Published online Nov 19, 2025. doi: 10.5498/wjp.v15.i11.108630
Revised: June 27, 2025
Accepted: October 9, 2025
Published online: November 19, 2025
Processing time: 199 Days and 1.6 Hours
In this commentary, we respond to Zhao et al’s recent paper which focuses on mechanisms underlying insomnia sufferers’ engagement with acupuncture. Insomnia, a prevalent condition characterized by difficulty falling asleep and poor sleep quality, is associated with increased risk of cardiovascular disease, diabetes, and psychiatric illness. Acupuncture, a method involving the therapeutic place
Core Tip: This medical-sociological interdisciplinary study examines factors influencing insomnia patients’ decisions to engage in acupuncture, utilizing the capability, opportunity, motivation - behavior model and theoretical domain framework. Key facilitators of patients’ pursuit of acupuncture include cultural beliefs, concerns about dependence on hypnotic medications, and encouragement from trusted opinion leaders, whereas barriers include limited knowledge, accessibility challenges, and needle phobia. The findings underscore the multifaceted nature of this decision, which is shaped by treatment efficacy, cultural context, economic factors, and communication dynamics. Recommendations for clinicians and policymakers include enhancing patient education, improving treatment accessibility through public health measures, fostering effective physician-patient communication, and addressing needle phobia through cognitive interventions to optimize treatment adherence and outcomes.
- Citation: Lucke-Wold B, Salam HD, Karayi G. Behavioral analysis of insomnia sufferers to acupuncture treatment. World J Psychiatry 2025; 15(11): 108630
- URL: https://www.wjgnet.com/2220-3206/full/v15/i11/108630.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i11.108630
Acupuncture is an ancient therapeutic approach rooted in traditional Chinese medicine, with a history extending back over two millennia. The practice aims to promote health and address disease by restoring equilibrium within the body’s opposing forces of yin and yang. Practitioners insert fine needles at carefully selected points along defined energy pathways, or meridians, to influence the circulation of qi and support internal balance. In China, acupuncture is widely used as a primary intervention for insomnia, and growing clinical evidence suggests that it can improve sleep quality and reduce insomnia symptoms[1]. Recently, cognitive behavioral therapy for insomnia (CBT-I), a nonpharmacological intervention, has become a widely adopted approach for managing insomnia[2]. In their observational study, Zhao et al[3] reported that some insomnia patients were receptive to acupuncture treatment, whereas others were reluctant. Some patients in this study were drawn to acupuncture because of their cultural values, worries about reliance on sleep medications, or encouragement from trusted sources. In contrast, some patients avoided acupuncture due to a lack of awareness, difficulties accessing treatment, and needle-related fears. Interestingly, although insomnia prevalence is higher in older adults (35%-50%), the largest acupuncture cohort studied consisted primarily of individuals under 50 years old (49.2%), perhaps reflecting generational differences in treatment preferences or attitudes toward needles.
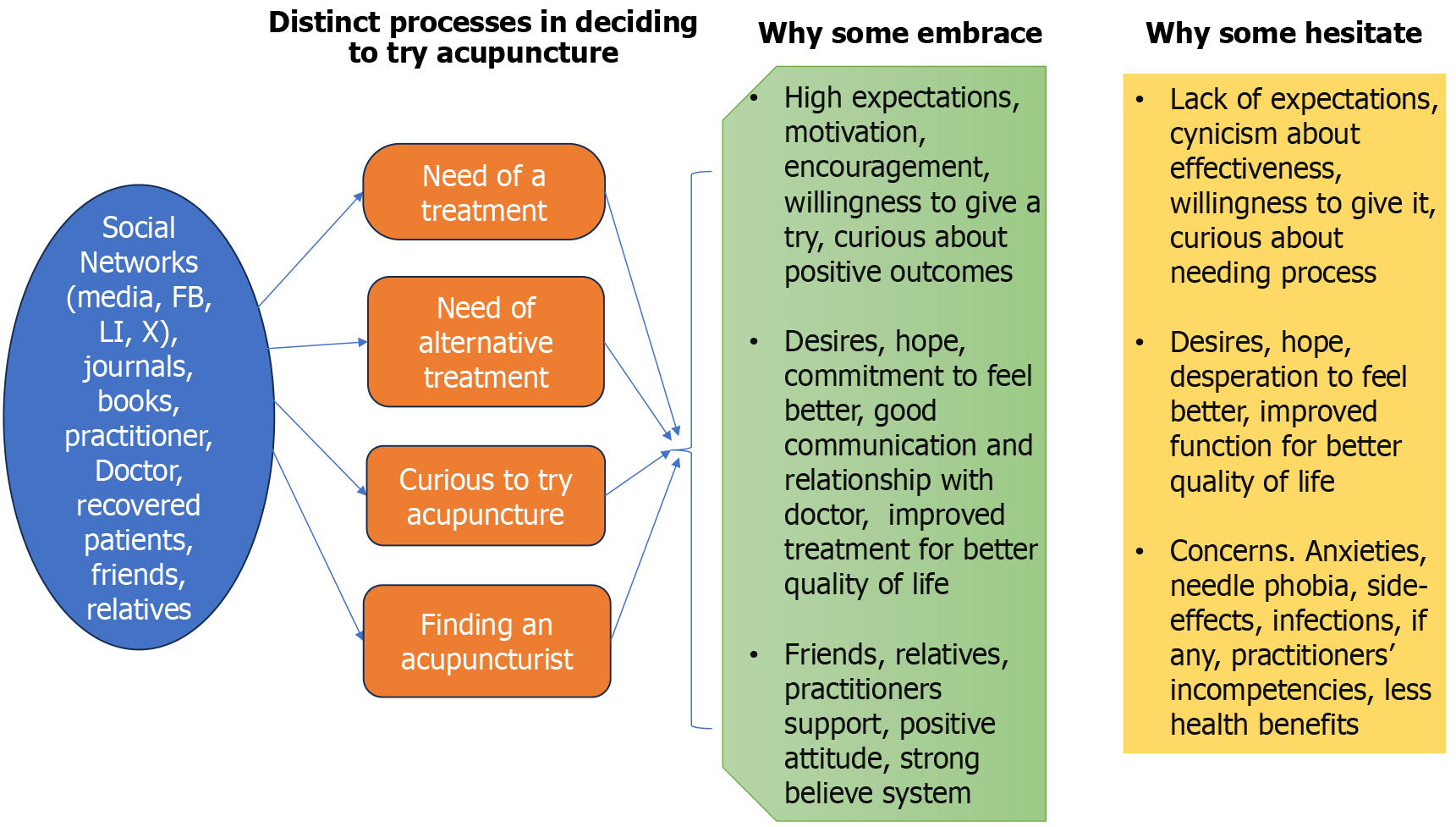
One proposed framework organizes these influences into five domains: Patient factors, practitioner attributes, the therapeutic relationship, features of the treatment itself, and the overall care environment[4,5]. Patients’ choices to pursue acupuncture are shaped by four key steps: Identifying a need for care, considering alternatives to conventional therapies, choosing acupuncture as an option, and locating a qualified practitioner. Throughout this process, guidance and encouragement from family, friends, and healthcare providers often influenced decisions by offering reassurance and increasing awareness. Participants also shared a mix of apprehensions, optimism, and strong expectations regarding both the process and potential benefits of acupuncture[6]. Patients’ preconceived notions and expectations about acupuncture - shaped by its cultural origins and perceived nature - can strongly influence their overall experience and the contextual effects of treatment[7].
As illustrated in the thematic map (Figure 1), participants described a progression of steps that led them from not considering acupuncture to scheduling their initial session. These stages included acknowledging a need for treatment, recognizing limitations of conventional approaches, and ultimately deciding to pursue acupuncture. Positive testimonials shared within personal networks frequently influenced this process. For many individuals, acupuncture was viewed as an attractive option, providing the possibility of therapeutic benefits not attained through conventional medical approaches[8,9]. While some individuals were attracted to acupuncture because of its deep historical roots and non-pharmacologic nature, others sought it out only after conventional treatments proved ineffective or their symptoms persisted, motivating them to explore alternative solutions.
Research suggests that acupuncture can meaningfully alleviate insomnia symptoms and enhance sleep quality, potentially by modulating neurotransmitters such as dopamine and norepinephrine[10]. CBT-I is recognized as the primary nonpharmacological treatment option for insomnia and is generally regarded as having a minimal risk of serious side effects[11]. Prior research has indicated that auricular acupuncture may be more effective than CBT-I in increasing sleep duration among individuals with insomnia[12,13]. Future research could further evaluate different forms of acupuncture alongside CBT-I to guide clinicians in selecting the most appropriate nonpharmacological treatment for patients with insomnia[14]. A wide range of acupuncture approaches is available, including traditional acupuncture, electroacupuncture (EA), eye acupuncture, auricular acupuncture, and transcutaneous acupoint electrical stimulation. The choice of technique often reflects both patient preferences and treatment goals. For example, individuals uncomfortable with needles may favor transcutaneous acupoint electrical stimulation or auricular acupressure, while those seeking stronger stimulation may select EA or combination therapies. However, evidence from comparative effectiveness studies and network meta-analyses indicates that differences in outcomes between these modalities are typically modest, and selection is generally guided by patient needs and practitioner expertise[15].
A third management strategy involves the use of pharmacologic therapies, including benzodiazepine receptor agonists, sedating antidepressants, and orexin receptor antagonists. While these agents can be effective for short-term relief of insomnia symptoms, prolonged use is discouraged due to risks such as dependence, tolerance, and adverse effects - among them cognitive decline, increased fall risk, and withdrawal syndromes. Both the American College of Physicians and the American Academy of Sleep Medicine advise that hypnotic medications be prescribed only for short-term or intermittent use, with close monitoring and gradual tapering if treatment extends beyond several weeks. These concerns are particularly relevant for older adults and patients with underlying health conditions[16].
Conversely, combining acupuncture with pharmacologic treatments has gained growing support in the literature. Evidence from meta-analyses and systematic reviews indicates that this integrative approach - pairing acupuncture with agents such as benzodiazepines or sedating antidepressants - can produce more substantial improvements in sleep quality and insomnia severity compared with medication alone[17]. For instance, a 2019 systematic review found that combining acupuncture with medication resulted in greater improvements in Pittsburgh Sleep Quality Index scores and overall treatment effectiveness compared with medication alone, while also reporting fewer adverse effects in both general and elderly patient groups[18].
Incorporating acupuncture with pharmacologic therapy represents a promising, evidence-based strategy to improve treatment outcomes, reduce the risks associated with prolonged medication use, and provide an alternative for patients reluctant to try acupuncture alone. Findings from Zhao et al[3] also highlight mixed perceptions of treatment. Although many participants preferred nonpharmacological approaches, these were often perceived as requiring greater effort, whereas medications were used cautiously due to concerns about dependency. In another study conducted in Australia, most participants (80.8%) were recruited from a sleep clinic specializing in CBT-I, which possibly biased their views toward psychotherapy, thus limiting the generalizability of these results to healthcare settings in other regions[19].
Practitioner attributes also shape how patients evaluate and prioritize their own health factors, with relaxation techniques, exercise routines, and dietary habits frequently highlighted as important. Expanding practitioner training in these areas could enhance care[20].
Future research should focus on investigating EA stimulation parameters in combination with advanced technologies such as electroencephalography, functional magnetic resonance imaging, and metabolomic profiling. These approaches could provide deeper insight into the multitarget and multidimensional mechanisms underlying EA, optimize its precision in treating various conditions, and ultimately enhance its clinical efficacy[21]. Clarifying the neural mechanisms through which acupuncture alleviates insomnia could also help patients better appreciate its therapeutic basis. Offering clear, evidence-based explanations of EA’s effects may ease treatment-related anxiety, strengthen trust, and support its acceptance as a credible therapy. Presenting these findings in accessible language would further boost patient confidence and encourage engagement with acupuncture[22].
Providing adaptable treatment choices - such as flexible scheduling, multiple treatment settings, options for provider gender, and a range of therapeutic modalities - has been associated with improved outcomes, enhanced perceptions of effectiveness, and greater overall patient satisfaction[23].
We recommend that future studies examine the long-term effects of acupuncture, as it is frequently used for both sustained health maintenance and short-term symptom relief. Further investigation into the client-practitioner relationship and broader relational dynamics within healthcare is also warranted. Notably, the observed negative association between treatment expectations and perceived outcomes, along with the influence of the “powerful others” health locus of control, underscores the importance of exploring factors such as trust, communication style, rapport, and patient engagement in shaping treatment experiences.
Some patients readily adopt acupuncture as a holistic strategy for managing insomnia, while others approach it with caution due to skepticism or specific concerns. Behavioral analyses suggest that decisions around acupuncture use are shaped by multiple factors, including beliefs about its suitability, expectations of its effectiveness, and perceptions that it carries fewer risks than previous treatments. Individuals who opt for acupuncture often display openness to alternative medicine, confidence in its potential benefits, or curiosity despite initial hesitation. Advances in AI-driven acupuncture may further improve outcomes, enable more personalized treatment approaches, and broaden access to effective care.
| 1. | Cao H, Pan X, Li H, Liu J. Acupuncture for treatment of insomnia: a systematic review of randomized controlled trials. J Altern Complement Med. 2009;15:1171-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 113] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 2. | Cho JH, Kremer S, Young J. Who to Refer to a Behavioral Insomnia Clinic? - Recommendations Based on Treatment Rationale and Response Prediction. Curr Sleep Med Rep. 2021;7:213-220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 3. | Zhao FY, Conduit R, Kennedy GA, Xu PJ, Zhang WJ, Ho YS, Fu QQ, Chow CM. Why some embrace and others hesitate? A behavioral analysis of insomnia sufferers' engagement with acupuncture treatment. World J Psychiatry. 2025;15:105802. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (3)] |
| 4. | Di Blasi Z, Harkness E, Ernst E, Georgiou A, Kleijnen J. Influence of context effects on health outcomes: a systematic review. Lancet. 2001;357:757-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 855] [Cited by in RCA: 833] [Article Influence: 33.3] [Reference Citation Analysis (0)] |
| 5. | Kleijnen J, de Craen AJ, van Everdingen J, Krol L. Placebo effect in double-blind clinical trials: a review of interactions with medications. Lancet. 1994;344:1347-1349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 111] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Bishop FL, Lewith GT. Patients' preconceptions of acupuncture: a qualitative study exploring the decisions patients make when seeking acupuncture. BMC Complement Altern Med. 2013;13:102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Evans M, Shaw A, Thompson EA, Falk S, Turton P, Thompson T, Sharp D. Decisions to use complementary and alternative medicine (CAM) by male cancer patients: information-seeking roles and types of evidence used. BMC Complement Altern Med. 2007;7:25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 101] [Cited by in RCA: 95] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 8. | Verhoef MJ, Mulkins A, Carlson LE, Hilsden RJ, Kania A. Assessing the role of evidence in patients' evaluation of complementary therapies: a quality study. Integr Cancer Ther. 2007;6:345-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Li X, Zhou X, Du X, Mei R, Zhang Y, Li D, Yang Q. Analysis of Clinical Characteristics of Insomnia Patients and Effect of Acupuncture Therapy. J Clin Med Res. 2024;5:227. [DOI] [Full Text] |
| 10. | Sateia M. Classification of Sleep Disorders. 3rd Ed. IL: American Academy of Sleep Medicine. 2014. |
| 11. | Bergdahl L, Broman JE, Berman AH, Haglund K, von Knorring L, Markström A. Sleep patterns in a randomized controlled trial of auricular acupuncture and cognitive behavioral therapy for insomnia. Complement Ther Clin Pract. 2017;28:220-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Bergdahl L, Broman J, Berman AH, Haglund K, von Knorring L, Markström A. Auricular acupuncture versus cognitive behavioural therapy in the discontinuation of hypnotic drug usage, and treatment effects on anxiety, depression and insomnia symptoms − a randomised controlled study. Eur J Integr Med. 2017;16:15-21. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Peng W, Zhao Y, Wang Y, Wang J, Hao Q, Tu Y, Zhu T. Comparison between acupuncture and cognitive behavioral therapy for primary insomnia: A protocol for systematic review and network meta-analysis. Medicine (Baltimore). 2020;99:e20453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Cheung JM, Bartlett DJ, Armour CL, Glozier N, Saini B. Insomnia patients' help-seeking experiences. Behav Sleep Med. 2014;12:106-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Lu Y, Zhu H, Wang Q, Tian C, Lai H, Hou L, Liu Y, Gao Y, Liu M, Yang F, Ni X, Lin L, Niu J, Tian J, Ge L. Comparative effectiveness of multiple acupuncture therapies for primary insomnia: a systematic review and network meta-analysis of randomized trial. Sleep Med. 2022;93:39-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 16. | Sateia MJ, Buysse DJ, Krystal AD, Neubauer DN, Heald JL. Clinical Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017;13:307-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 559] [Cited by in RCA: 903] [Article Influence: 100.3] [Reference Citation Analysis (0)] |
| 17. | Hu W, Zhou H, Zeng Y, Zeng Q, Huang Z, Wang C. Efficacy of acupuncture or moxibustion in treating senile insomnia compared with a control group: A systematic review and meta-analysis. Medicine (Baltimore). 2023;102:e34842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 18. | Cao HJ, Yu ML, Wang LQ, Fei YT, Xu H, Liu JP. Acupuncture for Primary Insomnia: An Updated Systematic Review of Randomized Controlled Trials. J Altern Complement Med. 2019;25:451-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 19. | Mayor DF, McClure LS, Clayton McClure JH. Individual Differences in Responsiveness to Acupuncture: An Exploratory Survey of Practitioner Opinion. Medicines (Basel). 2018;5:85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Nan LX, Qin S. Progress in the Treatment of Depression Combined with Insomnia with Different Amounts of Acupuncture Stimulation. Mod Health Sci. 2025;8:p105. [DOI] [Full Text] |
| 21. | Garland SN, Eriksen W, Song S, Dearing J, Barg FK, Gehrman P, Mao JJ. Factors that shape preference for acupuncture or cognitive behavioral therapy for the treatment of insomnia in cancer patients. Support Care Cancer. 2018;26:2407-2415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (3)] |
| 22. | Eriksen WT, Singerman L, Romero SAD, Bussell J, Barg FK, Mao JJ. Understanding the Use of Acupuncture for Insomnia Among Cancer Survivors: A Qualitative Study. J Altern Complement Med. 2018;24:962-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 23. | So DW. Acupuncture outcomes, expectations, patient-provider relationship, and the placebo effect: implications for health promotion. Am J Public Health. 2002;92:1662-1667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 36] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/