Published online Jan 19, 2025. doi: 10.5498/wjp.v15.i1.98737
Revised: October 10, 2024
Accepted: October 18, 2024
Published online: January 19, 2025
Processing time: 97 Days and 0.4 Hours
Urinary system tumors often cause negative psychological symptoms, such as depression and dysphoria which significantly impact immune function and indirectly affect cancer prognosis. While epirubicin (EPI) is recommended by the European Association of Urology and can improve prognosis, its long-term use can cause toxic side effects, reduce treatment compliance, and increase psychological burden. Therefore, an appropriate intervention mode is necessary.
To explore the clinical value of EPI combined with mindfulness intervention in patients with urinary system tumors and depression.
This was a retrospective study including 110 patients with urinary system tumors and depression admitted to Zhumadian Central Hospital between March 2021 and July 2023. Patients were divided into conventional (n = 55) and joint inter
Post-intervention, CD4+, CD8+, and CD4+/CD8+ levels increased in both groups, with the joint intervention group showing more significant improvement (P < 0.05). Tumor marker levels (NMP22, BTA, and UBC) were lower in the joint intervention group compared to the conventional group (P < 0.05). The joint intervention group also showed a greater reduction in HAMD-17 scores (9.38 ± 3.12 vs 15.45 ± 4.86, P < 0.05), higher QLQ-C30 scores, and lower CFS scores (both P < 0.05). Additionally, the joint intervention group had a lower incidence of adverse reactions and higher nursing satisfaction (P < 0.05).
EPI combined with mindfulness intervention significantly improved clinical outcomes in patients with urinary system tumors and depression and is worthy of clinical application.
Core Tip: Urinary system tumors often cause varying degrees of negative psychological symptoms, such as depression and dysphoria. These psychological factors significantly impact patients’ immune function and indirectly affect the intervention and prognosis of patients with cancer. Epirubicin (EPI) can improve the prognosis of patients with urinary system tumors, but it also has certain side effects. Mindfulness interventions are beneficial for enhancing psychological adaptability in cancer patients. In this study, the combination of EPI and mindfulness intervention achieved remarkable clinical results in patients with depression-complicated urinary system tumors.
- Citation: Liu J, Guo YP, Lu YM, Wang BL. Clinical value of combining epirubicin with mindfulness intervention in patients with urinary system tumors and depression. World J Psychiatry 2025; 15(1): 98737
- URL: https://www.wjgnet.com/2220-3206/full/v15/i1/98737.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i1.98737
Urinary system tumors refer to various tumors occurring in different parts of the urinary system, including kidney, bladder, and urethral cancers. The annual incidence of urinary tumors has increased in recent years, posing a serious threat to life, health, and quality of life. Global cancer statistics show that prostate cancer (PCa) cases accounts for 14.1% of all cancer cases in men and 6.8% of all deaths[1]. The incidences of bladder cancer (BCa) and kidney cancer are also increasing[2]. Clinically, surgical treatment is commonly used for urinary system tumors. However, surgery can cause trauma and stress, further compromising the body’s immunity. Importantly, the European Association of Urology guidelines recommend the anthracyclines epirubicin (EPI) and mitomycin as the most appropriate chemotherapeutic drugs for these patients[3].
Kang et al[4] conducted a meta-analysis in 2016 on the efficacy of chemotherapy drugs for BCa, comparing EPI with gemcitabine and tiotepa. They concluded that EPI not only prevents tumor recurrence in a localized area but also extends recurrence-free interval, thereby improving patient prognosis. However, the significant physiological impact of the disease on patients often results in negative emotions, such as anxiety and depression. Long-term chemotherapy has toxic side effects that exacerbate psychological stress and increase the incidence of postoperative depression. These adverse psychological significantly impact patients’ immune function and indirectly affect cancer intervention and prognosis[5]. Therefore, active clinical nursing interventions are essential.
In recent years, studies on mindfulness interventions have increased rapidly, confirming their benefits in enhancing psychological adaptability and reducing disease-related psychological stress in patients with cancer patients[6,7]. A meta-analysis[8] indicated that the implementation of mindfulness interventions significantly reduces symptoms of depression, anxiety, and cancer-related fatigue in patients with tumors. Most domestic studies primarily utilize mindfulness-based stress reduction techniques to address fatigue in cancer patients; however, these approaches often lack specificity. Currently, there are few studies on the application of EPI hydrochloride injection combined with mindfulness intervention in patients with depression-complicated urinary system tumors. Therefore, this study explores the application of EPI hydrochloride combined with mindfulness intervention in urinary system tumors complicated by depression, analyzing their combined influence on clinical outcomes to provide a theoretical basis for clinical deve
A total of 110 patients with urinary system tumors and depression admitted to Zhumadian Central Hospital between March 2021 and July 2023 were retrospectively included. According to the differences in intervention methods, the patients were divided into two groups: Conventional (n = 55) and joint intervention (n = 55). The inclusion criteria were: (1) Clinical diagnosis and pathological confirmation of urinary system tumors; (2) 17-item Hamilton depression scale (HAMD-17) score > 7; (3) No chemotherapy or at least 6 months after chemotherapy progression; (4) no metastasis; (5) No communication barriers; and (6) Completed relevant information. The exclusion criteria were: (1) Poor health or inability to tolerate chemotherapy; (2) History of mental illness; (3) Dysfunction of vital organs (heart, liver, lung, and kidney); (4) Contraindications or allergies to EPI; and (5) Infection before chemotherapy. The study was reviewed and approved by the Institutional Review Board of Zhumadian Central Hospital.
The conventional group received mitomycin (Zhejiang Haizheng Pharmaceutical Co., Sinopharm approval number: H33020786, Specification: 2 mg × 5 bottles), administered at 6-8 mg each time, dissolved in sodium chloride, and intravenously injected once a week. Routine nursing interventions included cancer-related knowledge education, medication care, diet care, and basic psychological support). The joint intervention group received EPI hydrochloride injections (Shandong New Times Pharmaceutical Co., Sinopharm Approval No. H20123260, Specification: 10 mg × 5 bottles) at a dosage of 60 mg/m2, administered as an intravenous drip on day 1 of each 21-day cycle. Mindfulness intervention included: (1) Psychological assessment through in-depth communication to understand the patient’s psychological state, introducing mindfulness intervention, and formulating personalized mindfulness intervention methods; (2) The zazen technique, which involved guided mindful breathing exercises in a quiet environment with calm and soothing music, focusing on breathing and body sensations; (3) Body scanning guided relaxation exercises helped patients feel the feelings different parts of their body and manage limb pain and negative emotions; and (4) Mindfulness yoga, which combined mindfulness with yoga, focusing on physical sensations during practice, with sessions lasting 30-50 minutes daily, at least 6 day a week. Both groups underwent three consecutive cycles of chemotherapy.
Data collected included sex, age, and tumor type for comparison between groups. Immune function was measured by collecting fasting venous blood samples (5 mL) and using a Beckmann FACS-Cali-bur500 flow cytometer to measure CD4+ and CD8+ cells calculate the CD4+/CD8+ ratio. Immune function indexes of the conventional and joint intervention groups before and after the intervention (intervention with three cycles of chemotherapy) were also calculated. Tumor markers were detected using enzyme-linked immunosorbent assays and electrochemiluminescence to measure the levels of urinary BCa antigen (UBC), bladder tumor antigen (BTA), and nuclear matrix protein 22 (NMP22) before and after intervention (three cycles of chemotherapy) according to the manufacturers’ instructions (Beijing Biolaibo Technology Co., Ltd., Shanghai Walan Biotechnology Co., Ltd.) Depressive mood improvement was evaluated using the HAMD-17, with scores indicating mild (8-17), moderate (18-24), and severe (> 24) depression, out of a total score of 52[9]. Quality of life was assessed using the quality of life questionnaire-core 30 (QLQ-C30), which includes physical, social, cognitive, role, emotional functioning, and general health dimensions with the scores for each dimension proportional to the corresponding living standards[10]. Cancer-related fatigue was evaluated using the cancer fatigue scale (CFS)[11], which includes emotional, physical, and cognitive fatigue dimensions, with scores ranging from 0 to 60. Adverse reactions were also observed, including symptoms such as urinary pain, hematuria, frequent urgency, and dysuria. Satisfaction was evaluated using a satisfaction questionnaire covering nursing attitude, skills, health education, and pain management, with scores > 80 indicating high satisfaction, 60-80 indicating general satisfaction, and < 60 indicating dissatisfaction [(total number – dissatisfied)/total number × 100%].
Data were recorded in Microsoft Excel 2007 (Microsoft, Redmond, WA, United States) and processed using SPSS 25.0 software (IBM, Armonk, NY, United States). Categorical variables are described as n (%) and intergroup comparisons are conducted using the χ2 test. For continuous data that conform to a normal distribution, assessed by the Kolmogorov-Smirnoff test, results are expressed in mean ± SD and analyzed using independent-samples t-tests. P < 0.05 indicates statistical significance.
In the conventional group, there were 35 males and 20 females, with an average age of 45.67 ± 6.51 years, ranging from 26 to 69 years. Tumor types included 28 cases of BCa, eight of PCa, 15 of kidney cancer, and four of ureter cancer. In the joint intervention group, there were 36 males and 19 females, with an average age of 47.05 ± 5.92 years, ranging from 25 to 70 years. Tumor types included 29 cases of BCa, nine of PCa, 12 of kidney cancer, and five of ureter cancer. The comparison of baseline data such as sex, age, and tumor type between the two groups showed no significant differences (P > 0.05), as shown in Table 1.
| Group | Sex (female/male) | Age (years) | Tumor type, n (%) | |||
| Bladder cancer | Prostate cancer | Kidney cancer | Ureter cancer | |||
| Conventional group (n= 55) | 20/35 | 45.67 ± 6.51 | 28 (50.91) | 8 (14.55) | 15 (27.27) | 4 (7.27) |
| Joint intervention group (n= 55) | 19/36 | 47.05 ± 5.92 | 29 (52.73) | 9 (16.36) | 12 (21.82) | 5 (9.09) |
| χ2/t | 0.040 | -1.165 | 0.521 | |||
| P value | 0.842 | 0.247 | 0.914 | |||
Before the intervention, the immune function indices of the conventional and joint intervention groups remained homogenous (all P > 0.05). Compared with before intervention, both groups demonstrated an increase in CD4+ cells and the CD4+/CD8+ ratio, along with a decrease in CD8+ cells after intervention (P < 0.05). After intervention, the joint intervention group showed an increase in CD4+ cells and the CD4+/CD8+ ratio to a mean value of 41.04 ± 2.30 and 1.03 ± 0.08, respectively, as opposed to 36.10 ± 1.87 and 0.90 ± 0.06 in the conventional group (P < 0.05). After intervention, CD8+ cells decreased to a mean value of 39.66 ± 1.52 in the joint intervention group, compared with 40.35 ± 1.75 in the conventional group (P < 0.05), suggesting an improvement in immune function. as shown in Table 2.
| Group | CD4+ (%) | CD8+ (%) | CD4+/CD8+ | |||
| Before intervention | After intervention | Before intervention | After intervention | Before intervention | After intervention | |
| Conventional group (n= 55) | 31.43 ± 1.62 | 36.10 ± 1.87a | 42.06 ± 1.87 | 40.35 ± 1.72a | 0.75 ± 0.05 | 0.90 ± 0.06a |
| Joint intervention group (n= 55) | 31.16 ± 1.54 | 41.04 ± 2.30a | 42.52 ± 1.60 | 39.66 ± 1.52a | 0.73 ± 0.04 | 1.03 ± 0.08a |
| t value | 0.919 | -12.331 | -1.403 | 2.259 | 1.772 | -11.054 |
| P value | 0.360 | < 0.001 | 0.163 | 0.026 | 0.079 | < 0.001 |
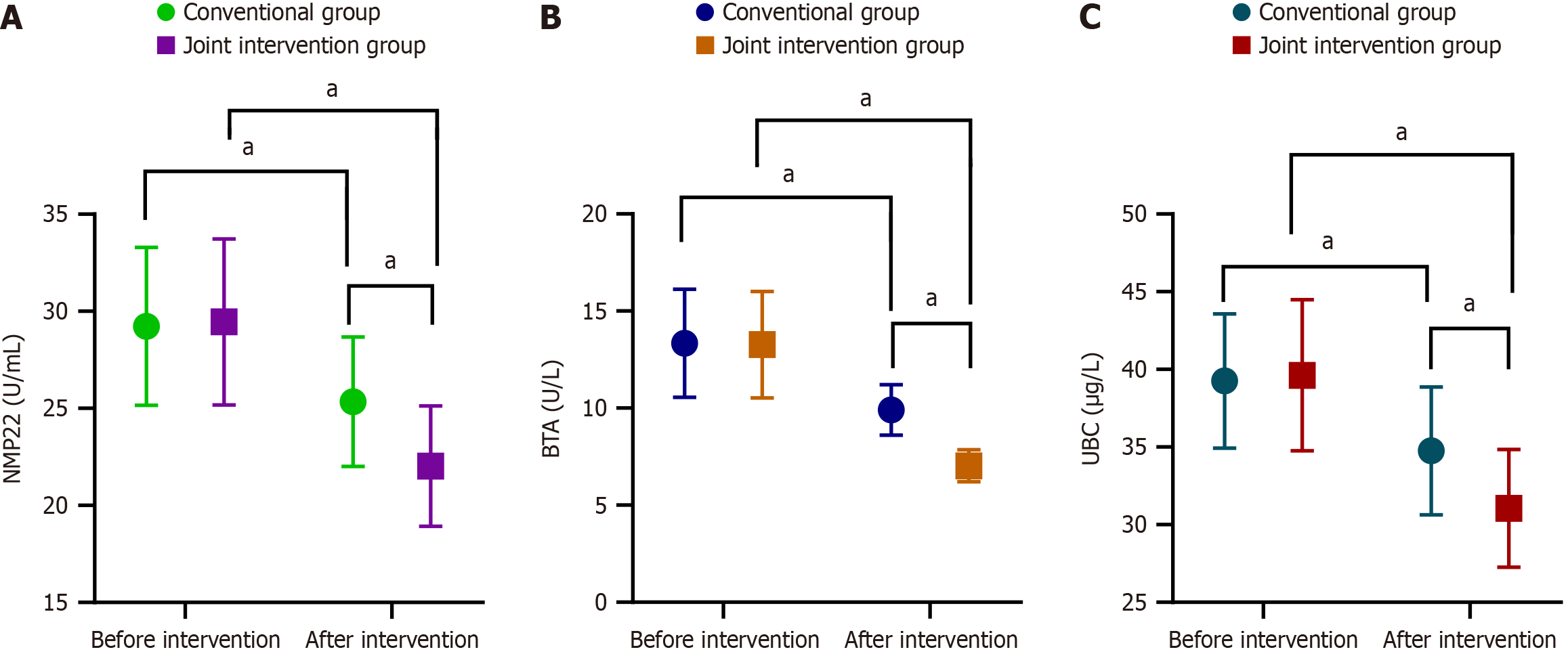
Before intervention, the NMP22 levels in the conventional and joint intervention groups were 29.23 ± 4.07 and 29.45 ± 4.28 mg/L, with no significant difference (P > 0.05). After the intervention, the NMP22 level in the joint intervention group was significantly lower than that in the conventional group (25.34 ± 3.34 U/mL, P < 0.05). Similarly, before the intervention, the BTA level in the conventional group was 13.34 ± 2.78 U/L, compared to 13.27 ± 2.74 U/L in the joint intervention group (P > 0.05). After the intervention, the BTA level in the joint intervention group was 7.03 ± 0.82 U/L, which was significantly lower than that in the conventional group (9.90 ± 1.30 U/mL, P < 0.05). The UBC level before the intervention in the conventional and joint intervention groups were 39.25 ± 4.33 and 39.62 ± 4.86 μg/L, respectively, with no significant difference (P > 0.05). After the intervention, the UBC level in the joint intervention group was significantly lower at 31.05 ± 3.80 μg/L, compared to 34.75 ± 3.80 μg/L in the conventional group (P < 0.05). These results suggest that the joint intervention can effectively reduce the level of tumor markers (Figure 1).
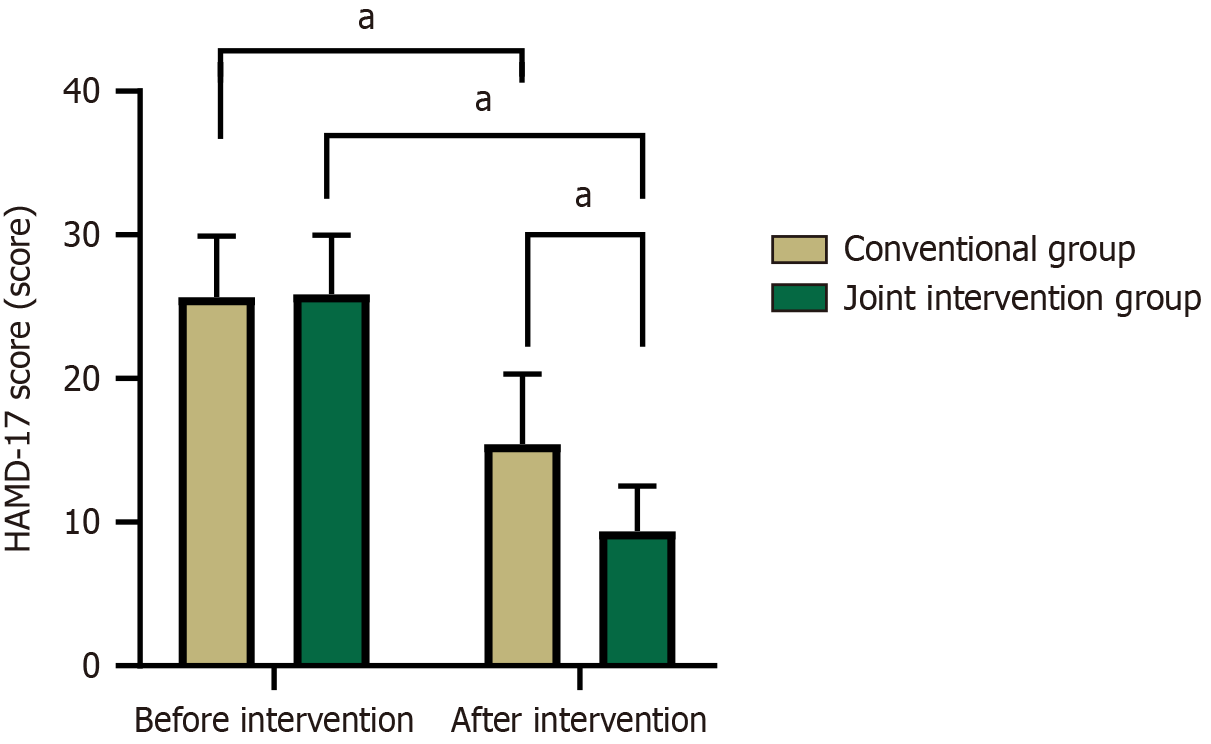
Before the intervention, the average HAMD-17 scores in the conventional and joint intervention groups were 25.67 ± 4.25 and 25.89 ± 4.09 points, respectively, with no significant difference (P > 0.05). After the intervention, the HAMD-17 score in the joint intervention group was significantly lower at 9.38 ± 3.12 points compared to 15.45 ± 4.86 points in the conventional group (P < 0.05), as shown in Figure 2.
Before the intervention, the QLQ-C30 scores in both the conventional and joint intervention groups were similar (P > 0.05). Compared with before the intervention, the QLQ-C30 scores in both groups were elevated after the intervention, and the joint intervention group exhibited higher scores than the conventional group (P < 0.05). After the intervention, the total QLQ-C30 score in the joint intervention group rose from 59.49 ± 4.09 to 87.71 ± 4.70, indicating a remarkable improvement in the quality of life (Table 3).
| Group | Social function | Emotional function | Cognitive function | Body function | Role function | General health | ||||||
| Before intervention | After intervention | Before intervention | After intervention | Before intervention | After intervention | Before intervention | After intervention | Before intervention | Before intervention | After intervention | Before intervention | |
| Conventional group (n= 55) | 68.22 ± 3.50 | 73.13 ± 4.47a | 65.29 ± 3.50 | 70.13 ± 3.52a | 67.21 ± 3.55 | 69.11 ± 4.40a | 66.36 ± 5.75 | 68.73 ± 5.99a | 60.11 ± 3.50 | 67.51 ± 4.11a | 60.22 ± 4.06 | 66.25 ± 3.89a |
| Joint intervention group (n= 55) | 68.73 ± 3.58 | 90.05 ± 5.11a | 66.00 ± 3.32 | 89.78 ± 4.77a | 66.56 ± 3.70 | 89.22 ± 4.30a | 65.62 ± 5.66 | 88.04 ± 5.94a | 59.24 ± 3.54 | 88.64 ± 6.39a | 59.49 ± 4.09 | 87.71 ± 4.70a |
| t value | -0.754 | -18.491 | -1.091 | -24.603 | 0.947 | -24.247 | 0.685 | -16.975 | 1.300 | -20.625 | 0.937 | -26.068 |
| P value | 0.453 | < 0.001 | 0.278 | < 0.001 | 0.346 | 0.495 | < 0.001 | 0.196 | < 0.001 | 0.351 | < 0.001 | |
Before the intervention, the CFS scores in the conventional group were comparable to those in the joint intervention group (P > 0.05). After the intervention, the CFS scores in all dimensions and the total scores decreased in both groups, but the decrease was more pronounced in the joint intervention group (P < 0.05). After the intervention, the total CFS score of the joint intervention dropped from 31.80 ± 2.67 to 25.76 ± 2.19, demonstrating a significant reduction in fatigue (Table 4).
| Group | Body fatigue | Emotional fatigue | Cognitive fatigue | CFS total score | ||||
| Before intervention | After intervention | Before intervention | After intervention | Before intervention | After intervention | Before intervention | After intervention | |
| Conventional group (n = 55) | 13.91 ± 1.28 | 12.96 ± 1.23 | 10.95 ± 1.66 | 10.22 ± 1.37c | 6.96 ± 1.95 | 6.02 ± 1.55b | 31.82 ± 2.67 | 29.20 ± 2.12c |
| Joint intervention group (n = 55) | 14.09 ± 1.42 | 11.13 ± 1.07a | 10.82 ± 1.76 | 9.13 ± 1.25b | 6.89 ± 1.80 | 5.29 ± 1.24c | 31.80 ± 2.67 | 25.76 ± 2.19c |
| t value | -0.706 | 8.339 | 0.390 | 4.365 | 0.203 | 2.720 | 0.036 | 8.975 |
| P value | 0.482 | < 0.001 | 0.698 | < 0.001 | 0.840 | 0.008 | 0.971 | < 0.001 |
The total adverse reaction rate in the joint intervention group was 20.00% (11/55), which was significantly lower the 40.00% (22/55) observed in the conventional group (P < 0.05), as shown in Table 5.
| Group | Urodynia | Hematuria | Dysuria | Frequent and urgent urination | Total incidence (%) |
| Conventional group (n = 55) | 7 (12.73) | 5 (9.01) | 4 (5.33) | 6 (10.91) | 22 (40.00) |
| Joint intervention group (n = 55) | 4 (5.33) | 2 (3.64) | 2 (3.64) | 3 (5.45) | 11 (20.00) |
| χ2 | 5.238 | ||||
| P value | 0.022 |
The total satisfaction rate in the joint intervention group was 92.73% (51/55), significantly higher than the 76.36% (42/55) observed in the conventional group (P < 0.05), as shown in Table 6.
| Group | Very satisfied | Satisfied | Dissatisfied | Satisfaction (%) |
| Conventional group (n = 55) | 22 (40.00) | 20 (36.36) | 13 (23.64) | 42 (76.36) |
| Joint intervention group (n = 55) | 32 (58.18) | 19 (34.55) | 4 (7.27) | 51 (92.73) |
| χ2 | 5.636 | |||
| P value | 0.018 |
The incidence of urinary system tumors has been increasing, becoming a significant factor endangering public health[12,13]. Although surgical treatment can improve the survival rate, it can cause cancer cell proliferation, risks leaving behind residual tumor, and comes with significant side effects, which can lead to relapse and weakened immune function. Relevant studies have shown that patients are often accompanied by immune dysfunction, which promotes tumor metastasis[14,15]. To improve the efficacy, chemotherapy is widely used as adjuvant therapy, especially mitomycin and EPI. Mitomycin is a common chemotherapy drug used to promote tumor cell apoptosis and prevent postoperative recurrence of malignant tumors[16]. EPI, a derivative of doxorubicin and part of the anthracycline class of antibiotics, works by embedding into DNA base pairs, blocking transcription, and interfering with mRNA synthesis, thus inhibiting nucleic acid synthesis and exerting antitumor effects. Importantly, EPI is known for its good permeability and strong lipophilicity, allowing it to exert local effects on the bladder[17,18]. However, chemotherapy also damages normal cells, aggravates the decline of immune function, is accompanied by toxicity and side effects, and affects patient compliance. In addition, diseases and adverse reactions from chemotherapy aggravate the psychological burden of patients and produce negative emotions. Therefore, optimizing nursing care is very important to improve the therapeutic effect.
Many patients with cancer experience cancer-related fatigue and, when under long-term tension and pain, may develop feelings of inadequacy, seriously affecting their life and health. Mindfulness intervention can help alleviate negative emotions, enabling patients to participate actively in disease management, improve cancer-related fatigue, and enhance their quality of life. Importantly, mindfulness emphasizes paying attention to the present moment without judgment, helping individuals live in harmony with pressure and pain and maintain an open and accepting attitude. During mindfulness practice, patients' emotional regulation abilities and cognition functions improve significantly[19]. Cognitive therapy helps replace unreasonable beliefs with reasonable ones, aiding in rebuilding cognitive structures and eliminating negative emotions[20]. Indeed, clinical trials have shown that mindfulness therapy is effective in treating mental disorders such as depression, fear, and anxiety[21]. Research also indicates that mindfulness meditation practice can strengthen insular function and change brain wiring, promoting a positive and optimistic outlook[22]. Furthermore, studies have shown that reasonable exercise can alleviate symptoms of depression and dysphoria[23].
This study showed that after the intervention, compared to the conventional group, the HAMD-17 and CFS scores were lower in the joint intervention group, while QLQ-C30 scores were higher. This indicates that mindfulness intervention can effectively reduce tension and depression in patients with urinary system tumors during EPI hydro
Antitumor immunity is primarily mediated by cellular immunity, with T lymphocytes playing a dominant role[24]. CD4+ helper T-cells promote the antitumor effect of effector cells, while CD8+ suppressor T-cells inhibit the immune response. A normal CD4+/CD8+ ratio ranges between 1.5 and 2.0, indicating stable immune function[25]. In this study, CD4+, CD8+, and CD4+/CD8+ levels increased after the intervention, with more significant increases observed in the joint intervention group, suggesting improved body immunity. EPI kills tumor cells in all growth cycles, removes residual tumor cells after surgery, improves immunity, and prevents or delays tumor metastasis and recurrence. Meanwhile, mindfulness intervention helps patients understand the nature and development of the disease, which eliminate doubts, improve coping ability and self-confidence, and recognize the importance of controlling emotions.
This study also observed the levels of NMP22, BTA, and UBC in the urine of both groups. UBC originates from BCa cells and effectively evaluates the prognosis of urinary system tumors[26]. BTA assists in immune monitoring of tumor cells, and tumor cell proliferation promotes BTA synthesis[27]. NMP22 is a nuclear matrix protein, and increased NMP22 Levels are associated with tumor proliferation[28]. In this study, the levels of NMP22, BTA, and UBC were lower in the joint intervention group compared to the conventional group, and adverse reactions were fewer, indicating that EPI hydrochloride injection combined with mindfulness intervention can reduce tumor marker levels and adverse reactions. EPI hydrochloride injection chemotherapy reduces residual tumor cells tumor marker levels, and adverse reactions due to its good affinity, rapid dispersion in local lesions, and lower blood entry. Notably, we found that the satisfaction rate in the joint intervention group was higher, indicating high patient satisfaction and recognition of EPI hydrochloride injection combined with mindfulness intervention.
This study still has some limitations. First, this study is a single-center intervention with a small sample size and a single source. Secondly, the observation period of this study was short, and patients were not followed up for a long time to observe the long-term prognosis of patients. In addition, the patients included in this study were patients with urinary system tumors combined with depression, and there were many tumor types, which may have a certain impact on the results. Future multicenter studies with larger sample sizes and longer durations that are more representative will be needed to further validate our findings.
EPI hydrochloride injection combined with mindfulness intervention has significant clinical effects in patients with urinary system tumors complicated by depression. This combination resulted in mild immunosuppression, lower levels of tumor markers, significant improvement in symptoms of depression and cancer-related fatigue, no increase in adverse reactions during the intervention period, and an effective improvement in quality of life for patients.
| 1. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 68753] [Article Influence: 13750.6] [Reference Citation Analysis (201)] |
| 2. | Lobo N, Mount C, Omar K, Nair R, Thurairaja R, Khan MS. Landmarks in the treatment of muscle-invasive bladder cancer. Nat Rev Urol. 2017;14:565-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 121] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 3. | Babjuk M, Burger M, Compérat EM, Gontero P, Mostafid AH, Palou J, van Rhijn BWG, Rouprêt M, Shariat SF, Sylvester R, Zigeuner R, Capoun O, Cohen D, Escrig JLD, Hernández V, Peyronnet B, Seisen T, Soukup V. European Association of Urology Guidelines on Non-muscle-invasive Bladder Cancer (TaT1 and Carcinoma In Situ) - 2019 Update. Eur Urol. 2019;76:639-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 651] [Cited by in RCA: 925] [Article Influence: 132.1] [Reference Citation Analysis (0)] |
| 4. | Kang M, Jeong CW, Kwak C, Kim HH, Ku JH. Single, immediate postoperative instillation of chemotherapy in non-muscle invasive bladder cancer: a systematic review and network meta-analysis of randomized clinical trials using different drugs. Oncotarget. 2016;7:45479-45488. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Song Q, Zhou R, Shu F, Fu W. Cuproptosis scoring system to predict the clinical outcome and immune response in bladder cancer. Front Immunol. 2022;13:958368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 117] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 6. | Kemerer BM, Zdaniuk B, Higano CS, Bossio JA, Camara Bicalho Santos R, Flannigan R, Brotto LA. A randomized comparison of group mindfulness and group cognitive behavioral therapy vs control for couples after prostate cancer with sexual dysfunction. J Sex Med. 2023;20:346-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 7. | Park S, Sato Y, Takita Y, Tamura N, Ninomiya A, Kosugi T, Sado M, Nakagawa A, Takahashi M, Hayashida T, Fujisawa D. Mindfulness-Based Cognitive Therapy for Psychological Distress, Fear of Cancer Recurrence, Fatigue, Spiritual Well-Being, and Quality of Life in Patients With Breast Cancer-A Randomized Controlled Trial. J Pain Symptom Manage. 2020;60:381-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 136] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 8. | Chayadi E, Baes N, Kiropoulos L. The effects of mindfulness-based interventions on symptoms of depression, anxiety, and cancer-related fatigue in oncology patients: A systematic review and meta-analysis. PLoS One. 2022;17:e0269519. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 76] [Reference Citation Analysis (0)] |
| 9. | Fava GA, Kellner R, Munari F, Pavan L. The Hamilton Depression Rating Scale in normals and depressives. Acta Psychiatr Scand. 1982;66:26-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 85] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Cocks K, Wells JR, Johnson C, Schmidt H, Koller M, Oerlemans S, Velikova G, Pinto M, Tomaszewski KA, Aaronson NK, Exall E, Finbow C, Fitzsimmons D, Grant L, Groenvold M, Tolley C, Wheelwright S, Bottomley A; European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life Group. Content validity of the EORTC quality of life questionnaire QLQ-C30 for use in cancer. Eur J Cancer. 2023;178:128-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 109] [Article Influence: 36.3] [Reference Citation Analysis (0)] |
| 11. | Okuyama T, Akechi T, Kugaya A, Okamura H, Shima Y, Maruguchi M, Hosaka T, Uchitomi Y. Development and validation of the cancer fatigue scale: a brief, three-dimensional, self-rating scale for assessment of fatigue in cancer patients. J Pain Symptom Manage. 2000;19:5-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 260] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 12. | Paner GP, Stadler WM, Hansel DE, Montironi R, Lin DW, Amin MB. Updates in the Eighth Edition of the Tumor-Node-Metastasis Staging Classification for Urologic Cancers. Eur Urol. 2018;73:560-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 464] [Article Influence: 58.0] [Reference Citation Analysis (0)] |
| 13. | Mistretta FA, Carrion DM, Nazzani S, Vásquez JL, Fiori C, De Cobelli O, Porpiglia F, Esperto F. Bladder recurrence of primary upper tract urinary carcinoma following nephroureterectomy, and risk of upper urinary tract recurrence after ureteral stent positioning in patients with primary bladder cancer. Minerva Urol Nefrol. 2019;71:191-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Song MJ, Pan QZ, Ding Y, Zeng J, Dong P, Zhao JJ, Tang Y, Li J, Zhang Z, He J, Yang J, Huang Y, Peng R, Wang QJ, Gu JM, He J, Li YQ, Chen SP, Huang R, Zhou ZQ, Yang C, Han Y, Chen H, Liu H, Xia S, Wan Y, Weng DS, Xia L, Zhou FJ, Xia JC. The efficacy and safety of the combination of axitinib and pembrolizumab-activated autologous DC-CIK cell immunotherapy for patients with advanced renal cell carcinoma: a phase 2 study. Clin Transl Immunology. 2021;10:e1257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Rice-Stitt T, Valencia-Guerrero A, Cornejo KM, Wu CL. Updates in Histologic Grading of Urologic Neoplasms. Arch Pathol Lab Med. 2020;144:335-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Kleinmann N, Matin SF, Pierorazio PM, Gore JL, Shabsigh A, Hu B, Chamie K, Godoy G, Hubosky S, Rivera M, O'Donnell M, Quek M, Raman JD, Knoedler JJ, Scherr D, Stern J, Weight C, Weizer A, Woods M, Kaimakliotis H, Smith AB, Linehan J, Coleman J, Humphreys MR, Pak R, Lifshitz D, Verni M, Adibi M, Amin MB, Seltzer E, Klein I, Konorty M, Strauss-Ayali D, Hakim G, Schoenberg M, Lerner SP. Primary chemoablation of low-grade upper tract urothelial carcinoma using UGN-101, a mitomycin-containing reverse thermal gel (OLYMPUS): an open-label, single-arm, phase 3 trial. Lancet Oncol. 2020;21:776-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 91] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 17. | Lu JL, Xia QD, Lu YH, Liu Z, Zhou P, Hu HL, Wang SG. Efficacy of intravesical therapies on the prevention of recurrence and progression of non-muscle-invasive bladder cancer: A systematic review and network meta-analysis. Cancer Med. 2020;9:7800-7809. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 18. | Suo N, Wang M, Jin Y, Ding J, Gao X, Sun X, Zhang H, Cui M, Zheng J, Li N, Jin X, Jiang S. Magnetic multiwalled carbon nanotubes with controlled release of epirubicin: an intravesical instillation system for bladder cancer. Int J Nanomedicine. 2019;14:1241-1254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 19. | Xunlin NG, Lau Y, Klainin-Yobas P. The effectiveness of mindfulness-based interventions among cancer patients and survivors: a systematic review and meta-analysis. Support Care Cancer. 2020;28:1563-1578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 139] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 20. | Knoerl R, Mazzola E, Woods H, Buchbinder E, Frazier L, LaCasce A, Li BT, Luskin MR, Phillips CS, Thornton K, Berry DL, Ligibel JA. Exploring the Feasibility of a Mindfulness-Music Therapy Intervention to Improve Anxiety and Stress in Adolescents and Young Adults with Cancer. J Pain Symptom Manage. 2022;63:e357-e363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 21. | Nissen ER, O'Connor M, Kaldo V, Højris I, Borre M, Zachariae R, Mehlsen M. Internet-delivered mindfulness-based cognitive therapy for anxiety and depression in cancer survivors: A randomized controlled trial. Psychooncology. 2020;29:68-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 85] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 22. | Farb NA, Segal ZV, Mayberg H, Bean J, McKeon D, Fatima Z, Anderson AK. Attending to the present: mindfulness meditation reveals distinct neural modes of self-reference. Soc Cogn Affect Neurosci. 2007;2:313-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 760] [Cited by in RCA: 634] [Article Influence: 33.4] [Reference Citation Analysis (0)] |
| 23. | Reich RR, Lengacher CA, Alinat CB, Kip KE, Paterson C, Ramesar S, Han HS, Ismail-Khan R, Johnson-Mallard V, Moscoso M, Budhrani-Shani P, Shivers S, Cox CE, Goodman M, Park J. Mindfulness-Based Stress Reduction in Post-treatment Breast Cancer Patients: Immediate and Sustained Effects Across Multiple Symptom Clusters. J Pain Symptom Manage. 2017;53:85-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 130] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 24. | Cumberbatch MGK, Jubber I, Black PC, Esperto F, Figueroa JD, Kamat AM, Kiemeney L, Lotan Y, Pang K, Silverman DT, Znaor A, Catto JWF. Epidemiology of Bladder Cancer: A Systematic Review and Contemporary Update of Risk Factors in 2018. Eur Urol. 2018;74:784-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 479] [Cited by in RCA: 567] [Article Influence: 70.9] [Reference Citation Analysis (0)] |
| 25. | Sun Z, Tao W, Guo X, Jing C, Zhang M, Wang Z, Kong F, Suo N, Jiang S, Wang H. Construction of a Lactate-Related Prognostic Signature for Predicting Prognosis, Tumor Microenvironment, and Immune Response in Kidney Renal Clear Cell Carcinoma. Front Immunol. 2022;13:818984. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 64] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 26. | Ecke TH, Scislowski M, Hassan N, Saura M, Hallmann S, Koch S, Vuolle S, Malakoutikhah M, Kopra K, Härmä H. Luminophore Chemistry for Detection of Urinary Bladder Cancer - Comparison to Cytology and Urinary Rapid Tests (BTA stat(®), NMP22(®) BladderChek(®) and UBC(®) Rapid Test). Anticancer Res. 2022;42:5249-5256. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 27. | Boman H, Hedelin H, Jacobsson S, Holmäng S. Newly diagnosed bladder cancer: the relationship of initial symptoms, degree of microhematuria and tumor marker status. J Urol. 2002;168:1955-1959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | van Rhijn BW, van der Poel HG, van der Kwast TH. Urine markers for bladder cancer surveillance: a systematic review. Eur Urol. 2005;47:736-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 364] [Cited by in RCA: 380] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/