Published online Dec 18, 2025. doi: 10.5500/wjt.v15.i4.108728
Revised: May 15, 2025
Accepted: August 25, 2025
Published online: December 18, 2025
Processing time: 211 Days and 19.2 Hours
The impact of long-term dialysis (LTD) therapy on the survival benefit of kidney transplantation compared to short-term dialysis (STD) remains unclear. Addi
To investigate the effects of the best graft function within three months post-transplant, as well as dialysis duration, on transplant outcomes.
A total of 255 patients were included in this retrospective cohort study. Patients were divided into two groups: Those with LTD (≥ 15 years; Group LTD) and those with STD (< 15 years; Group STD). Clinical backgrounds and outcomes were compared between the groups.
Group LTD comprised 28 patients, while Group STD included 227 patients. There were no significant differences between the two groups in terms of age at tran
These findings suggest that early graft dysfunction, rather than dialysis duration, may serve as a critical risk factor for poor transplant outcomes.
Core Tip: This retrospective cohort study investigated the impact of dialysis duration and early graft function on kidney transplant outcomes. Among 255 recipients, no significant differences were found between long- and short-term dialysis groups in key clinical variables. Multivariate analysis identified age, post-transplant cardiovascular events, and best serum creatinine within three months as independent predictors of mortality. In contrast, dialysis duration was not associated with post-transplant survival. These findings highlight that early graft function may be more critical than dialysis duration in determining long-term transplant outcomes.
- Citation: Shimada H, Iwai T, Uchida J. Clinical impact of early graft function in kidney transplant recipients on long-term dialysis: A retrospective cohort study. World J Transplant 2025; 15(4): 108728
- URL: https://www.wjgnet.com/2220-3230/full/v15/i4/108728.htm
- DOI: https://dx.doi.org/10.5500/wjt.v15.i4.108728
For end-stage kidney disease (ESKD) patients, transplantation is a cost-effective mode of treatment, and greater longevity has been demonstrated for recipients of kidney transplants compared to those remaining on dialysis therapy[1,2]. In addition, pre-transplant dialysis vintage has been associated with adverse effects on patient survival[3,4]. Patients on dialysis with prolonged waiting periods have an increased risk for patient mortality and post-transplant graft failure[5]. Pre-emptive kidney transplants may therefore be an optimal treatment for ESKD patients, because patient survival is better than those for dialysis patients receiving transplants[6].
The data from the Japanese registry for renal replacement therapy have shown that improvements in dialysis techniques have prevented uremic complications in the long term, increasing the number of patients on hemodialysis for more than 10 years[7]. The Dialysis Outcomes and Practice Patterns Study has reported that there is a significantly lower mortality risk in Japan compared to Europe or the United States[8]. Waiting periods for transplants are longer in Japan than in many other countries, and a patient over 20 years old must wait approximately 15 years before receiving a deceased kidney transplant[9].
Although whether recipients undergoing a transplant after long-term dialysis (LTD) therapy have a similar patient survival benefit to recipients experiencing short-term dialysis (STD) remain unknown, a recent study reported that transplantation was associated with better patient survival even in those undergoing dialysis for 10 years or more compared to waitlisted patients with the same dialysis duration[10]. However, the quality of the donor organ was reported to be a strong predictor of patient survival in those receiving kidneys from deceased donors[10]. Patients on dialysis for extended periods would not have the benefit of better patient survival, if they received low quality grafts. In the present study, we evaluated the effects of graft quality as defined by best graft function within 3 months of trans
A cohort study was retrospectively performed on recipients of kidney transplants at Osaka Metropolitan University Hospital (former Osaka City University Hospital), and the risk factors that affect prognosis after transplantation were examined. Approved for this study was obtained from the Ethics Committee of Graduate School of Medicine, Osaka Metropolitan University (No. 3604). Patient consent was verified not by written informed consent but by opt-out consent, providing the patients with information on our research plan including the purpose, required individual data, and duration of research on our hospital website. All the procedures performed in the study were under the Helsinki Declaration of 2000 and the Declaration of Istanbul 2008.
The medical records of all kidney transplant recipients at our institution from January 2001 to December 2016 were reviewed (n = 263). Of these patients, 2 patients with insufficient data and 6 patients who underwent a second transplant from a living donor were excluded. As a result, 255 patients were enrolled in our study.
The primary outcome was patient survival as of December 2017.
As the clinical data, recipient age at transplant, gender, body mass index, cause of ESKD, dialysis duration, pre-transplant cardiovascular disease history, co-morbidity (diabetes mellitus, dyslipidemia, hypertension) at transplant, donor age/gender, blood type and human leukocyte antigen mismatch, acute rejection episodes, cytomegalovirus (CMV) infection, malignancy, post-transplant history of cardiovascular disease, lowest serum creatinine (best S-Cr) level within 3 months of transplantation, and post-operative complications such as lymphatic leakage, urinoma and postoperative hematoma were collected, and the patients were divided into two groups (those with LTD): On dialysis for 15 years or more (Group LTD) and those with STD: On dialysis less than 15 years (Group STD).
Graft biopsies were conducted to verify all rejection episodes. Protocol biopsies were performed at about 1 month after transplantation. Episode biopsies were carried out when patients had increased S-Cr levels and/or proteinuria.
Improvements in immunosuppressive agents have been made since 1999, and the optimal protocol which was available at the time was used for our patients. Calcineurin inhibitor (CNI) (tacrolimus or cyclosporine), antimetabolite [azathi
For ABO-incompatible kidney transplantation, several sessions of double filtration plasmapheresis or plasma exchange were performed pre-transplant until the anti-A/B titers decreased to less than 1: 64. From 1999 to 2006, splenectomy was performed at the time of transplant to deplete B cells and inhibit antibody production. Since June 2006, rather than surgical splenectomy, we have administered rituximab (anti-cluster of differentiation 20 monoclonal antibody). That is, before their transplants, patients were given antimetabolite or mTOR inhibitor for 2 weeks to suppress B cell lymphocytes, and rituximab (150 mg/m2) was administered 2 weeks pre-transplant. This basic protocol was altered according to the age and anti-A/B antibody titers of the patients. In elderly patients (≥ 60 years), we administered MMF (0.5 g/day) to minimize its adverse events. Recipients who had high-titers (≥ 1:512), rebound of antibody titers, or donor-specific antibodies underwent both splenectomy and rituximab administration, and MMF or EVR was initiated 4 weeks pre-transplant.
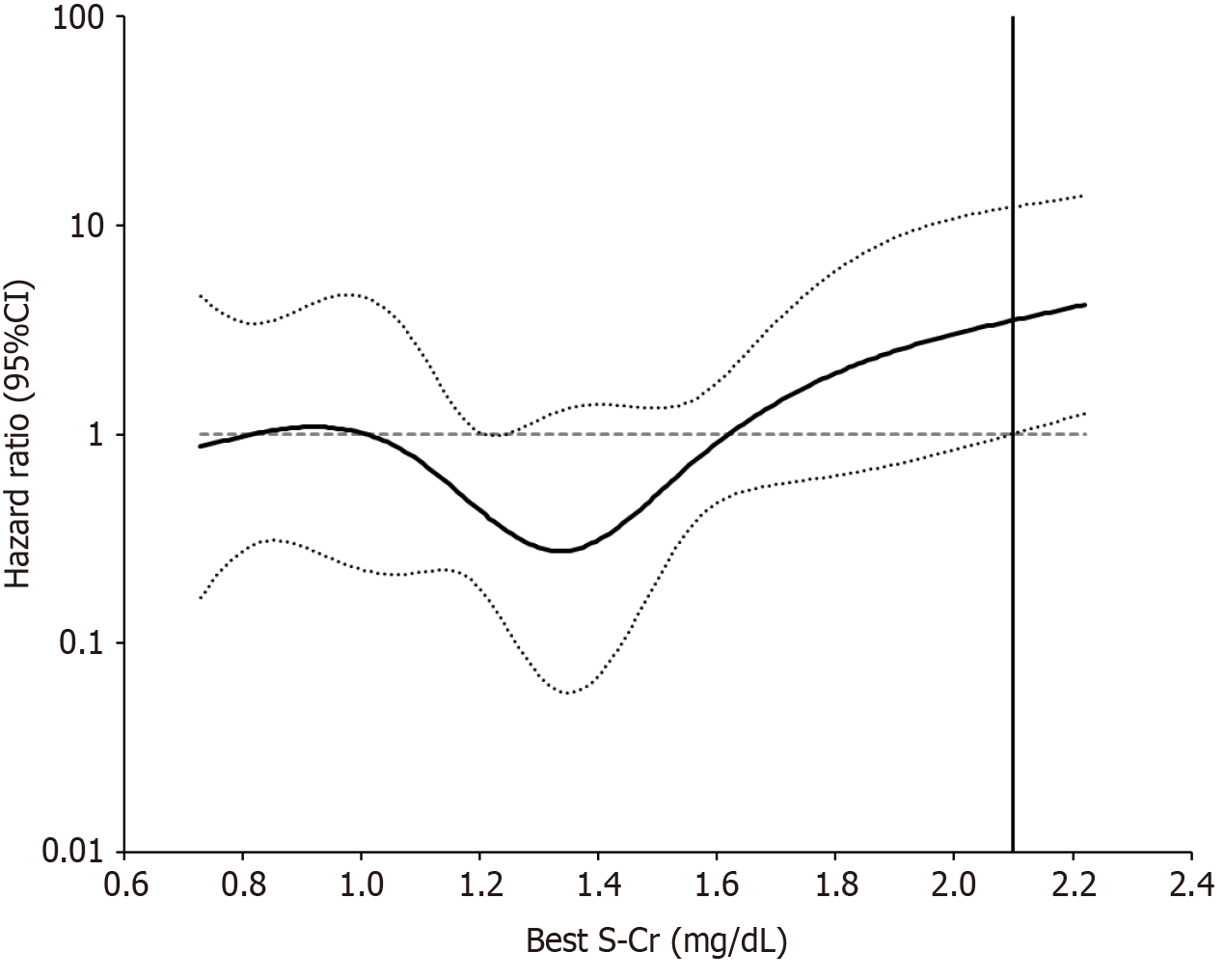
Categorical variables were expressed as counts and percentages and continuous variables as medians and interquartile ranges (IQR). Differences between the two groups divided by dialysis duration before kidney transplantation were examined with χ² test for categorical variables and with Mann-Whitney U test for continuous variables. The predictors of clinical events were analyzed and hazard ratios (HRs) and 95%CIs were calculated using the Cox proportional hazard regression model. Multivariate analysis (using stepwise forward likelihood ratio method) was performed using variables which were found to be significant by the univariate analysis. The effect of best S-Cr were continuously assessed after adjustment for age and post-transplant cardiovascular disease using cubic spline analysis in the Cox regression model. Best S-Cr were modeled as splines with knots at the 5th, 27.5th, 50th, 72.5th, and 95th percentiles. A value of P < 0.05 was considered statistically significant. All statistical analyses were made with SPSS for Windows version 22.0 (IBM Japan, Tokyo, Japan) and rms package and Hmics package in the R program (version 3.6.2).
The pre-transplant patient clinical characteristics are shown in Table 1. Age at transplant and donor age at transplant was not significantly different between Group LTD and STD. There was a significantly higher number of deceased donor kidney transplantation in Group LTD compared to Group STD. The pre-transplant prevalence of hypertension, diabetes mellitus, and dyslipidemia was 59.3% vs 82.8%, 0% vs 19.8%, and 17.2% vs 7.4%, respectively (Group LTD vs Group STD). There was a history of cardiovascular events in 24% of Group LTD patients and 14.5% of Group STD patients, which was not significantly different. Table 2 shows the post-transplant clinical characteristics. There was no significant difference in the type of CNI, best S-Cr, prevalence of rejection, and CMV infection. The frequency of cardiovascular events after transplantation was also not significantly different between the two groups. There was a higher frequency of malignancy after transplantation in Group LTD compared to Group STD.
| Variables | Group LTD (n = 28) | Group STD (n = 227) | P value1 |
| Age at Tx (years) | 51 (45-55) | 46 (36-57) | 0.123 |
| Male gender (%) | 57.1 | 60.8 | 0.838 |
| BMI at Tx (kg/m2) | 20.52 (18.87- 21.91) | 21.85 (19.41- 24.83) | 0.086 |
| Dialysis duration (years) | 20.2 (17.2-24.3) | 1.4 (0.5-4.9) | < 0.001 |
| Comorbidity at Tx | |||
| Hypertension (%) | 59.3 | 82.8 | 0.008 |
| Diabetes mellitus (%) | 0 | 19.8 | 0.006 |
| Dyslipidemia (%) | 17.2 | 7.4 | 0.271 |
| History of CVD event (%) | 24.0 | 14.2 | 0.236 |
| Cause of ESKD | |||
| CGN (%) | 75.0 | 21.6 | < 0.001 |
| ADPKD (%) | 3.6 | 8.4 | 0.707 |
| IgA nephropathy (%) | 3.6 | 13.7 | 0.221 |
| Diabetic kidney disease (%) | 0 | 19.4 | 0.006 |
| Other or unknown (%) | 17.9 | 33.9 | 0.132 |
| Deceased donor kidney Tx (%) | 85.7 | 2.2 | < 0.001 |
| Donor age at Tx (years) | 57 (44-62) | 58 (51-65) | 0.119 |
| Donor male gender (%) | 60.7 | 37.0 | 0.023 |
| ABO-incompatible (%) | 3.6 | 26.0 | 0.008 |
| HLA mismatch number | 3 (2-3) | 3 (3-5) | 0.007 |
| Variables | Group LTD (n = 28) | Group STD (n = 227) | P value1 |
| Immunosuppression | |||
| Methylprednisolone (%) | 96.4 | 94.3 | 1 |
| Tacrolimus (%) | 53.6 | 44.5 | 0.423 |
| Cyclosporine (%) | 46.4 | 55.5 | 0.423 |
| Mycophenolate mofetil (%) | 96.4 | 89.0 | 0.328 |
| Mizoribine (%) | 0 | 3.1 | 1 |
| Everolimus (%) | 3.6 | 7.9 | 0.704 |
| Outcomes | |||
| Best S-Cr (mg/dL) | 1.37 (1.18-2.04) | 1.33 (1.02-1.55) | 0.102 |
| Acute rejection (%) | 21.4 | 23.8 | 1 |
| CMV infection (%) | 42.9 | 25.1 | 0.069 |
| Surgical complications (%) | 14.3 | 15.0 | 1 |
| Hypertension (%) | 85.7 | 83.3 | 1 |
| Diabetes mellitus (%) | 14.3 | 27.8 | 0.172 |
| Dyslipidemia (%) | 46.4 | 59.4 | 0.225 |
| Malignancy (%) | 17.9 | 4.8 | 0.021 |
| CVD event (%) | 10.7 | 6.6 | 0.429 |
The patients who died after transplantation are summarized in Table 3. In Group LTD, four patients died of infectious disease including sepsis and varicella zoster, one died of renal cell carcinoma, and one died of cardiovascular disease. In Group STD, five patients died of cardiovascular disease, three died of malignant tumor, one died of alcoholic pancreatitis, and one died of bacterial pneumonia. Figure 1 shows the Kaplan-Meier estimates of death after transplantation. Patients in Group LTD had a shorter patient survival than those in Group STD (log-rank test, P < 0.001). The median follow-up period was 6.2 (IQR: 2.8-10.3) years in Group LTD and 6.4 (IQR: 3.4-10.2) years in Group STD.
| Case | Age (years) | Gender | Time from Tx to death (years) | Dialysis duration (years) | Best S-Cr (mg/dL) | Causes of death |
| Group LTD | ||||||
| 1 | 52 | Male | 2.1 | 30.0 | PNF | Sepsis |
| 2 | 53 | Male | 0.5 | 25.1 | 2.86 | Renal cell carcinoma |
| 3 | 65 | Female | 11.5 | 18.8 | 0.77 | Sepsis |
| 4 | 40 | Male | 1.5 | 15.5 | 4.28 | Varicella zoster |
| 5 | 54 | Male | 0.6 | 15.3 | 3.67 | Cardiovascular disease |
| 6 | 55 | Female | 8.6 | 15.0 | 1.28 | Sepsis |
| Group STD | ||||||
| 1 | 40 | Male | 3.1 | 13.2 | 2.19 | Alcoholic pancreatitis |
| 2 | 59 | Male | 2.0 | 10.3 | PNF | Cardiovascular disease |
| 3 | 71 | Male | 6.9 | 8.2 | 0.83 | Bacterial pneumonia |
| 4 | 65 | Male | 1.7 | 3.7 | 1.9 | Pancreatic carcinoma |
| 5 | 74 | Male | 4.2 | 3.3 | 2.04 | Cardiovascular disease |
| 6 | 56 | Male | 11.2 | 2.0 | 2.13 | Cardiovascular disease |
| 7 | 54 | Female | 13.3 | 1.0 | 1.03 | Myelodysplastic syndrome |
| 8 | 62 | Male | 5.8 | 0.9 | 0.82 | Cardiovascular disease |
| 9 | 77 | Male | 5.0 | 0 | 1.16 | Gastric carcinoma |
| 10 | 72 | Female | 6.3 | 0 | 0.84 | Cardiovascular disease |
The results of univariate and multivariate Cox proportional hazard regression analysis are shown in Table 4. In the univariate analysis, age (HR: 1.069; 95%CI: 1.022-1.118; P = 0.003), dialysis duration (HR: 1.076; 95%CI: 1.021-1.134; P = 0.006), malignancy (HR: 6.139; 95%CI: 2.170-17.369; P < 0.001), post-transplant cardiovascular disease (HR: 17.775; 95%CI: 6.421-49.206; P < 0.001), and best S-Cr (HR: 2.949; 95%CI: 1.704-5.104; P < 0.001) were significant predictors of death after kidney transplantation. Multivariate analysis indicated that age (HR: 1.058; 95%CI: 1.002-1.116; P = 0.040), post-transplant cardiovascular disease (HR: 20.264; 95%CI: 6.052-67.850; P < 0.001), and best S-Cr (HR: 4.155; 95%CI: 2.234-7.730; P < 0.001) were independent predictors of death after transplantation. The continuous effect of best S-Cr level on the HR of death after transplantation adjusted for age and post-transplant cardiovascular disease on multivariate analysis using cubic spline analysis is shown in Figure 2. The HR of death after kidney transplantation increased nonlinearly, especially at a best S-Cr level higher than 2.1 mg/dL.
| Variables | Factors | Univariate analysis | Multivariate analysis | ||||
| HR | 95%CI | P value | HR | 95%CI | P value | ||
| Age (years) | Increase of 1 year | 1.069 | 1.022-1.118 | 0.003 | 1.058 | 1.002-1.116 | 0.040 |
| Gender | Male vs female | 2.087 | 0.673-6.475 | 0.203 | - | ||
| Donor gender | Male vs female | 1.171 | 0.436-3.146 | 0.755 | |||
| BMI (kg/m2) | Increase of 1 kg/m2 | 0.993 | 0.864-1.142 | 0.927 | - | ||
| Dialysis duration (years) | Increase of 1 year | 1.076 | 1.021-1.134 | 0.006 | NE | ||
| Pre-Tx DM | Present vs absent | 1.089 | 0.243-4.881 | 0.912 | - | ||
| Malignancy | Present vs absent | 6.139 | 2.170-17.369 | < 0.001 | NE | ||
| Post-Tx CVD | Present vs absent | 17.775 | 6.421-49.206 | < 0.001 | 20.264 | 6.052-67.850 | < 0.001 |
| Best S-Cr (mg/dL) | Increase of 1 mg/dL | 2.949 | 1.704-5.104 | < 0.001 | 4.155 | 2.234-7.730 | < 0.001 |
In the present study, the patients in Group LTD had a shorter patient survival than those in Group STD. In the univariate Cox proportional hazard model, age, dialysis duration, post-transplant cardiovascular disease, malignancy, and best S-Cr level were significant predictors of death after kidney transplantation. However, multivariate analysis indicated that age, post-transplant cardiovascular disease, and best S-Cr level were independent predictors of death after transplantation. It has been reported that graft dysfunction at 3 months post-transplant is a significant indicator for poor outcomes[11]. This study demonstrated that not dialysis duration but early graft dysfunction may be a risk factor for poor kidney transplant outcomes.
There is increasing uncertainty as to whether patients with very long dialysis lead time actually benefit after kidney transplantation[12]. LTD has been reported to have adverse effects on outcomes of kidney transplants[3-5]. Meanwhile, other studies have shown that patient survival is not affected by the length of patients on dialysis[13,14]. Previously, Goto et al[15] reported that earlier kidney transplants could be beneficial to reduce the incidence of death in patients with a functioning graft, graft loss, and post-transplant cardiovascular disease in Japan, where patients on dialysis have excellent long-term outcomes. However, this report did not have an analysis on the details of graft function. Kohei et al[13] revealed that good prognoses can be expected in kidney transplant recipients from living donors with few complications, even if they had been on dialysis for long periods. Also, Kimura et al[14] reported that S-Cr level at 3 months after kidney transplantation was similar between patients on dialysis for 15 years or more and those on dialysis for less than 15 years. However, this report did not have a multivariate analysis that examined the effect of S-Cr level on patient survival. Our study revealed that early graft function may play an important role in the survival of recipients, although dialysis duration before transplantation did not affect patient survival. Moreover, our study revealed that the best S-Cr level higher than 2.1 mg/dL was an independent risk factor of post-transplant mortality.
This study demonstrated that dialysis duration did not affect the patient survival. Patients on LTD have a poor prognosis, owing to uncontrolled hypertension, malnutrition, and pre-dialysis comorbidities. Compared with general population, patients on LTD have a greater frequency of cardiovascular disease. Patients on dialysis for long periods also often have severe atherosclerosis and calcification of coronary arteries[16]. Cardiovascular screening is an essential component in the process of transplant evaluation[13]. If a patient on dialysis for long period is eligible for kidney tran
Previously, many studies have reported improvements in graft survival and patient survival after preemptive kidney transplantation[6,17]. However, recent researches have indicated that these improvements can only be seen in preemptive transplants using grafts from deceased donors[18]. A recent report showed that transplants using high-quality kidneys from deceased donors had a longer survival benefit in selected patients who had been on dialysis for more than 10 years[10]. However, whether transplants using lower-quality kidneys from deceased donors have a better patient survival remains unknown[10]. Graft quality may be an important factor for a longer patient survival after transplantation, especially in patients with long dialysis duration. Early graft function as assessed by best S-Cr level within 3 months of transplantation may serve as an indicator for graft quality. In the present study, transplantation in recipients with high quality grafts was associated with better patient survival than that in recipients with low quality grafts.
There may be some limitations to this study, because it was a single-center, retrospective, observational study. There were also many deceased donor kidney transplant recipients in Group LTD. However, there are few reports on the interaction between early graft function and dialysis duration in recipients of kidney transplants. In our study, the effects of dialysis duration and early graft function on patient survival were evaluated by multivariate Cox hazard proportion analysis, and we found that dialysis duration did not affect patient survival in our recipients.
Further prospective, multicenter studies are warranted to validate these findings and clarify the role of early graft function in transplant recipients with LTD.
In conclusion, our finding showed that not dialysis duration but early graft dysfunction may be a risk for poor transplant outcomes, although larger, prospective, and longitudinal studies may be necessary to verify our results.
| 1. | Haller M, Gutjahr G, Kramar R, Harnoncourt F, Oberbauer R. Cost-effectiveness analysis of renal replacement therapy in Austria. Nephrol Dial Transplant. 2011;26:2988-2995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 128] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 2. | Wong G, Howard K, Chapman JR, Chadban S, Cross N, Tong A, Webster AC, Craig JC. Comparative survival and economic benefits of deceased donor kidney transplantation and dialysis in people with varying ages and co-morbidities. PLoS One. 2012;7:e29591. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 110] [Cited by in RCA: 155] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 3. | Cosio FG, Alamir A, Yim S, Pesavento TE, Falkenhain ME, Henry ML, Elkhammas EA, Davies EA, Bumgardner GL, Ferguson RM. Patient survival after renal transplantation: I. The impact of dialysis pre-transplant. Kidney Int. 1998;53:767-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 241] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 4. | Haller MC, Kainz A, Baer H, Oberbauer R. Dialysis Vintage and Outcomes after Kidney Transplantation: A Retrospective Cohort Study. Clin J Am Soc Nephrol. 2017;12:122-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 89] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 5. | Meier-Kriesche HU, Port FK, Ojo AO, Rudich SM, Hanson JA, Cibrik DM, Leichtman AB, Kaplan B. Effect of waiting time on renal transplant outcome. Kidney Int. 2000;58:1311-1317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 473] [Cited by in RCA: 484] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 6. | Kasiske BL, Snyder JJ, Matas AJ, Ellison MD, Gill JS, Kausz AT. Preemptive kidney transplantation: the advantage and the advantaged. J Am Soc Nephrol. 2002;13:1358-1364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 350] [Cited by in RCA: 361] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 7. | Nakai S, Iseki K, Itami N, Ogata S, Kazama JJ, Kimata N, Shigematsu T, Shinoda T, Shoji T, Suzuki K, Taniguchi M, Tsuchida K, Nakamoto H, Nishi H, Hashimoto S, Hasegawa T, Hanafusa N, Hamano T, Fujii N, Masakane I, Marubayashi S, Morita O, Yamagata K, Wakai K, Wada A, Watanabe Y, Tsubakihara Y. An overview of regular dialysis treatment in Japan (as of 31 December 2010). Ther Apher Dial. 2012;16:483-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 106] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 8. | Goodkin DA, Bragg-Gresham JL, Koenig KG, Wolfe RA, Akiba T, Andreucci VE, Saito A, Rayner HC, Kurokawa K, Port FK, Held PJ, Young EW. Association of comorbid conditions and mortality in hemodialysis patients in Europe, Japan, and the United States: the Dialysis Outcomes and Practice Patterns Study (DOPPS). J Am Soc Nephrol. 2003;14:3270-3277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 535] [Cited by in RCA: 580] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 9. | Japan Organ Transplant Network. NEWS LETTER Vol. 28, 2024 (in Japanese). [cited 25 April 2025]. Available from: https://www.jotnw.or.jp/files/page/datas/newsletter/doc/nl28.pdf. |
| 10. | Rose C, Gill J, Gill JS. Association of Kidney Transplantation with Survival in Patients with Long Dialysis Exposure. Clin J Am Soc Nephrol. 2017;12:2024-2031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 11. | Woo YM, Jardine AG, Clark AF, MacGregor MS, Bowman AW, Macpherson SG, Briggs JD, Junor BJ, McMillan MA, Rodger RS. Early graft function and patient survival following cadaveric renal transplantation. Kidney Int. 1999;55:692-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 75] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Haller MC, Kammer M, Oberbauer R. Dialysis vintage and outcomes in renal transplantation. Nephrol Dial Transplant. 2019;34:555-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Kohei N, Sawada Y, Hirai T, Omoto K, Ishida H, Tanabe K. Influence of dialysis duration on the outcome of living kidney transplantation. Ther Apher Dial. 2014;18:481-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Kimura T, Ishikawa N, Fujiwara T, Sakuma Y, Nukui A, Yashi M, Yagisawa T. Kidney transplantation in patients with long-term (more than 15 years) prior dialysis therapy. Transplant Proc. 2012;44:75-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Goto N, Okada M, Yamamoto T, Tsujita M, Hiramitsu T, Narumi S, Katayama A, Kobayashi T, Uchida K, Watarai Y. Association of Dialysis Duration with Outcomes after Transplantation in a Japanese Cohort. Clin J Am Soc Nephrol. 2016;11:497-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 16. | Hernández D, Rufino M, Armas S, González A, Gutiérrez P, Barbero P, Vivancos S, Rodríguez C, de Vera JR, Torres A. Retrospective analysis of surgical complications following cadaveric kidney transplantation in the modern transplant era. Nephrol Dial Transplant. 2006;21:2908-2915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 75] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 17. | Meier-Kriesche HU, Kaplan B. Waiting time on dialysis as the strongest modifiable risk factor for renal transplant outcomes: a paired donor kidney analysis. Transplantation. 2002;74:1377-1381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 555] [Cited by in RCA: 565] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 18. | Witczak BJ, Leivestad T, Line PD, Holdaas H, Reisaeter AV, Jenssen TG, Midtvedt K, Bitter J, Hartmann A. Experience from an active preemptive kidney transplantation program--809 cases revisited. Transplantation. 2009;88:672-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |