Published online Jul 19, 2024. doi: 10.5498/wjp.v14.i7.1043
Revised: May 14, 2024
Accepted: June 17, 2024
Published online: July 19, 2024
Processing time: 92 Days and 19.2 Hours
Traumatic brain injury (TBI) imposes a substantial societal and familial burden due to its high disability and fatality rates, rendering it a serious public health problem. Some patients with TBI have poor treatment outcomes and are prone to postoperative delirium (POD), which affects their quality of life. Anxiety has been linked to increased POD incidence in some studies, while others have found no correlation.
To investigate the correlation of POD risk factors, preoperative inflammatory factors, and mood disorders in patients with TBI.
We retrospectively collected data on the treatment of 80 patients with TBI from November 2021 to September 2023. Patients were grouped as POD and non-POD, according to their POD status, and the general data of the two groups were compared. Inflammatory factor levels were detected preoperatively, and the Hamilton Depression Scale (HAMD) and Hamilton Anxiety Scale (HAMA) were used to investigate the risk factors associated with POD in these patients. Logistic regression was used to identify the independent risk factors.
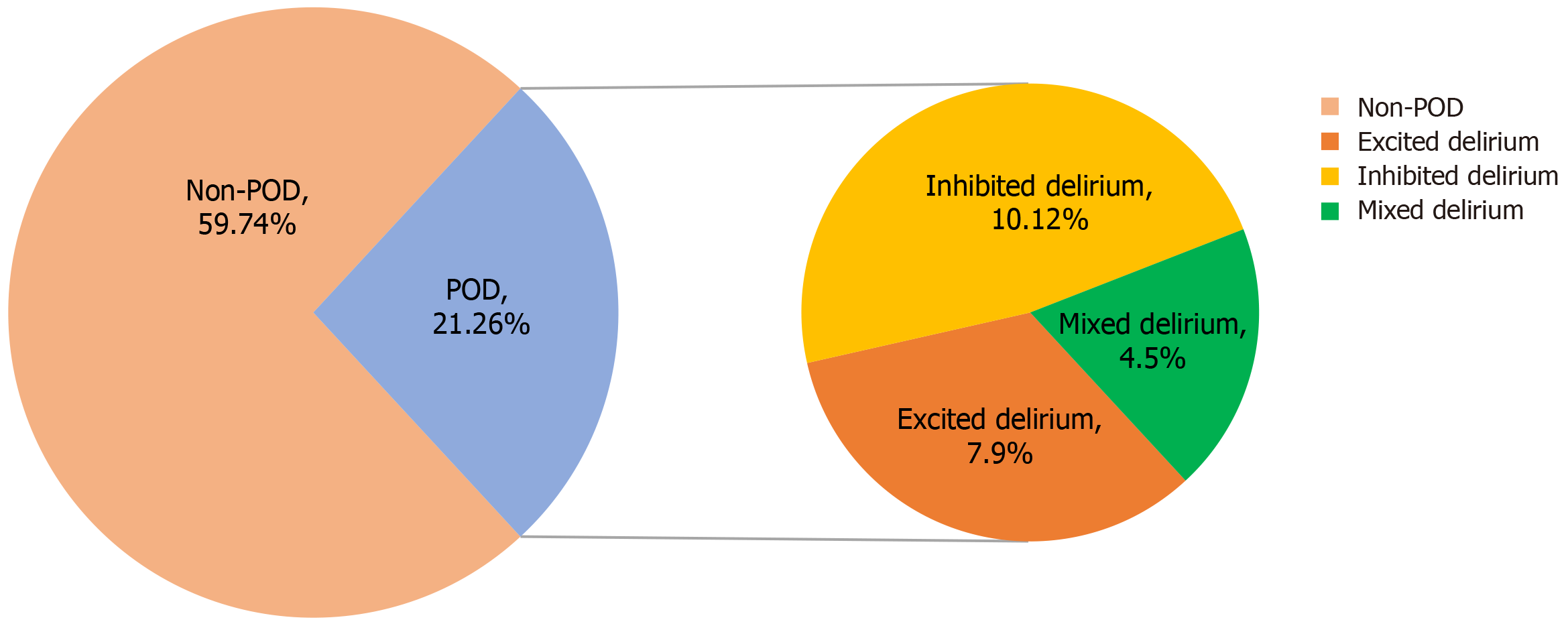
Twenty-one patients (26.25%) developed POD, including 7, 10, and 4 cases of the excitatory, inhibitory, and mixed types, respectively. There were 59 cases (73.75%) in the non-POD group. Compared with the non-POD group, the POD group had a significantly higher proportion of patients with low Glasgow Coma Scale (GCS) scores before admission, unilateral mydriasis, preoperative hemorrhagic shock, intraventricular hemorrhage (IVH), and postoperative hyperglycemic hyperosmolar disease (P < 0.05). In the POD group, interleukin-6 (IL-6), human tumor necrosis factor-α (TNF-α), myeloperoxidase levels, HAMA, and HAMD scores were higher than those in the non-POD group (all P < 0.05). Logistic multivariate analysis showed that GCS score at admission, IVH, IL-6, TNF-α, HAMA, and HAMD were independent risk factors for POD in patients with TBI (P < 0.05).
Low GCS score at admission, IVH, elevated IL-6 and TNF-α, other inflammatory indicators, anxiety, and depression, can increase the risk of POD in patients with TBI after surgery.
Core Tip: Traumatic brain injury (TBI) is a common form of trauma caused by external violence, resulting in head and brain injuries. TBI ranks second only to limb injuries in all body regions. It is a complex and severe injury with high disability and mortality rates, often manifesting symptoms such as disturbed consciousness, neurological dysfunction, and increased intracranial pressure, posing significant risks to patient safety. This study examines the risk factors for postoperative delirium (POD) in patients with TBI, aiming to enable early intervention and reduce POD occurrence.
- Citation: Cao P, Jia ZY, Zheng T, Mei T. Correlation of preoperative inflammatory factors and emotional disorders with postoperative delirium in patients with craniocerebral trauma. World J Psychiatry 2024; 14(7): 1043-1052
- URL: https://www.wjgnet.com/2220-3206/full/v14/i7/1043.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i7.1043
Traumatic brain injury (TBI), the most prevalent critical neurological condition, has a high mortality and disability rate, imposing significant burdens on society and families and posing substantial challenges to medical and health management[1]. Postoperative delirium (POD) is a common complication of TBI, characterized by fluctuations in consciousness, inattention, and confusion. POD usually occurs 2-5 days after surgery[2]. POD has a high incidence in patients with TBI, leading to long-term cognitive dysfunction, increased mortality risk, and significant impacts on patient prognosis[3]. Currently, there is no specific drug for treating POD, emphasizing the importance of early identification of high-risk patients. The etiology of POD includes various mechanisms, such as neuroinflammation, neurotransmitter imbalance, changes in biological rhythm, and changes in brain metabolism. Many studies have shown the crucial role of neuroinflammation in the onset and progression of POD[4-6]. In addition, psychiatric symptoms closely reflect the metabolism and function of the nervous system, serving as reliable indicators of POD onset and progression. Previous reports have indicated a significant association between anxiety and increased POD incidence, although some studies failed to establish a correlation between the two[7,8]. Therefore, this study examined the associated risk factors for POD in patients with TBI and investigated the correlation between preoperative inflammatory factors, emotional disorders, and POD in this population to provide a reference for the pathological mechanism and clinical treatment of patients with TBI.
Eighty patients with TBI treated at Changde Hospital, Xiangya School of Medicine, Central South University (The First People’s Hospital of Changde City) between November 2021 and September 2023 were included in the study.
Inclusion criteria included: Age > 18 years, a definite history of trauma, and trauma onset within 24 hours before admission.
Exclusion criteria were: Severe injury to other organs; the presence of hematological diseases, cancer, severe infections, autoimmune diseases, liver and kidney dysfunction; poor heart, lung, liver, and kidney function; inability to tolerate surgery or coagulation insufficiency caused by long-term use of antiplatelet or anticoagulant drugs; and death within 3 days after admission.
A postadmission computed tomography scan was required to confirm traumatic intracranial hematoma in all patients.
The patients were assessed by a trained physician using the confusion assessment method, which involves evaluating the following: (1) Acute changes in mental status; (2) Inattention; (3) Disorganized thinking; and (4) Change in consciousness level. Delirium is diagnosed if any one of the following conditions is met: (1) and (2), plus (3), or (4)[9]. Delirium can manifest in three types: Excited type: Increased activity, decreased ability to control activity, restlessness, and wandering; Inhibitory type: Decreased activity, slowed-down behavior, decreased ability for environmental recognition, reduced language quantity and speed, fatigue, and decreased arousal or autism; Mixed type: Alternating episodes of excitation and inhibition.
Assessments began on the first day after the completion of surgery and were performed once daily until the patient's discharge or death.
On the morning after admission, 10 mL of fasting venous blood was collected from each patient after an 8-hour fasting period and placed in a sodium citrate anticoagulant blood collection tube. After 15 min of centrifugation in a 3000 r/min centrifuge, the supernatant was collected and stored at -20 °C until testing. Interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α) levels in the samples were measured by a radioimmunoassay (ELISA kit), while serum myeloperoxidase (MPO) levels were measured using an ultraviolet spectrophotometer.
The Hamilton Depression Scale (HAMD, 17 items) was used to evaluate depression status and severity in patients with TBI before surgery. Scores on the scale range from 0-34 points, with a HAMD score ≥ 7 indicating depression[10]. Similarly, the Hamilton Anxiety Scale (HAMA, 14 items) was used to evaluate anxiety levels in patients with TBI. Scores on this scale range from 0-56 points, with a HAMA score ≥ 7 indicating anxiety[11].
Surgical procedures were performed based on the location and volume of the hematoma. This involved making a surgical incision, cutting through the scalp and muscles layer-by-layer, drilling a hole, milling the skull to remove the epidural hematoma, cutting the dura to remove the subdural hematoma, and extracting the intracerebral hematoma under a microscope. During surgery, the decision to remove the bone flap was made by the two doctors based on consensus and the swelling of the brain tissue. For patients treated with decompressive craniectomy, a dural tension-relieving suture was placed, a drainage tube was inserted, and the muscle scalp was sutured layer-by-layer. Postoperative care included analgesia, sedation, fluid infusion, intensive care, anti-infection therapy, and rehabilitation.
(1) General Information: Age, sex, body mass index (BMI), time from trauma to admission, Glasgow Coma Scale (GCS) score on admission, intracranial pressure on admission, pupil change, preoperative hemorrhagic shock, hematoma volume, midline shift, preoperative drilling and drainage, ventricular hemorrhage, basal cisterna compression, posto
SPSS 27.0 was used to analyze the data of the study patients. The measurement data were expressed as mean ± SD, and comparisons between the two groups were performed using independent sample t-tests. The rate of count data was expressed as percentages, and the chi-squared test was used for comparisons between groups. P < 0.05 was considered statistically significant. Logistic regression analysis was used to analyze the correlation between the study variables, with OR and 95%CI used to evaluate risk factors.
Among the 80 patients, 63 were male and 17 were female. Their ages ranged from 26 to 71 years, with a mean of 48.56 ± 8.62 years. A total of 21 patients (26.25%) developed POD, including seven cases of excitatory type, 10 cases of inhibitory type, and four cases of mixed type, while 59 cases (73.75%) were non-POD (Figure 1).
The proportion of patients with lower GCS scores before admission, unilateral mydriasis, preoperative hemorrhagic shock, intraventricular hemorrhage (IVH), postoperative hyperglycemia, and hyperosmolarity was higher in the POD group compared to the non-POD group (P < 0.05). Age, sex, BMI, time from trauma to admission, intracranial pressure on admission, pupil changes, hematoma volume, midline shift, and preoperative factors such as drilling and drainage and compression ring pool differences were not significant between the two groups (P > 0.05; Table 1).
| Index | POD group (n = 21) | Non-POD group (n = 59) | χ2/t | P value |
| Age (year) | 50.48 ± 8.53 | 47.88 ± 8.62 | 1.188 | 0.239 |
| Sex | 0.111 | 0.738 | ||
| Male | 16 (76.19) | 47 (79.66) | ||
| Female | 5 (23.81) | 12 (20.34) | ||
| BMI (kg/m2) | 22.08 ± 2.23 | 22.50 ± 2.76 | 0.631 | 0.530 |
| Time from trauma to admission (minutes) | 85.10 ± 15.51 | 83.39 ± 12.13 | 0.513 | 0.609 |
| Admission GCS score (score) | 7.770 | 0.005 | ||
| ≤ 3 | 10 (47.62) | 10 (16.95) | ||
| > 3 | 11 (52.38) | 49 (83.05) | ||
| Intracranial pressure at admission (mmHg) | 52.95 ± 10.73 | 49.85 ± 10.73 | 1.139 | 0.258 |
| Pupil changes | 4.195 | 0.041 | ||
| Single side scattered | 7 (33.33) | 35 (59.32) | ||
| Bilateral scattered | 14 (66.67) | 24 (40.68) | ||
| Prehemorrhagic shock | 6.792 | 0.009 | ||
| Yes | 11 (52.38) | 13 (22.03) | ||
| No | 10 (47.62) | 46 (77.97) | ||
| Hematoma volume (mL) | 55.95 ± 12.36 | 53.49 ± 11.55 | 0.823 | 0.413 |
| Midline shift | 1.566 | 0.211 | ||
| < 10 mm | 7 (33.33) | 29 (49.15) | ||
| ≥ 10 mm | 14 (66.67) | 30 (50.85) | ||
| Preoperative drilling and drainage | 0.007 | 0.934 | ||
| Yes | 18 (85.71) | 52 (88.14) | ||
| No | 3 (14.29) | 7 (11.86) | ||
| Ventricular hemorrhage | 3.975 | 0.046 | ||
| Yes | 7 (33.33) | 8 (13.56) | ||
| No | 14 (66.67) | 51 (86.44) | ||
| Compressed ring pool | 0.132 | 0.717 | ||
| Compressed unilateral ring pool | 9 (42.86) | 28 (47.46) | ||
| Compressed bilateral ring pool | 12 (57.14) | 31 (52.54) | ||
| Postoperative high glucose hyperpermeability | 8.366 | 0.004 | ||
| Yes | 8 (38.10) | 6 (10.17) | ||
| No | 13 (61.90) | 53 (89.83) |
The IL-6 score was 21.62 ± 5.68, the TNF-α score was 65.71 ± 14.19, and the MPO score was 132.24 ± 17.01 in the POD group. IL-6, TNF-α, and MPO levels were higher in the POD group compared to the non-POD group (χ2 = 4.105, 2.948, and 3.640, respectively, P < 0.05; Table 2).
| Index | POD group (n = 21) | non-POD group (n = 59) | t value | P value |
| IL-6 | 21.62 ± 5.68 | 16.78 ± 4.22 | 4.105 | < 0.05 |
| TNF-α | 65.71 ± 14.19 | 56.19 ± 12.18 | 2.948 | 0.004 |
| MPO | 132.24 ± 17.01 | 115.19 ± 18.09 | 3.640 | < 0.05 |
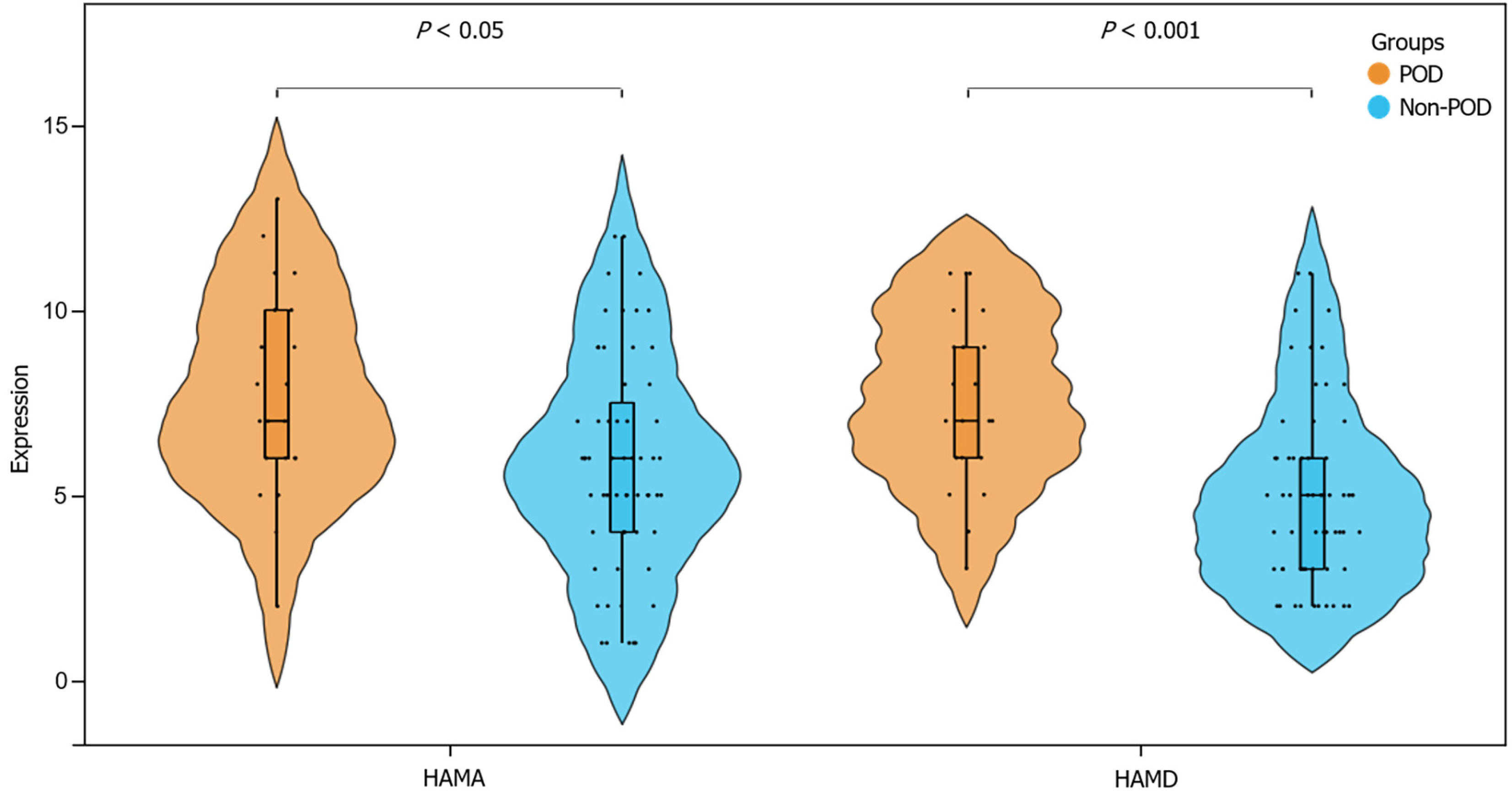
In the POD group, the HAMA score was 7.71 ± 2.80, and the HAMD score was 7.57 ± 2.34. Twelve patients (57.14%) had a HAMA score of 7, and 14 patients (66.67%) had a HAMD score of 7. In comparison, the HAMA score for the non-POD group was 5.86 ± 2.91, and the HAMD score was 4.98 ± 2.46. Twenty-one patients (35.59%) had a HAMA score of 7, and 13 patients had a HAMD score of 7. Compared to the non-POD group, the POD group had higher preoperative anxiety and depression (P < 0.05; Figure 2).
The relevant univariate variables were included in the multivariate logistic regression analysis, and the variable assignments are presented in Table 3. The optimal cutoff values of IL-6, TNF-α, and MPO were determined to be 17.5, 64.5, and 132.5, respectively. The results indicated that admission GCS score, IVH, IL-6, TNF-α, HAMA, and HAMD were identified as risk factors for POD in patients with TBI (P < 0.05; Table 4).
| Index | Assignment |
| POD circumstances | 1 = POD, 0 = non-POD |
| Admission GCS score | 1 = ≤ 3, 0 = > 3 |
| Pupil changes | 1 = Bilateral scattered, 0 = Single side scattered |
| Prehemorrhagic shock | 1 = yes, 0 = no |
| Ventricular hemorrhage | 1 = yes, 0 = no |
| Postoperative high glucose hyperpermeability | 1 = yes, 0 = no |
| IL-6 | 1 = ≥17.5, 0 = < 17.5 |
| TNF-α | 1 = ≥ 64.5, 0 = < 64.5 |
| MPO | 1 = ≥ 132.5, 0 = < 132.5 |
| HAMA | 1 = ≥ 7, 0 = < 7 |
| HAMD | 1 = ≥ 7, 0 = < 7 |
| Index | B | SE | Wald χ2 | P value | OR | 95%CI |
| Admission GCS score | 2.232 | 1.058 | 4.453 | 0.035 | 9.321 | 1.172-74.105 |
| Pupil changes | 1.060 | 0.955 | 1.230 | 0.267 | 2.886 | 0.444-18.770 |
| Prehemorrhagic shock | 1.365 | 1.109 | 1.516 | 0.218 | 3.918 | 0.446-34.444 |
| Ventricular hemorrhage | 2.878 | 1.151 | 6.249 | 0.012 | 17.777 | 1.862-169.742 |
| Postoperative high glucose hyperpermeability | 1.123 | 1.366 | 0.676 | 0.411 | 3.075 | 0.211-44.755 |
| IL-6 | 2.538 | 1.104 | 5.291 | 0.021 | 12.659 | 1.456-110.082 |
| TNF-α | 2.344 | 1.062 | 4.867 | 0.027 | 10.421 | 1.299-83.616 |
| MPO | 0.713 | 1.108 | 0.414 | 0.520 | 2.039 | 0.233-17.887 |
| HAMA | 2.127 | 1.020 | 4.349 | 0.037 | 8.394 | 1.137-61.993 |
| HAMD | 2.421 | 1.081 | 5.011 | 0.025 | 11.256 | 1.352-93.735 |
As economic and transportation infrastructures develop rapidly, the incidence of TBI is increasing annually. TBI is characterized by severe conditions, rapid progression, and high disability and mortality rates, presenting significant challenges to neurologists[12]. Therefore, it is necessary to explore the prognostic factors affecting patients with TBI.
Relevant studies have highlighted that patients with TBI are prone to POD, which not only causes neurological impairment but also increases the risk of other complications, prolongs the length of hospital stay, and leads to adverse outcomes such as permanent cognitive impairment and death[13,14]. Reports indicate an overall incidence of POD of 23%, consistent with the 26.25% incidence observed in patients with TBI in our study and similar to previous studies[15,16]. Recent studies have shown that POD is caused by dysregulation of basal neuronal activity secondary to systemic disorders and is mainly associated with neuroinflammation[17]. Therefore, focusing on inflammatory factors and responses can help elucidate the risk factors associated with POD in patients with TBI, thereby promoting TBI treatment and improving patient prognosis.
This study’s results showed that the proportion of patients with a low GCS score before admission, bilateral pupillary dilation, preoperative hemorrhagic shock, IVH, postoperative hyperglycemia, and hyperosmolarity was higher in the POD group compared to the non-POD group.
The GCS is the basic tool used to assess consciousness alterations in patients with TBI, with a score of 3-5 points indicating severe TBI. Patients with severe TBI experience rapid disease progression, severe secondary brain injury, significant treatment difficulty, high mortality rates, and severe disability rates, leading to traditionally low expectations for their treatment outcomes. This affects the patient’s family and even impacts the confidence of neurosurgeons[18,19].
During the progression of TBI, changes in the patient’s pupil are often indicative of the evolving condition. In healthy individuals, the pupil is symmetrical, round, centered, and possesses a smooth edge, with a diameter of approximately 2.5 mm-4.0 mm under diffuse natural light.
Mydriasis occurs when the iris dilator muscle contracts, causing the pupil to dilate beyond 5 mm in diameter. Bilateral mydriasis indicates bilateral nerve damage, which is a serious consequence of increased intracranial pressure resulting from various diseases, such as cerebrovascular disease and encephalitis, leading to poor patient prognosis[20,21].
Patients with TBI are prone to developing hemorrhagic shock. During this state, tissue perfusion decreases, leading to cellular anaerobic metabolism, elevated lactic acid levels, and metabolic acidosis. If left untreated, this condition can lead to organ failure or even death[22]. Some studies have pointed out that massive parenchymal hemorrhage or intracranial hematoma may compress the ventricular system, leading to IVH[23]. IVH is a type of large-scale intracerebral hemo
Patients with craniocerebral trauma often experience blood glucose elevation, peaking approximately 12-24 hours after injury and manifesting as a hyperglycemic hyperosmolar state. The primary mechanisms behind this phenomenon include nerve stimulation, damage to hormone-secreting structures such as the hypothalamus and pituitary gland, and the body's stress response, resulting in increased secretion of glucagon, catecholamines, and glucocorticoids. Simultaneously, hyperglycemia and hyperosmicity can aggravate nerve damage through lactic acidosis, electrolyte imbalances, and hyperosmolar coma, leading to a poor patient prognosis[25].
In the multivariate analysis of this study, GCS scores at admission and IVH were identified as risk factors for POD in patients with TBI. Conversely, the P values of bilateral pupil dilation, preoperative hemorrhagic shock, postoperative hyperglycemia, and hyperosmolarity were greater than 0.05, which were largely related to insufficient sample size or sampling bias.
The neuroinflammation theory states that inflammatory mediators can compromise the blood-brain barrier, infiltrate the central nervous system, and prompt microglia to produce inflammatory factors that induce central neuronal and synaptic damage, eventually leading to neuroinflammation and POD. This study found that, compared with the non-POD group, the POD group exhibited higher preoperative levels of IL-6, TNF-α, and MPO. Furthermore, the multivariate analysis showed that IL-6 and TNF-α were the influencing factors of POD in patients with TBI.
IL-6 is an important cytokine that promotes the production of C-reactive protein and fibrinogen, playing a key role in inflammatory responses. It is produced in response to infection or inflammation, leading to a rapid elevation in IL-6 Levels in a short time, peaking within 2 hour. This increase is consistent with the severity of inflammation[26,27]. Monocyte macrophages produce TNF-α, which is expressed only in small amounts in the brain tissue of healthy individuals. While moderate expression of TNF-α has a defensive effect, excessive expression may cause neurotoxicity. Studies have shown that TNF-α levels increase significantly during trauma and inflammatory response, followed by swelling and even necrosis of nerve cells in patients[28,29]. MPO is a functional activation marker of neutrophils and plays a role in the production and regulation of inflammatory responses in the body. Neutrophil infiltration is one of the main factors in the inflammatory response in patients with craniocerebral injuries. In states of inflammation and oxidative stress, MPO catalyzes reactions that generate excessive oxidants to protect the body. However, when the body's antioxidant defense range is exceeded, oxidative stress and tissue damage occurs, aggravating disease progression[30]. IL-6 and TNF-α, much like MPO, exhibit the capacity to promote the secretion of trophic factors by human glial cells to a certain extent, thereby promoting the repair of nerve tissue. However, overactivation of these factors induces chemokine release, triggering local inflammatory cascade burst reactions[31]. Therefore, monitoring these inflammatory factors can effectively evaluate the degree of the inflammatory response in patients.
Studies have found that compared with patients without depression, those with depression are nearly 1.3-9 times more likely to develop delirium, and a history of depression and the presence of subclinical depression levels are both high-risk factors for POD[32]. This study also found that the HAMA and HAMD scores and the proportion of patients with anxiety and depression in the POD group were higher than those in the Non-POD group, which is consistent with the results of the previously mentioned studies[32]. Multivariate analysis demonstrated that HAMA and HAMD scores were risk factors for POD in patients with TBI. Previous studies have also identified a correlation between depression and POD. On the one hand, depression has a certain predictive effect on POD. Depressed patients often show symptoms such as low mood, loss of interest, and sleep disorders, which may further affect their mental state and cognitive function, and increase the risk of POD. On the other hand, some epidemiological studies have included delirium as a risk factor for postoperative depression[33,34]. Thus, both may have similar pathophysiological mechanisms. Functional imbalances of dopaminergic and cholinergic neurotransmitters involved in delirium, abnormal stress, and the inflammatory response of the hypothalamic-pituitary-adrenocortical axis are also considered to be related to depression[35]. Recent studies have suggested that anxiety and delirium are associated with inflammatory cytokines. Therefore, anxiety is proposed as a new predictor of POD[36]. After migration, peripheral inflammatory cytokines interact with microglia, causing an inflammatory response and the onset of delirium. However, excessive anxiety can lead to tachycardia, hypertension, and arrhythmia, which in turn induce inflammatory responses. In addition, it has been reported that preoperative anxiety can lead to short- and long-term adverse consequences after surgery, such as complications, psychological distress, increased need for analgesics and anesthetics, and decreased quality of life and cognitive ability, which are not conducive to patient recovery[37]. Therefore, preoperative intervention and treatment of patients with emotional disorders can help to improve their psychological state, reduce the strees response to the surgery and the incidence of POD, and improve their experience during the surgical procedure and postoperative recovery. Previous studies have shown that preoperative treatment of emotional disorders can improve the psychological resilience of the patients and reduce their stress response, allowing them to cope better with the stress and challenges that having surgery entail, and improving their prognosis[38].
This study analyzed the risk factors related to POD in patients with TBI. We explored the correlation between preoperative inflammatory factors, emotional disorders, and POD in patients with TBI with the aim of reducing the risk of POD. The results showed that GCS score at admission, IVH, IL-6, TNF-α, HAMA, and HAMD were risk factors for POD in patients with TBI. Clinicians can observe the occurrence of these indicators and implement early interventions for high-risk patients, thereby improving their prognosis.
| 1. | Wang KK, Yang Z, Zhu T, Shi Y, Rubenstein R, Tyndall JA, Manley GT. An update on diagnostic and prognostic biomarkers for traumatic brain injury. Expert Rev Mol Diagn. 2018;18:165-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 384] [Article Influence: 48.0] [Reference Citation Analysis (0)] |
| 2. | Jin Z, Hu J, Ma D. Postoperative delirium: perioperative assessment, risk reduction, and management. Br J Anaesth. 2020;125:492-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 463] [Article Influence: 77.2] [Reference Citation Analysis (0)] |
| 3. | Meco M, Giustiniano E, Cecconi M, Albano G. Pharmacological prevention of postoperative delirium in patients undergoing cardiac surgery: a bayesian network meta-analysis. J Anesth. 2023;37:294-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Greaves D, Psaltis PJ, Davis DHJ, Ross TJ, Ghezzi ES, Lampit A, Smith AE, Keage HAD. Risk Factors for Delirium and Cognitive Decline Following Coronary Artery Bypass Grafting Surgery: A Systematic Review and Meta-Analysis. J Am Heart Assoc. 2020;9:e017275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 111] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 5. | Taylor J, Parker M, Casey CP, Tanabe S, Kunkel D, Rivera C, Zetterberg H, Blennow K, Pearce RA, Lennertz RC, Sanders RD. Postoperative delirium and changes in the blood-brain barrier, neuroinflammation, and cerebrospinal fluid lactate: a prospective cohort study. Br J Anaesth. 2022;129:219-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 151] [Article Influence: 37.8] [Reference Citation Analysis (2)] |
| 6. | Subramaniyan S, Terrando N. Neuroinflammation and Perioperative Neurocognitive Disorders. Anesth Analg. 2019;128:781-788. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 122] [Cited by in RCA: 314] [Article Influence: 44.9] [Reference Citation Analysis (0)] |
| 7. | Zainal Abidin H, Omar SC, Mazlan MZ, Hassan MH, Isa R, Ali S, Hassan SK, Marzuki A. Postoperative Maladaptive Behavior, Preoperative Anxiety and Emergence Delirium in Children Undergone General Anesthesia: A Narrative Review. Glob Pediatr Health. 2021;8:2333794X211007975. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Freedman Z, Hudock N, Hallan DR, Kelleher J. Anxiety as a Risk Factor for Postoperative Delirium in Elective Spine Deformity Surgeries: A National Database Study. Cureus. 2022;14:e28984. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Gusmao-Flores D, Salluh JI, Chalhub RÁ, Quarantini LC. The confusion assessment method for the intensive care unit (CAM-ICU) and intensive care delirium screening checklist (ICDSC) for the diagnosis of delirium: a systematic review and meta-analysis of clinical studies. Crit Care. 2012;16:R115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 418] [Cited by in RCA: 400] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 10. | Zimmerman M, Martinez JH, Young D, Chelminski I, Dalrymple K. Severity classification on the Hamilton Depression Rating Scale. J Affect Disord. 2013;150:384-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 553] [Cited by in RCA: 878] [Article Influence: 67.5] [Reference Citation Analysis (0)] |
| 11. | Thompson E. Hamilton Rating Scale for Anxiety (HAM-A). Occup Med (Lond). 2015;65:601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 332] [Article Influence: 33.2] [Reference Citation Analysis (0)] |
| 12. | Khellaf A, Khan DZ, Helmy A. Recent advances in traumatic brain injury. J Neurol. 2019;266:2878-2889. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 210] [Cited by in RCA: 312] [Article Influence: 44.6] [Reference Citation Analysis (0)] |
| 13. | Chaiwat O, Chanidnuan M, Pancharoen W, Vijitmala K, Danpornprasert P, Toadithep P, Thanakiattiwibun C. Postoperative delirium in critically ill surgical patients: incidence, risk factors, and predictive scores. BMC Anesthesiol. 2019;19:39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 94] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 14. | Zhou J, Xu X, Liang Y, Zhang X, Tu H, Chu H. Risk factors of postoperative delirium after liver transplantation: a systematic review and meta-analysis. Minerva Anestesiol. 2021;87:684-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | Yang Z, Wang XF, Yang LF, Fang C, Gu XK, Guo HW. Prevalence and risk factors for postoperative delirium in patients with colorectal carcinoma: a systematic review and meta-analysis. Int J Colorectal Dis. 2020;35:547-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 16. | Wu J, Yin Y, Jin M, Li B. The risk factors for postoperative delirium in adult patients after hip fracture surgery: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2021;36:3-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 114] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 17. | Zhou S, Deng F, Zhang J, Chen G. Incidence and risk factors for postoperative delirium after liver transplantation: a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci. 2021;25:3246-3253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 18. | Sheff ZT, Engbrecht BW, Rodgers R, Jacobson LE, Smith JL. Mortality of adolescents with isolated traumatic brain injury does not vary with type of level I trauma center. J Trauma Acute Care Surg. 2022;93:538-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 19. | Heydari F, Azizkhani R, Ahmadi O, Majidinejad S, Nasr-Esfahani M, Ahmadi A. Physiologic Scoring Systems versus Glasgow Coma Scale in Predicting In-Hospital Mortality of Trauma Patients; a Diagnostic Accuracy Study. Arch Acad Emerg Med. 2021;9:e64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 20. | Yang E, Kreuzer M, Hesse S, Davari P, Lee SC, García PS. Infrared pupillometry helps to detect and predict delirium in the post-anesthesia care unit. J Clin Monit Comput. 2018;32:359-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Tian R, Dong J, Liu W, Zhang J, Han F, Zhang B, Xu X, Niu F, Liu B. Prognostic Analysis of Emergency Decompressive Craniectomy for Patients with Severe Traumatic Brain Injury with Bilateral Fixed Dilated Pupils. World Neurosurg. 2021;146:e1307-e1317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Matsuyama S, Miki R, Kittaka H, Nakayama H, Kikuta S, Ishihara S, Nakayama S. Preoperative fluid restriction for trauma patients with hemorrhagic shock decreases ventilator days. Acute Med Surg. 2018;5:154-159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Guest M. Assessing and managing post-operative haemorrhage and haemorrhagic shock. Nurs Stand. 2021;36:77-82. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 24. | Panholzer B, Pilarczyk K, Huenges K, Aldinger C, Friedrich C, Nowak-Göttl U, Cremer J, Haneya A. Severe Pulmonary Bleeding after Assist Device Implantation: Incidence, Risk Factors and Prognostic Impact. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 25. | Matovu P, Kirya M, Galukande M, Kiryabwire J, Mukisa J, Ocen W, Lowery Wilson M, Abio A, Lule H. Hyperglycemia in severe traumatic brain injury patients and its association with thirty-day mortality: a prospective observational cohort study in Uganda. PeerJ. 2021;9:e10589. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 26. | Li Z, Xiao J, Xu X, Li W, Zhong R, Qi L, Chen J, Cui G, Wang S, Zheng Y, Qiu Y, Li S, Zhou X, Lu Y, Lyu J, Zhou B, Zhou J, Jing N, Wei B, Hu J, Wang H. M-CSF, IL-6, and TGF-β promote generation of a new subset of tissue repair macrophage for traumatic brain injury recovery. Sci Adv. 2021;7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 68] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 27. | Deng Y, Jiang X, Deng X, Chen H, Xu J, Zhang Z, Liu G, Yong Z, Yuan C, Sun X, Wang C. Pioglitazone ameliorates neuronal damage after traumatic brain injury via the PPARγ/NF-κB/IL-6 signaling pathway. Genes Dis. 2020;7:253-265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 28. | Xu W, Yue S, Wang P, Wen B, Zhang X. Systemic inflammation in traumatic brain injury predicts poor cognitive function. Immun Inflamm Dis. 2022;10:e577. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 29. | Aggarwal R, Jain AK, Mittal P, Kohli M, Jawanjal P, Rath G. Association of pro- and anti-inflammatory cytokines in preeclampsia. J Clin Lab Anal. 2019;33:e22834. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 166] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 30. | Aratani Y. Myeloperoxidase: Its role for host defense, inflammation, and neutrophil function. Arch Biochem Biophys. 2018;640:47-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 367] [Cited by in RCA: 690] [Article Influence: 86.3] [Reference Citation Analysis (0)] |
| 31. | Wang R, He M, Ou XF, Xie XQ, Kang Y. Serum Procalcitonin Level Predicts Acute Kidney Injury After Traumatic Brain Injury. World Neurosurg. 2020;141:e112-e117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 32. | Ma J, Li C, Zhang W, Zhou L, Shu S, Wang S, Wang D, Chai X. Preoperative anxiety predicted the incidence of postoperative delirium in patients undergoing total hip arthroplasty: a prospective cohort study. BMC Anesthesiol. 2021;21:48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 33. | Segernäs A, Skoog J, Ahlgren Andersson E, Almerud Österberg S, Thulesius H, Zachrisson H. Prediction of Postoperative Delirium After Cardiac Surgery with A Quick Test of Cognitive Speed, Mini-Mental State Examination and Hospital Anxiety and Depression Scale. Clin Interv Aging. 2022;17:359-368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 34. | Ren A, Zhang N, Zhu H, Zhou K, Cao Y, Liu J. Effects of Preoperative Anxiety on Postoperative Delirium in Elderly Patients Undergoing Elective Orthopedic Surgery: A Prospective Observational Cohort Study. Clin Interv Aging. 2021;16:549-557. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 35. | Stamenkovic DM, Rancic NK, Latas MB, Neskovic V, Rondovic GM, Wu JD, Cattano D. Preoperative anxiety and implications on postoperative recovery: what can we do to change our history. Minerva Anestesiol. 2018;84:1307-1317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 77] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 36. | Oteri V, Martinelli A, Crivellaro E, Gigli F. The impact of preoperative anxiety on patients undergoing brain surgery: a systematic review. Neurosurg Rev. 2021;44:3047-3057. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 37. | Falk A, Eriksson M, Stenman M. Depressive and/or anxiety scoring instruments used as screening tools for predicting postoperative delirium after cardiac surgery: A pilot study. Intensive Crit Care Nurs. 2020;59:102851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 38. | Nguyen Q, Uminski K, Hiebert BM, Tangri N, Arora RC. Midterm outcomes after postoperative delirium on cognition and mood in patients after cardiac surgery. J Thorac Cardiovasc Surg. 2018;155:660-667.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/