©The Author(s) 2022.
World J Gastroenterol. Mar 14, 2022; 28(10): 976-984
Published online Mar 14, 2022. doi: 10.3748/wjg.v28.i10.976
Published online Mar 14, 2022. doi: 10.3748/wjg.v28.i10.976
Figure 1 Endoscopic ultrasound-guided choledochoduodenostomy.
A: Endosonographic identification of a window for endoscopic ultrasound-guided choledochoduodenostomy in a potentially resectable patient. The common bile duct (CBD) is evaluated from liver hilum to the neoplasia. A spot without intervening vessels is chosen as close as possible to the neoplasia; the caliber of the CBD is evaluated in the direction of the operative channel of the endoscope (yellow dotted line); B: The tip (arrow) of the electrocautery-enhanced lumen apposing metal stent is visibly in touch with the duodenal wall adjacent to a dilated CBD; C: The electrocautery-enhanced lumen apposing metal stent has passed through duodenal and biliary walls, and the distal flange (arrow) has been released inside the CBD; D: The proximal flange has been released inside the bulb with successful drainage of bile flow at the end of the procedure.
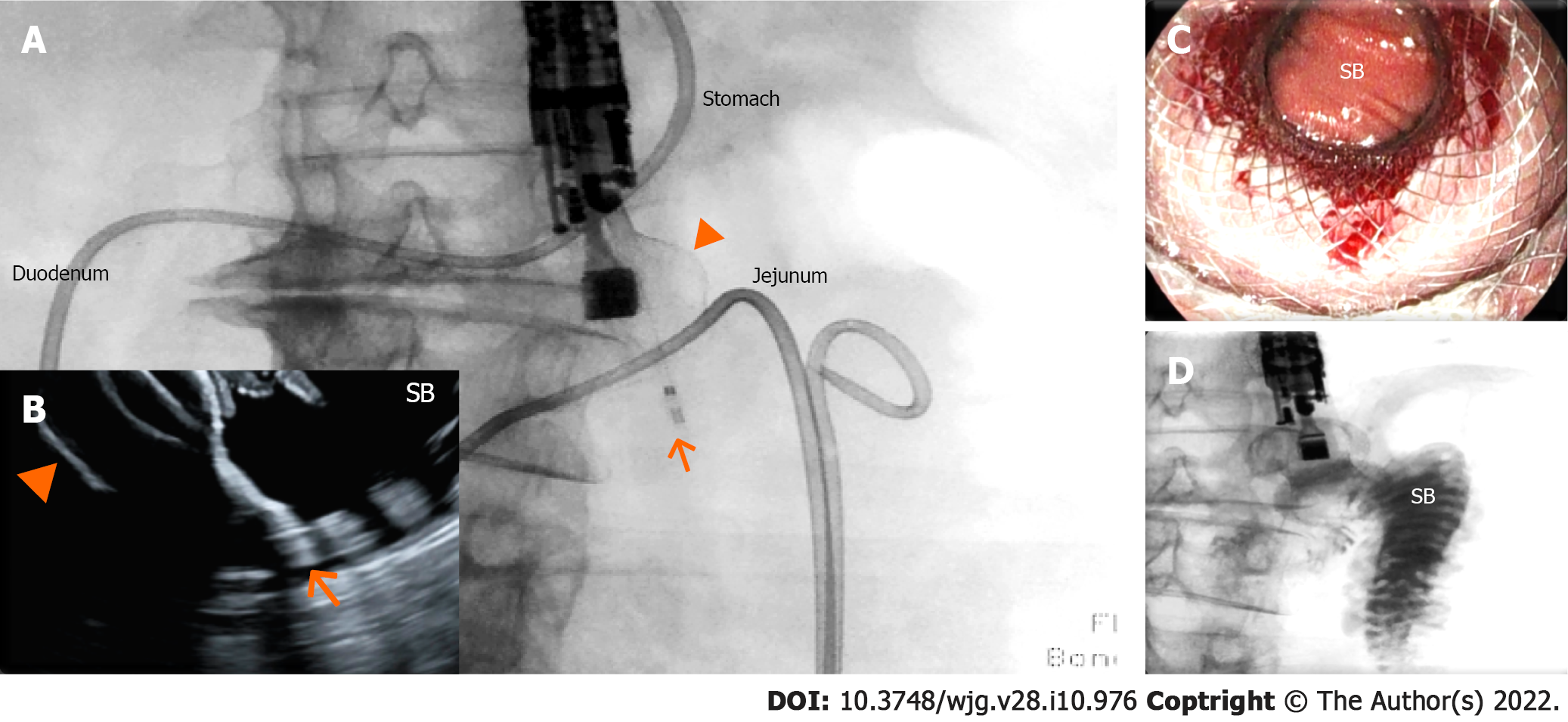
Figure 2 Endoscopic ultrasound-guided gastrojejunostomy.
A and B: The small bowel has been distended with saline infusion through a nasojejunal tube. The dilated jejunal loop has been identified through the gastric wall by endosonography and has been accessed through a 20 mm enhanced lumen apposing metal stent (arrow: tip of the catheter; arrowhead: distal flange); under fluoroscopic (A) and endosonographic (B) guidance, demonstrating the opening of the distal flange (arrowhead) inside the small bowel (SB); C: The proximal flange of the electrocautery-enhanced lumen apposing metal stent has been released and dilated, and the SB can be visualized through the lumen apposing metal stent; D: Contrast injected through the nasojejunal tube can be aspirated through the lumen apposing metal stent inside the stomach.
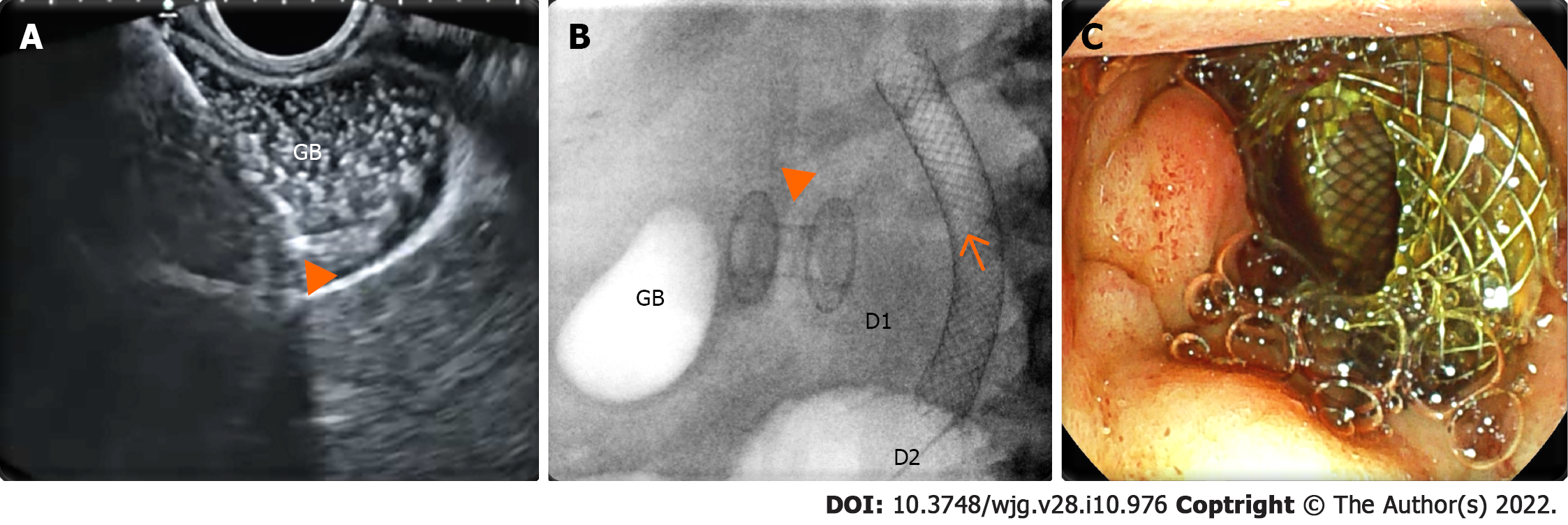
Figure 3 Endoscopic ultrasound-guided gallbladder drainage.
A: Endosonographic view of the delivery system (arrowhead) of the enhanced lumen apposing metal stent inside a distended gallbladder (GB) full of sludge; B: Radioscopic view of the lumen apposing metal stent (arrowhead) released between the gallbladder and duodenal bulb [D1; biliary stent (arrow) released in the second duodenal portion (D2)]; C: Endoscopic view of the proximal flange of the lumen apposing metal stent inside the duodenal bulb.
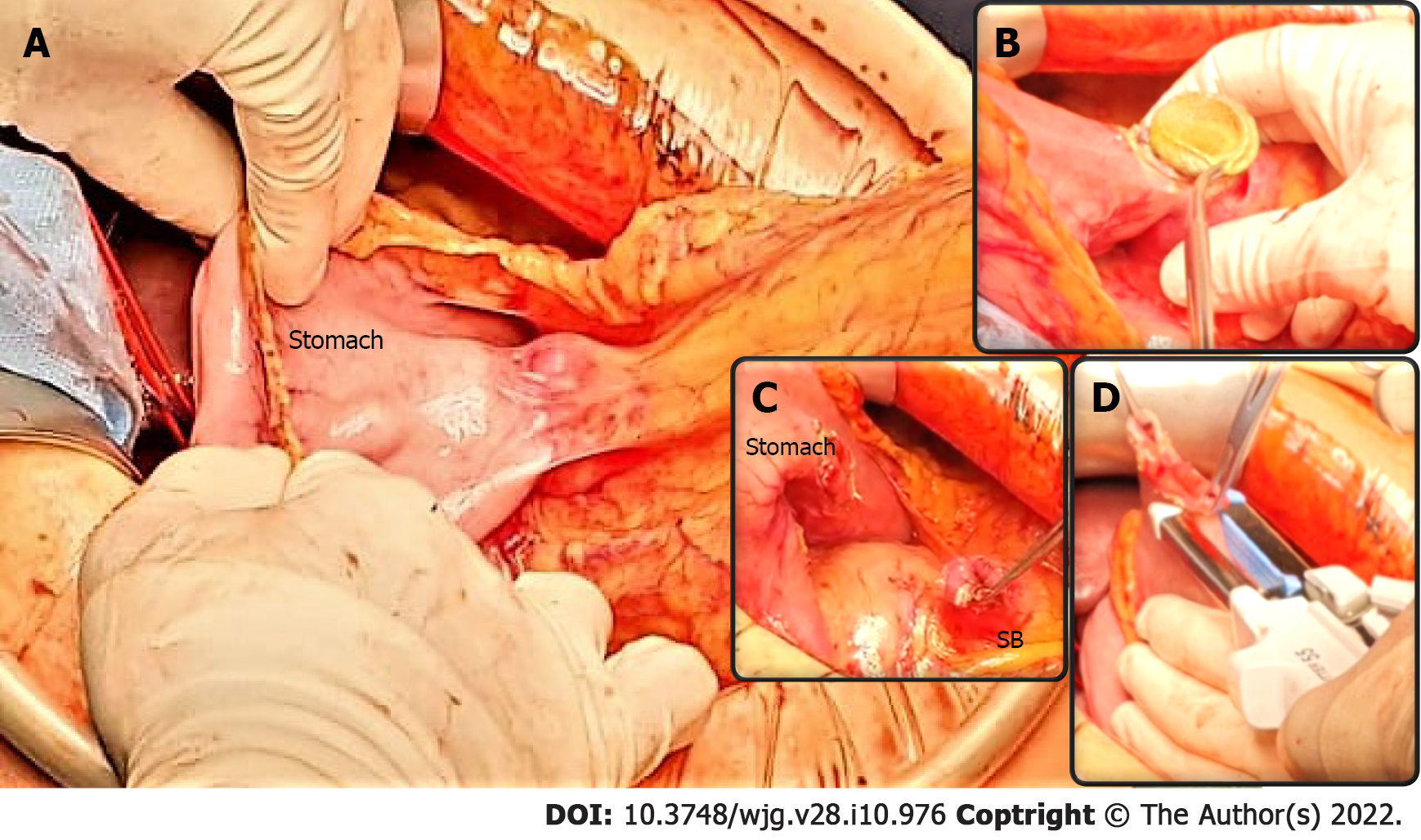
Figure 4 Pancreaticoduodenectomy following endoscopic ultrasound-guided double bypass.
A: The endoscopic ultrasound-guided gastrojejunostomy site is easily identified and a stable gastrojejunal anastomosis is visible (underlined by blue curves) between the stomach and the small bowel (SB); B-C: The endoscopic ultrasound-guided gastrojejunostomy site is opened with diathermic coagulation, the lumen apposing metal stent is removed (B), and the anastomosis cut (C); D: The SB is prepared for gastroenteric anastomosis, while the gastric defect will be closed using staplers. A classic pylorus-preserving pancreaticoduodenectomy is achievable.
Figure 5 Fluoroscopic final image of an endoscopic ultrasound-guided double bypass with choledochobulbostomy and gastroje
- Citation: Vanella G, Tamburrino D, Capurso G, Bronswijk M, Reni M, Dell'Anna G, Crippa S, Van der Merwe S, Falconi M, Arcidiacono PG. Feasibility of therapeutic endoscopic ultrasound in the bridge-to-surgery scenario: The example of pancreatic adenocarcinoma. World J Gastroenterol 2022; 28(10): 976-984
- URL: https://www.wjgnet.com/1007-9327/full/v28/i10/976.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i10.976