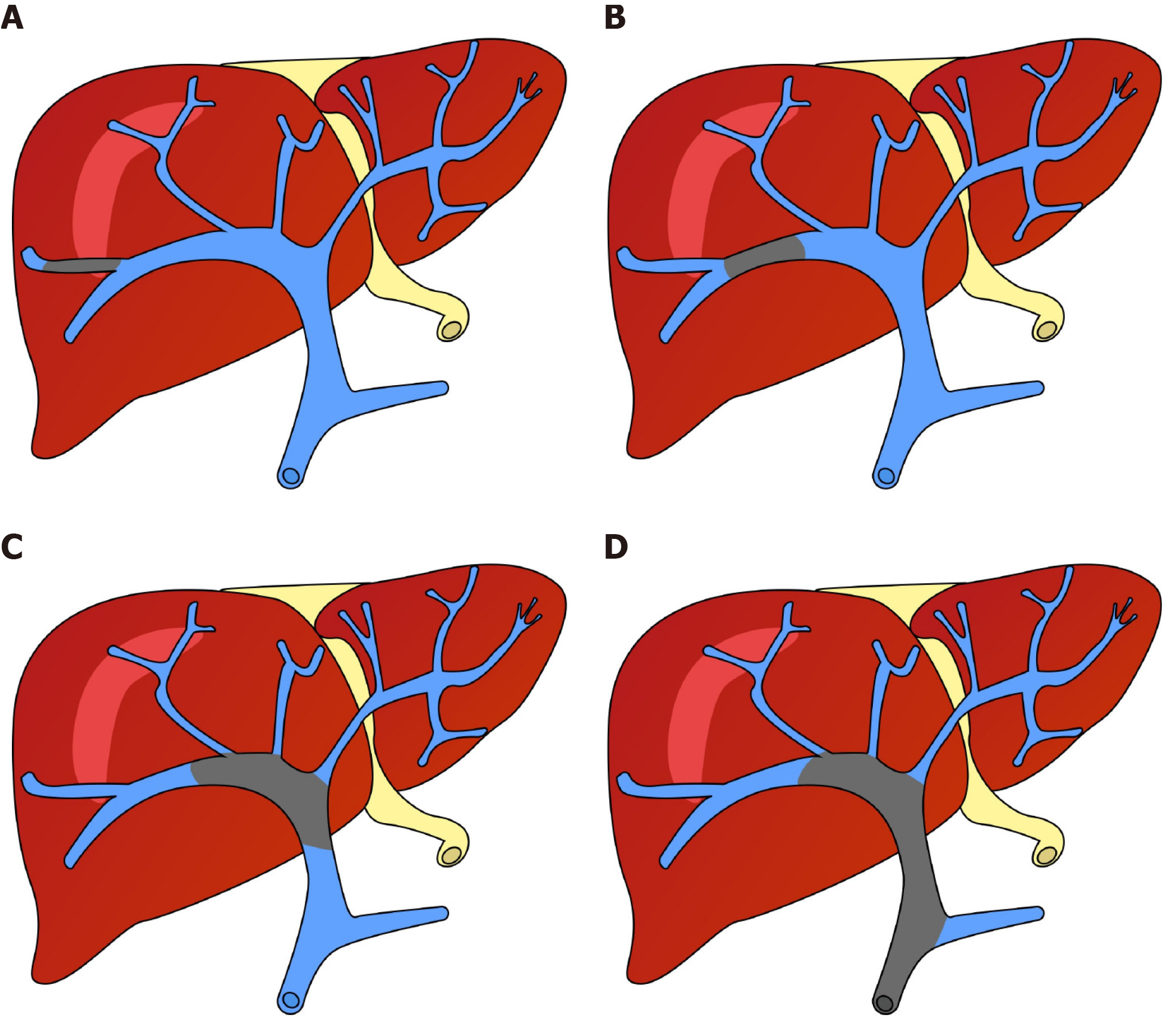
Figure 2 Illustration of two systems categorizing portal vein thrombus.
A: Invasion of the second-order branch of the portal vein: VP2 in the liver cancer study group of Japan (e.g., Vp1 denotes the invasion distal to the second-order branch) and Cheng’s classification type I; B: Invasion of the first-order branch: VP3 and Cheng’s type II; C: Invasion of the main branch and/or bilateral first-order branches: VP4 and Cheng’s type III; D: Invasion of the superior mesenteric vein: Cheng’s type IV.
- Citation: Choe JW, Lee HY, Rim CH. Will the collaboration of surgery and external radiotherapy open new avenues for hepatocellular carcinoma with portal vein thrombosis? World J Gastroenterol 2022; 28(7): 704-714
- URL: https://www.wjgnet.com/1007-9327/full/v28/i7/704.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i7.704