Published online Sep 25, 2025. doi: 10.5527/wjn.v14.i3.105288
Revised: March 26, 2025
Accepted: June 9, 2025
Published online: September 25, 2025
Processing time: 243 Days and 15.5 Hours
Urolithiasisposes challenges in patients with chronic kidney disease (CKD), nece
To assess the safety, feasibility, and efficacy of surgical interventions for uro
Systematic review adhering to PRISMA guidelines. Comprehensive searches of PubMed, Scopus, Cochrane Library, Web of Science, and Embase were conducted for studies published from January 2014 to June 2024. Studies involving adult patients (≥ 18 years) with CKD undergoing surgical interventions for urolithiasis, including randomized controlled trials, cohort studies, case-control studies, and observational studies. Studies involving pediatric patients, those not specifically addressing CKD patients, review articles, commentaries, and editorials. Despite an extensive search, only six studies met the strict inclusion criteria, reflecting the limited available data on this topic. This limitation has been acknowledged and discussed.
A total of 6 studies met the inclusion criteria, encompassing a diverse range of surgical interventions such as percutaneous nephrolithotomy (PCNL), ureteroscopy (URS), and extracorporeal shock wave lithotripsy (ESWL). Perioperative and postoperative complications varied across studies, with bleeding, infection, and acute kidney injury being the most common. The risk of complications was higher in patients with advanced CKD. Technical success rates were generally high, but feasibility was influenced by patient-specific factors such as CKD stage and comorbidities. Modifications to standard surgical techniques were often necessary. Stone-free rates and recurrence rates varied, with PCNL generally achieving higher stone-free rates compared to URS and ESWL. Long-term outcomes on renal function were inconsistent, highlighting the need for individualized treatment plans.
Surgical interventions for urolithiasis in CKD patients are associated with significant risks but can be effective in achieving stone clearance and symptom relief. The safety, feasibility, and efficacy of these interventions depend on patient-specific factors, necessitating a tailored approach. Further high-quality studies are needed to develop standardized guidelines and improve clinical outcomes in this complex patient population.
Core Tip: This systematic review evaluates the safety, feasibility, and efficacy of surgical interventions for urolithiasis in patients with chronic kidney disease (CKD). Key findings highlight that while techniques such as percutaneous nephrolithotomy, ureteroscopy, and shock wave lithotripsy achieve technical success rates, they are associated with significant risks, including bleeding, infection, and acute kidney injury, especially in advanced CKD. Modifications to standard surgical methods are often required to address patient-specific factors. Stone-free rates vary across interventions, and long-term renal outcomes remain inconsistent, emphasizing the need for individualized treatment plans and further high-quality research to guide optimal management of patients with CKD.
- Citation: Navriya SC, Yadav OK, Shettar A, Singh M, Jain J, Kumar S, Bhirud DP, Choudhary GR, Sandhu AS. Safety, feasibility, and efficacy of surgical intervention for Urolithiasis in patients with chronic kidney disease: A systematic review. World J Nephrol 2025; 14(3): 105288
- URL: https://www.wjgnet.com/2220-6124/full/v14/i3/105288.htm
- DOI: https://dx.doi.org/10.5527/wjn.v14.i3.105288
Urolithiasis, commonly known as kidney stones, is a prevalent urological condition characterized by the formation of calculi within the urinary tract. The global incidence and prevalence of urolithiasis have been increasing, contributing significantly to morbidity and healthcare costs. Urolithiasis, or kidney stone disease, is a prevalent condition with significant global incidence, affecting 1 in 11 people in the United States alone. Chronic kidney disease (CKD), a condition marked by a gradual loss of kidney function over time, exacerbates the complexity of managing urolithiasis. These patients are difficult to manage pertaining to metabolic abnormalities, coagulation dysfunction and comorbidities like hypertension associated with CKD. Patients with CKD are also at heightened risk for recurrent stone formation due to alterations in urinary composition and impaired renal function[1].
Calculi within the urinary tract, which can cause severe pain, hematuria, urinary tract infections, and obstructive uropathy. The risk factors for urolithiasis include metabolic disorders, dietary habits, genetic predisposition, and environmental factors. CKD, is a critical factor that exacerbates the risk and complexity of urolithiasis management[2].
Different modalities are available to manage stones in urinary tract viz. retrograde uretero or renoscopic surgery, percutaneous nephrolithotomy (PCNL), extracorporeal shock wave lithotripsy (ESWL). However, all these modalities may not be easily implacable in patients with CKD due to known complications. For example, these patients may be subject to excessive bleeding in case of PCNL while ESWL worsens the CKD status. Patients with CKD are predisposed to recurrent stone formation due to several pathophysiological changes, such as altered calcium, oxalate, and phosphate metabolism, and the resultant changes in urine composition. Furthermore, the impaired renal function in CKD patients complicates the management of urolithiasis, as the standard therapeutic interventions may pose additional risks and challenges in this vulnerable population[3].
The presence of urolithiasis in CKD patients presents a dual challenge: Managing the immediate issues caused by the stones and preventing further deterioration of renal function. The formation of stones can lead to acute episodes of pain and infection, necessitating urgent medical intervention. Chronic obstruction or recurrent infections can also accelerate the progression of CKD. Therefore, effective management of urolithiasis is critical to prevent further kidney damage and improve patient outcomes[4].
Surgical intervention is often required for the management of urolithiasis, especially in cases where the stones are large, symptomatic, or resistant to conservative management. The primary surgical options include PCNL, ureteroscopy (URS), and ESWL[5].
PCNL: PCNL involves creating a small incision in the back to access the kidney and remove the stones using specialized instruments. It is typically reserved for large or complex stones and has a high stone-free rate. However, it carries risks such as bleeding, infection, and potential renal injury, which are particularly concerning in CKD patients[6].
URS: URS is a minimally invasive procedure that uses a flexible or rigid scope passed through the urethra and bladder to reach the ureter and kidney. Stones are then fragmented using laser lithotripsy or other methods. URS is effective for stones located in the ureter and smaller renal stones but can be technically challenging in patients with CKD due to altered anatomy and fragile mucosa[7].
ESWL: SWL uses high-energy shock waves to fragment stones into smaller pieces that can be passed naturally through the urinary tract. It is less invasive than PCNL and URS but may be less effective for larger stones and carries a risk of renal and surrounding tissue injury, which is a significant consideration for CKD patients[8].
The management of urolithiasis in CKD patients poses unique challenges. The impaired renal function associated with CKD necessitates careful consideration of treatment modalities to avoid further renal damage while effectively addressing the stone burden. Surgical interventions, including PCNL, URS, and SWL, are often employed to manage urolithiasis. However, the safety, feasibility, and efficacy of these surgical interventions in the CKD population remain areas of active investigation and debate.
The safety of surgical interventions for urolithiasis in CKD patients is a paramount concern. Surgical procedures carry inherent risks, including bleeding, infection, and anesthesia-related complications. In CKD patients, these risks are magnified due to their compromised renal function and often coexisting comorbidities such as hypertension, diabetes, and cardiovascular disease. Additionally, the potential for postoperative renal deterioration necessitates a thorough preoperative assessment and meticulous perioperative management. Understanding the balance between the benefits of stone removal and the risks of surgery is crucial for optimizing patient outcomes[9].
Assessing the feasibility of surgical interventions in CKD patients involves evaluating the technical aspects and logistical considerations of performing these procedures. The altered anatomy and physiology associated with CKD can complicate surgical access and visualization. Moreover, CKD patients often require modifications in standard surgical techniques to minimize nephron loss and preserve renal function. This includes the use of advanced imaging modalities, minimally invasive approaches, and meticulous surgical planning[10].
The efficacy of surgical interventions in the CKD population is determined by the ability to achieve stone clearance while minimizing adverse outcomes. Factors influencing the success of surgical treatment include stone size, location, composition, and patient-specific characteristics such as residual renal function and comorbid conditions. Studies have shown that CKD patients may have different responses to surgical interventions compared to those with normal renal function, necessitating tailored approaches to optimize stone-free rates and minimize complications[11].
Managing urolithiasis in CKD patients is a complex and evolving field. Surgical interventions offer potential benefits in terms of stone clearance and symptom relief but are accompanied by significant risks and challenges. A systematic review of the available evidence will provide valuable insights into the safety, feasibility, and efficacy of these procedures, ultimately guiding clinical decision-making and improving patient care in this vulnerable population.
The prevalence of urolithiasis and CKD is rising globally, leading to a significant clinical and economic burden on healthcare systems. The coexistence of these conditions complicates patient management and necessitates a thorough understanding of the best therapeutic approaches. Given that both conditions independently contribute to morbidity and healthcare costs, addressing their intersection is crucial for improving patient outcomes and reducing the overall burden on healthcare resources[12]. Managing urolithiasis in patients with CKD presents unique challenges. These patients are at an elevated risk for complications from both the stones themselves and the surgical interventions required to treat them. The altered physiology and compromised renal function associated with CKD demand tailored approaches to minimize risks while achieving effective stone clearance. This complexity underscores the need for a systematic review to collate and analyze the available evidence on the safety, feasibility, and efficacy of surgical interventions in this specific patient population[13].
There is considerable variation in clinical practice regarding the management of urolithiasis in CKD patients. Differences in surgical techniques, perioperative care protocols, and postoperative management contribute to disparate outcomes. A systematic review can help identify the most effective and safest practices by comparing outcomes across different studies and interventions. This can lead to the development of standardized guidelines and protocols to improve consistency and quality of care. Despite the clinical significance, there is a lack of comprehensive data synthesizing the outcomes of surgical interventions for urolithiasis in CKD patients[14]. Most studies are limited by small sample sizes, heterogeneous patient populations, and varying definitions of clinical outcomes. This fragmentation of data makes it challenging for clinicians to draw definitive conclusions about the best management strategies. A systematic review can provide a more robust and evidence-based evaluation by aggregating data from multiple studies, thereby offering more definitive conclusions and recommendations[15].
Current clinical practice guidelines often lack specific recommendations for managing urolithiasis in CKD patients due to the limited and inconsistent evidence available[16]. A systematic review can fill this gap by providing a comprehensive analysis of the existing literature, identifying best practices, and highlighting areas where further research is needed. The findings can be instrumental in updating and refining clinical guidelines, thereby enhancing the quality of care for this complex patient population. A systematic review can identify gaps in the current understanding of the interplay between urolithiasis and CKD. By highlighting areas where evidence is lacking or inconclusive, the review can guide future research efforts to address these gaps. This can lead to more targeted studies that focus on the specific needs and challenges of managing urolithiasis in CKD patients, ultimately contributing to better patient outcomes and more efficient healthcare delivery.
The management of urolithiasis in CKD patients is fraught with challenges that demand a nuanced and evidence-based approach. A systematic review is warranted to synthesize the available data on the safety, feasibility, and efficacy of surgical interventions in this population. By addressing the current knowledge gaps and informing clinical practice guidelines, the review aims to enhance patient care and improve outcomes for individuals affected by these coexisting conditions.
This systematic review will adhere to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines[17]. A comprehensive search strategy will be employed to identify relevant studies, and rigorous criteria will be applied to select studies for inclusion. The review will synthesize data on the safety, feasibility, and efficacy of surgical interventions for urolithiasis in patients with CKD. A systematic search of electronic databases will be conducted to identify relevant studies. The databases to be searched include PubMed, Scopus, Cochrane Library, Web of Science, and Embase. The search covered studies published from January 2000 to June 2024. The search strategy will use a combination of MeSH terms and keywords related to urolithiasis, CKD, and surgical interventions. The specific search terms will include, but are not limited to Urolithiasis, Kidney stones, Nephrolithiasis, CKD, Surgical intervention, PCNL, URS, ESWL. Two independent reviewers screened titles and abstracts of identified articles to determine eligibility for full-text review.
Studies evaluating surgical interventions such as PCNL, URS, and SWL. Studies reporting on the safety, feasibility, and efficacy of the interventions, including perioperative and postoperative complications, stone-free rates, and impact on renal function. Randomized controlled trials (RCTs), cohort studies, case-control studies, and observational studies. Studies published in English.
Studies involving pediatric patients (< 18 years). Studies that do not separately report outcomes for patients with CKD. Review articles, commentaries, and editorials. Studies with insufficient data on surgical outcomes.
Data was extracted independently by two reviewers using a standardized data extraction form. The following data was extracted from each included study: The included studies represent a range of geographic regions, enhancing the external validity and global relevance of the findings.
Study characteristics: Author(s), publication year, country, study design, sample size.
Patient characteristics: Age, sex, CKD stage, comorbidities.
Intervention details: Type of surgical intervention, technique variations, perioperative care.
Outcomes: Perioperative and postoperative complications, stone-free rates, recurrence rates, changes in renal function, length of hospital stay, quality of life measures.
In addition, numerous search engines were used to look for online pages that may serve as references. Inclusion and exclusion criteria were documented. Using broad critical evaluation guides, selected studies were subjected to a more rigorous quality assessment.
Cochran's Q test was utilized to investigate heterogeneity and make conclusions about meta-analysis appropriateness. The criteria for evaluating the literature were developed with Population, Intervention, Comparison, Outcome, Time in mind.
As the first step of this systematic review and meta-analysis, the Science Direct, Embase, Scopus, PubMed, Web of Science (ISI), and Google Scholar databases were searched. To identify the articles, the search terms “Urolithiasis”, “Kidney stones”, “Nephrolithiasis”, “Chronic kidney disease”, “CKD”, “Surgical intervention”, “Percutaneous nephrolithotomy (PCNL)”, “Ureteroscopy (URS)”, and all the possible combinations of these keywords were used.
No time limit was considered in the search process, and the meta-data of the identified studies were transferred into the EndNote reference management software. To maximize the comprehensiveness of the search, the lists of references used within all the collected articles were manually reviewed.
Keywords used as per MeSH: Urolithiasis, Kidney stones, Nephrolithiasis, CKD, Surgical intervention.
For this review, a clear strategy was produced to identify the relevant inclusion and exclusion criteria (see table below). The inclusion and exclusion criteria for the literature review were written with Population, Intervention, Comparison, Outcome in mind. This ensured that the research question was followed and that appropriately designed research articles were found as suggested by Torgerson and Torgerson[18].
The inclusion and exclusion criteria within a literature search is a source of potential bias therefore higher trust and credibility can be gained by the clear documentation of such exclusion and inclusion criteria[19].
Studies involving adults with CKD of any stage who are diagnosed with urolithiasis.
Surgical interventions for urolithiasis.
Standard care or alternative surgical or non-surgical interventions.
Safety, feasibility, and efficacy of the interventions. We excluded articles that were not written in English as language bias could be prevalent due to the authors' limited understanding and with the risk of the translation being incorrect. This policy could be contradicted however by Jüni et al[20] who suggest that this exclusion generally has little effect on the results, but acknowledge that trials which are presented in English are more likely to be cited by other authors and are more likely to be published more than once. We started with a basic search of keywords using Boolean operators and then filtered these by adding different filters from my inclusion criteria. This enabled to narrow overall search to 28 articles from CINAHL, 39 from MEDLINE, and 75 from PubMed.
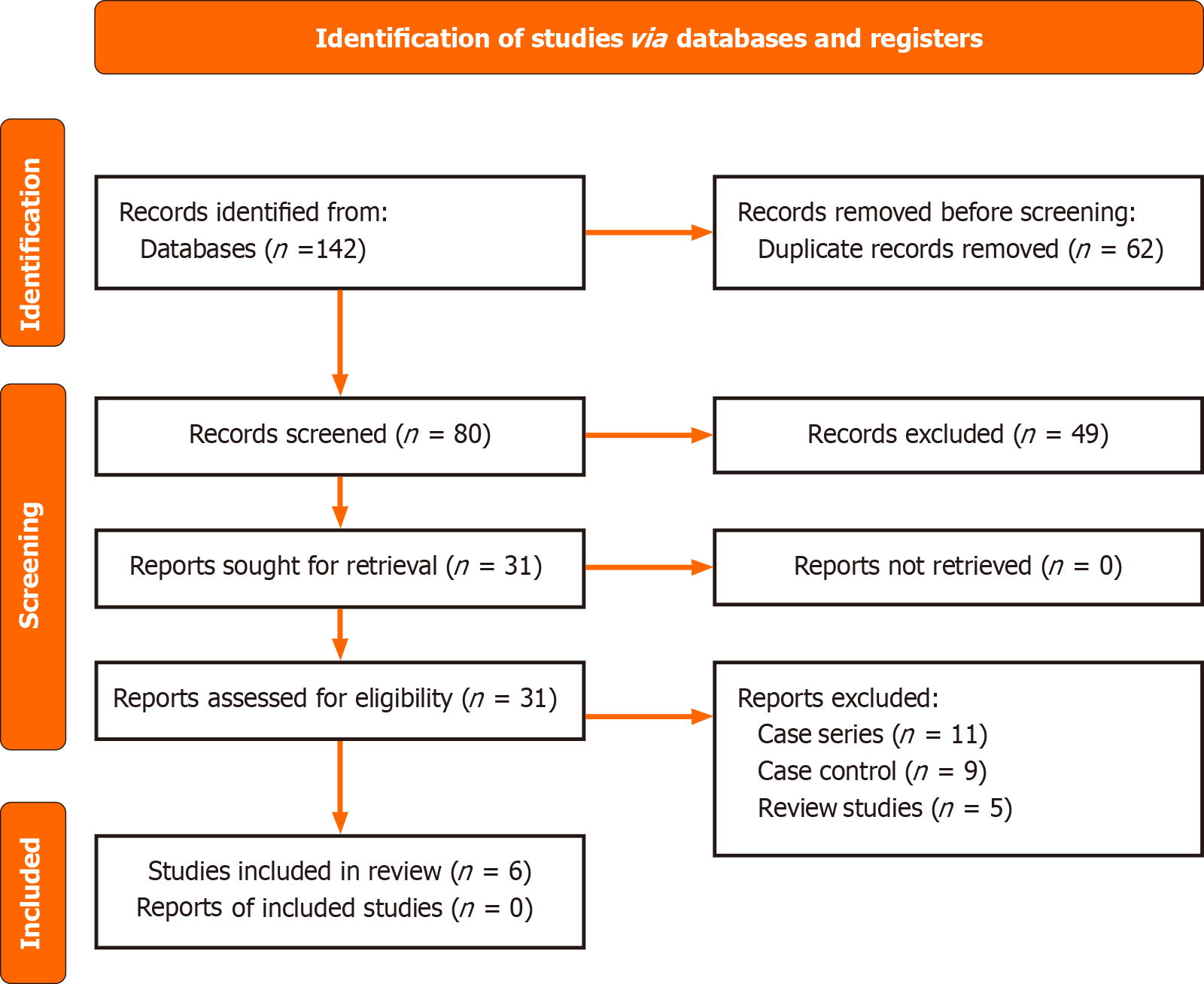
From these 142 articles, we used a PRISMA flow diagram to identify the article selection (See Figure 1). Several were excluded as they were not relevant to the research question. We then removed duplicates and then accessed the abstracts from each article. We also excluded articles that did not cover meta-analysis and this left a total of six articles that met the criteria for this systematic review and were therefore included.
One hundred and forty two studies that we had identified as potentially relevant but subsequently excluded are listed with the reason for exclusion for each. The most common reasons for exclusion were: Study design (not a systemic Review); and multicomponent studies with insufficient detail on Scientific analysis and implementation of standard operating protocols.
The final articles were critiqued and analyzed. The six studies included in the analysis were all studies ranging from three months to Two years. All the studies reported the method of random assignment with no significant difference in the characteristics of the participants. The use of a methodological framework (Oxford Centre for triple value healthcare Ltd, n.d.) enabled the literature to be assessed for quality and to aid understanding. The table below is used to display an overview of each article (Tables 1 and 2)[21-26].
| Ref. | Age range | Number of patients | Type of procedure | Post procedure status | Outcomes | Follow-up |
| AbdelRazek et al[1] | 40-65 (Group A), 45-72 (Group B) | 52 (25 in Group A, 27 in Group B) | PNL, SWL | Improvement in kidney function in both groups; PCNL shows better stone-free rates in a single session | Group A (PNL): Higher stone-free rate, fewer complications; Group B (SWL): May require multiple sessions, more complications reported | Stone-free rate measured at follow-up; regular check-ups on kidney function and imaging tests |
| Ram Dhayal et al[9] | 38.9 ± 15.32 (ESWL), 42.12 ± 11.02 (Mini-PCNL), 41.5 ± 13.20 (RIRS) | 160 (60 ESWL, 60 Mini-PCNL, 40 RIRS) | Mini-PCNL, RIRS, ESWL | Mini-PCNL has the highest SFR, followed by RIRS and ESWL | Mini-PCNL: 98.3% stone-free rate; RIRS: 85% stone-free rate; ESWL: 76.7% stone-free rate | Follow-up included CT urogram and check-up after 1 month |
| Dutta et al[11] | Median 59 (mPCNL) and 57 (URS) | 101 (51 mPCNL, 50 URS) | Mini-PCNL, URS | Stone-free rate higher in mPCNL using a 2-mm cutoff (76% vs 46%). Residual stone burden was significantly lower in mPCNL group (1.4 mm vs 3.6 mm in URS group) | Higher net revenue and direct costs in mPCNL; no significant difference in complications within 30 days | Follow-up included low-dose CT scan between POD 1-30 |
| Fankhauser et al[13] | URS: 50 (± 13.2), SWL: 47 (±14.7) | 44 (23 URS, 21 SWL) | URS, SWL | URS had higher stone-free rate (61%) compared to SWL (48%) after 3 months; URS associated with higher early post-treatment pain | URS: Routine stenting; SWL: No stenting; complications were low in both groups | Pain and stone-free rates assessed at 1, 7, 21 days, and 3 months; additional complications noted |
| Refaat et al[31] | M-PCNL: 36.93 ± 8.58, S-PCNL: 45.06 ± 10.65 | 60 (30 M-PCNL, 30 S-PCNL) | Mini-PCNL (M-PCNL), Standard-PCNL (S-PCNL) | M-PCNL had higher stone-free rate (100%) compared to S-PCNL (86.7%); M-PCNL associated with fewer complications, including lower hemoglobin drop and postoperative fever | M-PCNL: Shorter hospital stay, less postoperative pain, fewer complications; S-PCNL: Higher leakage, longer hospital stay | Follow-up included postoperative pain, stone clearance, and complications assessment |
| Wang et al[41] | SWL: Median 50, URS: Median 54 | 1230 (998 SWL, 232 URS) | SWL, URS | SWL had an equivalent stone-free rate to URS at 1 month (88.7% vs 83.6%) and 3 months (96.8% vs 98.2%), with fewer complications in SWL, particularly no ureteral injuries observed in SWL | SWL: Shorter hospital stay (1 day vs 2 days) and significantly lower cost compared to URS | Follow-up included assessment at 1 and 3 months for stone-free rate and complications |
| Ref. | Intervention | Stone-free rate | Complications | Effect on kidney function | Operative time (minute) | Hospital stay (days) |
| AbdelRazek et al[1] | PNL vs SWL | PNL: 84% SWL: 26.6% (1st session), 88.9% (overall) | PNL: 36% bleeding/hematuria SWL: 55.6% complications | Improvement in S. Creatinine and eGFR | PNL: 53.04 ± 7.6 SWL: 51.22 ± 5.5 | Not specified |
| Refaat et al[31] | M-PCNL vs S-PCNL | M-PCNL: 100%. S-PCNL: 86.7% | M-PCNL: 13.3% leakage S-PCNL: 86.7% leakage | M-PCNL: Lower hemoglobin drop | M-PCNL: 133.73 ± 29.18. S-PCNL: 48.6 ± 17.88 | M-PCNL: 1.4 ± 0.62. S-PCNL: 3.33 ± 1.21 |
| Dutta et al[11] | mPCNL vs URS | mPCNL: 76%, URS: 46% | No significant differences in 30-day complications | No significant change | Not specified | mPCNL: 1 day URS: Same-day discharge |
| Ram Dhayal et al[9] | ESWL vs mPCNL vs RIRS | mPCNL: 98.3%. RIRS: 85%. ESWL: 76.7% | ESWL: Fewer complications, mPCNL: More complications but higher stone-free rate | Not specified | ESWL: 136.4 ± 19.3. mPCNL: 32.3 ± 12.65. RIRS: 51.2 ± 8.63 | ESWL: 0.13 ± 0.05 mPCNL: 3.07 ± 1.6 RIRS: 3.02 ± 0.65 |
| Fankhauser et al[13] | URS vs SWL | URS: 61%, SWL: 48% | URS: Higher early postoperative pain, SWL: Painful ureteral obstruction in 4% | No significant change | Not specified | Not specified |
The first study was conducted by Dutta et al[11]. The study was conducted to evaluate the outcomes of URS vs prone mini-PCNL for 1-2–cm renal stones using a 2-group parallel randomized control trial. A total of 51 mini-PCNL and 50 URS patients were included. Baseline demographics were similar. Using a 2-mm cutoff, stone-free rate was higher in the mini-percutaneous nephrolithotomy group (76% vs 46%, P = 0.0023). The residual stone burden was significantly higher in the URS group than the mini-PCNL group (3.6 vs 1.4 mm, P = 0.0026). Fluoroscopy time was significantly higher in the mini-PCNL group (273 vs 49 seconds, P < 0.0001). There were no differences in postoperative complications within 30 days, the necessity of a secondary procedure within 30 days, and pre- to postoperative creatinine change (P > 0.05). Surgical time did not vary significantly (P = 0.1788). Average length of stay was higher in the mini-PCNL group (P < 0.0001). Both net revenue and direct costs were higher in mini-PCNL procedures (P < 0.05), though they offset each other with a nonsignificant operating margin (P = 0.2541).
The second study was conducted by AbdelRazek et al[1]. The study was conducted to analyze outcomes of PCNL and SWL and their effect on kidney function for patients with renal insufficiency. In this study, we compared the outcome and effect of PNL and SWL for renal stones in patients with renal insufficiency. The data of these patients was recorded and analyzed. 52 renal insufficiency patients with renal stones presented to our Urology department explaining mainly from pain and slight haematuria these patients were randomly divided into two groups using the closed envelope method group A (25 patients 48.1%) for patients who underwent PNL and group B (27 patients 51.9%) underwent SWL. The mean age in our study was 53.96 in group A (range 40-65) which did not differ from that of group B 59.04 (range 45-72). Stone free rate was about 84% of patients in group A (25 patients) and about 26.6% of patients in group B with first session, while it`s about 88.9% for all patients in group B (27 patients) with some degree of improvement of kidney function.
The third study was conducted by Fankhauser et al[13]. The study was conducted to compare effectiveness, complication rates, and pain scores between primary URS and SWL. The study was prematurely closed after randomizing 44 patients due to poor accrual. The 3-mo stone-free rate and mean residual stone size were, respectively, 61% and 1.8 mm after URS and 48% and 2.4 mm after SWL. Early post-treatment pain scores were significantly higher after URS than after SWL on day 1 (3.3 vs 1.6, P = 0.02) and day 7 (5.2 vs 3.4, P = 0.04), but were no longer detectable after 3 weeks and 3 months, respectively. One Clavien-Dindo grade II complication was observed after URS (5%) and SWL (4%), while one (4%) grade IIIb complication was observed after SWL.
The fourth study was conducted by Dhayal et al[9]. This study was conducted to compare ESWL, mini PCNL, and Retrograde Intrarenal Surgery (RIRS) in managing lower pole renal calculi of < 1.5 cm. The mean stone sizes in the present study were 12.99 mm × 3.56 mm in mini PCNL, 10.62 mm × 2.51 mm in RIRS, and 10.93 mm × 3.13 mm in ESWL. The mini PCNL group's stone-free rate (SFR) was significantly higher than those of other groups: 59 (98.3%) in mini PCNL, 34 (85%) in RIRS, and 46 (76.7%) in ESWL (P = 0.002). Out of the 60 patients in the mini PCNL group, only one (1.7%) required an ancillary procedure, while only six (10%) out of 40 patients in the RIRS group and 11 (18.33%) out of 60 patients in the ESWL group required the ancillary procedure (P = 0.031)[27-40].
The fifth study was conducted by Wang et al[41] The study was conducted to compare the effectiveness, safety, and cost of ultrasound-guided SWL with an early second session protocol and URS in patients with proximal ureteral stones. A total of 1230 patients were included, of whom 81.1% (998) were treated with SWL and 18.9% (232) were treated with URS. After PSM, the SWL group had an equivalent SFR at one month (88.7% vs 83.6%, P = 0.114) compared with the URS group. Complications were rare and comparable between the two groups, while the incidence of ureteral injuries was higher in the URS group compared with the SWL group (1.4% vs 0%, P = 0.011). The hospital stay was significantly shorter (1 day vs 2 days, P < 0.001), and the cost was considerably less (2000 vs 25053, P < 0.001) in the SWL group compared with the URS group[42].
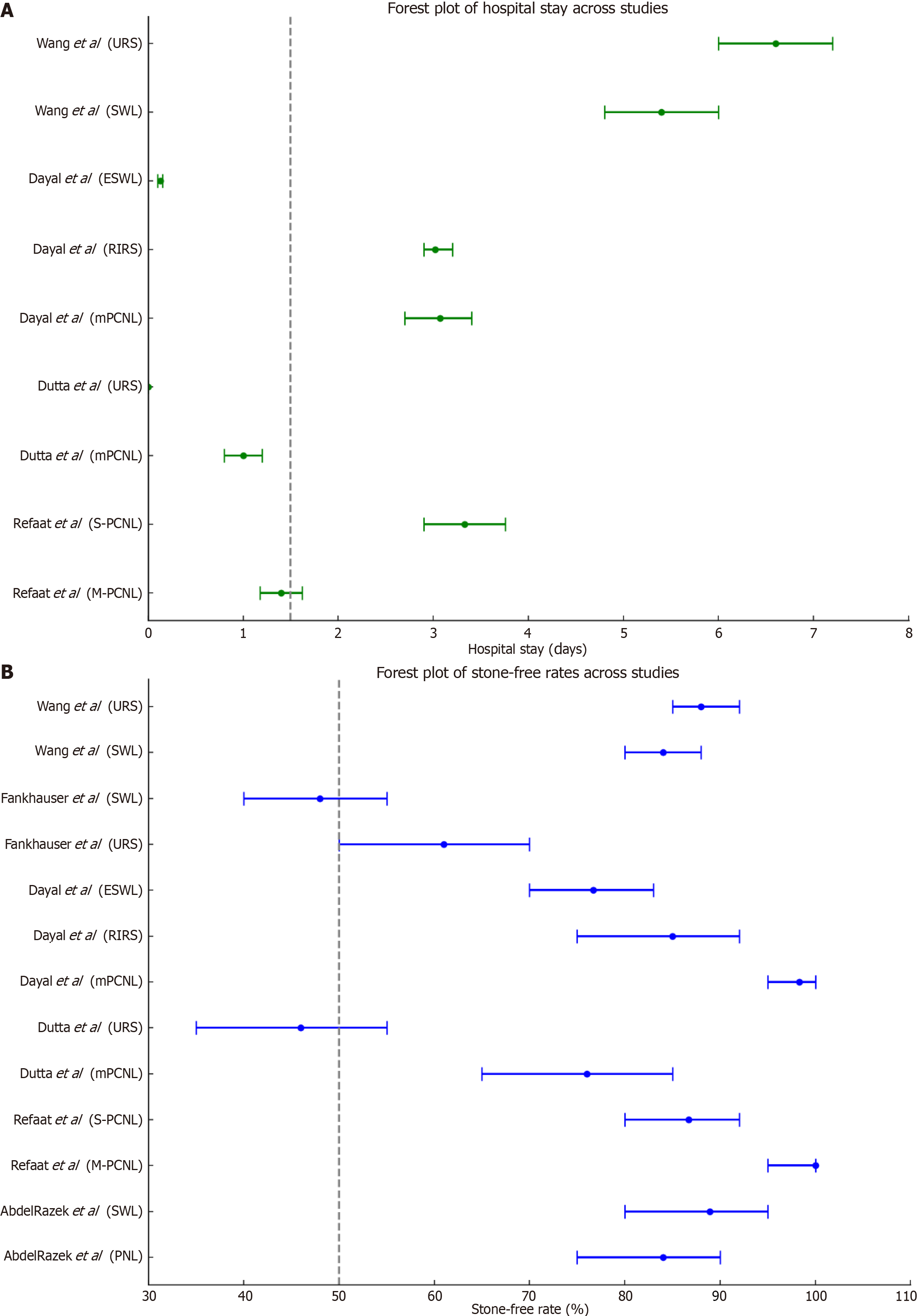
The sixth study was conducted by Refaat et al[31]. This study was conducted to compare the efficacy and safety outcomes of M-PCNL and S-PCNL for managing renal calculi. Findings reveal that M-PCNL had a longer operation time (133.73 ± 29.18 min) than S-PCNL (48.6 ± 17.88 min, P = 0.009) but a lower mean drop in hemoglobin levels (0.14 ± 0.01 g/dL vs 0.82 ± 0.05 g/dL, P = 0.032). The success rates (stone-free rate) were significantly different, with 100% in the M-PCNL group and 86.7% in the S-PCNL group (P = 0.040). Complications were generally fewer in the M-PCNL group, including postoperative fever in 2 cases (M-PCNL) vs 8 cases (S-PCNL) and mild collection in 4 cases (M-PCNL) vs 26 cases (S-PCNL). Forrest plot of hospital stay and stone free rates across studies is depicted in Figure 2.
Surgical management of urolithiasis in patients with CKD presents unique challenges due to the need to balance stone clearance efficacy with preserving renal function. This systematic review examines the efficacy and safety of various surgical interventions commonly used in this patient population. Interventions such as shockwave lithotripsy, URS, and PCNL differ in approach and are tailored based on stone size, location, and patient-specific factors. Understanding the comparative outcomes of these interventions is crucial for optimizing clinical decision-making and improving patient outcomes[27].
Among the reviewed studies, PCNL emerges as highly effective, particularly for larger renal stones in patients with CKD. Studies consistently report high stone clearance rates with PCNL, often exceeding 90%, making it a preferred choice for complex cases where ureterorenoscopy or shockwave lithotripsy may be less effective or feasible. Conversely, ureterorenoscopy demonstrates favorable outcomes for smaller stones, providing a less invasive alternative with comparable efficacy and reduced risk of significant renal injury[28].
Safety profiles vary across interventions, highlighting critical considerations for managing complications in this vulnerable patient population. PCNL, while effective, carries a higher risk of postoperative hemorrhage and infection, necessitating careful perioperative management. Ureterorenoscopy, although generally safer, may lead to ureteral injury or stricture formation, particularly in patients with compromised renal function. Understanding these risks informs clinical decision-making and underscores the importance of individualized treatment plans tailored to patient-specific factors and stone characteristics[29].
The feasibility of surgical interventions in patients with CKD encompasses procedural complexity, operative time, and recovery outcomes. PCNL, despite its invasiveness, offers rapid stone clearance and shorter hospital stays compared to historical approaches, thus optimizing resource utilization and patient recovery. Ureterorenoscopy, with advancements in miniaturized instruments and flexible scopes, enhances feasibility and reduces procedural morbidity, making it increasingly attractive for managing smaller stones in this population[30].
Long-term outcomes, including stone recurrence rates and renal function preservation, underscore the need for ongoing surveillance and management strategies post-intervention. Studies suggest varying rates of stone recurrence based on intervention type, with implications for follow-up care and preventive measures. Preservation of renal function remains a primary goal, influencing the choice of surgical approach and postoperative management strategies to mitigate potential complications and optimize patient outcomes[31].
The quality of evidence from reviewed studies varies, with limitations such as study design heterogeneity and potential biases influencing the strength of recommendations. Future research should prioritize prospective, multicenter trials with standardized outcome measures to enhance comparability and reliability of findings. Advancements in surgical techniques and adjunctive therapies, including medical expulsive therapy and metabolic stone management, hold promise for improving outcomes and minimizing recurrence rates in patients with CKD[32].
This structured discussion synthesizes current evidence on surgical interventions for urolithiasis in patients with CKD, highlighting efficacy, safety profiles, feasibility, long-term outcomes, and avenues for future research. Each paragraph addresses key aspects essential for informing clinical practice and guiding treatment decisions in this complex patient population.
A systematic review of published studies is limited by the fact that it excludes unpublished data and this may result in publication bias but till potential publication bias was not assessed using a funnel plot or other corrective analytical methods.
The review highlights the inconsistency in how outcomes such as 'stone-free rate' and 'complications' were defined across studies, advocating for uniform outcome criteria in future research.
Additionally, the heterogeneity in outcome measures and definitions among the studies limits direct comparability and strengthens the call for standardized reporting in future studies. Moreover, few studies employed multivariable adjustment for confounding factors such as age, comorbidities, or stone characteristics. Future studies should incorporate robust statistical methods for better comparative insight. The included studies vary significantly in terms of study design (e.g., RCT, cohort studies), patient demographics, stone characteristics, and surgical techniques. This heterogeneity can make it challenging to directly compare outcomes across studies and may limit the generalizability of findings. Specific patient characteristics, such as age, comorbidities, and stone composition, could influence treatment outcomes and generalizability to different clinical settings.
In conclusion, this systematic review provides a comprehensive assessment of the current literature on surgical interventions for urolithiasis in patients with CKD. The review aimed to evaluate the safety, feasibility, and efficacy of various surgical approaches commonly used in this population, including PCNL, URS, and SWL.
Clinicians should consider PCNL for large, complex stones in patients with preserved renal reserve, while URS may be more suitable for smaller stones and those at higher surgical risk. SWL can be considered for select patients, balancing its lower invasiveness with potentially lower efficacy.
Postoperative care strategies such as careful fluid management, infection prophylaxis, and early renal function monitoring are crucial. Emphasis should also be placed on improving patient-reported outcomes and quality of life following interventions.
Our review identified significant variations in the efficacy of different surgical interventions. PCNL demonstrated high efficacy rates, particularly for larger renal stones, with consistent reports of successful stone clearance exceeding 90%. URS emerged as a viable option for smaller stones, offering comparable efficacy with reduced invasiveness and shorter recovery times compared to PCNL. Safety profiles varied across interventions, highlighting important considerations for managing complications in patients with CKD. Vicentini et al[40] PCNL, while effective, was associated with higher risks of postoperative hemorrhage and infection, necessitating meticulous perioperative management strategies. URS, though generally safer, posed risks of ureteral injury or stricture formation, especially in this vulnerable patient population. The feasibility of surgical interventions was assessed in terms of procedural complexity, operative times, and recovery outcomes. PCNL demonstrated rapid stone clearance and shorter hospital stays, optimizing resource utilization and patient recovery[34]. Long-term outcomes, however, were often limited in the studies reviewed, emphasizing the need for extended follow-up to assess recurrence rates and renal function preservation. Understanding the strengths and limitations of each surgical approach is crucial for optimizing treatment strategies and improving outcomes in patients with CKD and urolithiasis. Clinicians should consider individual patient factors, stone characteristics, and the available evidence when selecting the most appropriate surgical intervention[35].
In conclusion, while surgical interventions such as PCNL and URS offer effective options for managing urolithiasis in patients with CKD, careful consideration of safety profiles, feasibility, and long-term outcomes is essential. Continued research efforts are needed to further refine treatment algorithms, enhance surgical techniques, and minimize complications in this complex patient population. This conclusion summarizes the key findings, discusses limitations, highlights clinical implications, and suggests future directions for research, providing a comprehensive overview of your systematic review on surgical intervention for urolithiasis in patients with CKD.
| 1. | Abdelrazek M, Abolyosr A, Abdel Kader MS, Hassan AM, Mohammed O, Fathy A, Abdelfattah A, Alsagheer G. Comparative Study between Outcome of Percutaneous Nephrolithotomy and Extracorporeal Shock Wave Lithotripsy in Patients with Renal Insufficiency. SVU-International J Med Sci. 2021;4:7-12. [DOI] [Full Text] |
| 2. | Akram M, Jahrreiss V, Skolarikos A, Geraghty R, Tzelves L, Emilliani E, Davis NF, Somani BK. Urological Guidelines for Kidney Stones: Overview and Comprehensive Update. J Clin Med. 2024;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 61] [Reference Citation Analysis (0)] |
| 3. | Ansari FM, Para SA, Wani MS, Bhat AH, Khawaja AR, Malik SA, Mehdi S, Ashraf W, Singh S, Maurya M, Mushtaq A. Mini-PCNL - a boon for CKD patients with nephrolithiasis. Arab J Urol. 2024;22:115-120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Carrion DM, Cansino JR, Quintana LM, Gómez Rivas J, Mainez Rodriguez JA, Pérez-Carral JR, Martínez-Piñeiro L. Prone percutaneous nephrolithotomy: its advantages and our technique for puncture. Transl Androl Urol. 2018;7:950-959. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Li T, Higgins JPT, Deeks JJ. Chapter 5: Collecting data. Cochrane Handbook for Systematic Reviews of Interventions version 6.5. Cochrane, 2024. |
| 6. | Cronin P, Ryan F, Coughlan M. Undertaking a literature review: a step-by-step approach. Br J Nurs. 2008;17:38-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 481] [Cited by in RCA: 487] [Article Influence: 27.1] [Reference Citation Analysis (0)] |
| 7. | Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, Thomas J. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:ED000142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1361] [Cited by in RCA: 3411] [Article Influence: 487.3] [Reference Citation Analysis (1)] |
| 8. | De Lorenzis E, Zanetti SP, Boeri L, Montanari E. Is There Still a Place for Percutaneous Nephrolithotomy in Current Times? J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Ram Dhayal I, Gupta R, Srivastava A, Rai P. A Comparative Study on Outcomes of Retrograde Intrarenal Surgery (RIRS), Mini Percutaneous Nephrolithotomy (PCNL), and Extracorporeal Shock Wave Lithotripsy (ESWL) for Lower Pole Renal Calculi of < 1.5 cm. Nephro-Urol Mon. 2023;15:e128168. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Ikizler TA, Burrowes JD, Byham-Gray LD, Campbell KL, Carrero JJ, Chan W, Fouque D, Friedman AN, Ghaddar S, Goldstein-Fuchs DJ, Kaysen GA, Kopple JD, Teta D, Yee-Moon Wang A, Cuppari L. KDOQI Clinical Practice Guideline for Nutrition in CKD: 2020 Update. Am J Kidney Dis. 2020;76:S1-S107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 837] [Cited by in RCA: 1180] [Article Influence: 196.7] [Reference Citation Analysis (1)] |
| 11. | Dutta R, Mithal P, Klein I, Patel M, Gutierrez-Aceves J. Outcomes and Costs Following Mini-percutaneous Nephrolithotomy or Flexible Ureteroscopic Lithotripsy for 1-2-cm Renal Stones: Data From a Prospective, Randomized Clinical Trial. J Urol. 2023;209:1151-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 12. | Faber J, Fonseca LM. How sample size influences research outcomes. Dental Press J Orthod. 2014;19:27-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 259] [Cited by in RCA: 511] [Article Influence: 46.5] [Reference Citation Analysis (0)] |
| 13. | Fankhauser CD, Weber D, Müntener M, Poyet C, Sulser T, Hermanns T. Effectiveness of Flexible Ureterorenoscopy Versus Extracorporeal Shock Wave Lithotripsy for Renal Calculi of 5-15 mm: Results of a Randomized Controlled Trial. Eur Urol Open Sci. 2021;25:5-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 14. | Gadelmoula M, Elderwy AA, Abdelkawi IF, Moeen AM, Althamthami G, Abdel-Moneim AM. Percutaneous nephrolithotomy versus shock wave lithotripsy for high-density moderate-sized renal stones: A prospective randomized study. Urol Ann. 2019;11:426-431. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Gameiro J, Marques F, Lopes JA. Long-term consequences of acute kidney injury: a narrative review. Clin Kidney J. 2021;14:789-804. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 70] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 16. | Glazer K, Brea IJ, Leslie SW, Vaitla P. Ureterolithiasis. 2024 Apr 20. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2025. [PubMed] |
| 17. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 48610] [Article Influence: 2859.4] [Reference Citation Analysis (3)] |
| 18. | Torgerson DJ, Torgerson CJ. Avoiding Bias in Randomised Controlled Trials in Educational Research. Br J Educ Studies. 2003;51:36-45. |
| 19. | Assimos D, Krambeck A, Miller NL, Monga M, Murad MH, Nelson CP, Pace KT, Pais VM Jr, Pearle MS, Preminger GM, Razvi H, Shah O, Matlaga BR. Surgical Management of Stones: American Urological Association/Endourological Society Guideline, PART I. J Urol. 2016;196:1153-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 481] [Cited by in RCA: 779] [Article Influence: 77.9] [Reference Citation Analysis (0)] |
| 20. | Jüni P, Holenstein F, Sterne J, Bartlett C, Egger M. Direction and impact of language bias in meta-analyses of controlled trials: empirical study. Int J Epidemiol. 2002;31:115-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 578] [Cited by in RCA: 628] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 21. | Lipscomb M. Exploring Evidence-based Practice: Debates and Challenges in Nursing (1st ed). London, United Kingdom: Routledge, 2015. |
| 22. | Kumar GM, Nirmal KP, Kumar GS. Postoperative infective complications following percutaneous nephrolithotomy. Urol Ann. 2021;13:340-345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Manzoor H, Leslie SW, Saikali SW. Extracorporeal Shockwave Lithotripsy. 2024 Oct 18. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2025. [PubMed] |
| 24. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18665] [Cited by in RCA: 18034] [Article Influence: 1060.8] [Reference Citation Analysis (1)] |
| 25. | Oxford centre for triple value healthcare Ltd. Critical Appraisal Skills Programme. Available from: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf. |
| 26. | Jüni P, Holenstein F, Sterne J, Bartlett C, Egger M. Direction and impact of language bias in meta-analyses of controlled trials: empirical study. Int J Epidemiol. 2002;31:115-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 578] [Cited by in RCA: 628] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 27. | Patel R, Agarwal S, Sankhwar SN, Goel A, Singh BP, Kumar M. A prospective study assessing feasibility of performing percutaneous nephrolithotomy in chronic kidney disease patients - What factors affect the outcome? Int Braz J Urol. 2019;45:765-774. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 28. | Pati D, Lorusso LN. How to Write a Systematic Review of the Literature. HERD. 2018;11:15-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 86] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 29. | Hemingway P. What is systematic review. Evi Based Med. 2009;2:1-8. |
| 30. | Poudyal S. Current insights on haemorrhagic complications in percutaneous nephrolithotomy. Asian J Urol. 2022;9:81-93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 31. | Refaat HM, Hassan M, Salem T, Zaza M. Mini-percutaneous nephrolithotomy versus Standard percutaneous nephrolithotomy: outcome and complications. Afr J Urol. 2023;29:31. [DOI] [Full Text] |
| 32. | Satav VP, Sharma S, Kapoor R, Sabale VP, Shah AS, Kandari A. Management of urolithiasis in patients with chronic kidney disease. Urol Ann. 2020;12:225-228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 33. | Shastri S, Patel J, Sambandam KK, Lederer ED. Kidney Stone Pathophysiology, Evaluation and Management: Core Curriculum 2023. Am J Kidney Dis. 2023;82:617-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 94] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 34. | Singh I, Gupta NP, Hemal AK, Aron M, Dogra PN, Seth A. Efficacy and outcome of surgical intervention in patients with nephrolithiasis and chronic renal failure. Int Urol Nephrol. 2001;33:293-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 35. | Song L, Maalouf NM. Nephrolithiasis. 2020 Mar 9. In: Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc., 2000. [PubMed] |
| 36. | Strohmaier WL. Recent advances in understanding and managing urolithiasis. F1000Res. 2016;5:2651. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 37. | Sultan S, Umer SA, Ahmed B. Urolithiasis. Practical Pediatric Urology. Cham: Springer, 2021. [DOI] [Full Text] |
| 38. | Torgerson DJ, Torgerson CJ. Avoiding Bias in Randomised Controlled Trials in Educational Research. British J Educ Studies. 2003;51:36-45. [DOI] [Full Text] |
| 39. | Tzelves L, Berdempes M, Mourmouris P, Mitsogiannis I, Skolarikos A. Optimal Delivery of Follow-Up Care for the Prevention of Stone Recurrence in Urolithiasis Patients: Improving Outcomes. Res Rep Urol. 2022;14:141-148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 40. | Vicentini FC, Gomes CM, Danilovic A, Neto EA, Mazzucchi E, Srougi M. Percutaneous nephrolithotomy: Current concepts. Indian J Urol. 2009;25:4-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 41. | Wang P, Zhan Y, Li J, Liu G, Li Z, Bai S. Comparison of shock wave lithotripsy and ureteroscopy in patients with proximal ureteral stones under the COVID-19 pandemic. World J Urol. 2023;41:797-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/