Published online Jan 19, 2025. doi: 10.5498/wjp.v15.i1.100730
Revised: November 3, 2024
Accepted: December 6, 2024
Published online: January 19, 2025
Processing time: 115 Days and 18.1 Hours
With the growing scholarly and clinical fascination with somatic symptom dis
To conduct a bibliometric analysis to investigate the current status and frontiers of SSD.
The documents related to SSD are obtained from the web of science core collection database (WoSCC), and VOSviewer 1.6.16 from January 1, 2000 to December 31, 2023, and the WoSCC’s literature analysis wire were used to conduct the bibliometric analysis.
A total of 567 documents related to SSD were included, and 2325 authors across 947 institutions from 57 countries/regions have contributed to SSD research, published in 277 journals. The most productive author, institution, country and journal were Löwe B, University of Hamburg, Germany, and Journal of Psychosomatic Research respectively. The first high-cited document was published in the Journal of Psychosomatic Research in 2013 by Dimsdale JE and colleagues, which explored the rationale behind the SSD diagnosis introduction in diagnostic and statistical manual of mental disorders.
In conclusion, the main research hotspots and frontiers in the field of SSD are validity and reliability of the SSD criteria, functional impairment of SSD, and the treatment for SSD. More high-quality studies are needed to assess the diagnosis and treatment of SSD.
Core Tip: To the best of our knowledge, this is the first comprehensive bibliometric analysis of the somatic symptom disorder (SSD). The main research hotspots and frontiers in the field of SSD are validity and reliability of the SSD criteria, functional impairment of SSD, and the treatment for SSD. More high-quality studies are needed to assess the diagnosis and treatment of SSD.
- Citation: Yang C, Zhang K, Wang Q, Wang S, Li H, Zhang K. Global research status and trends of somatic symptom disorder: A bibliometric study. World J Psychiatry 2025; 15(1): 100730
- URL: https://www.wjgnet.com/2220-3206/full/v15/i1/100730.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i1.100730
In 2013, somatic symptom disorder (SSD) was introduced as a new diagnosis in the diagnostic and statistical manual of mental disorders (DSM-5), which based on distressing somatic symptoms and the abnormal feelings, thoughts, and behaviors for them[1]. SSD presents a complex scenario where individuals experience profound and overwhelming distress or worry about physical symptoms that might not be linked to any identifiable medical condition[2]. Such distress significantly interferes with everyday life, impacting social, work, and other functional areas. Those with SSD often exhibit an increased awareness and concern for their bodily sensations, fearing that these symptoms could signal a severe, undiagnosed disease. Even after numerous medical assessments that typically don’t reveal a concrete physical cause, the concern for their health persists. SSD diagnosis highlights the critical connection between physical symptoms and psychological factors, with sufferers frequently experiencing intense health-related anxiety, leading them to seek medical attention often[3-6]. The introduction of SSD in DSM-5 represents a notable shift from previous versions, focusing less on the absence of a medical explanation for the symptoms and more on the individuals’ abnormal reactions, thoughts, and behaviors towards their symptoms. Treatment strategies aim at enhancing life quality, symptom management, and alleviating the distress and anxiety linked to the symptoms, often through a mix of psychotherapy, especially cognitive-behavioral therapy (CBT), and medication for managing anxiety and depression where applicable[7-9]. The objective is to foster healthier thought and reaction patterns to their symptoms, diminishing their impact on the individuals' lives.
With the growing scholarly and clinical fascination with SSD, a bibliometric analysis for the field of SSD is lacking. The bibliometric studies can compile research trends and spotlight new focal areas specifically for SSD research. Bibliometric analyses are crucial for mapping the development and broadening of literature, pinpointing key researchers, affiliations, and countries spearheading this research, and showcasing pivotal studies and innovative research directions[10,11]. They also help in uncovering yet-to-be-explored territories within the domain. Thus, we conducting a bibliometric analysis for offering the insights into the evolution of SSD research, highlighting its scientific achievements, and providing the reference for future research.
The primary source for our bibliometric study was the web of science core collection (WoSCC), which is extensive and credible compilation of academic papers. The search was conducted using specific keywords: “Somatic symptom disorder”, “somatic symptom and related disorders”, and “somatic symptom disorders”. Given that the initial discourse on the SSD emerged in 2013, the timeframe for the search was set from January 1, 2013 to December 31, 2023. This search encompassed all publication types related to SSD without imposing any language restrictions.
After gathering the pertinent literature, we delved into various bibliometric indicators through the WoSCC online analysis platform. This investigation covered metrics such as the yearly distribution of publications, identification of the top 10 most prolific countries/regions, institutions, authors, and journals, as well as the top 20 most-cited papers on the subject of “somatic symptom disorder”. For a comprehensive analysis, the dataset-including information on publication years, authors, countries, regions, institutions, journals, keywords, and citations-was downloaded in TXT format, selecting the “Full Record and Cited References” option. We employed VOSviewer software (version 1.6.16) for the visualization of data sets, creating maps of co-authorship networks for keyword co-occurrence network, countries/regions, institutions, authors, journal and reference citation patterns. The visualizations generated were then prepared for presentation, enriching the findings from our bibliometric review.
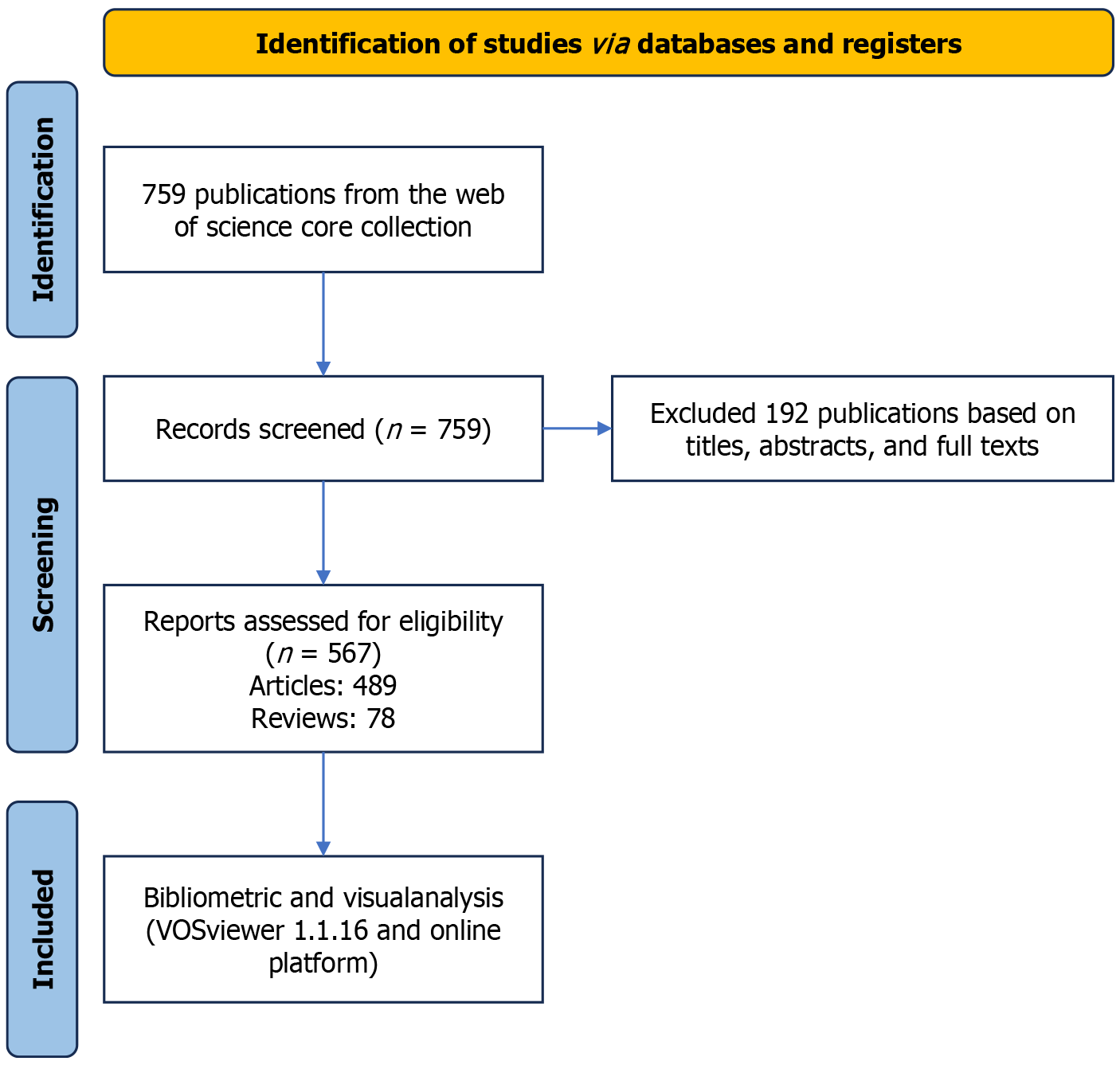
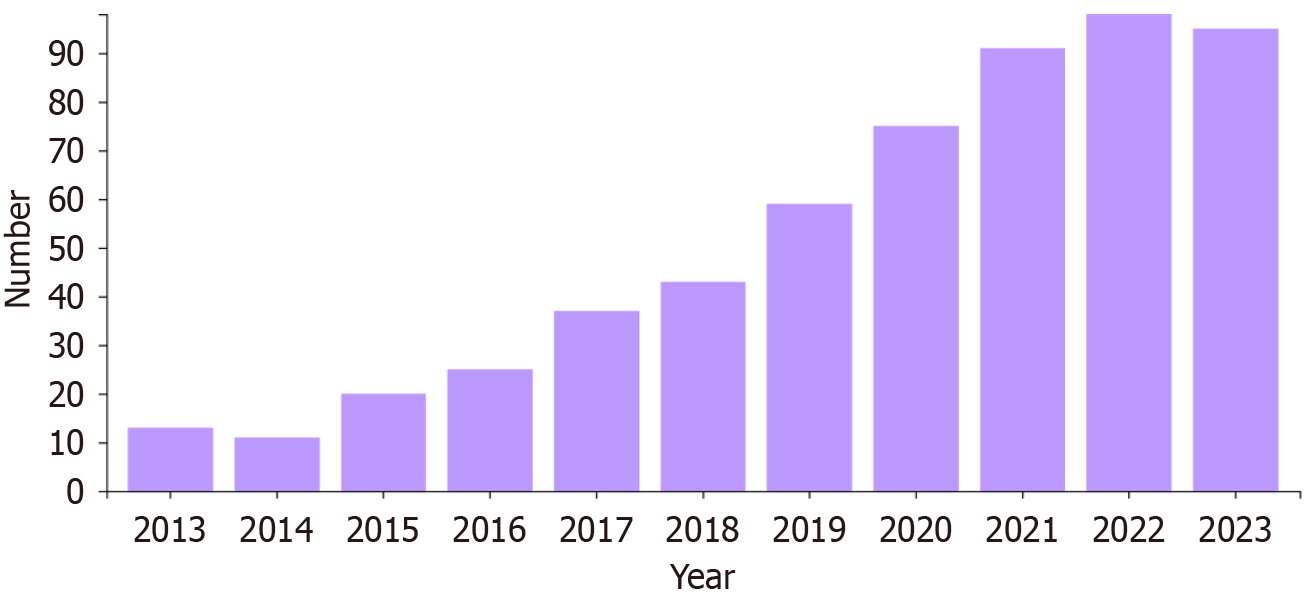
The bibliometric analysis unveiled a total of 567 documents related to “somatic symptom disorder” after a careful screening process, as depicted in Figure 1. Among these, there were 489 entries (86.2%) and 78 reviews (13.8%). The primary field of publication was psychiatry, claiming 311 documents and accounting for 66.6% of the total, with clinical psychology following at 83 publications (17.8%). The temporal trend observed from 2013 to 2023 in Figure 2 indicates a significant increase in scholarly output on SSD.
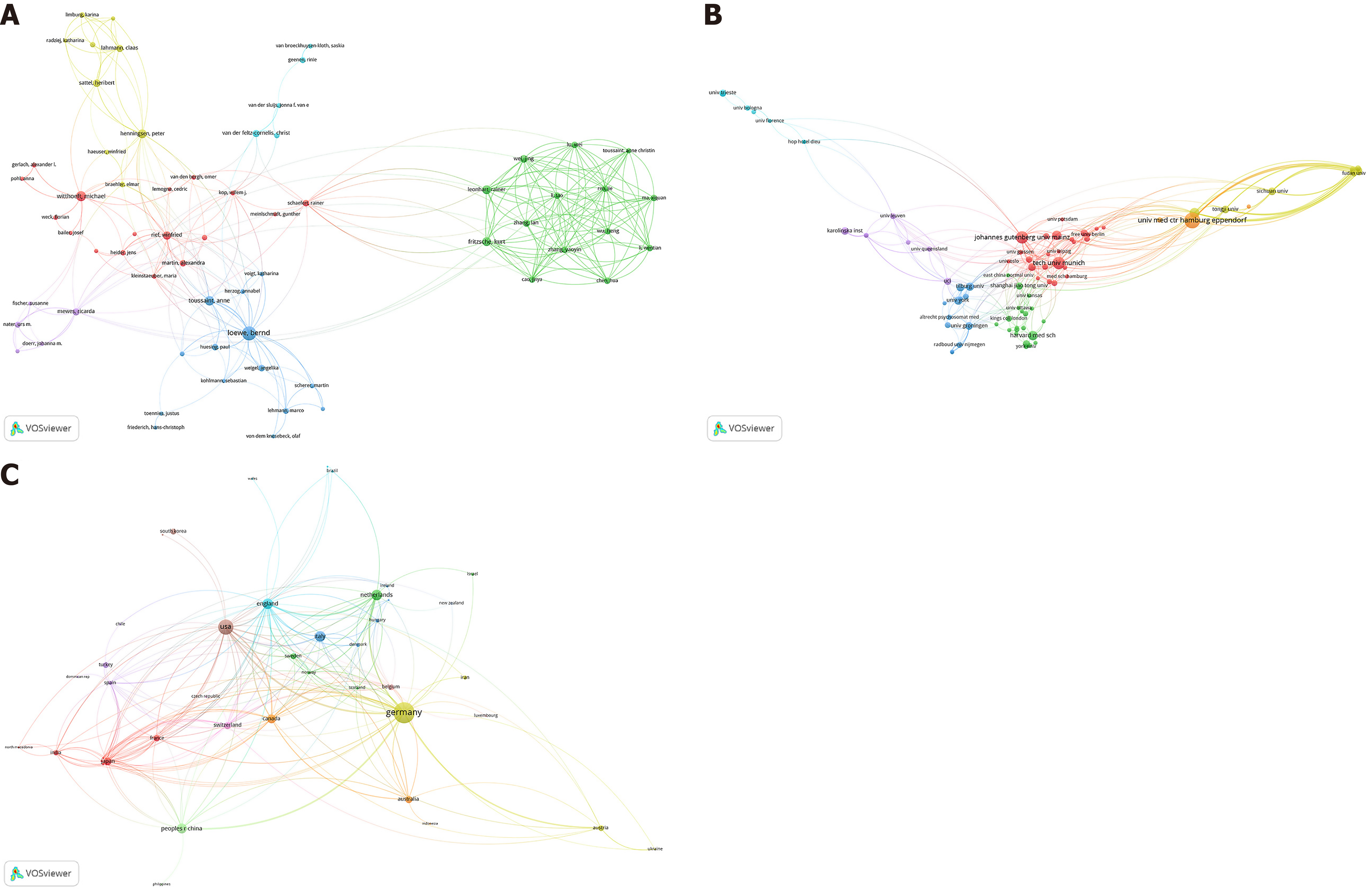
A total of 2325 authors across 947 institutions from 57 countries/regions have contributed to SSD research, published across 277 journals. Löwe B stands out with a notable impact in the field, leading with 38 publications and 825 citations, demonstrating his significant influence on SSD research. Witthöft M and Toussaint A also being notable for their substantial contributions of 23 and 18 publications, respectively. University of Hamburg is at the forefront among institutions with 60 publications, closely followed by the Johannes Gutenberg University of Mainz, and Technical University of Munich with 37 publications, and the University of Bologna with 33 publications. The Germany leads in terms of publications with 185 papers, which have attracted a noteworthy 2433 citations and achieved an H-index of 26, showcasing the significant volume and impact of its research contributions. United States and Netherlands also stand out with 102 and 50 publications, respectively. The Journal of Psychosomatic Research, Frontiers in Psychiatry and Psychosomatic Medicine are the most productive in the field, with 57, 29 and 25 publications, respectively. The most influential authors, institutions, countries/regions and journals within the SSD research community are detailed in Table 1 and Table 2, while network visualization maps illustrating relationships among institutions, countries/regions, authors, and journals are provided in Figure 3 and Figure 4A.
| Ranking | Items | Counts | % of 568 | Citations | H-index | |
| Authors | 1 | Löwe B | 38 | 6.69 | 825 | 15 |
| 2 | Witthöft M | 23 | 4.049 | 290 | 8 | |
| 3 | Toussaint A | 18 | 3.169 | 502 | 11 | |
| 4 | Fritzsche K | 16 | 2.817 | 205 | 7 | |
| 5 | Huang WL | 16 | 2.817 | 176 | 8 | |
| 6 | Henningsen P | 15 | 2.641 | 590 | 9 | |
| 7 | Leonhart R | 15 | 2.641 | 203 | 7 | |
| 8 | Van Der Feltz-cornelis CM | 15 | 2.641 | 163 | 9 | |
| 9 | Rief W | 14 | 2.465 | 492 | 8 | |
| 10 | Sattel H | 13 | 2.289 | 145 | 7 | |
| Affiliations | 1 | University of Hamburg | 60 | 10.563 | 941 | 16 |
| 2 | Johannes Gutenberg University of Mainz | 37 | 6.514 | 487 | 11 | |
| 3 | Technical University of Munich | 33 | 5.81 | 900 | 14 | |
| 4 | University of Freiburg | 26 | 4.577 | 294 | 10 | |
| 5 | Harvard University | 23 | 4.049 | 402 | 8 | |
| 6 | Ruprecht Karls University Heidelberg | 23 | 4.049 | 279 | 9 | |
| 7 | Philipps University Marburg | 21 | 3.697 | 576 | 12 | |
| 8 | University of London | 20 | 3.521 | 368 | 12 | |
| 9 | National Taiwan University | 16 | 2.817 | 176 | 8 | |
| 10 | University of Munich | 16 | 2.817 | 195 | 7 | |
| Countries | 1 | Germany | 185 | 32.57 | 2433 | 26 |
| 2 | United States | 102 | 17.958 | 1456 | 23 | |
| 3 | Netherlands | 50 | 8.803 | 657 | 14 | |
| 4 | England | 49 | 8.627 | 935 | 16 | |
| 5 | Italy | 46 | 8.099 | 609 | 14 | |
| 6 | China | 43 | 7.57 | 523 | 10 | |
| 7 | Canada | 34 | 5.986 | 557 | 13 | |
| 8 | Japan | 26 | 4.577 | 125 | 6 | |
| 9 | Australia | 23 | 4.049 | 508 | 11 | |
| 10 | Switzerland | 21 | 3.697 | 318 | 10 |
| Ranking | Publication titles | Record count | Citations |
| 1 | Journal of Psychosomatic Research | 57 | 865 |
| 2 | Frontiers In Psychiatry | 29 | 193 |
| 3 | Psychosomatic Medicine | 25 | 450 |
| 4 | Bmc Psychiatry | 18 | 107 |
| 5 | General Hospital Psychiatry | 11 | 174 |
| 6 | Frontiers In Psychology | 8 | 55 |
| 7 | Psychological Medicine | 6 | 158 |
| 8 | Psychosomatics | 6 | 76 |
| 9 | Psychotherapeut | 6 | 11 |
| 10 | Journal of Affective Disorders | 5 | 153 |
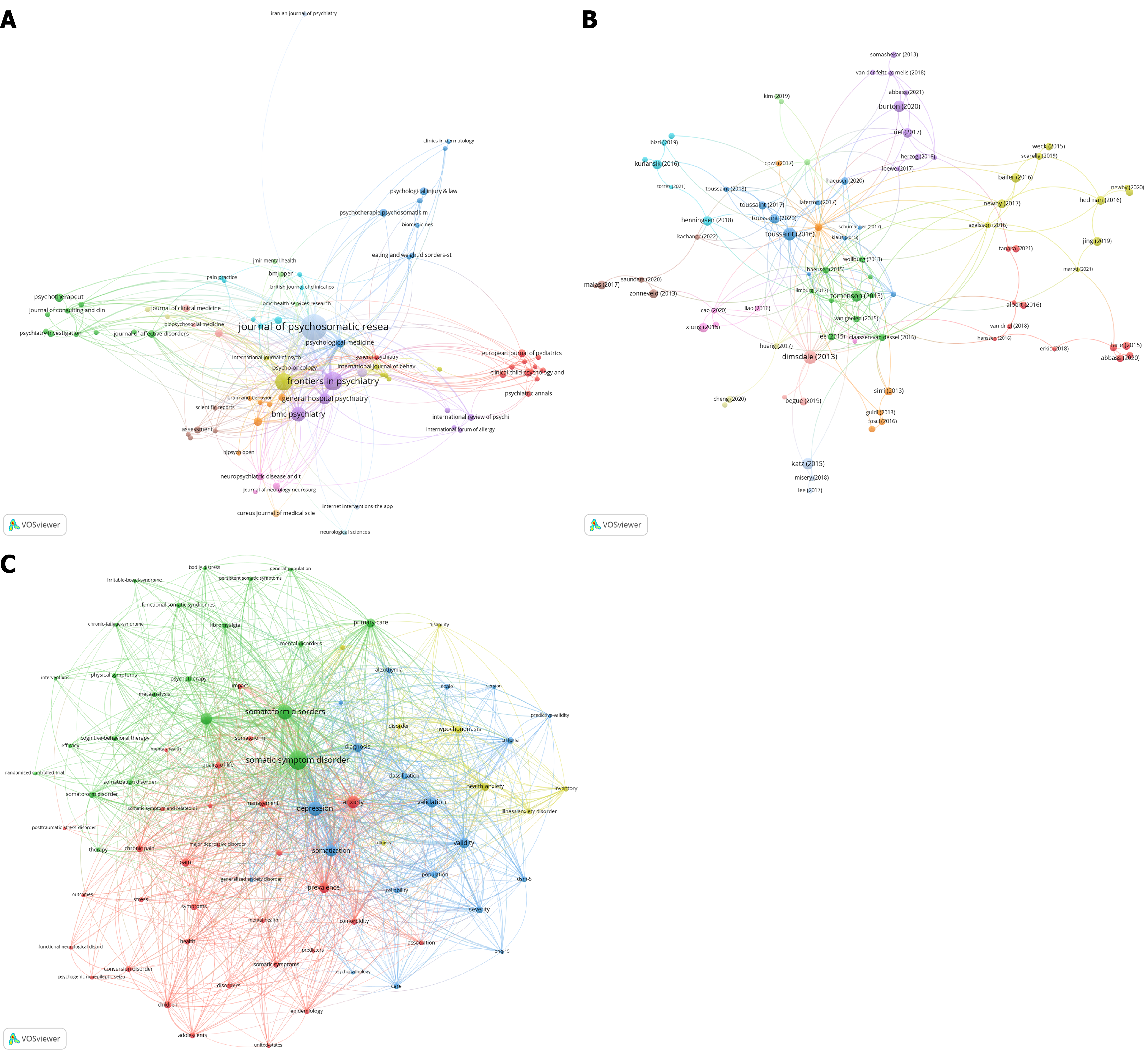
Figure 4B showcases a network visualization map detailing citation of publications. The characteristics of the top 20 most-cited articles are summarized in Table 3[12-31]. The leading article, appearing in the Journal of Psychosomatic Research in 2013 by Dimsdale et al[2], explores the rationale behind the SSD diagnosis introduction in DSM-5. This paper marks a pivotal shift in focus from symptoms lacking medical explanations to recognizing SSD based on persistent physical symptoms that profoundly affect an individual’s thoughts, emotions, and behaviors. It assesses the reliability, validity, and prevalence of SSD, pointing out directions for future research, educational endeavors, and clinical practices. The second noteworthy article, published in Psychosomatic Medicine in 2016 by Toussaint A and team, introduces the SSD-B criteria scale (SSD-12), a newly formulated self-report questionnaire for evaluating DSM-5’s psychological aspects. The study validates the scale's reliability and applicability for further exploration in both research and clinical settings. The third influential piece, authored by Burton C and published in BMC Medicine in 2020, critiques the DSM-5’s approach to SSD in the context of chronic pain. It argues that the diagnosis overly psychologizes individuals with chronic pain, leading to misdiagnosis and unnecessary stigma, suggesting that adjustment disorder offers a more precise and acceptable diagnostic alternative for those overly concerned with their pain. The fourth significant publication, featured in the Journal of the Canadian Journal of Psychiatry in 2015 by Katz J and co-authors, recommends adopting ‘functional somatic disorders’ as a collective term for conditions characterized by enduring and problematic physical symptoms. The fifth prominent publication by Tomenson B, appearing in the British Journal of Psychiatry in 2013, identifies the total somatic symptom score as a predictive tool for health status and healthcare utilization, beyond the impacts of anxiety, depression, and general medical conditions.
| Ranking | Publications | Journal | Year | Citations | First author |
| 1 | Somatic symptom disorder: An important change in DSM | Journal of Psychosomatic Research | 2013 | 154 | Dimsdale JE |
| 2 | Development and validation of the somatic symptom disorder-B criteria scale | Psychosomatic Medicine | 2016 | 136 | Toussaint A |
| 3 | Functional somatic disorders: Discussion paper for a new common classification for research and clinical use | BMC Medicine | 2020 | 103 | Burton C |
| 4 | Chronic pain, psychopathology, and DSM-5 somatic symptom disorder | Canadian Journal of Psychiatry | 2015 | 127 | Katz J |
| 5 | Total somatic symptom score as a predictor of health outcome in somatic symptom disorders | British Journal of Psychiatry | 2013 | 94 | Tomenson B |
| 6 | Irritable bowel syndrome: Relations with functional, mental, and somatoform disorders | World Journal of Gastroenterology | 2014 | 102 | Hausteiner-Wiehle C |
| 7 | Core outcome domains for clinical trials on somatic symptom disorder, bodily distress disorder, and functional somatic syndromes: European network on somatic symptom disorders recommendations | Psychosomatic Medicine | 2017 | 77 | Rief W |
| 8 | Detecting DSM-5 somatic symptom disorder: criterion validity of the patient health questionnaire-15 and the somatic symptom scale-8 in combination with the somatic symptom disorder-B criteria scale | Psychological Medicine | 2020 | 80 | Toussaint A |
| 9 | Management of somatic symptom disorder | Dialogues In Clinical Neuroscience | 2018 | 78 | Henningsen P |
| 10 | Validation of patient health questionnaire for major depression in Chinese outpatients with multiple somatic symptoms: A multicenter cross-sectional study | Journal of Affective Disorders | 2015 | 83 | Xiong NN |
| 11 | Somatic symptom disorder | American Family Physician | 2016 | 76 | Kurlansik SL |
| 12 | Health anxiety and hypochondriasis in the light of DSM-5 | Anxiety Stress and Coping | 2016 | 75 | Bailer J |
| 13 | DSM-5 illness anxiety disorder and somatic symptom disorder: Comorbidity, correlates, and overlap with DSM-IV hypochondriasis | Journal of Psychosomatic Research | 2017 | 70 | Newby JM |
| 14 | Pediatric somatic symptom disorders | Current Psychiatry Reports | 2017 | 66 | Malas N |
| 15 | Exposure-based cognitive-behavioral therapy via the Internet and as bibliotherapy for somatic symptom disorder and illness anxiety disorder: Randomized controlled trial | British Journal of Psychiatry | 2016 | 67 | Hedman E |
| 16 | The efficacy of cognitive behavioral therapy in somatoform disorders and medically unexplained physical symptoms: A meta-analysis of randomized controlled trials | Journal of Affective Disorders | 2019 | 61 | Jing L |
| 17 | Patients with unexplained physical symptoms have poorer quality of life and higher costs than other patient groups: A cross-sectional study on burden | BMC Health Services Research | 2013 | 60 | Zonneveld LNL |
| 18 | Health anxiety and illness-related fears across diverse chronic illnesses: A systematic review on conceptualization, measurement, prevalence, course, and correlates | Plos One | 2020 | 66 | Lebel S |
| 19 | Identifying the key characteristics of clinical fear of cancer recurrence: An international Delphi study | Psycho-Oncology | 2020 | 60 | Mutsaers B |
| 20 | Structural alterations in functional neurological disorder and related conditions: a software and hardware problem? | Neuroimage-Clinical | 2019 | 58 | Bègue I |
In the bibliometric network visualization, a complex interrelation of topics centered around SSD were observed, which was displayed in Figure 4C. The map is segmented into distinct color-coded clusters, each representing a thematic concentration within the research landscape. The green cluster, which anchors the network, is closely associated with ‘somatic symptom disorder’ and branches out to related terms such as ‘somatoform disorders’, ‘cognitive-behavioral therapy’, and ‘functional somatic syndromes’. This implies a strong research focus on the clinical and therapeutic aspects of somatic symptomatology and its treatment. Red clusters are tightly knit around ‘depression’, intersecting with ‘anxiety’, ‘chronic pain’, and ‘somatization’, highlighting the psychological dimensions of somatic symptoms and their comorbidity with mental health disorders. The blue cluster orbits around ‘health anxiety’ and ‘hypochondriasis’, suggesting an investigative thread into the anxiety disorders spectrum as it pertains to somatic symptomatology. Finally, the yellow cluster, though smaller and less dense, includes terms like ‘bodily distress’, which may denote a more specialized subset of research within the somatic symptom domain, possibly dealing with physical distress and its psychosocial components.
To the best of our knowledge, this is the first comprehensive bibliometric analysis of the SSD. In total, 567 publications were included and analyzed. From 2013 to 2023, the number of publications related to SSD increased annually, suggesting an escalating interest and expanding research volume over the decade. This surge might be attributed to increased recognition of the disorder, improvements in diagnosis, or a greater understanding of its effects on patient life quality. The rising trend signifies not only an increase in publication frequency but possibly also a boost in citation numbers, reflecting the growing influence and recognition of SSD research. Moreover, this trend may indicate a widening scope of interdisciplinary research contributions towards a comprehensive understanding of SSD. The most productive author, institution, country and journal were Löwe with 38 publications, University of Hamburg with 60 publications, Germany with 185 publications, and Journal of Psychosomatic Research with 57 publications, respectively. A landmark study by Dimsdale et al[2], published in the Psychosomatic Research in 2013, discusses the rationale behind the SSD diagnosis introduction in DSM-5. The keyword analysis underscores the multidisciplinary nature of SSD research, bridging mental health, physical health, therapy approaches, and the societal and psychological implications of the disorder.
Based on publications of SSD, important keywords related to SSD, and highly-cited publications, the research hotspots in the field of SSD were summarized as follows.
Validity and reliability of the SSD criteria: The criteria for SSD as detailed in the DSM-5 have been crucial for the progress in diagnosing and understanding SSD[32,33]. These criteria’s validity concerns how accurately they identify actual SSD cases, focusing on the presence of somatic symptoms that cause significant distress or impact daily life, rather than on the lack of a medical explanation for these symptoms. Research has largely affirmed the criteria’s validity, showing they effectively identify individuals significantly affected by their somatic symptoms. However, the criteria’s validity faces challenges due to the subjective assessment of what constitutes “excessive” thoughts, feelings, or actions related to these symptoms, which may differ greatly across individuals and cultures. Reliability pertains to how consistently SSD can be diagnosed across various clinicians and over time[34-36]. Studies have shown a reasonable level of agreement among healthcare professionals using the DSM-5 criteria to diagnose SSD, supporting the criteria’s reliability[37,38]. Yet, difficulties in reliably assessing the degree of thoughts, feelings, or behaviors and the subjective nature of determining distress or functional impairment challenge this reliability. Additionally, the criteria’s broad and somewhat ambiguous nature can result in differences in interpretation among clinicians. While introducing SSD in DSM-5 marked an advancement in acknowledging the intricate relationship between psychological and physical symptoms, ongoing research is essential to refine these criteria and improve their validity and reliability.
Functional impairment of SSD: DSM-5 defines SSD by emphasizing the occurrence of distressing physical symptoms along with significant impairment in functioning or overly intense and disproportionate thoughts, feelings, or actions concerning these symptoms[39-41]. The diagnosis of SSD is pivotal, highlighting the extent to which these symptoms and the person’s reaction to them can disrupt normal daily activities. Such disruptions can span across work, social engagements, and personal relationships, with individuals potentially facing difficulties in keeping a job, isolating themselves due to anxiety or shame related to their symptoms, or battling with routine tasks and self-care[42-46]. An obsessive preoccupation with health issues may result in repeated medical consultations, superfluous testing, and a relentless quest for assurance about one’s health status, aggravating the person’s distress and functional decline. Additionally, the psychological and emotional dimensions of SSD, including continuous concern over the severity of symptoms, a sense of powerlessness, and an acute focus on physical sensations, can hinder normal functioning. This creates a detrimental loop of deteriorating symptoms and further decline in day-to-day functioning. The profound effect on functional capabilities highlights the necessity to perceive and manage SSD not merely as a sum of physical symptoms but as an intricate condition impacting the person’s life quality and their participation in daily activities.
Treatment for SSD: Treating SSD requires a comprehensive and interdisciplinary strategy, encompassing physiotherapy, medication, psychological therapy, and a unified treatment program to tackle the disorder’s both physical and mental facets[47,48]. Psychological therapy is pivotal for the cognitive and emotional aspects of SSD, with CBT aiding in the identification and restructuring of negative thought patterns related to symptoms, and in developing strategies to handle distress[7,9,49-51]. Additionally, mindfulness-based practices can improve patients’ perception of bodily sensations in a non-critical manner, aiding in the reduction of symptom-driven anxiety and depression. In terms of medication, managing SSD focuses on symptom relief. Antidepressants like selective serotonin reuptake inhibitors and tricyclic antidepressants are often used for their benefits in easing depression and anxiety symptoms, which frequently accompany SSD[52-54]. These drugs may also lessen some physical symptoms, particularly those associated with mood disorders. Antidepressants or anticonvulsants in low doses may be employed for pain management, and benzodiazepines might be considered for short-term anxiety relief, with careful use to avoid dependency. It’s crucial that pharmacological treatment be part of a broader therapy plan, incorporating psychological and behavioral techniques, since medications alone may not fully resolve SSD’s multifaceted symptomatology. Physiotherapy can enhance patients’ physical capabilities and movement, employing specific exercises to boost strength, flexibility, endurance, and employing pain relief techniques such as thermotherapy, massage, and electrotherapy to ease discomfort[55]. These interventions not only aim to diminish the intensity of physical symptoms but also enhance patients’ ability to perform everyday tasks. The treatment for SSD should be personalized, considering the patient’s specific symptoms, medical history, and therapy response. Integrated therapy entails a collaborative effort among various healthcare professionals to formulate a tailored treatment plan, often involving joint discussions among physiotherapists, psychologists, general practitioners, and specialists to ensure care is cohesive and goals are comprehensive, aiming at enhancing the patient's life quality and functionality. Through such an integrated treatment approach, significant progress can be made in both alleviating physical symptoms and enhancing mental health in individuals with SSD.
Further research on SSD should aim to deepen the understanding of the biological, psychological, and social factors contributing to the development and persistence of the disorder. Longitudinal studies could provide insights into the progression of symptoms and identify early predictors of chronic SSD. Moreover, investigating the effectiveness of various therapeutic interventions, such as CBT, pharmacotherapy, and integrated care models, in diverse populations would be beneficial. Research should also explore the impact of SSD on individuals’ quality of life and functioning, including how comorbidities, such as anxiety and depression, may influence treatment outcomes. Additionally, incorporating neuroimaging and genetic studies could help uncover potential biomarkers and neurobiological underpinnings, ultimately paving the way for more personalized and effective treatment strategies.
There are several limitations in our study. Firstly, the publications related to SSD were exclusively retrieved from the WoSCC database, which may limit the generalizability of the findings. Secondly, the field of SSD is considered niche and emerging, so the overall volume of documents related to SSD is relatively small, potentially limiting the comprehensiveness of the investigation. In addition, although the DSM-5 has a detailed and clear descriptive diagnosis of SSD, the evaluation of SSD-related symptoms and severity still mainly relies on related psychological questionnaires or scales in clinical practice.
In conclusion, the main research hotspots and frontiers in the field of SSD are validity and reliability of the SSD criteria, functional impairment of SSD, and the treatment for SSD. More high-quality studies are needed to assess the diagnosis and treatment of SSD.
| 1. | American Psychiatric Association; DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5™ (5th ed). American Psychiatric Publishing, Inc.. [RCA] [DOI] [Full Text] [Cited by in Crossref: 66101] [Cited by in RCA: 61372] [Article Influence: 3610.1] [Reference Citation Analysis (5)] |
| 2. | Dimsdale JE, Creed F, Escobar J, Sharpe M, Wulsin L, Barsky A, Lee S, Irwin MR, Levenson J. Somatic symptom disorder: an important change in DSM. J Psychosom Res. 2013;75:223-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 149] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 3. | Galvin CR, De Souza AM, Armstrong KR. Somatic Symptom Disorder and the Physician's Role. JAMA Pediatr. 2020;174:1000-1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Lehmann M, Pohontsch NJ, Zimmermann T, Scherer M, Löwe B. Estimated frequency of somatic symptom disorder in general practice: cross-sectional survey with general practitioners. BMC Psychiatry. 2022;22:632. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 5. | Li J, Fritzsche K, Glinka M, Pang Y, Song L, Wang Y, Li Z, He Y, Zhang Y, He S, Leonhart R, Toussaint AK, Tang L. Prevalence of DSM-5 somatic symptom disorder in Chinese patients with breast cancer. Psychooncology. 2022;31:1302-1312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 6. | Löwe B, Levenson J, Depping M, Hüsing P, Kohlmann S, Lehmann M, Shedden-Mora M, Toussaint A, Uhlenbusch N, Weigel A. Somatic symptom disorder: a scoping review on the empirical evidence of a new diagnosis. Psychol Med. 2022;52:632-648. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 98] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 7. | Berezowski L, Ludwig L, Martin A, Löwe B, Shedden-Mora MC. Early Psychological Interventions for Somatic Symptom Disorder and Functional Somatic Syndromes: A Systematic Review and Meta-Analysis. Psychosom Med. 2022;84:325-338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | Hennemann S, Böhme K, Kleinstäuber M, Baumeister H, Küchler AM, Ebert DD, Witthöft M. Internet-based CBT for somatic symptom distress (iSOMA) in emerging adults: A randomized controlled trial. J Consult Clin Psychol. 2022;90:353-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 9. | Jongsma K, Darboh BS, Davis S, MacKillop E. A cognitive behavioural group treatment for somatic symptom disorder: a pilot study. BMC Psychiatry. 2023;23:896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 10. | Lin X, Wu G, Wang S, Huang J. Bibliometric and visual analysis of doxorubicin-induced cardiotoxicity. Front Pharmacol. 2023;14:1255158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 11. | Lin X, Wang S, Huang J. A Bibliometric Analysis of Alternate-Day Fasting from 2000 to 2023. Nutrients. 2023;15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 12. | Bailer J, Kerstner T, Witthöft M, Diener C, Mier D, Rist F. Health anxiety and hypochondriasis in the light of DSM-5. Anxiety Stress Coping. 2016;29:219-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 71] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 13. | Burton C, Fink P, Henningsen P, Löwe B, Rief W; EURONET-SOMA Group. Functional somatic disorders: discussion paper for a new common classification for research and clinical use. BMC Med. 2020;18:34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 191] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 14. | Hybelius J, Kosic A, Salomonsson S, Wachtler C, Wallert J, Nordin S, Axelsson E. Measurement Properties of the Patient Health Questionnaire-15 and Somatic Symptom Scale-8: A Systematic Review and Meta-Analysis. JAMA Netw Open. 2024;7:e2446603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 15. | Hausteiner-Wiehle C, Henningsen P. Irritable bowel syndrome: relations with functional, mental, and somatoform disorders. World J Gastroenterol. 2014;20:6024-6030. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 89] [Cited by in RCA: 95] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 16. | Hedman E, Axelsson E, Andersson E, Lekander M, Ljótsson B. Exposure-based cognitive-behavioural therapy via the internet and as bibliotherapy for somatic symptom disorder and illness anxiety disorder: randomised controlled trial. Br J Psychiatry. 2016;209:407-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 74] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 17. | Henningsen P. Management of somatic symptom disorder. Dialogues Clin Neurosci. 2018;20:23-31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 103] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 18. | Liu J, Gill NS, Teodorczuk A, Li ZJ, Sun J. The efficacy of cognitive behavioural therapy in somatoform disorders and medically unexplained physical symptoms: A meta-analysis of randomized controlled trials. J Affect Disord. 2019;245:98-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 71] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 19. | Katz J, Rosenbloom BN, Fashler S. Chronic Pain, Psychopathology, and DSM-5 Somatic Symptom Disorder. Can J Psychiatry. 2015;60:160-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 106] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 20. | Kurlansik SL, Maffei MS. Somatic Symptom Disorder. Am Fam Physician. 2016;93:49-54. [PubMed] |
| 21. | Lebel S, Mutsaers B, Tomei C, Leclair CS, Jones G, Petricone-Westwood D, Rutkowski N, Ta V, Trudel G, Laflamme SZ, Lavigne AA, Dinkel A. Health anxiety and illness-related fears across diverse chronic illnesses: A systematic review on conceptualization, measurement, prevalence, course, and correlates. PLoS One. 2020;15:e0234124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 107] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 22. | Malas N, Ortiz-Aguayo R, Giles L, Ibeziako P. Pediatric Somatic Symptom Disorders. Curr Psychiatry Rep. 2017;19:11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 23. | Mutsaers B, Butow P, Dinkel A, Humphris G, Maheu C, Ozakinci G, Prins J, Sharpe L, Smith AB, Thewes B, Lebel S. Identifying the key characteristics of clinical fear of cancer recurrence: An international Delphi study. Psychooncology. 2020;29:430-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 86] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 24. | Newby JM, Hobbs MJ, Mahoney AEJ, Wong SK, Andrews G. DSM-5 illness anxiety disorder and somatic symptom disorder: Comorbidity, correlates, and overlap with DSM-IV hypochondriasis. J Psychosom Res. 2017;101:31-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 87] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 25. | Rief W, Burton C, Frostholm L, Henningsen P, Kleinstäuber M, Kop WJ, Löwe B, Martin A, Malt U, Rosmalen J, Schröder A, Shedden-Mora M, Toussaint A, van der Feltz-Cornelis C; EURONET-SOMA Group. Core Outcome Domains for Clinical Trials on Somatic Symptom Disorder, Bodily Distress Disorder, and Functional Somatic Syndromes: European Network on Somatic Symptom Disorders Recommendations. Psychosom Med. 2017;79:1008-1015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 94] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 26. | Tomenson B, Essau C, Jacobi F, Ladwig KH, Leiknes KA, Lieb R, Meinlschmidt G, McBeth J, Rosmalen J, Rief W, Sumathipala A, Creed F; EURASMUS Population Based Study Group. Total somatic symptom score as a predictor of health outcome in somatic symptom disorders. Br J Psychiatry. 2013;203:373-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 97] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 27. | Toussaint A, Hüsing P, Kohlmann S, Löwe B. Detecting DSM-5 somatic symptom disorder: criterion validity of the Patient Health Questionnaire-15 (PHQ-15) and the Somatic Symptom Scale-8 (SSS-8) in combination with the Somatic Symptom Disorder - B Criteria Scale (SSD-12). Psychol Med. 2020;50:324-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 99] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 28. | Toussaint A, Löwe B, Brähler E, Jordan P. The Somatic Symptom Disorder - B Criteria Scale (SSD-12): Factorial structure, validity and population-based norms. J Psychosom Res. 2017;97:9-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 79] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 29. | Toussaint A, Murray AM, Voigt K, Herzog A, Gierk B, Kroenke K, Rief W, Henningsen P, Löwe B. Development and Validation of the Somatic Symptom Disorder-B Criteria Scale (SSD-12). Psychosom Med. 2016;78:5-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 174] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 30. | Xiong N, Fritzsche K, Wei J, Hong X, Leonhart R, Zhao X, Zhang L, Zhu L, Tian G, Nolte S, Fischer F. Validation of patient health questionnaire (PHQ) for major depression in Chinese outpatients with multiple somatic symptoms: a multicenter cross-sectional study. J Affect Disord. 2015;174:636-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 31. | Zonneveld LN, Sprangers MA, Kooiman CG, van 't Spijker A, Busschbach JJ. Patients with unexplained physical symptoms have poorer quality of life and higher costs than other patient groups: a cross-sectional study on burden. BMC Health Serv Res. 2013;13:520. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 32. | Regier DA, Narrow WE, Clarke DE, Kraemer HC, Kuramoto SJ, Kuhl EA, Kupfer DJ. DSM-5 field trials in the United States and Canada, Part II: test-retest reliability of selected categorical diagnoses. Am J Psychiatry. 2013;170:59-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 608] [Cited by in RCA: 655] [Article Influence: 50.4] [Reference Citation Analysis (0)] |
| 33. | Links PS, Aslam H, O'Donnell M. Personality Disorders and Clinical Disorders: The Challenge of Comorbid Autism Spectrum Disorder (ASD), Eating Disorders (EDs), Posttraumatic Stress Disorder (PTSD), or Somatic Symptom Disorder (SSD). Curr Psychiatry Rep. 2024;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 34. | Claassen-van Dessel N, van der Wouden JC, Dekker J, van der Horst HE. Clinical value of DSM IV and DSM 5 criteria for diagnosing the most prevalent somatoform disorders in patients with medically unexplained physical symptoms (MUPS). J Psychosom Res. 2016;82:4-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 35. | Axelsson E, Andersson E, Ljótsson B, Wallhed Finn D, Hedman E. The health preoccupation diagnostic interview: inter-rater reliability of a structured interview for diagnostic assessment of DSM-5 somatic symptom disorder and illness anxiety disorder. Cogn Behav Ther. 2016;45:259-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 36. | Hüsing P, Löwe B, Toussaint A. Comparing the diagnostic concepts of ICD-10 somatoform disorders and DSM-5 somatic symptom disorders in patients from a psychosomatic outpatient clinic. J Psychosom Res. 2018;113:74-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 37. | Münker L, Rimvall MK, Frostholm L, Ørnbøl E, Wellnitz KB, Jeppesen P, Rosmalen JGM, Rask CU. Infancy predictors of functional somatic symptoms in pre- and late adolescence: a longitudinal cohort study. Eur J Pediatr. 2024;184:57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 38. | Clarke DE, Narrow WE, Regier DA, Kuramoto SJ, Kupfer DJ, Kuhl EA, Greiner L, Kraemer HC. DSM-5 field trials in the United States and Canada, Part I: study design, sampling strategy, implementation, and analytic approaches. Am J Psychiatry. 2013;170:43-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 118] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 39. | Axelsson E, Hedman-Lagerlöf E. Validity and clinical utility of distinguishing between DSM-5 somatic symptom disorder and illness anxiety disorder in pathological health anxiety: Should we close the chapter? J Psychosom Res. 2023;165:111133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 40. | Huang WL, Chang SS, Wu SC, Liao SC. Population-based prevalence of somatic symptom disorder and comorbid depression and anxiety in Taiwan. Asian J Psychiatr. 2023;79:103382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 24] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 41. | Shen S, Dong Z, Zhang Q, Xiao J, Zhou D, Li J. The overlapping relationship among depression, anxiety, and somatic symptom disorder and its impact on the quality of life of people with epilepsy. Ther Adv Neurol Disord. 2022;15:17562864221138147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 42. | Huang WC, Liao SC, Huang WL. Chronicity of Somatic Distress and Healthy Anxiety in Patients With Somatic Symptom Disorder: One-Year Follow-up. J Acad Consult Liaison Psychiatry. 2022;63:647-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 43. | Lee S, Creed FH, Ma YL, Leung CM. Somatic symptom burden and health anxiety in the population and their correlates. J Psychosom Res. 2015;78:71-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 44. | Lyssenko L, Schmahl C, Bockhacker L, Vonderlin R, Bohus M, Kleindienst N. Dissociation in Psychiatric Disorders: A Meta-Analysis of Studies Using the Dissociative Experiences Scale. Am J Psychiatry. 2018;175:37-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 288] [Article Influence: 36.0] [Reference Citation Analysis (0)] |
| 45. | Sauer KS, Witthöft M, Rief W. Somatic Symptom Disorder and Health Anxiety: Assessment and Management. Neurol Clin. 2023;41:745-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 46. | Wolters C, Gerlach AL, Pohl A. Interoceptive accuracy and bias in somatic symptom disorder, illness anxiety disorder, and functional syndromes: A systematic review and meta-analysis. PLoS One. 2022;17:e0271717. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 34] [Reference Citation Analysis (0)] |
| 47. | Hijne K, van Eck van der Sluijs JF, van Broeckhuysen-Kloth SAM, Lucassen PLBJ, Reinders M, Tak LM, Gerritsen L, Geenen R. Individual treatment goals and factors influencing goal attainment in patients with somatic symptom disorder from the perspective of clinicians: A concept mapping study. J Psychosom Res. 2022;154:110712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 48. | Maroti D, Lumley MA, Schubiner H, Lilliengren P, Bileviciute-Ljungar I, Ljótsson B, Johansson R. Internet-based emotional awareness and expression therapy for somatic symptom disorder: A randomized controlled trial. J Psychosom Res. 2022;163:111068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 49. | Furutani N, Nagoshi Y. Vortioxetine as an alternative treatment for somatic symptom disorder: case report. Front Psychiatry. 2024;15:1496072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 50. | Newby JM, Smith J, Uppal S, Mason E, Mahoney AEJ, Andrews G. Internet-based cognitive behavioral therapy versus psychoeducation control for illness anxiety disorder and somatic symptom disorder: A randomized controlled trial. J Consult Clin Psychol. 2018;86:89-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 51. | Verdurmen MJ, Videler AC, Kamperman AM, Khasho D, van der Feltz-Cornelis CM. Cognitive behavioral therapy for somatic symptom disorders in later life: a prospective comparative explorative pilot study in two clinical populations. Neuropsychiatr Dis Treat. 2017;13:2331-2339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 52. | Hirakawa H, Terao T, Ishii N. A Case of Facial Pain in Somatic Symptom Disorder Responding to Duloxetine. J Clin Psychopharmacol. 2020;40:512-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 53. | Miyauchi T, Tokura T, Kimura H, Ito M, Umemura E, Sato Boku A, Nagashima W, Tonoike T, Yamamoto Y, Saito K, Kurita K, Ozaki N. Effect of antidepressant treatment on plasma levels of neuroinflammation-associated molecules in patients with somatic symptom disorder with predominant pain around the orofacial region. Hum Psychopharmacol. 2019;34:e2698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 54. | Wang S, Xu Y, Xiao X, Guo P, Lv L, Fang Y, Huang J, Zhang N, Feng M, Cheng S, Wang S, Chen H. Intravenous infusion with esketamine rapidly alleviates refractory somatic symptom disorder: A case report. Asian J Psychiatr. 2024;97:104076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 55. | Sartori R, Tessitore A, Della Torca A, Barbi E. Efficacy of physiotherapy treatments in children and adolescents with somatic symptom disorder and other related disorders: systematic review of the literature. Ital J Pediatr. 2022;48:127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/