Published online Jul 19, 2025. doi: 10.5498/wjp.v15.i7.106597
Revised: March 21, 2025
Accepted: April 7, 2025
Published online: July 19, 2025
Processing time: 130 Days and 13.8 Hours
Cognitive impairment in elderly patients with arterial hypertension is an urgent medical and social problem. This is especially important given the high preva
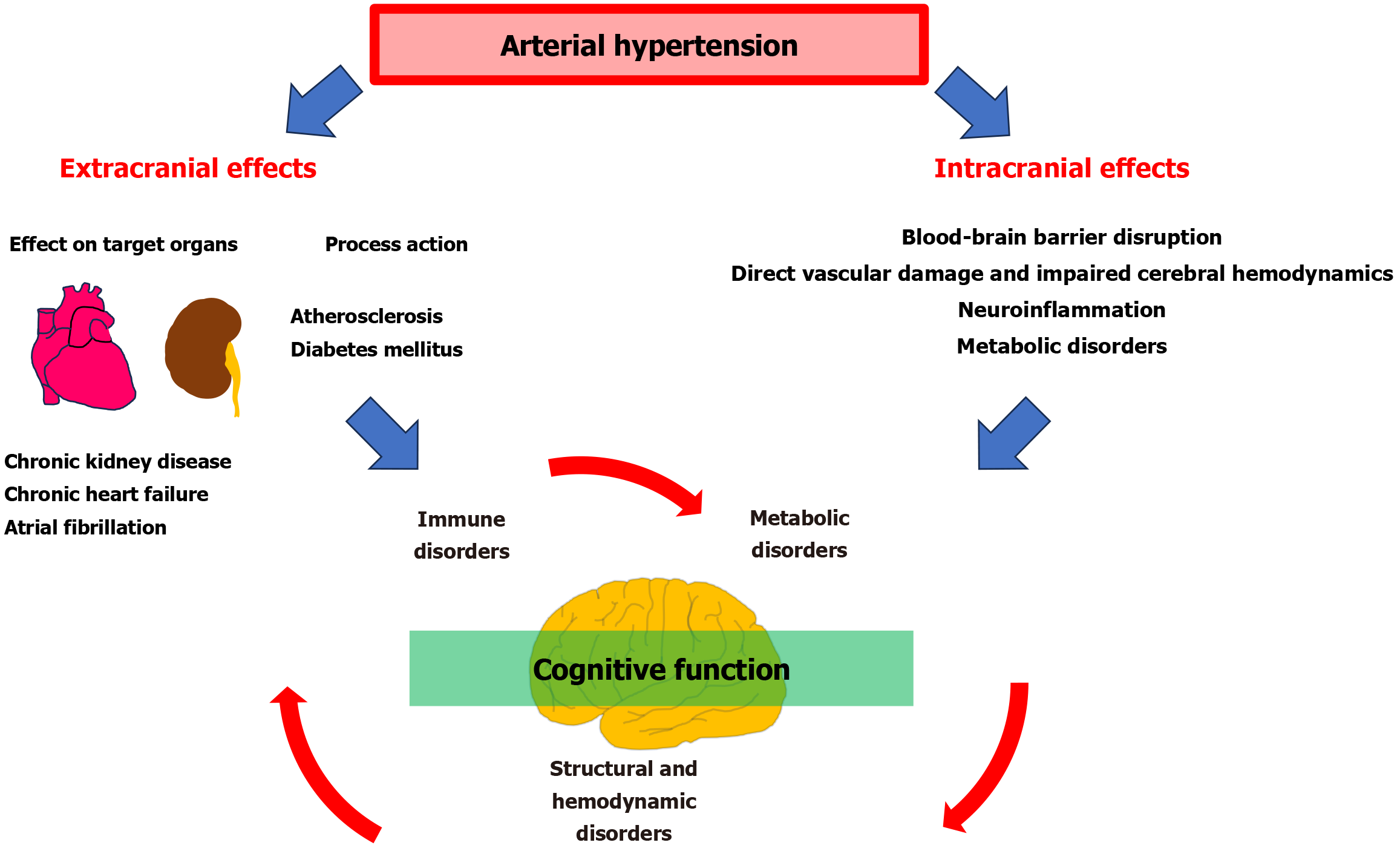
Core Tip: Arterial hypertension contributes to the development of cognitive impairment through several direct and indirect mechanisms involving hemodynamic, structural, immune, and metabolic abnormalities. There is a U-shaped relationship between blood pressure and the risk of cognitive impairment; that is, both high and low blood pressure can contribute to hemodynamic disturbances in the brain and its structural and func
- Citation: Kotlyarov SN. Mechanisms of cognitive impairment in arterial hypertension. World J Psychiatry 2025; 15(7): 106597
- URL: https://www.wjgnet.com/2220-3206/full/v15/i7/106597.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i7.106597
Arterial hypertension is one of the most widespread chronic diseases and contributes significantly to the structure of disability and mortality. The disease is often not diagnosed in a timely manner, and patients often do not pay proper attention to high blood pressure (BP) and do not receive adequate treatment, which leads to the development of numerous complications[1-3]. Arterial hypertension has multiple target organs, including the brain, kidney, and heart[4,5]. The prevalence of arterial hypertension increases with age, which is associated with increased comorbidity with other diseases characteristic of older age groups, such as diabetes mellitus and atherosclerosis, which together impair patients’ quality of life, cause cardiovascular events, and increase the risk of premature death[6-8].
Cognitive impairment in elderly patients with arterial hypertension is an unfavorable prognostic factor, as it impairs patients’ participation in the control of their disease and reduces adherence to treatment, including impaired regular intake of antihypertensive drugs. On the other hand, arterial hypertension itself is considered an important modifiable risk factor for cognitive impairment[9-12]. The results of a systematic review and meta-analysis of 209 prospective studies showed that hypertension in middle age was associated with a 1.19- to 1.55-fold increased risk of cognitive impairment, whereas taking antihypertensive drugs reduced the risk of dementia by 21%[9]. Importantly, there was a U-shaped relationship between BP and risk of cognitive impairment[13]. This is because cerebral hypoperfusion at low BP may also contribute to structural abnormalities in the brain, leading to cognitive impairment[14,15]. This is especially important in patients with atherosclerosis of the carotid and cerebral arteries, as atherosclerosis further impairs cerebral hemodynamics.
A decrease in BP for every 1 mmHg below established thresholds increased the risk of cognitive impairment by 0.7%, 1.1%, and 1.1% for systolic BP, diastolic BP, and mean arterial pressures, respectively. Conversely, exceeding thresholds by 1 mmHg increased the risk of cognitive impairment by 1.2%, 1.8%, and 2.1% for systolic BP, diastolic BP, and mean arterial pressures, respectively[14]. In addition, not only stable high BP is relevant, but also the more common variability of BP in clinical practice[16,17]. Thus, maintaining BP in the target range is an important and effective preventive strategy for complications of arterial hypertension, including the risk of cognitive impairment[18]. In this regard, the mechanisms of cognitive impairment in arterial hypertension are of clinical and research interest. In the article by Xu et al[19], nutritional indicators such as body mass index, Mini-Nutritional Assessment Scale score, hemoglobin, and albumin were found to be associated with indicators of cognitive dysfunction. In general, the current understanding of cognitive impairment in arterial hypertension is based on a complexity of causes that often act together (Figure 1).
Disruption of the structure and function of the blood-brain barrier (BBB) is considered to be the best-known mechanism of cognitive impairment in arterial hypertension. The BBB is formed by dense intercellular connections of endothelial cells, which regulate the entry of substances from the peripheral blood flow into the brain by various mechanisms. In addition to endothelial cells, microglia, pericytes, and astrocytes participate in the regulation of the BBB and form the neurovascular complex[20-22]. In hypertension, neurovascular unit function is impaired, which impairs neurovascular coupling, leads to decreased cerebral blood flow, contribute to neuronal dysfunction and cognitive impairment[23,24]. Hypertension also leads to endothelial dysfunction, impaired autoregulation of cerebral blood flow, causes cerebral small vessel disease, which is characterized by microhemorrhages, lacunar infarcts and white matter damage, contributing to cognitive impairment[25-27]. Ischemic and hemorrhagic stroke are serious complications of hypertension and are associated with various impairments of brain function, including cognitive impairment[28,29]. Small lacunar strokes often have no motor or sensory impairment, but manifest cognitive deficits, forming the clinic of vascular dementia[30,31]. Thus, hemodynamic abnormalities caused by high BP values can disrupt normal histologic and anatomic structures in the brain, which impairs their function. Macrovascular pathologies and microvascular abnormalities leading to structural changes in the brain are closely associated with accelerated cognitive decline and are increasingly recognized as a key factor in the pathogenesis of vascular cognitive impairment and dementia, as well as Alzheimer’s disease (AD)[32].
High BP can impair the function of the BBB, promoting the entry of substances and cells into the brain, which activates many different mechanisms including inflammation and oxidative stress and causes further vascular damage[33]. Infiltration of monocytes and their subsequent differentiation into macrophages promotes microglia activation. Microglia perform immune functions in the brain and, when activated, can produce reactive oxygen species and cytokines that contribute to neuroinflammation and further increase BP. The systemic and neurovascular inflammation that develops in hypertension further damages the BBB and neurovascular unit, contributing to cognitive impairment[34,35]. Chronic activation of renin angiotensin system plays an important role in neuroinflammation.
Under normal conditions, angiotensin II (Ang II) circulating in the bloodstream does not cross the BBB due to its hydrophilic nature. However, elevated blood levels of Ang II in hypertension and impaired BBB integrity promote Ang II entry into the brain, where it contributes to increased sympathetic activity and the development of neurogenic hypertension. Ang II also activates perivascular macrophages that produce superoxide, leading to BBB disruption and cognitive impairment[24,36]. Ang II and prorenin have been found to increase the production of reactive oxygen species and proinflammatory cytokines (interleukin-1 beta [IL-1β], IL-6, tumor necrosis factor alpha) while decreasing IL-10 production in the paraventricular nucleus of the hypothalamus and rostral ventral lateral medulla[37]. Proinflammatory cytokines can impair synaptic plasticity and neuronal communication and disrupt neurogenesis in the hippocampus, which is critical for learning and memory. In addition, neuroinflammation can lead to the loss of synaptic proteins such as postsynaptic density protein-95 and synaptophysin, which are essential for synaptic plasticity and cognitive function[38,39]. Intravenous administration of minocycline, a microglia inhibitor in experiment in rats with hypertension, results in a decrease in BP induced by Ang II administration, and deletion of microglia in transgenic mice with Ang II-induced hypertension results in decreased levels of tumor necrosis factor α and IL-1β and decreased BP[40,41].
Thus, immune mechanisms play an important role in the development of cognitive disorders in arterial hypertension and are a promising topic for further research. It is also relevant to study the relationship of systemic inflammation, which is often found in various chronic diseases and in older individuals with cognitive impairment[42,43]. Chronic systemic inflammation and oxidative stress, for example, are often found in patients with chronic obstructive pulmonary disease, and cognitive impairment is a serious prognostically significant problem in these patients[44-48].
Metabolic disorders including atherosclerosis, obesity, insulin resistance, and diabetes mellitus are common among patients with arterial hypertension, with arterial hypertension contributing to their progression[7]. Studies demonstrate a different association of body mass index (BMI) with cognitive impairment. Each 1 kg/m2 increase in BMI in obese older adults was associated with a 3% increase in the prevalence of cognitive impairment, regardless of comorbidities such as hypertension or diabetes[49]. Low BMI also increased the risk of cognitive impairment, whereas a BMI between 23.2 kg/m2 and 27.8 kg/m2 was associated with a reduced risk of cognitive impairment[50]. A study by Xu et al[19] found that the worse the nutritional status of elderly hypertensive patients, the higher the risk of cognitive impairment. These findings increase interest in the relationship between metabolic factors and cognitive function. The association of atherosclerosis with cerebral circulatory disorders is well known and are the subject of extensive research.
The role of insulin and insulin resistance on cognitive function is of growing interest. Glucose is the main source of energy for the central nervous system (CNS) and is essential for its normal function. However, unlike peripheral tissues, glucose supply to the CNS does not depend on insulin. Glucose transport into the CNS is accomplished by glucose transporter 1 by facilitated diffusion, because the level of glucose in the brain intercellular fluid and cerebrospinal fluid is much lower than in the blood. Insulin has no effect on both glucose transport across the BBB and virtually no effect on glucose utilization by CNS cells, but rather performs neuroprotective functions in the brain, which has deep evolutionary roots[51]. Notably, insulin itself also penetrates the CNS through the BBB (the possibility of insulin synthesis in the brain itself has also been discussed[52]) and in the brain supports neuronal growth, repair, and synaptic viability, and protects against oxidative stress, amyloid-β (Aβ) toxicity, and brain ischemia[53]. Insulin acts as a neuromodulator by affecting the metabolism of neurotransmitters, including dopamine, and modulating the release and uptake of catecholamines and gamma-aminobutyric acid[53-55]. Insulin is critical for cognitive functions, particularly memory formation and storage. It enhances synaptic plasticity, which is essential for learning and memory processes[53-55]. Insulin in the brain acts through two major signaling pathways: The phosphoinositide-3-kinase/Akt pathway, which is responsible for metabolic effects, and the mitogen-activated protein kinase pathway, which affects growth, survival, and gene expression[55]. Insulin and insulin-like growth factor-1 (IGF-1) are linked by some evolutionary and functional relationships in the brain. Insulin and IGF-1 receptors are expressed in all cell types of the CNS[51]. IGF-1 deficiency in hypertensive mice leads to decreased microvascular density, increased neuroinflammation, and impaired cognitive function, underscoring the role of IGF-1 in maintaining brain microvascular health[56,57]. On the other hand, insulin sensitivity index is potentially associated with increased risk of lacunes, severe age-related white matter changes[58]. Thus, insulin and IGF-1 have functions that are important for neuronal survival and maintenance of CNS integrity[59].
Insulin resistance in the brain is considered a cause of the development of AD and is known as type 3 diabetes mellitus, although the term is not universally accepted or used as a diagnostic category, but rather a theoretical concept[60-62]. According to the “type 3 diabetes” hypothesis, AD is proposed to be a form of brain-specific insulin resistance characterized by impaired insulin signaling in brain cells. Insulin resistance in the brain of Alzheimer’s patients is also associated with resistance to IGF-1[63-67]. Brain cell resistance to insulin, oxidative stress and neuroinflammation are thought to contribute to the accumulation of Aβ peptides through several mechanisms. Insulin can activate the extracellular excretion of Aβ and inhibit its intracellular accumulation by activating the cleavage of Aβ by the insulin-degrading enzyme (IDE). IDE regulates the levels of insulin, Aβ protein, and the Aβ precursor protein intracellular domain in vivo[68]. Insulin resistance causes IDE sequestration, thereby reducing Aβ clearance and promoting its aggregation[59,69]. Insulin resistance stimulates the mitogen-activated protein kinase signaling pathway and increases beta-secretase 1 expression, which ultimately leads to abnormal accumulation of Aβ peptides, as beta-secretase 1 is involved in Aβ formation. Insulin resistance also causes decreased activation of the phosphoinositide-3-kinase/Akt signaling pathway and then dephosphorylation and activation of glycogen synthase kinase-3β, which is one of the kinases involved in tau protein phosphorylation. In addition, insulin resistance leads to inhibition of protein phosphatase 2A, which leads to hyperphosphorylation of tau protein and accumulation of neurofibrillary tubules[69].
Thus, insulin and insulin resistance in the brain may have a complex effect on cognitive function. However, insulin resistance in the brain and peripheral tissues (in type 2 diabetes mellitus) are not necessarily related and may occur independently of each other. Furthermore, the functions of insulin in the brain and peripheral tissues differ, which has implications for understanding its role for cognitive function[70-73]. It should be noted that there is ongoing debate as to whether insulin resistance is a cause or consequence of abnormal Aβ expression and protein processing. In this regard, the hypothesis of type 3 diabetes mellitus as a mechanism of AD needs new research. Thus, metabolic abnormalities in arterial hypertension are a frequent phenomenon, especially among elderly patients. The contribution of metabolic abnormalities for cognitive function is still underestimated properly and is a promising topic of study to improve existing therapeutic approaches. In addition, metabolic and inflammatory mechanisms are often combined, which is of clinical importance[74,75].
It should be noted that hypertension may not only act directly through the mechanisms described above, but may also cause target organ damage that also increases the risk of cognitive impairment. Arterial hypertension contributes to the development of chronic kidney disease through several known mechanisms. Low renal function in elderly patients is associated with poorer cognitive function[76,77]. Moreover, in the early stages, chronic kidney disease has a negligible impact on cognitive abilities. At the same time, cognitive abilities are preserved until kidney function deteriorates significantly[78]. The prevalence of cognitive impairment is particularly high in patients on dialysis[79]. Arterial hypertension increases the likelihood of atrial fibrillation (AF), which is associated with structural remodeling of the heart[80]. Early onset of arterial hypertension has been associated with an increased risk of AF and earlier onset of AF[81]. In patients with hypertension, drug treatment can control structural cardiac remodeling and delay or prevent the onset of AF[82]. In turn, AF increases the risk of cognitive impairment and vascular dementia, which is largely mediated by the risk of thromboembolism[83].
Arterial hypertension is also an important cause of chronic heart failure (CHF), which develops as a final outcome of cardiac remodeling[84,85]. CHF is an important cause of reduced quality of life in patients and premature death. CHF is associated with impaired cognitive function through several known mechanisms[86,87]. It has been shown that approximately 62% of patients with CHF did not comply with physician orders due to cognitive impairment. Patients with CHF who did not comply with physician's orders had frontal cognitive impairment (58%), memory impairment (40%), and mixed forms (21%)[88]. Decompensation of CHF further impairs cognitive function[89]. Thus, arterial hypertension may contribute to the development of various diseases due to target organ damage, which may also be a cause of cognitive impairment.
Thus, arterial hypertension is characterized by an increased risk of cognitive impairment, which is based on multiple overlapping mechanisms. A better understanding of hemodynamic, immune and metabolic (including nutritional) causes of cognitive impairment can be used to improve their prognosis, diagnosis and treatment. It is important to note that many aspects of cognitive impairment in arterial hypertension are still unclear and are promising areas for future rese
The metabolic characteristics of cognitive impairment are also of interest. Obesity, insulin resistance and diabetes mellitus represent one side of a broad spectrum of metabolic disorders. Complex problems such as sarcopenic obesity, which includes a combination of obesity and decreased skeletal muscle mass and strength, are of growing interest. Sarco
There is also growing interest in the gut-brain axis, which suggests a link between the gut microbiota and brain function, including cognitive impairment. The gut microbiota under normal conditions produces a large number of bioactive substances, such as short-chain fatty acids, which enter the systemic bloodstream and exert complex effects on various organs[109]. Alterations in the composition of the gut microbiota are associated with cognitive impairment[110,111]. In this regard, the gut microbiota may be a potential biomarker of cognitive impairment and a potential therapeutic target[112-114]. Of interest are the data on how age, the presence of various diseases, and the intake of various medi
| 1. | Pallarés-Carratalá V, Ruiz-García A, Serrano-Cumplido A, Arranz-Martínez E, Divisón-Garrote JA, Moyá-Amengual A, Escobar-Cervantes C, Barrios V. Prevalence Rates of Arterial Hypertension According to the Threshold Criteria of 140/90 or 130/80 mmHg and Associated Cardiometabolic and Renal Factors: SIMETAP-HTN Study. Medicina (Kaunas). 2023;59:1846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 2. | Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16:223-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1423] [Cited by in RCA: 2321] [Article Influence: 386.8] [Reference Citation Analysis (3)] |
| 3. | Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, Chen J, He J. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation. 2016;134:441-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1626] [Cited by in RCA: 2541] [Article Influence: 254.1] [Reference Citation Analysis (1)] |
| 4. | Cortese F, Cecere A, Maria Cortese A, Andriani A, Truncellito L, Valente F, Giordano P, Matteo Ciccone M. Vascular, cardiac and renal target organ damage associated to arterial hypertension: which noninvasive tools for detection? J Hum Hypertens. 2020;34:420-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Kućmierz J, Frąk W, Młynarska E, Franczyk B, Rysz J. Molecular Interactions of Arterial Hypertension in Its Target Organs. Int J Mol Sci. 2021;22:9669. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Long AN, Dagogo-Jack S. Comorbidities of diabetes and hypertension: mechanisms and approach to target organ protection. J Clin Hypertens (Greenwich). 2011;13:244-251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 332] [Cited by in RCA: 318] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 7. | Poznyak AV, Sadykhov NK, Kartuesov AG, Borisov EE, Melnichenko AA, Grechko AV, Orekhov AN. Hypertension as a risk factor for atherosclerosis: Cardiovascular risk assessment. Front Cardiovasc Med. 2022;9:959285. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 106] [Reference Citation Analysis (0)] |
| 8. | Chen Y, Zhou ZF, Han JM, Jin X, Dong ZF, Liu L, Wang D, Ye TB, Yang BS, Zhang YP, Shen CX. Patients with comorbid coronary artery disease and hypertension: a cross-sectional study with data from the NHANES. Ann Transl Med. 2022;10:745. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 9. | Lee CJ, Lee JY, Han K, Kim DH, Cho H, Kim KJ, Kang ES, Cha BS, Lee YH, Park S. Blood Pressure Levels and Risks of Dementia: a Nationwide Study of 4.5 Million People. Hypertension. 2022;79:218-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 10. | Santisteban MM, Iadecola C, Carnevale D. Hypertension, Neurovascular Dysfunction, and Cognitive Impairment. Hypertension. 2023;80:22-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 170] [Article Influence: 56.7] [Reference Citation Analysis (0)] |
| 11. | Swan GE, DeCarli C, Miller BL, Reed T, Wolf PA, Jack LM, Carmelli D. Association of midlife blood pressure to late-life cognitive decline and brain morphology. Neurology. 1998;51:986-993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 271] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 12. | Huang L, Aronow WS. Association of Hypertension with Different Cognitive Disorders. J Clin Med. 2024;13:6029. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Theofilis P, Doumani G, Tsatsani GC, Volis N, Kampourelli A, Thimis V, Xanthopoulou E, Kalaitzidis R. The Role of Hypertension in Cognitive Dysfunction. J Clin Med. 2024;13:5979. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Lv YB, Zhu PF, Yin ZX, Kraus VB, Threapleton D, Chei CL, Brasher MS, Zhang J, Qian HZ, Mao C, Matchar DB, Luo JS, Zeng Y, Shi XM. A U-shaped Association Between Blood Pressure and Cognitive Impairment in Chinese Elderly. J Am Med Dir Assoc. 2017;18:193.e7-193.e13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 15. | Kim D, Yang PS, Jang E, Tae Yu H, Kim TH, Uhm JS, Kim JY, Sung JH, Pak HN, Lee MH, Lip GYH, Joung B. Blood Pressure Control and Dementia Risk in Midlife Patients With Atrial Fibrillation. Hypertension. 2020;75:1296-1304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 16. | Sabayan B, Wijsman LW, Foster-Dingley JC, Stott DJ, Ford I, Buckley BM, Sattar N, Jukema JW, van Osch MJ, van der Grond J, van Buchem MA, Westendorp RG, de Craen AJ, Mooijaart SP. Association of visit-to-visit variability in blood pressure with cognitive function in old age: prospective cohort study. BMJ. 2013;347:f4600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 127] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 17. | Ernst ME, Ryan J, Chowdhury EK, Margolis KL, Beilin LJ, Reid CM, Nelson MR, Woods RL, Shah RC, Orchard SG, Wolfe R, Storey E, Tonkin AM, Brodtmann A, McNeil JJ, Murray AM. Long-Term Blood Pressure Variability and Risk of Cognitive Decline and Dementia Among Older Adults. J Am Heart Assoc. 2021;10:e019613. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 18. | McEvoy JW, McCarthy CP, Bruno RM, Brouwers S, Canavan MD, Ceconi C, Christodorescu RM, Daskalopoulou SS, Ferro CJ, Gerdts E, Hanssen H, Harris J, Lauder L, McManus RJ, Molloy GJ, Rahimi K, Regitz-Zagrosek V, Rossi GP, Sandset EC, Scheenaerts B, Staessen JA, Uchmanowicz I, Volterrani M, Touyz RM; ESC Scientific Document Group. 2024 ESC Guidelines for the management of elevated blood pressure and hypertension. Eur Heart J. 2024;45:3912-4018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1279] [Cited by in RCA: 1096] [Article Influence: 548.0] [Reference Citation Analysis (0)] |
| 19. | Xu Q, Lu SR, Shi ZH, Yang Y, Yu J, Wang Z, Zhang BS, Hong K. Nutritional status of elderly hypertensive patients and its relation to the occurrence of cognitive impairment. World J Psychiatry. 2025;15:103092. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (1)] |
| 20. | McConnell HL, Mishra A. Cells of the Blood-Brain Barrier: An Overview of the Neurovascular Unit in Health and Disease. Methods Mol Biol. 2022;2492:3-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 76] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 21. | Obermeier B, Daneman R, Ransohoff RM. Development, maintenance and disruption of the blood-brain barrier. Nat Med. 2013;19:1584-1596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1302] [Cited by in RCA: 1873] [Article Influence: 144.1] [Reference Citation Analysis (0)] |
| 22. | Daneman R, Prat A. The blood-brain barrier. Cold Spring Harb Perspect Biol. 2015;7:a020412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1272] [Cited by in RCA: 2303] [Article Influence: 209.4] [Reference Citation Analysis (1)] |
| 23. | de Montgolfier O, Pouliot P, Gillis MA, Ferland G, Lesage F, Thorin-Trescases N, Thorin É. Systolic hypertension-induced neurovascular unit disruption magnifies vascular cognitive impairment in middle-age atherosclerotic LDLr(-/-):hApoB(+/+) mice. Geroscience. 2019;41:511-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 24. | Harrison DG, Guzik TJ. Macrophages come to mind as keys to cognitive decline. J Clin Invest. 2016;126:4393-4395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Markus HS, de Leeuw FE. Cerebral small vessel disease: Recent advances and future directions. Int J Stroke. 2023;18:4-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 244] [Reference Citation Analysis (0)] |
| 26. | Liu Y, Dong YH, Lyu PY, Chen WH, Li R. Hypertension-Induced Cerebral Small Vessel Disease Leading to Cognitive Impairment. Chin Med J (Engl). 2018;131:615-619. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 84] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 27. | Meissner A. Hypertension and the Brain: A Risk Factor for More Than Heart Disease. Cerebrovasc Dis. 2016;42:255-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 82] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 28. | El Husseini N, Katzan IL, Rost NS, Blake ML, Byun E, Pendlebury ST, Aparicio HJ, Marquine MJ, Gottesman RF, Smith EE; American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Radiology and Intervention; Council on Hypertension; and Council on Lifestyle and Cardiometabolic Health. Cognitive Impairment After Ischemic and Hemorrhagic Stroke: A Scientific Statement From the American Heart Association/American Stroke Association. Stroke. 2023;54:e272-e291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 285] [Cited by in RCA: 259] [Article Influence: 86.3] [Reference Citation Analysis (0)] |
| 29. | Hägg-Holmberg S, Dahlström EH, Forsblom CM, Harjutsalo V, Liebkind R, Putaala J, Tatlisumak T, Groop PH, Thorn LM; FinnDiane Study Group. The role of blood pressure in risk of ischemic and hemorrhagic stroke in type 1 diabetes. Cardiovasc Diabetol. 2019;18:88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 30. | Jacova C, Pearce LA, Costello R, McClure LA, Holliday SL, Hart RG, Benavente OR. Cognitive impairment in lacunar strokes: the SPS3 trial. Ann Neurol. 2012;72:351-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 92] [Article Influence: 6.6] [Reference Citation Analysis (1)] |
| 31. | Valdés Hernández MDC, Grimsley-Moore T, Chappell FM, Thrippleton MJ, Armitage PA, Sakka E, Makin S, Wardlaw JM. Post-stroke Cognition at 1 and 3 Years Is Influenced by the Location of White Matter Hyperintensities in Patients With Lacunar Stroke. Front Neurol. 2021;12:634460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 32. | Csiszar A, Ungvari A, Patai R, Gulej R, Yabluchanskiy A, Benyo Z, Kovacs I, Sotonyi P, Kirkpartrick AC, Prodan CI, Liotta EM, Zhang XA, Toth P, Tarantini S, Sorond FA, Ungvari Z. Atherosclerotic burden and cerebral small vessel disease: exploring the link through microvascular aging and cerebral microhemorrhages. Geroscience. 2024;46:5103-5132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 42] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 33. | van den Kerkhof M, de Jong JJA, Voorter PHM, Postma AA, Kroon AA, van Oostenbrugge RJ, Jansen JFA, Backes WH. Blood-Brain Barrier Integrity Decreases With Higher Blood Pressure: A 7T DCE-MRI Study. Hypertension. 2024;81:2162-2172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 34. | Nyúl-Tóth Á, Patai R, Csiszar A, Ungvari A, Gulej R, Mukli P, Yabluchanskiy A, Benyo Z, Sotonyi P, Prodan CI, Liotta EM, Toth P, Elahi F, Barsi P, Maurovich-Horvat P, Sorond FA, Tarantini S, Ungvari Z. Linking peripheral atherosclerosis to blood-brain barrier disruption: elucidating its role as a manifestation of cerebral small vessel disease in vascular cognitive impairment. Geroscience. 2024;46:6511-6536. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 50] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 35. | Schreiber S, Arndt P, Morton L, Garza AP, Müller P, Neumann K, Mattern H, Dörner M, Bernal J, Vielhaber S, Meuth SG, Dunay IR, Dityatev A, Henneicke S. Immune system activation and cognitive impairment in arterial hypertension. Am J Physiol Cell Physiol. 2024;327:C1577-C1590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 36. | Pelisch N, Hosomi N, Mori H, Masaki T, Nishiyama A. RAS inhibition attenuates cognitive impairment by reducing blood- brain barrier permeability in hypertensive subjects. Curr Hypertens Rev. 2013;9:93-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 37. | Winklewski PJ, Radkowski M, Wszedybyl-Winklewska M, Demkow U. Brain inflammation and hypertension: the chicken or the egg? J Neuroinflammation. 2015;12:85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 103] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 38. | Qian H, Gao F, Wu X, Lin D, Huang Y, Chen A, Deng J, Gong C, Chen X, Zheng X. Activation of the CD200/CD200R1 axis attenuates neuroinflammation and improves postoperative cognitive dysfunction via the PI3K/Akt/NF-κB signaling pathway in aged mice. Inflamm Res. 2023;72:2127-2144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 39. | Zhang Z, Yuan H, Zhao H, Qi B, Li F, An L. PPARγ activation ameliorates postoperative cognitive decline probably through suppressing hippocampal neuroinflammation in aged mice. Int Immunopharmacol. 2017;43:53-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 40. | Shen XZ, Li Y, Li L, Shah KH, Bernstein KE, Lyden P, Shi P. Microglia participate in neurogenic regulation of hypertension. Hypertension. 2015;66:309-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 130] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 41. | Shi P, Raizada MK, Sumners C. Brain cytokines as neuromodulators in cardiovascular control. Clin Exp Pharmacol Physiol. 2010;37:e52-e57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 74] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 42. | Wichmann MA, Cruickshanks KJ, Carlsson CM, Chappell R, Fischer ME, Klein BE, Klein R, Tsai MY, Schubert CR. Long-term systemic inflammation and cognitive impairment in a population-based cohort. J Am Geriatr Soc. 2014;62:1683-1691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 81] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 43. | Skelly DT, Griffin ÉW, Murray CL, Harney S, O'Boyle C, Hennessy E, Dansereau MA, Nazmi A, Tortorelli L, Rawlins JN, Bannerman DM, Cunningham C. Acute transient cognitive dysfunction and acute brain injury induced by systemic inflammation occur by dissociable IL-1-dependent mechanisms. Mol Psychiatry. 2019;24:1533-1548. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 61] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 44. | Kotlyarov S. Analysis of differentially expressed genes and signaling pathways involved in atherosclerosis and chronic obstructive pulmonary disease. Biomol Concepts. 2022;13:34-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 45. | Chen X, Yu Z, Liu Y, Zhao Y, Li S, Wang L. Chronic obstructive pulmonary disease as a risk factor for cognitive impairment: a systematic review and meta-analysis. BMJ Open Respir Res. 2024;11:e001709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 46. | Peiffer G, Underner M, Perriot J, Fond G. [COPD, anxiety-depression and cognitive disorders: Does inflammation play a major role?]. Rev Mal Respir. 2021;38:357-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 47. | Wang J, Li X, Lei S, Zhang D, Zhang S, Zhang H, Li J. Risk of dementia or cognitive impairment in COPD patients: A meta-analysis of cohort studies. Front Aging Neurosci. 2022;14:962562. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 30] [Reference Citation Analysis (0)] |
| 48. | Siraj RA. Comorbid Cognitive Impairment in Chronic Obstructive Pulmonary Disease (COPD): Current Understanding, Risk Factors, Implications for Clinical Practice, and Suggested Interventions. Medicina (Kaunas). 2023;59:732. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 26] [Reference Citation Analysis (0)] |
| 49. | Feinkohl I, Lachmann G, Brockhaus WR, Borchers F, Piper SK, Ottens TH, Nathoe HM, Sauer AM, Dieleman JM, Radtke FM, van Dijk D, Pischon T, Spies C. Association of obesity, diabetes and hypertension with cognitive impairment in older age. Clin Epidemiol. 2018;10:853-862. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 50. | Dong W, Kan L, Zhang X, Li M, Wang M, Cao Y. Association between body mass index and cognitive impairment in Chinese older adults. Front Public Health. 2023;11:1255101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 51. | Pelle MC, Zaffina I, Giofrè F, Pujia R, Arturi F. Potential Role of Glucagon-like Peptide-1 Receptor Agonists in the Treatment of Cognitive Decline and Dementia in Diabetes Mellitus. Int J Mol Sci. 2023;24:11301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 37] [Reference Citation Analysis (0)] |
| 52. | Mazucanti CH, Liu QR, Lang D, Huang N, O'Connell JF, Camandola S, Egan JM. Release of insulin produced by the choroid plexis is regulated by serotonergic signaling. JCI Insight. 2019;4:e131682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 79] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 53. | Ahlawat A, Walia V, Garg M. Role of Impaired Insulin Signaling in the Pathogenesis of Dementia. In: Current Thoughts on Dementia. Singapore: Springer, 2022: 63-84. [DOI] [Full Text] |
| 54. | Zhao WQ, Chen H, Quon MJ, Alkon DL. Insulin and the insulin receptor in experimental models of learning and memory. Eur J Pharmacol. 2004;490:71-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 333] [Cited by in RCA: 357] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 55. | Sędzikowska A, Szablewski L. Insulin and Insulin Resistance in Alzheimer's Disease. Int J Mol Sci. 2021;22:9987. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 224] [Article Influence: 44.8] [Reference Citation Analysis (0)] |
| 56. | Toth P, Tucsek Z, Tarantini S, Sosnowska D, Gautam T, Mitschelen M, Koller A, Sonntag WE, Csiszar A, Ungvari Z. IGF-1 deficiency impairs cerebral myogenic autoregulation in hypertensive mice. J Cereb Blood Flow Metab. 2014;34:1887-1897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 106] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 57. | Tarantini S, Tucsek Z, Valcarcel-Ares MN, Toth P, Gautam T, Giles CB, Ballabh P, Wei JY, Wren JD, Ashpole NM, Sonntag WE, Ungvari Z, Csiszar A. Circulating IGF-1 deficiency exacerbates hypertension-induced microvascular rarefaction in the mouse hippocampus and retrosplenial cortex: implications for cerebromicrovascular and brain aging. Age (Dordr). 2016;38:273-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 89] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 58. | Zhou M, Wang S, Jing J, Yang Y, Cai X, Meng X, Mei L, Lin J, Li S, Li H, Wei T, Wang Y, Pan Y, Wang Y. Insulin resistance based on postglucose load measure is associated with prevalence and burden of cerebral small vessel disease. BMJ Open Diabetes Res Care. 2022;10:e002897. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 59. | Nguyen TT, Ta QTH, Nguyen TKO, Nguyen TTD, Giau VV. Type 3 Diabetes and Its Role Implications in Alzheimer's Disease. Int J Mol Sci. 2020;21:3165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 249] [Article Influence: 41.5] [Reference Citation Analysis (0)] |
| 60. | Janoutová J, Machaczka O, Zatloukalová A, Janout V. Is Alzheimer's disease a type 3 diabetes? A review. Cent Eur J Public Health. 2022;30:139-143. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 61. | Michailidis M, Moraitou D, Tata DA, Kalinderi K, Papamitsou T, Papaliagkas V. Alzheimer's Disease as Type 3 Diabetes: Common Pathophysiological Mechanisms between Alzheimer's Disease and Type 2 Diabetes. Int J Mol Sci. 2022;23:2687. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 202] [Article Influence: 50.5] [Reference Citation Analysis (0)] |
| 62. | Chandarana CV, Roy S. Comprehensive Review on Neuro-degenerative Type 3 DM. Curr Diabetes Rev. 2022;18:e131221198790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 63. | de la Monte SM, Wands JR. Alzheimer's disease is type 3 diabetes-evidence reviewed. J Diabetes Sci Technol. 2008;2:1101-1113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 714] [Cited by in RCA: 800] [Article Influence: 44.4] [Reference Citation Analysis (0)] |
| 64. | Talbot K, Wang HY, Kazi H, Han LY, Bakshi KP, Stucky A, Fuino RL, Kawaguchi KR, Samoyedny AJ, Wilson RS, Arvanitakis Z, Schneider JA, Wolf BA, Bennett DA, Trojanowski JQ, Arnold SE. Demonstrated brain insulin resistance in Alzheimer's disease patients is associated with IGF-1 resistance, IRS-1 dysregulation, and cognitive decline. J Clin Invest. 2012;122:1316-1338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1129] [Cited by in RCA: 1478] [Article Influence: 105.6] [Reference Citation Analysis (0)] |
| 65. | Steen E, Terry BM, Rivera EJ, Cannon JL, Neely TR, Tavares R, Xu XJ, Wands JR, de la Monte SM. Impaired insulin and insulin-like growth factor expression and signaling mechanisms in Alzheimer's disease--is this type 3 diabetes? J Alzheimers Dis. 2005;7:63-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1100] [Cited by in RCA: 1271] [Article Influence: 60.5] [Reference Citation Analysis (0)] |
| 66. | Rivera EJ, Goldin A, Fulmer N, Tavares R, Wands JR, de la Monte SM. Insulin and insulin-like growth factor expression and function deteriorate with progression of Alzheimer's disease: link to brain reductions in acetylcholine. J Alzheimers Dis. 2005;8:247-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 463] [Cited by in RCA: 547] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 67. | de la Monte SM. Brain insulin resistance and deficiency as therapeutic targets in Alzheimer's disease. Curr Alzheimer Res. 2012;9:35-66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 283] [Cited by in RCA: 340] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 68. | Farris W, Mansourian S, Chang Y, Lindsley L, Eckman EA, Frosch MP, Eckman CB, Tanzi RE, Selkoe DJ, Guenette S. Insulin-degrading enzyme regulates the levels of insulin, amyloid beta-protein, and the beta-amyloid precursor protein intracellular domain in vivo. Proc Natl Acad Sci U S A. 2003;100:4162-4167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1033] [Cited by in RCA: 1142] [Article Influence: 49.7] [Reference Citation Analysis (2)] |
| 69. | Peng Y, Yao SY, Chen Q, Jin H, Du MQ, Xue YH, Liu S. True or false? Alzheimer's disease is type 3 diabetes: Evidences from bench to bedside. Ageing Res Rev. 2024;99:102383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 39] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 70. | Yonamine CY, Michalani MLE, Moreira RJ, Machado UF. Glucose Transport and Utilization in the Hippocampus: From Neurophysiology to Diabetes-Related Development of Dementia. Int J Mol Sci. 2023;24:16480. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 27] [Reference Citation Analysis (0)] |
| 71. | Talbot K. Brain insulin resistance in Alzheimer's disease and its potential treatment with GLP-1 analogs. Neurodegener Dis Manag. 2014;4:31-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 104] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 72. | Rhea EM, Leclerc M, Yassine HN, Capuano AW, Tong H, Petyuk VA, Macauley SL, Fioramonti X, Carmichael O, Calon F, Arvanitakis Z. State of the Science on Brain Insulin Resistance and Cognitive Decline Due to Alzheimer's Disease. Aging Dis. 2024;15:1688-1725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 31] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 73. | Affuso F, Micillo F, Fazio S. Insulin Resistance, a Risk Factor for Alzheimer's Disease: Pathological Mechanisms and a New Proposal for a Preventive Therapeutic Approach. Biomedicines. 2024;12:1888. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 74. | Vinuesa A, Pomilio C, Gregosa A, Bentivegna M, Presa J, Bellotto M, Saravia F, Beauquis J. Inflammation and Insulin Resistance as Risk Factors and Potential Therapeutic Targets for Alzheimer's Disease. Front Neurosci. 2021;15:653651. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 65] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 75. | Grigorescu ED, Lăcătușu CM, Floria M, Cazac GD, Onofriescu A, Ceasovschih A, Crețu I, Mihai BM, Șorodoc L. Association of Inflammatory and Metabolic Biomarkers with Mitral Annular Calcification in Type 2 Diabetes Patients. J Pers Med. 2022;12:1484. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 76. | Lee S, Shimada H, Park H, Makizako H, Lee S, Doi T, Yoshida D, Tsutsumimoto K, Anan Y, Suzuki T. The association between kidney function and cognitive decline in community-dwelling, elderly Japanese people. J Am Med Dir Assoc. 2015;16:349.e1-349.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 77. | Yaffe K, Ackerson L, Kurella Tamura M, Le Blanc P, Kusek JW, Sehgal AR, Cohen D, Anderson C, Appel L, Desalvo K, Ojo A, Seliger S, Robinson N, Makos G, Go AS; Chronic Renal Insufficiency Cohort Investigators. Chronic kidney disease and cognitive function in older adults: findings from the chronic renal insufficiency cohort cognitive study. J Am Geriatr Soc. 2010;58:338-345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 251] [Cited by in RCA: 236] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 78. | Passos VMA, Ladeira RM, Souza CCV, Santos IS, Barreto SM. First stages chronic kidney disease have mild effects on cognitive performance. Results of a 15,105 brazilian adult baseline cohort. J Bras Nefrol. 2018;40:18-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 79. | Murray AM, Tupper DE, Knopman DS, Gilbertson DT, Pederson SL, Li S, Smith GE, Hochhalter AK, Collins AJ, Kane RL. Cognitive impairment in hemodialysis patients is common. Neurology. 2006;67:216-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 452] [Cited by in RCA: 532] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 80. | Kallistratos MS, Poulimenos LE, Manolis AJ. Atrial fibrillation and arterial hypertension. Pharmacol Res. 2018;128:322-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 81. | Lee Y, Shin JH, Kim BS, Kook H, Kim W, Heo R, Lim YH, Shin J, Kim CK, Park JK. Association between Age of Onset of Hypertension and Incident Atrial Fibrillation. J Pers Med. 2022;12:1186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 82. | Naccache S, Ben Kilani M, Tlili R, Ben Ameur Y, Boujnah MR. Atrial fibrillation and hypertension: State of the art. Tunis Med. 2017;95:455-460. [PubMed] |
| 83. | Papanastasiou CA, Theochari CA, Zareifopoulos N, Arfaras-Melainis A, Giannakoulas G, Karamitsos TD, Palaiodimos L, Ntaios G, Avgerinos KI, Kapogiannis D, Kokkinidis DG. Atrial Fibrillation Is Associated with Cognitive Impairment, All-Cause Dementia, Vascular Dementia, and Alzheimer's Disease: a Systematic Review and Meta-Analysis. J Gen Intern Med. 2021;36:3122-3135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 87] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 84. | Oh GC, Cho HJ. Blood pressure and heart failure. Clin Hypertens. 2020;26:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 91] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 85. | Málek F. Arterial hypertension and chronic heart failure. Cor et Vasa. 2013;55:e259-e263. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 86. | Park MS, Kim EJ. A Correlative Relationship Between Heart Failure and Cognitive Impairment: A Narrative Review. J Korean Med Sci. 2023;38:e334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 87. | Goh FQ, Kong WKF, Wong RCC, Chong YF, Chew NWS, Yeo TC, Sharma VK, Poh KK, Sia CH. Cognitive Impairment in Heart Failure-A Review. Biology (Basel). 2022;11:179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 49] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 88. | Shestakova MV, Vasilenko AF, Karpova MI, Grigoricheva EA, Epaneshnikova NV, Kochetkov IV. [Cognitive impairment and compliance in chronic heart failure]. Zh Nevrol Psikhiatr Im S S Korsakova. 2017;117:53-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 89. | Kindermann I, Fischer D, Karbach J, Link A, Walenta K, Barth C, Ukena C, Mahfoud F, Köllner V, Kindermann M, Böhm M. Cognitive function in patients with decompensated heart failure: the Cognitive Impairment in Heart Failure (CogImpair-HF) study. Eur J Heart Fail. 2012;14:404-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 90. | Lithell H, Hansson L, Skoog I, Elmfeldt D, Hofman A, Olofsson B, Trenkwalder P, Zanchetti A; SCOPE Study Group. The Study on Cognition and Prognosis in the Elderly (SCOPE): principal results of a randomized double-blind intervention trial. J Hypertens. 2003;21:875-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1030] [Cited by in RCA: 961] [Article Influence: 41.8] [Reference Citation Analysis (0)] |
| 91. | Zhou Z, Orchard SG, Nelson MR, Fravel MA, Ernst ME. Angiotensin Receptor Blockers and Cognition: a Scoping Review. Curr Hypertens Rep. 2024;26:1-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 28] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 92. | Peters R, Beckett N, Forette F, Tuomilehto J, Clarke R, Ritchie C, Waldman A, Walton I, Poulter R, Ma S, Comsa M, Burch L, Fletcher A, Bulpitt C; HYVET investigators. Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial cognitive function assessment (HYVET-COG): a double-blind, placebo controlled trial. Lancet Neurol. 2008;7:683-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 569] [Cited by in RCA: 494] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 93. | Kartashova ES, Batischeva GA, Zhdanova OA, Sharapova YA. Pharmacoepidemiology of the administration of antihypertensive drugs by doctors in the Voronezh region in comparison with the results of the PYTHAGOR IV study. I P Pavlov Russian Medical Biological Herald. 2021;29:475-482. [DOI] [Full Text] |
| 94. | Qin H, Zhu B, Hu C, Zhao X. Later-Onset Hypertension Is Associated With Higher Risk of Dementia in Mild Cognitive Impairment. Front Neurol. 2020;11:557977. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 95. | Streit S, Poortvliet RKE, Gussekloo J. Lower blood pressure during antihypertensive treatment is associated with higher all-cause mortality and accelerated cognitive decline in the oldest-old. Data from the Leiden 85-plus Study. Age Ageing. 2018;47:545-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 84] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 96. | Iseli R, Nguyen VTV, Sharmin S, Reijnierse EM, Lim WK, Maier AB. Orthostatic hypotension and cognition in older adults: A systematic review and meta-analysis. Exp Gerontol. 2019;120:40-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 97. | Low S, Goh KS, Ng TP, Ang SF, Moh A, Wang J, Ang K, Subramaniam T, Sum CF, Lim SC. The prevalence of sarcopenic obesity and its association with cognitive performance in type 2 diabetes in Singapore. Clin Nutr. 2020;39:2274-2281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 98. | Someya Y, Tamura Y, Kaga H, Sugimoto D, Kadowaki S, Suzuki R, Aoki S, Hattori N, Motoi Y, Shimada K, Daida H, Ishijima M, Kaneko K, Nojiri S, Kawamori R, Watada H. Sarcopenic obesity is associated with cognitive impairment in community-dwelling older adults: The Bunkyo Health Study. Clin Nutr. 2022;41:1046-1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 64] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 99. | Wang H, Hai S, Liu YX, Cao L, Liu Y, Liu P, Yang Y, Dong BR. Associations between Sarcopenic Obesity and Cognitive Impairment in Elderly Chinese Community-Dwelling Individuals. J Nutr Health Aging. 2019;23:14-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 100. | Park SH, Park JH, Song PS, Kim DK, Kim KH, Seol SH, Kim HK, Jang HJ, Lee JG, Park HY, Park J, Shin KJ, Kim Di, Moon YS. Sarcopenic obesity as an independent risk factor of hypertension. J Am Soc Hypertens. 2013;7:420-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 90] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 101. | Yin T, Zhang JX, Wang FX, Zhao JH, Zhao Y, Liu L, Liu XY, Zhang YH, Zhao Y. The Association Between Sarcopenic Obesity and Hypertension, Diabetes, and Abnormal Lipid Metabolism in Chinese Adults. Diabetes Metab Syndr Obes. 2021;14:1963-1973. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 102. | Du R, Yuan J, Huang Y, Jiang G, Duan Z, Yang H, Huang W. Sarcopenia is not associated with hypertension, but sarcopenic obesity increases risk of hypertension: a 7-year cohort study. Front Public Health. 2024;12:1479169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 103. | Fantin F, Giani A, Manzato G, Zampieri A, Comellato G, Urbani S, Zoico E, Mazzali G, Zamboni M. Sarcopenia, sarcopenic obesity, and arterial stiffness among older adults. Front Cardiovasc Med. 2024;11:1272854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 104. | Minaglia C, Giannotti C, Boccardi V, Mecocci P, Serafini G, Odetti P, Monacelli F. Cachexia and advanced dementia. J Cachexia Sarcopenia Muscle. 2019;10:263-277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 105. | Rai M, Demontis F. Muscle-to-Brain Signaling Via Myokines and Myometabolites. Brain Plast. 2022;8:43-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 56] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 106. | Oudbier SJ, Goh J, Looijaard SMLM, Reijnierse EM, Meskers CGM, Maier AB. Pathophysiological Mechanisms Explaining the Association Between Low Skeletal Muscle Mass and Cognitive Function. J Gerontol A Biol Sci Med Sci. 2022;77:1959-1968. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 75] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 107. | Qi JY, Yang LK, Wang XS, Wang M, Li XB, Feng B, Wu YM, Zhang K, Liu SB. Irisin: A promising treatment for neurodegenerative diseases. Neuroscience. 2022;498:289-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 31] [Reference Citation Analysis (0)] |
| 108. | Zhang Y, Zhang X, Lin S. Irisin: A bridge between exercise and neurological diseases. Heliyon. 2022;8:e12352. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 32] [Reference Citation Analysis (0)] |
| 109. | Kincaid HJ, Nagpal R, Yadav H. Diet-Microbiota-Brain Axis in Alzheimer's Disease. Ann Nutr Metab. 2021;77 Suppl 2:21-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 110. | Li B, He Y, Ma J, Huang P, Du J, Cao L, Wang Y, Xiao Q, Tang H, Chen S. Mild cognitive impairment has similar alterations as Alzheimer's disease in gut microbiota. Alzheimers Dement. 2019;15:1357-1366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 345] [Article Influence: 49.3] [Reference Citation Analysis (0)] |
| 111. | Wang J, Zhang G, Lai H, Li Z, Shen M, Li C, Kwan P, O'Brien TJ, Wu T, Yang S, Zhang X, Zhang L. Characterizing Gut Microbiota in Older Chinese Adults with Cognitive Impairment: A Cross-Sectional Study. J Alzheimers Dis. 2024;101:761-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 112. | Sun Y, Baptista LC, Roberts LM, Jumbo-Lucioni P, McMahon LL, Buford TW, Carter CS. The Gut Microbiome as a Therapeutic Target for Cognitive Impairment. J Gerontol A Biol Sci Med Sci. 2020;75:1242-1250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 57] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 113. | Chapelet G, Noble W, Derkinderen P. Microbiota and cognitive impairment: Current challenges and future perspectives. J Alzheimers Dis. 2024;102:311-313. [PubMed] [DOI] [Full Text] |
| 114. | Kolobaric A, Andreescu C, Jašarević E, Hong CH, Roh HW, Cheong JY, Kim YK, Shin TS, Kang CS, Kwon CO, Yoon SY, Hong SW, Aizenstein HJ, Karim HT, Son SJ. Gut microbiome predicts cognitive function and depressive symptoms in late life. Mol Psychiatry. 2024;29:3064-3075. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 29] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/