Published online Dec 18, 2025. doi: 10.5500/wjt.v15.i4.111427
Revised: July 25, 2025
Accepted: September 2, 2025
Published online: December 18, 2025
Processing time: 143 Days and 9.5 Hours
Liver disease is a major cause of mortality in Mexico. Liver transplantation (LT) remains severely limited, and there are no reports on equity of access.
To analyze geographical disparities in LT access in Mexico.
LT waitlist registrations and LT rates in Mexico from 2014 to 2023 were assessed. LT listings per million persons (pmp) were calculated. Observed-to-expected listings were calculated by controlling listings pmp and mortality rate per 10000. LT and waitlist mortality was calculated as 90-day rate, overall rate and rate per 100 person-years. We compared access to waitlist, transplantation and mortality between patients living in Mexican States with higher LT activity and those living in other States.
There were 2600 new waitlist registrations; 1572 registrations (60.4%) living in Mexico City and State, Jalisco and Nuevo Leon. There were 1755 LT; 92.5% of them performed in States with higher LT activity, and 1101 (62.7% vs 37.3%; P < 0.001) done in patients living in those States. Listings pmp in the Mexican States with high LT activity were 3.8, 1.5 vs 1.2, 0.6 (P < 0.001); observed-to-expected listings were 1.3, 0.4 vs 0.4, 0.2 (P < 0.001); LT pmp were 2.7, 0.9 vs 0.7, 0.5 (P < 0.001). After controlling for other variables, patients living in high LT activity States had a HR 1.14 (95%CI: 1.03-1.26; P = 0.009) to be a case of transplantation after listing.
Geographic disparities substantially affect LT access in Mexico. The population living near Transplant Centers has a 3.2-fold higher access to the waiting list and a 3.8-fold higher likelihood of LT. Current referral system, and resource allocation need urgent revision to remove the barriers associated with geographic disparity.
Core Tip: Geographic disparities substantially affect liver transplantation (LT) access in Mexico. The population living near Transplant Centers has a 3.2-fold higher access to the waiting list and a 3.8-fold higher likelihood of LT.
- Citation: Leal-Leyte P, Rodriguez-Payan N, Cote MP, Noriega-Salas L, Lugo-Baruqui A, Dageforde LA, Zamora-Valdés D. Geographical disparities for liver transplantation access in Mexico. World J Transplant 2025; 15(4): 111427
- URL: https://www.wjgnet.com/2220-3230/full/v15/i4/111427.htm
- DOI: https://dx.doi.org/10.5500/wjt.v15.i4.111427
Endstage liver disease is one of the main causes of mortality globally, liver transplantation (LT) currently presents the only curative therapeutic option[1]. In Latin America, Mexico has the highest death rate due to liver diseases[2], and one of the lowest LT rates in the region[3]. Other than having a high disease burden compared to other countries, distribution of liver disease burden is markedly uneven across regions.
The healthcare system of Mexico is divided into multiple independent subsystems with tertiary care level hospitals in the major Metropolitan Areas of the country. Patients in need of LT from each subsystem are only referred to centers within their healthcare network, often requiring referral to different States where the center for their subsystem is located, despite having a closer LT center that might be from a different subsystem. The only additional option that patients may have to avoid additional traveling is to seek private hospital listing, which may imply out-of-pocket costs.
Healthcare disparities are defined as differences in access to or availability of medical facilities/services between population groups defined by age, ethnicity, economic resources, gender, geography, or other factors[4]. Geographical disparity in access to LT have been studied extensively in the United States[5], but there is no data on Latin American countries, even though disparity to access LT is considered among the major challenges in the region[6]. If the referral system in the country is fair, the distribution of patients dying from liver disease by Mexican State should be similar to the distribution of patients accessing the waitlist as well as the distribution of LT. The aim of this study is to analyze LT access in Mexico according to the State of Residence of the population in three layers: (1) Access to the LT waiting list; (2) Overall access to LT; and (3) Access to LT over time.
Census data from the Instituto Nacional de Estadística y Geografía from 2010 and 2020 were recorded by Mexican State and used to estimate the population in the years between[7]. Population data from 2021 to 2023 was estimated through exponential smoothing[8].
Mortality databases were obtained from the Dirección General de Información en Salud from 2014 to 2022[9]. These databases contain all deaths registered in Mexico, coded under the International Classification of Diseases version 10 (ICD-10) for the specific cause of death. Publicly available databases do not contain any identifiable data. We selected relevant variables from the 35 variables available in the registry, including: Sex, age, Mexican State of residence, and cause of death (ICD-10). We excluded deaths registered during the study period that occurred before 2014, as well as those with unknown date of death and/or state of residence. We used ICD-10 codes to identify liver diseases that could be treated with LT using the following codes: B15-B19, K70-K76, and Q44. We identified patients who died from acute liver failure as those with codes B150 (hepatitis A, hepatic coma), B160 (acute hepatitis B with delta agent, with hepatic coma), B162 (acute hepatitis B without delta agent, with hepatic coma), B179 (unspecified acute viral hepatitis), B190 (unspecified viral hepatitis with hepatic coma), K720 (acute and subacute hepatic failure), K762 (central hemorrhagic necrosis of the liver), and K763 (infarction of the liver)[10]. Hepatitis B was identified through codes B180 (chronic hepatitis B with delta agent), B181 (chronic hepatitis B without delta agent), and B191 (unspecified hepatitis B), whereas hepatitis C was identified using codes B182 (chronic hepatitis C) and B192 (unspecified hepatitis C). Alcoholic liver disease was identified through codes K70; other liver diseases were identified through codes K71-K76, except for those codes used for acute liver failure and liver abscess. Biliary atresia was identified using the code Q442.
We calculated mortality rate per 10000 persons in each Mexican State according to the data available from Instituto Nacional de Estadística y Geografía[7]. Mortality data from 2023 was estimated through exponential smoothing. Mor
We compared the number of listings per Mexican State with the number of deaths due to liver disease per Mexican State. We expected that, provided equal access, the number of listings per million persons (pmp) in each Mexican State would be proportional to the number of deaths per 10000 due to liver disease in the same region. We calculated “observed-to-expected (O:E) listings” as the ratio of listings pmp in each Mexican State per year, controlled by the liver disease mortality rate per 10000 in the same State. O:E listing ratio was therefore calculated using the following formula: (listings per year/million habitants) (liver-related deaths/10000 habitants). For example, a State with 10 Listings, 1000 Liver-related deaths and 1 million habitants will have a O:E listing rate of 1 [(10/1) (1000/100)].
The Centro Nacional de Trasplantes database was queried on July 12, 2024, for LT in Mexico from March 27, 2014, to December 31, 2023, and candidates registered on the waiting list by December 31, 2023[11]. We excluded multiorgan listings (n = 25). Information on patients removed from the list was obtained through the Instituto Nacional de Transparencia, Acceso a la Información y Protección de Datos Personales.
We analyzed the waiting time, LT-to-listings (T:L), waitlist mortality rate during the study period, and rates at 90 days. LT and deaths per 100 person-years were calculated as follows: Person-years in each category were calculated by dividing the waiting time in days by 365.25. Rate per 100 person-years was calculated as the number of events observed divided by the number of person-years, multiplied by 100[12]. Patients registered on the waitlist after the outcome occurred were not excluded for event recording purposes; however, the time between listing and outcome was recorded as a missing value (39 of 2600 cases, 1.5%).
We grouped residents of the States with highest rate of LT in the country as “LT States” including Mexico City and State (Metropolitan Area of the Valley of Mexico), Jalisco and Nuevo León, and compared them with residents of the rest of the country. Comparisons between the LT States and the rest of States were performed for all outcomes. Even when there is scarce LT activity in other states (Chihuahua, Sinaloa, Sonora, Yucatan, among others), we created this classification a priori with the rationale that 92 to 95% of the LT are performed in these four States.
Statistical analysis was performed using SPSS® Statistics software version 29 (IBM® 2023). Continuous variables are presented as median and interquartile range (IQR). Categorical variables were compared using χ2 test. Standardized values were calculated and outliers (Z values < -2.5 or > 2.5) were excluded from the final analysis. Median values between high and low LT activity States across each year of the study were compared using the Mann-Whitney’s U-test. A Cox regression model to be a case of transplantation was created controlling for sex, age group, ABO, and healthcare affiliation. Given the limited number of covariates available, all covariates available were entered into the model and multicollinearity assessment showed no variable with variance inflation factor > 10. Statistical significance was set at P < 0.05. This study used deidentified, public-access data, and no patient contact or intervention was performed. Our Institutional Review Board granted a waiver for review.
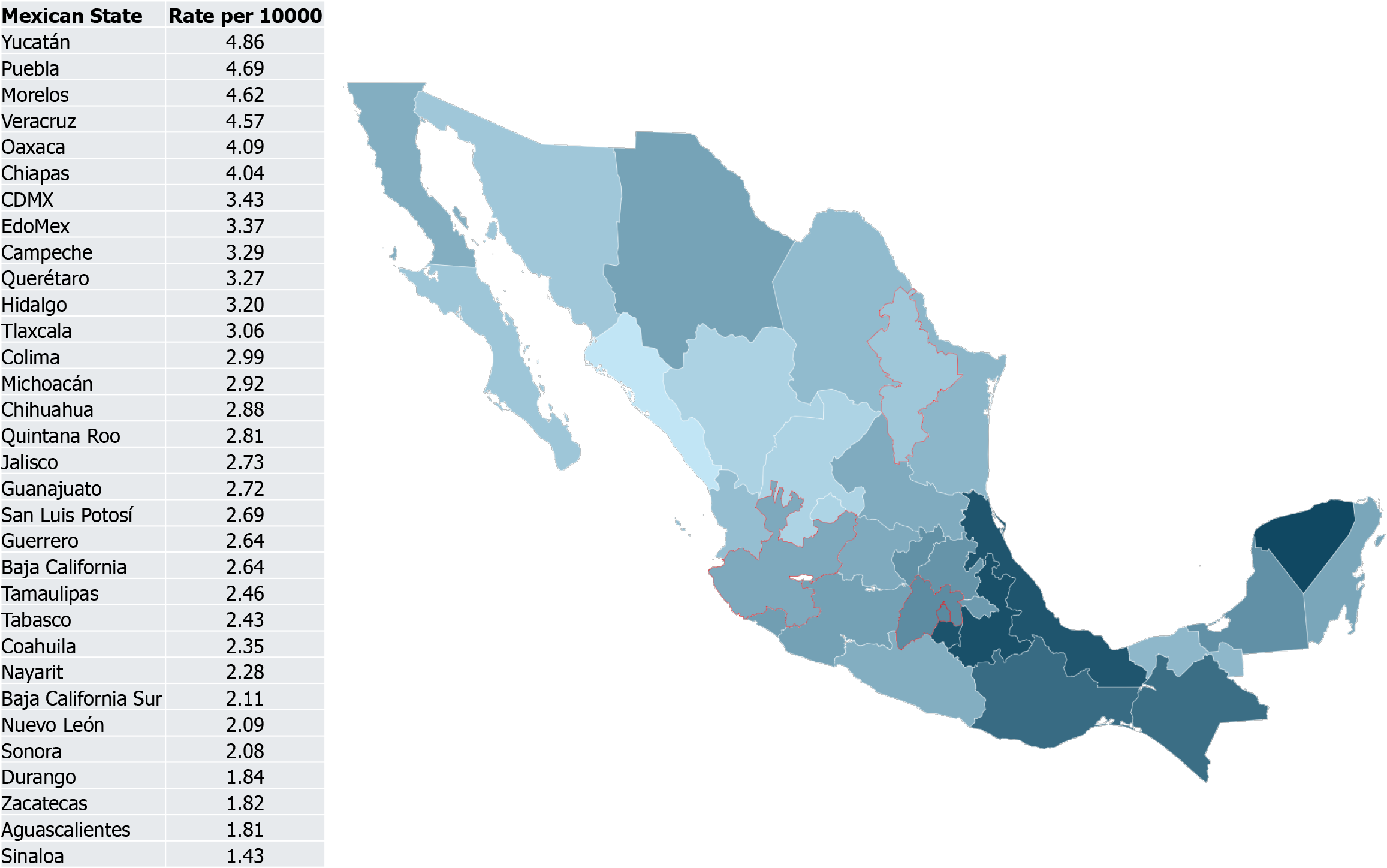
Between 2014-2023, there were 7031257 deaths in Mexico; 347880 (4.9%) were due to liver diseases, 72.4% were male and 99.2% were adults (≥ 18 years). Figure 1 shows the median liver disease mortality rate per 10000 individuals in each Mexican State during the study period. The States with the highest rates (≥ 4 Liver disease deaths per 10000 per year) were mostly in the Southeastern Region of the country: Yucatán (4.86), Puebla (4.69), Morelos (4.62), Veracruz (4.57), Oaxaca (4.09) and Chiapas (4.04). The liver disease mortality rate in Nuevo Leon (2.09), one of the LT States, was less than half of that observed in States with a high mortality rate. The liver disease mortality rate per 10000 in the LT states was lower than that observed in the other states (median 3.1, IQR 0.3 vs 3.2, 0.1; P = 0.047).
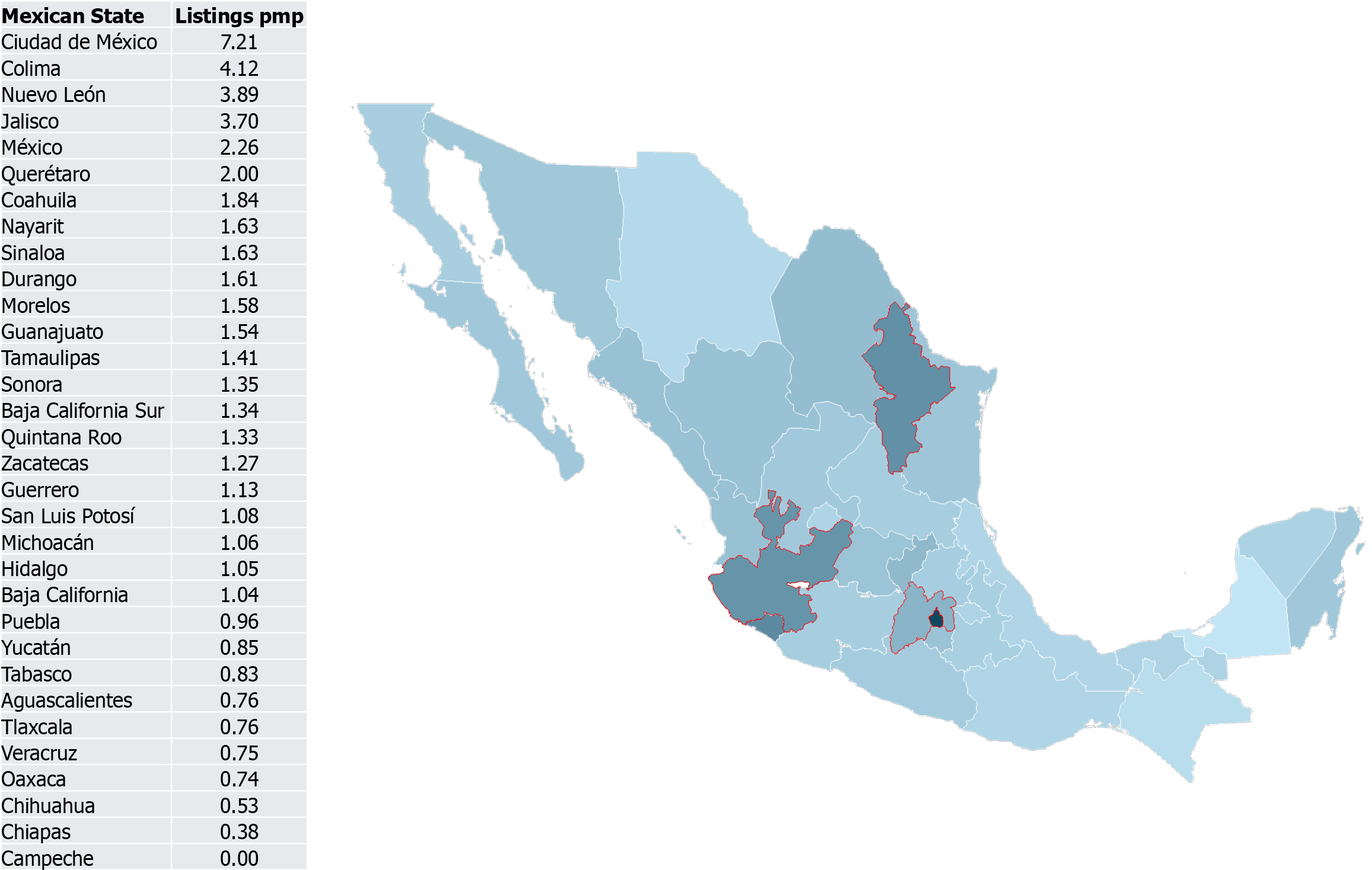
Between 2014 and 2023, there were 2600 new waitlist registrations; 1572 registrations (60.4%) were patients living in LT States. Figure 2 shows the median listings observed between 2014 and 2023 according to the Mexican State of residence, controlled by population. Listings pmp in the LT states were 3.2-fold higher (3.8, 1.5 vs 1.2, 0.6; P < 0.001). After controlling for liver disease deaths adjusted by the population of the State, O:E listings were 3.2-fold higher among the LT States (1.3, 0.4 vs 0.4, 0.2; P < 0.001). Quantitative variables comparing LT States and others are presented in Table 1.
| Variable | LT states | Rest | P value |
| Population (millions) | 39.7, 2.5 | 84.4, 4.6 | < 0.001 |
| Liver disease mortality rate per 10000 | 3.1, 0.3 | 3.2, 0.1 | 0.047 |
| Listings per million | 3.8, 1.5 | 1.2, 0.6 | < 0.001 |
| O:E listings | 1.3, 0.4 | 0.4, 0.2 | < 0.001 |
| T:L ratio | 70% | 63.6% | < 0.001 |
| Mortality | 15.2% | 19.4% | 0.006 |
Overall waiting time was not different between the LT States and the rest (person-years 74.3, 23.7 vs 56.4, 33; P = 0.174). LT rate at 90 days was higher in the LT states (45% vs 40.9%; P = 0.046), whereas the mortality rate at 90 days was not significantly different (9.1% vs 11.1%; P = 0.107). For every 100 person-years, a median of 38.2 patients in the waiting list died in LT states; the rate was not statistically different from that observed in the rest of the States (26.9 deaths per 100 person-years; P = 0.800).
During the study, there were 1755 LT; 1101 were done in patients living in LT states (62.7% vs 37.3%; P < 0.001). Figure 3 shows the median LT performed between 2014 and 2023 according to the Mexican State of residence, controlled by population. Table 2 summarizes the results of overall access to LT. LT pmp in LT states was 3.8-fold higher (2.7, 0.9 vs 0.7, 0.5; P < 0.001), while the overall likelihood of being transplanted (T:L ratio) was 70% in LT states vs 63.6% in low LT States (P < 0.001); overall waitlist mortality was 15.2% in LT States vs 19.4% in low LT States (P = 0.006).
| Variable | LT states | Rest | P value |
| Waiting time (days) | 74.3, 23.7 | 56.4, 33 | 0.42 |
| Time until transplant (days) | 51, 117 | 53, 132 | 0.56 |
| Transplant rate at 90 days | 45% | 40.9% | 0.046 |
| Mortality rate at 90 days | 9.1% | 11.1% | 0.10 |
| Transplants per 100 person-years | 151.7, 107.3 | 93.4, 105.1 | 0.11 |
| Deaths per 100 person-years | 38.2, 23.3 | 26.9, 28 | 0.8 |
Transplant and mortality at 90 days, as well as transplants and deaths per 100 person-years are compared between the LT States and the Rest in Table 2. For every 100 person-years, a median of 151.7 LT were performed in LT states; the rate was not statistically different from that observed in the rest of the States (93.4 LT per 100 person-years; P = 0.110). After controlling for sex (female vs male), age group (pediatric vs adult), blood type (0, A, B, and AB), and Healthcare Sector (Private vs Public), patients living in LT States had an HR of 1.14 (95%CI: 1.03-1.26; P = 0.009) for transplantation after listing (Table 3).
| Variable | Hazard ratio | 95%CI | P value |
| Age (adult vs pediatric) | 1.57 | 1.36-1.8 | < 0.001 |
| Gender (male vs female) | 1.1 | 0.99-1.21 | 0.06 |
| ABO group (reference group 0) | |||
| Group A | 1.24 | 1.12-1.39 | < 0.001 |
| Group B | 1.08 | 0.91-1.27 | 0.38 |
| Group AB | 1.29 | 0.9-1.86 | 0.166 |
| Healthcare Sector (public vs private) | 0.98 | 0.89-1.11 | 0.977 |
| Residence (LT state vs rest) | 1.14 | 1.03-1.26 | 0.009 |
Our findings reveal that Mexicans living in States with high LT activity (Mexico City and its Metropolitan Area, Nuevo Leon, and Jalisco) are 3.2 times more likely to access the LT waiting list and 3.8 times more likely to undergo LT than those living in States with lower LT activity. Over 90% of all LT in Mexico were performed in these high-activity States into a disproportionately high percentage of local residents. Centralization constitutes a barrier to equitable access and development of LT in the country, limiting access for patients living in less developed regions, such as the Southeast region of the country, where there is the highest mortality rate due to liver disease and the lowest LT access. These patients face barriers such as the need for long-distance travel, increased financial burden, and logistical challenges that further reduce their opportunity to access LT. This disparity highlights a critical public health issue.
Centralization leads to higher volume in a few centers, which has been associated with improved resource utilization and outcomes in different forms of liver disease care and LT[13-17]. Multiple individual studies have shown that some patients may prefer to receive local healthcare, even when other, potentially better options may be available[18,19]; however, a systematic review was not able to ascertain whether patients are willing to travel for a lower surgery-associated risk, identifying factors other than rational information on patient’s decision[20]. A survey showed that approximately 80% of patients were willing to trade shorter travel times for lower perioperative mortality and higher 3-year survival after LT[21]. However, only 2.8% of patients in the United States are listed at distant centers from its residence, even when a 22% reduction in the risk of death at 1 year after listing in a distant center has been demonstrated[22].
Centralization brings some problems. The current study shows that centralization leads to disparities in access to LT listing in our country. Centralization may reduce the availability of training positions and limit the diversity of clinical experience among trainees. Centralization of healthcare also leads to irregularities in organ allocation. For example, high-volume trauma centers generate more livers and hospital-based allocation leads to a higher allocation of those organs to patients listed in those hospitals, disadvantaging other centers, such as oncological centers[23].
Some countries have established strategies to reduce the negative impact of centralization in LT. In the United Kingdom, patients assessed for LT for chronic liver disease at satellite centers are more likely to result in acceptance of candidacy and less likely to result in a contraindication than patients referred from other centers to a large transplant program[24].
The significant breakdown of our healthcare system limits its capacity to provide equitable care. Patients affiliated to a specific subsystem must travel to designated centers for evaluation and listing, even when closer facilities exist. Referrals of patients living in the remaining 28 States must be performed by the local hospital from the subsystem to which the patient is affiliated, as no self-referral is possible. Referring and referral hospitals do not share patient data, and referral hospitals frequently repeat the same studies and evaluations performed by referring hospitals. In some instances, the patient must be evaluated in multiple hospitals from the same subsystem until they reach an active LT center. This highlights the urgency of adopting a different approach to improving access and fairness in LT.
This study has several policy implications. First, there is an urgent need to decentralize LT services and strengthen the existing transplant centers in underserved areas. This investment could range from medical infrastructure, training healthcare professionals, expansion of current programs and, in the long-term, establishing new LT centers strategically located to serving populations with higher needs. Second, improving coordination and communication within healthcare subsystems, and among them, could facilitate referral processes and reduce some of the logistical barriers that patients face. Third, allowing patients in need of LT to access other subsystems as exceptional cases could improve patient’s access without significant investment in infrastructure. Fourth, support programs for patients traveling from remote areas could relieve some of the financial challenges they face. Providing accommodation, transportation, or other forms of assistance will make it more feasible for this patient population to reach and stay around LT centers.
Our study had several limitations. First, the estimation of the need for LT comes from mortality data. Not all patients who die of liver disease are candidates for LT. However, there is no rationale to assume that the percentage of candidates would be significantly different across Mexican States; therefore, we used the number of deaths to estimate the “expected” number of registrations. Mortality data may be subject to misclassification, especially in underserved areas, potentially leading to biases in our estimation of O:E listings. Second, the database from Centro Nacional de Trasplantes provides very limited data on the characteristics of the registered patients and has no data on outcomes after LT. For example, the City of residence is not available in this database for patients registered on the waiting list; therefore, we had to limit our analysis to the State of residence. This could be important as it would further clarify the access disparities of patients living outside the three major Metropolitan areas. For example, we have previously shown that the donation activity in the State of Mexico is significantly different in the Metropolitan Area (approximately 12 million inhabitants) compared to the rest of the State (approximately 4 million inhabitants)[25]. In view of this limitation, in the present study, Mexico State is considered as a “high-activity” State, even though there are only two licensed centers and only one of them is active[11]. Third, selected liver tumors benefit from LT[26]. Liver tumors are coded under the ICD-10 as C22 and could be obtained from the Dirección General de Información en Salud database. However, no study has analyzed the percentage of patients with primary liver tumors in Mexico who are candidates for LT; it is likely that many patients with secondary liver tumors are included under “Malignant neoplasm of the liver, not otherwise specified”, which are only candidates for LT in highly selected circumstances. Therefore, we decided not to include liver tumors in the calculation of the liver disease burden. Fourth, although some monogenic metabolic diseases can be identified through ICD-10 codes, not all patients with these diagnoses require LT, and they represent a very low percentage of the burden of liver disease in Mexico; therefore, we decided not to include them in the calculation. Fifth, the lack of clinical data (disease severity scores, comorbidities, specific diagnosis) limits adjustment for disease severity, which likely affects both access and transplant probability. Sixth, the limitation of residency to state rather than city or zip code in the national database, prevented us from calculating the distance between the residence and the transplant center. This has been shown to be associated with greater waitlist mortality for adult candidates[27]. Furthermore, the lack of social and economic variables in the national database (e.g., income level, indigenous status, language barriers), prevented us from providing a more granular analysis which could further illuminate access barriers. Seventh, we limited our analysis to an arbitrary classification of “LT States” and “Others”. Even though there is limited activity in the states labelled as “Others” in our study, it corresponds to < 10%. A more complex classification could provide a more granular view of our data. However, we preferred to maintain this classification to provide a clearer message and limit statistical analysis.
Geographical disparities in LT access in Mexico represent a significant ongoing challenge. Addressing these disparities requires revisions of current healthcare policies, increased investment in healthcare infrastructure, and enhanced coordination within and across healthcare subsystems. These interventions may help create a more equitable distribution of healthcare, ultimately improving the outcomes for patients with liver disease in Mexico.
| 1. | GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403:2133-2161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2282] [Cited by in RCA: 2647] [Article Influence: 1323.5] [Reference Citation Analysis (0)] |
| 2. | GBD 2017 Cirrhosis Collaborators. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5:245-266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1184] [Cited by in RCA: 1109] [Article Influence: 184.8] [Reference Citation Analysis (5)] |
| 3. | Aguirre-Villarreal D, Servin-Rojas M, Sánchez-Cedillo A, Chávez-Villa M, Hernandez-Alejandro R, Arab JP, Ruiz I, Avendaño-Castro KP, Matamoros MA, Adames-Almengor E, Diaz-Ferrer J, Rodriguez-Aguilar EF, Paez-Zayas VM, Contreras AG, Alvares-da-Silva MR, Mendizabal M, Oliveira CP, Navasa M, García-Juárez I. Liver transplantation in Latin America: reality and challenges. Lancet Reg Health Am. 2023;28:100633. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 4. | Riley WJ. Health disparities: gaps in access, quality and affordability of medical care. Trans Am Clin Climatol Assoc. 2012;123:167-72; discussion 172. [PubMed] |
| 5. | Yilma M, Dalal N, Wadhwani SI, Hirose R, Mehta N. Geographic disparities in access to liver transplantation. Liver Transpl. 2023;29:987-997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 6. | Contreras AG, McCormack L, Andraus W, de Souza M Fernandes E; Latin America Liver Transplantation Group. Current status of liver transplantation in Latin America. Int J Surg. 2020;82S:14-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | INEGI. Instituto Nacional de Estadística y Geografía. [cited 25 June 2024]. Available from: https://www.inegi.org.mx/. |
| 8. | McClain JO. Exponential smoothing: appropriate and inappropriate applications. Health Serv Res. 1971;6:256-259. [PubMed] |
| 9. | DGIS. Dirección General de Información en Salud. [cited 5 July 2024]. Available from: http://www.dgis.salud.gob.mx/contenidos/basesdedatos/Datos_Abiertos_gobmx.html. |
| 10. | Chávez-Tapia NC, Barrientos-Gutiérrez T, Guerrero-López CM, Santiago-Hernández JJ, Méndez-Sánchez N, Uribe M. Increased mortality from acute liver failure in Mexico. Ann Hepatol. 2012;11:257-262. [PubMed] |
| 11. | CENATRA. Datos Abiertos. [cited 12 July 2024]. Available from: https://www.datos.gob.mx/busca/organization/cenatra. |
| 12. | SRTR. What is the formula for patient years? [cited 23 May 23 2024]. Available from: https://www.srtr.org/faqs/for-transplant-center-professionals/. |
| 13. | Oh SY, Jang EJ, Kim GH, Lee H, Yi NJ, Yoo S, Kim BR, Ryu HG. Association between hospital liver transplantation volume and mortality after liver re-transplantation. PLoS One. 2021;16:e0255655. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Yoo S, Jang EJ, Yi NJ, Kim GH, Kim DH, Lee H, Jung CW, Ryu HG. Effect of Institutional Case Volume on In-hospital Mortality After Living Donor Liver Transplantation: Analysis of 7073 Cases Between 2007 and 2016 in Korea. Transplantation. 2019;103:952-958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 15. | Lee H, Jang EJ, Kim GH, Yi NJ, Kim DH, Yoo S, Row HS, Jung CW, Oh SY, Ryu HG. Effect of Case Volume on Mortality After Pediatric Liver Transplantation in Korea. Transplantation. 2019;103:1649-1654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Yoo S, Jang EJ, Kim GH, Kim DH, Kwon SM, Lee H, Jung CW, Ryu HG. Effect of Institutional Case Volume on In-Hospital Mortality After Deceased Donor Liver Transplantation: A Nationwide Retrospective Cohort Study in Korea. Transplant Proc. 2018;50:3644-3649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Macomber CW, Shaw JJ, Santry H, Saidi RF, Jabbour N, Tseng JF, Bozorgzadeh A, Shah SA. Centre volume and resource consumption in liver transplantation. HPB (Oxford). 2012;14:554-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 60] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 18. | Alvino DML, Chang DC, Adler JT, Noorbakhsh A, Jin G, Mullen JT. How Far Are Patients Willing to Travel for Gastrectomy? Ann Surg. 2017;265:1172-1177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 19. | Shalowitz DI, Nivasch E, Burger RA, Schapira MM. Are patients willing to travel for better ovarian cancer care? Gynecol Oncol. 2018;148:42-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 20. | Bühn S, Holstiege J, Pieper D. Are patients willing to accept longer travel times to decrease their risk associated with surgical procedures? A systematic review. BMC Public Health. 2020;20:253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 21. | Burkamp JR, Bühn S, Schnitzbauer A, Pieper D. Preference between medical outcomes and travel times: an analysis of liver transplantation. Langenbecks Arch Surg. 2022;407:707-716. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Kwong AJ, Mannalithara A, Heimbach J, Prentice MA, Kim WR. Migration of Patients for Liver Transplantation and Waitlist Outcomes. Clin Gastroenterol Hepatol. 2019;17:2347-2355.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 23. | Altomare M, Chierici A, Virdis F, Spota A, Cioffi SPB, Bekhor SS, Del Prete L, Reitano E, Sacchi M, Ambrogi F, Chiara O, Cimbanassi S. Centralization of Major Trauma Influences Liver Availability for Transplantation in Northern Italy: Lesson Learned from COVID-19 Pandemic. J Clin Med. 2022;11:3658. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 24. | Tavabie OD, Kronsten VT, Przemioslo R, McDougall N, Ramos K, Joshi D, Prachalias A, Menon K, Agarwal K, Heneghan MA, Valliani T, Cash J, Cramp ME, Aluvihare V. Satellite liver transplant centres significantly improve transplant assessment outcomes for patients with chronic liver disease but not hepatocellular carcinoma: a retrospective cohort study. Frontline Gastroenterol. 2023;14:334-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 25. | Zamora-Valdés D, Leal-Leyte P, Díaz-Muñoz I, Méndez-Sánchez N. Liver Recovery and Transplantation From Deceased Donors in the Metropolitan Area of the Valley of Mexico. Transplant Proc. 2020;52:1062-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 26. | Pullen LC. Liver disease is changing and transplant oncology is rising to the challenge. Am J Transplant. 2024;24:313-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 27. | Zhou K, Albertian R, Wong C, Kuo LS, Thompson LK, Dodge JL, Mehta N, Terrault NA, Cockburn MG. Longer travel and traffic are associated with adult liver transplant waitlist mortality in the United States. Am J Transplant. 2025;25:1515-1525. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |