Peer-review started: July 26, 2022
First decision: October 21, 2022
Revised: November 19, 2022
Accepted: December 8, 2022
Article in press: December 8, 2022
Published online: January 25, 2023
Processing time: 175 Days and 6.9 Hours
The incidence of human immunodeficiency virus (HIV)-infected cases that need total joint replacement (TJR) is generally rising. On the other hand, modern management of HIV-infected cases has enabled them to achieve longevity while increasing the need for arthroplasty procedures due to the augmented dege-nerative joint disease and fragility fractures, and the risk of osteonecrosis. Although initial investigations on joint replacement in HIV-infected cases showed a high risk of complications, the recent ones reported acceptable outcomes. It is a matter of debate whether HIV-infected cases are at advanced risk for adverse TJR consequences; however, the weak immune profile has been associated with an increased probability of complications. Likewise, surgeons and physicians should be aware of the complication rate after TJR in HIV-infected cases and include an honest discussion of the probable unwelcoming complication with their patients contemplating TJR. Therefore, a fundamental review and understanding of the interaction of HIV and arthroplasty are critical.
Core Tip: The outcome and prevalence of complications are controversial among human immunodeficiency virus-infected cases who need arthroplasty. According to our literature review, total joint replacement procedures are recommended based on patient-specific factors such as viral load, CD4+ T-cell count, clinical classification, history of intravenous drug addiction, and the patient's overall health. Optimization with antiviral drugs is also suggested before elective arthroplasty.
- Citation: Salimi M, Mirghaderi P, Mosalamiaghili S, Mohammadi A, Salimi A. Joint replacement and human immunodeficiency virus. World J Virol 2023; 12(1): 1-11
- URL: https://www.wjgnet.com/2220-3249/full/v12/i1/1.htm
- DOI: https://dx.doi.org/10.5501/wjv.v12.i1.1
Human immunodeficiency virus (HIV) infection in humans was initially recognized in the early 1980s and documented as the reason for acquired immunodeficiency syndrome (AIDS). With an estimated 37 million affected people in 2015, the pandemic has grown to all corners of the world. Southern and Eastern Africa have tolerated the extreme impact of this problem, with 52% of the total infected people, 19 million cases, and more than 1 million new annual infections. The yearly occurrence of newly infected cases has decreased by 38%, from 2001 (3.4 million) to 2015 (2.1 million), with the successful advent and introduction of antiretroviral therapy (ART) programs in the last years[1,2]. AIDS-related expiries have also dropped from a high in 2005 (2.0 million), distinguished to be the topmost of the epidemic, to 1.1 million yearly in 2015, which means a reduction of about 45%[3].
The etiology varies according to highly active antiretroviral treatment (HAART) and disease-related mechanisms[4].
Femoral head osteonecrosis was initially reported in HIV-infected cases in the early 1990s - before the ART time. Several investigations have considered ART drugs as an independent factor for osteonecrosis development[5-7]. Therefore, HIV-positive individuals would need TJR at a much earlier age due to the osteonecrosis of the hip, in comparison to their counterparts who are affected by osteoarthritis and mostly are bilaterally involved[8].
Furthermore, a reduction in the density of bone minerals is more frequently seen in HIV-positive cases compared to non-infected controls[9,10]. The stimulation of interleukin-1 (IL-1) and tumor necrosis factor-alpha (TNF-α) is followed by an imbalance of the receptor stimulator of nuclear factor kappa-B (RANK)/RANK ligand (RANKL)/osteoprotegerin (OPG) system, which eventually motivates bone resorption by osteoclasts and inhibits osteoclastic action. The cascade mentioned above in the long term accelerates osteopenia and would augment the probability of fragility fractures, particularly fractures of the femur neck in HIV-infected males[11].
It is controversial whether HIV-infected cases are at advanced menace for adverse TJR consequences; however, the weak immune profile may have been correlated to the increased probability of complications. Although initial investigations on hip and knee arthroplasty in HIV-infected cases showed a high risk of complications, the recent ones reported acceptable outcomes[12]. Despite the increasing number of the HIV-infected population, there is scarce literature investigating outcomes after TJR in infected ones. Periprosthetic joint infection (PJI) is one of the most prevalent causes of revision arthroplasties, and its underlying risk factors could be both non-modifiable and modifiable. Non-modifiable factors include chronic diseases such as cirrhosis, coagulopathies, kidney disease, and obstructive pulmonary as well as race, gender, and age[13,14]. Modifiable issues have been proven to increase early revision rates and complications and prolong the hospital stay. These factors include diabetes, smoking, opioid use, poor dentition, obesity, HIV, and Staphylococcus aureus colonization[14]. A bunch of risk factors may also have been developed in HIV-positive cases undergoing TJR[15]. Initial studies in orthopedic trauma patients infected with HIV showed a significant rate of postoperative infection rate[16,17]. Parvizi et al[18] demonstrated a similar finding in arthroplasty cases. However, their study involved patients with hemophilia, which may have been demonstrated as an independent risk factor for PJI[19,20]. Further investigations among non-hemophilic HIV-positive cases have displayed a remarkably lower rate of infection but a worryingly high rate of total complications[1].
Furthermore, Orthopedic Infections International Consensus in 2018 announced that HIV is an independent factor in increasing the risk of PJI[21]. However, the importance was reduced when HAART managed HIV-positive cases, and preoperative optimization was performed for them[21]. Therefore, identification and optimization of HIV-positive patients before surgery are mandatory to reduce the burden of already serious healthcare systems.
According to the above, a fundamental approach and understanding of the TJR and HIV interaction are inevitable. Therefore, we conduct a literature review on joint replacement in the HIV-positive group. Moreover, this minireview highlights the critical aspect of complications and outcomes.
Clinical staging methods help determine the prognosis and treatment for HIV-positive patients. Orthopedic surgeons who plan to operate on these patients must understand these systems well. The two most commonly used HIV classification systems were introduced by the Centers for Disease Control (CDC) and the World Health Organization (WHO). In 2014, the CDC released the modified definition of surveillance case for HIV infection[22]. This surveillance case explanation for HIV has been revised and combined into a sole case definition for people of every age. New multi-test algorithms, such as HIV-I and HIV-II detection criteria and direct detection of HIV infection, have been added to laboratory criteria to define an approved case. The surveillance case definition refers to monitoring the burden of HIV infection at the population level and planning for care and prevention, not for individual patient treatment decisions. A proven case of HIV infection is classified into five stages (0, 1, 2, 3, or unknown) (Table 1).
| Age on date of CD4+ T-lymphocyte test | ||||||
| Stage | < 1 yr | 1–5 yr | ≥ 6 yr | |||
| Cells/µL | % | Cells/µL | % | Cells/µL | % | |
| 1 | ≥ 1500 | ≥ 34 | ≥ 1000 | ≥ 30 | ≥ 500 | ≥ 26 |
| 2 | 750-1499 | 26-33 | 500-999 | 22-29 | 200-499 | 14-25 |
| 3 | < 750 | < 26 | < 500 | < 22 | < 200 | < 14 |
The CDC proposes three descriptive classifications based on the presence or absence of specific clinical symptoms (Table 2). The CD4+ T-cell count further subdivides these three types. CD4+ T-cell counts above 500/µL are categorized as types A1, B1, and C1. CD4+ T-cell counts within 200/µL and 400/µL are A2, B2, and C2 categories. Infections in patients having CD4+ T-cell numbers lower than 200/μL are classified as A3, B3, or C3.
| Clinicalcategory | Symptomatic conditions |
| A | Asymptomatic HIV infection, persistent generalized lymphadenopathy, acute (primary) HIV infection complicated by illness, or a history of acute HIV infection. Bacillary angiomatosis |
| B | Candida infection, cervical dysplasia, constitutional symptoms, hairy leukoplakia, herpes zoster, unexplained thrombocytopenic purpura, listeriosis, pelvic inflammatory disease, and peripheral neuropathy. |
| C | AIDS-defining diseases: Toxoplasmosis, Kaposi's sarcoma, Pneumocystis pneumonia |
Orthopedic surgeons mostly use the WHO staging system[23]. Patients are divided into four clinical groups using this classification system: Stage one patients are asymptomatic or accompanied by persistent generalized lymphadenopathy; patients with stage two present with a slight disease along with 10% weight loss and skin exhibition; those with stage three experienced moderate disease and weight loss of more than 10%, severe bacterial infections, and chronic diarrhea lasting more than a month; and patients with the last stage have a severe disease, AIDS, cryptosporidiosis, toxoplasmosis, HIV wasting syndrome, Kaposi's sarcoma, and pneumonia caused by Pneumocystis jirovecii.
In HIV-infected persons, osteonecrosis is still the most common reason for TJR. Since the first case was reported in 1990, the annual osteonecrosis prevalence among HIV-infected ones has consistently grown, ranging from 0.08% to 1.33%[24,25]. Although the specific origin of osteonecrosis in HIV-positive people is unknown, various risk variables have been identified[26,27].
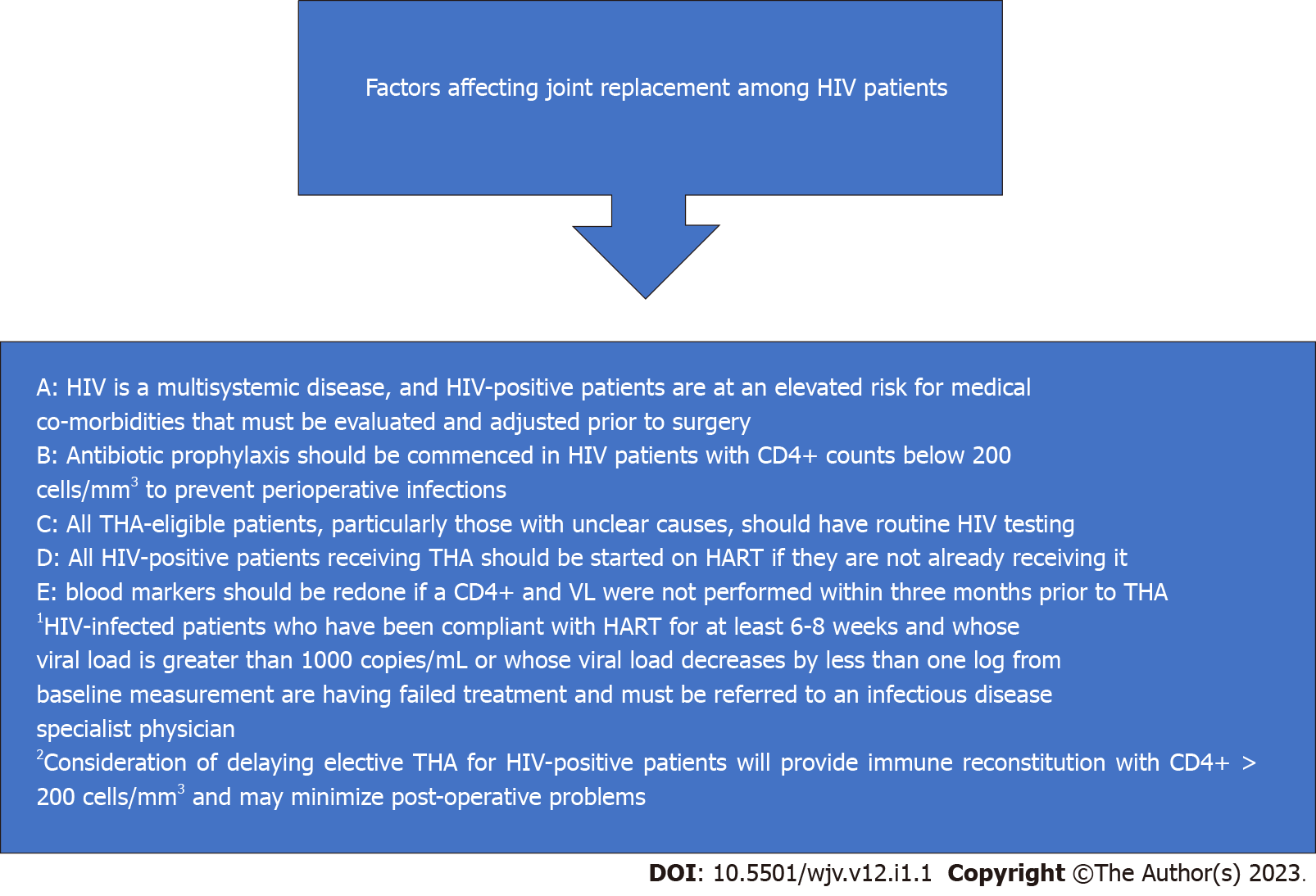
Alcohol, corticosteroids, hyperlipidemia, anticardiolipin and antiphospholipid antibodies, cigarette smoking, course of HIV infection, and antiretroviral therapy are some of the most common risk factors for changes in the bloodstream to the bone[26,27]. Although many researchers believe that the multiple effects of several factors that impair bone blood flow would lead to osteonecrosis, some investigators provide evidence that HIV infection alone can cause osteonecrosis[7,22,28]. According to a study by Ries et al[28], there was a much higher percentage of HIV-infected individuals with nontraumatic osteonecrosis without any identified risk factors than HIV-negative cases. Figure 1 demonstrates factors affecting joint replacement among HIV-infected patients.
Some factors stimulate osteonecrosis in both HIV-positive and -negative cases. Steroids alter bone metabolism and the growth of bone marrow stromal cells, resulting in fat penetration into the bone marrow and blockage of the bloodstream inside the bone. The cascade above increases intraosseous pressure. Moreover, steroids may cause acute fat embolization in capillary arteries[23-26], which are widely used to manage HIV-related diseases, such as pneumocystis pneumonia and also central nervous system toxoplasmosis[29-31]. Miller et al[29] also verified the abovementioned association and determined that even short-term consumption of a corticosteroid drug could significantly raise the incidence of osteonecrosis. Hyperlipidemia, a known subsequent event of HIV infection and HAART diets, is substantially implicated in atherosclerotic pathways and is known to be a causative agent in steroid-induced osteonecrosis. Several investigations have linked high serum cholesterol levels and the consumption of fat-reduction drugs to the pathogenesis of osteonecrosis[7,26,31].
HIV has a detrimental effect on the density of the bone mineral, and patients with HIV infection are prone to develop osteoporosis 3.7 times greater than non-infected people[1,32]. Consequently, there is an augmented fragility fracture risk in HIV-positive cases[1]. Low bone mineral density is associated with low CD4+ T-cell count and long-term HIV infection[1]. Another reason for generated osteopenia is the constant inhibition of osteoblasts and activation of osteoclasts, which is a result of miss-balanced receptor activation of the nuclear factor kappa-B (RANK)/RANKL/OPG system[11,33]. This pattern is triggered by the virus, which causes activation of TNF-α and IL-1[10].
Increased levels of antiphospholipid antibodies and further thrombophilic factors are correlated with osteonecrosis in HIV-infected cases. Antiphospholipid antibodies are considered a risk factor for venous and arterial thrombosis and are generally found in HIV-infected patients. In a new investigation, the incidence of antiphospholipid antibodies in HIV-infected cases was predicted to be around 44%[34]. It is well known that these antibodies are involved in the progression of osteonecrosis in systemic lupus erythematosus patients, and similar processes have been suggested for HIV-infected cases[25,35].
Recent studies have engrossed the role of antiretroviral therapies, mainly protease inhibitors, in the pathogenesis of osteonecrosis. Even though the precise processes of HAART that may play a role in osteonecrosis are unclear, the association of protease inhibitors and conventional osteonecrosis risk factors has been recognized[8,22,26]. Hypertriglyceridemia due to HAART has been widely cited as a potential cause of osteonecrosis. Through interactions with cytochrome P450, protease inhibitors may increase the effectiveness of steroid therapy. A study by Penzak et al[36] showed that treatment with ritonavir dramatically amplified the concentration of prednisolone in healthy cases. Several HIV-positive cases with osteonecrosis were reported before the introduction of HAART, suggesting that HIV treatment regimens could not be the primary cause of the disease. Osteonecrosis has a complex etiology and is highly prevalent among HIV-positive individuals, thus increasing the need for total joint arthroplasties in this patient population.
While the incidence of HIV infection is steadily increasing, broad access to HAART has upgraded from 25% in 2010 to 73% in 2021[37]. Increased access to HAART has reduced global AIDS-related mortality by 64% since its peak in 2004 and by 47% since 2010[37]. HIV and HAART are independently associated with joint pathology that ultimately requires joint replacement[4].
HAART should be started in all HIV-positive patients, regardless of clinical stage or CD4+ T-cell count[1]. This is particularly significant for cases pending elective TJR. First-line HAART almost always consists of a combination of two nucleoside reverse transcriptase inhibitors (NRTIs) and an agent of a different drug class. Protease inhibitors (PIs) are believed to form the primary drug class that aids avascular necrosis (AVN) in the hip[4]. In addition, drugs containing tenofovir have been linked to the progression of osteopenia[1]. Remarkably, all first-line regimens in every corner of the world include tenofovir agents.
Due to osteodegenerative and renal complication of tenofovir disoproxil fumarate (TDF), tenofovir alafenamide (TAF) was developed[38]. TAF continues to cause renal disease and bone loss, but to a lesser extent than TDF. The WHO recommended that integrase strand transfer inhibitors (InSTIs) replace PIs as the ideal first-line regimen. However, more than half of the global HIV prevalence is in East and South Africa, which cannot easily access InSTIs[38].
There are several side effects to HAART drugs, and the patient's diet should be monitored. There are significant drug interactions between anesthetic drugs and NRTIs and PIs that are usually prescribed for induction and sedation. TDF is nephrotoxic, so patients need to be checked for blood urea nitrogen; the urine protein-to-creatine ratio is sometimes assessed to evaluate their renal function[39]. Anemia and neutropenia are side effects of zidovudine. Thus, these patients need a complete blood count, white cell count, and differential amount[40].
Different studies show how immune system impairment is a key factor in postoperative risk of infection and complications[41]. Any major disease which causes impaired immune system like diabetes mellitus, which results in impaired leukocyte function[42,43], and even malnutrition[44], can be risk factors for PJI[41].
CD4+ T-cell count is an alternative indicator of immunological status, and the number of CD4+ T cells less than 200 cells/mm3 confirms the diagnosis of AIDS[39]. Optimistic monitoring of the patient's immune status is essential in managing HIV-infected patients undergoing HAART. The opportunistic infections-related prevalence, mortality, and morbidity are higher in patients with a CD4+ T-cell count of 200 cells/mm3[45]. Patients with opportunistic infections and abandoned viral status should be recognized to reduce perioperative and postoperative complications[45]. Antibiotic prophylaxis should be initiated for all patients with a CD4+ T-cell count < 200 cells/mm3[45]. The guidelines recommend trimethoprim-sulfamethoxazole (TMP-SMX) as an effective treatment for opportunistic infections[45].
Viral load (VL) is a reliable indicator of treatment effectiveness and is influenced by patient adherence to HAART. Elective procedures should be delayed for those with higher VL[45]. If, after 6 to 8 wk of careful treatment, the VL is greater than 1000 copies/mL or less than one log below starting point, there is a viral failure[45].
Multiple systems can be affected by HIV, and patients should be thoroughly evaluated for perioperative risk classification before TJR. HIV-positive cases often suffer cardiovascular disease, nephropathy, liver disaster, neurological problems, and non-AIDS-related malignancies[46]. Evaluation of the patients mentioned before surgery should contain suitable blood work, nutritional status, and immune deficiency syndrome stage[47]. In HIV-positive patients, postoperative complications are mainly due to immunodeficiency, not the procedure itself. Therefore, a comprehensive evaluation is required to prevent anesthetic and surgery problems[45].
HIV-infected cases who developed advanced stages of the disease should also have their nutritional status evaluated since there is a higher risk for nutritional deficiencies and wasting[45]. Hypoalbuminemia is an independent risk factor for mortality in HIV-infected cases postoperatively compared to the non-infected control group[48].
Malnutrition is related to several problems following THA, such as delayed wound healing and prolonged wound damage, which increases the risk of infection[21]. If the diet is inadequate, dietary supplements may be necessary and should be consulted with a nutritionist[45].
On the other hand, compared to the HIV-negative control group, HIV-positive individuals are at higher risk for coronary artery disease, which may be due to persistent chronic inflammation[45]. HAART drugs have decreased the risk of perioperative cardiovascular problems[46].
HIV-infected patients treated with HAART have an increased incidence of insulin resistance, diabetes, and hypercholesterolemia. This may increase the risk of AVN in the femoral head and thus upsurge the need for TJR among HIV-infected cases. All HIV-infected patients should undergo a thorough clinical evaluation for lipodystrophy and fasting lipograms, mainly if they consume a HAART diet containing PI[45].
In HIV-positive patients, smoking is approximately 40% more prevalent than in the general population, and the probability of quitting is also lower[49]. This makes the patients susceptible to atherosclerotic developments, chronic lung disease, and postoperative respiratory infections[45]. Before elective surgery, the respiratory function should be evaluated in all HIV-infected smokers to determine their capacity for diffusion[45]. In addition, AIDS patients are susceptible to nosocomial invasive bacterial infections, and elective TJR should be delayed to optimize immune system reconstruction[45].
As the global number of HIV-infected cases rises, the need to evaluate the results of orthopedic treatment in them also increases. Due to the growing demand for these treatments, the consequences and complications of TJR among them are also receiving particular attention. In addition to functional implications, many of these studies have investigated the incidence of postoperative infections. Previously, HIV was known as an independent factor for infection after surgery. Therefore, the benefits and safety of elective surgery in these patients have been questioned. However, some recent investigations of TJR in HIV-infected patients have raised doubts about this theory.
The treatment algorithms for HIV-positive patients should be similar to algorithms used for non-infected cases, with two-step revision surgery. We suggest a long course of intravenous antibiotics: Up to 6 mo vs 6 wk. The medical condition of patients, especially their VL and CD4+ T-cell count, should always be considered.
Several studies focusing on the results of complete joint arthroplasty in HIV-infected cases have focused on hemophilic ones. Due to recurrent periarticular and intra-articular hemorrhage, people with hemophilia are at a much higher risk for joint degeneration. The risk of developing joint arthropathy increased with the higher rates of HIV infection in these people between 1979 and 1985 due to the application of polluted blood products. During that period, injection of infected factor VIII resulted in serum conversion in about 80% of hemophilia patients. Preliminary research conducted by Gregg-Smith et al[50] and Wiedel et al[51], evaluated the infection prevalence in HIV-infected hemophiliac cases who underwent complete knee arthroplasty before the extensive use of HAART. Wiedel et al[51], in a 1989 study, found an advanced rise in acute postoperative infections. The result, as mentioned earlier, was also confirmed by Gregg-Smith et al[50].
Hicks et al[52] and several other researchers confirmed that the growing risks are related to TJR in HIV-positive hemophiliacs, linking the probability of these problems to the number of CD4+ T-cells. Hicks et al[52] evaluated the results of 102 TJR in 73 hemophiliac patients infected by HIV in a large multicenter retrospective study. The incidence of surgical site infection was 18.7% for initial surgeries and 36.3% for revision after an average five-year follow-up. About 62.5% of the infected group had a preoperative CD4+ T-cell count of less than 0.2 × 109/L, while 16.7% were non-infectious. Ragni et al[19] found a similar increase in the rate of postoperative infections in HIV-positive hemophiliac patients with CD4+ T-cell counts of less than 0.2 × 109/L in patients who underwent knee and hip arthroplasty surgeries. An infection rate of 15% was observed in a retrospective analysis of 115 hemophilia clinics in the United States in 1995, which the authors highlighted was three times more likely than the risk of infection at surgical sites among HIV-negative arthroplasty patients.
In contrast, many current investigations could not confirm the extensive risk of problems in this population of patients after total joint replacement. For instance, Powell et al[53] evaluated the incidence of postoperative infections following total TJR of the knee and hip in HIV-negative and HIV-positive hemophilia patients between 1975 and 2002. Three of the 30 joints among HIV-infected cases developed primary joint infections, compared to two of the 21 non-infected groups. The perusal above did not show an elevated relative risk of surgical site infection in HIV-positive patients (relative risk = 1.49). The researchers concluded that TJR is a viable treatment choice for hemophilic patients with concomitant HIV infection.
The relative safety of the orthopedic procedures in HIV-positive hemophiliac patients was further supported by Unger et al[54], who evaluated 26 knee arthroplasties of 15 patients with HIV infection and type A hemophilia; all of them experienced an improvement in function after arthroplasty, and also during 6.4 years of follow-up, no infection occurred at the surgical site.
Subsequent research has evaluated the outcomes of TJR procedures in HIV-infected adults who are not hemophiliacs. For instance, Parvizi et al[18] conducted a study on total hip and knee arthroplasties in 21 infected cases and reported a significant incidence of postoperative complications. Twelve of 21 arthroplasties needed to be reconsidered at the subsequent evaluation due to recurrent infection. Furthermore, there was a significant relationship between the immunological status of patients and the probability of deep infection (six joints). The authors mentioned above discovered a significant prevalence of Staphylococcus epidermidis, Pseudomonas aeruginosa, and Staphylococcus aureus among deep-seated infections[18].
In parallel to prior investigations, Habermann et al[55] have compared the incidence of total complications in non-hemophiliac infected cases and hemophiliac patients after TJR. However, they found no significant difference in functional outcomes[55].
Recently, Mahoney et al[56] conducted a study among non-hemophiliac HIV-infected patients who had total hip arthroplasty, demonstrating favorable functional results. Three years afterward, only one in 40 patients with a history of intravenous drug abuse had severe infection with antibiotic-resistant Staphylococcus aureus.
Moreover, further comorbidities associated with HIV, including intravenous drug abuse, negatively and significantly influence the clinical outcome of TJR surgery. On the other hand, Lehman et al[57] assessed the risk of PJI in HIV-infected patients and simultaneous infection from IV drug use (IVDU) following TJR. In the study mentioned above, patients with co-infection of HIV and IVDU had a more than 40% surgical site infection rate. Infections did not occur in four HIV-positive patients without comorbidities (IVDU, hemophilia). The findings of this study suggest an individual-based evaluation of the benefits and risks of TJR.
The functional consequences of THA in HIV-positive individuals are controversial in the literature. There is still considerable debate about the relative efficacy and safety of TJR in these patients. It was traditionally believed that HIV infection was associated with an augmented complication risk, particularly infectious adverse effects. In addition, the growing use of HAART has reduced the related complications. HIV-infected patients who do not receive HAART are more prone to unfavorable outcomes. Parvizi et al[18] found a substantial complication rate among HIV-infected cases who had undergone total hip arthroplasty; it is worth mentioning that 80% of them did not receive HAART. This amount included 29% of PJIs[58]. The mean CD4+ T-cell count for those who developed PJI was 239 cells/mm3, while the mean for the entire study population was 523 cells/mm3[58]. A similar result was displayed by Lehman et al[57]; they reported a PJI rate of 14.3% among HIV-infected cases receiving THA. It is worth mentioning that none of them were optimized by HAART.
Several studies have shown ambiguous functional results when comparing HIV-positive patients treated with HAART with the HIV-negative control group. Graham et al[59] conducted a survey among 43 THAs which had been performed on 29 HIV-positive patients in 2014; they reported no occurrences of dislocations, deep or superficial infections, or venous thrombotic events, either in late (> 6 wk) or early ( < 6 wk) follow-ups. Significant postoperative functional benefits and tangible progress in the Harris hip scores were recorded. Between 1998 and 2010, likewise, Naziri et al[60] conducted a study among 9275 HIV-positive patients with THA to evaluate the outcomes of THA and compare it to the results of 2.7 million non-infected cases. The rates of minor and major complications in HIV-infected individuals were 5.2% and 2.9%, respectively, meaningfully higher than the respective rates of 4.8% and 2.7% in non-infected individuals. In addition, a longer duration of hospitalization was observed in the HIV-positive group[60].
Sadoghi et al[61] analyzed global registration data from New Zealand, Australia, Denmark, Finland, Norway, and Sweden, showing that aseptic loosening is the main reason for revising THAs, which accounts for 55.7% of them. PJI was the third cause of revision[61]. The onset of aseptic loosening does not appear to be due to HIV[1,46].
One- and five-year survival rates after THA surgery in HIV-positive patients are similar to those of non-HIV-positive patients[1]. Issa et al[62] evaluated the lifespan of prostheses after ten years; there was no difference in the survival of infected and non-infected cases. Moreover, Novikov et al[63] showed that a significant amount of revision THA (80%) happened during the first year after surgery. Still, the revision rate in the long-term analysis was similar to that among non-infected patients[1]. Although functional outcomes of infected cases optimized with HAART are equal to those of HIV-negative cases, a higher probability of PJI has been reported.
Previously, THA outcomes in HIV-positive individuals with simultaneous hemophilia[19] or IVDU[57] showed a high proportion of poor outcomes and late deep infections. In a comprehensive assessment of 722 THAs out of 25 research studies, Enayatollahi et al[58] found that PJI is significantly more prevalent among those with simultaneous HIV infection and hemophilia than in HIV-infected alone. The corresponding PJI rates were 10.98% and 2.28%, respectively. Nevertheless, before HAART, the frequency of PJI was up to 50%[58]. The onset of HAART coincided with a reduction in the incidence of THA infections in HIV-positive individuals[46,58]. Also, Youngman et al[64] found that the complication rate of HIV-positive patients who were not treated with the HAART and did not undergo THAs due to femoral head osteonecrosis is 12.5% higher than that of patients who were optimized with HAART.
Given the increasing need for TJR and the HIV pandemic, it is essential to determine if a threshold should be proposed for elective arthroplasty. King et al[48] evaluated 30-d postoperative THA mortality in the United States retrospectively and found that HIV-positive patients had a higher mortality rate (3.4%) than HIV-negative patients (1.6%). Regardless of CD4+ T-cell count, the HIV-positive group had a higher mortality rate than the control group, even though lower CD4+ T-cell count was correlated with a greater mortality rate[48]. There is a hypothesis that a CD4+ T-cell count threshold of 200 cells/mm3 is associated with a higher risk of postoperative complications, such as PJI. However, this has not been proven[1,46].
There is considerable evidence that HIV-positive cases, particularly the poorly controlled ones, are more susceptible to postoperative complications[46]. Serum markers should be monitored periodically, as the infection is perilous, mainly if CD4+ T-cell counts decrease[46,65]. Many studies have not linked the CD4+ T-cell count consistently and accurately. Dimitriou et al[1] reported that THA might be safely administered to HIV-positive patients regardless of their CD4+ T-cell status, while Shah et al[46] suggested a CD4+ T-cell count of more than 400 cells/mm3 was essential for a safe THA. On the other hand, Sax et al[66] suggested that elective THA can be done in both groups of HIV-infected patients who are actively taking ART or not, and the complication rates are similar to those not infected by HIV.
Preoperative VL may be more important than CD4+ T-cell count. A higher level of the virus may indicate unsuccessful surgery and require a referral to an infectious disease specialist. Horberg et al[47] conducted a retrospective study on more than 5000 HIV-infected individuals; they believed that VL > 30000 copies/mL was related to a 3-fold bigger chance of postoperative complications.
In a systematic evaluation, Shah et al[46] recommended a VL of 50 copies/mL before elective procedures. It is suggested that patients continue the HAART regimen, and full compliance is essential. If the subsequent studies show a decrease in CD4+ T-cell count or an increase in VL, treatment mismatch or failure should be considered.
Currently, reports on HIV-positive patients and TJR afford contradictory information. While some authors reported significant complications and reconsideration rates following TJR on HIV-positive patients, most of these collections include a large proportion of HIV-infected cases with hemophilia. Thus, it is a critical confounder in the results described in prior studies. Future studies should evaluate the results of HIV-positive patients with no simultaneous disease to identify its risks, especially for patients with complete joint arthroplasty. Before surgery, we now examine each patient and try to optimize the general health of HIV-positive patients. Total joint replacement procedures are recommended based on patient-specific factors such as viral load, CD4+ T-cell count, clinical classification, history of intravenous drug addiction, and the patient's overall health. The risks and frequency of perioperative problems should be made clear to patients. We expect TJR to improve the quality of life of these patients. In Figure 1, we have recommendations for better outcomes of TJR in HIV-positive cases.
| 1. | Dimitriou D, Ramokgopa M, Pietrzak JRT, van der Jagt D, Mokete L. Human Immunodeficiency Virus Infection and Hip and Knee Arthroplasty. JBJS Rev. 2017;5:e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Mirghaderi SP, Sharifpour S, Moharrami A, Ahmadi N, Makuku R, Salimi M, Mortazavi SMJ. Determining the accuracy of preoperative total hip replacement 2D templating using the mediCAD® software. J Orthop Surg Res. 2022;17:222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 3. | Pietrzak JRT, Maharaj Z, Mokete L, Sikhauli N. Human immunodeficiency virus in total hip arthroplasty. EFORT Open Rev. 2020;5:164-171. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Permpalung N, Ungprasert P, Summachiwakij S, Leeaphorn N, Knight EL. Protease inhibitors and avascular necrosis: a systematic review and meta-analysis. Int J Antimicrob Agents. 2014;44:93-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Molia AC, Strady C, Rouger C, Beguinot IM, Berger JL, Trenque TC. Osteonecrosis in six HIV-infected patients receiving highly active antiretroviral therapy. Ann Pharmacother. 2004;38:2050-2054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Valencia ME, Barreiro P, Soriano V, Blanco F, Moreno V, Lahoz JG. Avascular necrosis in HIV-infected patients receiving antiretroviral treatment: study of seven cases. HIV Clin Trials. 2003;4:132-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Mary-Krause M, Billaud E, Poizot-Martin I, Simon A, Dhiver C, Dupont C, Salmon D, Roudiere L, Costagliola D; Clinical Epidemiology Group of the French Hospital Database. Risk factors for osteonecrosis in HIV-infected patients: impact of treatment with combination antiretroviral therapy. AIDS. 2006;20:1627-1635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 8. | Morse CG, Mican JM, Jones EC, Joe GO, Rick ME, Formentini E, Kovacs JA. The incidence and natural history of osteonecrosis in HIV-infected adults. Clin Infect Dis. 2007;44:739-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 83] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 9. | Knobel H, Guelar A, Vallecillo G, Nogués X, Díez A. Osteopenia in HIV-infected patients: is it the disease or is it the treatment? AIDS. 2001;15:807-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 124] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 10. | Warriner AH, Mugavero MJ. Bone changes and fracture risk in individuals infected with HIV. Curr Rheumatol Rep. 2010;12:163-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Triant VA, Brown TT, Lee H, Grinspoon SK. Fracture prevalence among human immunodeficiency virus (HIV)-infected vs non-HIV-infected patients in a large U.S. healthcare system. J Clin Endocrinol Metab. 2008;93:3499-3504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 401] [Cited by in RCA: 395] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 12. | Mirghaderi SP, Baghdadi S, Salimi M, Shafiei SH. Scientometric Analysis of the Top 50 Most-Cited Joint Arthroplasty Papers: Traditional vs Altmetric Measures. Arthroplast Today. 2022;15:81-92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Eka A, Chen AF. Patient-related medical risk factors for periprosthetic joint infection of the hip and knee. Ann Transl Med. 2015;3:233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 64] [Reference Citation Analysis (0)] |
| 14. | Edwards PK, Mears SC, Stambough JB, Foster SE, Barnes CL. Choices, Compromises, and Controversies in Total Knee and Total Hip Arthroplasty Modifiable Risk Factors: What You Need to Know. J Arthroplasty. 2018;33:3101-3106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 71] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 15. | Moharrami A, Mirghaderi SP, Hoseini-Zare N, Kaseb MH, Moazen-Jamshidi SMM, Mansour AK, Mortazavi SMJ. Restoring femoral medial offset could reduce pelvic obliquity following primary total hip arthroplasty, an observational study. Int Orthop. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Jellis JE. Orthopaedic surgery and HIV disease in Africa. Int Orthop. 1996;20:253-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 53] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Paiement GD, Hymes RA, LaDouceur MS, Gosselin RA, Green HD. Postoperative infections in asymptomatic HIV-seropositive orthopedic trauma patients. J Trauma. 1994;37:545-50; discussion 550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Parvizi J, Sullivan TA, Pagnano MW, Trousdale RT, Bolander ME. Total joint arthroplasty in human immunodeficiency virus-positive patients: an alarming rate of early failure. J Arthroplasty. 2003;18:259-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 76] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 19. | Ragni MV, Crossett LS, Herndon JH. Postoperative infection following orthopaedic surgery in human immunodeficiency virus-infected hemophiliacs with CD4 counts < or = 200/mm3. J Arthroplasty. 1995;10:716-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 112] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Rodriguez-Merchan EC, Wiedel JD. Total knee arthroplasty in HIV-positive haemophilic patients. Haemophilia. 2002;8:387-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Zainul-Abidin S, Amanatullah DF, Anderson MB, Austin M, Barretto JM, Battenberg A, Bedard NA, Bell K, Blevins K, Callaghan JJ, Cao L, Certain L, Chang Y, Chen JP, Cizmic Z, Coward J, DeMik DE, Diaz-Borjon E, Enayatollahi MA, Feng JE, Fernando N, Gililland JM, Goodman S, Greenky M, Hwang K, Iorio R, Karas V, Khan R, Kheir M, Klement MR, Kunutsor SK, Limas R, Morales Maldonado RA, Manrique J, Matar WY, Mokete L, Nung N, Pelt CE, Pietrzak JRT, Premkumar A, Rondon A, Sanchez M, Novaes de Santana C, Sheth N, Singh J, Springer BD, Tay KS, Varin D, Wellman S, Wu L, Xu C, Yates AJ. General Assembly, Prevention, Host Related General: Proceedings of International Consensus on Orthopedic Infections. J Arthroplasty. 2019;34:S13-S35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 22. | Centers for Disease Control and Prevention (CDC). Revised surveillance case definition for HIV infection--United States, 2014. MMWR Recomm Rep. 2014;63:1-10. [PubMed] |
| 23. | Harrison WJ. HIV/AIDS in trauma and orthopaedic surgery. J Bone Joint Surg Br. 2005;87:1178-1181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Goorney BP, Lacey H, Thurairajasingam S, Brown JD. Avascular necrosis of the hip in a man with HIV infection. Genitourin Med. 1990;66:451-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Allison GT, Bostrom MP, Glesby MJ. Osteonecrosis in HIV disease: epidemiology, etiologies, and clinical management. AIDS. 2003;17:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Yombi JC, Vandercam B, Wilmes D, Dubuc JE, Vincent A, Docquier PL. Osteonecrosis of the femoral head in patients with type 1 human immunodeficiency virus infection: clinical analysis and review. Clin Rheumatol. 2009;28:815-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | de Larrañaga G, Bottaro E, Martinuzzo M, Figueroa R, Iglesias Varela ML, Perés Wingeyer S, Forastiero R, Adamczuk Y, Corti M, Puga L, Benetucci J. Thrombophilia in human immunodeficiency virus-infected patients with osteonecrosis: Is there a real connection? Clin Appl Thromb Hemost. 2009;15:340-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Ries MD, Barcohana B, Davidson A, Jergesen HE, Paiement GD. Association between human immunodeficiency virus and osteonecrosis of the femoral head. J Arthroplasty. 2002;17:135-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Miller KD, Masur H, Jones EC, Joe GO, Rick ME, Kelly GG, Mican JM, Liu S, Gerber LH, Blackwelder WC, Falloon J, Davey RT, Polis MA, Walker RE, Lane HC, Kovacs JA. High prevalence of osteonecrosis of the femoral head in HIV-infected adults. Ann Intern Med. 2002;137:17-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 118] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 30. | Brown P, Crane L. Avascular necrosis of bone in patients with human immunodeficiency virus infection: report of 6 cases and review of the literature. Clin Infect Dis. 2001;32:1221-1226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 61] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 31. | Gutiérrez F, Padilla S, Masiá M, Flores J, Boix V, Merino E, Galindo J, Ortega E, López-Aldeguer J, Galera C; HIV-related Osteonecrosis Study Group. Osteonecrosis in patients infected with HIV: clinical epidemiology and natural history in a large case series from Spain. J Acquir Immune Defic Syndr. 2006;42:286-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 32. | Rothman MS, Bessesen MT. HIV infection and osteoporosis: pathophysiology, diagnosis, and treatment options. Curr Osteoporos Rep. 2012;10:270-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 33. | Muthumani K, Choo AY, Zong WX, Madesh M, Hwang DS, Premkumar A, Thieu KP, Emmanuel J, Kumar S, Thompson CB, Weiner DB. The HIV-1 Vpr and glucocorticoid receptor complex is a gain-of-function interaction that prevents the nuclear localization of PARP-1. Nat Cell Biol. 2006;8:170-179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 58] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 34. | Galrão L, Brites C, Atta ML, Atta A, Lima I, Gonzalez F, Magalhães F, Santiago M. Antiphospholipid antibodies in HIV-positive patients. Clin Rheumatol. 2007;26:1825-1830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 35. | Santos JL, Cruz I, Martín Herrero F, Albarrán C, González Matas JM, Martín Luengo C. [Recurrent coronary thrombosis, factor V Leiden, primary antiphospholipid syndrome and HIV]. Rev Esp Cardiol. 2004;57:997-999. [PubMed] |
| 36. | Penzak SR, Formentini E, Alfaro RM, Long M, Natarajan V, Kovacs J. Prednisolone pharmacokinetics in the presence and absence of ritonavir after oral prednisone administration to healthy volunteers. J Acquir Immune Defic Syndr. 2005;40:573-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 39] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 37. | Morty RE, Morris A. World AIDS Day 2021: highlighting the pulmonary complications of HIV/AIDS. Am J Physiol Lung Cell Mol Physiol. 2021;321:L1069-L1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 38. | Barnhart M, Shelton JD. ARVs: the next generation. Going boldly together to new frontiers of HIV treatment. Glob Health Sci Pract. 2015;3:1-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 39. | Meintjes G, Moorhouse MA, Carmona S, Davies N, Dlamini S, van Vuuren C, Manzini T, Mathe M, Moosa Y, Nash J, Nel J, Pakade Y, Woods J, Van Zyl G, Conradie F, Venter F. Adult antiretroviral therapy guidelines 2017. South Afr J HIV Med. 2017;18:776. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 139] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 40. | Fletcher C, Bartlett J, Sax P, Mitty J. Overview of antiretroviral agents used to treat HIV. UpToDate. 2018. Available from: https://www.uptodate.com/contents/overview-of-antiretroviral-agents-used-to-treat-hiv. |
| 41. | Kunutsor SK, Whitehouse MR, Blom AW, Beswick AD; INFORM Team. Patient-Related Risk Factors for Periprosthetic Joint Infection after Total Joint Arthroplasty: A Systematic Review and Meta-Analysis. PLoS One. 2016;11:e0150866. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 378] [Cited by in RCA: 362] [Article Influence: 36.2] [Reference Citation Analysis (0)] |
| 42. | Reusch JE. Diabetes, microvascular complications, and cardiovascular complications: what is it about glucose? J Clin Invest. 2003;112:986-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 43. | Seneviratne CJ, Yip JW, Chang JW, Zhang CF, Samaranayake LP. Effect of culture media and nutrients on biofilm growth kinetics of laboratory and clinical strains of Enterococcus faecalis. Arch Oral Biol. 2013;58:1327-1334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 55] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 44. | Berbari EF, Osmon DR, Lahr B, Eckel-Passow JE, Tsaras G, Hanssen AD, Mabry T, Steckelberg J, Thompson R. The Mayo prosthetic joint infection risk score: implication for surgical site infection reporting and risk stratification. Infect Control Hosp Epidemiol. 2012;33:774-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 118] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 45. | Libman H, Bartlett J, Bloom A. Surgical issues in HIV infection. UpToDate Literature review current through: October. 2018. |
| 46. | Shah KN, Truntzer JN, Touzard Romo F, Rubin LE. Total Joint Arthroplasty in Patients with Human Immunodeficiency Virus. JBJS Rev. 2016;4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 47. | Horberg MA, Hurley LB, Klein DB, Follansbee SE, Quesenberry C, Flamm JA, Green GM, Luu T. Surgical outcomes in human immunodeficiency virus-infected patients in the era of highly active antiretroviral therapy. Arch Surg. 2006;141:1238-1245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 95] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 48. | King JT Jr, Perkal MF, Rosenthal RA, Gordon AJ, Crystal S, Rodriguez-Barradas MC, Butt AA, Gibert CL, Rimland D, Simberkoff MS, Justice AC. Thirty-day postoperative mortality among individuals with HIV infection receiving antiretroviral therapy and procedure-matched, uninfected comparators. JAMA Surg. 2015;150:343-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 49. | Mdodo R, Frazier EL, Dube SR, Mattson CL, Sutton MY, Brooks JT, Skarbinski J. Cigarette smoking prevalence among adults with HIV compared with the general adult population in the United States: cross-sectional surveys. Ann Intern Med. 2015;162:335-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 386] [Article Influence: 35.1] [Reference Citation Analysis (0)] |
| 50. | Gregg-Smith SJ, Pattison RM, Dodd CA, Giangrande PL, Duthie RB. Septic arthritis in haemophilia. J Bone Joint Surg Br. 1993;75:368-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 51. | Wiedel J, Luck J, Gilbert M. Total knee arthroplasty in the patient with haemophilia: evaluation and long-term results. Musculoskeletal problems in hemophilia National Hemophilia Foundation. 1989: 152-7. |
| 52. | Hicks JL, Ribbans WJ, Buzzard B, Kelley SS, Toft L, Torri G, Wiedel JD, York J. Infected joint replacements in HIV-positive patients with haemophilia. J Bone Joint Surg Br. 2001;83:1050-1054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 53. | Powell DL, Whitener CJ, Dye CE, Ballard JO, Shaffer ML, Eyster ME. Knee and hip arthroplasty infection rates in persons with haemophilia: a 27 year single center experience during the HIV epidemic. Haemophilia. 2005;11:233-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 56] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 54. | Unger AS, Kessler CM, Lewis RJ. Total knee arthroplasty in human immunodeficiency virus-infected hemophiliacs. J Arthroplasty. 1995;10:448-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 46] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 55. | Habermann B, Eberhardt C, Kurth AA. Total joint replacement in HIV positive patients. J Infect. 2008;57:41-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 56. | Mahoney CR, Glesby MJ, DiCarlo EF, Peterson MG, Bostrom MP. Total hip arthroplasty in patients with human immunodeficiency virus infection: pathologic findings and surgical outcomes. Acta Orthop. 2005;76:198-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 57. | Lehman CR, Ries MD, Paiement GD, Davidson AB. Infection after total joint arthroplasty in patients with human immunodeficiency virus or intravenous drug use. J Arthroplasty. 2001;16:330-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 86] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 58. | Enayatollahi MA, Murphy D, Maltenfort MG, Parvizi J. Human Immunodeficiency Virus and Total Joint Arthroplasty: The Risk for Infection Is Reduced. J Arthroplasty. 2016;31:2146-2151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 59. | Graham SM, Lubega N, Mkandawire N, Harrison WJ. Total hip replacement in HIV-positive patients. Bone Joint J. 2014;96-B:462-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 60. | Naziri Q, Boylan MR, Issa K, Jones LC, Khanuja HS, Mont MA. Does HIV infection increase the risk of perioperative complications after THA? Clin Orthop Relat Res. 2015;473:581-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 61. | Sadoghi P, Liebensteiner M, Agreiter M, Leithner A, Böhler N, Labek G. Revision surgery after total joint arthroplasty: a complication-based analysis using worldwide arthroplasty registers. J Arthroplasty. 2013;28:1329-1332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 265] [Cited by in RCA: 317] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 62. | Issa K, Naziri Q, Rasquinha V, Maheshwari AV, Delanois RE, Mont MA. Outcomes of cementless primary THA for osteonecrosis in HIV-infected patients. J Bone Joint Surg Am. 2013;95:1845-1850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 63. | Novikov D, Anoushiravani AA, Chen KK, Wolfson TS, Snir N, Schwarzkopf R. Total Hip Arthroplasty in Human Immunodeficiency Virus-Positive Patients: A Concise Follow-Up at 10 to 14 Years. J Arthroplasty. 2019;34:522-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 64. | Youngman TR, Riepen DW, Rinehart DB, Thota DR, Sun JJ, Telford CL, Huo MH. Complications of primary total hip arthroplasty in human immunodeficiency virus-positive patients with femoral head osteonecrosis. Hip Int. 2021;11207000211005750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 65. | Lin CA, Kuo AC, Takemoto S. Comorbidities and perioperative complications in HIV-positive patients undergoing primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2013;95:1028-1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 89] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 66. | Sax OC, Mohamed NS, Pervaiz SS, Douglas SJ, Aboulafia AJ, Delanois RE. The Effect of Modern Antiretroviral Therapy on Complication Rates After Total Hip Arthroplasty. JB JS Open Access. 2021;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Iran
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bharara T, India S-Editor: Liu JH L-Editor: Wang TQ P-Editor: Liu JH