Published online Jul 19, 2024. doi: 10.5498/wjp.v14.i7.999
Revised: May 14, 2024
Accepted: June 19, 2024
Published online: July 19, 2024
Processing time: 92 Days and 18.8 Hours
Cognitive-behavioral therapy (CBT) and habit reversal training (HRT) have shown application potential in addressing tic symptoms and comorbid psychiatric conditions. Despite their theoretical potential, empirical evidence on their combined efficacy remains limited.
To evaluate the efficacy of CBT combined with HRT on anxiety disorders in children with Tourette’s syndrome (TS).
Clinical data of children with TS admitted to our hospital from January 2022 to June 2023 were collected, and the patients were grouped into the conventional therapy (control) group and the CBT combined with HRT group. Baseline characteristics, anxiety scores, tic severity scores, treatment adherence, and parental satisfaction were assessed. Statistical analysis was performed using t-tests, chi-square tests, and correlation analysis.
A total of 136 patients, including 65 patients in the control group and 71 patients in the CBT combined with HRT group, were included. The CBT combined with HRT group showed remarkable improvements compared with the control group. Post-intervention assessment revealed a decrease in anxiety scores from 63.52 ± 1.81 to 40.53 ± 1.64 (t = 2.022, P = 0.045), and the Yale Global Tic Severity Scale total score decreased from 22.14 ± 5.67 to 16.28 ± 4.91 (t = 2.288, P = 0.024). Treatment adherence was significantly higher in the CBT combined with HRT group (85.47 ± 7.62%) compared with the control group (82.32 ± 6.54%; t = 2.596, P = 0.010). Parental satisfaction scores were also higher in the CBT combined with HRT group (8.69 ± 1.77) compared with the control group (7.87 ± 1.92; t = 2.592, P = 0.011).
This study demonstrates that CBT combined with HRT significantly reduces anxiety symptoms and tic severity in children with TS, with higher treatment adherence and parental satisfaction. These findings support the potential application of this comprehensive therapeutic approach for TS treatment.
Core Tip: This study aimed to evaluate the relationship between the levator ani muscle hiatus (LH) area and pelvic organ prolapse (POP) in parturients with gestational diabetes mellitus using perineal ultrasound. Conclusion: Three-dimensional perineal ultrasonography evaluation of the LH size and shape changes can effectively diagnose POP.
- Citation: Wang YZ, Zhang X, Han XM. Efficacy of cognitive-behavioral therapy combined with habit reversal training on anxiety disorders in children with Tourette’s syndrome. World J Psychiatry 2024; 14(7): 999-1008
- URL: https://www.wjgnet.com/2220-3206/full/v14/i7/999.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i7.999
Tourette’s syndrome (TS) is a complex neurodevelopmental disorder characterized by multiple motor and one or more vocal tics, with onset in childhood or adolescence[1]. The manifestation of tics can be highly variable, in terms of their nature (motor vs vocal tics) and severity, affecting the quality of life and psychosocial functioning of those diagnosed[2]. Apart from the primary tic symptoms, TS is frequently associated with comorbid psychiatric conditions and notable anxiety disorders, which can exacerbate the overall disease burden on affected individuals[3]. Anxiety disorders in children with TS are particularly concerning as they can interfere with social development, educational attainment, and overall well-being[4].
The conventional therapeutic approach to managing TS focuses on pharmacological treatment to mitigate the severity of tics[5,6]. However, medications such as antipsychotics, which is often used in treatment, can have a variety of adverse effects that may dissuade patients and their families from pursuing these options[7]. Given these challenges, alternative treatment modalities to address tics and the often-associated psychiatric comorbidities have been receiving increasing interest[8].
Cognitive-behavioral therapy (CBT) has emerged as a promising psychological intervention for a range of psychiatric disorders, including anxiety[7,9]. It is grounded in the conceptual framework that maladaptive thoughts and beliefs underlie and perpetuate psychological symptoms[10]. CBT works by helping individuals identify and challenge these unhelpful thought patterns, thereby reducing psychiatric symptoms and enhancing coping strategies[11]. Habit reversal training (HRT), another behavioral intervention, specifically targets the tic symptoms of TS by increasing the awareness of tic behaviors and teaching competing responses[12,13]. By combining CBT and HRT, there exists a potentially synergistic therapeutic approach that targets the tic symptoms and psychiatric comorbidities of TS, particularly anxiety disorders[13].
The rationale for combining CBT with HRT in treating children with TS stems from the multidimensional nature of the disorder[14]. Tics in TS were not merely neurological symptoms but were significantly influenced by psychological stressors, with anxiety known to exacerbate tic severity[15]. By addressing the psychological aspects of the disorder through CBT, alongside the specific tic behaviors through HRT, a more holistic approach to treatment was offered[16]. Such an approach not only aims at reducing tic severity but also at improving the overall mental health and quality of life of the affected children[17].
Despite the theoretical potential of this combined treatment modality, empirical evidence on its efficacy remains relatively limited[13]. Given the chronic nature of TS and the impact of psychiatric comorbidities such as anxiety disorders on treatment outcomes, understanding these aspects of the therapeutic process is essential. Thus, this study aimed to fill these gaps by conducting a rigorous evaluation of the efficacy of CBT combined with HRT on anxiety disorders in children with TS. By leveraging a retrospective cohort design, this research seeks to compare the outcomes of a CBT and HRT combined treatment modality against conventional therapy, focusing on measures of anxiety, tic severity, treatment adherence, and parental satisfaction.
This study was retrospective in nature. Clinical data of children with TS admitted to our hospital from January 2022 to June 2023 were collected, and the patients were grouped into the conventional therapy (control) group and the CBT combined with HRT group. The patient selection involved several steps to ensure respect for and consideration of patient preferences. First, the physicians provided comprehensive information about existing treatment options, including their benefits and potential risks, to all patients in a clear and understandable manner, ensuring that the patients fully comprehended their choices. Subsequently, mutual decision-making between the patients and physicians, considering the patients’ medical conditions, personal values, and preferences, involved open and honest discussions of available treatment modalities. This study was approved by the Ethics Committee of Affiliated Hospital of Nanjing University of Chinese Medicine, and it obtained an informed consent form.
The inclusion criteria were as follows: (1) Children diagnosed with TS in accordance with the diagnostic criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition[18]; (2) Normal intelligence; (3) Age between 4 and 14 years; (4) Normal physical function; (5) Symptoms of TS not attributable to the physiological effects of a substance (such as cocaine) or other conditions (such as Huntington’s disease and viral encephalitis); (6) Moderate-to-severe TS, assessed using the Yale Global Tic Severity Scale (YGTSS) with a score greater than 20; (7) Completion of 6 months of follow-up; and (8) Complete medical records.
The exclusion criteria were as follows: (1) Tourette-like symptoms caused by conditions such as rheumatic chorea, Sydenham’s chorea, Wilson’s disease, encephalitis, or drug-induced disorders; (2) Concurrent severe primary diseases involving the cardiovascular, pulmonary, hepatic, renal, or hematopoietic systems; (3) Patients with additional diseases requiring specific treatment during the study, which could affect the primary diagnosis, or those with severe physical illnesses; and (4) Inability to adhere to the treatment plan.
The control group received Clonidine transdermal patches (Shanxi Ruifulei Pharmaceutical Co., Ltd.), which were applied below the shoulder blade on the back and replaced every 7 days (alternating sides of the shoulder blade), concluding after 24 weeks. The Clonidine dosage was as follows: 1.0 mg per patch for body weight between 20 and 40 kg, 1.5 mg per patch for body weight between 40 and 60kg, and 2.0 mg per patch for body weight over 60 kg.
The CBT combined with HRT group underwent CBT combined with HRT, administered once a week for 60 minutes, concluding after 24 weeks. The cognitive-behavioral interventions were as follows: (1) Regular education for parents and children about TS, promoting understanding and support and dispelling misconceptions; (2) Encouraging children not to blame themselves for the disorder, to manage social interactions, and to build confidence in treatment; explaining the fluctuating nature of symptoms and the favorable overall prognosis to alleviate anxiety; (3) Encouraging appropriate physical activities while avoiding competitive or aggressive behaviors and stimuli such as violent media or gaming; and (4) Collaboratively identifying and addressing triggers for tic symptoms with family and therapists to develop coping strategies.
HRT: (1) Awareness training: Response description: Children were instructed to face a mirror and provide detailed descriptions of their tics, reenacting the tic movements; Response detection: When tics occur, the therapist promptly points them out to enhance the children’s ability to notice their tics through this training; Early warning procedure: Children were taught to recognize the premonitory urges of tics, including the impulse to tic preceding the actual tic or the early signs of motor tics, and to identify the earliest premonitory signs when tics occur; Situational awareness training: The common situations triggering tics were determined through data analysis, which involves direct video feedback using video recorders and mirrors, as well as the use of smart wearable watches, small notebooks, and other devices to record tic occurrences; (2) Response competition training: Once children have developed a reliable ability to detect tics and premonitory urges, they were educated to perform response competition every time premonitory urges or tics occur, maintaining this competition for 1-3 minutes or until the urge to tic subsides. Response competition behavior should meet the following criteria: Be neurologically opposite; Be sustainable for several minutes; Produce equal muscle tension as the target movement; Not attract attention in social activities, easily compatible with ongoing normal activities, but incompatible with habits (referring to tics); For muscular tics, the behavior must strengthen muscle movements that compete with the tic; (3) Anxiety management techniques: Deep breathing, progressive muscle relaxation, and visualization were the commonly used anxiety management techniques for tic disorders. For children experiencing anxiety or stress, integrating relaxation techniques were an essential part of HRT; and (4) Motivational and assistance techniques: Reviewing the troubles of habits: In the early stages of treatment, children and therapists create a “Tic Trouble Chart,” listing all the negative impacts of tics (such as embarrassment, discomfort, interference, and need for medical attention). Occasionally, reviewing the chart continues until improvements were made to render the chart obsolete. Apart from breaking the children’s denial of symptoms and reinforcing treatment motivation, the chart can also serve as a step for them to explore the causal relationship of tic disorders and promote a more realistic acceptance of their situation; Tic severity rating: At the beginning of treatment, children and therapists create a comprehensive list of the child’s tics, and then they rate each tic on a scale of 1 to 10 based on the extent of disturbance or distress caused by the tic (10 points = most distressing). For young children or those who deny that tics cause distress, classifying tic severity based on the frequency of occurrence rather than distress and using different measurement criteria were necessary. Then, the tic symptoms were arranged in the order of least to most distressing (or frequency). Reviewing this chart and reassessing the tic levels before each treatment provide a systematic and immediate method for setting treatment goals and challenges; Social support: If a child successfully applies awareness skills or completes other treatment tasks, then the child has a period free of tics and adheres to the treatment protocol. Other family members, sometimes even teachers and friends, should commend and support the child; Behavioral reward system: A systematic reward system was developed to incentivize and enhance the compliance of children who complete the behavioral treatment plan.
Through systematic case retrieval, the general information of the pediatric patients was gathered, including age, gender, body mass index (BMI), age of onset, duration of TS and coprolalia, comorbidities such as ADHD and OCD, previous treatment rates, parental education level, parental marital status, family history of ADHD, family history of OCD, and family history of TS and coprolalia.
The anxiety status of the two groups of patients was assessed before treatment and at the 24th week of treatment using the Self-rating Anxiety Scale (SAS). The SAS consists of 20 items with a total score of 100, covering emotional symptoms, physical dysfunction, mental agitation, and psychological distress. The anxiety level was inversely related to the total score; scores below 50 indicate no anxiety, 50-59 indicate mild anxiety, 60-69 indicate moderate anxiety, and 70 and above indicate severe anxiety. The scale demonstrated a Cronbach’s alpha coefficient of 0.849[19].
Compared with the YGTSS scores, the YGTSS score was obtained by combining the scores for motor tics, vocal tics, and functional impairment. Higher YGTSS scores indicate more severe symptoms, with a maximum score of 100 and a Cronbach’s alpha coefficient of 0.84[20].
Clinical symptoms of the enrolled subjects were collected using the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) assessment. The Y-BOCS includes 10 items, each rated on a five-point scale (0-4) to evaluate the severity of obsessions and compulsions, with a total score of 40. Higher scores represent more severe symptoms, with a Cronbach’s alpha coefficient of 0.875[21].
Patients were evaluated using the Clinical Global Impression-Severity (CGI-S) scale, which measures illness severity on a scale of 0-7, with scores inversely correlated to treatment effectiveness and a Cronbach’s alpha coefficient of 0.839[22].
The Family Adaptability and Cohesion Evaluation Scale (FACES-III) was used to assess emotional connectedness and adaptability among family members, comprising 20 items with a five-point scoring system (1 being “never” and 5 being “always”). Higher scores indicate greater family cohesion and adaptability.
At week 24 post-treatment, patient adherence was evaluated using the Treatment Adherence Rating Scale, which consists of five items assessing compliance with regard to agreement and adherence to psychological therapy on a scale of 0% to 100%. A higher total score indicates better adherence to psychological therapy. In addition, patient treatment satisfaction was assessed through a self-made questionnaire, which results in a 10-point score. The scores were categorized as follows: highly satisfied (8-10 points), satisfied (7-8 points), fair (6-7 points), and dissatisfied (< 6 points). The statistical assessment of patient treatment recommendations was also included.
Before conducting data analysis, this study performed a standardized data cleaning process to identify and correct any inconsistencies, errors, or missing values. This process involved thorough examination of the dataset, removal of duplicate entries, correction of data input errors, and handling missing values. In Python 3.6.0, the Impyute library was utilized for KNN imputation to fill in missing values. Initially, a basic mean imputation was created in the complete list to construct a KDTree. Subsequently, the KDTree was used to calculate the nearest distances (NN) and find the K nearest points, followed by taking the weighted average of these points. The missing data were kept within 5% to control potential selection bias and underwent sensitivity analysis. The outcomes of loss to follow-up cases were calculated separately on the basis of the worst and best outcomes. If no significant difference was observed, then the loss to follow-up had minimal impact on the conclusions, thereby ensuring the reliability of the conclusions. The final output consisted of the results after filling in the missing values.
Using G*Power 3.1.9.7, the “Means: Difference between two independent means (two groups)” option based on t-tests was used for post hoc analysis, with two-tailed mode, effect size d = 0.6, α err prob = 0.05. Subsequently, the sample sizes of the two groups were input to calculate power (1-β err prob), resulting in a power value of 0.934.
The data were analyzed using SPSS 29.0 statistical software (SPSS Inc., Chicago, IL, United States). Categorical data were represented as [n (%)]. The χ2 test was applied with the basic formula when the sample size was ≥ 40 and the theoretical frequency T was ≥ 5, with the test statistic represented by χ2. When the sample size was ≥ 40 but the theoretical frequency was 1 ≤ T < 5, the χ2 test was adjusted using the correction formula. Statistical analysis for cases where the sample size was < 40 or the theoretical frequency was T < 1 was conducted using the Fisher’s exact probability method. Continuous variables underwent normal distribution testing using the Shapiro-Wilk method. For normally distributed continuous data, the format (mean ± SD) was used. Non-normally distributed data were analyzed using the Wilcoxon rank-sum test, and the [median (25% quantile, 75% quantile)] was used for presentation. Statistical significance was set at P < 0.05. Correlation analysis used Pearson correlation analysis for continuous variables and Spearman correlation analysis for categorical variables.
A total of 136 patients, including 65 patients in the control group and 71 patients in the CBT combined with HRT group, were included. The baseline characteristics of the participants in the study are presented in Table 1. These two groups had similar baseline characteristics, including age, gender distribution, BMI, age of onset of TS, duration of TS, comorbid ADHD, comorbid OCD, previous treatment, parental education, parental marital status, family history of ADHD, family history of OCD, and family history of TS. No statistically significant differences in any of the baseline characteristics were observed between the two groups, as evidenced by the non-significant P-values for all comparisons (P > 0.05).
| Characteristic | Control (n = 65) | CBT combined with HRT (n = 71) | t/χ2 | P value |
| Age (years) | 11.54 ± 2.31 | 11.72 ± 2.13 | 0.465 | 0.643 |
| Gender [male/female, n (%)] | 40 (61.54)/25 (38.46) | 45 (63.38)/26 (36.62) | 0.002 | 0.965 |
| BMI | 16.73 ± 2.14 | 17.24 ± 2.35 | 1.326 | 0.187 |
| Age of onset (years) | 8.74 ± 2.46 | 8.61 ± 2.38 | 0.302 | 0.763 |
| Duration of Tourette’s syndrome (months) | 16.28 ± 4.67 | 15.92 ± 5.01 | 0.434 | 0.665 |
| Comorbid ADHD, n (%) | 17 (26.15) | 20 (28.17) | 0.005 | 0.943 |
| Comorbid OCD, n (%) | 11 (16.92) | 10 (14.08) | 0.048 | 0.826 |
| Previous treatment, n (%) | 27 (41.54) | 27 (38.03) | 0.059 | 0.808 |
| Parental education | None | 0.779 | ||
| High school or less | 23 (35.38) | 20 (28.17) | ||
| Some college | 16 (24.62) | 21 (29.58) | ||
| Bachelor’s degree | 13 (20.00) | 18 (25.35) | ||
| Master’s degree | 10 (15.38) | 8 (11.27) | ||
| Doctoral degree | 3 (4.62) | 4 (5.63) | ||
| Parental marital status, n (%) | None | 0.919 | ||
| Married | 45 (69.23) | 52 (73.24) | ||
| Divorced/separated | 10 (15.38) | 9 (12.68) | ||
| Single parent | 7 (10.77) | 6 (8.45) | ||
| Other | 3 (4.62) | 4 (5.63) | ||
| Family history of ADHD, n (%) | 7 (10.77) | 9 (12.68) | 0.006 | 0.938 |
| Family history of OCD, n (%) | 7 (10.77) | 9 (12.68) | 0.006 | 0.938 |
| Family history of Tourette’s syndrome, n (%) | 16 (24.62) | 21 (29.58) | 0.209 | 0.648 |
The pre-intervention anxiety and tic severity scores for the control group and the CBT combined with HRT group are summarized in Table 2. No statistically significant differences in the anxiety score, YGTSS total score, Children's Yale-Brown Obsessive Compulsive Scale (CY-BOCS) total score, CGI-S score, and FACES IV score were found between the two groups, as indicated by non-significant P-values for all comparisons (P > 0.05). The mean scores for anxiety and tic severity were comparable between the control and intervention groups before the intervention.
| Measure | Control (n = 65) | CBT combined with HRT (n = 71) | t value | P value |
| Anxiety score | 63.52 ± 1.81 | 64.03 ± 1.67 | 1.703 | 0.091 |
| YGTSS total score | 22.14 ± 5.67 | 21.89 ± 5.12 | 0.274 | 0.785 |
| CY-BOCS total Score | 18.25 ± 4.92 | 18.51 ± 4.57 | 0.324 | 0.747 |
| CGI-S score | 3.48 ± 0.82 | 3.56 ± 0.75 | 0.632 | 0.528 |
| FACES IV score | 15.89 ± 5.12 | 14.72 ± 4.78 | 1.374 | 0.172 |
Statistically significant improvements in anxiety and tic severity scores were observed following the intervention with CBT combined with HRT compared with the control group (Table 3). In particular, post-intervention assessment revealed a decrease in anxiety scores from 40.53 ± 1.64 to 39.97 ± 1.58 in the CBT combined with HRT group, with a t-value of 2.022 and a P-value of 0.045. Furthermore, the YGTSS total score decreased from 16.28 ± 4.91 to 14.49 ± 4.12 (t = 2.288, P = 0.024); the CY-BOCS total score decreased from 13.36 ± 3.82 to 11.75 ± 3.49 (t = 2.555, P = 0.012); the CGI-S score decreased from 2.31 ± 0.68 to 2.08 ± 0.59 (t = 2.146, P = 0.034), and the FACES IV score increased from 24.77 ± 6.28 to 27.48 ± 5.93 (t = 2.586, P = 0.011). These findings indicate that CBT combined with HRT has a beneficial impact on anxiety and tic severity in children with TS.
| Measure | Control (n = 65) | CBT combined with HRT (n = 71) | t value | P value |
| Anxiety score | 40.53 ± 1.64 | 39.97 ± 1.58 | 2.022 | 0.045 |
| YGTSS total score | 16.28 ± 4.91 | 14.49 ± 4.12 | 2.288 | 0.024 |
| CY-BOCS total Score | 13.36 ± 3.82 | 11.75 ± 3.49 | 2.555 | 0.012 |
| CGI-S score | 2.31 ± 0.68 | 2.08 ± 0.59 | 2.146 | 0.034 |
| FACES IV score | 24.77 ± 6.28 | 27.48 ± 5.93 | 2.586 | 0.011 |
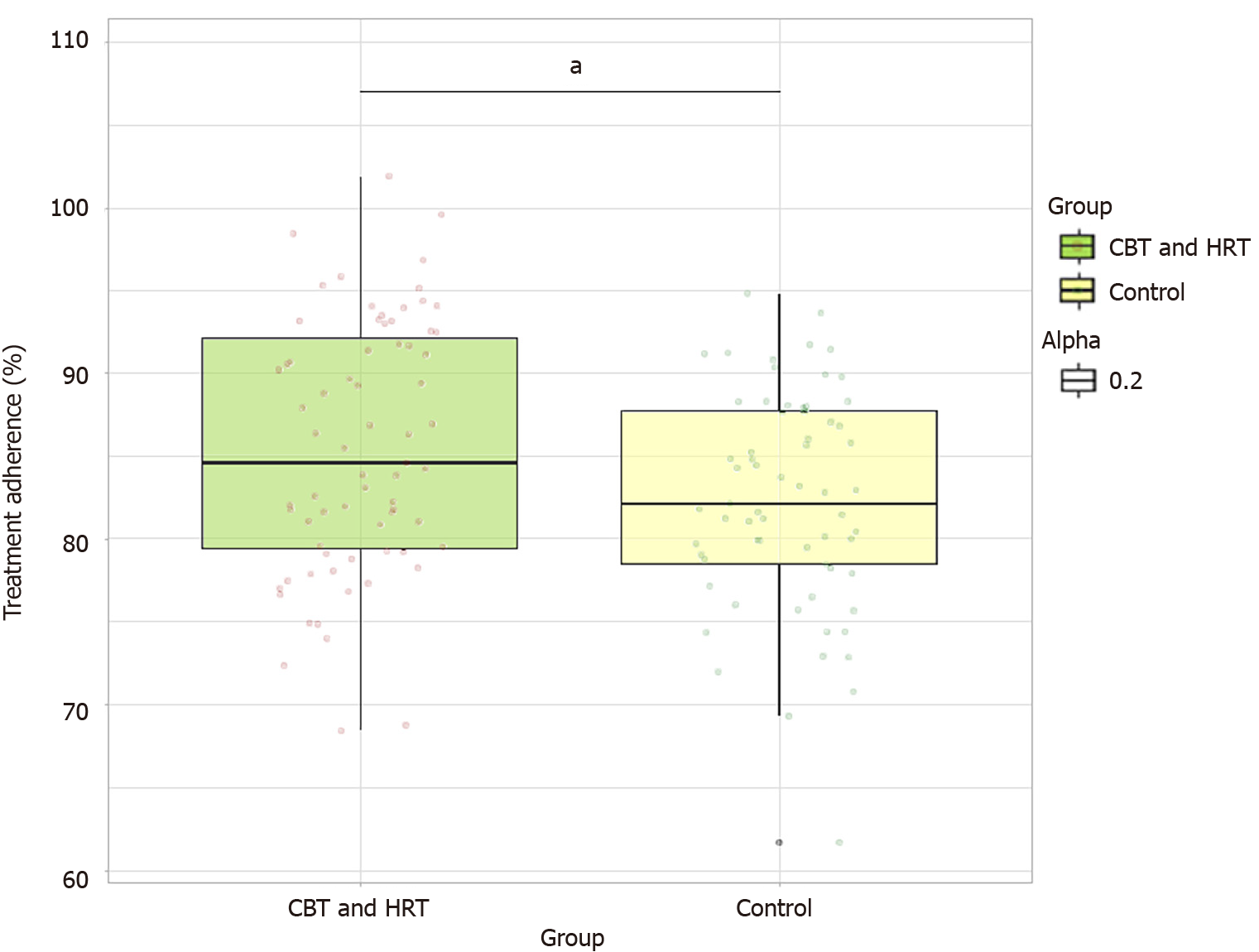
Upon evaluating treatment adherence, the group undergoing CBT combined with HRT demonstrated significantly higher adherence compared with the control group (Figure 1). In particular, the CBT combined with HRT group exhibited a treatment adherence of 85.47% ± 7.62%, whereas the control group showed a treatment adherence of 82.32% ± 6.54% (t = 2.596, P = 0.010).
Analysis of the parental satisfaction survey results indicated notable findings regarding the perception of the CBT combined with HRT intervention (Table 4). The CBT combined with HRT group demonstrated higher levels of satis
| Measure | Control (n = 65) | CBT combined with HRT (n = 71) | t/χ2 | P value |
| Satisfaction score (1-10) | 7.87 ± 1.92 | 8.69 ± 1.77 | 2.592 | 0.011 |
| Would recommend, n (%) | 51 (78.46) | 66 (92.96) | 4.788 | 0.029 |
Correlation analysis revealed associations between CBT combined with HRT treatment and post-intervention anxiety and tic severity scores (Table 5). The analysis demonstrated statistically significant negative correlations among the CBT combined with HRT treatment and anxiety scores (r = -0.172, R2 = 0.03, P = 0.045), YGTSS total score (r = -0.195, R2 = 0.038, P = 0.023), CY-BOCS total score (r = -0.216, R2 = 0.047, P = 0.011), and CGI-S score (r = -0.183, R2 = 0.034, P = 0.033). Moreover, a statistically significant positive correlation was observed between the CBT combined with HRT treatment and FACES IV score (r = 0.219, R2 = 0.048, P = 0.011), indicating the potential impact of the intervention on anxiety and tic severity measures.
| Measure | r | R2 | P value |
| Anxiety score (1-10) | −0.172 | 0.03 | 0.045 |
| YGTSS total score | −0.195 | 0.038 | 0.023 |
| CY-BOCS total Score | −0.216 | 0.047 | 0.011 |
| CGI-S score | −0.183 | 0.034 | 0.033 |
| FACES IV score | 0.219 | 0.048 | 0.011 |
This study aimed to evaluate the efficacy of CBT combined with HRT on anxiety disorders in children diagnosed with TS. The results indicate significant improvements in anxiety scores and tic severity measures in the group that underwent CBT combined with HRT, compared with the control group receiving conventional therapy.
The choice of combining CBT with HRT stems from their respective efficacy in managing tic disorders and associated psychological conditions, such as anxiety[23]. CBT was known for its success in modifying thought patterns and behaviors that contribute to psychological stress[24]. On the contrary, HRT focuses on increasing awareness of tic behaviors and implementing competing responses. The integration of these two therapies targets the dual aspects of TS-its physical manifestations and associated psychological impacts, thereby providing a comprehensive treatment approach[25].
Consistent with existing literature[24], this study found that the combination of CBT and HRT effectively reduced anxiety levels in pediatric patients with TS. Studies have previously shown that CBT can reduce symptoms of anxiety and improve the overall quality of life in this patient population[25,26]. For example, Billnitzer and Jankovic[27] highlighted the positive impact of behavioral interventions on tic severity, advocating for their early implementation in the thera
Understanding the enduring effects and sustainability of the intervention over an extended period is important to ascertain its continued efficacy. In addition, investigating potential moderators of treatment response, such as age, gender, or specific tic symptomatology, could provide valuable insights into the nuanced factors influencing the effectiveness of the combined therapeutic approach. Furthermore, comparative effectiveness studies comparing CBT combined with HRT with other therapeutic modalities could provide comprehensive insights into the relative benefits and limitations of different treatment approaches, aiding in the development of evidence-based guidelines for the management of TS and anxiety disorders in children. These future research directions could contribute to a more nuanced and tailored approach to treatment while enhancing the overall understanding of the optimal management of TS and its comorbidities.
Moreover, the finding that CBT combined with HRT results in better treatment adherence and parental satisfaction further strengthens the case for this treatment modality. Previous research[28] has emphasized the importance of patient and caregiver engagement in the treatment process, as it directly influences treatment outcomes. The high adherence rates observed in this study could be attributed to the active involvement and empowerment of children and their families throughout the treatment process, enhancing their commitment and satisfaction.
From a theoretical standpoint, this study contributes to the understanding of how comprehensive behavioral therapies can modulate the manifestation of TS and its comorbidities, such as anxiety disorders. The positive correlation between CBT combined with HRT and reduced anxiety and tic severity corroborates the notion that these therapeutic approaches can alter the neurological and psychological underpinnings of this condition.
The remarkable reduction in anxiety symptoms and tic severity in children with TS following a CBT combined with HRT intervention can be understood through several interconnected mechanisms. These reasons were rooted in the psychological framework of TS and the neurobiological underpinnings that govern its manifestation.
In the HRT framework, HRT focuses on increasing patient’s awareness of their tic behaviors and urges and then teaches competing responses. By consciously implementing a behavior that is physically incompatible with the tic, the patient can inhibit the manifestation of tic. This process reduces tic severity while empowering the child, leading to reduced anxiety over the loss of control associated with tic outbreaks. In addition, many children with TS experience premonitory urges, such as uncomfortable sensations that precede tics[29]. HRT helps children recognize these urges and apply techniques to alleviate them before they escalate into full-blown tics. Reducing these premonitory urges can decrease the severity of tics and the anxiety associated with anticipating these urges.
In neurobiological mechanisms, emerging research suggests that behavioral therapies, including CBT and HRT, can modulate the neural circuits implicated in TS[30]. These therapies may help normalize the functioning of cortico-striato-thalamo-cortical circuits, which were often dysregulated in TS[31]. Improved regulation of these neural pathways can lead to reduced tic severity and can decrease anxiety by enhancing the overall neurological function and emotional regulation[32,33]. In addition, stress is known to exacerbate tics and anxiety[34]. CBT and HRT can effectively reduce stress levels, potentially through the downregulation of the hypothalamic-pituitary-adrenal axis and the modulation of neurotransmitter systems involved in stress and anxiety, such as serotonin and dopamine[34]. By reducing stress, these therapies indirectly contribute to a decrease in tic severity and anxiety symptoms.
Practically, the implications of these findings were far-reaching. Implementing CBT combined with HRT as a standard treatment option could transform the therapeutic landscape for children with TS. By prioritizing treatments that show higher efficacy and satisfaction among patients and caregivers, healthcare providers can improve treatment outcomes and the quality of life for this population.
However, this study has some limitations. The retrospective nature of the study and the reliance on existing medical records might introduce biases related to data accuracy and completeness. In addition, although the study’s sample size is adequate for statistical analysis, it might not fully capture the diversity and complexity of TS presentations in the broader population.
Further research, particularly prospective studies with larger and more diverse cohorts, is necessary to validate these findings. Investigating the long-term outcomes of CBT combined with HRT, beyond the 24-week follow-up period, would provide insights into the enduring effects of this treatment modality. In addition, exploring individual com
This study demonstrates that CBT combined with HRT remarkably reduces anxiety symptoms and tic severity in children with TS. The observed improvements in treatment adherence and parental satisfaction further support the application of this comprehensive therapeutic approach. These findings indicate that healthcare providers who manage children with TS and comorbid anxiety should consider integrating CBT combined with HRT as a first-line or adjunctive treatment modality. Given the potential impact of this combined approach on reducing anxiety and tic severity, healthcare providers should be encouraged to undergo specific training to effectively implement and integrate CBT and HRT into their practice. Furthermore, promoting active involvement of parents and caregivers in the treatment process is crucial for healthcare providers, emphasizing the importance of their support and adherence.
| 1. | Rusheen AE, Rojas-Cabrera J, Goyal A, Shin H, Yuen J, Jang DP, Bennet KE, Blaha CD, Lee KH, Oh Y. Deep brain stimulation alleviates tics in Tourette syndrome via striatal dopamine transmission. Brain. 2023;146:4174-4190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 2. | Lin K, Wang Y, Wang J, Zhang C, Feng Q. Treatment of Tourette syndrome by acupuncture combined with Chinese medicine based on syndrome differentiation: A review. Medicine (Baltimore). 2023;102:e34268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Pringsheim T, Ganos C, Nilles C, Cavanna AE, Gilbert DL, Greenberg E, Hartmann A, Hedderly T, Heyman I, Liang H, Malaty I, Malik O, Debes NM, Vahl KM, Munchau A, Murphy T, Nagy P, Owen T, Rizzo R, Skov L, Stern J, Szejko N, Worbe Y, Martino D. European Society for the Study of Tourette Syndrome 2022 criteria for clinical diagnosis of functional tic-like behaviours: International consensus from experts in tic disorders. Eur J Neurol. 2023;30:902-910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 48] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 4. | Hartmann A, Andrén P, Atkinson-Clément C, Czernecki V, Delorme C, Monique Debes NM, Müller-Vahl K, Paschou P, Szejko N, Topaloudi A, Ueda K, Black KJ. Tourette syndrome research highlights from 2022. F1000Res. 2023;12:826. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Pringsheim T, Piacentini J. Internet-Based Cognitive Behavioral Therapy for Tourette Syndrome-Meaningfully Improving Access to Behavioral Therapy for Tics. JAMA Netw Open. 2022;5:e2225627. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Gur N, Zimmerman-Brenner S, Fattal-Valevski A, Rotstein M, Pilowsky Peleg T. Group comprehensive behavioral intervention for tics contribution to broader cognitive and emotion regulation in children. Eur Child Adolesc Psychiatry. 2023;32:1925-1933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Tsetsos F, Topaloudi A, Jain P, Yang Z, Yu D, Kolovos P, Tumer Z, Rizzo R, Hartmann A, Depienne C, Worbe Y, Müller-Vahl KR, Cath DC, Boomsma DI, Wolanczyk T, Zekanowski C, Barta C, Nemoda Z, Tarnok Z, Padmanabhuni SS, Buxbaum JD, Grice D, Glennon J, Stefansson H, Hengerer B, Yannaki E, Stamatoyannopoulos JA, Benaroya-Milshtein N, Cardona F, Hedderly T, Heyman I, Huyser C, Mir P, Morer A, Mueller N, Munchau A, Plessen KJ, Porcelli C, Roessner V, Walitza S, Schrag A, Martino D; PGC TS Working Group; TSAICG; TSGeneSEE Initiative; EMTICS Collaborative Group; TS-EUROTRAIN Network; TIC Genetics Collaborative Group, Tischfield JA, Heiman GA, Willsey AJ, Dietrich A, Davis LK, Crowley JJ, Mathews CA, Scharf JM, Georgitsi M, Hoekstra PJ, Paschou P. Genome-wide Association Study Points to Novel Locus for Gilles de la Tourette Syndrome. Biol Psychiatry. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 8. | McGuire JF, Sturm A, Ricketts EJ, Montalbano GE, Chang S, Loo SK, Woods DW, McCracken J, Piacentini J. Cognitive control processes in behavior therapy for youth with Tourette's disorder. J Child Psychol Psychiatry. 2022;63:296-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 9. | Friedrich J, Rawish T, Bluschke A, Frings C, Beste C, Münchau A. Cognitive and Neural Mechanisms of Behavior Therapy for Tics: A Perception-Action Integration Approach. Biomedicines. 2023;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 10. | Kim KM, Bae E, Lee J, Park TW, Lim MH. A Review of Cognitive and Behavioral Interventions for Tic Disorder. Soa Chongsonyon Chongsin Uihak. 2021;32:51-62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Morand-Beaulieu S, O'Connor KP, Blanchet PJ, Lavoie ME. Electrophysiological predictors of cognitive-behavioral therapy outcome in tic disorders. J Psychiatr Res. 2018;105:113-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Nissen JB, Kaergaard M, Laursen L, Parner E, Thomsen PH. Combined habit reversal training and exposure response prevention in a group setting compared to individual training: a randomized controlled clinical trial. Eur Child Adolesc Psychiatry. 2019;28:57-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 13. | Andrén P, Jakubovski E, Murphy TL, Woitecki K, Tarnok Z, Zimmerman-Brenner S, van de Griendt J, Debes NM, Viefhaus P, Robinson S, Roessner V, Ganos C, Szejko N, Müller-Vahl KR, Cath D, Hartmann A, Verdellen C. European clinical guidelines for Tourette syndrome and other tic disorders-version 2.0. Part II: psychological interventions. Eur Child Adolesc Psychiatry. 2022;31:403-423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 93] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 14. | Yu L, Li Y, Zhang J, Yan C, Wen F, Yan J, Wang F, Liu J, Cui Y. The therapeutic effect of habit reversal training for Tourette syndrome: a meta-analysis of randomized control trials. Expert Rev Neurother. 2020;20:1189-1196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | Li Y, Yan J, Cui L, Chu J, Wang X, Huang X, Li Y, Cui Y. Protocol of a randomized controlled trial to investigate the efficacy and neural correlates of mindfulness-based habit reversal training in children with Tourette syndrome. Front Psychiatry. 2022;13:938103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 16. | Martino D, Hedderly T. Tics and stereotypies: A comparative clinical review. Parkinsonism Relat Disord. 2019;59:117-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 17. | Seragni G, Chiappedi M, Bettinardi B, Zibordi F, Colombo T, Reina C, Angelini L. Habit reversal training in children and adolescents with chronic tic disorders: an Italian randomized, single-blind pilot study. Minerva Pediatr. 2018;70:5-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Park SC, Kim YK. Anxiety Disorders in the DSM-5: Changes, Controversies, and Future Directions. Adv Exp Med Biol. 2020;1191:187-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 19. | Fu Y, Wu J, Zhao B, Lai C, Xue E, Wang D, Wang M, Tang L, Shao J. Development of a Chinese version of the Stress Adaption Scale and the assessment of its reliability and validity among Chinese patients with multimorbidity. Zhejiang Da Xue Xue Bao Yi Xue Ban. 2023;52:361-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 20. | Wen F, Gu Y, Yan J, Liu J, Wang F, Yu L, Li Y, Cui Y. Revisiting the structure of the Yale Global Tic Severity Scale (YGTSS) in a sample of Chinese children with tic disorders. BMC Psychiatry. 2021;21:394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 21. | Liao Z, Ding L, You C, Chen Y, Zhang W. The Chinese version of the family accommodation scale for obsessive-compulsive disorder self-rated: reliability, validity, factor structure, and mediating effect. Front Psychiatry. 2022;13:970747. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 22. | Qiao Y, He S, Su L, Zhu JZ, Sheng JH, Li HF. Applicability of the Chinese version of the Personal and Social Performance scale in patients with severe mental disorders. Asia Pac Psychiatry. 2017;9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Dijkstra JM, Nagatsu T. Cognitive behavioral therapy (CBT), acceptance and commitment therapy (ACT), and Morita therapy (MT); comparison of three established psychotherapies and possible common neural mechanisms of psychotherapies. J Neural Transm (Vienna). 2022;129:805-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 24. | Apolinário-Hagen J, Drüge M, Fritsche L. Cognitive Behavioral Therapy, Mindfulness-Based Cognitive Therapy and Acceptance Commitment Therapy for Anxiety Disorders: Integrating Traditional with Digital Treatment Approaches. Adv Exp Med Biol. 2020;1191:291-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 25. | Heyne D. Practitioner Review: Signposts for Enhancing Cognitive-Behavioral Therapy for School Refusal in Adolescence. Z Kinder Jugendpsychiatr Psychother. 2023;51:61-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 26. | Lee SH, Cho SJ. Cognitive Behavioral Therapy and Mindfulness-Based Cognitive Therapy for Depressive Disorders. Adv Exp Med Biol. 2021;1305:295-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 27. | Billnitzer A, Jankovic J. Current Management of Tics and Tourette Syndrome: Behavioral, Pharmacologic, and Surgical Treatments. Neurotherapeutics. 2020;17:1681-1693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 71] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 28. | Gong H, Du X, Su A, Du Y. Pharmacological treatment of Tourette's syndrome: from the past to the future. Neurol Sci. 2024;45:941-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 29. | Rozenman M, Johnson OE, Chang SW, Woods DW, Walkup JT, Wilhelm S, Peterson A, Scahill L, Piacentini J. Relationships between Premonitory Urge and Anxiety in Youth with Chronic Tic Disorders. Child Health Care. 2015;44:235-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 30. | Morand-Beaulieu S, O'Connor KP, Richard M, Sauvé G, Leclerc JB, Blanchet PJ, Lavoie ME. The Impact of a Cognitive-Behavioral Therapy on Event-Related Potentials in Patients with Tic Disorders or Body-Focused Repetitive Behaviors. Front Psychiatry. 2016;7:81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 31. | Morand-Beaulieu S, O'Connor KP, Sauvé G, Blanchet PJ, Lavoie ME. Cognitive-behavioral therapy induces sensorimotor and specific electrocortical changes in chronic tic and Tourette's disorder. Neuropsychologia. 2015;79:310-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 32. | O'Connor KP, Laverdure A, Taillon A, Stip E, Borgeat F, Lavoie M. Cognitive behavioral management of Tourette's syndrome and chronic tic disorder in medicated and unmedicated samples. Behav Res Ther. 2009;47:1090-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 33. | Scahill L, Woods DW, Himle MB, Peterson AL, Wilhelm S, Piacentini JC, McNaught K, Walkup JT, Mink JW. Current controversies on the role of behavior therapy in Tourette syndrome. Mov Disord. 2013;28:1179-1183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 34. | Shitova AD, Zharikova TS, Kovaleva ON, Luchina AM, Aktemirov AS, Olsufieva AV, Sinelnikov MY, Pontes-Silva A, Zharikov YO. Tourette syndrome and obsessive-compulsive disorder: A comprehensive review of structural alterations and neurological mechanisms. Behav Brain Res. 2023;453:114606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/