Published online Jan 19, 2026. doi: 10.5498/wjp.v16.i1.112733
Revised: October 1, 2025
Accepted: November 7, 2025
Published online: January 19, 2026
Processing time: 118 Days and 21.8 Hours
Anxiety, depression, and other negative emotions are common among patients with chronic renal failure (CRF). Analyzing the factors related to negative emo
To explore the correlations among life satisfaction, pleasure levels, and negative emotions in patients with CRF.
One hundred patients with CRF who received therapy at the First Affiliated Hospital of Jinzhou Medical University between December 2022 and February 2025 were included. The Depression, Anxiety, and Stress Scale (DASS-21), Satisfaction with Life Scale (SWLS), and Temporal Experience of Pleasure Scale (TEPS) were used to evaluate negative emotions, life satisfaction, and pleasure level, respectively. Pearson’s correlation coefficient analyzed the correlation between life satisfaction, pleasure level, and negative emotions. Linear regression analysis identified the factors affecting negative emotions.
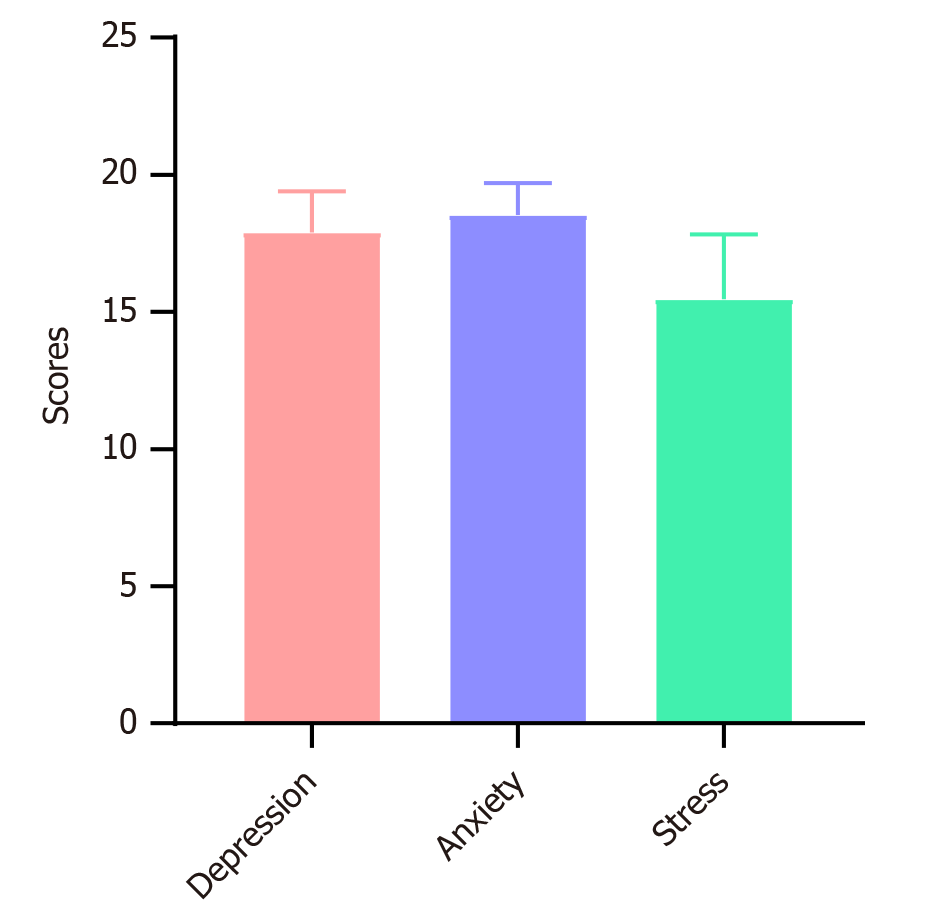
The average DASS-21 score among patients with CRF was 51.90 ± 2.30, with subscale scores of 17.90 ± 1.50 for depression, 18.53 ± 1.18 for anxiety, and 15.47 ± 2.36 for stress, all significantly higher than the domestic norm (P < 0.05). The average SWLS score was 22.17 ± 4.90. Correlation analysis revealed a negative correlation between the SWLS and total DASS-21 scores (P < 0.05), but not with the individual depression, anxiety, or stress dimensions. The average TEPS score was 67.80 ± 8.34. TEPS scores were negatively correlated with the DASS-21 score and the stress dimension (P < 0.05), but not with depression or anxiety. Linear regression analysis showed that TEPS scores significantly influenced DASS-21 scores (P < 0.05).
Patients with CRF experience high levels of negative emotions, which are negatively correlated with life satis
Core Tip: Evidence on how life satisfaction and pleasure levels influence negative emotions in patients with chronic renal failure is limited. In this study of 100 patients with chronic renal failure, life satisfaction and pleasure levels were negatively correlated with negative emotions. Notably, pleasure level affected negative emotions. The findings highlight the need for emotional care during treatment.
- Citation: Zhang LL, Zhang YL, Liu T, Wang J, Chen C, Wang XY. Correlation between life satisfaction, pleasure level, and negative emotion in patients with chronic renal failure. World J Psychiatry 2026; 16(1): 112733
- URL: https://www.wjgnet.com/2220-3206/full/v16/i1/112733.htm
- DOI: https://dx.doi.org/10.5498/wjp.v16.i1.112733
Chronic renal failure (CRF) is a clinical syndrome characterized by acid-base imbalance and systemic organ involvement due to persistent chronic renal dysfunction, resulting in significant renal atrophy and an inability to maintain basic functions[1]. Patients with CRF are prone to different degrees of mental health problems due to the long-term burden of illness, lack of social function, and adverse treatment effects. Negative emotions such as anxiety and depression are particularly common[2]. Traditionally, psychological interventions for patients with CRF were mostly aimed at eliminating negative emotions. However, the role of positive psychological dimensions has been neglected. Life satisfaction refers to an individual’s overall subjective evaluation of their living conditions, while pleasure reflects the experience of happiness derived from daily activities. Both are cognitive components of psychological well-being and the main indicators in quality-of-life evaluation. Currently, it is believed that anxiety, depression, and other negative emotions negatively affect the quality of life of patients with CRF[3,4]. However, there are few reports on the effects of life satisfaction and pleasure levels on negative emotions. Therefore, this study aimed to examine the correlations among life satisfaction, pleasure level, and negative emotions in patients with CRF to provide a reference for psychological intervention.
A total of 100 patients with CRF who received therapy at The First Affiliated Hospital of Jinzhou Medical University between December 2022 and February 2025 were included in the study. The inclusion criteria were as follows: (1) Clinical diagnosis of CRF; (2) Age ≥ 18 years; (3) Received standard maintenance hemodialysis for 4 hours 3 times a week using bicarbonate dialysate; (4) Hemodialysis treatment for ≥ 6 months; (5) Ability to communicate verbally; and (6) Willingness to participate in the study. The exclusion criteria were as follows: (1) An estimated survival time of < 6 months; (2) Serious accidents in the past three months; (3) Severe physical diseases; (4) Mental illness; (5) Cognitive impairment; and (6) Poor compliance or inability to cooperate with the survey. This study was reviewed and approved by the Ethics Committee of The First Affiliated Hospital of Jinzhou Medical University.
According to the Kendall method[5], the sample size should be 5-10 times the number of variables, with a total of 12 variables in this study, and considering 20% inefficiency, the sample size range is 72-144 cases, that is, at least 72 cases are required for this study.
(1) Demographic characteristics questionnaire: A self-designed questionnaire was used to collect general demographic data, including age, sex, marital status, education level, course of disease, and source of medical expenses; (2) Depression, Anxiety, and Stress Scale (DASS-21)[6]. The DASS-21 includes three dimensions: Depression, anxiety, and stress. Each dimension contains seven questions (21 items total). Responses are scored on a 4-point Likert scale (0-3), ranging from “did not apply to me” to “applied to me always”. The total score ranges from 0 to 63, with higher scores indicating severe depression, anxiety, and stress. The Chinese version of the DASS-21 has a Cronbach’s alpha of 0.91; (3) Satisfaction with Life Scale (SWLS)[7]: The SWLS includes five questions rated on a 7-point Likert scale, where responses range from “strongly disagree” to “strongly agree”. The total score ranges from 5 to 35, with higher scores indicating greater life satisfaction. The Chinese version of the SWSL has a Cronbach’s alpha of 0.78; and (4) Temporal Experience of Pleasure Scale (TEPS)[8]: The TEPS assesses pleasure through 20 items describing various pleasurable situations. Items are rated on a 6-point Likert scale (1-6), from “not like me at all” to “very true of me”. The total score ranges from 20 to 120, with higher scores indicating a greater capacity to experience pleasure. The Chinese version of the TEPS has a Cronbach’s alpha of 0.83.
The study was conducted by researchers who received uniform training. A questionnaire survey was administered at the hospital. Before the survey, the researchers used standardized and unified instructions to introduce the purpose, significance, questionnaire completion requirements, and data confidentiality measures to the respondents. To ensure accuracy and authenticity, all questionnaires were completed anonymously. Upon collection, the investigators examined the recovered questionnaires. Incomplete or invalid responses (e.g., careless answers or substantial missing data) were excluded. Valid questionnaires were numbered and entered for analyses.
Data analysis was performed using SPSS version 26.0. General demographic data were described using frequency distributions. Quantitative data with non-normal distributions were presented as mean ± SD, and an independent sample t-test was adopted for comparison. Pearson correlation coefficients were used for correlation analyses, while linear regression analysis was used to identify the factors influencing negative emotions. Statistical significance was set at P < 0.05.
The average DASS-21 score among patients with CRF was 51.90 ± 2.30. Scores for the three dimensions (depression, anxiety, and stress) were significantly higher than those of the domestic norm (P < 0.05; Table 1). Among the three dimensions, the mean scores ranked from highest to lowest as follows: Anxiety, depression, and stress (Figure 1).
Differences in total DASS-21 scores were analyzed across various demographic and clinical variables. There were no statistically significant differences in average DASS-21 scores based on age, sex, disease course, duration of dialysis, hypertension or diabetes, marital status, education level, place of residence, monthly income per capita, or medical expenses (P > 0.05; Table 2).
| Variable | Case | Mean | SD | t/F | P value |
| Age | 1.118 | 0.266 | |||
| < 48 years | 49 | 52.24 | 2.98 | ||
| ≥ 48 years | 51 | 51.57 | 3.01 | ||
| Disease course | 0.415 | 0.679 | |||
| < 4.3 years | 47 | 51.77 | 2.94 | ||
| ≥ 4.3 years | 53 | 52.02 | 3.07 | ||
| Hemodialysis age | 0.199 | 0.843 | |||
| < 4.0 years | 49 | 51.84 | 2.92 | ||
| ≥ 4.0 years | 51 | 51.96 | 3.10 | ||
| Gender | 1.218 | 0.226 | |||
| Male | 59 | 52.20 | 2.98 | ||
| Female | 41 | 51.46 | 3.00 | ||
| Hypertension | 0.779 | 0.438 | |||
| No | 63 | 52.08 | 2.78 | ||
| Yes | 37 | 51.59 | 3.34 | ||
| Diabetes | 1.334 | 0.185 | |||
| No | 84 | 51.73 | 2.96 | ||
| Yes | 16 | 52.81 | 3.12 | ||
| Marital status | 0.036 | 0.964 | |||
| Married | 84 | 51.92 | 2.97 | ||
| Divorced | 12 | 51.92 | 3.06 | ||
| Loss of spouse | 4 | 51.50 | 4.20 | ||
| Educational level | 1.584 | 0.210 | |||
| Junior high school and below | 49 | 52.18 | 3.13 | ||
| High school or technical secondary school | 35 | 51.20 | 2.82 | ||
| College and above | 16 | 52.56 | 2.83 | ||
| Place of abode | 0.594 | 0.554 | |||
| City | 22 | 52.50 | 2.82 | ||
| Town | 32 | 51.63 | 2.84 | ||
| Village | 46 | 51.80 | 3.20 | ||
| Family per capita monthly income | 0.371 | 0.774 | |||
| ≤ 1000 yuan | 28 | 52.39 | 3.39 | ||
| 1000-3000 yuan | 34 | 51.73 | 3.01 | ||
| 3000-5000 yuan | 30 | 51.68 | 2.97 | ||
| ≥ 5000 yuan | 8 | 51.50 | 1.77 | ||
| Source of medical expenses | 0.898 | 0.371 | |||
| Medical insurance | 94 | 51.97 | 3.02 | ||
| Private expense | 6 | 50.83 | 2.64 |
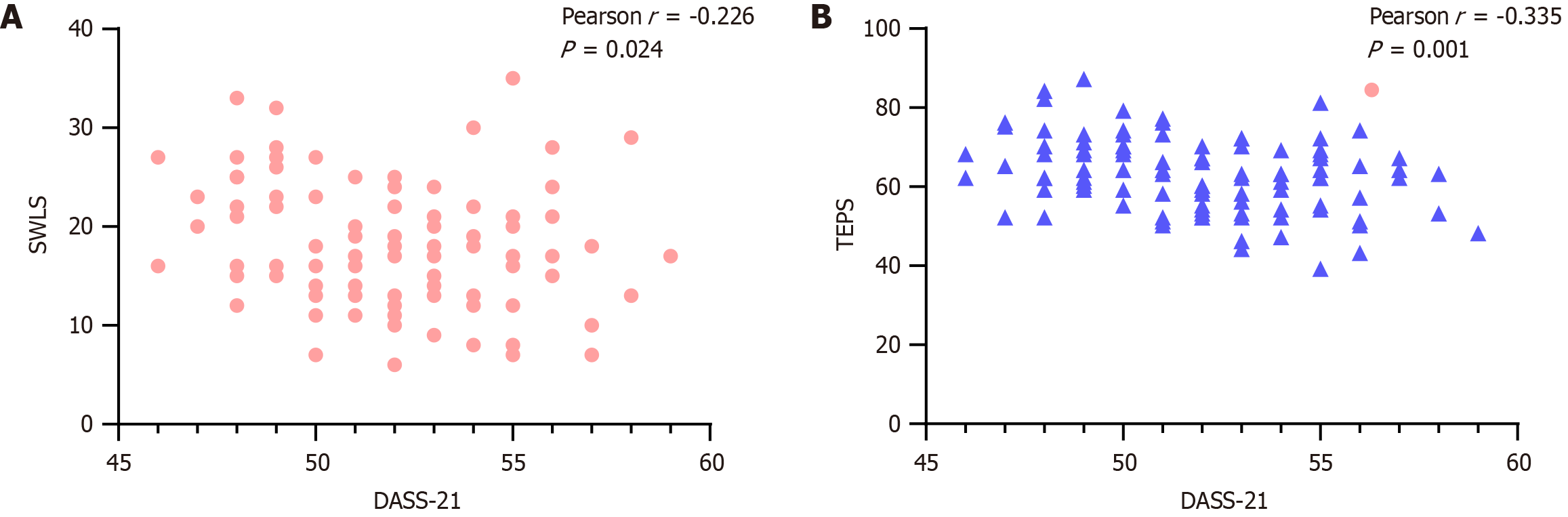
The SWLS scores ranged from 7 to 32, with an average of 22.17 ± 4.90. TEPS scores ranged from 45 to 90, with an average of 67.80 ± 8.34. Pearson correlation analysis revealed a negative correlation between SWSL and DASS-21 scores (r = -0.226, P = 0.024; Figure 2A). Similarly, TEPS scores were negatively correlated with DASS-21 scores (r = -0.335, P = 0.001; Figure 2B). When analyzing the individual dimensions of the DASS-21, SWLS scores were not significantly correlated with any of the three dimensions (P > 0.05). However, TEPS scores were negatively correlated with the stress dimension (r = -0.284, P = 0.004; Table 3).
| Depression | Anxiety | Stress | ||||
| r | P value | r | P value | r | P value | |
| SWLS | -0.156 | 0.120 | 0.014 | 0.894 | -0.195 | 0.052 |
| TEPS | -0.121 | 0.231 | -0.131 | 0.194 | -0.284 | 0.004 |
To identify influencing factors, DASS-21 scores were used as the dependent variable, while SWLS and TEPS scores were included as independent variables in a linear regression equation. The results showed that TEPS scores had a statistically significant effect on DASS-21 scores (P < 0.05; Table 4).
| Variable | B | SE | β | t | P value |
| Constant | 59.425 | 1.958 | 30.352 | < 0.001 | |
| SWLS | -0.082 | 0.047 | -0.168 | -1.751 | 0.083 |
| TEPS | -0.096 | 0.030 | -0.303 | -3.160 | 0.002 |
According to statistics from the International Association of Kidney Diseases, the global annual incidence of CRF is approximately 98-198 cases/million population[9]. In China, the incidence is estimated at 1.7%, with about 100 patients with CRF per million population[10]. As the disease progresses irreversibly toward end-stage renal failure, kidney transplantation remains the only curative treatment. However, due to the scarcity of donor kidneys, maintenance hemodialysis is the primary clinical intervention. Based on the principle of a semi-permeable membrane, hemodialysis removes harmful metabolic wastes and excess electrolytes; purifies the blood; corrects fluid, electrolyte, and acid-base imbalances; partially replaces renal function; and prolongs survival time[11].
Despite its benefits, long-term maintenance hemodialysis is often accompanied by endocrine dysfunction that may lead to complications such as hypertension, arrhythmia, and heart failure[12]. These complications not only threaten physical health but also cause psychological distress. Many patients perceive themselves as burdens on their families and experience reduced self-worth owing to their dependence and limited autonomy, often resulting in persistent negative emotional states. In this study, the DASS-21 was used to evaluate the emotional state of patients with CRF. Among the three subscales, anxiety had the highest average score, and all subscales were higher than the domestic norms, indicating that patients with CRF experience elevated negative emotions, with anxiety being the most prominent.
Gadia et al[13] found that among 100 patients with chronic kidney disease undergoing continuous blood purification, the prevalence rates of anxiety and depression were 66% and 61%, respectively, and were significantly correlated with sex, occupation, and dialysis duration. Similarly, Mosleh et al[14] found that among 122 patients with chronic kidney disease who received hemodialysis, 24.6% had depressive symptoms and 19.7% had anxiety symptoms, both significantly correlated with age and sex, but not with disease course, dialysis duration, or education level. Our study analyzed the demographic characteristics and found no significant differences in DASS-21 scores based on age, sex, or disease course. This discrepancy may be related to differences in inclusion and exclusion criteria as well as the different scales used. Additionally, this study showed that SWLS scores were negatively correlated with DASS-21 scores, indicating that lower life satisfaction is associated with higher levels of negative emotions in patients with CRF.
Patients experiencing negative emotions often have impaired psychological adjustment abilities, which can directly exacerbate physical symptoms. After physical and social function decline, patients commonly experience reduced capacity for daily activities and social participation, leading to a diminished quality of life. This decline may, in turn, negatively impact their life satisfaction[15]. A study has shown that life satisfaction in patients with chronic kidney disease is positively correlated with positive coping styles[16]. We believe that reduced life satisfaction and poor treatment compliance negatively affect treatment outcomes and may further aggravate negative emotions. Our results also showed a negative correlation between TEPS scores and DASS-21 scores in patients with CRF. Linear regression analysis confirmed that TEPS scores had a statistically significant effect on DASS-21 scores, suggesting that the level of pleasure experienced influences negative emotional states in these patients. This may be because, due to energy depletion and physical fatigue, patients often abandon former hobbies and social activities. Additionally, psychological distress can cause loss of interest in previously enjoyed activities and social withdrawal, resulting in social alienation. Social alienation is a negative coping style that can contribute to the development of negative emotions[17,18].
Currently, healthcare providers often focus on physical disease management, ignoring patients’ psychological well-being. The psychological burden is usually assessed subjectively by patients themselves or their families[19]. Therefore, based on the findings of this study, it is recommended to implement a personalized pleasure activation program in which healthcare professionals assess and encourage patients to regain or develop personal interests (such as listening to music, gardening), and ensure that it is feasible during treatment through adaptive adjustments. In addition, structured group psychological interventions, such as mindfulness training or art therapy groups should be implemented to help patients find pleasure in the present experience, and enhance social support and counter social alienation in group interactions. Family collaborative participation must be promoted, family members should be encouraged to consciously recreate shared happy moments (such as preparing meals together, reviewing family photos) through health education, and transform family support into real-time enjoyable experiences. In addition, the role of positive communication of medical staff should be adequately defined, affirming the patient’s efforts and value in daily interactions, encouraging them to share positive experiences, and enhancing their sense of self-worth from medical relationships.
This study has certain limitations. First, this is a cross-sectional study that reveals correlations between variables, but cannot infer causality, which needs to be clarified through longitudinal studies or intervention trials in the future. Secondly, although no significant impact of demographic variables on negative emotional total scores has been found, there may be undetected interactions or subgroup effects, and more complex statistical models (such as moderation or mediating effect models) need to be introduced in the future to further explore the mechanism of social support, coping styles and other factors in the relationship between life satisfaction, pleasure and negative emotions. In addition, this study is a single-center study with a limited sample size, which may affect the generalizability of the results, and therefore, the outcomes of this study should be interpreted with caution.
In summary, patients with CRF exhibited high levels of negative emotions, which were negatively correlated with life satisfaction and pleasure levels. Notably, pleasure level significantly influenced negative emotions.
| 1. | Pabst D, Sanchez-Cueva PA, Soleimani B, Brehm CE. Predictors for acute and chronic renal failure and survival in patients supported with veno-arterial extracorporeal membrane oxygenation. Perfusion. 2020;35:402-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Huang J, Mao Y, Zhao X, Liu Q, Zheng T. Association of anxiety, depression symptoms and sleep quality with chronic kidney disease among older Chinese. Medicine (Baltimore). 2023;102:e35812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 3. | Alencar SBV, de Lima FM, Dias LDA, Dias VDA, Lessa AC, Bezerra JM, Apolinário JF, de Petribu KC. Depression and quality of life in older adults on hemodialysis. Braz J Psychiatry. 2020;42:195-200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 4. | Guerra F, Di Giacomo D, Ranieri J, Tunno M, Piscitani L, Ferri C. Chronic Kidney Disease and Its Relationship with Mental Health: Allostatic Load Perspective for Integrated Care. J Pers Med. 2021;11:1367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 5. | Charan J, Biswas T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med. 2013;35:121-126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 941] [Cited by in RCA: 1667] [Article Influence: 128.2] [Reference Citation Analysis (0)] |
| 6. | Guo K, Ouyang J, Minhat HS. The mediating role of health literacy between the presence of chronic disease and psychological distress among older persons in Xi'an city of China. BMC Public Health. 2023;23:2530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | Lai CYY, Chen LH, Lai FHY, Fung AWT, Ng SSM. The association between satisfaction with life and anxiety symptoms among Chinese elderly: a moderated mediation analysis. BMC Geriatr. 2023;23:855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Zhou H, Liu W, Fan J, Xia J, Zhu J, Zhu X. The Temporal Experience of Pleasure Scale (TEPS): Measurement Invariance Across Gender in Chinese University Students. Front Psychol. 2019;10:2130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Lubart E, Boguslavsky T, Goltsman G, Muhtaseb S, Matveychuk A. The incidence of acute renal failure and high mortality rate in elderly patients hospitalized with community acquired pneumonia. Exp Gerontol. 2023;179:112242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 10. | Rodriguez RA. Separate and Unequal: Residential Segregation by Race and Incidence of Kidney Failure. J Am Soc Nephrol. 2023;34:1475-1478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Chen Y, Wang S, Huang J, Fu Y, Wen J, Zhou C, Fu Y, Liu L. Application of extracorporeal carbon dioxide removal combined with continuous blood purification therapy in ARDS with hypercapnia in patients with critical COVID-19. Clin Hemorheol Microcirc. 2021;78:199-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Ahmadmehrabi S, Tang WHW. Hemodialysis-induced cardiovascular disease. Semin Dial. 2018;31:258-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 110] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 13. | Gadia P, Awasthi A, Jain S, Koolwal GD. Depression and anxiety in patients of chronic kidney disease undergoing haemodialysis: A study from western Rajasthan. J Family Med Prim Care. 2020;9:4282-4286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Mosleh H, Alenezi M, Al Johani S, Alsani A, Fairaq G, Bedaiwi R. Prevalence and Factors of Anxiety and Depression in Chronic Kidney Disease Patients Undergoing Hemodialysis: A Cross-sectional Single-Center Study in Saudi Arabia. Cureus. 2020;12:e6668. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 15. | Price JD, Amerson NL, Barbour KE, Emuze DV. Prevalence of Frequent Mental Distress Among Illinois Adults With Chronic Conditions: Estimates From the Behavioral Risk Factor Surveillance System, 2011 to 2017. Am J Health Promot. 2020;34:608-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 16. | García Montes JM, Sánchez Elena MJ, Valverde Romera M. The Influence of Coping and Personality Styles on Satisfaction with Life in Patients with Chronic Kidney Disease. Psychol Belg. 2020;60:73-85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Rhee SY, Song JK, Hong SC, Choi JW, Jeon HJ, Shin DH, Ji EH, Choi EH, Lee J, Kim A, Choi SW, Oh J. Intradialytic exercise improves physical function and reduces intradialytic hypotension and depression in hemodialysis patients. Korean J Intern Med. 2019;34:588-598. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 65] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 18. | Sun FK, Hung CM, Yao Y, Fu CF, Tsai PJ, Chiang CY. The Effects of Logotherapy on Distress, Depression, and Demoralization in Breast Cancer and Gynecological Cancer Patients: A Preliminary Study. Cancer Nurs. 2021;44:53-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 19. | Bartholomäus M, Zomorodbakhsch B, Micke O, Prott FJ, Rudolph I, Seilacher E, Hochhaus A, Huebner J. Cancer patients' needs for virtues and physicians' characteristics in physician-patient communication: a survey among patient representatives. Support Care Cancer. 2019;27:2783-2788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/