©The Author(s) 2022.
World J Virol. Nov 25, 2022; 11(6): 453-466
Published online Nov 25, 2022. doi: 10.5501/wjv.v11.i6.453
Published online Nov 25, 2022. doi: 10.5501/wjv.v11.i6.453
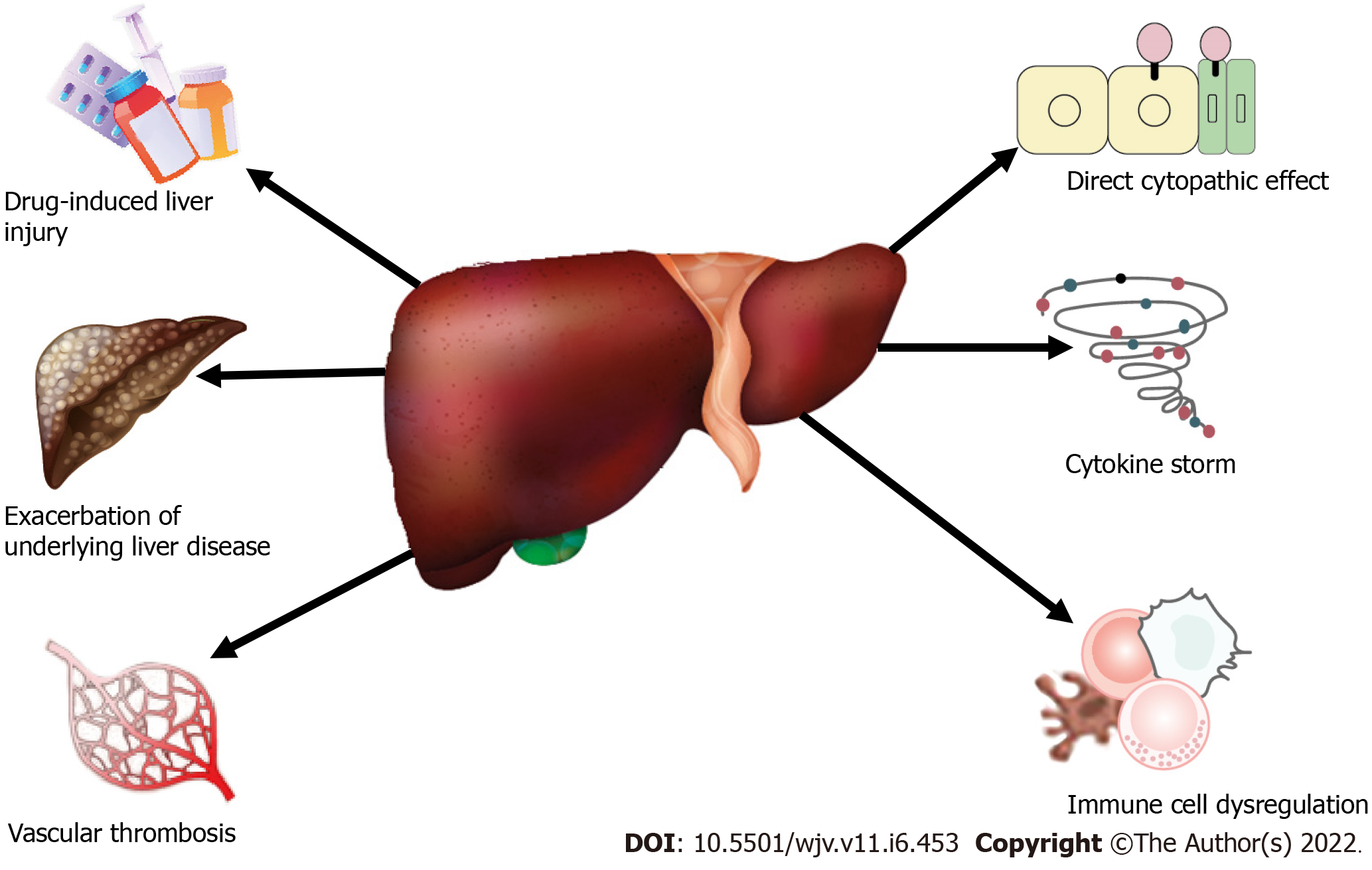
Figure 1 Schematic illustration of possible mechanisms of liver injury in coronavirus disease 2019.
Other mechanisms (not shown) may be involved.
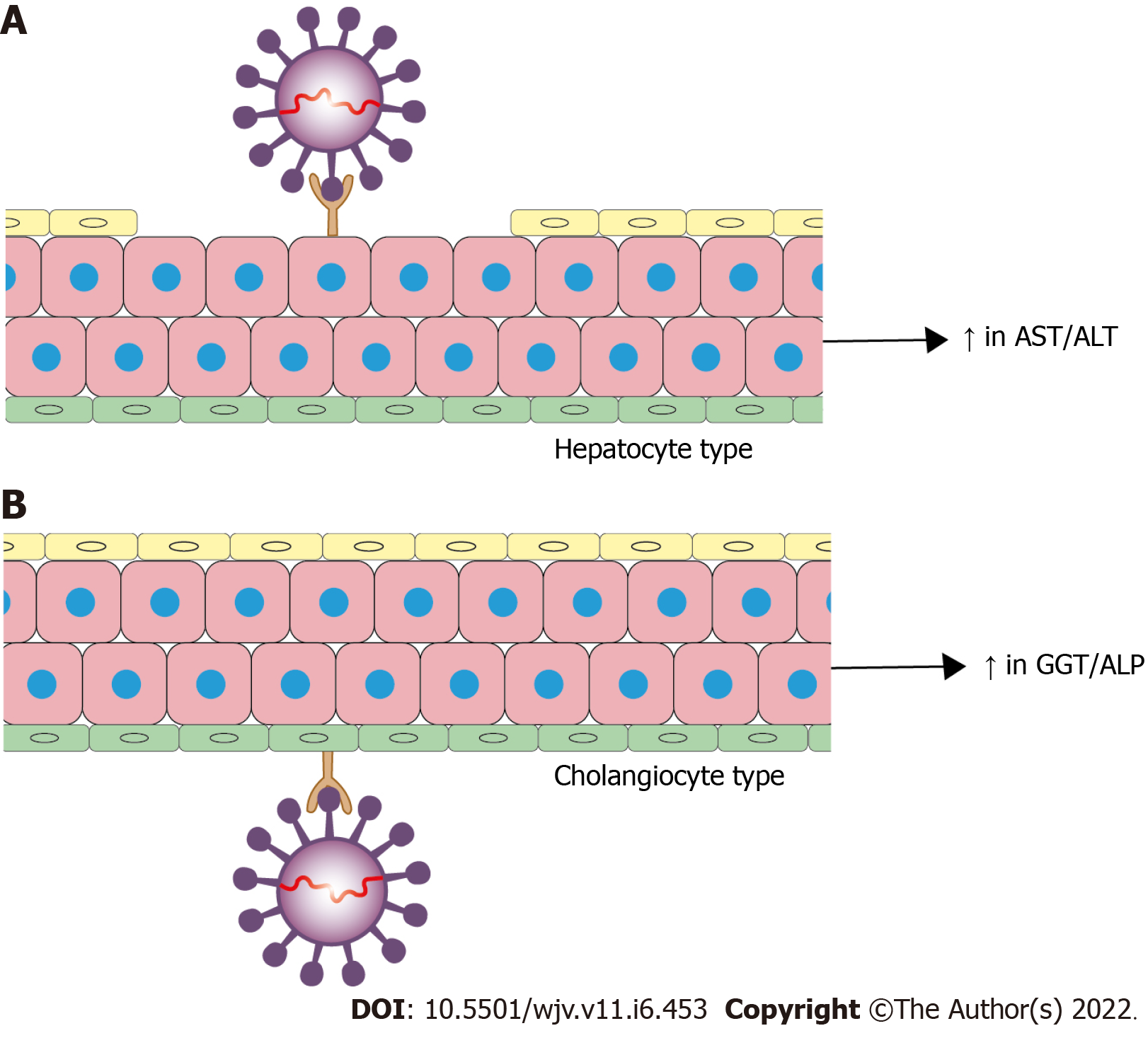
Figure 2 Two principal types of severe acute respiratory syndrome coronavirus 2 infection of the liver parenchyma.
A: Direct severe acute respiratory syndrome coronavirus 2 infection targeted to hepatocytes is designated as hepatocellular type; B: Direct viral entry into biliary epithelial cells is known as the cholangiocyte type. AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; GGT: γ-Glutamyltransferase; ALP: Alkaline phosphatase.
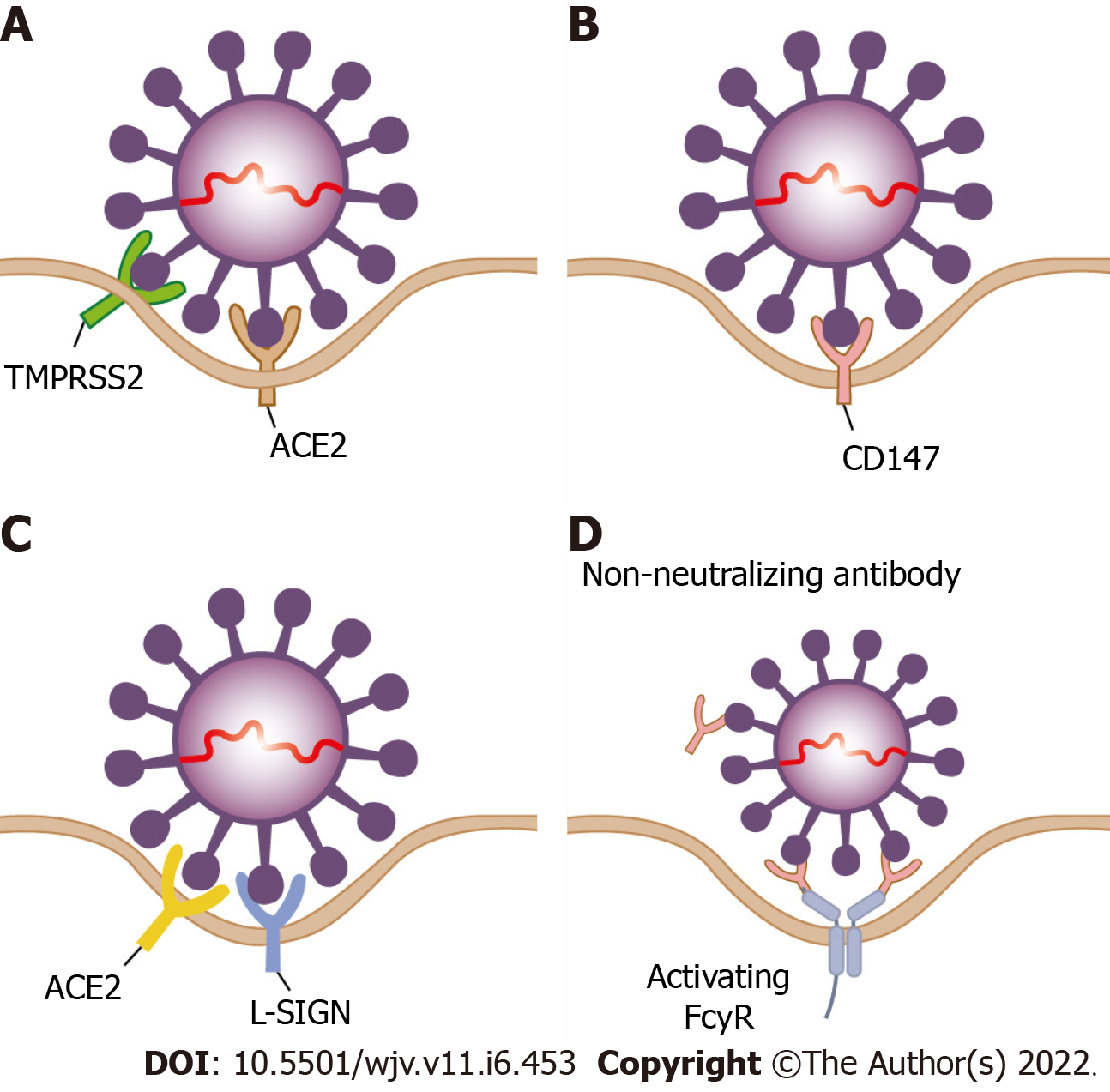
Figure 3 Possible pathways of virus entry in hepatocytes.
A: The angiotensin converting enzyme-2 in conjunction with transmembrane protease serine protease 2 is considered the predominant receptor for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) entry into cells; B: CD147 is another possible receptor for SARS-CoV-2 entry into hepatocytes. CD147 is highly expressed in tumor tissues, inflamed tissues and pathogen-infected cells including hepatocytes; C: L-SIGN (CD209L) may serve as a liver-specific cell receptor for SARS-CoV-2 infection of hepatocytes; D: Antibody-dependent enhancement may also facilitate SARS-CoV-2 infection of hepatocytes. During antibody-dependent enhancement of infection, suboptimal non-neutralizing antibodies cannot completely neutralize the virus; instead, they bind with the Fc receptors expressed on hepatocytes, leading to virus entry and infection. ACE2: Angiotensin-converting enzyme 2.
- Citation: Hanif FM, Majid Z, Ahmed S, Luck NH, Mubarak M. Hepatic manifestations of coronavirus disease 2019 infection: Clinical and laboratory perspective. World J Virol 2022; 11(6): 453-466
- URL: https://www.wjgnet.com/2220-3249/full/v11/i6/453.htm
- DOI: https://dx.doi.org/10.5501/wjv.v11.i6.453