Published online Dec 18, 2025. doi: 10.5500/wjt.v15.i4.104399
Revised: March 23, 2025
Accepted: April 11, 2025
Published online: December 18, 2025
Processing time: 334 Days and 9.5 Hours
Detailed data on the relation of post-operative complications with clinical out
To compare Clavien-Dindo classification (CDC) and comprehensive complication index (CCI) in predicting outcomes after SPK.
Data for patients undergoing SPK between 1999-2019 were analyzed. Information on recipients’ baseline characteristics, peri-operative management and post-operative complications were collated. Length of hospital stay (LOS) was the primary study outcome, and the associations with CDC and CCI were evaluated using Spearman’s (ρ) correlation coefficients.
In the study period, data were available for 128 patients (female n = 44, 34.4%). Sixty-nine patients had at least one complication with the highest CDC grade of I, II, III, and IV in 8 (6.3%), 22 (17.2%), 32 (25%), and 7 (5.5%) patients, respectively. The mean LOS was 21.4 ± 17.7 days. Both classification systems were correlated with LOS, yet CCI was stronger (Spearman’s ρ: 0.694 vs 0.602, P < 0.001). Female patients (P = 0.019) and patients with pre-transplant cardiova
This study showed that the CCI was better linked with LOS compared to CDC and might represent a useful score to evaluate the overall burden of postoperative complications in patients undergoing SPK.
Core Tip: This is a retrospective single-center study to compare Clavien-Dindo classification and comprehensive complication index (CCI) in predicting outcomes after simultaneous pancreas-kidney transplantation. CCI has shown a stronger correlation with length of hospital stay when compared to Clavien-Dindo classification due to its cumulative nature. We advocate the utilization of CCI for future studies as it represents a more sensitive tool to better evaluate the overall burden of postoperative complications in patients undergoing simultaneous pancreas-kidney transplantation.
- Citation: Parente A, Verhoeff K, Marfil-Garza BA, Sanchez-Fernandez N, Anderson BL, Bigam DL, Shapiro AJ, Dajani KZ. Comparison of Clavien–Dindo classification and comprehensive complication index in patients undergoing simultaneous pancreas-kidney transplantation. World J Transplant 2025; 15(4): 104399
- URL: https://www.wjgnet.com/2220-3230/full/v15/i4/104399.htm
- DOI: https://dx.doi.org/10.5500/wjt.v15.i4.104399
Pancreas transplantation is currently the most effective method to establish durable normoglycemia for patients with diabetes mellitus[1]. In patients with concomitant end-stage renal disease, simultaneous pancreas-kidney (SPK) transplant is the treatment of choice. Recent data from the United States have shown that the number of adult candidates added to the waiting list increased for SPK in 2021 to 1487 from 1307 in the previous year[2]. The long-term results of SPK are encouraging, with a half-life longer than 14 years[2]. However, the widespread adoption of SPK has been hampered by high rates of surgical complications, such as bleeding, infection and thrombosis which frequently require relaparotomy and can lead to graft loss[3]. The most frequent method to evaluate post operative complication is the Clavien-Dindo classification (CDC)[4], which however utilizes an ordinal scale in order of severity, namely from grade I to grade V. As a result, when patients present with multiple complications, they are usually categorized according to the highest grade of CDC, which ignores the cumulative burden of multiple complications that may occur, especially after major surgery such as SPK. In 2013, the comprehensive complication index (CCI) was developed and validated in a large cohort of patients[5]. This combines the CDC grades of all complications developed by a patient cumulatively to generate a continuous score between 0 (no complications) and 100 (death). CCI offers a better evaluation of the overall burden of post-operative complications due its progressive and linear nature. The CCI has never been validated in SPK. Therefore, the present study aimed to compare the CCI with the conventional CDC in relation to hospital length of stay in patients undergoing SPK.
A retrospective study of all consecutive pancreas transplants completed at a single site was conducted. All adult patients undergoing SPK transplantation at the University of Alberta Hospital between January 1999 and October 2019 were included. Data collected included information about patients' characteristics, such as gender, age, and body mass index (BMI) in kg/m2. Additional recipient data, including indication for transplant, pre-transplant morbidities, total duration of diabetes, and time in the waiting list were collected. Patients undergoing pancreas transplant alone or pancreas after kidney were excluded. The study was submitted to the Health Research Ethics Board - Health Panel of the University of Alberta Hospital and Alberta Health Services. The Health Research Ethics Board approved the study with approval No. Pro00087040.
Peri and post-operative management SPK were routinely performed through a midline laparotomy. The kidney was implanted in a left-side retroperitoneal pouch and the pancreas was implanted intraperitoneally on the right side. Exocrine pancreatic drainage was restored performing a duodenojejunostomy. Immunosuppression consisted of induction immunosuppression (IS) with non-depletion anti-CD25 for non-sensitized patients, and thymoglobulin for those with elevated panel reactive antibodies or deemed to be of higher immunological risk. Maintenance immunosuppression consisted of corticosteroid taper down to a level of 5 mg daily, together with tacrolimus and mycophenolate mofetil. Historically, we used induction with prednisolone, daclizumab, or thymoglobulin or muromonab-CD3. Post-operatively, acetylsalicylic acid and heparin infusion or subcutaneous low-molecular weight heparin were given to all recipients. Complications were defined as “any deviation from the normal postoperative course” as per the CDC[4]. For each patient, data were collected for all postoperative complications that occurred within 90 days of the index hospitalization. Medical records were retrospectively reviewed for every patient to identify any complications, assigning a CDC grade between I and V, with the highest grade for a patient used in the analysis of CDC. Afterwards, the CCI was calculated for each patient accounting for each complication on the coded CDC grade. The CCI resulted in a score between 0 (no complications) and 100 (death). The CCIs were calculated utilizing the online tool[6].
The primary outcome was the length of hospital stay (LOS) which was calculated for each patient from the day of the operation to the day of discharge.
Continuous values are presented as means with standard deviation and medians with interquartile range when values were non-normally distributed; discrete values are presented as absolute numbers with percentages. While analyzing the CDC and CCI, we only considered those recipients who had at least one complication to eliminate bias from patients without complications. Associations between the complication classification scores and the LOS were then quantified using Spearman’s (ρ) correlation coefficients. In order to quantify further the relationship between complication classification scores and LOS, we produced univariate and multivariate regression models that included each score and associated demographic factors. The classification scores were treated as continuous covariates, with CDC grades coded between 1 and 6, in order to allow a differentiation for the CDC grades III and IV in the subcategories of “a” (IIIa, IVa) and “b” (IIIb, IVb). In this analysis, patients who had no complications were considered for this analysis and this was coded as a value of zero on both CCI and CDC. Statistical analysis was performed using Stata 17 (STATACorp LP, College Station, TX) and a P value of < 0.05 was considered statistically significant throughout.
Data were available for 146 patients of whom 11 (7.5%) and 7 (4.7%) underwent pancreas transplant alone and pancreas after kidney. These recipients were excluded, and therefore all the subsequent analyses were based on the 128 patients undergoing SPK. All patients had type 1 diabetes mellitus with end-stage chronic kidney disease as indication for SPK. These patients had a mean age at transplant of 40.9 ± 7.4 years, a mean BMI of 25.4 ± 3.9 kg/m2 and 44 (34.4%) were female. The mean age at diagnosis of diabetes was 12.9 ± 7.5 years, with a mean duration of 36.3 ± 9.6 years. Preoperative macrovascular diabetes related complications including myocardial infarction, coronary vascular events, or peripheral vascular disease were present in 45 (35.1%) recipients and the whole cohort had microvascular diabetes related complications. The majority of the patients had hypertension (n = 105, 82.0%) and dyslipidemia (n = 87, 68.0%) pre-transplant. These are summarized in Table 1.
| Characteristic | Whole cohort (n = 128) | No complication (n = 59) | At least one complication (n = 69) | P value |
| Age (years), mean ± SD | 40.9 ± 7.4 | 39.8 ± 7.5 | 41.9 ± 7.3 | 0.120 |
| Male | 84 (65.6) | 35 (59.3) | 49 (71.1) | 0.165 |
| Female | 44 (34.4) | 24 (40.7) | 20 (29.0) | - |
| BMI, kg/m2, mean ± SD | 25.4 ± 3.9 | 24.8 ± 4.0 | 25.8 ± 3.9 | 0.244 |
| Indication for transplant type 1 DM | 128 (100) | 59 (100) | 69 (100) | - |
| Age (years) at diagnosis of type 1 DM, mean ± SD | 12.9 ± 7.5 | 12.7 ± 7.6 | 13.2 ± 7.5 | 0.677 |
| Duration (years) of diabetes, mean ± SD | 36.3 ± 9.6 | 35.4 ± 9.2 | 37.1 ± 9.9 | 0.329 |
| Vascular pretx | ||||
| Macro1 | 45 (35.1) | 19 (32.2) | 26 (37.7) | 0.518 |
| Micro | 128 (100) | 59 (100) | 69 (100) | - |
| Comorbidities pretx | ||||
| Hypertension | 105 (82) | 45 (76.3) | 60 (87.0) | 0.117 |
| Dyslipidemia | 87 (68) | 38 (64.4) | 49 (71.0) | 0.424 |
| CKD | 128 (100) | 59 (100) | 69 (100) | - |
| Stroke | 1 (0.8) | 1 (1.7) | 0 (0) | 0.278 |
| MI | 1 (0.8) | 1 (1.7) | 0 (0) | 0.278 |
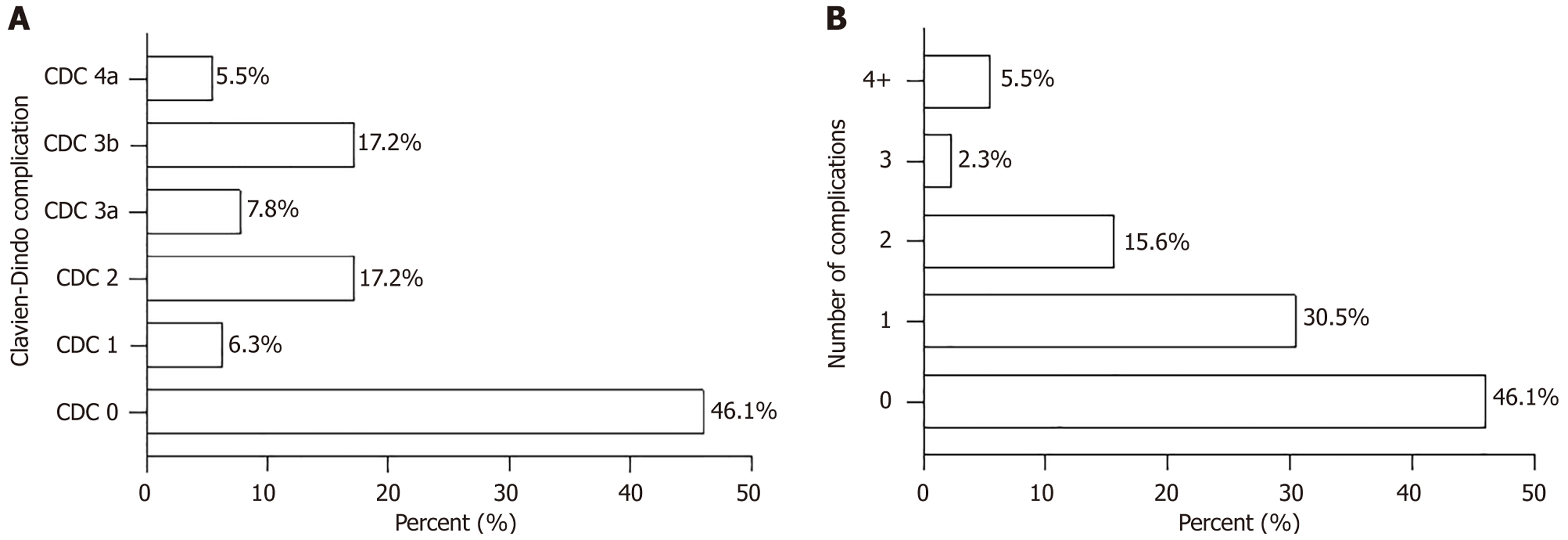
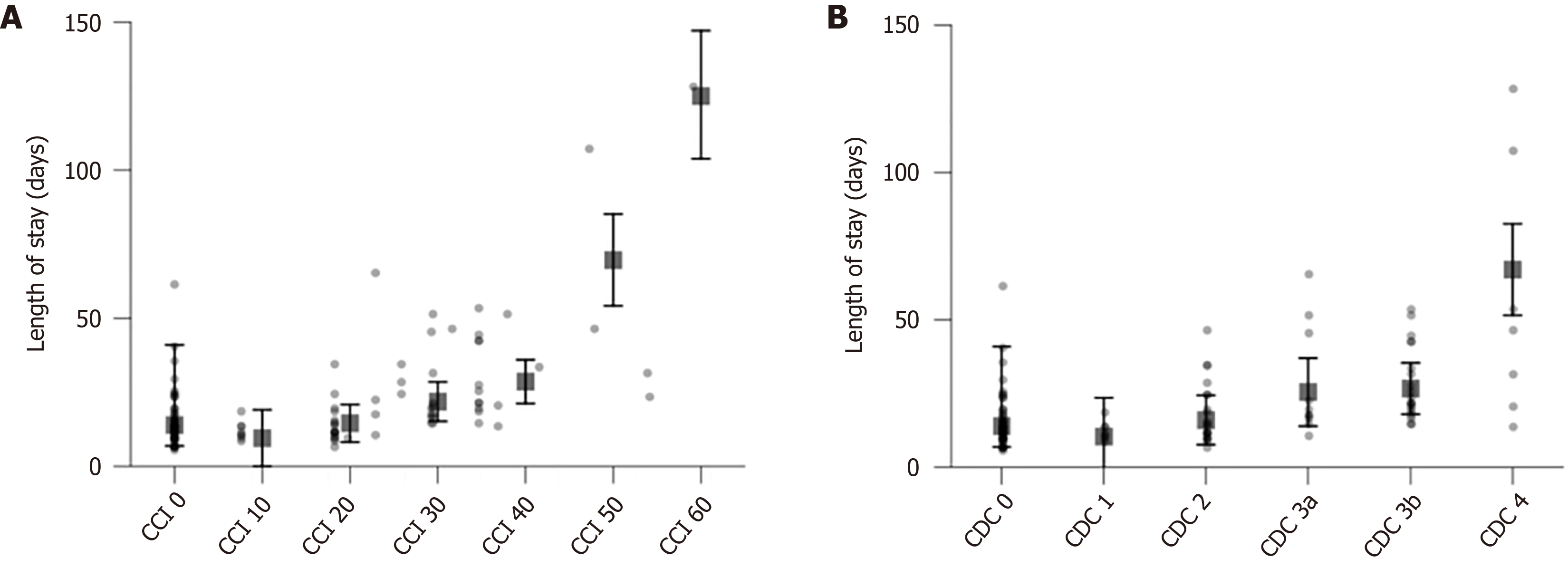
Looking at the IS induction, 93 (72.6%) patients received basiliximab, whereas 17 (13.3%) patients had daclizumab, 10 (7.8%) patients received thymoglobulin, and eight (6.3%) patients received muromonab-CD3. Tacrolimus and mycophenolate were used as maintenance IS for all patients. Complication data were recorded for each patient. Overall, 69 patients (53.9%) had a postoperative complication, with the highest CDC grade being I, II, III, and IV in 8 (6.3%), 22 (17.2%), 32 (25%), and 7 (5.5%) patients, respectively (Figure 1A). Reoperation (CDC 3b) was necessary in 27 patients, with the most common causes being sepsis/abscess/collection (n = 12), bleeding/hematoma evacuation (n = 5), graft thrombosis/pseudoaneurysm (n = 3), wound complications (n = 4), bowel obstruction (n = 2), and pancreatic fistula (n = 1). No post-operative deaths (CDC Grade V) were recorded. Of the total population, 39 (30.5%) had one complication, 20 (15.6%) had two, 3 (2.3%) had three, and 6 (4.7%) had four or more complications; importantly for this study, these results in 30 (23.4%) patients having two or more complications whose complications may better be captured by a cumulative complication index (Figure 1B). Cumulatively, the median CCI was 8.7 (interquartile range: 0-33.5) points and the mean LOS for the whole cohort was 21.4 ± 17.7 days. Comparing patients who had no complications to those with at least one complication demonstrated that groups had a similar percentage of females, age, BMI, diabetes diagnosis age, and diabetes duration (Table 1). They also had similar macrovascular and microvascular comorbidities (Table 1). The LOS for patients without any complications (15.7 ± 9.3 days) was significantly shorter compared to those ones with a complication (26.3 ± 21.4 days; P < 0.001). Primary outcome and evaluation of CDC and CCI For the evaluation of CDC and CCI, the 59 patients who had no complications were excluded, and therefore the analyses were conducted on the 69 recipients with at least one complication. For these, the two scores demonstrated a significant correlation with LOS, with Spearman’s ρ of 0.934 (P < 0.001). Both CDC and CCI had significantly correlation with the LOS, with a better performance of the CCI, giving a Spearman’s ρ of 0.602 (P < 0.001) for the CDC and 0.694 (P < 0.001) for the CCI. In addition, the correlations with LOS were compared using a regression analysis and including all 128 patients. Univariable analysis of the two scores showed estimated increases in the LOS of 5.01 days [95% confidence interval (CI): 3.41-6.61] per grade of the CDC, or 5.27 days (95%CI: 3.86-6.68 days, P < 0.001) per 10-point increase in the CCI (Figure 2). Furthermore, another analysis was conducted which adjusted for potential confounding factors and two different multivariable models were calculated for CDC and CCI, evaluating the association with LOS. It was found that patients with cardiovascular events pre-transplant (myocardial infarction, cerebrovascular event, peripheral vascular disease) had significantly longer LOS (7.82 days, 95%CI: 1.25-14.38; P = 0.02) as did female patients (8.14 days, 95%CI: 1.39-14.89; P = 0.019). After adjusting for these factors, the association between LOS and the CDC (P < 0.001) and CCI (P < 0.001) remained statistically significant (Table 1). The model including CCI had superior fit for predicting LOS (r2 = 0.729) compared to the model including CDC (r2 = 0.481) (Table 2, Figure 2A and B).
| Factor | Univariable | Multivariable 1 | Multivariable 2 | |||
| Coefficient | P value | Coefficient | P value | Coefficient | P value | |
| CCI | 5.27 (3.86-6.68) | < 0.001 | 5.96 (4.14-7.77) | < 0.001 | - | - |
| CDC | 5.01 (3.41-6.61) | < 0.001 | - | - | 5.37 (3.36-7.39) | < 0.001 |
| Age | 0.08 (-0.34 to 0.50) | 0.709 | -0.27 (-0.78 to 0.25) | 0.309 | -0.22 (-0.77 to 0.33) | 0.436 |
| BMI | 0.06 (-0.91 to 1.03) | 0.904 | -0.11 (-0.95 to 0.74) | 0.802 | -0.01 (-0.91 to 8.91) | 0.985 |
| Female (compared to male) | 4.18 (-2.46 to 10.81) | 0.215 | 8.14 (1.39-14.89) | 0.019 | 7.91 (0.70-15.11) | 0.032 |
| Duration of diabetes | 0.241 (-0.10 to 0.58) | 0.166 | 0.26 (-0.12 to 0.64) | 0.171 | 0.31 (-0.10 to 0.71) | 0.134 |
| Macrovascular1 | 4.90 (-1.64 to 11.45) | 0.141 | 7.82 (1.25-14.38) | 0.020 | 8.19 (1.20-15.19) | 0.022 |
| Dyslipidemia | -3.83 (-10.64 to 2.99) | 0.269 | -2.20 (-10.45 to 6.05) | 0.597 | -3.31 (-12.08 to 5.46) | 0.454 |
| Hypertension | -3.16 (-11.73 to 5.42) | 0.467 | -1.67 (-15.43 to 12.09) | 0.810 | -1.13 (-15.81 to 13.54) | 0.878 |
This is the first study comparing the differences between CDC and the CCI in quantifying post-operative LOS after SPK. Whilst both scores were associated with prolonged LOS, we have showed that the CCI has a significantly stronger association with LOS than the conventional CDC. This finding suggests that it is advisable to consider both the number and severity of complications in the evaluation of complications after SPK transplantation. According to multivariate linear analysis, cardiovascular events pre-transplant, together with female sex, were found to be independent predictors of longer LOS. However, the correlation between LOS and the two classification scores remained relevant even following adjusted analyses.
In our study, 38 (30.5%) patients had major complications (≥ CDC IIIa) with no post-operative mortality. These results appear to be slightly better than previously reported in literature[3,7,8]. The reasons behind these differences might be multifactorial. Troppmann et al[3] demonstrated an overall early laparotomy (defined as relaparotomy done during the first 3 months posttransplant, or during the initial pancreas transplant hospital stay if it exceeded 3 months) of 36% among 236 recipients. This study was conducted before the introduction of tacrolimus, advanced IS induction drugs, such as anti-CD25 and improvement in medical and surgical management of these patients. These differences could have played a role when evaluating the number of major complications. Two other studies[7,8] reported a major complication rate exceeding 50%, but the number of cases is overall modest therefore no robust conclusions could be drawn. Both CDC and CCI performed well in predicting LOS in this study, with the CCI showing a better correlation. This superiority might be better understood by the fact that each patient might develop more than one complication following SPK. In fact, several CDC grade I/II or multiple laparotomies are frequent in SPK[3,7,8] and this is corroborated by the fact that almost one quarter of patients (n = 30, 23.4%) in our cohort developed more than one postoperative complication. In this regard, the progressive cumulative scoring of the CCI had a stronger link to LOS, highlighting the importance of evaluating the severity as well as the frequency of each complication grade per patient. However, calculating the CCI entails a detailed and thorough review of all patients records, including minor (CDC I/II) complications which are not routinely recorded in most of the databases. Consequently, the amount of work could be labor-intensive and not widely available. Nevertheless, we support the utilization of CCI for future studies as it represents an easily availably and reliable tool to evaluate the overall burden of post-operative complications in SPK. Its cumulative scoring could be useful to assess the relation with other relevant clinical outcomes such as quality of life, graft survival, and long-term morbidity which we were unable to analyze in this study due to the relatively small number of patients. At multivariable analysis we found that female sex and patients with cardiovascular events pre-transplant, such as myocardial infarction, cerebrovascular event, peripheral vascular disease, had significantly longer LOS. While it is easy to understand the reasons behind longer LOS in patients who had a previous cardiovascular event, the association between female sex and longer LOS is not clear. However, there were only 20 female recipients in the complication group and given these small numbers it is difficult to draw robust conclusions, and therefore the clinically significance remains uncertain. A number of studies evaluated the comparison between CDC and CCI, to assess which complication index performs best in predicting outcomes after surgery[9-15]. These have been focusing mainly on surgical oncology major operations, such as hyperthermic intraperitoneal chemotherapy, gastrectomy for gastric cancer, esophagectomy, pancreatic surgery, urology and retroperitoneal sarcoma. All studies reported that the CCI was superior to CDC in evaluating post-operative outcomes. Overall, these results are in line with ours, underlying the relevance of using the CCI in various major surgeries, including SPK.
The present study has several limitations which need to be acknowledged when interpreting its results. Firstly, due to the retrospective nature of our study, some data might have been inherently lost. This is likely to have introduced some bias, as there could be other unmeasured complications which would result in confounding. Secondly, this study makes the underlying assumption that all patients are discharged when deemed appropriate by the physicians, using criteria from the same center adopting similar discharge policies. However, some other circumstances not related to the clinical setting (e.g., distance from home, patients’ social status, availability of post-discharge home care) could have influenced the decision-making processes during discharge, thus artificially introducing biases when evaluating the LOS. It was not possible to record in our database such information and this poses an additional limitation to our study. Thirdly, our cohort is based on a single center data in a span period of 20 years which potentially could have causes selection bias due to improvement in medical and surgical management throughout the years. Finally, the results of this study are based on data from a single center in Canada, thus the findings might not be generalizable to other population or countries, particularly those where healthcare system and population demographics differ considerably from Canada.
In summary, the present study has demonstrated that both CDC and CCI scores resulted in high correlation with LOS after SPK transplant, with a superiority of the CCI due to its cumulatively scoring. It appears that the calculation of CCI in patients undergoing SPK is a feasible and useful tool, therefore, its utilization should be encouraged to quantify the total burden of postoperative complications after SPK for future research. Whilst we advocate the utilization of CCI for patients undergoing SPK due to its more sensitive correlation with LOS, additional multicenter studies are required to corroborate our results.
| 1. | Dean PG, Kukla A, Stegall MD, Kudva YC. Pancreas transplantation. BMJ. 2017;357:j1321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 96] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 2. | Kandaswamy R, Stock PG, Miller JM, White J, Booker SE, Israni AK, Snyder JJ. OPTN/SRTR 2021 Annual Data Report: Pancreas. Am J Transplant. 2023;23:S121-S177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 24] [Reference Citation Analysis (0)] |
| 3. | Troppmann C, Gruessner AC, Dunn DL, Sutherland DE, Gruessner RW. Surgical complications requiring early relaparotomy after pancreas transplantation: a multivariate risk factor and economic impact analysis of the cyclosporine era. Ann Surg. 1998;227:255-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 153] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 4. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 26150] [Article Influence: 1188.6] [Reference Citation Analysis (2)] |
| 5. | Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA. The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg. 2013;258:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 764] [Cited by in RCA: 1434] [Article Influence: 110.3] [Reference Citation Analysis (0)] |
| 6. | AssesSurgery GmbH. Home of AssesSurgery. [cited 19 December 2024]. Available from: http://www.assessurgery.com/calculator_single. |
| 7. | Michalak G, Czerwiński J, Kwiatkowski A, Danielewicz R, Kosieradzki M, Lisik W, Chmura A, Lao M, Durlik M, Wałaszewski J, Rowiński W. Surgical complications observed in simultaneous pancreas-kidney transplantation: thirteen years of experience of one center. Transplant Proc. 2002;34:661-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Khubutia MS, Pinchuk AV, Dmitriev IV, Balkarov AG, Storozhev RV, Anisimov YA. Surgical complications after simultaneous pancreas-kidney transplantation: A single-center experience. Asian J Surg. 2016;39:232-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Slaman AE, Lagarde SM, Gisbertz SS, van Berge Henegouwen MI. A Quantified Scoring System for Postoperative Complication Severity Compared to the Clavien-Dindo Classification. Dig Surg. 2015;32:361-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Dumitra S, O'Leary M, Raoof M, Wakabayashi M, Dellinger TH, Han ES, Lee SJ, Lee B. The Comprehensive Complication Index: a New Measure of the Burden of Complications After Hyperthermic Intraperitoneal Chemotherapy. Ann Surg Oncol. 2018;25:688-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Kim TH, Suh YS, Huh YJ, Son YG, Park JH, Yang JY, Kong SH, Ahn HS, Lee HJ, Slankamenac K, Clavien PA, Yang HK. The comprehensive complication index (CCI) is a more sensitive complication index than the conventional Clavien-Dindo classification in radical gastric cancer surgery. Gastric Cancer. 2018;21:171-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 84] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 12. | Ricci C, Ingaldi C, Grego DG, Alberici L, De Raffele E, Pagano N, Mosconi C, Di Marco M, Palloni A, Brandi G, Minni F, Casadei R. The use of comprehensive complication Index® in pancreatic surgery: a comparison with the Clavien-Dindo system in a high volume center. HPB (Oxford). 2021;23:618-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Tirotta F, Parente A, Hodson J, Desai A, Almond LM, Ford SJ. Cumulative Burden of Postoperative Complications in Patients Undergoing Surgery for Primary Retroperitoneal Sarcoma. Ann Surg Oncol. 2021;28:7939-7949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (1)] |
| 14. | Tirotta F, Parente A, Richardson T, Almonib A, Evenden C, Max Almond L, Desai A, Hodson J, Ford SJ. Comparison of comprehensive complication index and Clavien-Dindo classification in patients with retroperitoneal sarcoma. J Surg Oncol. 2021;124:1166-1172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Geiger S, Kocher N, Illinsky D, Xylinas E, Chang P, Dewey L, Wagner AA, Petros F, Matin SF, Tobert C, Tracy C, Patard PM, Roumiguie M, Monteiro LL, Kassouf W, Raman JD. Comparison of the Comprehensive Complication Index and Clavien-Dindo systems in predicting perioperative outcomes following radical nephroureterectomy. Transl Androl Urol. 2020;9:1780-1785. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/