Peer-review started: November 4, 2020
First decision: December 11, 2020
Revised: December 22, 2020
Accepted: January 8, 2021
Article in press: January 8, 2021
Published online: March 25, 2021
Processing time: 132 Days and 3.3 Hours
Human immunodeficiency virus (HIV) infection is a major global public health concern. North African countries carry a disproportionate burden of HIV representing one of the highest rates in Africa.
To characterize the epidemiological and spatial trends of HIV infection in this region.
A systematic review was carried out on all the published data regarding HIV/acquired immunodeficiency syndrome in North African countries over ten years (2008-2017) following the PRISMA guidelines. We performed a comprehensive literature search using Medline PubMed, Embase, regional and international databases, and country-level reports with no language restriction. The quality, quantity, and geographic coverage of the data were assessed at both the national and regional levels. We used random-effects methods, spatial variables, and stratified results by demographic factors. Only original data on the prevalence of HIV infection were included and independently evaluated by professional epidemiologists.
A total of 721 records were identified but only 41 that met the criteria were included in the meta-analysis. There was considerable variability in the prevalence estimates of HIV within the countries of the region. The overall prevalence of HIV ranged from 0.9% [95% confidence interval (CI) 0.8-1.27] to 3.8% (95%CI 1.17-6.53). The highest prevalence was associated with vulnerable groups and particularly drug abusers and sexually promiscuous individuals. The dense HIV clustering noted varied from one country to another. At least 13 HIV subtypes and recombinant forms were prevalent in the region. Subtype B was the most common variant, followed by CRF02_AG.
This comprehensive review indicates that HIV infection in North African countries is an increasing threat. Effective national and regional strategies are needed to improve monitoring and control of HIV transmission, with particular emphasis on geographic variability and HIV clustering.
Core Tip: North Africa is a unique geographical region located on the southern Mediterranean basin and represents the largest region of Africa. Human immunodeficiency virus (HIV) infection is an increasing threat in this region. Previous studies analyzed mainly the risk factors associated with risk groups at a national level and no single study has yet analyzed the actual epidemiological situation of HIV/acquired immunodeficiency syndrome (AIDS) in the whole region. This review aims to analyze and characterize the epidemiological and geographic variation of HIV/AIDS in North African countries and to highlight the strategies needed to combat this epidemic at the national and regional levels.
- Citation: Daw MA, Ahmed MO. Epidemiological characterization and geographic distribution of human immunodeficiency virus/acquired immunodeficiency syndrome infection in North African countries. World J Virol 2021; 10(2): 69-85
- URL: https://www.wjgnet.com/2220-3249/full/v10/i2/69.htm
- DOI: https://dx.doi.org/10.5501/wjv.v10.i2.69
Human immunodeficiency virus (HIV) is one of the most important viruses and has had demographic, economic, social, and even political consequences. Since its discovery in the 1980s, HIV/acquired immunodeficiency syndrome (AIDS) has remained an important public health concern worldwide. Its prevalence has rapidly increased, particularly in developing countries[1,2]. As of 2012, over 70 million people have become infected with HIV, of whom over 35 million have died. Africa is the most severely affected geographical area, and over 70% of the people infected with HIV reside in Africa[3,4].
A variety of factors have contributed to the spread of HIV/AIDS. These factors vary from one region to another and even within districts in the same region. Recent reports indicate that homosexuality (men who have sex with men, MSM) has become the dominant mode of transmission among newly diagnosed HIV infections in North America, East, Southeast and South Asia, and Latin America[5-7].
North Africa is a vast region representing over 30% of the African continent, with a coast extending from the Atlantic Ocean to the Mediterranean basin facing the southern part of the European Union[8]. The region has experienced major political and demographic challenges, particularly in the previous decade after the Arab spring. This has been complicated by wars, lack of security, major population displacements, weakening of public health systems, and the influx of immigrants, particularly from western and sub-Saharan Africa[9-11].
The incidence of HIV has been increasing more rapidly in North Africa than in any other global region, and AIDS-related mortality has almost doubled in the past decade. Comparable to West and Central African regions, HIV transmission rates in the region rose by over 10% during this decade, with a substantial increase in HIV morbidity and mortality. This has been faced by ignorance and polemic thinking even among health professionals[12,13]. Too often, patients living with HIV face denial of care, stigma, discrimination, and breach of confidentiality[14].
Furthermore, HIV infection has not been well addressed as a public health challenge in the region, and the hidden pandemic is believed to be driven by risky behaviors (such as sexual and drug-related factors) that are not well tolerated in society. The epidemiology of HIV in the region remains poorly defined. This has been complicated by the lack of accurate surveillance data, and even the existing data are prone to underestimation biases that mask the real picture of new HIV infections in the region[12].
Few studies have been conducted on the prevalence of HIV and its associated factors in North Africa. These studies present inconclusive findings on the prevalence of HIV and its associated factors[15]. Therefore, this systematic review was conducted to assess the prevalence of HIV and its associated factors in the region based on the published evidence (http://www.prisma-statement.org/). The findings of this review could be useful for designing strategies to reduce the prevalence of HIV and implement effective programs to combat its consequences.
A systematic search was conducted using PubMed, Medline, Google Scholar and Embase to identify studies on HIV in North African countries published between January 1st, 2008 and December 31st, 2017 without language restriction using the search terms HIV or AIDS, OR ‘‘human immunodeficiency virus’’ OR ‘‘acquired immunodeficiency syndrome’’ prevalence, incidence in “Northern Africa”, and in every country within the region. The search was restricted to North African countries and encompassed Egypt, Libya, Tunisia, Algeria, Morocco, Mauritania and Sudan, which share historical, sociocultural, linguistic and religious characteristics. Reports from the World Health Organization were also included. To minimize publication bias, we retrieved the reference lists and manually searched for relevant studies that met our inclusion criteria, in addition to regional and country-level scientific databases. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses, http://www.prisma-statement.org/) guidelines were followed to aggregate the data[16,17].
Studies of any design that estimated the prevalence or incidence of HIV in North African countries were initially included. The inclusion criteria were based on whether the study provided sufficient information on the prevalence, incidence, and demographic and risk factors. Studies were accepted if descriptions of HIV testing methods were included, such as laboratory-derived HIV status using biological specimens and primary data from populations in the North African countries. To be included, studies had to have a minimum sample size of 25, detailed descriptions of the sampling procedure, HIV testing, and analytical methods. The sources included peer-reviewed journals and non-peer-reviewed publications meeting other criteria and available online in the public domain. Duplicates were identified by comparing detailed study characteristics, including author names, study period, study location, number of infected cases, and sample size. If two publications were found to be from the same data source, only the earlier publication was included. Excluded were case reports, case series, editorials, letters to editors, commentaries, literature reviews, studies reporting HIV prevalence based on self-reporting, studies on HIV status rather than biological testing, and studies that do not mention the study period/time and geographical location.
The titles and abstracts of all the records retrieved were screened for relevance independently and categorized according to the quality of the study design and methods. The following information was extracted from all the eligible studies: first author, publication year, study location, study period, sampling method, sample size, and the laboratory testing method for HIV infection. The studies were categorized according to countries and the type of population. Details of each study were entered into a database by one investigator and rechecked in full. Quality assessment was carried out using a standard procedure[6].
Two trained epidemiologists (MD, MO) independently reviewed these publications and examined the sample size, sampling method, testing procedures, results, and interpretation of the data. Disagreements were resolved by consensus or arbitration by MD. A quality score between 1 and 5 was calculated for every paper based on these criteria.
Statistical analysis was carried out by calculating the percentages and confidence intervals (CI), random-effects model, crude odds ratios (OR), sensitivity analysis, and cut-off P value (P < 0.1). Heterogeneity was tested by the chi-square test. The prevalence of HIV was calculated as an average of the pooled infection prevalence of each country weighted by the ratio of the country’s population to the study’s sample size. The risk of bias in reporting the prevalence and cumulative incidence was independently calculated by the authors. Publication bias was assessed by inspection of a funnel plot and Egger’s test. Analyses of the aggregated prevalence rates of each country were performed with metan, which is an average of the individual study results weighted by the inverse of their variances using a fixed/random model[18]. Geographic mapping and spatial variables were carried out using the national data in each country and localized clusters of spots are reported as previously published[19,20].
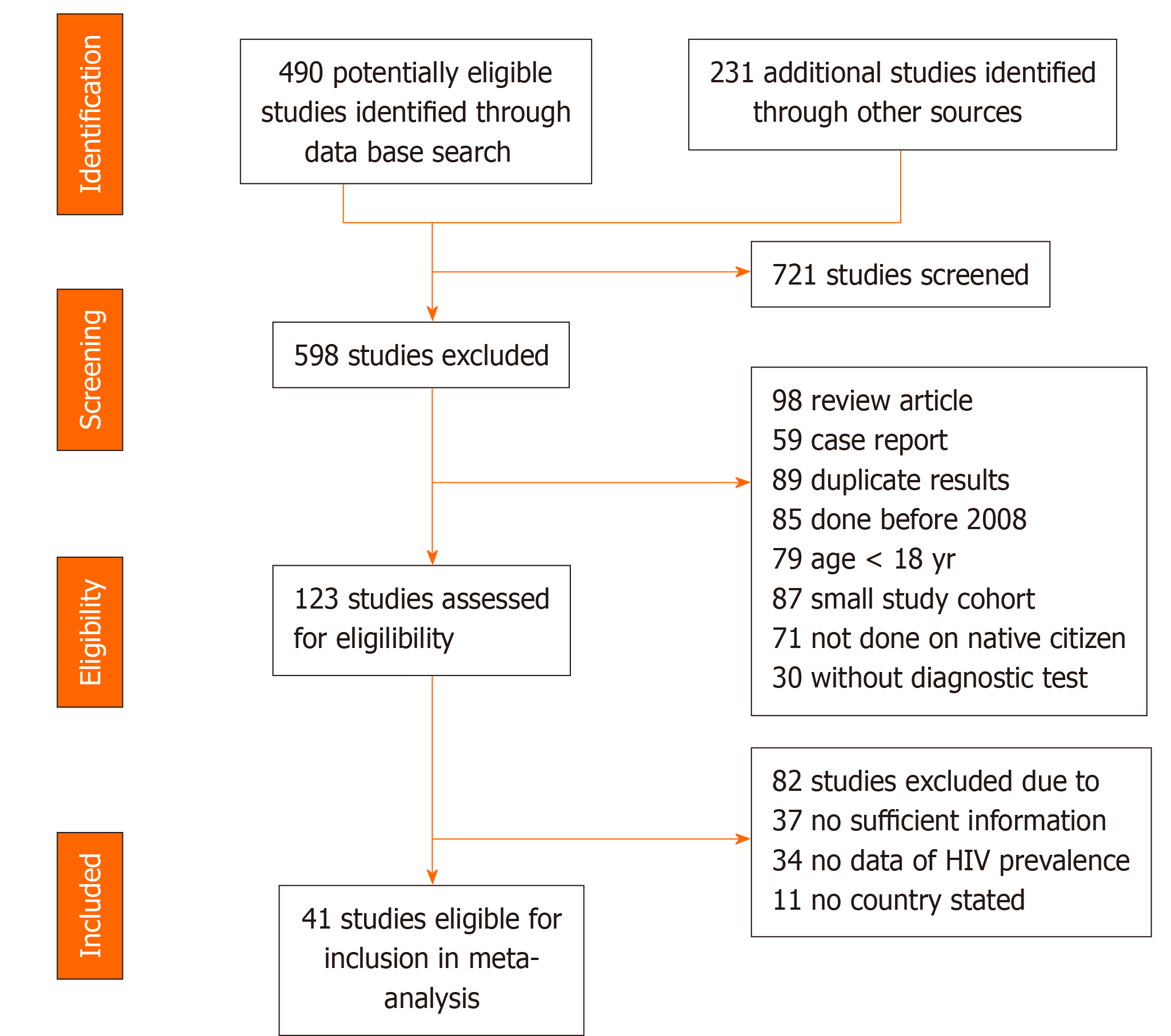
A total of 721 records were identified during the 10-year period (2008-2017). Following the elimination of duplicates, 646 studies remained. When the titles and abstracts were screened, 598 not fulfilling the selection criteria were excluded and only 48 were assessed for eligibility. Seven of these were excluded and only 41 were finally included in the meta-analysis. The steps of study selection are illustrated diagramattically in Figure 1. There was a steady increase in the number of publications and HIV records in North Africa with a slight increase in the last two years. The highest population and HIV data notification were reported in Morocco, Egypt, Sudan and to lesser extent in Libya and Tunisia. It was very low in Algeria and Mauritania. The characteristics of the studies included in the analysis are presented in Table 1.
| Characteristics | Studies, n |
| Country | |
| Algeria | 4 |
| Egypt | 7 |
| Libya | 6 |
| Mauritania | 2 |
| Morocco | 11 |
| Sudan | 7 |
| Tunisia | 4 |
| Study design | |
| Cross-sectional | 30 |
| Cohort study | 11 |
| Data collection | |
| Prospective | 32 |
| Retrospective | 9 |
| Study area/site | |
| Hospital oriented | 19 |
| Population oriented | 22 |
| Sampling method | |
| Random | 21 |
| Consecutive | 14 |
| Not reported | 6 |
Study quality assessment showed that seven studies were of a low quality and no full text was available, 28 had moderate quality, and only six high-quality studies were identified. However, after analysis according to quality assessment, no significant difference was noted between studies of high/medium quality and those with low/medium quality.
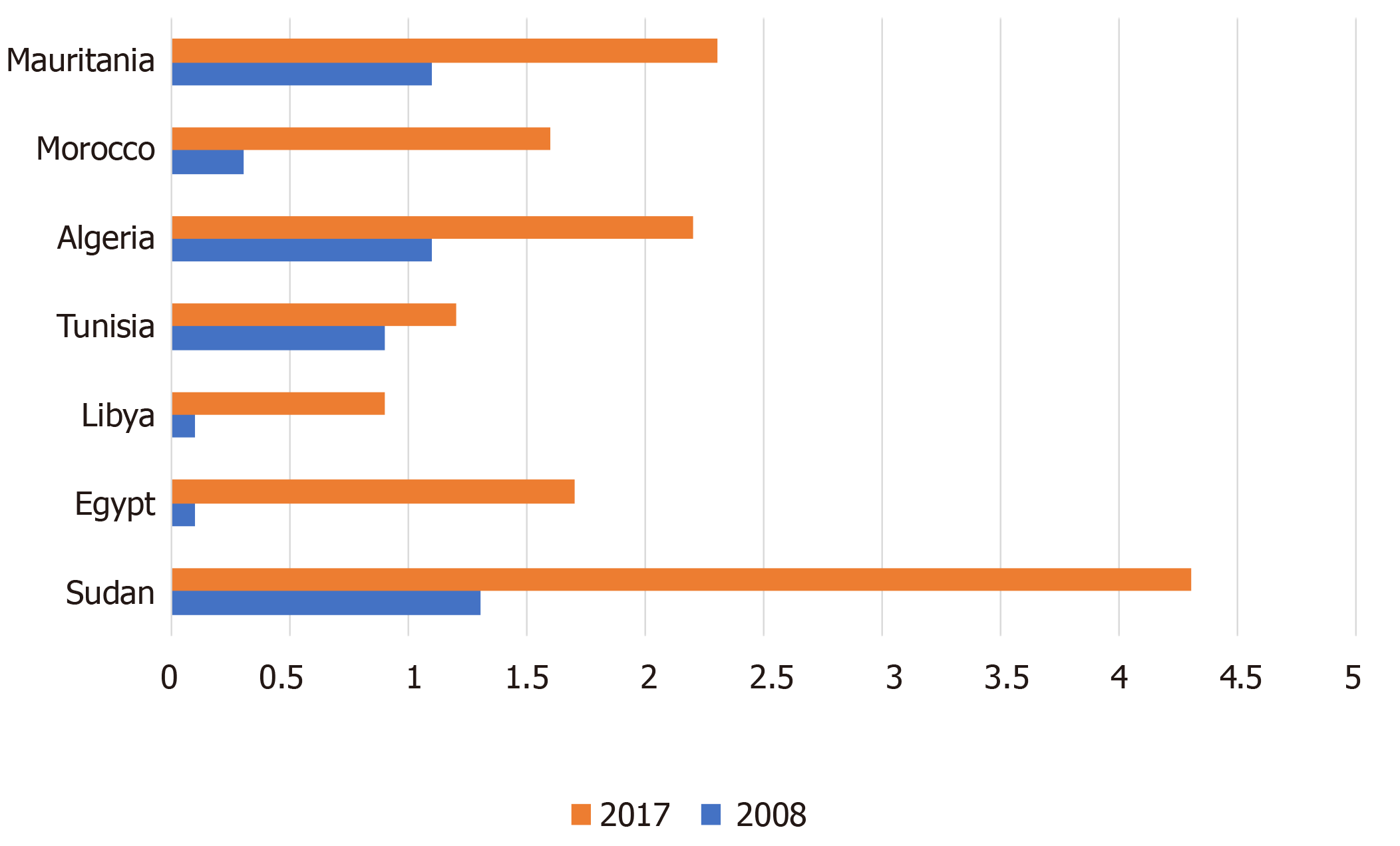
During the study period, there was an increasing trend in the prevalence of HIV/AIDS in the North African region with much variation among the countries (Figure 2). In 2008, the highest prevalence was reported in Sudan (1.3%) followed by Algeria (1.2%) and Mauritania (1.3%)[21-23]. However, it was less than 1% in Tunisia (0.9%), Morocco (0.3%), Egypt (0.2%) and Libya (0.2%)[24-27]. Ten years later, the overall prevalence increased significantly by more than four-fold (P ≤ 0.001). In 2017, the highest prevalence rate was reported in Sudan (4.3%), followed by Mauritania (2.3%), Algeria (2.2%), Egypt (1.8%), Morocco (1.6%), Tunisia (1.2%) and Libya (0.9%). The overall prevalence of HIV in North Africa varied not only among the countries but also within the population of the same country, as illustrated in the Forest plot (Figure 3). There was a clear relationship between the prevalence of HIV and attributable risk factors. The general population and ordinary patients had low HIV prevalence comparable to other studied groups. For instance, studies on blood donors and pregnant women in Egypt, Mauritania, Sudan and Morocco, and those carried out on the general population in Libya, Tunisia and Algeria showed a low HIV prevalence, but the prevalence was elevated in the risk groups within the same country. The overall odds ratio in the meta-analysis demonstrated a statistically significant variation among the populations studied, and the association appears stronger in the studies related to high-risk groups. The test of heterogeneity showed significant variation among the studies, indicating the nature and quality of these studies.
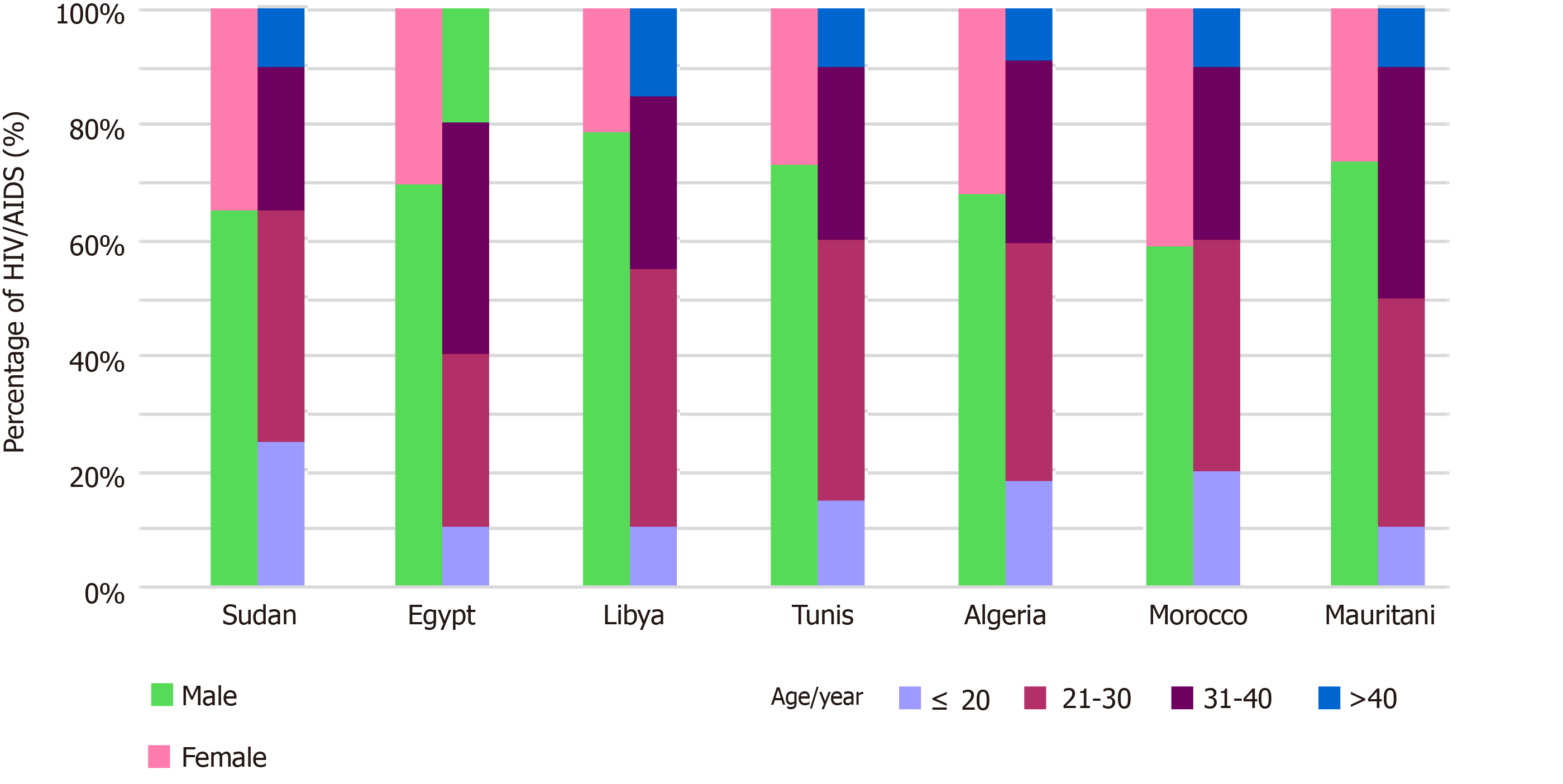
Figure 4 illustrates the sex- and age-specific distribution of HIV/AIDS in North African countries. Between 2008 and 2017, 76.9% of the reported cases were males and 25.1% were females, giving a male to female ratio of 3.1:1. Although his trend was found in most North African countries, the number of infected females was similar to that of males in Morocco. Among the HIV/AIDS cases reported, the prevalence of infection was highest among the 21-30 years age group (45%) compared to the 31-40 years age group (30%). A marked increase in the number of HIV/AIDS cases was reported among those aged < 20 years, particularly in Sudan, Algeria and Morocco. The prevalence of HIV/AIDS infections among those aged above 40 years was similar among all countries at 20%, apart from Libya, which showed a higher rate of up to 30%. A few studies from Libya, Morocco and Sudan have reported on the relation between HIV/AIDS and educational level and marital status. Most of the infected cases were found among unmarried individuals who were mainly illiterate or had a low level of education[28-31].
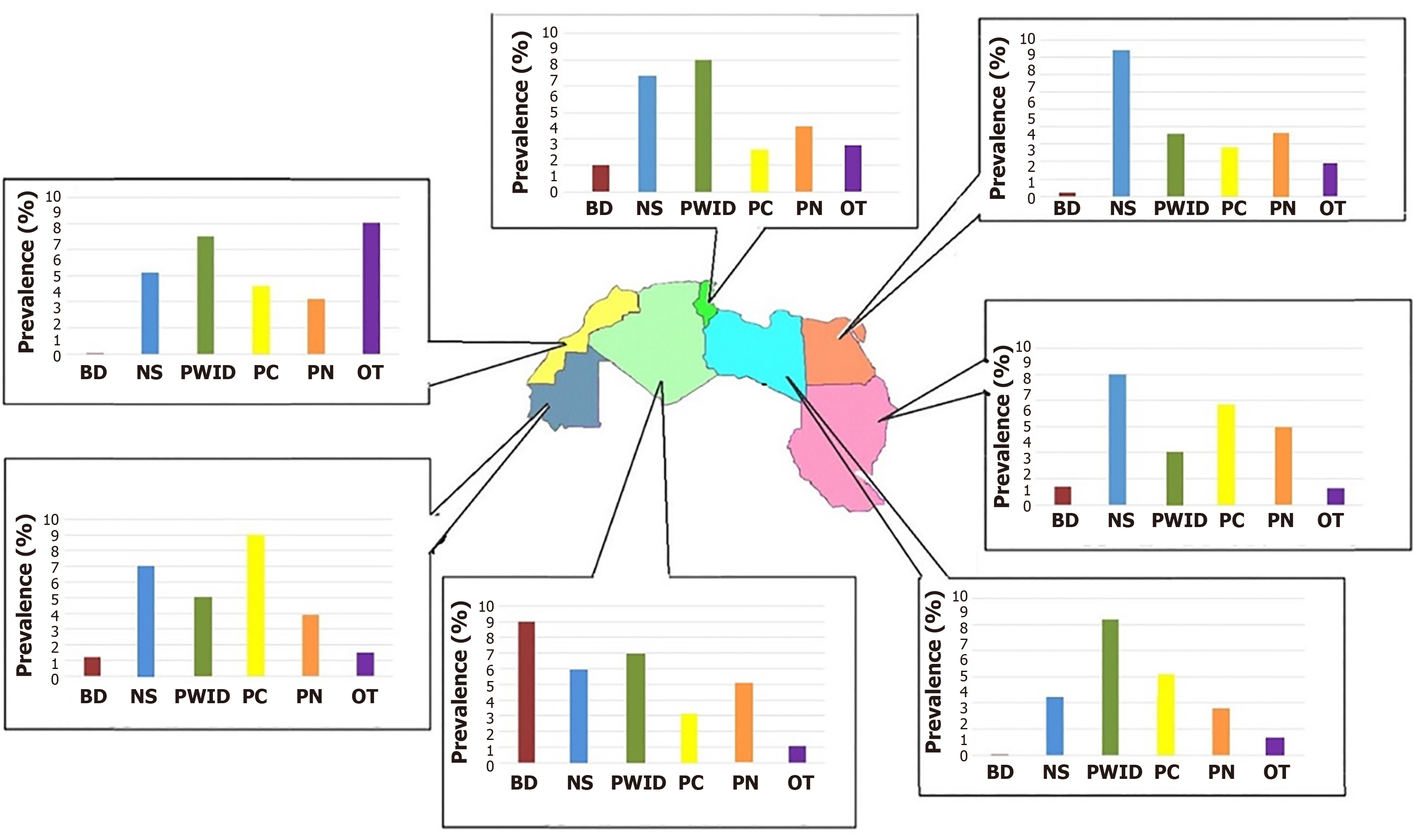
Figure 5 shows the prevalence of HIV/AIDS among high-risk groups in North African countries. The highest prevalence was reported among injection drug users (IDUs), with an estimated median of 8% and a range from 3.80% (95%CI 2.46-4.67) to 15.7% (95%CI 9.46-18.67). This was particularly high in Morocco, Egypt, Sudan and Libya.
HIV/AIDS among sexually promiscuous individuals was reported to average 2.8% (1.7%-11.3%). It was reported to be 4.9% in Morocco, Algeria, Tunisia and Egypt and > 10.5% in Tunisia and Sudan[32-35]. Among prisoners, it was reported to be high in Libya, Sudan, Morocco and Egypt, but less in Mauritania and Algeria. HIV was also reported to be high in hospital care settings in North African countries, with a range of 0.8% to 9.7%[36-40]. The highest prevalence rates were reported in Mauritania, Algeria and Egypt, followed by Sudan, Tunisia, Morocco and Libya.
Based on our data, the genotype distribution of HIV in the seven North African countries is shown in Figure 6. Analysis of HIV-1 subtype distribution is scanty, particularly in Algeria and Mauritania, where only one study was reported in each of these two countries[41,42]. The Tunisian sequences belong to six HIV-1 subtypes (B, A1, G, D, C, and F2), five circulating recombinant forms (CRF02_AG, CRF25_cpx, CRF43_02G, CRF06_cpx and CRF19_cpx) and 11 unique recombinant forms. Subtype B (46.4%) and CRF02_AG (39.4%) were the predominant genetic forms[43]. Genetic analysis of HIV-1 strains in Libya demonstrated low subtype heterogeneity with the evolution of subtype B, which represents 74%, followed by CRF_20 AG (18%) and HIV-1 subtype A (8%). In Sudan, 50% were subtype D and 30% were subtype C. Subtypes A and B and three unique recombinants were also found, some partially unclassifiable[44-46]. In Morocco, subtype B was the predominant subtype (76.7%), followed by a high diversity of non-B subtypes, especially CRF02_AG recombinant (15%), and to a smaller extent subtype A (1.0%) and F strains (0.5%). In Egypt, the commonly isolated strains of subtype B comprise 95%, followed by CRF01_AE and A (1%). In Algeria, there was considerable HIV-1 diversity with a predominance of the B subtype followed by CRF02_AG and CRF06_cpx.5,6. Studies have indicated that the diversity was maintained, but CRF06_cpx became widely predominant. Phylogenetic analysis of different strains in Mauritania revealed that CRF02_AG (64.6%) was the predominant strain followed by B variants with a predominance of 10%.
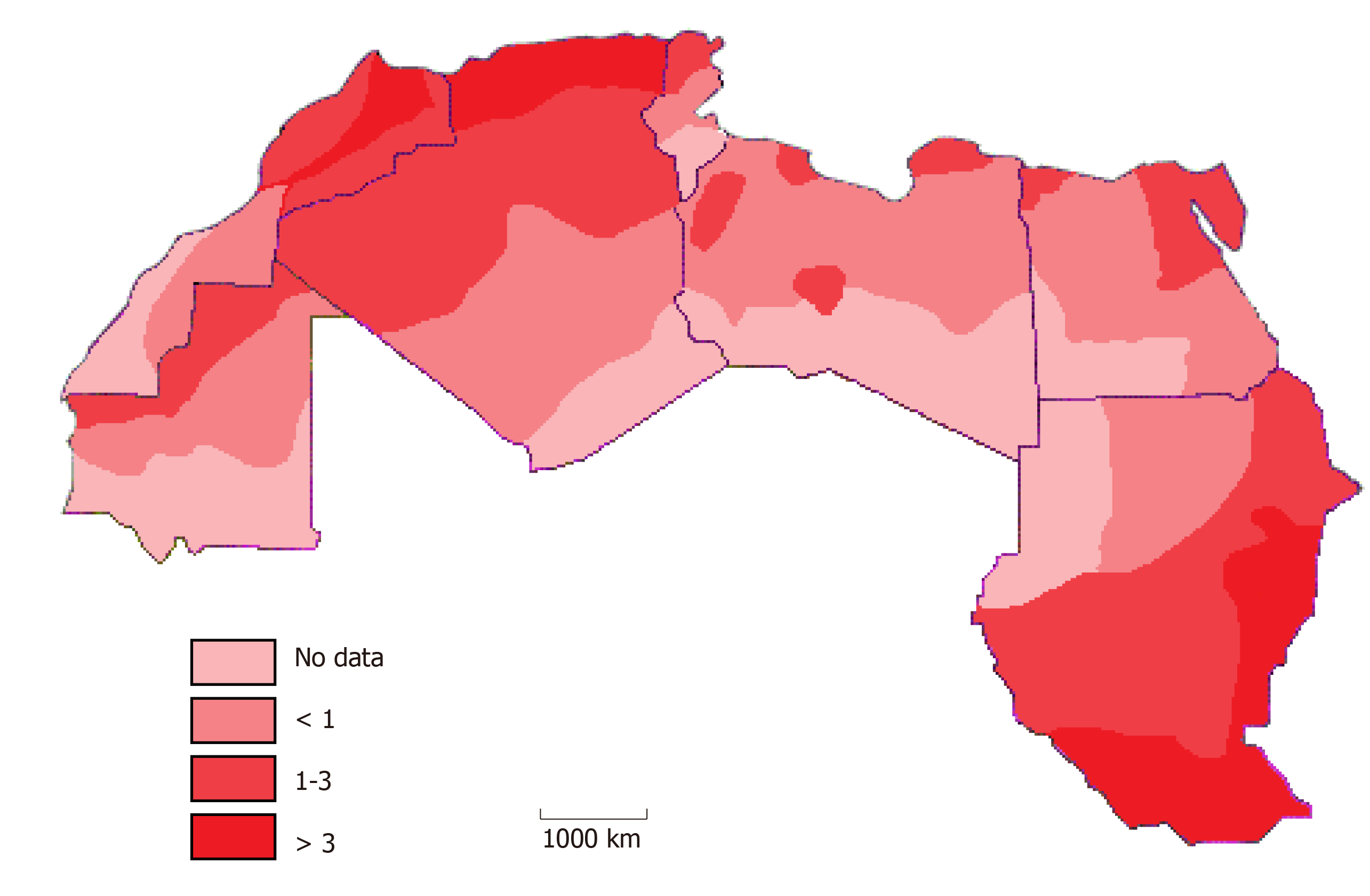
HIV/AIDS infections are reported to be high in the capital coastal cities in comparison to the other regions of North African countries. Figure 7 shows the spatial distribution of HIV-seropositive individuals living in North Africa between 2008 and 2017[47-50]. There is a clear change in the regional patterns of HIV with significant spatial heterogeneity within each country. The substantial variability ranged from 0.01% to 5%, with no clear regional patterning of the space-time interaction. A higher level was reported in Sudan, Morocco and Algeria and to a lower extent Mauritania and Tunisia. However, patterning persisted in Libya and Egypt. In Sudan, the HIV patterns reached the highest in southern regions. It is estimated that HIV prevalence in the 10 states that now make up South Sudan was 3.0%, ranging from zero in Northern Bahr el Ghazal to 7.2% in Western Equatoria State, followed by Kassala State in Eastern Sudan (0.2%-3%), Khartoum (0%-5.7%), Gadarif State (0.1%-0.4%), and Kosti (0.1%-0.7%). In Morocco, the highest was reported in Agadir Souss-Massa-Drâa in the south, Fes and Rabat in the central region, followed by Nador and Tanger in the north, and Marrakech in the southwest. In Egypt, the prevalence was high in east Cairo, followed by Alexandria and South Sinai. In Libya, it was high in both the eastern and western coastal regions, followed by the central south part of the Sebha area. In Tunisia, the prevalence was highest in the capital, Bizerte and Hammamet, followed by the other coastal cities of Sousse and Sfax, but it was lower in the middle and southern regions of the country. In Algeria, the northeastern region reported the highest HIV prevalence, particularly in the area neighboring Tunisia, followed by Oran and Sidi Bel Abbes. The prevalence was low in the central and southern regions of Algeria. In Mauritania, HIV prevalence reached its highest (1%-2%) in the Nouakchott area, followed by the central region. However, no data are available on most of the eastern and western Sahara regions.
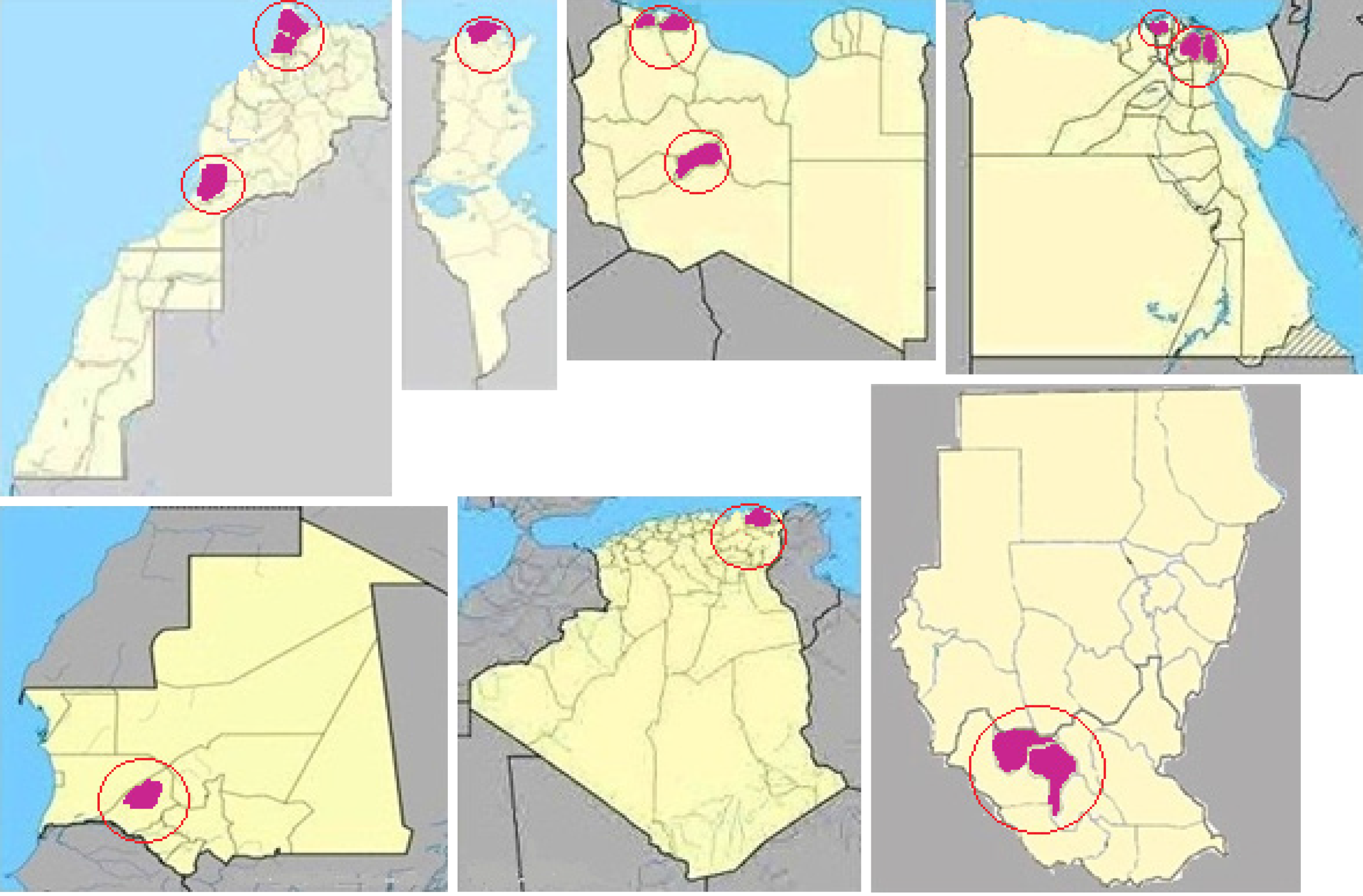
North African countries showed spatial variation in HIV/AIDS cases during the 10-year study period. Figure 8 shows the HIV spatial clustering in the region, with dark red areas indicating statistically significant hotspots of higher than expected rates. The results of the spatiotemporal analysis suggest a special characteristic in the temporal and spatial distribution of HIV/AIDS incidents. A total of 11 statistically significant high-risk areas at different times were reported in several regions and provinces of the seven countries. In Morocco, which experienced two clusters, the largest cluster area was located in Agadir Souss-Massa-Drâa in the south in 2011 and Fes and Rabat in the central region, followed by Nador and Tanger. The second was reported in the north in 2012 and Marrakech in the southwest in 2014. The main clusters were reported among IDUs followed by MSM and female sex workers (FSWs). For IDU networks (6%; 95%CI 3-10), most transmission appears to have been in northern Morocco. The epidemic in the commercial heterosexual networks and MSM appears to have been most intense in the south of Morocco, especially in Souss-Massa-Drâa. The largest contribution to HIV incidence was among clients of FSWs (25%; 95%CI 14-37), followed by MSM (22%; 95%CI 12-35), stable heterosexual couples (corresponding to HIV serodiscordant couples; 22%; 95%CI 12-34), and FSWs (11%; 95%CI 6-18).
In Sudan, the biggest cluster was reported in Southern Sudan in the Western Equatoria State in 2012. Among 420 antenatal clinic attendees, HIV seropositivity was 10.7% (95%CI 8.0-14.2), and among 388 voluntary counseling and testing attendees, HIV seropositivity was 13.1% (95%CI 10.0-17.0), indicating high HIV prevalence in Western Equatoria State. In Libya, three clusters were reported during 2008-2017. The first cluster, which occurred during 2008-2012, consisted of 203 cases in Tripoli in the western region. The second one was reported in Musrata (the largest city in the central region) and consisted of 406 HIV cases detected between 2013 and 2017. The third cluster was detected in Sebha (the largest city in the south) between 2013 and 2017 and consisted of 317 HIV cases.
In 2011, Egypt experienced a concentrated epidemic among MSM and IDUs in the east Cairo sector, Alexandria, and southern Sinai. The HIV prevalence ranged from 5.4% to 6.9%. It was 6.9% among MSM and 6.7%-7.7% among IDUs. Minor clusters were reported in Algeria, Tunisia and Mauritania. In a study carried out in 2013 in two hospitals in northeastern Algeria, HIV was reported to be high among pregnant women, in whom the prevalence rate reached up to 5.3/1000. In Tunisia, a small cluster was reported in 2011 in the north of the country, particularly within the capital Tunis and mainly associated with FSWs and MSM. In Mauritania, a minor cluster was reported among blood donors in December 2015 in the Hodh El Gharbi region located 800 km from Nouakchott (the capital) in the south-east of the country.
There are insufficient data on HIV prevalence in the North African region and no formal, national, population-based surveillance studies have been reported apart from those in Libya and Morocco[19,25]. Worryingly, health planners and strategists in this region are inadequately attentive to the ongoing HIV epidemic situation. It seems that cultural understanding and social perception are still not fully aware of the serious consequences of the epidemic. Infected individuals, particularly women, often face denial of care, stigmatizing attitudes, discrimination, and breaches of confidentiality[51].
In this review, we comprehensively analyzed the actual situation of HIV prevalence in North African countries. HIV prevalence has increased significantly in the region over the last ten years. The overall prevalence increased from 0.2%-1.4% in 2008 to 4.4% in 2017. The highest prevalence was reported in Sudan, Algeria, Mauritania and Egypt, followed by Morocco, Tunisia and Libya. However, there are concerns over the reliability of the data in certain countries. For instance, the prevalence in Egypt, which has the largest population in the region (over 100 million), Algeria and Tunisia was much lower than in Sudan and Morocco, and even in Mauritania (which has a population of only four million). However, the HIV epidemic seems to be alarming particularly in Algeria, Sudan, Mauritania and Morocco.
In the region, there is inadequate research on marginalized groups such as MSM and sex workers, particularly in Algeria, Egypt and Mauritania. The data on IDUs are even sparser, particularly in Libya, Mauritania and Algeria. However, emerging data from Morocco and Sudan indicate that HIV prevalence is significantly higher in these groups than in the general population. Hence, further studies at the national and regional levels are needed[52].
Different demographic factors have been reported to influence the prevalence of HIV among the North African populations. The highest prevalence was reported among younger individuals. Over 45% of HIV cases were aged 21-30 years, followed by the middle-aged group (31-40 years) at 30%. The infected individuals were predominantly unmarried individuals who were illiterate or had a low level of education. However, with the exception of Sudan, no country reported HIV infection among children younger than five years despite evidence of mother-to-child transmission. Furthermore, a steady increase among the older age group has been reported, particularly in Libya. The epidemic is no longer confined to males in the region. A considerable number of females are also affected. In Morocco, Sudan and Tunisia, the prevalence of HIV among women seems to be exceeding that of men. Studies in sub-Saharan Africa have shown that girls and young women have up to eight-fold higher rates of HIV infection compared to their male peers[53-55]. However, there remains a gap in young women employing HIV prevention technologies.
The patterns of HIV transmission have evolved and the epidemic concentration varies from one country to another in North Africa. Cases among blood donors have been eliminated in Morocco, Tunisia and Libya and decreased in Egypt, but they are still reported in Mauritania, Sudan and Algeria.
The prevalence was higher in healthcare settings in most of the countries. However, the epidemic is currently concentrated among IDUs and FSWs, particularly in Morocco, Egypt, Tunisia and Algeria, but to a lesser extent in Libya, Mauritania and Sudan, where incarceration was the main factor. This demographic variability is similar to that in other nations, such as in sub-Saharan Africa[56,57]. These findings indicate that drug injection might be the major risk factor for HIV transmission in the region. This is probably due to shared drug paraphernalia[58]. Hence, understanding the HIV dynamics in North Africa is an important step towards facing the challenges of this epidemic.
HIV sequences from cases identified in North African countries have been published sporadically, providing a mosaic overview of the molecular epidemiology of HIV in the region. The epidemics in Algeria, Morocco, Mauritania and Tunisia have been dominated by subtype B and CRF02_AG, as well as CRF06-cpx in Algeria. In Libya, 75% of the reported cases were subtype B and 18% were CRF 20 AG. On the other hand, in Sudan, 50% of the cases were subtype D and 30% were subtype C, while in Egypt subtype B represented 95% of cases. Given the wide distribution of subtypes in the region, HIV-1 was probably introduced multiple times in these countries. The broad array of subtypes/CRFs indicates that the epidemic is more complicated than in many other regions of the world, where one subtype usually predominates. Studies in North America and Southern Africa have shown that the main circulating subtypes represent more than 95% of all HIV-1 infections in these regions[59,60]. Furthermore, there is a lack of studies on phylodynamics in tracing the origins and transmission routes of HIV infection in the region. This is a particularly important aspect of the HIV outbreak among Libyan children associated with the Bulgarian Nurses saga[61].
Our study indicates that the spread of HIV varies greatly within North African countries and shows much geographical variation in the prevalence of HIV infection. However, there seems to be considerable inter- and intra-country variability ranging from 0% in some parts of Libya and Tunisia to over 3% in the coastal areas of Morocco, Algeria and Southern Sudan. These observed spatial variations highlight the clustering of HIV across North African countries, indicating that a generalized epidemic may be evident in this region[62]. Certain pockets within the region harbor the threat of a generalized epidemic, as the virus spreads from the most-at-risk to the general population. Over 11 clusters have been reported. The driving factors of the dynamics of these clusters were mainly FSWs and IDUs, particularly in Morocco, Tunisia and Egypt. The rates of incidence of reported cases in Algeria, Mauritania and Sudan were associated with pregnant women and blood donation antenatal clinics. These findings should be considered in future research and clinical practice[63]. Public health policymakers should give careful consideration to the substantial variation in the spread of HIV through populations and communities within each country when formulating HIV control measures. This is especially important if one considers that there is no single global HIV epidemic. The Joint United Nations Program on HIV/ AIDS has adopted the mantra ‘‘Know your epidemic; know your response”[64].
The findings of this review shed light on key features of the epidemic in North Africa, but several gaps remain. There is a major gap in the data on HIV-related mortality in the region, particularly among HIV-infected children, and no studies have been carried out on mother-to-child transmission. Hence, emphasis needs to be placed on diagnosing and treating HIV infection in pregnant women to prevent perinatal transmission, early screening for HIV infection in infants born to HIV-infected mothers, and treating those who are infected before they develop more advanced disease as the world moves toward the goal of eliminating mother-to-child transmission of HIV[65]. Furthermore, most of these countries are plagued by internal conflicts and have persistent difficulty in addressing healthcare needs. Thus, immigrants, refugees, internally displaced persons and insurgent groups may play a role in the spread of HIV in North Africa. Further studies are needed in North Africa as data from sub-Saharan African countries suggest that reconstruction periods after conflict might be a more vulnerable time for HIV transmission than during conflict[66-68].
This meta-analysis has some limitations. One of the challenges was the fact that the studies adopted different methods in categorizing population groups and used different durations. Quality assessment of the studies included in this review showed that most studies obtained a medium-quality rating and few of them obtained a high score, which indicates that more rigorous research is needed. Moreover, we did not analyze some contributing factors, namely, the level of education and personal income of the HIV infected individuals. Furthermore, FSWs and MSM cannot be followed or even mentioned in some countries, and particularly in Libya and Mauritania, as these acts are considered crimes that may lead to the death penalty[69,70].
HIV is at an alarming status in North African countries, which face serious epidemics. Sudan, Egypt, Morocco and Algeria have concentrated epidemics, but HIV seems less concentrated in Mauritania, Libya and Tunisia. Furthermore, HIV seems to be moving towards concentrated clusters and measures have been challenged and hampered by massive population displacement associated with chaotic economic and sociopolitical situations. The endemicity of HIV in these countries is complicated by a lack of registry data and follow-up programs, particularly in the Saharan and countryside areas. The Joint United Nations Programme on HIV/AIDS (UNAIDS) definition of a generalized epidemic is an HIV prevalence of more than 1% in the general adult population (15-59 years) and more than 5% in vulnerable adult groups[71]. Hence, generalized epidemics persist in Sudan in particular and even in Algeria, Morocco and Egypt. There is an urgent need to establish a standardized epidemiological platform at both the national and regional levels that can reliably quantify individual differences in risk and understand the chain of HIV transmission and geographic clusters of HIV. Few studies have examined how geographic disparities may impact trends in HIV seropositive cases in North African countries. Identifying such social and geographic factors is important for better screening and treatment, and thus for reducing the burden among high-risk populations[19,72,73].
Acquired immunodeficiency syndrome (AIDS) is a serious health problem in Africa but few studies have highlighted the epidemiological and spatiotemporal patterns of this infection, particularly in the North African region. Evidence is increasing regarding the magnitude of this problem and its social and economic impact in these countries. Analyzing the epidemiological situation of human immunodeficiency virus (HIV)/AIDS infection in this region has become one of the necessities for better understanding the current situation and for future planning.
There has been a dearth of information on the epidemiological status of HIV/AIDS in North African countries. This raises a serious concern regarding the impact of this infection in the region and how it could be controlled.
The aim of this comprehensive review was to analyze and characterize the epidemiological and geographic variation and clustering of HIV/AIDS in North Africa and outline the policies needed to combat this problem at both the national and regional levels.
This is a comprehensive review of published data on different aspects of HIV/AIDS in North African countries in the last ten years (2008-2017). Every reported study was analyzed and all epidemiological parameters and risk factors associated with the spread of HIV in the region were determined. This will alert healthcare professionals and researchers to act immediately to implement proper policies to overcome this increasing problem.
The results indicate an increasing spread of HIV/AIDS in North African countries, with certain variations in prevalence, clustering and HIV subtypes between the countries and within regions of the same county. Higher prevalence rates have been reported among vulnerable populations.
Based on the evidence of the collected data, North African countries are facing an intensifying problem of HIV infection. There are not enough reliable data to determine the magnitude of this problem and no clear policy to combat the infection in the region.
We strongly suggest that specific and well-designed epidemiological studies should be conducted at national and regional levels to quantify the magnitude of the problem. Furthermore, clearly defined policies should be implemented to overcome this increasing problem.
We are deeply grateful to the Libyan Study Group of Hepatitis and HIV and the Department of Medical Microbiology and Immunology, Faculty of Medicine, University of Tripoli.
| 1. | Piot P, Quinn TC. Response to the AIDS pandemic--a global health model. N Engl J Med. 2013;368:2210-2218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 104] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 2. | German Advisory Committee Blood (Arbeitskreis Blut); Subgroup ‘Assessment of Pathogens Transmissible by Blood’. Human Immunodeficiency Virus (HIV). Transfus Med Hemother. 2016;43:203-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 210] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 3. | Gökengin D, Doroudi F, Tohme J, Collins B, Madani N. HIV/AIDS: trends in the Middle East and North Africa region. Int J Infect Dis. 2016;44:66-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 110] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 4. | Fortson JG. Mortality risk and human capital investment: The Impact of HIV/AIDS in Sub-Saharan Africa. Rev Econ Stat. 2011;93:1-5. |
| 5. | Kharsany AB, Karim QA. HIV Infection and AIDS in Sub-Saharan Africa: Current Status, Challenges and Opportunities. Open AIDS J. 2016;10:34-48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 568] [Cited by in RCA: 606] [Article Influence: 60.6] [Reference Citation Analysis (0)] |
| 6. | Poteat T, Ackerman B, Diouf D, Ceesay N, Mothopeng T, Odette KZ, Kouanda S, Ouedraogo HG, Simplice A, Kouame A, Mnisi Z, Trapence G, van der Merwe LLA, Jumbe V, Baral S. HIV prevalence and behavioral and psychosocial factors among transgender women and cisgender men who have sex with men in 8 African countries: A cross-sectional analysis. PLoS Med. 2017;14:e1002422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 126] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 7. | Tengan FM, Abdala E, Nascimento M, Bernardo WM, Barone AA. Prevalence of hepatitis B in people living with HIV/AIDS in Latin America and the Caribbean: a systematic review and meta-analysis. BMC Infect Dis. 2017;17:587. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Esterhuysen P. Africa a to z: Continental and country profiles. Africa Institute of South Africa; 2013. |
| 9. | Daw MA, El-Bouzedi A, Dau AA. Libyan armed conflict 2011: mortality, injury, and population displacement. Afr J Emerg Med. 2015;5:101-107. |
| 10. | Daw MA, El-Bouzedi A, Dau AA. The assessment of efficiency and coordination within the Libyan health care system during the armed conflict-2011. Clin Epidemiol Glob Health. 2016;4:120-127. |
| 11. | Daw MA, El-Bouzedi A, Ahmed MO, Dau AA, Agnan MM, Drah AM, Deake AO; In association with Libyan Study Group of Hepatitis & HIV. Prevalence of human immune deficiency virus in immigrants crossing to Europe from North and Sub-Saharan Africa. Travel Med Infect Dis. 2016;14:637-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Karamouzian M, Madani N, Doroudi F, Haghdoost AA. Improving the Quality and Quantity of HIV Data in the Middle East and North Africa: Key Challenges and Ways Forward. Int J Health Policy Manag. 2017;6:65-69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 13. | Granich R, Gupta S, Hersh B, Williams B, Montaner J, Young B, Zuniga JM. Trends in AIDS Deaths, New Infections and ART Coverage in the Top 30 Countries with the Highest AIDS Mortality Burden; 1990-2013. PLoS One. 2015;10:e0131353. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 113] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 14. | Rutledge SE, Whyte J, Abell N, Brown KM, Cesnales NI. Measuring stigma among health care and social service providers: The HIV/AIDS Provider Stigma Inventory. AIDS Patient Care STDS. 2011;25:673-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Setayesh H, Roudi-Fahimi F, El Feki S, Ashford LS. HIV and AIDS in the Middle East and North Africa. Washington, DC: Population Reference Bureau. 2014. |
| 16. | Panic N, Leoncini E, de Belvis G, Ricciardi W, Boccia S. Evaluation of the endorsement of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement on the quality of published systematic review and meta-analyses. PLoS One. 2013;8:e83138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 541] [Cited by in RCA: 618] [Article Influence: 47.5] [Reference Citation Analysis (0)] |
| 17. | Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7463] [Cited by in RCA: 8612] [Article Influence: 782.9] [Reference Citation Analysis (0)] |
| 18. | Daw MA, Daw AM, Sifennasr NEM, Draha AM, Ahmed MO, Mokhtar ES, El-Bouzedi A, Daw IM. The Epidemiology of Hepatitis D Virus in North Africa: A Systematic Review and Meta-Analysis. ScientificWorldJournal. 2018;2018:9312650. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Daw MA, Daw AM, Sifennasr NEM, Draha AM, Daw AA, Ahmed MO, Mokhtar ES, El-Bouzedi AH, Daw IM, Adam SI, Warrag S; In association with Libyan Study Group of Hepatitis & HIV. Spatiotemporal analysis and epidemiological characterization of the human immunodeficiency virus (HIV) in Libya within a twenty five year period: 1993-2017. AIDS Res Ther. 2019;16:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Kouyoumjian SP, El Rhilani H, Latifi A, El Kettani A, Chemaitelly H, Alami K, Bennani A, Abu-Raddad LJ. Mapping of new HIV infections in Morocco and impact of select interventions. Int J Infect Dis. 2018;68:4-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Badawi MM, Atif MS, Mustafa YY. Systematic review and meta-analysis of HIV, HBV and HCV infection prevalence in Sudan. Virol J. 2018;15:148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 22. | Ouyahia A, Rais M, Gasmi A, Guenifi W, Mechakra S, Lacheheb A. HIV/AIDS epidemic features and trends in setif city (Algeria) from 1986 to 2009. Retrovirology. 2010;7:99. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Boushab BM, Mohamed Limame OCM, Fatim Zahra FM, Mamoudou S, Roseline Darnycka BM, Saliou SM. Estimation of seroprevalence of HIV, hepatitis B and C virus and syphilis among blood donors in the hospital of Aïoun, Mauritania. Pan Afr Med J. 2017;28:118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Kilani B, Ammari L, Marrakchi C, Letaief A, Chakroun M, Ben Jemaa M, Ben Aïssa HT, Kanoun F, Ben Chaabène T. Seroepidemiology of HCV-HIV coinfection in Tunisia. Tunis Med. 2007;85:121-123. [PubMed] |
| 25. | Kouyoumjian SP, Mumtaz GR, Hilmi N, Zidouh A, El Rhilani H, Alami K, Bennani A, Gouws E, Ghys PD, Abu-Raddad LJ. The epidemiology of HIV infection in Morocco: systematic review and data synthesis. Int J STD AIDS. 2013;24:507-516. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | Soliman HH, Almotgly MM. Psychosocial profile of people with AIDS and their caregivers in Egypt. Psychol Rep. 2011;108:883-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Daw MA, El-Bouzedi A, Ahmed MO, Dau AA; In association with the Libyan Study Group of Hepatitis & HIV. Molecular and epidemiological characterization of HIV-1 subtypes among Libyan patients. BMC Res Notes. 2017;10:170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Mohamed BA, Mahfouz MS. Factors associated with HIV/AIDS in Sudan. Biomed Res Int. 2013;2013:971203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Fall-Malick FZ, Bara AO, Lam M, Mint Beibacar M, Ba K, Ba H, Ould Ghady I, Ould Horma A, Toure-Kane NC, Mboup S, Lo B. [HIV sentinel surveillance of pregnant women in Mauritania from 2001 to 2007]. Bull Soc Pathol Exot. 2010;103:243-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 30. | Aidaoui M, Bouzbid S, Laouar M. [Seroprevalence of HIV infection in pregnant women in the Annaba region (Algeria)]. Rev Epidemiol Sante Publique. 2008;56:261-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Daw MA, Shabash A, El-Bouzedi A, Dau AA; Association with the Libyan Study Group of Hepatitis & HIV. Seroprevalence of HBV, HCV & HIV co-infection and risk factors analysis in Tripoli-Libya. PLoS One. 2014;9:e98793. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 32. | Henry E, Bernier A, Lazar F, Matamba G, Loukid M, Bonifaz C, Diop S, Otis J, Préau M; Partages study group. "Was it a mistake to tell others that you are infected with HIV? AIDS Behav. 2015;19:311-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 33. | Tebourski F, Ben Alaya D. Knowledge and attitudes of high school students regarding HIV/AIDS in Tunisia: does more knowledge lead to more positive attitudes? J Adolesc Health. 2004;34:161-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 34. | Kabbash IA, Abdul-Rahman I, Shehata YA, Omar AA. HIV infection and related risk behaviours among female sex workers in greater Cairo, Egypt. East Mediterr Health J. 2012;18:920-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 35. | Dean J, Wollin J, Stewart D, Debattista J, Mitchell M. Hidden yet visible: methodological challenges researching sexual health in Sudanese refugee communities. Cult Health Sex. 2012;14:911-924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 36. | Bozicevic I, Guezzar F, Stulhofer A, Bennani A, Handanagic S, Barbaric J, El Rhilani H, Alami K, Khattabi H, Riedner G, Maaroufi A. HIV prevalence and related risk behaviours in female seasonal farm workers in Souss Massa Draa, Morocco: results from a cross-sectional survey using cluster-based sampling. Sex Transm Infect. 2018;94:515-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 37. | Mohamed HI, Saad ZM, Abd-Elreheem EM, Abd-ElGhany WM, Mohamed MS, Abd Elnaeem EA, Seedhom AE. Hepatitis C, hepatitis B and HIV infection among Egyptian prisoners: seroprevalence, risk factors and related chronic liver diseases. J Infect Public Health. 2013;6:186-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 38. | Kabbash IA, Abo Ali EA, Elgendy MM, Abdrabo MM, Salem HM, Gouda MR, Elbasiony YS, Elboshy N, Hamed M. HIV/AIDS-related stigma and discrimination among health care workers at Tanta University Hospitals, Egypt. Environ Sci Pollut Res Int. 2018;25:30755-30762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 39. | Ba K, Keita M, Fall-Malick FZ, Mint Beibakar M, Diallo M, Lo BB. [Serological and Behavioral Survey on HIV/AIDS among prisoners in Nouakchott (Mauritania)]. Bull Soc Pathol Exot. 2015;108:208-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 40. | Courtney LP, Goco N, Woja J, Farris T, Cummiskey C, Smith E, Makuach L, Chun HM. HIV prevalence and behavioral risk factors in the Sudan People's Liberation Army: Data from South Sudan. PLoS One. 2017;12:e0187689. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 41. | Abdellaziz A, Papuchon J, Khaled S, Ouerdane D, Fleury H, Recordon-Pinson P. Predominance of CRF06_cpx and Transmitted HIV Resistance in Algeria: Update 2013-2014. AIDS Res Hum Retroviruses. 2016;32:370-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (1)] |
| 42. | Fall-Malick FZ, Tchiakpé E, Ould Soufiane S, Diop-Ndiaye H, Mouhamedoune Baye A, Ould Horma Babana A, Touré Kane C, Lo B, Mboup S. Drug resistance mutations and genetic diversity in adults treated for HIV type 1 infection in Mauritania. J Med Virol. 2014;86:404-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 43. | El Moussi A, Thomson MM, Delgado E, Cuevas MT, Nasr M, Abid S, Ben Hadj Kacem MA, Benaissa Tiouiri H, Letaief A, Chakroun M, Ben Jemaa M, Hamdouni H, Tej Dellagi R, Kheireddine K, Boutiba I, Pérez-Álvarez L, Slim A. Genetic Diversity of HIV-1 in Tunisia. AIDS Res Hum Retroviruses. 2017;33:77-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 44. | Lo Presti A, Farcomeni S, Fontanelli Sulekova L, Grieco S, Sernicola L, Baesso M, Maggiorella MT, Angeletti S, Foley B, Ciccozzi M, Taliani G, Borsetti A. Characterization of HIV-1 Subtypes Among South Sudanese Patients. AIDS Res Hum Retroviruses. 2019;35:968-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 45. | Boutros S, Skordis J. HIV/AIDS surveillance in Egypt: current status and future challenges. East Mediterr Health J. 2010;16:251-258. [PubMed] |
| 46. | Bouzeghoub S, Jauvin V, Recordon-Pinson P, Garrigue I, Amrane A, Belabbes el-H, Fleury HJ. High diversity of HIV type 1 in Algeria. AIDS Res Hum Retroviruses. 2006;22:367-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 47. | Centers for Disease Control and Prevention (CDC). . Notes from the field: Investigation of high HIV prevalence in Western Equatoria State--South Sudan, 2012. MMWR Morb Mortal Wkly Rep. 2013;62:453-454. [PubMed] |
| 48. | Kebe M, Fall-Malick FZ, Elghady OI, Ebnou OH, Bara OA, Lam M, Beibacar MO, Diallo MY, Keita M, Sy I, Bellaty AJ, Ly C, Lô BB. [HIV seroprevalence among STD patients in Nouakchott and Nouadhibou (Mauritania)]. Bull Soc Pathol Exot. 2011;104:374-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 49. | Himmich H, Ouarsas L, Hajouji FZ, Lions C, Roux P, Carrieri P. Scaling up combined community-based HIV prevention interventions targeting truck drivers in Morocco: effectiveness on HIV testing and counseling. BMC Infect Dis. 2015;15:208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 50. | Soliman C, Rahman IA, Shawky S, Bahaa T, Elkamhawi S, El Sattar AA, Oraby D, Khaled D, Feyisetan B, Salah E, El Taher Z, El Sayed N. HIV prevalence and risk behaviors of male injection drug users in Cairo, Egypt. AIDS. 2010;24 Suppl 2:S33-S38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 51. | Abdool Karim SS. Stigma impedes AIDS prevention. Nature. 2011;474:29-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 52. | Baral S, Beyrer C, Muessig K, Poteat T, Wirtz AL, Decker MR, Sherman SG, Kerrigan D. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:538-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 967] [Cited by in RCA: 910] [Article Influence: 65.0] [Reference Citation Analysis (0)] |
| 53. | Leclerc PM, Garenne M. Commercial sex and HIV transmission in mature epidemics: a study of five African countries. Int J STD AIDS. 2008;19:660-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 54. | Peltzer K. Early sexual debut and associated factors among in-school adolescents in eight African countries. Acta Paediatr. 2010;99:1242-1247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 80] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 55. | Chen L, Jha P, Stirling B, Sgaier SK, Daid T, Kaul R, Nagelkerke N; International Studies of HIV/AIDS (ISHA) Investigators. Sexual risk factors for HIV infection in early and advanced HIV epidemics in sub-Saharan Africa: systematic overview of 68 epidemiological studies. PLoS One. 2007;2:e1001. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 149] [Cited by in RCA: 157] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 56. | Nnko S, Kuringe E, Nyato D, Drake M, Casalini C, Shao A, Komba A, Baral S, Wambura M, Changalucha J. Determinants of access to HIV testing and counselling services among female sex workers in sub-Saharan Africa: a systematic review. BMC Public Health. 2019;19:15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 62] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 57. | Seidu AA, Oduro JK, Ahinkorah BO, Budu E, Appiah F, Baatiema L, Ameyaw EK, Sambah F. Women's healthcare decision-making capacity and HIV testing in sub-Saharan Africa: a multi-country analysis of demographic and health surveys. BMC Public Health. 2020;20:1592. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 58. | Clatts MC, Heimer R, Abdala N, Goldsamt LA, Sotheran JL, Anderson KT, Gallo TM, Hoffer LD, Luciano PA, Kyriakides T. HIV-1 transmission in injection paraphernalia: heating drug solutions may inactivate HIV-1. J Acquir Immune Defic Syndr. 1999;22:194-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 45] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 59. | Sikavi C, Chen PH, Lee AD, Saab EG, Choi G, Saab S. Hepatitis C and human immunodeficiency virus coinfection in the era of direct-acting antiviral agents: No longer a difficult-to-treat population. Hepatology. 2018;67:847-857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 60. | Rolland M, Modjarrad K. Multiple co-circulating HIV-1 subtypes in the Middle East and North Africa. AIDS. 2015;29:1417-1419. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 61. | Hemelaar J, Gouws E, Ghys PD, Osmanov S; WHO-UNAIDS Network for HIV Isolation and Characterisation. Global trends in molecular epidemiology of HIV-1 during 2000-2007. AIDS. 2011;25:679-689. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 561] [Cited by in RCA: 553] [Article Influence: 36.9] [Reference Citation Analysis (0)] |
| 62. | Boyda DC, Holzman SB, Berman A, Grabowski MK, Chang LW. Geographic Information Systems, spatial analysis, and HIV in Africa: A scoping review. PLoS One. 2019;14:e0216388. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 63. | Manda S, Haushona N, Bergquist R. A Scoping Review of Spatial Analysis Approaches Using Health Survey Data in Sub-Saharan Africa. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 64. | Wilson D, Halperin DT. "Know your epidemic, know your response": a useful approach, if we get it right. Lancet. 2008;372:423-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 145] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 65. | Adetokunboh OO, Oluwasanu M. Eliminating mother-to-child transmission of the human immunodeficiency virus in sub-Saharan Africa: The journey so far and what remains to be done. J Infect Public Health. 2016;9:396-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 66. | Spiegel PB, Bennedsen AR, Claass J, Bruns L, Patterson N, Yiweza D, Schilperoord M. Prevalence of HIV infection in conflict-affected and displaced people in seven sub-Saharan African countries: a systematic review. Lancet. 2007;369:2187-2195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 127] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 67. | Spiegel PB. HIV/AIDS among conflict-affected and displaced populations: dispelling myths and taking action. Disasters. 2004;28:322-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 122] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 68. | Spiegel PB, Checchi F, Colombo S, Paik E. Health-care needs of people affected by conflict: future trends and changing frameworks. Lancet. 2010;375:341-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 193] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 69. | Siegfried N, Clarke M, Volmink J. Randomised controlled trials in Africa of HIV and AIDS: descriptive study and spatial distribution. BMJ. 2005;331:742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 70. | Egger M, Smith GD. Bias in location and selection of studies. BMJ. 1998;316:61-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 903] [Cited by in RCA: 933] [Article Influence: 33.3] [Reference Citation Analysis (0)] |
| 71. | UNAIDS. AIDS Epidemic Update. Geneva: WHO/UNAIDS. 2006. |
| 72. | Cuadros DF, Li J, Mukandavire Z, Musuka GN, Branscum AJ, Sartorius B, Mugurungi O, Tanser F. Towards UNAIDS Fast-Track goals: targeting priority geographic areas for HIV prevention and care in Zimbabwe. AIDS. 2019;33:305-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 73. | Nunn A, Yolken A, Cutler B, Trooskin S, Wilson P, Little S, Mayer K. Geography should not be destiny: focusing HIV/AIDS implementation research and programs on microepidemics in US neighborhoods. Am J Public Health. 2014;104:775-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Virology
Country/Territory of origin: Libya
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: McQuillan GM S-Editor: Gao CC L-Editor: Webster JR P-Editor: Xing YX