Published online Jun 28, 2021. doi: 10.13105/wjma.v9.i3.297
Peer-review started: March 27, 2021
First decision: May 12, 2021
Revised: June 5, 2021
Accepted: July 2, 2021
Article in press: July 2, 2021
Published online: June 28, 2021
Processing time: 107 Days and 3.6 Hours
Fixed ratio combinations (FRCs) of analogue basal insulin and glucagon-like peptide-1 receptor agonists are a newer addition to the therapeutic armamen
To describe and contrast the glycated haemoglobin reduction of two FRCs of analogue basal insulin and glucagon like peptide-1 receptor agonist in adults with type 2 diabetes mellitus.
The following Population, Intervention, Comparison, Outcome question was used for the primary analysis: Among adult patients with type 2 diabetes mellitus [P], what is the effect of iGlarLixi [I] compared to IDegLira [C] for bringing about glycaemic control (as measured by reduction in glycosylated haemoglobin) [O]? The Prisma Statement was used as a guideline for framing this systematic review. We searched PubMed, EMBASE and Cochrane library databases and Clinicaltrials.gov using various keywords and medical search headings related to type 2 diabetes mellitus, iGlarlixi, IDegLira and glycated haemoglobin A1c.
All 14 studies identified by the systematic search met the primary efficacy endpoint of reduction in glycated haemoglobin. There were no head-to-head studies between the FRCs of iGlarlixi and IDegLira, and we therefore did an indirect comparison based on a common comparator of insulin glargine U100. Both iGlarLixi and IDegLira effectively reduce glycated haemoglobin when compared to insulin glargine U100. However, using indirect comparisons, IDegLira had a greater haemoglobin A1c reducing ability (0.6% vs 0.3%). The indirect comparison is limited by the differences between the studies; the fasting blood glucose targets were slightly higher for iGlarLixi studies when compared to the IDegLira studies (4.0-5.0 mmol/L and 4.4-5.6 mmol/L), and the IDegLira study used a greater average dose of insulin glargine when compared to the iGlarLixi studies (66 U/d vs 40 U/d).
Both iGlarLixi and IDegLira effectively reduce glycated haemoglobin. Indirect comparisons, using insulin glargine as the common comparator, suggest that IDegLira reduces glycated haemoglobin to a greater extent than iGlarLixi. However, given the limitations of indirect comparisons, robust head to head studies and real-world data would better inform clinician choice and clinical practice guidelines.
Core Tip: This systematic review investigates the effect of fixed ratio combinations of analogue insulin and glucagon like peptide-1 agonists on reduction of glycated haemoglobin. This systematic review helps fulfil a data gap that will help clinicians decide on comparative efficacy of members of the fixed ratio combination class.
- Citation: Naidoo P, Bouharati C, Rambiritch V, Karamchand S, Tafuto BA, Leisegang RF. Glycated haemoglobin reduction and fixed ratio combinations of analogue basal insulin and glucagon-like peptide-1 receptor agonists: A systematic review. World J Meta-Anal 2021; 9(3): 297-308
- URL: https://www.wjgnet.com/2308-3840/full/v9/i3/297.htm
- DOI: https://dx.doi.org/10.13105/wjma.v9.i3.297
Diabetes mellitus is a heterogeneous disorder of carbohydrate, protein and fat metabolism, characterized by hyperglycaemia secondary to defects in insulin secretion, insulin action or both[1]. In 2019, approximately half a billion patients were living with diabetes, and this number is projected to increase to 700 million by 2045[2]. Globally, diabetes is the 9th most common cause of death[3], and 9.3% of adults aged 20-79 years have diabetes[4]. The economic impact of managing diabetes and its complications are significant, with an estimated global gross domestic product cost of 2.2% by the year 2030[5].
The majority of patients with diabetes can be classified as having either type 1 (± 5%-10%) or type 2 (± 90%-95%) diabetes mellitus[1]. Good glycaemic control prevents microvascular and macrovascular complications in patients with diabetes[6]. Despite the vast armamentarium of therapies that include oral antidiabetic agents and injectables, attainment of glycaemic control remains suboptimal, and the World Health Organization lists diabetes mellitus as a top 10 cause of death[7,8]. Managing adults with diabetes cost US$1.31 trillion globally in 2015[9]. Beyond the medical complications of diabetes, patients may also be negatively impacted from an emotional, psychological and quality of life perspective[10].
The reasons for non-attainment of glycaemic goals are multifactorial and include complexity of treatment regimens and multiple injections. To reduce complexity and the number of daily injections, fixed ratio combinations (FRCs) of analogue basal insulin and glucagon-like peptide-1 (GLP-1) receptor agonists have recently been added[11]. There are currently two FRCs that are marketed: IGlarLixi and IDegLira. Both have the same mode of action, i.e. the analogue basal insulin component increases cellular uptake of glucose and reduces hepatic glucose production, while the GLP-1 receptor agonist stimulates insulin release and inhibits glucagon release[11]. FRCs reduce haemoglobin A1c (HbA1c) by approximately 0.5%[12], and their most common adverse effects are gastro-intestinal events (nausea, vomiting), nasopharyngitis and hypoglycaemia[13,14]. Both are indicated for the management of patients with type 2 diabetes mellitus not controlled on lifestyle modification.
Given the high cost of FRCs and their recent market introduction, there are not many clinical practice guidelines that have assessed them for inclusion. For instance, the World Health Organization[15] and International Diabetes Federation[16] guidelines on diabetes mellitus do not currently include FRCs. In the diabetes field, the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) are leading the path with the publication of a joint guideline for the management of diabetes mellitus which includes FRCs[17]. FRCs have been positioned for patients who are on both GLP-1 receptor agonists and basal analogue insulin.
The joint ADA/EASD consensus statement on the management of patients with type 2 diabetes mellitus does not differentiate between the two FRCs[17]. Clinicians who wish to use FRCs need to consider the body of evidence before choosing between the two marketed products. However, the guideline does not differentiate between the two currently marketed FRCs, and there is no systematic review to assist clinicians decision making. The only systematic review and meta-analysis compare efficacy of FRCs with other classes of anti-diabetic treatments, but none compare iGlarLixi with IDeglira[18]. Both are administered via a once daily subcutaneous injection and present similar adverse effects of hypoglycaemia, nasopharyngitis, nausea and vomiting[13,14]. The average United States cost of a month supply of iGlarLixi and IDegLira is $851.09 and $1245.96, respectively[19,20]. It is important to investigate the efficacy of iGlarLixi compared to IDegLira since it may guide the clinicians when making their decision.
The aim of this systematic review is to describe and contrast the glycated haemog
The review protocol for this systematic review has not been registered. The following Population, Intervention Comparison, Outcome (PICO) question was used for the primary analysis: Among adult patients with type 2 diabetes mellitus [P], what is the effect of iGlarLixi [I] compared to IDegLira [C] for bringing about glycaemic control (as measured by reduction in glycosylated haemoglobin) [O]?
The preferred reporting items for PRISMA Statement was used as a guideline for framing this systematic review[21].
Clinical trials and observational studies investigating the efficacy of FRCs in patients with type 2 diabetes mellitus were identified. We included observational studies to get a sense of the real-world efficacy of FRCs.
Study inclusion criteria were: (1) Male or female, age ≥ 18 years; (2) Subjects diagnosed with type 2 diabetes mellitus; (3) Outpatients receiving treatment with FRCs of iGlarLixi or IDegLira; (4) HbA1c 7.0%-11.0% (both inclusive) (53-97 mmol/mol) by central laboratory analysis; (5) Body mass index ≥ 20 kg/m2 and < 40 kg/m2; (6) Randomised clinical trial or observational study; (7) At least 10 patients per each study group; (8) Dropout rate < 20%; (9) Typically, if an author is included on more than one primary research article that is similar in content, the most recent review or article will be accepted and earlier versions will be rejected; (10) If an author is included on more than one primary research article and the content is different, then both reviews may be accepted; and (11) Studies published in English language.
Study exclusion criteria consisted of: (1) Patients < 18 years; (2) HbA1c > 11%; (3) Hospitalized; (4) History of pancreatic cancer; (5) Renal failure (estimated glomerular filtration rate < 30 mL/min); (6) Liver failure or impairment defined as alanine aminotransferase or aspartate aminotransferase ≥ 2.5 times upper limit of normal; (7) Screening calcitonin ≥ 50 ng/L; (8) Type 1 diabetes mellitus; (9) History of pancreatitis (acute or chronic); (10) Personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia type 2; (11) Subjects presently classified as being in New York Heart Association Class IV; (12) Screening calcitonin ≥ 50 ng/L; (13) Currently pregnant or breastfeeding or not using a reliable method of birth control for the duration of the trial in all females with childbearing potential; (14) < 10 subjects per intervention group; (15) Studies of less than 3-mo duration; (16) Dropout rate > 20%; and (17) Studies not reported in English.
Sixty-six articles were identified by searching PubMed, Embase and Cochrane library databases as well as Clinicaltrials.gov using various keywords and medical search headings (MeSH) related to type 2 diabetes mellitus, iGlarlixi, IDegLira and glycated HbA1c. The complete search syntax conducted on March 21, 2021 was as follows: (1) Patient (((((((((((((((type 2 diabetes mellitus[MeSH Terms]) OR adult-onset diabetes mellitus) OR ketosis-resistant diabetes mellitus) OR maturity-onset diabetes mellitus) OR non-insulin dependent diabetes mellitus) OR non-insulin dependent diabetes mellitus) OR noninsulin dependent diabetes mellitus) OR noninsulin-dependent diabetes mellitus) OR slow-onset diabetes mellitus) OR stable diabetes mellitus) OR type II) OR MODY) OR maturity-onset diabetes)) OR maturity onset diabetes mellitus)) OR NIDDM) OR type 2 diabetes))); (2) Outcome (((((((((((((((((((((glycated hemoglobin[MeSH Terms]) OR (a) OR glycated hemoglobin a1c)) OR OR glycated haemoglobins) OR OR glycohemoglobin a) OR OR glycosylated hemoglobin a) OR OR glycosylated hemoglobin a1c) OR OR hb A1) OR OR Hb A1a+b) OR OR Hb A1a-1) OR OR hb A1a-2) OR OR hb a1b) OR OR hb A1c) OR OR HbA1) OR OR hemoglobin A(1)) OR hemoglobin A)) OR OR glycosylated) OR OR hemoglobin, glycated A1a-2) OR OR hemoglobin, glycated A1b) OR OR hemoglobin, glycosylated) OR OR hemoglobin, glycosylated A1a-1) OR OR hemoglobin, glycosylated A1b)); (3) (1) AND (2); (4) Intervention ((((((glarlixi[MeSH Terms]) OR insulin glargine/lixisenatide) OR (insulin glargine and lixisenatide)) OR soliqua)); (5) Comparator (((((ideglira[MeSH Terms]) OR insulin degludec/Liraglutide) OR (liraglutide and insulin degludec)) OR xultrophy) OR xultrophy 100/3.6)); and (6) (4) OR (5); and (7) (3) AND (6).
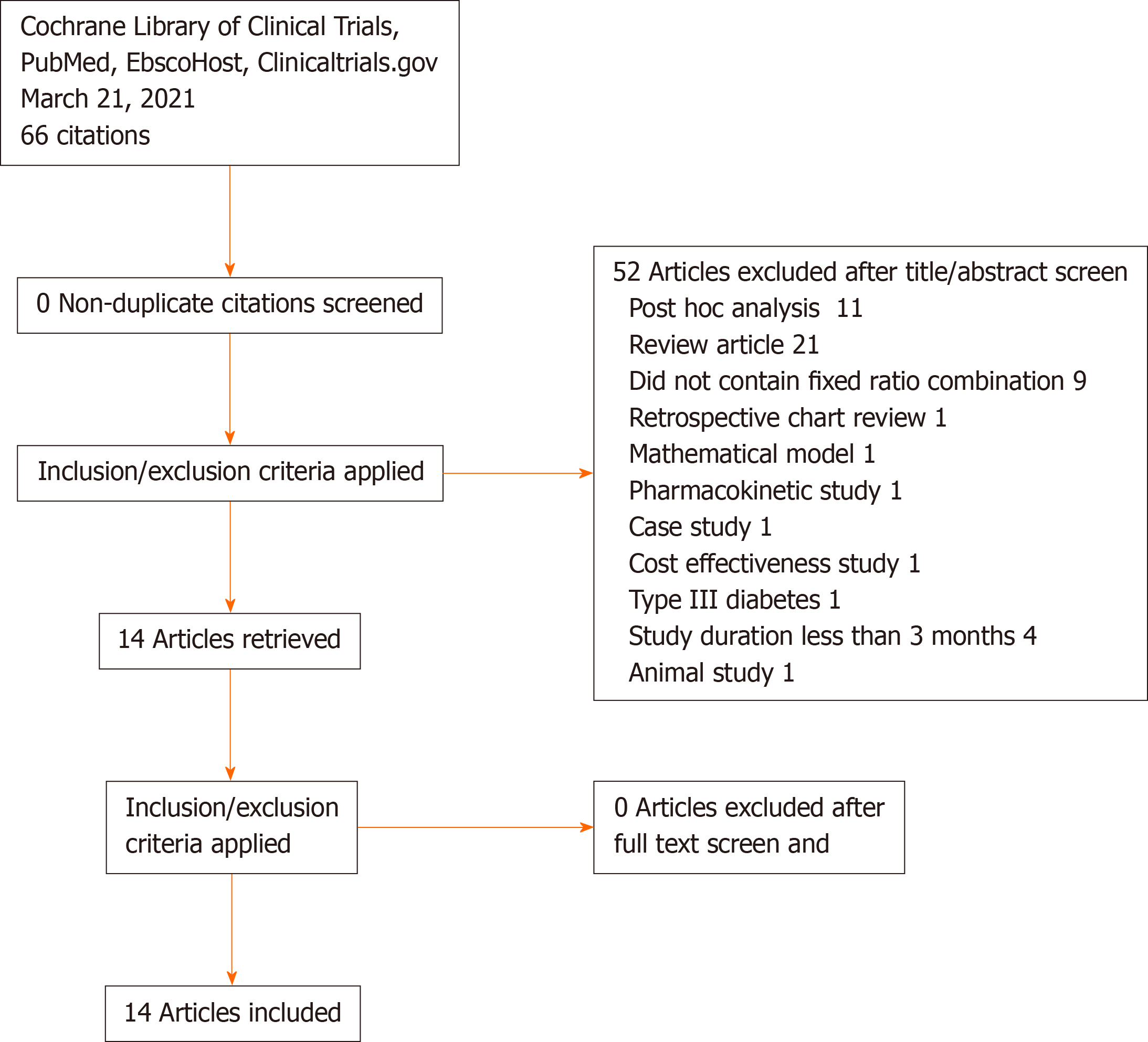
Of the 66 articles that were screened (duplicate n = 0), 52 articles were excluded for the following reasons: Post-hoc analysis (n = 11), review article (n = 21), did not contain FRC (n = 9), retrospective chart review (n = 1), mathematical model (n = 1), pharmacokinetic model (n = 1), case study (n = 1), cost-effectiveness study (n = 1), type III diabetes mellitus (n = 1), study duration less than 3 mo (n = 1) and animal study (n = 1). The remaining 14 articles were used for qualitative synthesis. The PRISMA flow diagram outlining the search process used is provided in Figure 1.
A PICO tracker was used for data extraction. We included key elements from each study, i.e. country location, clinical trial phase, patient population, intervention, comparison, outcome measure, response assessment day, time-points of study measurements and study design. The two study arms were FRC vs comparator.
Bias was assessed using the Cochrane Risk of Bias tool[22]. Studies with seven or greater individual dimensions rated as “High” were assigned an overall “Poor” bias rating, studies with between three and six dimensions rated as “High” were given a “Moderate” overall bias rating and studies with less than three “High” dimensions were given a “Good” overall bias rating.
Since there were no head-to-head studies comparing iGlarLixi with IDeglira, we conducted an indirect comparison. We compared the FRCs if they had a common comparator to ensure that we are comparing “like with like.” From the 14 studies identified, three studies had a common comparison.
The primary outcome measure was reduction in glycated haemoglobin after at least 6 mo of treatment, as per the aim of this systematic review.
In total, 14 studies were identified through the systematic review process. All studies met their primary efficacy endpoint of reduction in glycated haemoglobin. The details of these studies are contained in Supplementary Tables 1 and 2. The majority of the studies were phase III studies, with one phase II study. Except for three studies conducted in Japan, the rest of the studies were multi-country clinical trials. The studies were a minimum of 24 wk and a maximum of 104 wk.
Of the 14 studies identified, none were direct comparisons between FRCs. There
| Ref. | Study design | Patient population | Intervention | Comparator | Efficacy endpoint | Efficacy outcome time-point |
| Lingvay et al[25] | Multinational, multicentre, 26-wk, randomised, open-label, 2-group, treat-to-target trial | Adults with type 2 diabetes | Insulin degludec/liraglutide | Insulin glargine U100 | Baseline HbA1c level was 8.4% for the degludec/liraglutide group and 8.2% for the glargine group. HbA1c level reduction was greater with degludec/liraglutide vs glargine [-1.81% for the degludec/liraglutide group vs -1.13% for the glargine group; estimated treatment difference, -0.59% (95%CI: -0.74 to -0.45)], meeting criteria for noninferiority (P < 0.001) and meeting criteria for statistical superiority (P < 0.001) | 26-wk |
| Rosenstock et al[26] | Randomised, open-label, parallel group, multicentre | Adults with type 2 diabetes | iGlarLixi | Insulin Glargine U100 | Mean HbA1c was reduced from 8.0% at baseline to 6.3% and 6.5% with LixiLan and Gla-100, respectively, establishing statistical noninferiority and superiority of LixiLan [least-squared mean (95%CI) difference: -0.17% (-0.31, -0.04) (-1.9 mmol/mol, -3.4, -0.4); P = 0.01] | 24-wk |
| Rosenstock et al[28] | Randomised, parallel, open label, 3-arm-treatment | Adults with type 2 diabetes | iGlarLixi | Insulin glargine U100; Lixisenatide | Greater reductions in HbA1c from baseline (8.1%) were achieved with iGlarLixi compared with iGlar and Lixi (-1.6%, -1.3%, -0.9%, respectively), reaching mean final HbA1c levels of 6.5% for iGlarLixi vs 6.8% and 7.3% for iGlar and Lixi, respectively (both P < 0.0001) | 30-wk |
In the phase III multinational DUAL V study, Lingvay et al[25] investigated whether IDegLira was non-inferior to up-titration of glargine, with reduction in glycated haemoglobin as the primary efficacy endpoint measured at week 26. Patients had type 2 diabetes and were uncontrolled (HbA1c 7%-10%) despite the use of metformin (≥ 1500 mg/d or maximum tolerated) and insulin glargine (20-50 U/d). Patients were randomised to U100 or IDeglira in a 1:1 ratio. IDeglira was initiated at 16 dose steps (16 U of degludec/0.6 mg of liraglutide). The maximum dose of degludec and liraglutide was 50 U and 1.8 mg, respectively. Patients randomised to glargine continued with their glargine dose, with no maximum allowable dose. Both treatments were titrated to achieve a fasting blood glucose of 4.0-5.0 mmol/L. The final dose of insulin glargine and insulin degludec was 66 U and 41 U, respectively. At week 26, HbA1c had decreased by 1.81% for the IDegLira group (standard deviation 1.08%) and by 1.13% for the glargine group (standard deviation 0.98%); the estimated treatment difference was of 0.59% [95% confidence interval (CI): -0.74-0.45; P < 0.001] and was clinically and statistically significant. Further details of the DUAL V study are contained in Tables 1-3.
In a phase II, proof-of-concept, randomised, open label study, Rosenstock et al[26] investigated the safety and efficacy of iGlarLixi compared to insulin glargine U100 in insulin naïve patients with uncontrolled type 2 diabetes (HbA1c ≥ 7% to ≤ 10%) on a background of metformin (≥ 1500 mg/d for ≥ 3 mo). The primary efficacy endpoint was a reduction in HbA1c at week 24. The starting dose was of 10 U of iGlarLix and 10 U in the U100 group. iGlarlixi and U100 were titrated based on a fasting blood glucose target of 4.4-5.6 mmol/L. The maximum daily dose of iGlarLixi was 60 units U100, which corresponded to a lixisenatide dose of 30 µg. There was no upper limit for the dose of glargine U100. The mean baseline HbA1c ranged from 8.0% to 8.1%. IGlarLixi and insulin glargine U100, resulted in reduction in HbA1c of 1.82% and 1.64%, respectively. The difference between mean change from baseline for iGlarLixi and insulin glargine U100 was -0.17% (P = 0.01). The average dose of insulin glargine U100 was 39 U at week 24.
As a follow up of the above proof-of-concept study, Rosenstock et al[26] conducted a multinational, randomised, open label phase III study in which iGlarLixi was compared to its components, i.e. insulin glargine U100 and lixisenatide. The primary efficacy endpoint was change in HbA1c at week 30. Adults with type 2 diabetes who were uncontrolled on metformin (HbA1c ≥ 7.5% and ≤ 10%) or metformin in combination with other oral antidiabetic agents (HbA1c ≥ 7.0% and ≤ 9.0%) were included. Patients on metformin and second oral agent were asked to discontinue the second oral agent during the run-in phase. During the run-in phase metformin was titrated to at least 2000 mg or the maximum tolerated dose of at least 1500 mg/d. After the run in, patients with an HbA1c of ≥ 7.0% and ≤ 10.0% and fasting plasma glucose ≤ 13.9 mmol/L were randomised to one of the three arms in a 2:2:1 ratio (iGlarLixi; insulin glargine U100; lixisenatide). iGlarLixi and insulin glargine U100 was started at 10 U/d with the maximum allowed dose of 60 U/d. Lixisenatide was started at 10 µg for the first 2 wk and then 20 µg for the rest of the study period. The final mean basal insulin daily dose was 39.8 U and 40.3 U for iGlarLixi and insulin glargine U100, respectively. The baseline HbA1c was 8.1% in all three groups, and mean HbA1c at week 30 were 6.5%, 6.8% and 7.3% for iGlarLixi, insulin glargine U100 and lixisenatide, respectively. The HbA1c difference at week 30 between iGlarLix and insulin glargine U100 was -0.3% (95%CI: -0.4% to -0.2%, P < 0.0001).
All participants were adults with type 2 diabetes with a disease duration of 7-11 years. Both genders were included in the studies, and the majority of participants were Caucasian (89%-98%). Patients were obese (31-32 kg/m2) with a baseline glycated haemoglobin of approximately 8.0%-8.4%. The patient characteristics are listed in Table 2.
| Baseline characteristics | |||||||||||||||||
| Gender | Ethnic origin | OAD at screening | |||||||||||||||
| Ref. | Arms | M (%)/F (%) | White (%) | Black (%) | Asian (%) | Other (%) | Age (yr) | Bodyweight | BMI (kg/ m2) | Duration of Diabetes (yr) | HbA1 (%) | Hb (mmol/mol) | FPG (mmol/L) | Metformin | Metformin plus pioglitazone | Sulphonylurea | Other |
| Lingvay et al[25] | Degludec/liraglutide (n = 278) | 51.4/48.6 | 94.2 | 2.2 | 3.2 | 0.4 | 58.4 | 88.3 | 31.7 | 11.64 | 8.4 | NA | 8.9 | NA | NA | NA | NA |
| Glargine (n = 279) | 49.1/50.9 | 95.0 | 1.8 | 3.2 | 0.0 | 59.1 | 87.3 | 31.7 | 11.33 | 8.2 | NA | 8.9 | NA | NA | NA | NA | |
| Rosenstock et al[26] | LixiLan (n = 161) | 49.7/50.3 | 98.1 | NA | NA | NA | 56.9 | 90.1 | 32.2 | 6.3 | 8.1 | 64 | 9.8 | Yes | NA | NA | NA |
| Gla-100 (n = 162) | 52.5/47.5 | 98.8 | NA | NA | NA | 56.6 | 91.6 | 32.0 | 7.1 | 8.0 | 64 | 9.5 | Yes | NA | NA | NA | |
| Rosenstock et al[28] | iGlarLixi (n = 469) | 47.3/52.7 | 88.9 | 7.0 | 1.7 | 2.3 | 58.2 | NA | 31.6 | 8.9 | 8.1 | 65 | 9.9 | Yes | NA | 55.2 | Glinide, Sodium glucose co-transporter inhibitor, dipeptidyl dipeptidase 4 inhibitor |
| iGlar (n = 467) | 50.7/49.3 | 90.1 | 7.1 | 1.5 | 1.3 | 58.3 | NA | 31.7 | 8.7 | 8.1 | 65 | 9.8 | Yes | NA | 53.3 | ||
| Lixi (n = 234) | 56.8/43.2 | 92.3 | 5.1 | 1.3 | 1.3 | 58.7 | NA | 32.0 | 8.9 | 8.1 | 65 | 9.8 | Yes | NA | 52.6 | ||
| All (n = 1170) | 50.6/49.4 | 90.1 | 6.7 | 1.5 | 1.7 | 58.4 | NA | 31.7 | 8.8 | 8.1 | 65 | 9.8 | Yes | NA | 53.9 | ||
| Ref. | Selection bias: Random sequence generation | Selection bias: Allocation concealment | Performance bias: Blinding of participants | Performance bias: Blinding of personnel/care providers | Detection bias: Blinding of outcome assessor | Attrition bias: Incomplete outcome data | Reporting bias: Selective outcome reporting | Intention-to-treat-analysis | Selection bias: Group similarity at baseline | Performance bias: Co-interventions | Performance bias: Compliance | Detection bias: Timing of outcome assessments | Additional bias | Overall quality |
| Lingvay et al[25] | L | H | H | H | L | L | L | L | L | L | L | L | L | Moderate |
| Rosenstock et al[26] | L | H | H | H | L | L | L | L | L | L | L | L | L | Moderate |
| Rosenstock et al[28] | L | H | H | H | L | L | L | L | L | L | L | L | L | Moderate |
Given that treatment was randomly allocated, the intervention and comparator arms were balanced with respect to baseline characteristics and glycated haemoglobin. The interventions were the FRCs compared with insulin glargine U100.
The primary efficacy outcome was reduction of glycated haemoglobin assessed after at least 24 wk. We did not assess secondary efficacy outcomes of reduction in fasting and postprandial glucose levels. We also did not assess safety as this was beyond the scope of this systematic review.
Risk of bias and study quality were assessed for each included study using Cochrane Risk of Bias tool[22]. Differences in rating were resolved via discussion and consensus among all authors. The quality assessment for each study is contained in Table 3. The studies were industry sponsored randomised phase II-III studies with a moderate risk of bias. The major limitation was the open-label design.
This systematic review described the ability of FRCs to reduce glycated haemoglobin. Both iGlarLixi and IDeglira reduced HbA1c and met their primary efficacy endpoints in the 14 clinical trials identified in this systematic review. Our findings are similar to those of the systematic review and meta-analysis of Liakopoulou et al[27] who showed effective glycaemic control with FRCs when compared with each individual component alone (change in HbA1c -0.31%; 95%CI: -0.47 to -0.16; I2 = 81 and -0.73%; 95%CI: -0.87 to -0.58; I2 = 74% compared with basal insulin and GLP-1 RA, respectively).
The studies identified in our systematic review were well designed in general with a moderate risk of bias as assessed by the Cochrane risk of bias tool[22]. The key limitation of the studies was the use of an open label design in which both study participants and investigators were not blinded to interventions.
Given the lack of head-to-head studies of iGlarLixi and IDeglira, we used an indirect comparison to get a sense if there were differences in HbA1c reducing ability of the FRCs. There were three studies in which insulin glargine U100 was the common comparator[25,26,28]. IDegLira reduced glycated haemoglobin to a greater extent than iGlarLixi (approximately 0.6% vs 0.3%). However, indirect comparisons have challenges as the studies do have differences that do not allow for firm conclusions. For example, although the studies were treat-to target studies, the target ranges were different with IDegLira and iGlarLixi being 4.0-5.0 mmol/L and 4.4-5.6 mmol/L, respectively[25,28]. Furthermore, the IDegLira study used greater average doses of glargine when compared to the iGlarLixi studies (66 U/d vs 40 U/d)[25,28].
Based on indirect comparison, the difference in HbA1c reduction may be a chance finding or due to inherent differences between the studies, e.g., different countries, different investigators and varying doses. Furthermore, there is no biological plausibility that would explain the HbA1c reducing difference between iGlarLixi and IDeglira.
Glycated haemoglobin is only a validated surrogate measure of microvascular complications (retinopathy, nephropathy, neuropathy)[29-37]; ideally one would need to have studies that determine the effect of FRCs on major adverse cardiovascular events, e.g., myocardial infarction, cerebro-vascular accident, peripheral vascular disease and ultimately mortality.
Although the studies were of reasonable duration (at least 24 wk), one would require long term studies to determine the durability of glycated haemoglobin. Ideally one would need a head to head study to determine the differences in safety, efficacy and tolerability between the two FRCs. However, it is unlikely that this would be done given the high costs of doing such a study. Perhaps real-world evidence may help differentiate between the FRCs. A network meta-analysis may assist with informing the relative efficacy and safety of the FRCs. Pharmacoeconomic considerations may also help differentiate between these agents.
Clinical trials help inform clinical practice guidelines. However, there are many factors influencing the translation of clinical practice guidelines to clinical practice. Factors include the level of evidence and the grade of recommendation, the credibility and expertise of the guideline committee, economic factors and physician and patient preference. Given the current lack of head-to-head studies between iGlarLixi and IDeglira, it is not surprising that the joint ADA/EASD guideline[15] does not differentiate between the individual FRCs. It is unlikely that this systematic review would result in a change of the clinical trial guidelines given that it only looks at differences in reduction of glycated haemoglobin and is also an indirect comparison, with its inherent limitations.
Both iGlarLixi and IDegLira effectively reduce glycated haemoglobin. Indirect comparisons, using insulin glargine as a common comparator, indicate that IDegLira reduces glycated haemoglobin to a greater extent than does iGlarLixi. However, given the limitations of indirect comparisons, robust head to head studies and real-world data are needed to inform clinical practice guidelines.
Fixed ratio combinations of insulin and glucagon-like peptide-1 analogues are novel therapy for the management of patients with type 2 diabetes mellitus.
There is minimal data comparing the fixed ratio combinations of iGlarlixi and IDegLira.
We aimed to compare the glucose lowering effect of iGlarLixi vs IDegLira.
We used a Population, Intervention, Comparison, Outcome (PICO) question for the primary analysis.
Both iGlarLixi and IDegLira effectively reduce glycated haemoglobin when compared to insulin glargine U100. However, using indirect comparisons, IDegLira had a greater HbA1c reducing ability (0.6% vs 0.3%).
Both iGlarLixi and IDegLira effectively reduce glycated haemoglobin.
Head to head studies between iGlarlixi and IDegLira are required to determine if there are clinically relevant differences between the two aforementioned fixed ratio combinations.
Dr. Roopnarain C for assisting with construction of tables.
| 1. | American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2004;27 Suppl 1:S5-S10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 955] [Cited by in RCA: 1016] [Article Influence: 46.2] [Reference Citation Analysis (0)] |
| 2. | Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R; IDF Diabetes Atlas Committee. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5345] [Cited by in RCA: 6393] [Article Influence: 913.3] [Reference Citation Analysis (12)] |
| 3. | World Health Organization. The top 10 causes of death. [cited 21 March 2021]. In: World Health Organization [Internet]. Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death#:~:text=The%20top%20global%20causes%20of%20death, %20in%20order,neonatal%20sepsis%20and%20infections,%20and%20preterm%20birth%20complications. |
| 4. | International Diabetes Federation. IDF Diabetes Atlas. 9th edition 2019. [cited 29 November 2019]. In: International Diabetes Federation [Internet]. Available from: https://www.diabetesatlas.org/en/. |
| 5. | Bommer C, Sagalova V, Heesemann E, Manne-Goehler J, Atun R, Bärnighausen T, Davies J, Vollmer S. Global Economic Burden of Diabetes in Adults: Projections From 2015 to 2030. Diabetes Care. 2018;41:963-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 484] [Cited by in RCA: 707] [Article Influence: 88.4] [Reference Citation Analysis (0)] |
| 6. | Nathan DM; DCCT/EDIC Research Group. The diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: overview. Diabetes Care. 2014;37:9-16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 866] [Cited by in RCA: 1061] [Article Influence: 88.4] [Reference Citation Analysis (0)] |
| 7. | Foster NC, Beck RW, Miller KM, Clements MA, Rickels MR, DiMeglio LA, Maahs DM, Tamborlane WV, Bergenstal R, Smith E, Olson BA, Garg SK. State of Type 1 Diabetes Management and Outcomes from the T1D Exchange in 2016-2018. Diabetes Technol Ther. 2019;21:66-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1048] [Cited by in RCA: 1497] [Article Influence: 213.9] [Reference Citation Analysis (0)] |
| 8. | World Health Organization. The top 10 causes of death. 2018. [cited 14 September 2019]. In: World Health Organization [Internet]. Available from: https://www.who.int/en/news-room/fact-sheets/detail/the-top-10-causes-of-death (Links to an external site.). |
| 9. | Bommer C, Heesemann E, Sagalova V, Manne-Goehler J, Atun R, Bärnighausen T, Vollmer S. The global economic burden of diabetes in adults aged 20-79 years: a cost-of-illness study. Lancet Diabetes Endocrinol. 2017;5:423-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 415] [Cited by in RCA: 521] [Article Influence: 57.9] [Reference Citation Analysis (0)] |
| 10. | Pearce MJ, Pereira K, Davis E. The psychological impact of diabetes: a practical guide for the nurse practitioner. J Am Assoc Nurse Pract. 2013;25:578-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Blumer I, Pettus JH, Santos Cavaiola T. Fixed-ratio combination therapy for type 2 diabetes: the top ten things you should know about insulin and glucagon-like peptide-1 receptor agonist combinations. Postgrad Med. 2018;130:375-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Maiorino MI, Chiodini P, Bellastella G, Capuano A, Esposito K, Giugliano D. Insulin and Glucagon-Like Peptide 1 Receptor Agonist Combination Therapy in Type 2 Diabetes: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Diabetes Care. 2017;40:614-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 100] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 13. | Food and Drug Administration. Center for Drug Evaluation and Research. Soliqua label. [cited 11 November 2019]. In: Food and Drug Administration [Internet]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2016/208673Orig1s000Lbl.pdf. |
| 14. | Food and Drug Administration. Xultrophy label. Center for Drug Evaluation and Research. [cited 11 November 2019]. In: Food and Drug Administration [Internet]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/Label/2016/208583s000Lbl.pdf. |
| 15. | Davies MJ, D'Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, Rossing P, Tsapas A, Wexler DJ, Buse JB. Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2018;61:2461-2498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 944] [Cited by in RCA: 812] [Article Influence: 101.5] [Reference Citation Analysis (0)] |
| 16. | Roglic G, Norris SL. Medicines for Treatment Intensification in Type 2 Diabetes and Type of Insulin in Type 1 and Type 2 Diabetes in Low-Resource Settings: Synopsis of the World Health Organization Guidelines on Second- and Third-Line Medicines and Type of Insulin for the Control of Blood Glucose Levels in Nonpregnant Adults With Diabetes Mellitus. Ann Intern Med. 2018;169:394-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 17. | International Diabetes Federation. Recommendations for Managing Type 2 Diabetes in Primary Care, 2017. [cited 10 October 2019]. In: International Diabetes Federation [Internet]. Available from: https://www.idf.org/managing-type2-diabetes. |
| 18. | Cai X, Gao X, Yang W, Ji L. Comparison between insulin degludec/Liraglutide treatment and insulin glargine/Lixisenatide treatment in type 2 diabetes: a systematic review and meta-analysis. Expert Opin Pharmacother. 2017;18:1789-1798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | GoodRx. Soliqua 100/33. [cited 29 November 2019]. In: GoodRx [Internet]. Available from: https://www.goodrx.com/soliqua-100-33. |
| 20. | GoodRx. Xultrophy. [cited 29 November 2019]. In: GoodRx [Internet]. Available from: https://www.goodrx.com/xultophy. |
| 21. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6253] [Cited by in RCA: 7869] [Article Influence: 462.9] [Reference Citation Analysis (3)] |
| 22. | Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18487] [Cited by in RCA: 26218] [Article Influence: 1747.9] [Reference Citation Analysis (4)] |
| 23. | Kaku K, Araki E, Tanizawa Y, Ross Agner B, Nishida T, Ranthe M, Inagaki N. Superior efficacy with a fixed-ratio combination of insulin degludec and liraglutide (IDegLira) compared with insulin degludec and liraglutide in insulin-naïve Japanese patients with type 2 diabetes in a phase 3, open-label, randomized trial. Diabetes Obes Metab. 2019;21:2674-2683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | Kiefer C, Sturtz S, Bender R. Indirect Comparisons and Network Meta-Analyses. Dtsch Arztebl Int. 2015;112:803-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 25. | Lingvay I, Pérez Manghi F, García-Hernández P, Norwood P, Lehmann L, Tarp-Johansen MJ, Buse JB; DUAL V Investigators. Effect of Insulin Glargine Up-titration vs Insulin Degludec/Liraglutide on Glycated Hemoglobin Levels in Patients With Uncontrolled Type 2 Diabetes: The DUAL V Randomized Clinical Trial. JAMA. 2016;315:898-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 174] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 26. | Rosenstock J, Diamant M, Aroda VR, Silvestre L, Souhami E, Zhou T, Perfetti R, Fonseca V; LixiLan PoC Study Group. Efficacy and Safety of LixiLan, a Titratable Fixed-Ratio Combination of Lixisenatide and Insulin Glargine, Versus Insulin Glargine in Type 2 Diabetes Inadequately Controlled on Metformin Monotherapy: The LixiLan Proof-of-Concept Randomized Trial. Diabetes Care. 2016;39:1579-1586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 63] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 27. | Liakopoulou P, Liakos A, Vasilakou D, Athanasiadou E, Bekiari E, Kazakos K, Tsapas A. Fixed ratio combinations of glucagon like peptide 1 receptor agonists with basal insulin: a systematic review and meta-analysis. Endocrine. 2017;56:485-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 28. | Rosenstock J, Aronson R, Grunberger G, Hanefeld M, Piatti P, Serusclat P, Cheng X, Zhou T, Niemoeller E, Souhami E, Davies M; LixiLan-O Trial Investigators. Benefits of LixiLan, a Titratable Fixed-Ratio Combination of Insulin Glargine Plus Lixisenatide, Versus Insulin Glargine and Lixisenatide Monocomponents in Type 2 Diabetes Inadequately Controlled on Oral Agents: The LixiLan-O Randomized Trial. Diabetes Care. 2016;39:2026-2035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 213] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 29. | FDA-NIH Biomarker Working Group. BEST (Biomarkers, EndpointS, and other Tools) Resource [Internet]. Silver Spring (MD): Food and Drug Administration (US); 2016-. Validated Surrogate Endpoint. 2017 Sep 25. Co-published by National Institutes of Health (US), Bethesda (MD). [cited 21 November 2019]. In: National Center for Biotechnology Information [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK453484/. |
| 30. | Watada H, Kaneko S, Komatsu M, Agner BR, Nishida T, Ranthe M, Nakamura J. Superior HbA1c control with the fixed-ratio combination of insulin degludec and liraglutide (IDegLira) compared with a maximum dose of 50 units of insulin degludec in Japanese individuals with type 2 diabetes in a phase 3, double-blind, randomized trial. Diabetes Obes Metab. 2019;21:2694-2703. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 31. | Rodbard HW, Bode BW, Harris SB, Rose L, Lehmann L, Jarlov H, Thurman J; Dual Action of Liraglutide and insulin degludec (DUAL) IV trial investigators. Safety and efficacy of insulin degludec/Liraglutide (IDegLira) added to sulphonylurea alone or to sulphonylurea and metformin in insulin-naïve people with Type 2 diabetes: the DUAL IV trial. Diabet Med. 2017;34:189-196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 79] [Cited by in RCA: 90] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 32. | Philis-Tsimikas A, Billings LK, Busch R, Portillo CM, Sahay R, Halladin N, Eggert S, Begtrup K, Harris S. Superior efficacy of insulin degludec/Liraglutide vs insulin glargine U100 as add-on to sodium-glucose co-transporter-2 inhibitor therapy: A randomized clinical trial in people with uncontrolled type 2 diabetes. Diabetes Obes Metab. 2019;21:1399-1408. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 58] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 33. | Aroda VR, González-Galvez G, Grøn R, Halladin N, Haluzík M, Jermendy G, Kok A, Őrsy P, Sabbah M, Sesti G, Silver R. Durability of insulin degludec plus liraglutide vs insulin glargine U100 as initial injectable therapy in type 2 diabetes (DUAL VIII): a multicentre, open-label, phase 3b, randomised controlled trial. Lancet Diabetes Endocrinol. 2019;7:596-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 34. | Billings LK, Doshi A, Gouet D, Oviedo A, Rodbard HW, Tentolouris N, Grøn R, Halladin N, Jodar E. Efficacy and Safety of IDegLira Versus Basal-Bolus Insulin Therapy in Patients With Type 2 Diabetes Uncontrolled on Metformin and Basal Insulin: The DUAL VII Randomized Clinical Trial. Diabetes Care. 2018;41:1009-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 147] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 35. | Harris SB, Kocsis G, Prager R, Ridge T, Chandarana K, Halladin N, Jabbour S. Safety and efficacy of IDegLira titrated once weekly vs twice weekly in patients with type 2 diabetes uncontrolled on oral antidiabetic drugs: DUAL VI randomized clinical trial. Diabetes Obes Metab. 2017;19:858-865. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 36. | Gough SC, Bode B, Woo V, Rodbard HW, Linjawi S, Poulsen P, Damgaard LH, Buse JB; NN9068-3697 (DUAL-I) trial investigators. Efficacy and safety of a fixed-ratio combination of insulin degludec and liraglutide (IDegLira) compared with its components given alone: results of a phase 3, open-label, randomised, 26-week, treat-to-target trial in insulin-naive patients with type 2 diabetes. Lancet Diabetes Endocrinol. 2014;2:885-893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 271] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 37. | Gough SC, Bode BW, Woo VC, Rodbard HW, Linjawi S, Zacho M, Reiter PD, Buse JB. One-year efficacy and safety of a fixed combination of insulin degludec and liraglutide in patients with type 2 diabetes: results of a 26-week extension to a 26-week main trial. Diabetes Obes Metab. 2015;17:965-973. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 102] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Africa
Peer-review report’s scientific quality classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): E, E
P-Reviewer: Al-Hadhrami R, Athyros VG, Duan W, Li SY S-Editor: Gao CC L-Editor: Filipodia P-Editor: Li JH