Published online Mar 22, 2016. doi: 10.5498/wjp.v6.i1.143
Peer-review started: September 6, 2015
First decision: October 27, 2015
Revised: November 19, 2015
Accepted: January 5, 2016
Article in press: January 7, 2016
Published online: March 22, 2016
Processing time: 200 Days and 12.2 Hours
AIM: To provide a comprehensive overview of clinical studies on the clinical picture of Internet-use related addictions from a holistic perspective. A literature search was conducted using the database Web of Science.
METHODS: Over the last 15 years, the number of Internet users has increased by 1000%, and at the same time, research on addictive Internet use has proliferated. Internet addiction has not yet been understood very well, and research on its etiology and natural history is still in its infancy. In 2013, the American Psychiatric Association included Internet Gaming Disorder in the appendix of the updated version of the Diagnostic and Statistical Manual for Mental Disorders (DSM-5) as condition that requires further research prior to official inclusion in the main manual, with important repercussions for research and treatment. To date, reviews have focused on clinical and treatment studies of Internet addiction and Internet Gaming Disorder. This arguably limits the analysis to a specific diagnosis of a potential disorder that has not yet been officially recognised in the Western world, rather than a comprehensive and inclusive investigation of Internet-use related addictions (including problematic Internet use) more generally.
RESULTS: The systematic literature review identified a total of 46 relevant studies. The included studies used clinical samples, and focused on characteristics of treatment seekers and online addiction treatment. Four main types of clinical research studies were identified, namely research involving (1) treatment seeker characteristics; (2) psychopharmacotherapy; (3) psychological therapy; and (4) combined treatment.
CONCLUSION: A consensus regarding diagnostic criteria and measures is needed to improve reliability across studies and to develop effective and efficient treatment approaches for treatment seekers.
Core tip: Internet addiction has appeared as new mental health concern. To date, reviews have focused on clinical and treatment studies of Internet addiction and Internet Gaming Disorder, limiting the analysis to a specific diagnosis of a potential disorder that has not yet been officially recognised, rather than a comprehensive investigation of Internet-use related addictions (including problematic Internet use) more generally. This systematic literature review outlines and discusses the current empirical literature base for clinical studies of Internet addiction and problematic Internet use. A total of 46 relevant studies on treatment seeker characteristics, psychopharmacotherapy, psychological therapy, and combined treatment were identified.
- Citation: Kuss DJ, Lopez-Fernandez O. Internet addiction and problematic Internet use: A systematic review of clinical research. World J Psychiatr 2016; 6(1): 143-176
- URL: https://www.wjgnet.com/2220-3206/full/v6/i1/143.htm
- DOI: https://dx.doi.org/10.5498/wjp.v6.i1.143
Over the last 15 years, the number of Internet users has increased by 1000%[1], and at the same time, research on addictive Internet use has proliferated. Internet addiction has not yet been understood very well, and research on its etiology and natural history is still in its infancy[2]. Currently, it is estimated that between 0.8% of young individuals in Italy[3] and 8.8% of Chinese adolescents[4] are affected. The reported higher prevalence rates in China suggest Internet addiction is a serious problem in China, and the country has acknowledged Internet addiction as official disorder in 2008[5].
A comprehensive systematic review of epidemiological research of Internet addiction for the last decade[6] indicated Internet addiction is associated with various risk factors, including sociodemographic variables (including male gender, younger age, and higher family income), Internet use variables (including time spent online, using social and gaming applications), psychosocial factors (including impulsivity, neuroticism, and loneliness), and comorbid symptoms (including depression, anxiety, and psychopathology in general), suggesting these factors contribute to an increased vulnerability for developing Internet-use related problems. Despite the gradually increasing number of studies concerning Internet addiction, classification is a contentious issue as a total of 21 different assessment instruments have been developed to date, and these are currently used to identify Internet addiction in both clinical and normative populations[6]. Conceptualisations vary substantially and include criteria derived from pathological gambling, substance-related addictions and the number of problems experienced. In addition to this, the cut-off points utilised for classification differ significantly, which impedes research and cultural cross-comparisons and limits research reliability.
Increasing research efforts on Internet addiction have led the American Psychiatric Association (APA) to include Internet Gaming Disorder in the appendix of the updated version of the Diagnostic and Statistical Manual for Mental Disorders (DSM-5) in 2013 as condition that requires further research before it can be accepted for inclusion in the main manual[7]. This has resulted in researchers commencing efforts to reach an international consensus for assessing Internet Gaming Disorder using the new DSM-5 approach based on an international expert panel[8]. However, various limitations to this recently proposed “consensus” have been identified, including the lack of a representative international community of experts in the field, the voting method used to arrive at the consensus, the criteria and nosology identified, lack of critical measurement of the disorder and lack of field testing[9]. For the purpose of a comprehensive and inclusive understanding of the potential disorder, in this systematic literature review, Internet addiction will be referred to as encompassing Internet-use related addictions and problematic Internet use, including Internet Gaming Disorder. It is argued that until this concept is understood more fully (including nosology, etiology and diagnostic criteria), limiting our understanding of Internet-use related addictions to Internet gaming-related problems does neither pay sufficient respect to the affected individuals’ personal experience nor to the variety of online behaviours that can be engaged in excessively online. For example, other potential online addictions and Internet-use related disorders have been recently reviewed[10], suggesting that limiting a diagnosis to online gaming exclusively misses out many cases of individuals who experience negative consequences and significant impairment due to their Internet use-related behaviours.
For some individuals, their online behaviours are problematic and they require professional help as they cannot cope with their experiences by themselves, suggesting treatment is necessary. Based on in-depth interviews with 20 Internet addiction treatment experts from Europe and North America, Kuss and Griffiths[11] found that in inpatient and outpatient clinical settings, Internet addiction and Internet-use related problems are associated with significant impairment and distress for individuals, which have been emphasised as the criteria demarcating mental disorders[12]. This suggests that in the clinical context, Internet addiction can be viewed as mental disorder requiring professional treatment if the individual presents with significant levels of impairment. Psychotherapists treating the condition indicate the symptoms experienced by the individuals presenting for treatment appear similar to traditional substance-related addictions, including salience, mood modification, tolerance, withdrawal, conflict and relapse[11]. This view is reflected by patients who seek treatment for their excessive gaming[13].
In 2002, the South Korean government-funded National Information Society Agency has opened the first Internet addiction prevention counselling centre worldwide, and has since developed large-scale projects (including prevention, training, counselling, treatment, and policy formulation) to tackle the pervasive problem of technology overuse[14]. Across the United States and Europe, Internet addiction treatment is not funded by the government, often leaving individuals seeking help either for other primary disorders or through private organisations, although new clinical centres that specialise in treating Internet-use related problems are being developed[15]. Based on the available evidence, recent research furthermore suggests that the best approach to treating Internet addiction is an individual approach, and a combination of psychopharmacotherapy with psychotherapy appears most efficacious[16].
To date, reviews have focused on clinical and treatment studies of Internet addiction[16-19] and Internet Gaming Disorder[2]. This arguably limits the analysis to a specific diagnosis of a potential disorder that has not yet been officially recognised in the Western world, rather than a comprehensive and inclusive investigation of Internet-use related addictions (including problematic Internet use) more generally. Previous reviews relied on overly restrictive inclusion criteria, and this has led to ambiguities in the conceptualisation of the problem, and consequently resulted in limitations regarding both validity and reliability. In order to overcome these problems, the aim of this literature review is to provide a comprehensive overview of clinical studies on the more inclusive clinical picture of Internet-use related addictions from a holistic perspective.
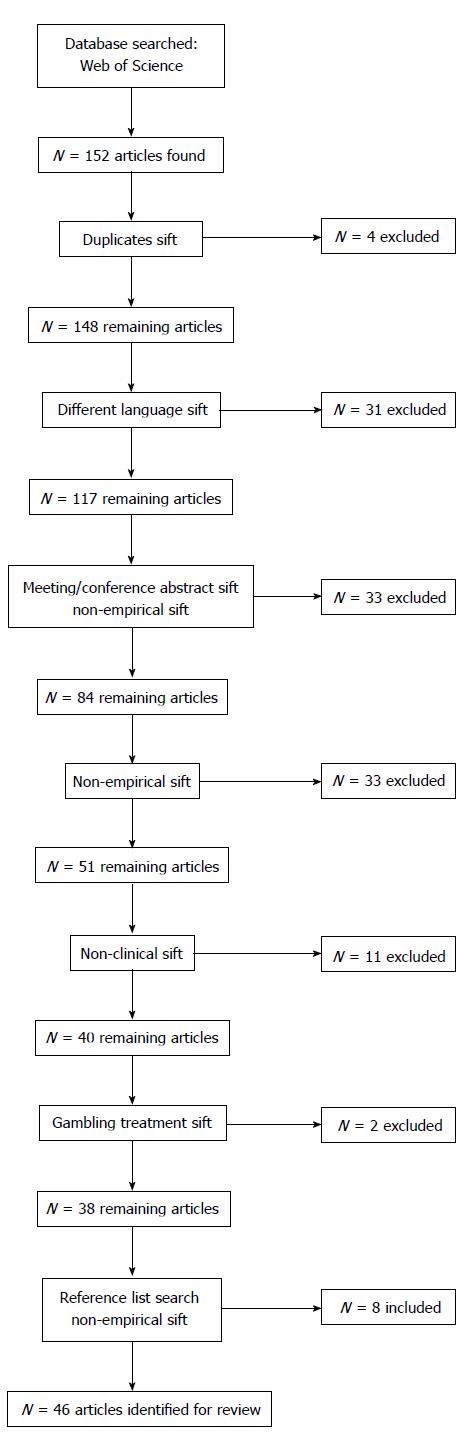
Between July and August 2015, a literature search was conducted using the database Web of Science. This database is more comprehensive than other commonly used databases, such as PsycINFO or PubMed because it includes various multidisciplinary databases. The following search terms (and their derivatives) were entered: “Internet addict*”, “Internet gaming addiction”, “gaming addiction”, “Internet Gaming Disorder”, “compuls* Internet use”, “compuls* gam*”, “pathological Internet use”, “excessive internet use”, or “problematic Internet use”, and “clinic*”, “diagnos*”, “treat*, “therap*”, or “patient*”. Studies were selected based on the following inclusion criteria. Studies had to (1) contain quantitative empirical data; (2) have been published after 2000; (3) include clinical samples and/or clinical interventions for Internet and/or gaming addiction; (4) provide a full-text article (rather than a conference abstract); and (5) be published in English, German, Polish, Spanish, Portuguese, or French as the present authors speak these languages. The initial search yielded 152 results. Following a thorough inspection of the articles’ titles and abstracts, the articles that did not meet the inclusion criteria were excluded. The search strategy is presented in Figure 1.
Additional articles were identified through searching the citations in the literature selected, resulting in the inclusion of another eight studies[20-27].
A total of 46 studies met the inclusion criteria. These studies are presented in Table 1. The included studies used clinical samples, and focused on characteristics of treatment seekers and online addiction treatment. Four main types of clinical research studies were identified, namely research involving (1) treatment seeker characteristics; (2) psychopharmacotherapy; (3) psychological therapy; and (4) combined treatment. The results section will outline each of these.
| Study | Aims | Sample and design | Treatment approach | Instruments | Results |
| Atmaca[28] | To describe a case of problematic Internet use successfully treated with an SSRI-antipsychotic combination | Case report | SSRI-antipsychotic combination: Citalopram 20 mg/d increased to 40 mg/d within 1 wk, continued for 6 wk; then quetiapine (50 mg/d) added and increased to 200 mg/d within 4 d | SCID-IV to assess Axis I psychiatric comorbidity[29] | Y-BOCS score decreased from 21 to 7 after treatment |
| n = 1 male 23-yr old single 4th year medical student | YBOCS[30,31] | Nonessential Internet use decreased from 27 to 7 h/wk; essential Internet use decreased from 4.5 to 3 h/wk | |||
| Improvement maintained at 4 mo follow-up with the same medication | |||||
| Bernardi et al[32] | To describe a clinical study of individuals with Internet addiction, comorbidities and dissociative symptoms | n = 50 adult outpatients self-referred for internet overuse in Italy (age M = 23.3, SD = 1.8 yr) | N/A | Youngs Internet Addiction Scale IAS[33] | Clinical diagnoses included 14% ADHD, 7% hypomania, 15% generalized anxiety disorder, 15% social anxiety disorder; 7% dysthymia, 7% obsessive compulsive personality disorder, 14% borderline personality disorder, and 7% avoidant personality disorder, 2% binge eating disorder |
| 9 women and 6 men scored ≥ 70 on Internet Addiction Scale; 19 with “possible Internet addiction” (scoring 40-69 on IAT) | Clinical interview | ||||
| DES[34] | |||||
| CGI[35] | |||||
| Sheehan Disability Scale[36] | |||||
| Structured Clinical Interviews for DSM-IV (SCID I and II)[37,38] | IAD associated with higher perception of family disability and higher Yale-Brown Obsessive Compulsive Severity score | ||||
| Hamilton Rating Scale for Depression[39] | Scores for the Dissociative Experience Scale were higher than expected and related to higher obsessive compulsive scores, hours per week on the Internet, and perception of family disability | ||||
| Hamilton Rating Scale for Anxiety[40] | |||||
| Liebowitz Social Anxiety Scale[41] | |||||
| YBOCS[30] | |||||
| CAARS:S[42] | |||||
| Beutel et al[43] | To present the assessment and clinical characterisation of individuals seeking help for computer and Internet addiction via a telephone hotline | N = 346 phone consultations (85.8% relatives, 14.2% persons affected) | Telephone consultations | Skala zum Computerspielverhalten [CSV-S (Scale for the Assessment of Pathological Computer Gaming)][44] | Consultation mainly sought by relatives (86% mothers) |
| 48% reported achievement failure and social isolation, lack of control (38%), family conflicts (33%) | |||||
| n = 131 patients (M = 21.9, SD = 6.6, range 13-47 yr, 96.2% male) | First diagnostic interview with expert clinicians | Symptom-Checklist SCL-90-R[45] | 96% of patients (n = 131) met criteria for pathological computer gaming | ||
| Specialised clinic for behavioural addictions in Germany | |||||
| Bipeta et al[46] | To compare control subjects with or without Internet addiction with patients with pure obsessive compulsive disorder with or without Internet addiction | n = 34 control subjects with or without Internet addiction (age M = 26.9, SD = 6.6 yr) | OCD patients treated for 1 year with standard pharmacological treatment for OCD (TAU), received clonazepam, tapered off in three weeks, and an SSRI or clomipramine | Youngs Diagnostic Questionnaire[47] | 11 OCD patients (28.95%) diagnosed with IA compared to 3 control subjects |
| n = 38 patients with obsessive compulsive disorder with or without Internet addiction (age M = 27.0, SD = 6.1 yr) | IA OCD group: 5 received 150-200 mg fluvoxamine/d, 4 received 150-200 mg sertraline/d, 1 received 60 mg fluoxetine/d, 1 received 200 mg clomipramine/d | IAT[48] | OCD group, no difference in OCD scores btw IA/OCD and non-IA/OCD groups | ||
| Non-IA OCD group: 8 received 150-300 mg fluvoxamine/d, 5 received 100-200 mg sertraline/d, 11 received 40-80 mg fluoxetine/d, 3 received 150-200 mg clomipramine/d | Diagnostic and Statistical Manual of Mental Disorders, DSM-IV (psychiatric interview)[12] | IA scores higher in IA/OCD group | |||
| BIS-11[49] | Treatment improved test scores | ||||
| YBOCS[30] | At 12 mo, 2/11 patients with OCD fulfilled IA criteria | ||||
| Claes et al[50] | To investigate the association among CB, CIU, and reactive/regulative temperament in patients with ED | n = 60 female patients with eating disorders in the Netherlands (38.3% with Anorexia nervosa, 6.7% with Anorexia binging-purging type, 26.7% with bulimia nervosa, and 28.3% with Eating Disorder not otherwise specified; age range 15-57 yr, mean age = 27.8, SD = 9.8 yr) | N/A | DSM-IV, standardised clinical interview[51] | Positive association btw CB and CIU, emotional lability, excitement seeking, lack of effortful control (lack of inhibitory and lack of activation control) |
| EDI-2[52,53] | 11.7% of CB patients with IA | ||||
| CBS[54] | No significant differences between ED subtypes regarding CIU | ||||
| Dutch Compulsive Internet Use Scale[55] | |||||
| BIS/BAS scales[56,57] | |||||
| DAPP[58,59] | |||||
| Adult Temperament Questionnaire-Short Form[60,61] | |||||
| Cruzado Díaz et al[62] | To describe clinical and epidemiological characteristics of inpatients in a clinical centre in Perú between 2001-2006 | n = 30 patients with “IA“ 90% devoted themselves to online games) in Perú | N/A | Reviewed 30 clinical registers through FEIA[63], a semi-structured instrument for psychiatric evaluation applied to clinical histories | Patient characteristics: |
| Young age (18.3 ± 3.8 yr old) | |||||
| All single males from 13 to 28 yr old (M = 18.3, SD = 3.8), 63.3% with secondary education completed and 66.7% dropped out | Patients completed a brief survey through an interview regarding information about their Internet use and online behaviours | Extensive daily Internet use (50% remained online for more than 6 h/d) | |||
| Descriptive, retrospective and transversal study | Primary Internet use: Online gaming (43.3% excessive gaming and 6.7% excessive gambling) | ||||
| Comorbidities (DSM-IV): High frequency of psychopathic behaviours (antisocial personality traits: 40%), 56.7% affective disorders (30% major depression and 26.7% dysthymia), 26.7% other addictions (13.3% gambling, 10% alcohol, 10% marihuana, 6.7% nicotine and 3.3% cocaine), 16.7% antisocial disorders (13.3% ADHD, social phobia 10% and 3.3% dysmorphic corporal disorder) | |||||
| DellOsso et al[20] | To assess the safety and efficacy of escitalopram in IC-IUD using a double-blind placebo-controlled trial | n = 19 adult subjects (12 men, mean age = 38.5, SD = 12.0 yr) with IC-IUD (as primary disorder) | Escitalopram started at 10 mg/d, increased and maintained at 20 mg/d for 10 wk | Structured Clinical Interview for DSM-IV Axis I[64] | Following double-blind phase, there were no significant differences in weekly non-essential Internet use and overall clinical response between treatment and placebo group |
| 19 wk prospective trial with 2 consecutive phases: 10 wk treatment phase (n = 17, 11 men, mean age = 37.5, SD = 12.0 yr = and 9 wk randomised double-blind placebo controlled trial (n = 14, 10 men, mean age = 40.0, SD = 11.5 yr) | Subsequently, participants randomly assigned to placebo or escitalopram for 9 wk | Time spent in non-essential Internet use (hours/wk) | |||
| CGI-I[35] | Side effects: Fatigue and sexual side effects in treatment, but not placebo group | ||||
| BIS[49] | |||||
| IC-IUD version of YBOCS[30] | |||||
| Du et al[65] | To evaluate the therapeutic effectiveness of group CBT for Internet addiction in adolescents | n = 56 adolescents with IA (age range 12-17 yr) | Group cognitive behavioural therapy: | Beards Diagnostic Questionnaire for Internet addiction[66] | Internet use decreased in both groups |
| n = 32 active treatment group (28 male, mean age = 15.4, SD = 1.7 yr) | Active treatment group: 8 1.5-2 h sessions of multimodal school-based group CBT with 6-10 students/group run by two child and adolescent psychiatrists (topics: Control, communication, Internet awareness, cessation techniques); group CB parent training; psychoeducation delivered to teachers | Internet Overuse Self-Rating Scale[67,68] | Only treatment group had improved time management skills and better emotional, cognitive and behavioural symptoms | ||
| Time Management Disposition Scale[69] | |||||
| Strength and Difficulties Questionnaire (Chinese edition)[70] | |||||
| n = 24 clinical control group (17 male, mean age = 16.6, SD = 1.2 yr) | Clinical control group: No intervention | SCARED[71] | |||
| Dufour et al[72] | To describe the sociodemographic characteristics of Internet addicts in a CDR, and to document their problems associated with other dependencies (alcohol, drugs, game practices), self-esteem, depression and anxiety | n = 57 Internet addiction treatment seekers (88.4% males, 11.6% females; age range = 18-62 yr (M = 30.5, SD = 11.8 yr). | N/A | IAT[48,73] | 88% of Internet addicts were male, with a mean age of 30, living with their parents with low income |
| Canada | Becks Anxiety inventory[74] | M = 65 h of Internet use per week: 57.8% MMORPGs, 35,1% video streaming, and 29.8% chat rooms | |||
| Becks Depression inventory[75] | Rosenberg test: 66.6% weak and very weak self-esteem; Depression in only 3.5% and anxiety in 7.5% | ||||
| DÉBA-Alcohol/Drugs/Gaming[76] | 45.6% received pharmacological treatment for mental disorders (psychotropic) and 33.3% had a chronic physical problem | ||||
| Self-esteem[77] | |||||
| Duven et al[78] | To investigate whether an enhanced motivational attention or tolerance effects are reported by patients with IGD | n = 27 male clinical sample from specialised behavioural addiction centre in Germany (n = 14 with IGD, n = 13 casual computer gamers) | N/A | AICA-S[44] | Attenuated P300 for patients with IGD in response to rewards relative to a control group |
| Semi-natural EEG designed with participants playing a computer game during the recording of event-related potentials to assess reward processing | SCL-90-R[45] | Prolonged N100 latency and increased N100 amplitude, suggesting tolerance during computer game play, and gaming reward attention uses more cognitive capacity in patients | |||
| Floros et al[79] | To assess the comorbidity of IAD with other mental disorders in a clinical sample | n = 50 clinical sample of college students presenting for treatment of IAD in Greece (39 males, mean age = 21.0, SD = 3.2 yr; 11 females, mean age = 22.6, SD = 4.5 yr) | N/A | OCS[80] | 25/50 presented with comorbidity of another Axis I disorder (10% with major depression, 5% with dysthymia and psychotic disorders, respectively), and 38% (19/50) with a concurrent Axis II personality disorder (22% with narcissistic, and 10% with borderline disorder) |
| DSQ[81] | |||||
| ZKPQ[82,83] | |||||
| SCL-90[84,85] | |||||
| Cross-sectional study | The majority of Axis I disorders (51.85%) were reported before IAD onset, 33.3% after onset | ||||
| Ge et al[86] | To investigate the association between P300 event-related potential and IAD | n = 41 IAD subjects (21 males, age M = 32.5, SD = 3.2 yr) | CBT | Standard auditory oddball task using American Nicolet BRAVO Instrument | IA individuals had longer P300 latencies, but similar P300 amplitudes compared to controls |
| n = 48 volunteers (25 males, age M = 31.3, SD = 10.5 yr) | Following treatment, P300 latencies decreased significantly, suggesting cognitive function deficits associated with IAD can be ameliorated with CBT | ||||
| Experimental task | |||||
| Han and Renshaw[21] | To test whether bupropion treatment reduces the severity of EOP and MDD | n = 50 male subjects with EOP and MDD (aged 13-45 yr) | Random allocation to either bupropion and EDU group or placebo and EDU group | Structured Clinical Interview for DSM-IV[64] | During active treatment period, Internet addiction, gaming, and depression decreased relative to placebo group |
| n = 25 treatment group (mean age = 21.2, SD = 8.0 yr, range = 13-42) | 12-wk treatment (8 wk active treatment phase and 4-wk post treatment follow-up period) | Youngs Internet Addiction Scale[87,88] | During follow-up, bupropion-associated reductions in gaming persisted, while depressive symptoms recurred | ||
| n = 25 placebo group (mean age = 19.1, SD = 6.2 yr, range = 13-39) | |||||
| Randomised controlled double-blind clinical trial | 150 mg/d Bupropion SR given and increased to 300 mg/d during first week | Becks Depression Inventory[89] | |||
| Han et al[24] | To test the effects of bupropion sustained release treatment on brain activity for Internet video game addicts | n = 11 IAG (IAG; mean age = 21.5, SD = 5.6 yr; mean craving score = 5.5, SD = 1.0; mean playing time = 6.5, SD = 2.5 h/d; mean YIAS score = 71.2, SD = 9.4) | Placebo group started with one pill and then raised to two pills | Structured Clinical Interview for DSM-IV[64] | Bupropion sustained release treatment works for IAG in a similar way as it works for patients with substance dependence |
| n = 8 HC (HC; mean age = 11.8, SD = 2.1 yr; mean craving score = 3.9, SD = 1.1; mean Internet use = 1.9, SD = 0.6 h/d; mean YIAS score = 27.1, SD = 5.3) in South Korea | Buproprion sustained release treatment: 6 wk | Beck Depression Inventory[89] | During exposure to game cues, IAG had more brain activation in left occipital lobe cuneus, left dorsolateral prefrontal cortex, left parahippocampal gyrus relative to HC | ||
| Youngs Internet Addiction Scale[87] | |||||
| Experimental design | Participants underwent 6 wk of bupropion sustained release treatment (150 mg/d for first week, 300 mg/d afterwards) | Craving for Internet video game play: 7-point visual analogue scale | After treatment, craving, play time, cue-induced brain activity decreased in IAG | ||
| Brain activity measured at baseline and after treatment using 1.5 Tesla Espree fMRI scanner | |||||
| Han et al[22] | To assess the effect of methylphenidate on Internet video game play in children with ADHD | n = 62 children (52 males, mean age = 9.3, SD = 2.2 yr, range = 8.12), drug-naïve, diagnosed with ADHD, and Internet video game players in South Korea | Treatment with Concerta (OROS methylphenidate HCI, South Korea) | YIAS-K[87,88] | Following treatment, Internet addiction and Internet use decreased |
| Initial dosage: 18 mg/d, and maintenance dosage individually adjusted based on changes in clinical symptoms and weight | Korean DuPaul's ADHD Rating Scale[90,91] | ||||
| Changes in IA between baseline and treatment completion correlated with changes in ADHD, and omission errors from the Visual Continuous Performance Test | |||||
| Visual Continuous Performance Test using the Computerised Neurocognitive Function Test[92] | |||||
| Hwang et al[93] | To directly compare patients with IA to patients with AD regarding impulsiveness, anger expression, and mood | n = 30 patients with IA (mean age = 22.7, SD = 6.7 yr) | N/A | Korean version of Youngs IAT[48,94] | IA and AD groups showed lower agreeableness and higher neuroticism, impulsivity, and anger expression compared to the HC group (all related to aggression) |
| n = 30 patients with AD (mean age = 30.0, SD = 5.9 yr) | SCID[64] | Addiction groups had lower extraversion, openness to experience, and conscientiousness, were more depressive and anxious than HCs | |||
| n = 30 HCs (HCs, mean age = 25.3, SD = 2.8 yr) | Alcohol Use Disorder Identification Test-Korean version[95] | Severity of IA and AD positively correlated with these symptoms | |||
| Outpatient clinic in South Korea | Korean version of the NEO-PI-R[96,97] | ||||
| Korean version of the BIS-11[98,99] | |||||
| Korean version of the STAXI-K[100,101] | |||||
| Kim[23] | To examine the effect of a reality therapy (R/T) group counselling programme for Internet addiction and self-esteem | n = 25 university students in South Korea (20 males, mean age = 24.2 yr) | Treatment group (n = 13, 10 males): Participated in R/T group counselling programme, 2 60-90 min sessions/wk for 5 consecutive weeks (with the purpose of taking control and changing thinking and behaviours) | K-IAS[102] | Treatment programme reduced addiction level and increased self-esteem |
| CSEI[103] | |||||
| Randomised controlled trial/quasi- experimental design | |||||
| Control group (n = 12, 10 males): No treatment | |||||
| Kim et al[25] | To evaluate the efficacy of CBT combined with bupropion for treating POGP in adolescents with MDD | n = 65 adolescents with MDD and POGP in South Korea (aged 13-18 yr) | n = 32 CBT group (medication and CBT): 8 wk intervention; 159 mg bupropion/d for 1 wk, then 300 mg/d for 7 wk; participated in 8 session weekly group CBT; weekly 10 min interviews | BDI[89] | Internet addiction decreased and life satisfaction increased in CBT and medication group relative to medication only group, but no changes in depression |
| BAI[74] | |||||
| YIAS[87,88] | |||||
| Modified-School Problematic Behaviour Scale[104] | Anxiety increased in medicated group | ||||
| Prospective trial | n = 33 clinical control group (medication only, as above) | Modified Students Life Satisfaction scale[105] | |||
| Kim et al[106] | To investigate the value of Youngs IAT for subjects diagnosed with Internet addiction | n = 52 individuals presenting with Internet addiction at university hospital in South Korea (47 males; mean age = 21.7, SD = 7.1 yr, range: 11-38) | N/A | Clinical interview | Samples mean IAT score below cut-off (70) |
| Youngs IAT[107,108] | |||||
| Classification of IA severity via DSM-IV-TR[12] | IAT detected only 42% of sample as having Internet addiction | ||||
| No significant differences in IAT scores between mild, moderate and severe Internet addition found | |||||
| No association between IAT scores and Internet addiction duration of illness found | |||||
| IAT has limited clinical utility for evaluating IA severity | |||||
| Kim et al[109] | To compare patients with IGD with patients with AUD and HC regarding resting-state ReHo | n = 45 males seeking treatment in South Korea | N/A | Youngs IAT[87] | Significantly increased ReHo in PCC of the IGD and AUD groups |
| n = 16 IGD patients (mean age = 21.6, SD = 5.9 yr) | SCID[64] | Decreased ReHo in right STG of IGD, compared with AUD and HC groups | |||
| n = 14 AUD patients (mean age = 28.6, SD = 5.9 yr) | AUDIT-K[110] | Decreased ReHo in anterior cingulate cortex of AUD patients | |||
| n = 15 HCs (mean age = 25.4, SD = 5.9 yr) | BDI[89] | Internet addiction severity positively correlated with ReHo in medial frontal cortex, precuneus/PCC, and left ITC in IGD | |||
| BAI[74] | Impulsivity negatively correlated with ReHo in left ITC in IGD | ||||
| BIS-11[111] | Increased ReHo in PCC: Neurobiological feature of IGD and AUD | ||||
| FMRI resting data acquired via Philips Achieva 3-T MRI scanner using standard whole-head coil, obtaining 180 T2 weighted EPI volumes in each of 35 axial planes parallel to anterior and posterior commissures | Reduced ReHo in STG: Neurobiological marker for IGD specifically relative to AUD and HCs | ||||
| King et al[112] | To present a case study of an individual with GPIU | n = 1, 16-yr old male in Australia | N/A | N/A | PIU identified due to: (1) use of several different Internet functions; (2) social isolation; (3) procrastination and time-wasting tendencies |
| Case study | Problems unlikely to have occurred without the Internet | ||||
| Ko et al[113] | To evaluate the diagnostic validity of IGD criteria, and to determine the cut-off point for IGD in DSM-5 | n = 225 adults in Taiwan (n = 75 individuals with IGD (63 males, mean age = 23.4, SD = 2.6 yr), no IGD (63 males, mean age = 22.9, SD = 2.5 yr), and IGD in remission (63 males, mean age = 23.8, SD = 2.9 yr), respectively) | N/A | Diagnostic interview based on DSM-5 IGD criteria[7] | Diagnostic accuracy of DSM-5 IGD items between 77.3% and 94.7% (except for deceiving and escape), and differentiated IGD from remitted individuals |
| DC-IA-C[114] | Meeting ≥ 5 IGD criteria: Best cut-off point to differentiate IGD from non-IGD and remitted individuals | ||||
| Chinese version of the MINI[115] | |||||
| QGU-B[116] | |||||
| CIAS[117] | |||||
| Liberatore et al[118] | To describe the prevalence of IA in a clinical sample of Latino adolescents receiving ambulatory psychiatric treatment | n = 71 adolescent patients in Puerto Rico (39 males, aged 13-17 yr), 39.4% diagnosed with disruptive disorder, 31.0% with mood disorder, 19.7% with mood and disruptive disorder | N/A | Spanish version of the Internet Addiction Test (IAT)[87] | Sample did not involve any cases of severe IA |
| 71.8% of the sample had no IA problem | |||||
| 11.6% discussed Internet use with therapists | |||||
| IA correlated with mood disorders | |||||
| Liu et al[119] | To test the effectiveness and underlying MFGT | n = 92 (46 adolescents with 12-18 yr old, and 46 parents, aged 35-46 yr old) | MFGT is a new approach to treat Internet addiction (IA) behaviours that has not been tested before | Structured questionnaires at pre-test (T1), post-test (T2) and follow-up (T3): | Significantly decreased IA in EG at T2 and maintained in T3 (adolescents IA rate dropped from 100% at baseline to 4.8% after intervention, then remained at 11.1%) |
| 2 groups: 1 experimental (EG; MFGT adolescents and parents) and 1 control (CG; waiting-list similar adolescents and parents) | MFGT = group therapy for families, both adults and adolescents that have the same problem (IA) | Adolescents scales: | |||
| Significantly better reports in the EG from adolescents and parents compared with those in the CG | |||||
| Adolescent Pathological Internet Use Scale APIUS[120] | Underlying mechanism of less IA was partially explained by adolescent satisfaction of their psychological needs and improved parent-adolescent communication and closeness | ||||
| EG: Adolescents: 17 males and 4 females (age: M = 15, SD = 1.73); | Advantage: Peer group (support and learn from peer confrontation) | Parents scales: | |||
| Parents: 5 males and 16 females (age: M = 40.9, SD = 2.85) | Transference reactions occur within and between families | Closeness to Parents[121] | |||
| CG: Adolescents: 21 males and 4 females (age: M = 15.7, SD = 1.2); Parents: Idem to EG (no sign. Diff). | Parent-Adolescent Communication Scale[122] | ||||
| China | College Students Psychological Needs and Fulfillment Scale[123] | ||||
| Quasi-experimental design | |||||
| Müller et al[124] | To characterize German treatment seekers and to determine the diagnostic accuracy of a self-report scale for | n = 290 mostly male (93.8%) treatment seekers between 18 and 64 yr (M = 26.4, SD = 8.22) | Treatment of behavioural addictions | SCL-90R[125] | 71% met clinical IA diagnosis |
| PHQ[126] | Displayed higher levels of psychopathology, especially depressive and dissociative symptoms | ||||
| IA | Germany | Non-experimental design | GAD-7[127] | Half met criteria for one further psychiatric disorder, especially depression | |
| CDS-2[128] | Level of functioning decreased in all domains | ||||
| AICA-S showed | |||||
| AICA-S[129] | good psychometric properties and satisfying diagnostic accuracy (sensitivity: 80.5%; specificity: 82.4%) | ||||
| Müller et al[130] | To compare personality profiles of a sample of patients in different rehabilitation centres | IA group: 70 male patients with an addiction disorder that additionally met the criteria for IA; M =29.3 yr (SD = 10.66; range 16-64) | N/A | Computer game | Patients with comorbid IA can be discriminated from other patients by higher neuroticism and lower extraversion and lower conscientiousness |
| Non-experimental design | Addiction (AICA-S)[129] | ||||
| AD group: 48 male patients suffering from AD; M = 31.7 yr; SD = 9.18; range 17-65) | NEO-FFI[131] | After controlling for depressive symptoms, lower conscientiousness turned out to be a disorder-specific risk factor | |||
| Germany | BDI-II[132] | ||||
| Müller et al[133] | To evaluate the relationships between personality traits and IGD | n = 404 males aged 16 yr and above | N/A | AICA-S[44] | IGD associated with higher neuroticism, decreased conscientiousness and low extraversion |
| 4 groups: | Experimental design: Characteristics of people selected for assigning them to two groups, non-random allocation | The comparisons to pathological gamblers indicate that low conscientiousness and low extraversion in particular are characteristics of IGD | |||
| IGD group: 115 patients with IGD | AICA-C[134] | Etiopathological model proposed for addictive online gaming | |||
| Clinical CG: 74 controls seeking treatment for IGD, but not diagnosable | Berlin Inventory for Gambling[135] | ||||
| Gambling group: 115 gambling patients | NEO Five-Factor Inventory[131] | ||||
| Healthy CG: 93 individuals with regular or intense use of online games | |||||
| Germany | |||||
| Park et al[136] | To examine the effectiveness of treating an Internet-addicted young adult suffering from interpersonal problems based on the MRI interactional model and Murray Bowen's family systems theory | 1 family case study consisting of husband (age 50), wife (age 50), 2 sons (ages 22, 23), older son with Internet addiction and interpersonal problems | Comparative analysis method | Characteristics of the parents family of origin and dysfunctional communication pattern associated with interpersonal problems revealed by participants | |
| South Korea | Miles and Huberman's matrix and network[137] | Both the MRI model and Bowen's family systems theory produced effective treatments | |||
| Poddar et al[138] | To describe a pilot intervention using MET and CBT principles to treat IGD in an adolescent | n = 1 | Initial therapy session: Rapport building with patient, detailed interview, primary case formulation | IQ ESDST, | IGD due to child neglect and boredom, consolidated by subsequent negative reinforcements |
| 14-yr-old boy | Subsequent sessions: Psychoeducation, cost/benefit analysis of behaviour (motivation level improved) | BVMGT, and TAT | |||
| India | Progressive muscle relaxation because gaming urge accompanied by physiological/emotional arousal | IAT | Individual interventions encouraged as there are varied antecedents and consequences for IGD development | ||
| Case study | MET-CBT principles for IGD resulted in improvement | ||||
| Subsequently: Game addiction assessment, contract for behaviour modification (reduce gaming time, increase other activities) | Therapy terminated when gains had consolidated | ||||
| Tokens introduced as positive reinforcement | Good exam scores achieved | ||||
| Less time spent gaming on weekdays, but excess on weekends | Weekend gaming times reduced | ||||
| Patient recorded Thoughts, | IAT score reduced to 48 (from 83) | ||||
| Emotions and Behaviors (TE and B) contributing to gaming (result: Gaming due to boredom) | |||||
| Non-gaming behaviour reinforced via scooty rides | |||||
| Santos et al[139] | To describe a treatment of a patient with PD, OCD (both anxiety disorders) and IA involving pharmacotherapy and CBT and test its efficacy | Case report | Pharmacotherapy and CBT | Hamilton Anxiety Scale (HAMA-A)[40] | Treatment effective for anxiety and IA |
| n = 1 | CBT 1x/week for 10 wk | Hamilton Depression Scale (HAM-D)[39] | |||
| 24-yr-old Caucasian woman | Pharmacotherapy [clonazepam (0.5 mg) and sertraline (50 mg) once daily] | Chambless BSQ[140] | |||
| A patient with PD, OCD and IA | Both (pharmaco and CBT) started together | Bandelow PA[141] | |||
| Brazil | CBT focus: Teach patient how to deal with anxiety and internet use (i.e., breathing retraining with diaphragmatic breathing exercise, education about PD and OCD symptoms and internet use, time management, identifying PIU triggers, changing habits, cognitive restructuring, exposure and response prevention, social support promotion, building alternative activities, functional internet use promotion) | IAT | |||
| CGI[142] | |||||
| Senormanci et al[143] | To investigate the attachment styles and family functioning of patients with IA | n = 60 | N/A | IAT[48] | Patients with IA had higher BDI and higher attachment anxiety sub-scores on the ECR-r compared with those in the CG |
| 2 groups: | BDI[89] | ||||
| EG: 30 male patients with IA [age: M = 21.6 (18-20) yr] | Experiences in Close Relationships Questionnaire-r [144] | IA patients evaluated their family functioning as more negative and reported problems in every aspect addressed by the FAD | |||
| CG: 30 healthy males without IA | |||||
| Non-experimental | Family Assessment Device[145] | Scores on the FAD behaviour control, affective responsiveness, and problem-solving subscales (and on the FAD communication, roles, and general functioning subscales) significantly higher in patients compared with CG | |||
| Senormanci et al[146] | To determine the predictor effect of depression, loneliness, anger and interpersonal relationship styles for IA in patients diagnosed with IA | n = 40 male IA patients with at least 18-yr-old | N/A | IAT[48] | Duration of Internet use (hours/day) and STAXI anger in subscale predicted IA. Although the duration is not adequate for IA diagnosis, it predicts IA |
| Turkey | BDI[89] | It is helpful for clinicians to regulate the hours of Internet use for patients with excessive or uncontrolled internet use | |||
| STAXI[100] | |||||
| UCLA Loneliness Scale[147] | |||||
| IRSQ, subscale “Contributing and inhibiting styles”[148] | Psychiatric treatments for expressing anger and therapies focussing on emotion validation may be useful | ||||
| Shek et al[149] | To described an indigenous multi-level counselling programme designed for young people with IA problems based on the responses of clients | n = 59 | Indigenous multilevel counselling program designed to provide services for young people with Internet addictive behaviour in Hong Kong: | 3 versions of IA Young's assessment tools[150]: 10-item, 8-item and 7-item measures[151-153] | The outcome evaluation, pretest and posttest data showed IA problems decreased after joining programme |
| 58 male and 1 female | (1) Emphasis on controlled and healthy use of the Internet; (2) Understanding the change process in adolescents with Internet addiction behaviour; (3) Utilization of motivational interviewing model; (4) Adoption of a family perspective; (5) Multi-level counselling model; (6) Utilization of case work and group work | Goldberg's framework[154] | |||
| Most in early adolescence (aged 11-15 yr; n = 29) and late adolescence (aged 16-18 yr; n = 27), while 3 were over 18 | Chinese Internet Addiction Scale (CIA-Goldberg) | Slight positive changes in parenting attributes | |||
| China | Items for assessing beliefs and behaviours for using Internet: 7 items from Computer Use Survey[155] | Participants subjectively perceived the programme was helpful | |||
| 6 items from OCS[80] | |||||
| 6 items from Internet Addiction-Related Perceptions and Attitudes Seale[156] | |||||
| 2 items from IAD-Related Experience Scale[157] | |||||
| 33-item C-FAI developed[158] | |||||
| Chinese Purpose in Life Questionnaire[159] | |||||
| Chinese Beck Depression Inventory[160] | |||||
| Chinese Hopelessness Seale[161] | |||||
| Chinese Rosenberg Self-Esteem Seale[162] | |||||
| Tao et al[163] | To develop diagnostic criteria for IAD and to evaluate the validity of proposed diagnostic criteria for discriminating non-dependent from dependent Internet use in the general population | 3 stages: Criteria development and item testing; criterion-related validity testing; global clinical impression and criteria evaluation; | N/A | N/A: Authors developed the proposed Internet addiction diagnostic criteria, which have been one of the main sources for the APAs IGD criteria | Proposed Internet addiction diagnostic criteria: Symptom criterion (7 clinical IAD symptoms ), clinically significant impairment criterion (functional and psychosocial impairments), course criterion (duration of addiction lasting at least 3 mo, with at least 6 h of non-essential Internet use per day) and exclusion criterion (dependency attributed to psychotic disorders) |
| Stage 1: n = 110 patients with IA in SG, M = 17.9 SD = 2.9 yr (range: 12-30 yr), 91.8% (n = 101) males; 408 patients in IA in TG, M = 17.6, SD = 2.7 yr (range: 12-27 yr), 92.6% (n = 378) male; Stage 2: n = 405; Stage 3: n = 150 (M = 17.7, SD = 2.8, (92.7% males) | Diagnostic score of 2 + 1, where first 2 symptoms (preoccupation and withdrawal symptoms) and min. 1/5 other symptoms (tolerance, lack of control, continued excessive use despite knowledge of negative effects/affects, loss of interests excluding Internet, and Internet use to escape or relieve a dysphoric mood) was established | ||||
| China | Inter-rater reliability: 98% | ||||
| Te Wildt et al[164] | To examine the question whether the dependent use of the Internet can be understood as an impulse control disorder, an addiction or as a symptom of other psychiatric conditions | EG: n = 25 patients (76% male, M = 29.36 yr, SD = 10.76) | 2 groups matched: The EG and CG | Preliminary telephone interview to test inclusion criteria with Young's and Beard's IA criteria[48,66] | Compared to controls, patient group presented significantly higher levels of depression (BDI), impulsivity (BIS) and dissociation (DES) |
| CG: Matched for age (M = 29.48; SD = 9.56), sex (76% males) and school education, and similar level of intelligence | Non-experimental design | Statistical Clinical Interview for DSM-IV[64] | PIU shares common psychopathological features and comorbidities with substance-related disorders | ||
| German Internet Addiction Scale ISS[165] | |||||
| German version of the Barratt Impulsiveness Scale BIS[49] | Should be viewed as diagnostic entity in itself within a spectrum of behavioural and substance dependencies | ||||
| Derogatis Symptom Checklist (SCL-90-R)[166,167] | |||||
| BDI[89,168] | |||||
| DES[169,170] | |||||
| SOC[171,172] | |||||
| IIP-D[173,174] | |||||
| Tonioni et al[26] | To test whether patients with IA present different psychological symptoms, temperamental traits, coping strategies and relational patterns relative to patients with PG | Two clinical groups: | N/A | IAT[48] | IA and PG had higher scores than control group on depression, anxiety and global functioning |
| 31 IA patients (30 males) and 11 PG patients (10 males) and a control group (38 healthy subjects; 36 males) matched with the clinical groups for gender and age were enrolled | Hamilton Anxiety Rating Scale[40] | IA patients had higher mental and behavioural disengagement associated with an important interpersonal impairment relative to PG patients | |||
| Hamilton Depression Scale[39] | IA and PG groups used impulsive coping, and had socio-emotional impairment | ||||
| Global Assessment of Functioning[112] | |||||
| Snaith-Hamilton Pleasure Scale[175] | |||||
| Temperament and Character Inventory-Revised[176] | |||||
| Coping Orientation to Problems Experienced[177] | |||||
| Inventory of Parent and Peer Attachment[178] | |||||
| Tonioni et al[27] | To investigate psychopathological symptoms, behaviours and hours spent online in patients with IAD | n = 86: 21 clinical patients in hospital-based psychiatric IAD service (mean age=24, SD = 11 yr); 65 control subjects | N/A | Internet addiction interview[47] | IAD patients had significantly higher scores on IAT relative to controls |
| IAT[179] | Only item 7 (how often do you check your e-mail before something else that you need to do?) showed a significant inverse trend | ||||
| Symptom Checklist-90-Revised[125] | SCL-90-R anxiety and depression scores and IAT item 19 (How often do you choose to spend more time online over going out with others?) positively correlated with weekly online hours in IAD patients | ||||
| van Rooij et al[180] | To evaluate the pilot treatment for IA created for the Dutch care organization (to explore the possibility of using an existing CBT and MI based treatment programme (lifestyle training) from therapists experiences with 12 Internet addicts | n = 12 Internet addicts and n = 5 therapists treating them | Treatment: A manual-based CBT | Data sources: (1) Session Reports; (2) Case Review Meeting Minutes; (3) Questionnaires: | Therapists report programme (originally used for substance dependence and pathological gambling) fits problem of Internet addiction well |
| The Netherlands | Standard Lifestyle Training programme, a manual-based treatment programme[181,182] | Compulsive Internet Use Scale (CIUS)[55] | Interventions focused on controlling and reducing Internet use, and involved expanding (real life) social contacts, regaining proper daily structure, constructive use of free time, and reframing beliefs | ||
| Therapy combines CBT and MI[183,184] | Brief Situational Confidence questionnaire[187] | Therapist report: Treatment achieved progress for all 12 treated patients | |||
| Focuses on eliciting and strengthening motivation to change, choosing a treatment goal, gaining self-control, relapse prevention, and coping skills training[185,186] | Patient report: Satisfaction with treatment and behavioural improvements | ||||
| 10 outpatient sessions of 45 min each, with 7 of these taking place within a period of 10 wk, the remaining 3 within a period of 3 mo | |||||
| Each session: Introduction, evaluation of current status, discussing homework, explaining theme of the day, practicing a skill, receiving homework, and finally closing the session | |||||
| Wölfling et al[188] | To investigate whether IA is an issue in patients in addiction treatment | n = 1826 clients in impatient centres | N/A | Internet and Computer Game Addiction (AICA-S)[189,190] | Comorbid IA associated with higher levels of psychosocial symptoms, especially depression, obsessive-compulsive symptoms, and interpersonal sensitivity |
| Male patients meeting criteria for comorbid IA (EG; n = 71) compared with a matched control group of male patients treated for alcohol addiction without addictive Internet use (CG; n = 58) | Symptom Checklist 90R (SCL-90-R)[191] | ||||
| PHQ[126] | IA patients meet criteria for additional mental disorders more frequently and display higher rates of psychiatric symptoms, especially depression, and might be in need of additional therapeutic treatment | ||||
| GAD-7[127] | |||||
| Germany | |||||
| Wölfling et al[192] | To test the effects of a standardized CBT programme for IA | n = 42 patients with IA, all male from 16-yr-old (M = 26.1, SD = 6.60, range: 18-47) | Short-Term outpatient Treatment for Internet and Computer Game | Inclusion criteria: | 70.3% of patients completed therapy |
| Addiction STICA (127) based on CBT techniques known from treatment programmes of other forms of addictive behaviour, consisting of 15 group sessions and additional 8 individual therapy sessions | AICA-S[193,194] | After treatment, symptoms of IA decreased significantly | |||
| Standardized clinical interview of IA (AICA-C; Checklist for the Assessment of Internet and Computer Game Addiction)[132] | Psychopathological symptoms and associated psychosocial problems decreased | ||||
| Individual sessions dealt with individual contents; group sessions followed clear thematic structure: First third of programme: Main themes about development of individual therapy aims, identification of Internet application associated with symptoms of IA, conducting holistic diagnostic investigation of psychopathological symptoms, deficits, resources, and comorbid disorders | GSE[195] | ||||
| NEO Five-Factor Inventory[131] | |||||
| Symptom Checklist 90R[196] | |||||
| Motivational techniques applied to enhance patients intention to cut down dysfunctional behaviour | |||||
| Second third: Psychoeducation elements; deepened Internet use behaviour analysis (focusing on triggers and patient reactions on cognitive, emotional, psychophysiological, and behavioural levels in that situation (SORKC scheme)[193] for development of a personalized model of IA for each patient based on interaction between online application, predisposing and maintaining factors of the patient (e.g., personality traits) and the patients social environment | |||||
| Last stage: Situations with heightened craving for getting online further specified and strategies to prevent relapse developed | |||||
| Wölfling et al[197] | To investigate the occurrence of BSD in patients with excessive Internet use and IA | n = 368 treatment seekers with excessive to addictive Internet use screened for bipolar spectrum disorders | N/A | AICA-S[194] | Comorbid BSD more frequent in patients meeting criteria for IA (30.9%) than among excessive users (5.6%) |
| Germany | BSD assessed using MDQ[198] | This subgroup showed heightened psychopathological symptoms, including substance use disorders, affective disorders and personality disorders | |||
| SCL-90R[199,200] | |||||
| Further differences were found regarding frequency of Internet use regarding social networking sites and online-pornography in patients with BSD who engage more frequently | |||||
| Patients with IA have heightened probability for meeting BSD criteria | |||||
| Recommendation: Implement BSD screening in patients presenting with IA | |||||
| Young[201] | To investigate the efficacy of using CBT with Internet addicts | n = 114 Internet addicts in treatment (42% women (mean age = 38; men mean age = 46) | Sessions conducted between client and principle investigator | IAT[48] | Preliminary analyses indicated most clients managed their presenting complaints by the eighth session |
| Initial sessions gathered familial background, nature of presenting problem, its onset and severity | Self-devised Client Outcome Questionnaire administered after 3rd, 8th, and 12th online session, and at 6 mo follow-up: | Symptom management sustained at 6-mo follow-up | |||
| CBT utilized to address presenting symptoms related to computer use, specifically abstinence from problematic online applications and strategies to control online use | 12 items regarding clients behaviour patterns and treatment successes during counselling process; questions rated how effective counselling was at helping clients achieve targeted treatment goals associated with Internet addiction recovery; questions assessed motivation to quit Internet abuse, ability to control online use, engagement in offline activities, improved relationship functioning, and improved offline sexual functioning (if applicable) | ||||
| Counselling also focused on behavioural issues or other underlying factors contributing to online abuse, such as marital discord, job burnout, problems with co-workers, and academic troubles, depending on respective client | |||||
| Young[202] | To test a specialized form of CBT, CBT-IA | n = 128 clients to measure treatment outcomes using CBT-IA (65% male; age range: 22-56 yr) | CBT-IA: 3-phase approach including behaviour modification to control compulsive Internet use, cognitive restructuring to identify, challenge, and modify cognitive distortions that lead to addictive use, and harm reduction techniques to address and treat co-morbid issues associated with the disorder | IAT[48] | Over 95% of clients managed symptoms at the end of the 12 wk period |
| 78% sustained recovery six months following treatment | |||||
| Administered in 12 weekly sessions | CBT-IA ameliorated IA symptoms after 12 weekly sessions and consistently over 1, 3 and 6 mo after therapy | ||||
| Sessions conducted between client and principle investigator | |||||
| Initial sessions gathered familial background, | |||||
| symptoms of the presenting problem, its onset, and severity | |||||
| CBT-IA addressed presenting symptoms related to computer use, specifically abstinence from problematic online applications and strategies to control use | |||||
| CBT-IA also focused on cognitive issues and harm reduction for underlying factors contributing to Internet abuse such as marital discord, job burnout, problems with co-workers, or academic troubles, depending on respective client | |||||
| Internet use routinely evaluated and treatment outcomes evaluated after 12 sessions and at 1, 3 and 6 mo follow-up | |||||
| Yung et al[203] | To improve IAD involving Google Glass through residential treatment for alcohol use disorder | n = 1 (31-yr-old man who exhibited problematic use of Google Glass) | Navys SARP | N/A regarding SARP and measures, only about his reactions (e.g., withdrawal, craving, etc.) | Following treatment, reduction in irritability, movements to temple to turn on device, and improvements in short-term memory and clarity of thought processes |
| Case report | All electronic devices and mobile computing devices customarily removed from patient during substance rehabilitation treatment | ||||
| United States | 35-d residential treatment | Patient continued to intermittently experience dreams as if looking through the device | |||
| Zhou et al[204] | To examine whether Internet addicted individuals share impulsivity and executive dysfunction with alcohol-dependent individuals | n = 66 | N/A | BIS-11 | Impulsiveness scores, false alarm rate, total response errors, perseverative errors, failure to maintain set of IAD and AD group significantly higher than that of NC group |
| 22 IAD, 22 patients with AD, and 22 NC (NC consisting of citizens living in the city) | Go/no-go task | ||||
| Wisconsin Card Sorting Test (Beijing Ka Yip Wise Development Co., Ltd, computerized version VI) | Hit rate, percentage of conceptual level responses, number of categories completed, forward scores, backwards scores of IAD and AD group significantly lower than that of NC group | ||||
| China | Digit span task | ||||
| Experimental design | Modified Diagnostic Questionnaire for Internet Addiction (YDQ)[66] | No differences in above variables between IAD group and AD group | |||
| Structured clinical interview (Chinese version) | Internet addicted individuals share impulsivity and executive dysfunction with alcohol-dependent patients | ||||
| SADQ[205] | |||||
| Hamilton Depression Scale[206] | |||||
| Barratts Impulsivity Scale (BIS-11)[49] | |||||
| Zhu et al[207] | To observe the effects of CT with EA in combination with PI on cognitive function and ERP, P300 and MMN in patients with IA | n = 120 patients in China with IA randomly divided into 3 groups: | Overall treatment period = 40 d | Internet Addiction Test[208] | Following treatment, IA decreased in all groups |
| n = 39 EA group (n = 40, 27 male, mean age = 22.5, SD = 2.1 yr) | EA applied at acupoints Baihui (GV20), Sishencong (EX-HN1), Hegu (LI4), Neiguan (PC6), Taichong (LR3), Sanyinjiao (SP6) and retained for 30 min once every other day | Wechsler Memory Scale (WMS)[209] | Decrease stronger in CT group relative to both other groups | ||
| n = 36 PI group (n = 25 male, mean age = 21.0, SD = 2.0 yr) | PI with cognitive-behaviour mode every 4 d | ERP observation[210] using MEB 9200-evoked detector | P300 latency depressed and amplitude raised n EA group | ||
| n = 37 CT group (n = 40, 27 males, mean age = 22.5, SD = 2.3 yr) | EA and PI used in CT group | Latency and amplitude of MMN and P300 recorded via EEG | MMN amplitude increased in CT group | ||
| Short-term memory capacity and short-term memory span improved | |||||
| EA and PI improves cognitive function in IA via acceleration of stimuli discrimination and information processing on brain level |
A total of 25 studies[19,26,27,32,43,50,62,72,78,79,93,106,109,111,112,118,124,130,133,143,146,163,164,188,204] investigated the characteristics of treatment seekers. Here, treatment seekers are defined as individuals seeking professional support for online addiction-related problems. The following paragraphs will outline the treatment seekers’ sociodemographic characteristics, Internet/gaming addiction measures used to ascertain diagnostic status in the respective studies, differential diagnoses and comorbidities.
In the included studies, sample sizes ranged from a case study of a male in Australia presenting with the problem of generalised pathological Internet use[112] to a total of 1826 clients sampled from 15 inpatient alcohol addiction rehabilitation centres in Germany, of which 71 also presented with Internet addiction and were then compared to a control group of 58 patients treated for alcohol addiction only[188]. Ages ranged from 16 years[112] to a mean age of 30.5 years[72]. The majority of studies used male participants, with one study using female participants only[50]. Most studies included individuals seeking treatment for Internet addiction and/or problematic Internet use in specialised inpatient and outpatient treatment centres. A number of studies included particular samples, such as individuals sampled via phone consultations (i.e., including 86% relatives of the affected individuals)[43], patients sampled in alcohol rehabilitation centres[130], patients diagnosed with obsessive compulsive disorder (OCD)[46], and female patients treated for eating disorders[50].
Treatment seekers were sampled from various continents. Within Europe, samples included treatment seekers in Germany[43,78,124,130,133,164,188,197], The Netherlands[50], Italy[26,27,32], and Greece[79]. In North America, a Canadian sample was included[72]. In South America, samples included individuals from Perú[62], Puerto Rico[118], and Brazil[139]. In Western Asia, Turkish individuals were sampled in two studies[143,146], whereas in East Asia, participants were from China[163,204], South Korea[93,106,109], and Taiwan[113]. One case study included an Australian adolescent[112].
Internet and/or gaming addiction were measured with a number of different psychometric tools in the included studies, sometimes combined with structured clinical interviews. Clinical interviews were explicitly mentioned in the reports of eight studies[32,50,62,93,106,109,164,204], and these consisted mostly of the Structured Clinical Interview for DSM-IV[64], a semi-structured interview for DSM-IV Axis I diagnoses for mental disorders.
In terms of psychometric measures, in the majority of studies, Young’s popular Internet Addiction Test[48], the IAT, was used[26,32,72,93,106,109,118,143,146]. The IAT is a 20-item self-report scale that measures the extent of Internet addiction based on criteria for substance dependence and pathological gambling[51], and includes loss of control, neglecting everyday life, relationships and alternative recreational activities, behavioural and cognitive salience, negative consequences, escapism/mood modification, and deception. Significant problems due to Internet use are identified if individuals score between 70-100 on the test, and frequent problems when they score between 40-69[48]. However, previous research has suggested that across studies, different cut-off scores for the IAT have been used to classify individuals[6], impairing comparisons across studies.
Another popular measure appeared to be the Assessment of Internet and Computer Game Addiction Scale (AICA-S)[44,194], which was used in seven studies[43,78,124,130,133,188,197]. The AICA-S is a 16-item scale and includes questions about the frequency of specific Internet usage, associated negative consequences and the extent to which use is pathological from a diagnostic point of view. Fourteen out of the total sixteen main questions are used to calculate a clinical score, and to distinguish normal from potentially addictive use[211].
Other measures included the Compulsive Internet Use Scale (CIUS)[55], a 14-item unidimensional self-report questionnaire including loss of control, preoccupation (cognitive and behavioural), withdrawal symptoms, coping/mood modification, and conflict (inter- and intrapersonal). The CIUS classification is based on the DSM-IV TR diagnoses for substance dependence and pathological gambling[12], and was used in one study[50]. Moreover, in one study[79], the Online Cognitions Scale was used[80], which is a 36-item questionnaire that measures cognitions related to problematic Internet use, and includes subscales on loneliness/depression, diminished impulse control, social comfort, and distraction. In another study[113], Chen’s Internet Addiction Scale[117] was administered, which is a 26-item self-report measure of core Internet addiction symptoms, including tolerance, compulsive use, withdrawal, and related problems (i.e., negative impact on social activities, interpersonal relationships, physical condition, and time management). Another study[164] used the Internet Addiction Scale[212], as well as a combination of Young’s[213] and Beard’s[66] Internet addiction criteria, including preoccupation, tolerance, loss of control, withdrawal, overall impairment, deception, and escapism[164]. The latter was also used in another study[204].
A different approach was taken by Tao et al[163], who intended to develop diagnostic criteria for Internet Addiction Disorder (IAD) and to evaluate the validity of these criteria. Accordingly, in order to be diagnosed with IAD, patients had to fulfil the following criteria: The presence of preoccupation and withdrawal (combined with at least one of the following: Tolerance, lack of control, continued excessive use despite knowledge of negative effects/affects, loss of interests excluding the Internet, and Internet use to escape or relieve a dysphoric mood). In addition to this, clinically significant impairment had to be identified (i.e., functional and psychosocial impairment), and the problematic behaviour had to last a minimum of three months, with at least six hours of non-essential Internet use a day. This study has been used as a basis for the APA’s research classification of Internet Gaming Disorder in the DSM-5.
As this section demonstrates, a wide variety of measurements have been applied in order to ascertain Internet or Internet-use related addiction, sometimes involving an expert assessment by an experienced professional. As has been stated in previous research[6], no gold standard exists to measure Internet addiction with high sensitivity and specificity, which is exacerbated by the use of different cut-off points on the same measures across studies. To mitigate this diagnostic conundrum, a diagnosis of Internet addiction would significantly benefit from including a structured clinical interview administered by a trained professional[214], and this would help eliminating false positives and false negatives in the context of diagnosis.
A number of studies investigated differential diagnoses and/or comorbidity of Internet addiction and other psychopathology. In terms of assessing potential comorbidities, the Structured Clinical Interview for DSM-IV mental disorders[64] was used by five studies[32,50,93,106,164]. Psychopathological symptomatology was also assessed using the Symptom-Checklist, SCL-90-R[125,191] and the Chinese version of the Mini International Neuropsychiatric Interview[115]. Personality disorders were identified by using the Dimensional Assessment of Personality Pathology-Short Form[58,59]. Other addiction-related assessments included alcohol and drug addiction measured with the DÉBA[76], the Alcohol Use Disorder Identification Test-Korean version[95], and the Severity of Alcohol Dependence Questionnaire[205], as well as shopping addiction, assessed via the Compulsive Buying Scale[54]. The presence of eating disorders was assessed using the Eating Disorder Inventory 2[52,53]. Mood disorders were assessed using the Hamilton Rating Scale for Depression[39], Beck’s Depression Inventory[132], and the Mood Disorder Questionnaire[198]. Levels of anxiety were measured with the Hamilton Rating Scale for Anxiety[40], Beck’s Anxiety Inventory[74], and the Generalized Anxiety Disorder scale (GAD-7)[127]. Symptoms of Attention Deficit Hyperactivity Disorder (ADHD) were investigated by means of Conners’ Adult ADHD Rating Scales Self (CAARS:S)[42]. Finally, dissociation and depersonalisation were measured using the Dissociative Experiences Scale[34] and the Cambridge Depersonalization Scale[128].
The results of comorbidity and differential diagnosis analyses revealed the following. Of 50 adult outpatients self-referred for their Internet overuse, 14% presented with comorbid ADHD, 7% hypomania, 15% GAD, 15% social anxiety disorder, 7% dysthymia, 7% obsessive compulsive personality disorder, 14% borderline personality disorder, 7% avoidant personality disorder, and 2% binge eating disorder[32]. Higher frequencies of comorbid psychopathology were reported in a sample of 30 male patients with Internet gaming addiction[62], namely 40% antisocial personality traits, 56.7% affective disorders (30% major depression and 26.7% dysthymia), 26.7% other addictions (13.3% gambling, 10% alcohol, 10% marihuana, 6.7% nicotine and 3.3% cocaine addiction), and 16.7% antisocial disorders (13.3% ADHD, social phobia 10% and 3.3% dysmorphic corporal disorder). Generally smaller prevalence rates were reported in a sample of 57 Internet addiction treatment seekers in Canada[72]: 3.5% presented with comorbid depression and 7.5% with anxiety.
Half of a sample of 50 students with Internet addiction[79] presented with a comorbidity of another Axis I disorder (10% with major depression, 5% with dysthymia and psychotic disorders, respectively). This finding was corroborated by another study of 290 male treatment seekers, half of whom met criteria for another psychiatric disorder[124]. In addition to this, of the former sample, 38% presented with a concurrent Axis II personality disorder (22% with narcissistic, and 10% with borderline disorder, respectively)[79]. Significantly higher levels of depression and dissociation were furthermore found in a sample of 25 patients with Internet addiction as compared to a matched healthy control group[164]. Moreover, relative to a control group of male patients treated for alcohol addiction, 71 male patients with alcohol addiction and comorbid Internet addiction presented with higher levels of depression and obsessive-compulsive symptoms[188]. Furthermore, another study[197] including 368 Internet addiction treatment seekers showed that 30.9% met the diagnostic criteria for bipolar spectrum disorders, and this study also evidenced generally increased psychopathological symptomatology (including substance use disorders, affective and personality disorders). Finally, significant positive correlations were reported between compulsive buying and compulsive Internet use, as 11.7% of a sample of 60 female patients displaying patterns of compulsive buying also presented with addictive Internet use. This study reported no differences between individuals presenting with different types of eating disorders regarding compulsive Internet use[50].
Moreover, patients with Internet addiction and patients with pathological gambling received higher scores on depression, anxiety[26,27], and lower scores on global functioning relative to healthy controls, used impulsive coping strategies, and experienced more socio-emotional impairment. Additionally, patients with Internet addiction differed from patients with pathological gambling in that the former experienced higher mental and behavioural disengagement, which was found to be associated with interpersonal impairments[26].
Overall, the presence of comorbidities for Internet-use related addiction in the clinical context appears to be the norm rather than an exception. Individuals seeking treatment for their Internet overuse frequently present with mood and anxiety disorders, and other impulse-control and addictive disorders appear common. This indicates Internet addiction treatment may benefit from therapeutic approaches that combine evidence-based treatments for co-occurring disorders in order to increase treatment efficacy and acceptability for the patient.
In five studies, psychopharmacotherapy[20,22,24,28,46] for online addictions was used. Atmaca[28] reported the case of a 23-year-old male 4th year medical student who presented with the problems of problematic Internet use and anxiety. The patient was treated with a combination of selective serotonine reuptake inhibitors (SSRI) and antipsychotic medication. The antidepressant citalopram was administered at a dose of 20 mg/d and was increased to 40 mg/d within the period of a week, which was continued for six weeks. Subsequently, quetiapine (an atypical antipsychotic typically used for schizophrenia spectrum disorders) was added to the treatment, starting with a dose of 50 mg/d, which was increased to 200 mg/d within four days. The treatment resulted in decreased Internet addiction as measured with the Y-BOCS[30] modified for Internet use, decreased non-essential and essential Internet use, and improved control over Internet use. The improvements persisted until four-month follow up.
Bipeta et al[46] compared 34 control subjects with or without Internet addiction assessed via Young’s Diagnostic Questionnaire[48] with patients with pure OCD with or without Internet addiction (mean age = 27 years, SD = 6.5 years). OCD patients were treated with standard pharmacological treatment for OCD (treatment as usual) for one year, received the benzodiazepine clonazepam (often used in the treatment of anxiety disorders), which was tapered off in three weeks, an SSRI or the tricyclic antidepressant clomipramine for 12 mo. The individuals with Internet addiction in the OCD group received the following doses of medication: Five patients received 150-200 mg fluvoxamine/d, four received 150-200 mg sertraline/d, one received 60 mg fluoxetine/d, and the final one received 200 mg clomipramine/d. In the OCD group that included individuals who were not addicted to using the Internet, the following doses of medication were administered: Eight patients received 150-300 mg fluvoxamine/d, five received 100-200 mg sertraline/d, eleven received 40-80 mg fluoxetine/d, and three received 150-200 mg clomipramine/d. Overall, the OCD treatment improved scores for both OCD and Internet addiction, while only two of the eleven OCD patients still fulfilled Internet addiction criteria after twelve months of treatment[46].
Dell’Osso et al[20] assessed the safety and efficacy of the antidepressant SSRI escitalopram (typically used for mood disorders) in 19 adult patients (12 men, mean age = 38.5, SD = 12.0 years) who presented with the problem of impulsive-compulsive Internet usage disorder assessed via the YBOCS[30], modified for Internet use. The trial consisted of a total of 19 wk, composed of a ten week treatment phase in which escitalopram was administered starting with 10 mg/d, and increased and maintained at 20 mg/d for 10 wk, and subsequent nine weeks of a randomised double-blind placebo controlled trial with or without administration of escitalopram at previous dosages. The treatment phase resulted in a significant decrease in Internet use. However, there were no differences in treatment effect between the treatment and placebo group following the second stage of the study. The authors also note that the group treated with escitalopram experienced negative side effects, including fatigue and sexual side effects, whereas side effects did not occur in the placebo group[20].
Han et al[26] used a controlled trial to test the effects of the antidepressant bupropion sustained release treatment (with a dose of 150 mg/d for the first week and 300 mg/d for five subsequent weeks) on the brain activity of eleven Internet video game addicts (mean age = 21.5, SD = 5.6 years), assessed via Young’s Internet Addiction Scale[216]. The results indicated that the administered psychopharmacological treatment provided successful results for the video game addiction group, as it decreased craving, playing time, and cue-induced brain activity. These authors[22] also used the central nervous system stimulant concerta (methylphenidate commonly used for ADHD) in 62 video game playing children with ADHD (52 males, mean age = 9.3, SD = 2.2 years) who had not previously been given medication. Internet addiction was assessed using the Korean version of Young’s Internet Addiction Scale[87]. The initial concerta dosage was 18 mg/d, with the maintenance dosage being individually adjusted based on the respective children’s clinical symptoms and weight. Following treatment, Internet addiction and Internet use significantly decreased, as did ADHD symptoms and omission errors in a Visual Continuous Performance Test[22].
Taken together, the studies including psychopharmacological treatment for Internet addiction and/or gaming addiction showed positive effects in decreasing Internet addiction symptomatology and Internet/gaming use times. In the few studies conducted, antidepressant medication has been used most, suggesting mood disorders may be comorbid with Internet use addiction. The research also indicated that if other (primary or secondary) disorders are present (specifically, OCD and ADHD), medication typically used to treat these disorders is also effective in reducing Internet addiction-related problems.
Ten studies[23,65,86,119,136,149,174,201-203] described some form of psychological therapy for treating Internet addiction. The majority of psychological therapies used an individual approach, which was applied to outpatients, apart from three studies that used group therapy approaches[23,65,119,136,149].
The most common approach used to treat Internet addiction was Cognitive Behavioural Therapy (CBT)[86,202]. This approach was usually individualised (apart from one study which used a group approach[65]). A further study used a combination of individualised and group therapy, namely Short-Term Treatment for Internet and Computer Game Addiction[192]. The typical CBT programme was administered for the duration of a few months, ranging from eight sessions[65] to 28 sessions, which included both group and individual sessions[192], and sessions lasted between one[86] and two hours[65]. The topics covered with patients in these sessions were: (1) identification of the Internet application associated with symptoms of addiction; (2) control issues (e.g., examining the self, feelings, impulsivity, and the relation between the individual and the Internet to self-manage and self-restrain Internet use); (3) principles of healthy communication, namely interpersonal communication, such as between parent-children[65], and sharing success stories[86]; (4) Internet awareness (with regards to relationships established and developed through the Internet, and dealing with online content); (5) cessation techniques applied to the Internet (e.g., recognizing the addictive behaviour and discontinuing it); and (6) additional elements (e.g., college career planning, covering underlying factors contributing to Internet abuse, such as marital discord, job burnout, problems with co-workers, or academic problems). In general, CBT followed a number of stages, including team building or a probatory stage to review sessions or stabilization and relapse prevention. All sessions were run by therapists[119,192] or psychiatrists[86] who were supporting adults, apart from one case that involved children and adolescents[65].
The treatment outcomes were measured through scores on a number of psychometric scales covering excessive Internet use, including the Internet Overuse Self-Rating Scale[67,68], the Adolescent Pathological Internet Use Scale[120], the Internet Addiction Diagnostic Questionnaire[48], and the assessment of emotional, cognitive and behavioural symptoms. The following emotional skills and problems were measured in some studies. Anxiety was assessed using the Screen for Child Anxiety Related Emotional Disorders[71] and self-esteem was measured with Coopersmith’s Self-Esteem Inventory[103]. Cognitive skills covered were diverse, and measures included the Online Cognition Scale (OCS)[80], and the Time Management Disposition Scale[69]. The behavioural characteristics related to Internet addiction primarily concerned the individual, but also included their peer and family relationships, and were measured using the Chinese version of the Strength and Difficulties Questionnaire[70], and the Parent-Child Communication Scale[122]. Only one study[86] did not make use of questionnaires because it was a neuropsychological and electrophysiological study conducted using an event-related potential approach, focused on cognitive function by detecting a P300 component. The results of this study indicated there was a deficit in cognitive functioning in Internet addicts, which is a finding that has also been observed in other addictive disorders[215].
Four of the included group therapy approaches (out of five studies) included Internet addicts and family groups treated simultaneously. These included (1) a CBT modality called “multimodal school-based group” (MSBG)[65]; (2) a “multi-family group therapy” (MFGT), which was used for treating Internet addiction for the first time[119]; (3) a traditional family therapy for a young adult addicted to using the Internet[136]; and (4) a “multi-level intervention model” that is usually applied to substance abuse, which included family counselling and peer support groups[149].
The psychotherapeutic MSBG approach was applied in a school setting and involved students, parents and teachers. The group of Internet addicts were students treated using classical CBT in a group ranging from six to ten participants. The students’ parents were also administered cognitive behavioural training to recognize their children’s Internet addiction (through children’s feeling states, communication and solving-problem skills in the family, and through controlling the parents’ own feelings and behaviours to manage their children’s excessive Internet use). Teachers were provided psychoeducation, which was delivered by means of workshops in didactic teaching, analysis and discussion, with the purpose of recognising and treating Internet addiction in students, and of supporting their parents.
MFGT is a new psychotherapy approach for adolescent Internet addicts[119]. This intervention provides therapeutic groups for both adults (parents) and adolescents (Internet addicts), and the aim is to provide peer support, allowing transferential reactions, engagement with the treatment and promoting family cohesion. The main goal of this form of psychotherapy is to reduce Internet addiction whilst improving parent-adolescent communication and closeness, and to fulfil the family members’ psychological needs, rather than these needs being fulfilled by Internet use. Altogether, six active sessions were used, with a subsequent three-month follow-up to target potential relapse and discuss new issues and solutions to maintain the effectiveness of the intervention. Each of the sessions lasted for two hours and included five parts: a warm-up exercise, feedback on homework from the last session, a main structured activity, a brief summary and the family assignment. The topics treated per session were: Understanding a family with the problem of excessive Internet use (session 1), parent-adolescent communication skills training (session 2), parent-adolescent communication practices related to the problem (sessions 2 and 3), parent-adolescent relationship building skills training (session 4), associations between psychological needs and Internet use, how to satisfy the unfulfilled need in the family relationships (session 5), and setting up healthy expectations for the family system (session 6).
The classical family therapy approach used in one study[136] was based on Bowen’s[216] family system theory, which focused on the distinction of the self-inside from the self within the family constellation, and was based on an extensive analysis of family-of-origin problems and communication patterns. The treatment was focused on current interactions and changes in behaviour in the family system[217] to modify the family’s communication method by changing behaviours that maintain problematic Internet use, and coping with Internet overuse related problems. The therapy focused on an undesirable online behaviour and replacing it with a healthy behaviour, which would simultaneously induce a change in the family relationships. The intervention lasted three months and included 15 sessions. It treated emotional problems to enhance control over Internet use, and included functional and emotional expression to solve interpersonal relationship problems associated with Internet addiction.
The multi-level intervention model included an individual-based counselling approach with motivational interviewing (MI), complementary techniques, and traditional family-based counselling[149]. It consisted of six phases, lasting between 15 and 19 mo. The phases included (1) emphasising controlled and healthy Internet use; (2) promoting understanding of the change process through different stages from pre-contemplation to relapse, (3) using the MI model[218] for Internet addiction; (4) adopting a family perspective by using a systemic approach; (5) applying a multi-level counselling model including the patient, his/her family and his/her peers; and (6) using individual and group therapy to facilitate the intervention.
The only group approach that did not include a family intervention was the R/T group counselling programme, which specifically addressed Internet addiction[23]. It consisted of ten group sessions (two per week) within the period of one month, which varied in length between one and 1.5 h. Accredited specialists provided this intervention for university students. The content included an introduction to the therapy goal, teaching, activities, homework assignment and sharing. Each session furthermore included four sections: The purpose, materials (e.g., blank paper, topic-oriented games, posters, videos), strategies (e.g., discussion topics, homework assignments) and session evaluation for both the individual and their family, in order to assess whether the aim of the sessions had been achieved.
Overall, the psychological studies which included a control group to compare the effect of the interventions achieved varying results, impeding a general analysis of psychotherapy impact. Du et al[65] did not find significant differences between experimental and control groups in the post-test measure of Internet overuse, although the intervention group improved their time management (efficacy and time control) and other skills (emotional symptoms, conduct problems, hyperactivity, peer relationships and prosocial behaviours) significantly, and this was maintained until a six-month follow-up. Other comparative findings included a longer P300 component duration in Internet addicts treated by CBT compared to healthy controls[86]. However, the amplitudes were similar in both groups. Moreover, although Internet addiction symptoms were reduced after treatment in the experimental group[149], this was not the case for the group’s scores on beliefs and behaviours related to Internet use and psychological well-being, and there was only a small improvement in parental monitoring and functioning following treatment.
Only two studies (out of four experimental studies) showed a clear effectiveness of psychological therapy, and both of these used a group approach. Kim[23] used a quasi-experimental design and an intervention with a group psychotherapy approach, and found a significant reduction in Internet addiction and significantly higher self-esteem in the experimental group compared to the control group. Liu et al[119] found that their MFGT approach was effective in three aspects. It resulted in a significant reduction of time spent online (reduced by half in comparison to the controls), a decrease in the Internet addiction measure, and, from the parents’ perspective, more satisfaction regarding their child’s online behaviours. Moreover, the most important factor to reduce Internet addiction in this study was found to be the parent-adolescent relationship.
Six studies used combined therapy to treat Internet addiction, consisting of some form of psychological treatment in combination with one of the following: Other psychological therapies[138,180], pharmacotherapy[21,25,139] or electroacupuncture therapy[221].
CBT was the most frequently applied psychological therapy to treat Internet addiction. Subsequently, add-ons to the CBT approach included in the identified studies will be elaborated on. Motivational Enhancement Therapy (MET) was developed by Poddar et al[138] and was tested in the context of treating IGD. This MET-CBT approach consisted of a series of stages: (1) a contemplation stage (i.e., initial sessions of rapport building, a detailed interview and case formulation); (2) a preparation stage (i.e., sessions delivered in an empathetic atmosphere to emphasise psychoeducation, including managing physiological and emotional arousal through relaxation techniques, and a cost-benefit analysis of game addiction); and (3) a contract stage with the patient, a parent and the therapist (i.e., behaviour modification of gaming, reducing time spent online and promoting healthy activities). By applying these stages, a reduction of IGD and online gaming was achieved, and school performance was improved.
Another case study[139] combined CBT with psychopharmacotherapy [i.e., administering clonazepam (a benzodiazepine typically used to treat anxiety disorders) and sertraline (an SSRI antidepressant)] to treat Internet addiction. The intervention lasted for three months, and consisted of the following. The CBT approach aimed to support self-recognition and modify and restructure feelings and dysfunctional cognitions related to Internet use, with the goal to prevent relapse. CBT was administered for ten weekly sessions to teach the patient to handle her anxiety and other symptoms related to her Internet use (in this case panic and obsessive symptomatology, which was comorbid to her Internet addiction). Clonazepam (0.5 mg) and sertraline (50 mg) were also administrated once daily. The applied treatment proved effective for reducing both anxiety and Internet addiction.
A new treatment approach to treat Internet addiction combined CBT and MI with an on-the-job Lifestyle Training programme[180]. Treatment was delivered by qualified therapists who were supervised by a senior therapist for both main psychological therapies. The treatment consisted of eliciting and strengthening the motivation to change, choosing a treatment goal, gaining self-control, preventing relapse, and coping skills training. Ten outpatient sessions of 45 min were used, and seven of these took place within a period of 2.5 mo. The remaining sessions were optional and were administered as a follow-up within 3 mo. Each of the sessions had a fixed format: (1) introduction; (2) evaluation of current status; (3) discussing homework; (4) explaining the theme of the day; (5) practicing a skill; (6) receiving homework; and (7) closing the session. This study was the only study that provided three perspectives for data collection: The patients’, the therapists’ and the researchers’ perspectives. This intervention, which is commonly used for other addictive disorders, was found to work well for Internet addiction as it reduced Internet use, increased social contacts, provided a daily structure, and encouraged alternative uses of free time and positive beliefs.
Moreover, CBT was most frequently used in combination with a psychopharmacological treatment, such as administering bupropion. The reason to select this medication is because a proportion of patients with major depressive disorder (MDD) are also excessive online gamers, and this drug has been previously evaluated as potential treatment for MDD and other drug-addictions. Recently, its effectiveness has been tested and confirmed experimentally[21,25]. Han and Renshaw[21] tested this combined treatment in Chinese male adolescent and adult patients with mood disorders and online gaming addiction, and treated them with bupropion sustained release (from 150 mg/d until 300 mg/d during 8 wk) and a psychological intervention (i.e., education for Internet use). The treatment resulted in significantly decreased depression and Internet addiction levels, and time spent playing online games compared with the control group. At follow-up (i.e., four weeks post treatment), the reduction in gaming hours and level of Internet addiction was maintained, while the depression recurred.
Similarly, Kim et al[25] tested the effectiveness of CBT in an active treatment group vs a control group who did not receive CBT in Korean male adolescent patients with MMD and online gaming addiction. Both groups were treated using the same levels of bupropion. Following treatment, Internet addiction was significantly reduced in the CBT group and other measures showed improvement (e.g., anxiety and life satisfaction), while depression severity did not change. These findings were maintained at follow-up. Therefore, the combination of psychotherapy with bupropion is effective in MDD patients with online gaming addiction in the long term only for online gaming addiction, and the time spent using online games. Both studies with bupropion were managed by psychiatrists, and one[25] used a multidisciplinary treatment team including a psychiatrist, nurse, psychologist, and social worker.
One study used clonazepam (0.5 mg/d) and sertraline (50 mg/d) combined with CBT to treat Internet addiction[139]. This study reported the case of a young Brazilian woman with Internet addiction and comorbid psychiatric disorders (i.e., panic and OCDs). During the treatment period of ten weeks, both drugs were administered daily whilst CBT was provided once a week, and focused on teaching the patient how to handle anxiety and Internet use through breathing training with diaphragmatic exercises, education about both disorders’ symptoms and about Internet use (e.g., time management, triggers of problematic Internet use, changing habits, cognitive restructuring, exposure and response prevention, promotion of social support, alternative activities, and promotion of functional Internet use). This combined treatment was effective for all conditions treated.
Zhu et al[207] combined a psychological intervention (i.e., CBT with sessions every four days for a total treatment period of 40 d) with electroacupuncture in 120 patients presenting with Internet addiction in China. They used three groups: 40 participants in the electroacupuncture group, 36 participants in the psychological intervention group, and 37 individuals participated in the comprehensive therapy group combining both treatment ingredients. Electroacupuncture was applied at acupoints Baihui (GV20), Sishencong (EX-HN1), Hegu (LI4), Neiguan (PC6), Taichong (LR3), and Sanyinjiao (SP6), and retained for 30 min once every other day. Overall, treatment was effective in all groups as Internet addiction symptomatology was successfully decreased, whereas this effect was significantly stronger in the combined therapy group relative to the other groups. The authors furthermore note that the combined treatment improved cognitive function in Internet addiction by means of accelerating stimuli discrimination and information processing on the level of the brain.
Combined therapies have shown effective results for treating Internet addiction, including both post-treatment and follow-up measures. The use of electroacupuncture in combination with a psychological intervention improved treatment success for Internet addiction more than providing cognitive-behavioural treatment only, suggesting the novel therapy electroacupuncture may be beneficial in the treatment of Internet addiction. It is suggested to replicate this study to verify the positive results.
Conversely, given the results found by the included studies, psychopharmacotherapy does not always appear to be as efficacious for psychological problems, such as major depression, as it is for Internet and gaming addiction. This is an interesting finding, because it seems that Internet addiction is usually accompanied by other psychological disorders. Therefore, combining therapies may be a good option for some clients, and should be managed by interdisciplinary teams with structured mid-term interventions.
This systematic literature review has sought to provide an overview of the currently available clinical research on Internet addiction and problematic Internet use using a holistic perspective. Clinical studies concerning Internet addiction, problematic Internet use and excessive online gaming have been included to offer a comprehensive insight into the relevant research to date. A total of 46 empirical clinical studies were identified, which focused on treatment seeker characteristics and different types of therapy provisions. Treatments included psychopharmacotherapy, psychological therapy, and combined treatment. Each of these will be discussed subsequently.
In terms of treatment seeker characteristics, the included studies indicated that the published research ranged from case studies to including patients treated for problematic Internet use in both inpatient and outpatient settings across 13 countries and four continents. It is worth noting that a number of studies indicated that comorbidities appear to be the norm, rather than an exception for individuals who present with the problem of Internet addiction or problematic Internet use. Comorbid mood and anxiety disorders appear to be particularly common. A link between mood disorders and Internet addiction has been suggested in previous research, including both adolescent[88,210-227] and adult samples[228-233]. A possible explanation for this strong and frequent link may be the fact that as Internet use increases, online activities take up gradually more time in the lives of Internet users. This reduces the time available to participate in alternative enjoyable pastime activities and to engage with real-life family and friendship circles, which may lead to increased loneliness and stress[234]. Alternatively, Internet use and gaming may serve as a method to escape real-life problems, effectively resulting in avoidance coping, which may exacerbate stress and negative feelings, and lead to negative consequences, including addiction and depression[235].
Moreover, a number of earlier studies have shown that anxiety disorders and anxiety-related symptoms, including social phobia, phobic anxiety, and OCD co-occur with Internet addiction in adolescents[88,236-238] and adults[230,238]. Previous research including Internet addiction treatment experts from six countries indicated that a large percentage of individuals presenting with Internet addiction at both in-patient and out-patient treatment facilities suffer from comorbid anxiety disorders, most commonly social anxiety and social phobia[11]. This may be explained through the mechanism of compensation, suggesting individuals who have difficulties engaging and bonding with their peers in real life may instead use the Internet for social interaction, as the online space removes the embodied (and potentially anxiety-provoking) elements from the interaction. These elements include the individual’s outward appearance and the exclusion of (often feared) face-to-face contact in favour of virtual (and often text-based) interaction. This may facilitate social interaction by increased likelihood of self-disclosure[239], online disinhibition[240], and hyperpersonal communication, characterised by the increased speed of developing social bonds and intimacy online[241].
The research presented indicated that comorbidities complicate treatment. This literature review has shown that comorbidities are very common in the context of Internet addiction, emphasising the necessity to investigate the extent to which Internet addiction can be considered a primary or a secondary disorder (i.e., secondary to some other psychopathology). Researchers have suggested that given the presence of comorbidity, it is questionable whether Internet addiction deserves an individual diagnosis, as this may lead to other (primary) disorders being underdiagnosed. This may lead to problems regarding efficient treatment choices on behalf of the mental healthcare professionals given that efficacious treatments exist for the more prevalent disorders, such as anxiety and mood disorders[242], whereas the evidence base for Internet addiction treatment is still rather limited in comparison. However, research has also indicated that some symptoms of Internet addiction appear as stand-alone symptoms and can be differentiated from other psychopathology, providing empirical evidence for the discriminant validity and specificity of the Internet addiction construct[243]. If comorbidity is present in individuals presenting with Internet addiction or problematic Internet use, clinicians need to target both problems in treatment as research has indicated that individuals with comorbid psychopathology (specifically co-occurring Axis I mental disorders) present with more clinical problems[79].
In terms of psychopharmacotherapy, the five studies included in this systematic literature review showed that SSRIs (i.e., citalopram, clomipramine, fluvoxamine, sertraline, fluoxetine, escitalopram), norepinephrine-dopamine reuptake inhibitors (NDRI; i.e., buproprion), benzodiazepines (i.e., clonazepam), antipsychotic medication (i.e., quetiapine), and methylphenidate (i.e., concerta) were used to treat Internet addiction and Internet-use related problems. Overall, in the included studies, the use of psychopharmacological treatment to alleviate Internet and gaming addiction symptomatology and time spent online appeared successful, suggesting that Internet addiction is an indication for the use of the administered medications[20,22,24,28,46].
The diverse range of administered medication corresponds with the diverse range of presenting problems of the samples included. For instance, concerta is a drug which is efficacious in treating ADHD and therefore commonly used in ADHD treatment[244] as it has been shown to improve inhibition, motivation and memory by increasing dopamine and norephinephrine concentrations in the brain[245]. Moreover, given the relatively high prevalence of both mood and anxiety disorders with comorbid Internet addiction as described above, it is not surprising that antidepressant medications and benzodiazepines are frequently used in the pharmacological treatment of Internet addiction. SSRIs are the method of choice for mood and anxiety disorders and related symptoms[246], and benzodiazepines have anti-anxiety and relaxing properties[247]. Despite their off-label status in countries including the United Kingdom and Australia, NDRIs are often prescribed for depression-related symptoms and disorders[248]. In sum, the studied psychopharmacological treatments for Internet addiction proved efficacious in decreasing both Internet addiction symptoms as well as symptoms of other psychopathologies for which the specific medications have been licensed. Even so, clinicians need to assess the costs and benefits of the medication they are prescribing for treating Internet addiction as some side effects may impact treatment acceptability and treatment adherence in patients.
Regarding psychological therapy for Internet addiction and problematic Internet use, ten studies were identified, most of which used a group therapy framework to support clients. Group therapy has a number of advantages over individual therapy. According to the American Psychological Association[249], the benefits of group therapy include establishing a support network of individuals who experience similar problems and are faced with similar difficulties. Other group members’ stories may put the patients’ own problems into perspective. Moreover, group therapy may create a safe environment in which the sensitive topic of Internet-use related addiction can be discussed openly. Group therapy has the benefit of offering the possibility to learn from others and consequently improve coping skills as individuals differ in their ways they face the world and deal with their lives. These benefits explain why group therapy frameworks are popular psychological therapies for Internet addiction and Internet use-related problems.
The addition of the family network into therapy sessions as evidenced in studies on multimodal school based groups[65], MFGT[119], family therapy[136], and a multi-level intervention model[149] appears particularly fruitful for young patients, as families are important social groups supporting the young patients’ development. Families teach values, offer emotional attachment, model appropriate behaviours, and discourage high-risk behaviours[250]. The efficacy of group-based and systemic therapy for adolescents with problems of substance use and addiction has been long established[251], and suggests that therapeutic frameworks derived from family-based therapies for these disorders may be similarly efficacious in the treatment of Internet addiction and problematic Internet use. The included studies have verified this contention, and therefore clinicians are advised to incorporate families in the psychological treatment of young patients (including adolescents and young adults).
The most commonly applied therapy form was CBT or some variation thereof (e.g., CBT-IA)[202], which has frequently been used in an individual format. The primary goal of CBT is to change maladaptive cognitions and behaviours associated with Internet use, and this therapy form is in line with Davis’[252] cognitive-behavioural model of pathological Internet use. The model suggests cognitive factors are particularly important in the development and maintenance of Internet addiction. In the included studies, cognitive measures indicated that CBT is efficacious in reducing cognitive impairment associated with Internet addiction[86]. However, Winkler et al[17] examined the efficacy of different treatments for Internet addiction in a meta-analysis which included 13 studies, and their results showed that CBT did not perform significantly better than other psychological treatments, although CBT appears to be the most popular approach for treating Internet addiction.
Finally, a number of studies have simultaneously included different forms of therapy, namely psychological treatment supplemented with other types of psychological therapy[138,180], pharmacotherapy[21,25,139] or electroacupuncture therapy[219]. Taken together, all of the combined therapies were efficacious in treating Internet use-related problems, whereas the benefits for comorbid psychopathology (e.g., depression) were limited. This suggests that in cases where comorbidity is present and psychopharmacological treatment is administered, the clinician and researcher need to carefully monitor the patient’s progress, adjust the dosage of the medication and/or change the medication administered to achieve the best possible results for the patient. Moreover, as the new treatment modality of electroacupuncture outperformed psychological interventions, it is suggested that researchers replicate these positive results to ensure they hold across other samples.
A number of limitations need to be highlighted in the included studies. Only a few studies (e.g.,[20,21,23,24,26,27,46,65,78,93,109,119,133,143,188,204]) included a control group, making it difficult to ascertain whether the positive effects of treatment on Internet addiction symptom and related problem reduction were due to the administered treatment, or to non-specific factors of treatment [i.e., the placebo effect (the improvement of symptoms with no treatment)], which can be due to natural history and statistical regression to the mean, among other factors[253]. Moreover, a lack of intention-to-treat analysis in the reported studies might have caused bias in the results due to treatment non-compliance, changes from the initial treatment protocol, or leaving out data from individuals who dropped out of the study before or during the course of treatment[254].
For future research, the need to utilise validated and reliable measures of Internet addiction and/or problematic Internet use needs to be stressed. Currently, the diagnostic and research landscape appears particularly broad, and diagnostic criteria used to identify the potential disorder are not globally agreed upon. Researchers are recommended to collaborate to establish a consensus regarding diagnostic criteria and measures in order to improve the reliability across studies and to develop effective and efficient treatment approaches for treatment seekers. This will furthermore contribute to providing an incentive for public policy and healthcare providers to offer funding for those who need professional help. Ultimately, research and clinical initiatives need to focus on providing the best possible care for individuals who experience significant impairment and distress as a consequence of their Internet use.
Over the last 15 years, the number of Internet users has increased by 1000%, and at the same time, research on addictive Internet use has proliferated. Internet addiction has not yet been understood very well, and research on its etiology and natural history is still in its infancy. In 2013, the American Psychiatric Association included Internet Gaming Disorder in the appendix of the updated version of the Diagnostic and Statistical Manual for Mental Disorders as condition that requires further research prior to official inclusion in the main manual, with important repercussions for research and treatment.
To date, reviews have focused on clinical and treatment studies of Internet addiction and Internet Gaming Disorder. This arguably limits the analysis to a specific diagnosis of a potential disorder that has not yet been officially recognised in the Western world, rather than a comprehensive and inclusive investigation of Internet-use related addictions (including problematic Internet use) more generally.
The aim of this literature review is to provide a comprehensive overview of clinical studies on the clinical picture of Internet-use related addictions from a holistic perspective.
Researchers are recommended to collaborate to establish a consensus regarding diagnostic criteria and measures in order to improve the reliability across studies and to develop effective and efficient treatment approaches for treatment seekers. This will furthermore contribute to providing an incentive for public policy and healthcare providers to offer funding for those who need professional help. Ultimately, research and clinical initiatives need to focus on providing the best possible care for individuals who experience significant impairment and distress as a consequence of their Internet use.
Internet addiction is a condition that requires further research prior to official inclusion in the diagnostic manuals, with important repercussions for research and treatment. To date, reviews have focused on clinical and treatment studies of Internet addiction and Internet Gaming Disorder. This arguably limits the analysis to a specific diagnosis of a potential disorder that has not yet been officially recognised in the Western world, rather than a comprehensive and inclusive investigation of Internet-use related addictions (including problematic Internet use) more generally.
In this systematic review, the authors have presented a thorough and critical analysis of clinical research on Internet addiction related studies.
| 1. | Internet Live Stats. Internet users, 2015. . |
| 2. | King DL, Delfabbro PH. Internet gaming disorder treatment: a review of definitions of diagnosis and treatment outcome. J Clin Psychol. 2014;70:942-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 105] [Article Influence: 8.8] [Reference Citation Analysis (1)] |
| 3. | Poli R, Agrimi E. Internet addiction disorder: prevalence in an Italian student population. Nord J Psychiatry. 2012;66:55-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 76] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 4. | Xu J, Shen LX, Yan CH, Hu H, Yang F, Wang L, Kotha SR, Zhang LN, Liao XP, Zhang J. Personal characteristics related to the risk of adolescent internet addiction: a survey in Shanghai, China. BMC Public Health. 2012;12:1106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 57] [Article Influence: 4.1] [Reference Citation Analysis (1)] |
| 5. | Barkoviak M. China makes Internet addiction an official disorder. Daily Tech. 2012. Available from: http://www.dailytech.com/China+Makes+Internet+Addiction+an+Official+Disorder/article13403.htm. |
| 6. | Kuss DJ, Griffiths MD, Karila L, Billieux J. Internet addiction: a systematic review of epidemiological research for the last decade. Curr Pharm Des. 2014;20:4026-4052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 949] [Cited by in RCA: 682] [Article Influence: 56.8] [Reference Citation Analysis (0)] |
| 7. | American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Arlington, VA: American Psychiatric Association 2013; . |
| 8. | Petry NM, Rehbein F, Gentile DA, Lemmens JS, Rumpf HJ, Mößle T, Bischof G, Tao R, Fung DS, Borges G. An international consensus for assessing internet gaming disorder using the new DSM-5 approach. Addiction. 2014;109:1399-1406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 562] [Cited by in RCA: 564] [Article Influence: 47.0] [Reference Citation Analysis (0)] |
| 9. | Griffiths MD, van Rooij A, Kardefelt-Winther D, Starcevic V, Király O, Pallesen S, Müller K, Dreier M, Carras M, Prause N. Working towards an international consensus on criteria for assessing Internet Gaming Disorder: A critical commentary on Petry et al. (2014). Addiction. 2015;In press. |
| 10. | Lopez-Fernandez O. How has Internet addiction research evolved since the advent of Internet Gaming Disorder? An overview of cyberaddictions from a psychological perspective. Curr Addiction Rep. 2015;2:263-271. [RCA] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 11. | Kuss DJ, Griffiths MD. Internet addiction in psychotherapy. London: Palgrave; 2015; . |
| 12. | American Psychiatric Association. Diagnostic and Statistical Manual for Mental Disorders IV, Text-Revision. Washington, D. C. : American Psychiatric Association; 2000; . |
| 13. | Kuss DJ. ‘I can’t do it by myself’ - An IPA of clients seeking psychotherapy for their MMORPG addiction. In: Bishop J. Psychological and Social Implications Surrounding Internet and Gaming Addiction. IGI Global 2015; . |
| 14. | Koh YS. The Korean national policy for Internet addiction. Internet addiction. Neuroscientific approaches and therapeutic interventions. London: Springer 2015; 219-234. |
| 15. | Thorens G, Achab S, Billieux J, Khazaal Y, Khan R, Pivin E, Gupta V, Zullino D. Characteristics and treatment response of self-identified problematic Internet users in a behavioral addiction outpatient clinic. J Behav Addict. 2014;3:78-81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 16. | Przepiorka AM, Blachnio A, Miziak B, Czuczwar SJ. Clinical approaches to treatment of Internet addiction. Pharmacol Rep. 2014;66:187-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 17. | Winkler A, Dörsing B, Rief W, Shen Y, Glombiewski JA. Treatment of internet addiction: a meta-analysis. Clin Psychol Rev. 2013;33:317-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 199] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 18. | King DL, Delfabbro PH, Griffiths MD, Gradisar M. Assessing clinical trials of Internet addiction treatment: a systematic review and CONSORT evaluation. Clin Psychol Rev. 2011;31:1110-1116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 130] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 19. | Huang XQ, Li MC, Tao R. Treatment of internet addiction. Curr Psychiatry Rep. 2010;12:462-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 20. | Dell’Osso B, Hadley S, Allen A, Baker B, Chaplin WF, Hollander E. Escitalopram in the treatment of impulsive-compulsive internet usage disorder: an open-label trial followed by a double-blind discontinuation phase. J Clin Psychiatry. 2008;69:452-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 72] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Han DH, Renshaw PF. Bupropion in the treatment of problematic online game play in patients with major depressive disorder. J Psychopharmacol. 2012;26:689-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 84] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 22. | Han DH, Lee YS, Na C, Ahn JY, Chung US, Daniels MA, Haws CA, Renshaw PF. The effect of methylphenidate on Internet video game play in children with attention-deficit/hyperactivity disorder. Compr Psychiatry. 2009;50:251-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 157] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 23. | Kim JU. The effect of a R/T group counseling program on the Internet addiction level and self-esteem of Internet addiction in university students. Int J Reality Therapy. 2008;27:4-12. |
| 24. | Han DH, Hwang JW, Renshaw PF. Bupropion sustained release treatment decreases craving for video games and cue-induced brain activity in patients with Internet video game addiction. Exp Clin Psychopharmacol. 2010;18:297-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 174] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 25. | Kim SM, Han DH, Lee YS, Renshaw PF. Combined cognitive behavioral therapy and bupropion for the treatment of problematic on-line game play in adolescents with major depressive disorder. Comp Hum Behav. 2012;28:1954-1959. [RCA] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 100] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 26. | Tonioni F, Mazza M, Autullo G, Cappelluti R, Catalano V, Marano G, Fiumana V, Moschetti C, Alimonti F, Luciani M. Is Internet addiction a psychopathological condition distinct from pathological gambling? Addict Behav. 2014;39:1052-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 27. | Tonioni F, D’Alessandris L, Lai C, Martinelli D, Corvino S, Vasale M, Fanella F, Aceto P, Bria P. Internet addiction: hours spent online, behaviors and psychological symptoms. Gen Hosp Psychiatry. 2012;34:80-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 86] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 28. | Atmaca M. A case of problematic internet use successfully treated with an SSRI-antipsychotic combination. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:961-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 28] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P). New York: Biometrics Research, New York State Psychiatric Institute 2002; . |
| 30. | Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46:1006-1011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5101] [Cited by in RCA: 5187] [Article Influence: 140.2] [Reference Citation Analysis (0)] |
| 31. | Shapira NA, Goldsmith TD, Keck PE, Khosla UM, McElroy SL. Psychiatric features of individuals with problematic internet use. J Affect Disord. 2000;57:267-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 546] [Cited by in RCA: 422] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 32. | Bernardi S, Pallanti S. Internet addiction: a descriptive clinical study focusing on comorbidities and dissociative symptoms. Compr Psychiatry. 2009;50:510-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 213] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 33. | Aboujaoude E, Koran LM, Gamel N, Large MD, Serpe RT. Potential markers for problematic internet use: a telephone survey of 2,513 adults. CNS Spectr. 2006;11:750-755. [PubMed] |
| 34. | Bernstein-Carlson E, Putnam FW. An update on the Dissociative Experiences Scale. Dissociat. 1993;6:16-27. |
| 35. | Guy W. ECDEU Assessment Manual for Psychopharmacology. Revised DHEW Pub. (ADM). National Institute for Mental Health, 1976. . |
| 36. | Sheehan DV. The anxiety disease. New York: Scribner 1983; . |
| 37. | First MB, Spitzer RL, Gibbon M. Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Version (SCID-P), version 2. New York: NewYork State Psychiatric Institute Biometrics Research 1995; . |
| 38. | Pfohl B, Blum N, Zimmerman M. Structured Interview for DSM-IV Personality Disorders (SIDP-IV). Iowa City, Iowa: University of Iowa Department of Psychiatry 1995; . |
| 39. | Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56-62. |
| 40. | Hamilton M. The assessment of anxiety states by rating. Brit J Med Psychol. 1959;32:50-55. |
| 41. | Heimberg RG, Horner KJ, Juster HR, Safren SA, Brown EJ, Schneier FR, Liebowitz MR. Psychometric properties of the Liebowitz Social Anxiety Scale. Psychol Med. 1999;29:199-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 570] [Cited by in RCA: 591] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 42. | Conners C, Erhardt D, Sparrow E. Conners’ Adult ADHD Rating Scales (CAARS): Technical Manual. North Tonawanda, NY: Multi-Health Systems 1999; . |
| 43. | Beutel ME, Hoch C, Wölfling K, Müller KW. Klinische Merkmale der Computerspiel- und Internetsucht am Beispiel der Inanspruchnehmer einer Spielsuchtambulanz. Psychosomat Med Psychother. 2011;57:77-90. [RCA] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 44. | Wölfling K, Müller KW, Beutel M. [Reliability and validity of the Scale for the Assessment of Pathological Computer-Gaming (CSV-S)]. Psychother Psychosom Med Psychol. 2011;61:216-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 45. | Franke GH. SCL-90-R. Die Symptom-Checkliste von Derogatis - Deutsche Version - Manual, 2. vollständig überarbeitete und neu normierte Auflage. Göttingen: Beltz 2002; . |
| 46. | Bipeta R, Yerramilli SS, Karredla AR, Gopinath S. Diagnostic Stability of Internet Addiction in Obsessive-compulsive Disorder: Data from a Naturalistic One-year Treatment Study. Innov Clin Neurosci. 2015;14-23. [PubMed] |
| 47. | Young K. Internet addiction: The emergence of a new clinical disorder. Cyberpsychol Behav. 1998;3:237-244. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2427] [Cited by in RCA: 2034] [Article Influence: 72.6] [Reference Citation Analysis (1)] |
| 48. | Young K. Caught in the net. New York: Wiley 1998; . |
| 49. | Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51:768-774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 50. | Claes L, Müller A, Norré J, Van Assche L, Wonderlich S, Mitchell JE. The relationship among compulsive buying, compulsive internet use and temperament in a sample of female patients with eating disorders. Eur Eat Disord Rev. 2012;20:126-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 51. | American Psychiatric Association. Diagnostic and Statistical Manual for Mental Disorders IV. Washington, D. C. : American Psychiatric Association 1994; . |
| 52. | Garner DM. Eating Disorder Inventory-2: Professional manual. Odessa, FL: Psychological Assessment Resources 1991; . |
| 53. | van Strien T, Ouwens M. Validation of the Dutch EDI-2 in one clinical and two nonclinical populations. Europ J Psychol Assessm. 2003;19:66-84. [RCA] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 56] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 54. | Faber RJ, O’Guinn TC. A clinical screener for compulsive buying. J Consum Res. 1992;19:459-69. [DOI] [Full Text] |
| 55. | Meerkerk GJ, Van Den Eijnden RJ, Vermulst AA, Garretsen HF. The Compulsive Internet Use Scale (CIUS): some psychometric properties. Cyberpsychol Behav. 2009;12:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 467] [Cited by in RCA: 457] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 56. | Carver CS, White TL. Behavioural inhibition, behavioural activation, and affective responses to impending reward and punishment: The BIS/BAS scales. J Pers Soc Psychol Bull. 1994;67:319-333. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4098] [Cited by in RCA: 4167] [Article Influence: 130.2] [Reference Citation Analysis (0)] |
| 57. | Beck I, Smits DJM, Claes L, Vandereycken W, Bijttebier P. Psychometric evaluation of the behavioral inhibition/behavioral activation system scales and the sensitivity to punishment and sensitivity to reward questionnaire in a sample of eating disordered patients. Personal Ind Diff. 2009;47:407-412. [RCA] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 70] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 58. | Livesley WJ, Jackson DN. Manual for the Dimensional Assessment of Personality Pathology - Basic Questionnaire (DAPP-BQ). Port Huron: Sigma 2002; . |
| 59. | van Kampen D, de Beurs E, Andrea H. A short form of the Dimensional Assessment of Personality Pathology-Basic Questionnaire (DAPP-BQ): the DAPP-SF. Psychiatry Res. 2008;160:115-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 60. | Evans DE, Rothbart MK. Developing a model for adult temperament. J Res Personal. 2007;41:868-888. [RCA] [DOI] [Full Text] [Cited by in Crossref: 391] [Cited by in RCA: 409] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 61. | Hartman CA, Rothbart MK. Dutch version of the Adult Temperament Questionnaire-Short Form. Groningen, NL: Groningen Faculteit der Medische Wetenschappen 2001; . |
| 62. | Cruzado Díaz L, Matos Retamozo L, Kendall Folmer R. Adicción a internet: Perfil clínico y epidemiológico de pacientes hospitalizados en un instituto nacional de salud. Revista Med Herediana. 2006;17:196-205. |
| 63. | Mezzich JE, Saavedra JE. Evaluación clínica semiestructurada: El formato de evaluación inicial abreviado. 2nd ed. Perales A, Mendoza A, Vásquez-Caicedo G, Zambrano M. Manual de Psiquiatría Humberto Rotondo. Lima: Universidad Nacional Mayor de San Marcos 1998; . |
| 64. | First MB, Gibbon M, Spitzer RL, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders: Clinician Version (SCID-CV): Administration booklet. Washington, D. C. : American Psychiatric Press 1996; . |
| 65. | Du YS, Jiang W, Vance A. Longer term effect of randomized, controlled group cognitive behavioural therapy for Internet addiction in adolescent students in Shanghai. Aust N Z J Psychiatry. 2010;44:129-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 166] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 66. | Beard KW, Wolf EM. Modification in the proposed diagnostic criteria for Internet addiction. Cyberpsychol Behav. 2001;4:377-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 561] [Cited by in RCA: 444] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 67. | Cao F, Su L. The factors related to Internet overuse in middle school students. Chin J Psychiatry. 2006;39:141-144. |
| 68. | Jiang W, Du Y. The relationship between Internet overuse in middle school students in Shanghai and time management disposition. Shanghai Arch Psychiatry. 2006;18:129-33. |
| 69. | Huang X, Zhang Z. The compiling of the adolescence time management disposition scale. Acta Psychol Sinica. 2001;33:338-343. |
| 70. | Du Y, Kou J. A study of the Strengths and Difficulties Questionnaire (SDQ). Psychol Sci. 2006;29:1419-1421. |
| 71. | Jiao M, Du Y. The clinical application of screening for anxiety related emotional disorders. Shanghai Arch Psychiatry. 2005;17:72-74. |
| 72. | Dufour M, Nadeau L, Gagnon SR. [Internet addiction: a descriptive clinical study of people asking for help in rehabilitation treatment center in Quebec: exploratory study]. Sante Ment Que. 2014;39:149-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 73. | Khazaal Y, Billieux J, Thorens G, Khan R, Louati Y, Scarlatti E, Theintz F, Lederrey J, Van Der Linden M, Zullino D. French validation of the internet addiction test. Cyberpsychol Behav. 2008;11:703-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 199] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 74. | Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7560] [Cited by in RCA: 8927] [Article Influence: 241.3] [Reference Citation Analysis (0)] |
| 75. | Bourque P, Beaudette D. Étude psychométrique du questionnaire de dépression de Beck auprès d’un échantillon d’étudiants universitaires francophones. Rev Canad Scien Comportement. 1982;14:211-218. [RCA] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 211] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 76. | Tremblay J, Blanchette-Martin N. Manuel d’utilisation du DÉBA Alcool/Drogues/Jeu; version adaptée pour la formation de la première ligne en dépendance, version 1.08. Québec: Service de recherche CRUV/CRAT-CA en collaboration avec le Centre Dollard-Cormier - Institut universitaire sur les dépendances 2009; . |
| 77. | Rosenberg M. Society and adolescent self-image. New Jersey: Princeton University Press 1965; . |
| 78. | Duven EC, Müller KW, Beutel ME, Wölfling K. Altered reward processing in pathological computer gamers--ERP-results from a semi-natural gaming-design. Brain Behav. 2015;5:13-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 79. | Floros G, Siomos K, Stogiannidou A, Giouzepas I, Garyfallos G. Comorbidity of psychiatric disorders with Internet addiction in a clinical sample: the effect of personality, defense style and psychopathology. Addict Behav. 2014;39:1839-1845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (1)] |
| 80. | Davis RA, Flett GL, Besser A. Validation of a new scale for measuring problematic internet use: implications for pre-employment screening. Cyberpsychol Behav. 2002;5:331-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 428] [Cited by in RCA: 284] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 81. | Hyphantis T. The Greek version of the Defense Style Questionnaire: psychometric properties in three different samples. Compr Psychiatry. 2010;51:618-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 82. | Zuckerman M, Kuhlman DM, Joireman J, Teta P, Kraft M. A comparison of three structural models for personality: The Big Three, the Big Five, and the Alternative Five. J Personal Soc Psychol. 1993;65:757-768. [RCA] [DOI] [Full Text] [Cited by in Crossref: 793] [Cited by in RCA: 849] [Article Influence: 25.7] [Reference Citation Analysis (1)] |
| 83. | Hyphantis T, Antoniou K, Floros D, Valma V, Pappas A, Douzenis A, Assimakopoulos K, Iconomou G, Kafetzopoulos E, Garyfallos G. Assessing personality traits by questionnaire: psychometric properties of the Greek version of the Zuckerman-Kuhlman personality questionnaire and correlations with psychopathology and hostility. Hippokratia. 2013;17:342-350. [PubMed] |
| 84. | Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13:595-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4449] [Cited by in RCA: 4239] [Article Influence: 98.6] [Reference Citation Analysis (0)] |
| 85. | Donias S, Karastergiou A, Manos N. Standardization of the symptom checklist-90-R rating scale in a Greek population. Psihiatrike. 1991;2:42-48. |
| 86. | Ge L, Ge X, Xu Y, Zhang K, Zhao J, Kong X. P300 change and cognitive behavioral therapy in subjects with Internet addiction disorder A 3-month follow-up study. Neur Regenerat Res. 2011;6:2037-2041. [DOI] [Full Text] |
| 87. | Young KS. Psychology of computer use: XL. Addictive use of the Internet: a case that breaks the stereotype. Psychol Rep. 1996;79:899-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 635] [Cited by in RCA: 477] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 88. | Ha JH, Yoo HJ, Cho IH, Chin B, Shin D, Kim JH. Psychiatric comorbidity assessed in Korean children and adolescents who screen positive for Internet addiction. J Clin Psychiatry. 2006;67:821-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 224] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 89. | Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23191] [Cited by in RCA: 23694] [Article Influence: 846.2] [Reference Citation Analysis (0)] |
| 90. | DuPaul GJ. Parent and teacher ratings of ADHD symptoms: Psychometric properties of a community sample. J Clin Child Psychol. 1991;20:245-253. [RCA] [DOI] [Full Text] [Cited by in Crossref: 388] [Cited by in RCA: 389] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 91. | So YK, Noh JN, Kim YS, Ko SG, Koh YJ. The reliability and validity of Korean parent and teacher ADHD rating scale. J Korean Neuropsychiat Assoc. 2002;41:283-289. |
| 92. | Kim SW, Shin IS, Kim JM, Yang SJ, Shin HY, Yoon JS. Association between attitude toward medication and neurocognitive function in schizophrenia. Clin Neuropharmacol. 2006;29:197-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 93. | Hwang JY, Choi JS, Gwak AR, Jung D, Choi SW, Lee J, Lee JY, Jung HY, Kim DJ. Shared psychological characteristics that are linked to aggression between patients with Internet addiction and those with alcohol dependence. Ann Gen Psychiatry. 2014;13:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 94. | Song MJ. Internet addictive users’ communicative satisfaction in online and offline situation. Seoul: Korea University 2000; . |
| 95. | Lee BO, Lee CH, Lee PG, Choi MJ, Namkoong K. Development of Korean version of alcohol use disorders identification test (AUDIT-K): Its reliability and validity. J Korean Acad Addict Psychiatry. 2000;4:83-92. |
| 97. | Kim DY, Yoo TY. The relationship between the Big Five personality factors and contextual performance in work organizations. Korean J Indust Organisat Psychol. 2002;15:1-14. |
| 98. | Chung YO, Lee CW. A study of factor structures of the Barratt impulsiveness scale in Korean university students. Korean J Indust Organisat Psychol. 1997;16:111-114. |
| 99. | Lee HS. Impulsivity Test. Seoul: Korea Guidance 1992; . |
| 100. | Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983; . |
| 101. | Chon KK, Hahn DW, Lee CH, Spielberger CD. Korean adaptation of the state-trait anger expression inventory: Anger and blood pressure. Korean J Health Psychol. 1997;2:60-78. |
| 102. | Korea Agency for Digital Opportunity and Promotion. The present conditions of use of Internet: Author, 2002. . |
| 103. | Coopersmith S. Self-esteem inventories. Palo Alto: Consulting Psychologists Press 1981; . |
| 104. | Baker RW, Siryk B. Measuring adjustment to college. J Counsel Psychol. 1984;31:179-189. [DOI] [Full Text] |
| 105. | Huebner ES. Initial development of the Student’s Life Satisfaction Scale. School Psychol Int. 1991;12:231-240. [RCA] [DOI] [Full Text] [Cited by in Crossref: 625] [Cited by in RCA: 630] [Article Influence: 63.0] [Reference Citation Analysis (0)] |
| 106. | Kim SJ, Park DH, Ryu SH, Yu J, Ha JH. Usefulness of Young’s Internet addiction test for clinical populations. Nord J Psychiatry. 2013;67:393-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 107. | Ha JH, Cho DY, Lee HJ, Yang EJ, Woo JI, Lyoo IK. Patterns of Internet addiction in Korea. J Korean Soc Psychopathol. 2000;9:59-68. |
| 108. | Yoo HJ, Cho SC, Ha J, Yune SK, Kim SJ, Hwang J, Chung A, Sung YH, Lyoo IK. Attention deficit hyperactivity symptoms and internet addiction. Psychiatry Clin Neurosci. 2004;58:487-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 306] [Cited by in RCA: 252] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 109. | Kim H, Kim YK, Gwak AR, Lim JA, Lee JY, Jung HY, Sohn BK, Choi SW, Kim DJ, Choi JS. Resting-state regional homogeneity as a biological marker for patients with Internet gaming disorder: A comparison with patients with alcohol use disorder and healthy controls. Prog Neuropsychopharmacol Biol Psychiatry. 2015;60:104-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 65] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 110. | Kim KB, Han KS, Lee JK, Rhee MK, Kim YK, Kim CK. The preliminary study of the Korean alcoholism screening test (III): Alcoholism Screening Test of Seoul National Mental Hospital. J Korean Neuropsychiat Assoc. 1991;30:569-581. |
| 111. | Barratt ES. Impulsiveness subtraits: Arousal and information processing. Motivation, emotion and personality. New York, NY: Elsevier Science 1985; 137-146. |
| 112. | King DL, Delfabbro PH, Griffiths MD, Gradisar M. Cognitive-behavioral approaches to outpatient treatment of internet addiction in children and adolescents. J Clin Psychol. 2012;68:1185-1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 70] [Article Influence: 5.0] [Reference Citation Analysis (1)] |
| 113. | Ko CH, Yen JY, Chen SH, Wang PW, Chen CS, Yen CF. Evaluation of the diagnostic criteria of Internet gaming disorder in the DSM-5 among young adults in Taiwan. J Psychiatr Res. 2014;53:103-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 199] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 114. | Ko CH, Yen JY, Chen SH, Yang MJ, Lin HC, Yen CF. Proposed diagnostic criteria and the screening and diagnosing tool of Internet addiction in college students. Compr Psychiatry. 2009;50:378-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 144] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 115. | Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59 Suppl 20:22-33; quiz 34-57. [PubMed] |
| 116. | Ko CH, Liu GC, Yen JY, Chen CY, Yen CF, Chen CS. Brain correlates of craving for online gaming under cue exposure in subjects with Internet gaming addiction and in remitted subjects. Addict Biol. 2013;18:559-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 163] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 117. | Chen SH, Weng LC, Su YJ, Wu HM, Yang PF. Development of Chinese Internet Addiction Scale and its psychometric study. Chin J Psychol. 2003;45:279-294. |
| 118. | Liberatore KA, Rosario K, Colón-De Martí LN, Martínez KG. Prevalence of Internet addiction in Latino adolescents with psychiatric diagnosis. Cyberpsychol Behav Soc Netw. 2011;14:399-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 119. | Liu QX, Fang XY, Yan N, Zhou ZK, Yuan XJ, Lan J, Liu CY. Multi-family group therapy for adolescent Internet addiction: exploring the underlying mechanisms. Addict Behav. 2015;42:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 108] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 120. | Wartberg L, Petersen KU, Kammerl R, Rosenkranz M, Thomasius R. Psychometric validation of a German version of the compulsive Internet use scale. Cyberpsychol Behav Soc Netw. 2014;17:99-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 121. | Buchanan CM, Maccoby EE, Dornbusch SM. Caught between parents: adolescents’ experience in divorced homes. Child Dev. 1991;62:1008-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 42] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 122. | Barnes HL, Olson DH. Parent-adolescent communication and circumplex model. Child Dev. 1985;56:438-447. [RCA] [DOI] [Full Text] [Cited by in Crossref: 486] [Cited by in RCA: 485] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 123. | Wan JJ, Zhang JT, Liu QX, Deng LY, Fang XY. Development of college students’ psychological need Internet gratification questionnaire. Stud Psychol Behav. 2010;8:118-125. |
| 124. | Müller KW, Beutel ME, Wölfling K. A contribution to the clinical characterization of Internet addiction in a sample of treatment seekers: validity of assessment, severity of psychopathology and type of co-morbidity. Compr Psychiatry. 2014;55:770-777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 125. | Derogatis LR. SCL-90-R: Administration, scoring, and procedures manual II for the revised version. Towson, MD: Clinical Psychometric Research 1983; . |
| 126. | Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737-1744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6086] [Cited by in RCA: 7101] [Article Influence: 263.0] [Reference Citation Analysis (0)] |
| 127. | Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, Herzberg PY. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46:266-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1978] [Cited by in RCA: 3064] [Article Influence: 170.2] [Reference Citation Analysis (0)] |
| 128. | Michal M, Zwerenz R, Tschan R, Edinger J, Lichy M, Knebel A, Tuin I, Beutel M. [Screening for depersonalization-derealization with two items of the cambridge depersonalization scale]. Psychother Psychosom Med Psychol. 2010;60:175-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 129. | Wölfling K, Jo C, Bengesser I, Beutel ME, Müller KW. Computerspiel- und Internetsucht. Ein kognitiv-behaviorales Behandlungsmanual. Stuttgart: Kohlhammer 2013; . |
| 130. | Müller KW, Koch A, Dickenhorst U, Beutel ME, Duven E, Wölfling K. Addressing the question of disorder-specific risk factors of internet addiction: a comparison of personality traits in patients with addictive behaviors and comorbid internet addiction. Biomed Res Int. 2013;2013:546342. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 131. | Costa PT, McCrae RR. Revised NEO personality inventory (NEO-PI-R) and the NEO Five-Factor inventory (NEO-FFI): Professional manual. Odessa, FL: Psychological Assessment Resources 1992; . |
| 132. | Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory. 2nd ed. San Antonio, TX: The Psychological Corporation 1996; . |
| 133. | Müller KW, Beutel ME, Egloff B, Wölfling K. Investigating risk factors for Internet gaming disorder: a comparison of patients with addictive gaming, pathological gamblers and healthy controls regarding the big five personality traits. Eur Addict Res. 2014;20:129-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 121] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 134. | Wölfling K, Beutel ME, Müller KW. Construction of a standardized clinical interview to assess internet addiction: First findings regarding the usefulness of AICA-C. J Addict Res Ther. 2012;S6:003. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 135. | Grüsser S, Hesselbarth U, Albrecht U, Mörsen C. Berliner Inventar zur Glücksspielsucht - Screener (Berlin Inventory for Gambling). Berlin, 2006. . |
| 136. | Park TY, Kim S, Lee J. Family therapy for an Internet-addicted young adult with interpersonal problems. J Famil Ther. 2014;36:394-419. [DOI] [Full Text] |
| 137. | Miles MB, Huberman AM. Qualitative data analysis. Thousand Oaks, CA: Sage 1994; . |
| 138. | Poddar S, Sayeed N, Mitra S. Internet gaming disorder: Application of motivational enhancement therapy principles in treatment. Indian J Psychiatry. 2015;57:100-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 139. | Santos V, Nardi AE, King AL. Treatment of internet addiction in patient with panic disorder and obsessive compulsive disorder: a case report. CNS Neurol Disord Drug Targets. 2015;14:341-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 140. | Chambless DL, Caputo GC, Bright P, Gallagher R. Assessment of fear of fear in agoraphobics: the body sensations questionnaire and the agoraphobic cognitions questionnaire. J Consult Clin Psychol. 1984;52:1090-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 890] [Cited by in RCA: 800] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 141. | Bandelow B. Assessing the efficacy of treatments for panic disorder and agoraphobia. II. The Panic and Agoraphobia Scale. Int Clin Psychopharmacol. 1995;10:73-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 207] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 142. | Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont). 2007;4:28-37. [PubMed] |
| 143. | Şenormancı Ö, Şenormancı G, Güçlü O, Konkan R. Attachment and family functioning in patients with internet addiction. Gen Hosp Psychiatry. 2014;36:203-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 144. | Fraley RC, Waller NG, Brennan KA. An item response theory analysis of self-report measures of adult attachment. J Pers Soc Psychol. 2000;78:350-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 141] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 145. | Epstein NB, Baldwin LM, Bishop DS. The McMaster family assessment device. J Marit Famil Ther. 1983;9:171-180. [DOI] [Full Text] |
| 146. | Senormancı O, Konkan R, Güçlü O, Senormancı G. Depression, loneliness, anger behaviours and interpersonal relationship styles in male patients admitted to internet addiction outpatient clinic in Turkey. Psychiatr Danub. 2014;26:39-45. [PubMed] |
| 147. | Russell D, Peplau LA, Cutrona CE. The revised UCLA Loneliness Scale: concurrent and discriminant validity evidence. J Pers Soc Psychol. 1980;39:472-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2593] [Cited by in RCA: 2546] [Article Influence: 55.3] [Reference Citation Analysis (0)] |
| 148. | Şahin NH, Durak A, Yasak Y. Interpersonal style, loneliness and depression. 23rd International Congress of Applied Psychology; 1994; Madrid, Spain. . |
| 149. | Shek DT, Tang VM, Lo CY. Evaluation of an Internet addiction treatment program for Chinese adolescents in Hong Kong. Adolescence. 2009;44:359-373. [PubMed] |
| 150. | Shek DT, Tang VM, Lo CY. Internet addiction in Chinese adolescents in Hong Kong: assessment, profiles, and psychosocial correlates. ScientificWorldJournal. 2008;8:776-787. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 78] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 151. | Griffiths MD, Hunt N. Dependence on computer games by adolescents. Psychol Rep. 1998;82:475-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 153] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 152. | Suler J. Computer and cyberspace addiction. Int J App Psychoanal Stud. 2004;1:359-356. [RCA] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 153. | Young K. Internet addiction: Evaluation and treatment. Stud Brit Med J. 1999;7:351-352. |
| 154. | Suler J. Internet addiction support group: Is there truth in jest? Psychol Cyberspace. 1998;2:3-5. |
| 155. | Pratarelli ME, Browne BL, Johnson K. The bits and bytes of computer/Internet addiction: a factor analytic approach. Behav Res Methods Instrum Comput. 1999;31:305-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 52] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 156. | Xie JH, Yang SQ. Study of relationship between Internet use attitudes and behaviors among college students. 2004. . |
| 157. | Wang Q, Ross MW. Differences between chat room and e-mail sampling approaches in Chinese men who have sex with men. AIDS Educ Prev. 2002;14:361-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 29] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 158. | Shek DTL. Assessment of family functioning in Chinese adolescents: The Chinese Family Assessment Instrument. International perspectives on child and adolescent mental health. Amsterdam: Elsevier; 2002; 297-316. |
| 159. | Shek DTL. Meaning in life and adjustment amongst early adolescents in Hong Kong. Int For Logother. 1999;22:36-43. |
| 160. | Shek DT. Reliability and factorial structure of the Chinese version of the Beck Depression Inventory. J Clin Psychol. 1990;46:35-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 161. | Shek DTL. Measurement of pessimism in Chinese adolescents: The Chinese Hopelessness Scale. Soc Behav Pers. 1993;21:107-119. [RCA] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 66] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 162. | Shek DT. Perceived parent-child relational qualities and parental behavioral and psychological control in Chinese adolescents in Hong Kong. Adolescence. 2006;41:563-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 54] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 163. | Tao R, Huang X, Wang J, Zhang H, Zhang Y, Li M. Proposed diagnostic criteria for internet addiction. Addiction. 2010;105:556-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 345] [Cited by in RCA: 283] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 164. | Te Wildt BT, Putzig I, Drews M, Lampen-Imkamp S, Zedler M, Wiese B, Dillo W, Ohlmeier MD. Pathological Internet use and psychiatric disorders: A cross-sectional study on psychiatric phenomenology and clinical relevance of Internet dependency. Eur J Psychiatry. 2010;24:136-145. [RCA] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 165. | Hahn A, Jerusalem M. Reliabilität und Validität in der Online-Forschung. Handbuch zur Online-Marktforschung. Beiträge aus Wissenschaft und Praxis. Wiesbaden: Gabler 2001; . |
| 166. | Derogatis LR, Cleary PA. Confirmation of the dimensional structure of the SCL-90: A study in construct validation. J Clin Psychol. 1977;33:981-989. [DOI] [Full Text] |
| 167. | Hessel A, Schumacher J, Greyer M, Brähler E. Symptom-Checkliste SCL-90R: Testtheoretische Überprüfung und Normierung an einer bevölkerungsrepräsentativen Stichprobe. Diagnostika. 2001;47:27-39. [RCA] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 59] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 168. | Hautzinger M, Bailer M, Worall H, Keller F. Becks Depressionsinventar. Testhandbuch. Bern: Gruber; 1995; . |
| 169. | Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis. 1986;174:727-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2320] [Cited by in RCA: 2112] [Article Influence: 52.8] [Reference Citation Analysis (0)] |
| 170. | Freyberger HJ, Spitzer C, Stieglitz RD, Kuhn G, Magdeburg N, Bernstein-Carlson E. Fragebogen zu dissoziativen Symptomen (FDS). Deutsche Adaptation. Reliabilität und Validität der amerikanischen Dissociative Experience Scale (DES). Psychother Psychosom Med Psychol. 1998;48:223-229. |
| 171. | Eriksson M, Lindström B. Validity of Antonovsky’s sense of coherence scale: a systematic review. J Epidemiol Community Health. 2005;59:460-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 870] [Cited by in RCA: 880] [Article Influence: 41.9] [Reference Citation Analysis (0)] |
| 172. | Schumacher J, Gunzelmann T, E . B. Deutsche Normierung der Sense of Coherence Scale von Antonovsky. Diagnostica. 2000;46:208-213. [RCA] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 71] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 173. | Gude T, Moum T, Kaldestad E, Friis S. Inventory of interpersonal problems: a three-dimensional balanced and scalable 48-item version. J Pers Assess. 2000;74:296-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 174. | Brähler E, Horowitz LM, Kordy H, Schumacher J, Strauss B. [Validation of the Inventory for Interpersonal Problems (IIP). Results of a representative study in East and West Germany]. Psychother Psychosom Med Psychol. 1999;49:422-431. [PubMed] |
| 175. | Snaith RP, Hamilton M, Morley S, Humayan A, Hargreaves D, Trigwell P. A scale for the assessment of hedonic tone the Snaith-Hamilton Pleasure Scale. Br J Psychiatry. 1995;167:99-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 864] [Cited by in RCA: 1187] [Article Influence: 38.3] [Reference Citation Analysis (0)] |
| 176. | Fossati A, Cloninger CR, Villa D, Borroni S, Grazioli F, Giarolli L, Battaglia M, Maffei C. Reliability and validity of the Italian version of the Temperament and Character Inventory-Revised in an outpatient sample. Compr Psychiatry. 2007;48:380-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 76] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 177. | Carver CS. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med. 1997;4:92-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3872] [Cited by in RCA: 4272] [Article Influence: 147.3] [Reference Citation Analysis (0)] |
| 178. | Armsden GC, Greenberg MT. The inventory of parent and peer attachment: Individual differences and their relationship to psychological well-being in adolescence. J Youth Adolesc. 1987;16:427-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2142] [Cited by in RCA: 1687] [Article Influence: 129.8] [Reference Citation Analysis (0)] |
| 179. | Yang CK. Sociopsychiatric characteristics of adolescents who use computers to excess. Acta Psychiatr Scand. 2001;104:217-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 56] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 180. | van Rooij AJ, Zinn MF, Schoenmakers TM, van de Mheen D. Treating Internet addiction With Cognitive-Behavioral Therapy: A thematic analysis of the experiences of therapists. Int J Ment Health Addict. 2012;10:69-82. [RCA] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 181. | De Wildt W. Leefstijltraining 2. Handleiding voor de trainer [Lifestyle training 2. Trainer’s manual]. Nijmegen: Cure and Care; 2000; . |
| 182. | Oudejans S. Routine outcome monitoring and learning organizations in substance abuse treatment. Amsterdam: University of Amsterdam; 2009; . |
| 183. | Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York, NY: Guilford; 2002; . |
| 184. | Rollnick S, Allison J. Motivational interviewing. The essential handbook of treatment and prevention of alcohol problems. West Sussex: Wiley 2004; 105-116. |
| 185. | Marlatt GA, Donovan DM. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. New York, NY: Guilford; 2005; . |
| 186. | Monti PM. Treating alcohol dependence: A coping skills training guide. New York, NY: Guilford; 2002; . |
| 187. | Breslin FC, Sobell LC, Sobell MB, Agrawal S. A comparison of a brief and long version of the Situational Confidence Questionnaire. Behav Res Ther. 2000;38:1211-1220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 118] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 188. | Wölfling K, Beutel ME, Koch A, Dickenhorst U, Müller KW. Comorbid internet addiction in male clients of inpatient addiction rehabilitation centers: psychiatric symptoms and mental comorbidity. J Nerv Ment Dis. 2013;201:934-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 189. | Müller KW, Wölfling K. Pathologische Computerspiel- und Internetnutzung - Wissenschaftliche Erkenntnisse zu Phänomenologie, Epidemiologie, Diagnostik und Komorbidität. Suchtmed. 2010;12:45-55. |
| 190. | Wölfling K, Leménager T, Peukert P, Batra A. Computerspiel- und Internetsucht und pathologisches Glücksspiel. Nervenarzt. 2013;84:576-583. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 191. | Franke GH. SCL-90-R - Die Symptom-Checkliste von L. R. Derogatis. Göttingen: Beltz Test 2002; . |
| 192. | Wölfling K, Beutel ME, Dreier M, Müller KW. Treatment outcomes in patients with internet addiction: a clinical pilot study on the effects of a cognitive-behavioral therapy program. Biomed Res Int. 2014;2014:425924. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 193. | Kanfer FH, Phillips JS. Learning foundations of behavior therapy. New York, NY: JohnWiley and Sons 1970; . |
| 194. | Wölfling K, Müller K, Beutel M. Diagnostic measures: Scale for the Assessment of Internet and Computer Game Addiction (AICA-S). Prevention, diagnostics, and therapy of computer game addiction. Lengerich: Pabst Science; 2010; 212-215. |
| 195. | Schwarzer R, Jerusalem M. Generalized Self-Efficacy scale. Measures in health psychology: A user’s portfolio. Causal and control beliefs. Windsor: NFER-NELSON; 1995; 35-37. |
| 196. | Derogatis LR. SCL-90-R administration, scoring and procedure manual II. Towson, MD: Clinical Psychometric Research; 1994; . |
| 197. | Wölfling K, Beutel ME, Dreier M, Müller KW. Bipolar spectrum disorders in a clinical sample of patients with Internet addiction: hidden comorbidity or differential diagnosis? J Behav Addict. 2015;4:101-105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 198. | Hirschfeld RM, Williams JB, Spitzer RL, Calabrese JR, Flynn L, Keck PE, Lewis L, McElroy SL, Post RM, Rapport DJ. Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry. 2000;157:1873-1875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 921] [Cited by in RCA: 979] [Article Influence: 37.7] [Reference Citation Analysis (0)] |
| 199. | Derogatis LR. SCL-90. Administration, scoring and procedures manual-I for the R (revised) version and other instruments of the Psychopathology Rating Scales Series. Chicago: John Hopkins University School of Medicine; 1977; . |
| 200. | Brophy CJ, Norvell NK, Kiluk DJ. An examination of the factor structure and convergent and discriminant validity of the SCL-90R in an outpatient clinic population. J Pers Assess. 1988;52:334-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 78] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 201. | Young KS. Cognitive behavior therapy with Internet addicts: treatment outcomes and implications. Cyberpsychol Behav. 2007;10:671-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 374] [Cited by in RCA: 271] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 202. | Young KS. Treatment outcomes using CBT-IA with Internet-addicted patients. J Behav Addict. 2013;2:209-215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 112] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 203. | Yung K, Eickhoff E, Davis DL, Klam WP, Doan AP. Internet addiction disorder and problematic use of Google Glass™ in patient treated at a residential substance abuse treatment program. Addict Behav. 2015;41:58-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 204. | Zhou Z, Zhu H, Li C, Wang J. Internet addictive individuals share impulsivity and executive dysfunction with alcohol-dependent patients. Front Behav Neurosci. 2014;8:288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 65] [Article Influence: 5.4] [Reference Citation Analysis (1)] |
| 205. | Stockwell T, Murphy D, Hodgson R. The severity of alcohol dependence questionnaire: its use, reliability and validity. Br J Addict. 1983;78:145-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 319] [Article Influence: 7.4] [Reference Citation Analysis (1)] |
| 206. | Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6:278-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5785] [Cited by in RCA: 5930] [Article Influence: 100.5] [Reference Citation Analysis (0)] |
| 207. | Zhu TM, Jin RJ, Zhong XM, Chen J, Li H. [Effects of electroacupuncture combined with psychologic interference on anxiety state and serum NE content in the patient of internet addiction disorder]. Zhongguo Zhen Jiu. 2008;28:561-564. [PubMed] |
| 208. | Widyanto L, McMurran M. The psychometric properties of the internet addiction test. Cyberpsychol Behav. 2004;7:443-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 519] [Cited by in RCA: 465] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 209. | Zhu YH. Recovery evaluation and assessment. Shanghai: Shanghai Scientific and Technical Press; 2008; . |
| 210. | Su H, Jiang KD, Lou FY, Chen XS, Liang JH. Changes of P300 and mismatch negativity in the treatment of first episode depression. J Shanghai Jiaotong Univ. 2006;26:111-113. |
| 211. | Müller KW, Wölfling K. Computer game and Internet addiction: Aspects of diagnostics, phenomenology, pathogenesis, and therapeutic intervention. Suchtther. 2011;12:57-63. |
| 212. | Hahn A, Jerusalem M. Internetsucht: Validierung eines Instruments und explorative Hinweise auf personale Bedingungen (Internet addiction: Validation of an instrument and explorative evidence on personal causes. Handbuch zur Online-Marktforschung. Beiträge aus Wissenschaft und Praxis. Wiesbaden: Gabler; 2001; 213-233. |
| 213. | Young K, Pistner M, O‘Mara J, Buchanan J. Cyber disorders: the mental health concern for the new millennium. Cyberpsychol Behav. 1999;2:475-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 129] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 214. | Beard KW. Internet addiction: a review of current assessment techniques and potential assessment questions. Cyberpsychol Behav. 2005;8:7-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 172] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 215. | Kuss DJ, Griffiths MD. Internet and gaming addiction: a systematic literature review of neuroimaging studies. Brain Sci. 2012;2:347-374. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 274] [Cited by in RCA: 225] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 216. | Bowen M. Family therapy in clinical practice. New York, NY: Rowman and Littlefield; 2008; . |
| 217. | Watzlawick P, Beavin JH, Jackson DD. Pragmatics of human communication: A study of interactional patterns, pathologies and paradoxes. New York, NY: W. W. Norton 1967; . |
| 218. | Rolnick S, Miller WR. What is motivational interviewing? Behav Cog Psychother. 1995;23:325-334. [RCA] [DOI] [Full Text] [Cited by in Crossref: 992] [Cited by in RCA: 864] [Article Influence: 50.8] [Reference Citation Analysis (0)] |
| 219. | Zhu TM, Li H, Jin RJ, Zheng Z, Luo Y, Ye H, Zhu HM. Effects of electroacupuncture combined psycho-intervention on cognitive function and event-related potentials P300 and mismatch negativity in patients with internet addiction. Chin J Integr Med. 2012;18:146-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 220. | Liu TC, Desai RA, Krishnan-Sarin S, Cavallo DA, Potenza MN. Problematic Internet use and health in adolescents: data from a high school survey in Connecticut. J Clin Psychiatry. 2011;72:836-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 107] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 221. | Mythily S, Qiu S, Winslow M. Prevalence and correlates of excessive Internet use among youth in Singapore. Ann Acad Med Singapore. 2008;37:9-14. [PubMed] |
| 222. | Guo J, Chen L, Wang X, Liu Y, Chui CH, He H, Qu Z, Tian D. The relationship between Internet addiction and depression among migrant children and left-behind children in China. Cyberpsychol Behav Soc Netw. 2012;15:585-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 77] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 223. | Wang L, Luo J, Bai Y, Kong J, Gao W, Sun X. Internet addiction of adolescents in China: Prevalence, predictors, and association with well-being. Addict Res Theor. 2013;21:62-69. [DOI] [Full Text] |
| 224. | Ko CH, Yen JY, Yen CF, Chen CS, Wang SY. The association between Internet addiction and belief of frustration intolerance: the gender difference. Cyberpsychol Behav. 2008;11:273-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 52] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 225. | Yen JY, Ko CH, Yen CF, Wu HY, Yang MJ. The comorbid psychiatric symptoms of Internet addiction: attention deficit and hyperactivity disorder (ADHD), depression, social phobia, and hostility. J Adolesc Health. 2007;41:93-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 506] [Cited by in RCA: 430] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 226. | Yen CF, Ko CH, Yen JY, Chang YP, Cheng CP. Multi-dimensional discriminative factors for Internet addiction among adolescents regarding gender and age. Psychiatry Clin Neurosci. 2009;63:357-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 112] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 227. | Kim K, Ryu E, Chon MY, Yeun EJ, Choi SY, Seo JS, Nam BW. Internet addiction in Korean adolescents and its relation to depression and suicidal ideation: a questionnaire survey. Int J Nurs Stud. 2006;43:185-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 454] [Cited by in RCA: 381] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 228. | Morrison CM, Gore H. The relationship between excessive Internet use and depression: a questionnaire-based study of 1,319 young people and adults. Psychopathology. 2010;43:121-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 214] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 229. | Whang LS, Lee S, Chang G. Internet over-users’ psychological profiles: a behavior sampling analysis on internet addiction. Cyberpsychol Behav. 2003;6:143-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 388] [Cited by in RCA: 283] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 230. | Ni X, Yan H, Chen S, Liu Z. Factors influencing internet addiction in a sample of freshmen university students in China. Cyberpsychol Behav. 2009;12:327-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 164] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 231. | Huang RL, Lu Z, Liu JJ, You YM, Pan ZQ, Wei Z, He Q, Wang ZZ. Features and predictors of problematic internet use in Chinese college students. Behav Inform Tech. 2009;28:485-490. [DOI] [Full Text] |
| 232. | Lin MP, Ko HC, Wu JY. Prevalence and psychosocial risk factors associated with internet addiction in a nationally representative sample of college students in Taiwan. Cyberpsychol Behav Soc Netw. 2011;14:741-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 142] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 233. | Yeh YC, Ko HC, Wu JY, Cheng CP. Gender differences in relationships of actual and virtual social support to Internet addiction mediated through depressive symptoms among college students in Taiwan. Cyberpsychol Behav. 2008;11:485-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 63] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 234. | Nie NH, Hillygus DS, Erbring L. Internet use, interpersonal relations, and sociability: A time diary study. The Internet in everyday life. Oxford: Blackwell 2002; 215-243. |
| 235. | Kuss DJ, Louws J, Wiers RW. Online gaming addiction? Motives predict addictive play behavior in massively multiplayer online role-playing games. Cyberpsychol Behav Soc Netw. 2012;15:480-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 176] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 236. | Ko CH, Yen JY, Chen CS, Yeh YC, Yen CF. Predictive values of psychiatric symptoms for internet addiction in adolescents: a 2-year prospective study. Arch Pediatr Adolesc Med. 2009;163:937-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 304] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 237. | Yen JY, Ko CH, Yen CF, Chen SH, Chung WL, Chen CC. Psychiatric symptoms in adolescents with Internet addiction: Comparison with substance use. Psychiatry Clin Neurosci. 2008;62:9-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 157] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 238. | Bakken IJ, Wenzel HG, Götestam KG, Johansson A, Oren A. Internet addiction among Norwegian adults: a stratified probability sample study. Scand J Psychol. 2009;50:121-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 162] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 239. | Markham AN. Life online. Researching real experience in virtual space. Walnut Creek, CA: AltaMira 1998; . |
| 240. | Suler J. The online disinhibition effect. Cyberpsychol Behav. 2004;7:321-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1942] [Cited by in RCA: 998] [Article Influence: 45.4] [Reference Citation Analysis (0)] |
| 241. | Walther JB. Computer-mediated communication: Impersonal, interpersonal, and hyperpersonal interaction. Communicat Res. 1996;23:3-43. [DOI] [Full Text] |
| 242. | Huang MP, Alessi NE. Internet addiction, Internet psychotherapy - Reply. Amer J Psychiatry. 1997;154:890. |
| 243. | Fu KW, Chan WS, Wong PW, Yip PS. Internet addiction: prevalence, discriminant validity and correlates among adolescents in Hong Kong. Br J Psychiatry. 2010;196:486-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 151] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 244. | Lange KW, Reichl S, Lange KM, Tucha L, Tucha O. The history of attention deficit hyperactivity disorder. ADHD. 2010;2:241-255. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 205] [Cited by in RCA: 171] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 245. | Hunt RD. Functional roles of norepinephrine and dopamine in ADHD. Medscape Psychiatry. 2006;11:1-4. |
| 246. | Preskorn SH, Ross R, Stanga CY. Selective Serotonin Reuptake Inhibitors. Antidepressants: Past, present and future. Berlin: Springe 2004; 241-262. |
| 247. | Olkkola KT, Ahonen J. Midazolam and other benzodiazepines. Handb Exp Pharmacol. 2008;182:335-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 291] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 248. | Brayfield A. Martindale: The complete drug reference. 38th ed, 2014. . |
| 249. | American Psychological Association. Psychotherapy: Understanding group therapy: American Psychological Association, 2015. . |
| 250. | Moretti MM, Peled M. Adolescent-parent attachment: Bonds that support healthy development. Paediatr Child Health. 2004;9:551-555. [PubMed] |
| 251. | Liddle HA. Family-based therapies for adolescent alcohol and drug use: research contributions and future research needs. Addiction. 2004;99 Suppl 2:76-92. [PubMed] |
| 252. | Davis RA. A cognitive-behavioral model of pathological Internet use. Comp Hum Behav. 2001;17:187-195. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1401] [Cited by in RCA: 1241] [Article Influence: 49.6] [Reference Citation Analysis (0)] |
| 253. | Lohr JM, Olatunji BO, Parker L, DeMaio C. Experimental analysis of specific treatment factors: efficacy and practice implications. J Clin Psychol. 2005;61:819-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 254. | Gupta SK. Intention-to-treat concept: A review. Pers Clin Res. 2011;2:109-112. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1242] [Cited by in RCA: 1322] [Article Influence: 88.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Lai C S- Editor: Qi Y L- Editor: A E- Editor: Jiao XK