Published online Jun 19, 2024. doi: 10.5498/wjp.v14.i6.857
Revised: May 6, 2024
Accepted: May 8, 2024
Published online: June 19, 2024
Processing time: 112 Days and 2 Hours
The diagnosis and treatment of depression in patients with chronic heart failure (CHF) is challenging, with no ideal treatment at present.
To analyze the clinical intervention effect of Xuefu Zhuyu decoction (XFZYD) on CHF complicated with depression.
The study cohort comprised 116 patients with CHF complicated with depression who received treatment from July 2020 to July 2023, of which 55 received Western medicine (control group) and 61 received XFZYD (research group). Data on clinical effectiveness, traditional Chinese medicine (TCM) syndrome score, cardiac function, negative emotions, and serum inflammatory factors, were collected for comparative analyses.
Compared with the control group, the research group had an evidently higher total effective rate. Furthermore, there were marked reductions in TCM symptom score, left ventricular end-diastolic diameter, left ventricular end-systolic dia
Our findings conclusively proved that XFZYD was considerably superior to Western medicine for treating CHF complicated with depression because it significantly alleviated patients’ symptoms, improved cardiac function, relieved negative emotions, and reduced the levels of serum inflammatory factors.
Core Tip: Chronic heart failure (CHF) is a hemodynamic disorder that leads to systolic and diastolic dysfunction and increases the risk of diabetes and chronic kidney disease. Additionally, the risk of depression in patients with CHF can reach up to 60%, and the diagnosis and treatment of depression in this patient population is challenging because there is no ideal therapy for this comorbidity. This study comparatively analyzed the clinical effects of Xuefu Zhuyu decoction (XFZYD) vs Western medicine in patients with CHF complicated with depression from the perspectives of clinical efficacy, traditional Chinese medicine symptom score, cardiac function, negative emotions, and serum inflammatory factor levels. We found that the clinical efficacy of XFZYD was significantly higher than Western medicine for treating CHF complicated with depression and significantly reduced patients’ symptoms, improved cardiac function, alleviated negative emotions, and inhibited serum inflammatory factors. Therefore, XFZYD is highly beneficial for improving the efficacy and clinical outcomes of patients with CHF complicated with depression.
- Citation: Wang Y, Wang J, Lv W, Chen H, Yang Q, Zhang Y, Guo R, Ma XL, Zhang QY. Clinical intervention effect of Xuefu Zhuyu decoction on chronic heart failure complicated with depression. World J Psychiatry 2024; 14(6): 857-865
- URL: https://www.wjgnet.com/2220-3206/full/v14/i6/857.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i6.857
Chronic heart failure (CHF) is a cardiovascular disease with high prevalence and a high frequency of hospitalization and death. CHF symptoms include fatigue, dyspnea, fluid retention, and poor exercise tolerance[1,2]. Because CHF is a hemodynamic disorder, it may lead to systolic and diastolic dysfunction and increase the risk of diabetes and chronic kidney disease[3]. Additionally, the risk of depression in CHF can reach 60%, and it has been associated with worsening patient conditions, particularly in older adults[4,5]. The cause of depression in CHF patients may be related to factors such as limited activities of daily living and functional symptoms, like immobility[6]. The comorbidity mechanism of CHF combined with depression is related to inflammatory overreaction and abnormal cardiac autonomic control and regulation[7]. The diagnosis and treatment of depression in patients with CHF are challenging, and there is currently no ideal treatment for this comorbidity[8,9]. Thus, solving the abovementioned issues will be of great value in improving the treatment effectiveness and clinical outcomes of patients with CHF complicated with depression.
There applications of traditional Chinese medicine (TCM) therapy for patients with CHF complicated with depression are increasing. Cai et al[10] reported that the practice of Tai Chi as a Chinese medicine exercise therapy by patients with CHF complicated with depression significantly alleviated their negative emotions. According to Wang et al[11], Buxin Yiqi decoction, as a TCM therapy, effectively reduced symptoms in patients with CHF and enhanced their prognosis, with a lower risk of adverse reactions compared with Western medicine therapy. Collectively, these findings indicate the high therapeutic potential of TCM therapy for patients with CHF complicated with depression. Xuefu Zhuyu decoction (XFZYD) is a Chinese herbal medicine that was introduced in the Qing Dynasty to regulate qi and disperse stagnation. It is composed of various Chinese herbs, including Poria cocos, Paeonia lactiflora, ginger, Atractylodes macrocephala, Radix Paeoniae Rubra, peach kernel, and Fructus Aurantii[12]. This prescription is used for treating angina pectoris, exerting positive effects on symptom relief, blood lipid metabolism, and quality of life[13]. TCM classifies CHF complicated with depression in the categories of chest obstruction and stagnation syndrome, which mainly manifests as blood stasis syndrome, with etiology associated with blood stasis obstruction of the heart pulse, stagnation of qi activity, and pro
Given the current scanty research on the therapeutic effect of XFZYD in patients with CHF complicated with depression, we performed this study to confirm the clinical effectiveness of this TCM therapy in such patients.
We enrolled 116 patients with CHF complicated with depression who received treatment at Cangzhou Central Hospital, China, between July 2020 and July 2023. The control group (n = 55) was administered Western medicine, and the research group (n = 61) was treated with XFZYD.
All patients met the diagnostic criteria for CHF[16], with the syndrome of blood stasis and qi stagnation diagnosed by referring to the Guidelines for the Diagnosis and Treatment of Common Internal Diseases in Chinese Medicine[17]. The inclusion criteria were New York Heart Association (NYHA) classification grade II–III and TCM symptoms of depression, impatience, headache, insomnia, forgetfulness, pain in the chest and hypochondrium, chills or fever in a certain part of the body, a dark purple tongue or a tongue with petechiae and ecchymosis, and a stringy or uneven pulse. The exclusion criteria were as follows: use of other TCM decoctions 1 wk prior to enrollment or antidepressant medications within 1 month of enrollment; coagulation or immune dysfunction; uncontrollable hypertension and hyperglycemia; severe heart failure, severe ventricular arrhythmia, or constrictive pericarditis; other organ dysfunction; history of heart surgery; history of mental illness; infectious or blood system diseases; pregnancy or lactation; and incomplete clinical data.
All patients received conventional treatment according to the European Society of Cardiology 2016 Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure, as well as conventional psychological care interventions[18].
The control group was treated with Western medicine (flupentixol and melitracen tablets administered in the morning and at noon, one tablet at a time). The research group received XFZYD. The prescription comprised 12 g peach kernel; 9 g each of Carthamus tinctorius L., angelica, Radix Rehmanniae, and Achyranthis Bidentatae; 10 g each of chuanxiong rhizome and Platycodon grandiflorus; 6 g each of Radix Paeoniae Rubra, Fructus Aurantii, and licorice; and 15 g of Radix Bupleuri. The above components were boiled in 500 mL of clear water and simmered to reduce the volume to 400 mL. The drug was taken warm, with 200 mL in the morning and evening, respectively, for a course of treatment of 4 weeks. Both groups were treated for two consecutive courses.
Efficacy: The therapeutic effectiveness of both groups was observed and recorded. Marked effectiveness was defined as the basic or complete disappearance of clinical symptoms, including the evaluation of cardiac function as NYHA grade I or an improvement by more than two grades and a ≥ 70% reduction in the TCM symptom score. Effectiveness was defined as an obvious improvement of clinical symptoms, including an improvement of cardiac function by one grade but not by up to two grades, and a reduction of 30%–70% in the TCM symptom score. Ineffectiveness was defined as no significant improvement or deterioration of clinical symptoms, improvement of cardiac function by less than one grade or worsening of cardiac function, and a reduction of < 30% in the TCM symptom score or a higher score than before treatment. The total effective rate was the sum of the marked effectiveness rate and effectiveness rate.
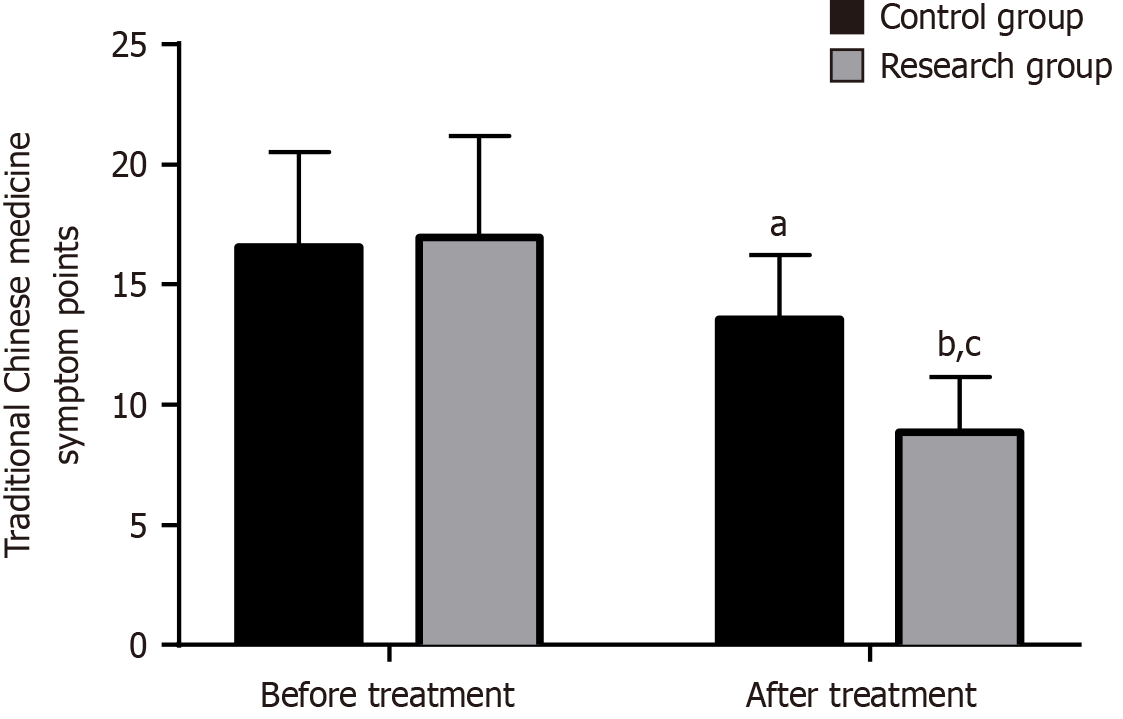
TCM symptom score: All patients were scored by the same physician before and after treatment for seven symptoms: Depression, frequent sighing, palpitations, fatigue, shortness of breath and weakness, pale complexion, and cold hands and feet, with a total score of 7–21, proportional to the symptoms and signs.
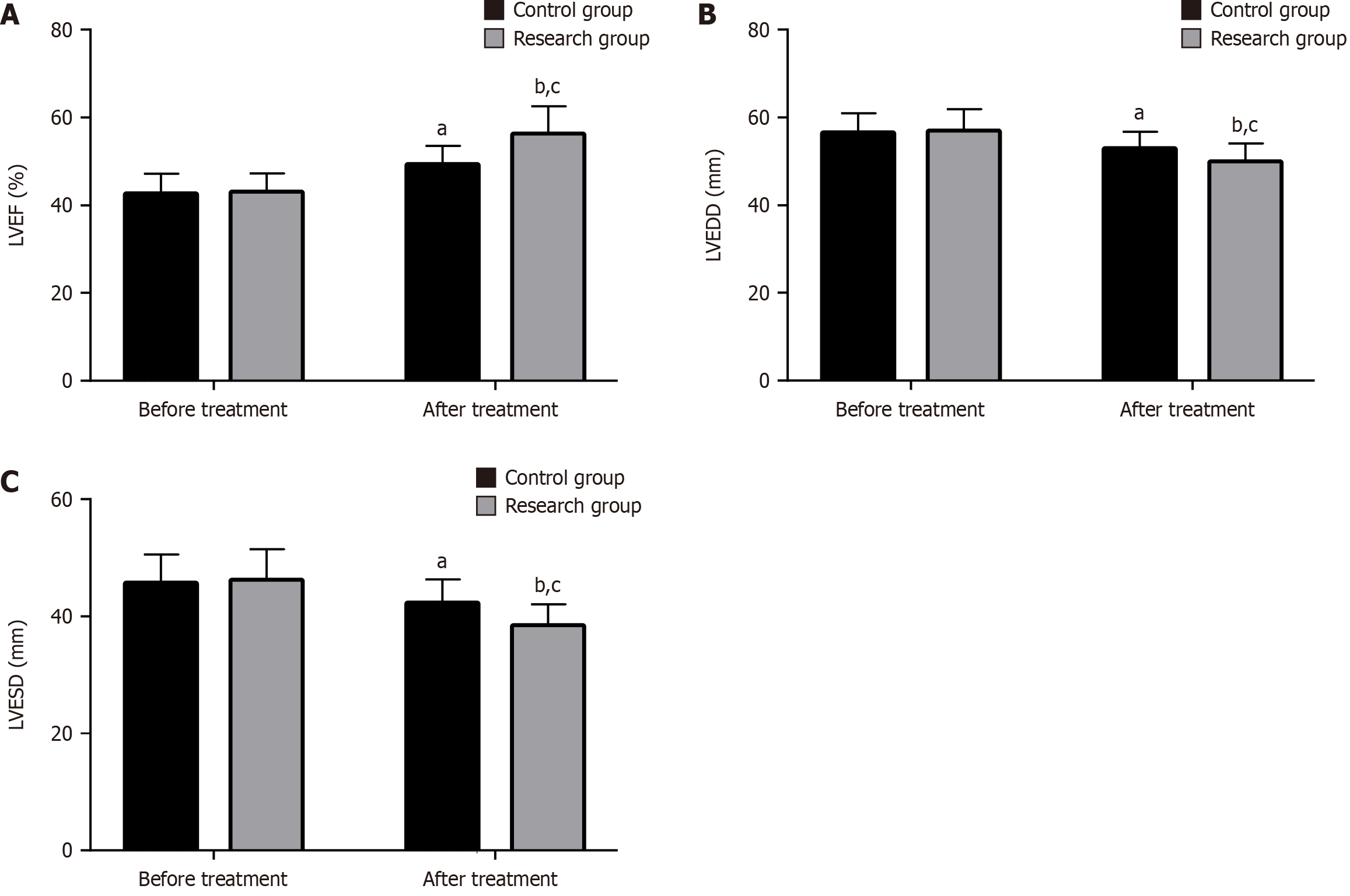
Cardiac function: The left ventricular ejection fraction (LVEF), left ventricular end-diastolic diameter (LVEDD), and left ventricular end-systolic diameter (LVESD) were measured by echocardiography before and after treatment.
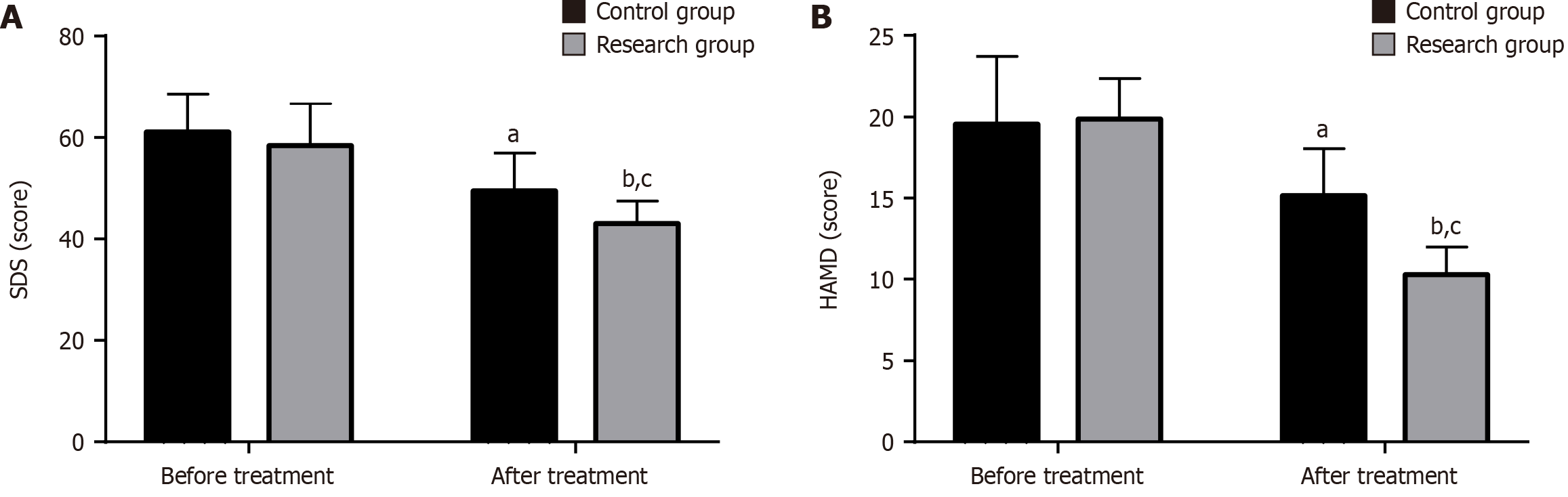
Negative emotions: The depressive mood of the patients was assessed using the Self-Rating Depression Scale (SDS), which comprises 20 items with a score of 0–80. Patients’ depression was also evaluated using the Hamilton Depression Scale (HAMD), which comprises 17 items, with a score of 0–68. For both the SDS and HAMD, the higher the score, the more serious the depression.
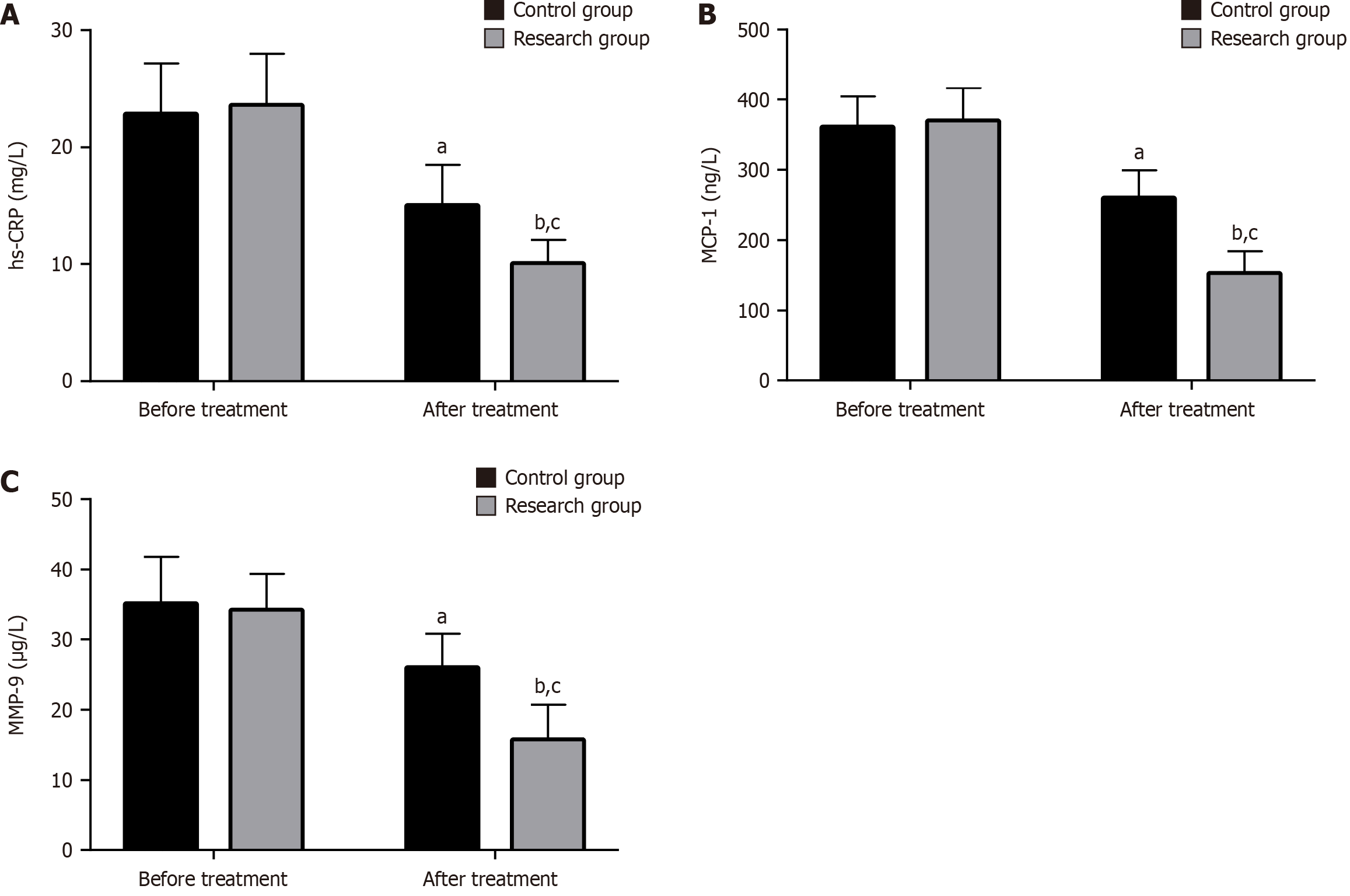
Serum inflammatory factors: We collected 5 mL of venous blood before and after treatment. The serum was obtained after centrifugation and used to determine the levels of high-sensitivity C-reactive protein (hs-CRP), monocyte chemoattractant protein-1 (MCP-1), and matrix metalloproteinase-9 (MMP-9) by enzyme-linked immunosorbent assay.
Continuous variables were described as mean ± SD, with intergroup and intragroup comparisons performed using t-test and paired t-test, respectively. Categorical variables were described as numbers and percentages, and intergroup comparisons were performed using χ2 test. SPSS v24.0 software was used for statistical analysis. P values < 0.05 were considered statistically significant.
The two groups were similar in sex, age, CHF course, NYHA grade, and the course and degree of depression (P > 0.05; Table 1).
| Indicators | Control group (n = 55) | Research group (n = 61) | χ2/t-test | P value |
| Sex (male/female) | 35/20 | 37/24 | 0.109 | 0.741 |
| Age (yr) | 58.00 ± 5.97 | 58.77 ± 7.06 | 0.631 | 0.530 |
| CHF course (yr) | 3.89 ± 0.66 | 3.84 ± 0.82 | 0.359 | 0.720 |
| NYHA classification (II/III) | 31/24 | 35/26 | 0.012 | 0.912 |
| Depression course (months) | 4.53 ± 0.77 | 4.67 ± 0.94 | 0.872 | 0.385 |
| Depression degree (mild/moderate) | 17/38 | 20/41 | 0.047 | 0.829 |
The total effective cases in the control and research groups were 43 and 58, respectively, indicating a significantly higher total effective rate in the research group compared with the control group (P < 0.05; Table 2).
| Indicators | Control group (n = 55) | Research group (n = 61) | χ2 | P value |
| Marked effectiveness | 16 (29.09) | 22 (36.07) | ||
| Effectiveness | 27 (49.09) | 36 (59.02) | ||
| Ineffectiveness | 12 (21.82) | 3 (4.92) | ||
| Total effective rate | 43 (78.18) | 58 (95.08) | 7.337 | 0.007 |
We calculated the TCM symptom scores of both groups before and after treatment. There were no significant differences between groups before treatment (P > 0.05). However, the scores decreased significantly (P < 0.05) after treatment in both groups, particularly in the research group (Figure 1).
The main evaluation indices of cardiac function were LVEF, LVEDD, and LVESD. The two groups did not differ markedly in the pretreatment levels of these three indices (P > 0.05). However, LVEF significantly increased (P < 0.05) in both groups after treatment, with an even higher increase in the research group. Furthermore, LVEDD and LVESD were significantly reduced (P < 0.05) after treatment and were lower in the research group than in the control group (Figure 2).
We used the SDS and HAMD scales to evaluate changes in depressive mood in the two groups. No notable intergroup differences were identified in the two scale scores before treatment (P > 0.05). A significant reduction (P < 0.05) was observed in SDS and HAMD scores in both groups after treatment, and these were more significantly decreased in the research group compared with the control group (Figure 3).
We measured the levels of the major serum inflammatory factors hs-CRP, MCP-1, and MMP-9. There were no significant intergroup differences before treatment (P > 0.05). After treatment, both the research and control groups showed markedly lowered hs-CRP, MCP-1, and MMP-9 Levels, and the levels in the research group were lower than those in the control group (P < 0.05; Figure 4).
Depression is a debilitating mental illness characterized by persistent low spirits, reduced enthusiasm for daily life, and a dulled ability to experience happiness[19]. The disease is common in patients with CHF and is not only harmful to patient recovery but also increases the risk of suicide[20]. This study analyzed the clinical intervention effect of XFZYD on CHF complicated with depression, with the aim of improving the curative effect in such patients.
The total effective rate in the research group was 95.08%, which was significantly higher than that of the control group (78.18%), indicating that the use of XFZYD in patients with CHF and depression is conducive to a significant improve
In summary, XFZYD is superior to Western medicines such as flupentixol and melitracen in treating patients with CHF complicated with depression and exerts a significant therapeutic effect. Besides significantly relieving clinical TCM symptoms and enhancing cardiac function, this TCM therapy also relieves depression and markedly inhibits the levels of serum inflammatory factors. Our findings provide an optimized direction for the treatment of patients with CHF complicated with depression, as evidenced by changes in certain clinical values.
| 1. | Brennan EJ. Chronic heart failure nursing: integrated multidisciplinary care. Br J Nurs. 2018;27:681-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Ziaeian B, Fonarow GC. Epidemiology and aetiology of heart failure. Nat Rev Cardiol. 2016;13:368-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 791] [Cited by in RCA: 1350] [Article Influence: 135.0] [Reference Citation Analysis (1)] |
| 3. | Vijay K, Neuen BL, Lerma EV. Heart Failure in Patients with Diabetes and Chronic Kidney Disease: Challenges and Opportunities. Cardiorenal Med. 2022;12:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 51] [Reference Citation Analysis (0)] |
| 4. | Yohannes AM, Willgoss TG, Baldwin RC, Connolly MJ. Depression and anxiety in chronic heart failure and chronic obstructive pulmonary disease: prevalence, relevance, clinical implications and management principles. Int J Geriatr Psychiatry. 2010;25:1209-1221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 316] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 5. | Liguori I, Russo G, Curcio F, Sasso G, Della-Morte D, Gargiulo G, Pirozzi F, Cacciatore F, Bonaduce D, Abete P, Testa G. Depression and chronic heart failure in the elderly: an intriguing relationship. J Geriatr Cardiol. 2018;15:451-459. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 30] [Reference Citation Analysis (0)] |
| 6. | Jiang CH, Zhu F, Qin TT. Relationships between Chronic Diseases and Depression among Middle-aged and Elderly People in China: A Prospective Study from CHARLS. Curr Med Sci. 2020;40:858-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 154] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 7. | Bucciarelli V, Caterino AL, Bianco F, Caputi CG, Salerni S, Sciomer S, Maffei S, Gallina S. Depression and cardiovascular disease: The deep blue sea of women's heart. Trends Cardiovasc Med. 2020;30:170-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 137] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 8. | Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129-2200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10348] [Cited by in RCA: 9587] [Article Influence: 958.7] [Reference Citation Analysis (3)] |
| 9. | Yan L, Ai Y, Xing Y, Wang B, Gao A, Xu Q, Li H, Chen K, Zhang J. Citalopram in the treatment of elderly chronic heart failure combined with depression: A systematic review and meta-analysis. Front Cardiovasc Med. 2023;10:1107672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 10. | Cai Q, Cai SB, Chen JK, Bai XH, Jing CX, Zhang X, Li JQ. Tai Chi for anxiety and depression symptoms in cancer, stroke, heart failure, and chronic obstructive pulmonary disease: A systematic review and meta-analysis. Complement Ther Clin Pract. 2022;46:101510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Wang Y, Lv W, Chen H, Yang Q, Zhang Y. Clinical Value of Heart Qi in the Treatment of Chronic Heart Failure With Depression. Altern Ther Health Med. 2024;30:36-41. [PubMed] |
| 12. | Liu J, Dong B, Yang L, Huang W, Tang S. Xuefu Zhuyu decoction for nonalcoholic fatty liver disease: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2021;100:e25358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Yi GZ, Qiu YQ, Xiao Y, Yuan LX. The usefulness of xuefu zhuyu tang for patients with angina pectoris: a meta-analysis and systematic review. Evid Based Complement Alternat Med. 2014;2014:521602. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Wang Y, Wang Q, Li C, Lu L, Zhang Q, Zhu R, Wang W. A Review of Chinese Herbal Medicine for the Treatment of Chronic Heart Failure. Curr Pharm Des. 2017;23:5115-5124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 62] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 15. | Chen L, Yu D, Ling S, Xu JW. Mechanism of tonifying-kidney Chinese herbal medicine in the treatment of chronic heart failure. Front Cardiovasc Med. 2022;9:988360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 16. | McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Kathrine Skibelund A; ESC Scientific Document Group. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599-3726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8225] [Cited by in RCA: 8646] [Article Influence: 1729.2] [Reference Citation Analysis (1)] |
| 17. | Wang TF, Wang JJ, Xue XL, Han P, Zhang YJ, Li GR, Wu XY, Zhao Y, Tang LL, Liu YY, Sui CL, Fu C, Shang YM, Zhou B. [Distribution characteristics of traditional Chinese medicine syndromes and their elements in people with subhealth fatigue]. Zhong Xi Yi Jie He Xue Bao. 2010;8:220-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Oeing CU, Tschöpe C, Pieske B. [The new ESC Guidelines for acute and chronic heart failure 2016]. Herz. 2016;41:655-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Szyguła-Jurkiewicz B, Duszańska A, Poloński L. Is depression a problem in patients with chronic heart failure? Pol Arch Med Wewn. 2008;118:52-56. [PubMed] |
| 20. | Korkmaz H, Korkmaz S, Çakar M. Suicide risk in chronic heart failure patients and its association with depression, hopelessness and self esteem. J Clin Neurosci. 2019;68:51-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 21. | Huang L, Yu Q, Peng H, Zhen Z. The mechanism of peach kernel and safflower herb-pair for the treatment of liver fibrosis based on network pharmacology and molecular docking technology: A review. Medicine (Baltimore). 2023;102:e33593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 22. | Zhou Y, Jiang H, Huang X, Rao K, Wang D, Wu Q, Zhang P, Pei J. Indistinct assessment of the quality of traditional Chinese medicine in precision medicine exampling as safflower. J Pharm Biomed Anal. 2023;227:115277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 23. | Minami M, Takase H, Taira M, Makino T. In Vitro Effect of the Traditional Medicine Hainosan (Painongsan) on Porphyromonas gingivalis. Medicines (Basel). 2019;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Tao F, Cai Y, Deng C, Chen Z, Shen Y, Sun H. A narrative review on traditional Chinese medicine prescriptions and bioactive components in epilepsy treatment. Ann Transl Med. 2023;11:129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 25. | Pan L, Peng C, Wang L, Li L, Huang S, Fei C, Wang N, Chu F, Peng D, Duan X. Network pharmacology and experimental validation-based approach to understand the effect and mechanism of Taohong Siwu Decoction against ischemic stroke. J Ethnopharmacol. 2022;294:115339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 56] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 26. | Singh A, Zhao K. Treatment of Insomnia With Traditional Chinese Herbal Medicine. Int Rev Neurobiol. 2017;135:97-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 78] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 27. | Zhang S, Chen ZL, Tang YP, Duan JL, Yao KW. Efficacy and Safety of Xue-Fu-Zhu-Yu Decoction for Patients with Coronary Heart Disease: A Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med. 2021;2021:9931826. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 28. | Qi G, Jiang K, Qu J, Zhang A, Xu Z, Li Z, Zheng X. The Material Basis and Mechanism of Xuefu Zhuyu Decoction in Treating Stable Angina Pectoris and Unstable Angina Pectoris. Evid Based Complement Alternat Med. 2022;2022:3741027. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 29. | Wang XR, Song DD, Tao TQ, He T, Wu XD, Li XM, Liu XH. Qi-Regulating and Blood Circulation-Promoting Therapy Improves Health Status of Stable Angina Pectoris Patients with Depressive Symptoms. Evid Based Complement Alternat Med. 2021;2021:7319417. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/