Published online Jun 19, 2024. doi: 10.5498/wjp.v14.i6.848
Revised: April 23, 2024
Accepted: May 9, 2024
Published online: June 19, 2024
Processing time: 112 Days and 2.1 Hours
Depression is a common, chronic, and recurrent mood disorder that has become a worldwide health hazard. Fluoxetine hydrochloride, a common treatment method, can inhibit 5-hydroxytryptamine (5-HT) recycling in the presynaptic membrane; however, the efficacy of a single drug is inadequate. At present, mild-to-moderate depression can be treated with acupuncture of ghost caves, but the clinical curative effect of combined therapy with fluoxetine hydrochloride has not been sufficiently reported.
To evaluate the clinical effect of acupuncture at ghost points combined with fluoxetine hydrochloride in the treat
This retrospective study included 160 patients with mild-to-moderate depression who were admitted to Shanghai Hospital of Integrated Traditional Chinese and Western Medicine, Affiliated to Shanghai University of Traditional Chinese Medicine, between January 2022 and June 2023. Patients were separated into a single-agent group (fluoxetine hydrochloride treatment, n = 80) and a coalition group (fluoxetine hydrochloride treatment combined with acupuncture at ghost points, n = 80). Pre-treatment symptoms were recorded, and the clinical curative effect and adverse reactions [Asberg Antidepressant Side Effects Scale (SERS)] were assessed. Depression before and after treatment [Hamilton Depression Scale (HAMD)-24], neurotransmitter levels [5-HT, norepinephrine (NE), dopamine (DA)], oxidative stress indicators [superoxide dismutase (SOD), malondialdehyde (MDA)], and sleep quality [Pittsburgh Sleep Quality Index (PSQI)] were compared.
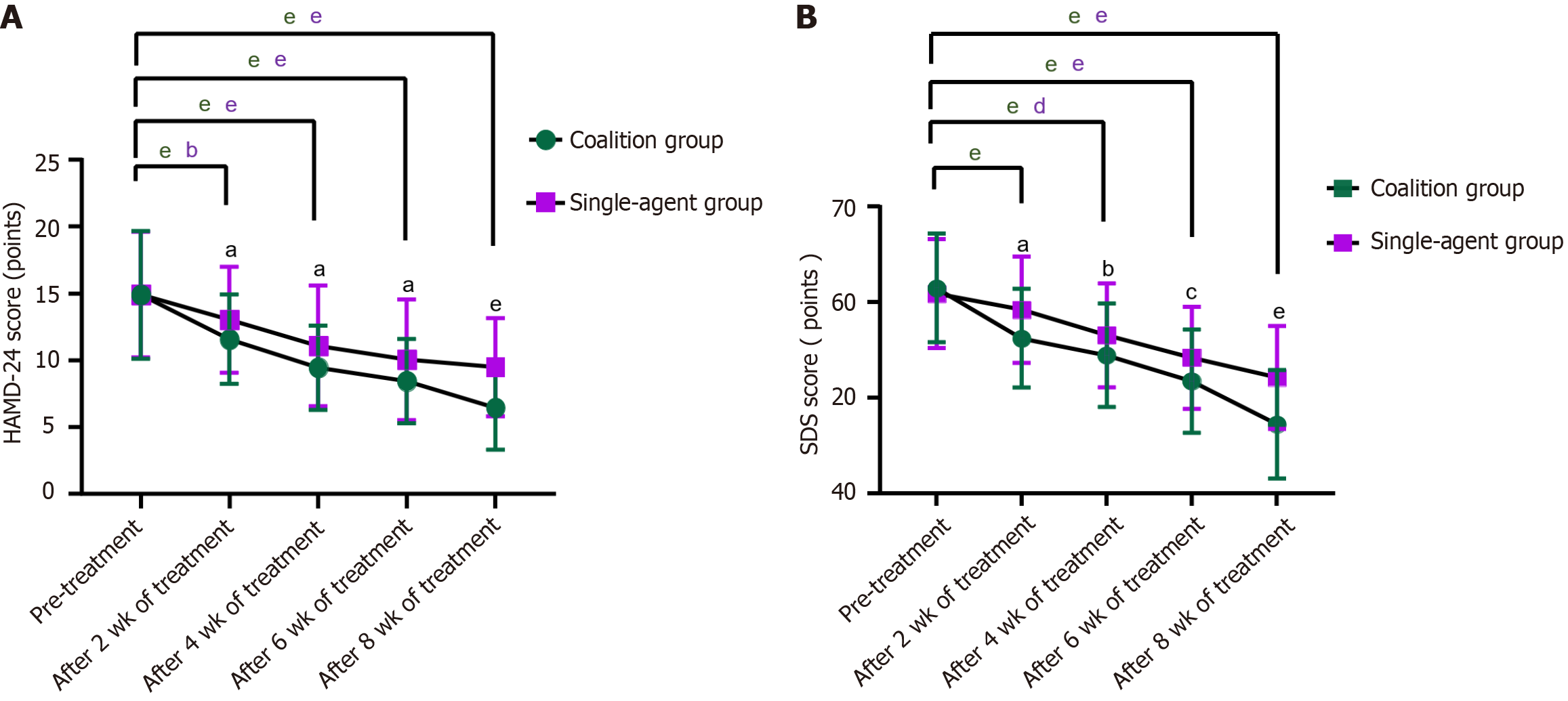
The total efficacy rate was 97.50% in the coalition group and 86.25% in the single-agent group (P < 0.05). After 2, 4, 6, and 8 wk of treatment, the HAMD, self-rating depression scale, and SERS scores of the coalition and single-agent groups decreased compared with pre-treatment, and the decrease was more significant in the coalition group (P < 0.05). After 8 wk of treatment, the levels of NE, DA, 5-HT, and SOD in the coalition and single-agent groups increased, while the levels of MDA decreased; the increases and decrease in the coalition group were more significant (P < 0.05). The PSQI scores of the coalition and single-agent groups decreased, and the decrease was more significant in the coalition group (P < 0.05).
Acupuncture at ghost points combined with paroxetine tablets can safely improve depressive symptoms and sleep disorders, regulate neurotransmitter levels, and reduce stress responses in patients with mild-to-moderate depression.
Core Tip: Depression is a common psychiatric disease that can manifest as low mood, decreased interest, and energy fatigue. The rates of suicide and self-harm associated with depression are very high. In this study, we found that, compared with fluoxetine treatment alone, acupuncture at ghost points combined with paroxetine hydrochloride can improve mild-to-moderate depression and sleep disturbance in patients, regulate neurotransmitter levels, reduce stress responses, and improve safety.
- Citation: Wang Y, Lu Q, Penpat I, Wu J, Abulikemu D, Zeng FC, Huang JY, Hu ZH. Clinical effect of acupuncture at ghost points combined with fluoxetine hydrochloride on mild-to-moderate depression. World J Psychiatry 2024; 14(6): 848-856
- URL: https://www.wjgnet.com/2220-3206/full/v14/i6/848.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i6.848
Depression is a mental and psychological disease characterized by persistent low mood, slow thinking, decline in cognitive function, decreased volitional activity, and physical symptoms, and it is an important cause of global mental disability[1,2]. Depression is expected to become the world’s largest disease threatening human physical and mental health by 2030[3]. Selective serotonin reuptake inhibitor antidepressants including fluoxetine hydrochloride are currently one of the typical drug types used in the clinical treatment of depression[4]. They act on the synapses of the central nervous system to inhibit the reuptake of serotonin by the presynaptic membrane, thereby achieving therapeutic effects. However, satisfactory results are difficult to achieve owing to shortcomings, such as a long period of stable plasma concentration, a narrow antidepressant spectrum, and obvious side effects[5].
Depression aligns with the traditional Chinese medicine ‘depressive syndrome’ category and is closely associated with the Yang-deficiency constitution. Based on the theory that Yang deficiency causes depression, some studies have verified the feasibility of treating depression with Yang support[6,7]. Acupuncture plays a unique role in the treatment of diseases and is a common therapy in traditional Chinese medicine. Current clinical trials on acupuncture’s effects on brain mechanisms of the central nervous system have aroused medical attention. Studies have shown that acupuncture plays a significant role in protecting neurons[8]. In addition, domestic and foreign doctors have achieved remarkable results in the clinical treatment of patients with depression using acupuncture. Its mechanism of action is related to the regulation of the cortical striatum reward/motivation circuit in the brains of patients with depression. Studies have shown that acupuncture combined with drug treatment for depression can improve the depressive state and physical symptoms of patients with depression. Compared with drug use alone, acupuncture combined with drug treatment has been shown to improve efficacy, reduce adverse reactions, and reduce drug dose[9]. Acupuncture at effective thirteen ghost points is used in traditional Chinese medicine to treat emotional diseases. In recent years, acupuncture has been commonly used to treat intractable insomnia, Alzheimer’s disease, vascular dementia, and other brain diseases, and can effectively alleviate conditions with significant curative effects[10,11]. However, few reports exist on the clinical effects of acupuncture at ghost points combined with fluoxetine hydrochloride in mild-to-moderate depression. This study aimed to explore the clinical effects of acupuncture at ghost points combined with fluoxetine hydrochloride on mild-to-moderate depression to provide a reference for clinical treatment.
This retrospective study included 160 patients with mild-to-moderate depression who were admitted to Shanghai Hospital of Integrated Traditional Chinese and Western Medicine, Affiliated to Shanghai University of Traditional Chinese Medicine, between January 2022 and June 2023. The diagnostic criteria for depression included core symptoms and additional symptoms[12]. Core symptoms were as follows: (1) Majority of time spent in a depressed state unaffected by external factors for > 2 wk; (2) Disinterest or inability to obtain pleasure from things that were once of interest or love; and (3) Regular feelings of tiredness and powerlessness. Additional symptoms were as follows: (1) Inattention; (2) Regular feelings of self-denial and lack of self-confidence; (3) Feelings of responsibility for mistakes with the concept of self-incrimination; (4) Thoughts of having no future; (5) Insomnia; (6) Regular suicidal tendencies and behavior; (7) Loss of appetite; and (8) Mild-to-moderate depression, namely a Hamilton Depression Scale-24 (HAMD-24) score of 7 to 24 points.
The inclusion criteria for this study were as follows: (1) Symptoms meeting the above diagnostic criteria; (2) No history of other antipsychotic drugs or hypnotic drugs before treatment; (3) Age of 18-70 years; and (4) Availability of complete data. The exclusion criteria were as follows: (1) Presence of severe, life-threatening organic lesions; (2) Presence of a malignant tumor, infection, or hemorrhage; (3) History of serious suicide attempts and behaviors; (4) Pregnancy or lactation; and (5) Presence of unhealed moxibustion site trauma skin lesions, local ulcers, red and swollen skin, or allergies. Based on the differences in intervention methods, patients were separated into single-agent and coalition groups (n = 80 cases each). No significant differences were identified in baseline data between the coalition and single-agent groups (P > 0.05) (Table 1).
| Group | Sex | Age (yr) | Degree of depression | Duration of disease (yr) | ||
| Male | Female | Mild | Moderate | |||
| Coalition group (n = 80) | 35 | 45 | 35.33 ± 9.06 | 46 | 34 | 2.41 ± 0.69 |
| Single-agent group (n = 80) | 37 | 43 | 36.16 ± 9.00 | 48 | 32 | 2.51 ± 0.72 |
| χ2/t | 0.101 | -0.587 | 0.103 | -0.826 | ||
| P value | 0.751 | 0.558 | 0.748 | 0.410 | ||
The single-agent group received oral fluoxetine hydrochloride capsules (Lilai Suzhou Pharmaceutical Co., Ltd., Sinopharm Approval No.: J20170022). The specific method of administration was performed according to the physicians’ advice. Oral administration of a 20 mg/d dose for 8 wk was recommended. The coalition group was based on single drug administration plus acupuncture at ghost points. Acupoint selection included ghost points “above the star”: Shuigou, Shaoshang, Yinbai, Daling, and Shenmai. The operation method was as follows: The patient was placed in the supine position and underwent routine skin disinfection. A Hua Tuo card (0.25 mm in diameter) was used with a disposable stainless steel filiform needle (diameter, 0.25 mm; length, 40 mm) for acupuncture. The Shuigou point was obliquely punctured in the direction of the nasal septum, which should stimulate tears. The needle was then sequentially inserted into the Shaoshang, Yinbai, Daling, and Shenmai points with a strong needle sensation. Among them, the Shaoshang and Yinbai points were obliquely punctured from the outside to the nail angle at a depth of 0.1-0.2, and the Daling point was punctured directly with electric shock. The Shangxing point was punctured with a flat thorn at an acupuncture depth of 0.5-0.8 in using the extraction method. All acupuncture operators had equal training performing the standardized operation. Each treatment lasted 30 min and was administered once per day, 5 times per week. Four treatment cycles took place: One observation cycle comprised ten occurrences, and continuous treatment was administered for three cycles.
Clinical efficacy: To evaluate clinical efficacy in patients, the improvement rate of HAMD-24 scores was calculated prior to treatment and 8 wk after treatment to obtain the efficacy index. The efficacy index was calculated as follows: (HAMD-24 score pre-treatment-HAMD-24 score 8 wk after treatment)/HAMD-24 score pre-treatment × 100%. The efficacy index was categorized as follows: Clinical control, efficacy index ≥ 75%; obvious effect, 50% ≤ efficacy index < 75%; effective, 25% ≤ efficacy index < 50%; and ineffective, efficacy index < 25%. The total effective rate was calculated as follows: (Effective + obvious + clinical control)/total disease × 100%. The efficacy evaluation was completed at 0, 2, and 8 wk.
Depressive symptoms: The HAMD-24[13] and self-rating depression scale (SDS)[14] were used to score depressive symptoms before and after treatment (2, 4, 6, and 8 wk after treatment). HAMD-24 scores were categorized as follows: Normal, scores of < 7; mild depression, scores of 7-16; moderate depression, scores of 17-23; severe depression, scores of 24-34; and further division of severe depression, scores of > 34. With a total of 20 items in the scale, the SDS was categorized as follows [standard score = rough score × 1.25 (integer part)]: Normal, 25-49 points; mild depression, 50-59 points; moderate depression, 60-69 points; and severe depression, 70 points.
Neurotransmitter levels: Neurotransmitter levels were analyzed. Before treatment and 8 wk after treatment, 10 mL of fasting peripheral venous blood was extracted from patients in the two groups, and 5 mL was placed into a 4 °C centrifuge for centrifugation. The upper serum was absorbed using a pipette and divided into 0.6-mL EP tubes. Serum levels of norepinephrine (NE), 5-hydroxytryptamine (5-HT), and dopamine (DA) were measured using high-pressure liquid chromatography-electrochemistry (North Institute of Biotechnology, Beijing).
Oxidative stress index: To measure the oxidative stress index, another 5 mL blood sample was taken. After centrifugation of the supernatant, an enzyme-linked immunosorbent assay (Wuhan Bode Biotechnology Co., Ltd.) was used to detect malondialdehyde (MDA) and superoxide dismutase (SOD) levels.
Sleep quality: The Pittsburgh Sleep Quality Index (PSQI)[15] was used to evaluate sleep quality. The PSQI consists of 19 self-rating questions and 5 other rating questions. The total score ranges from 0 to 21 points, with 0-5 indicating very good sleep quality, 6-10 indicating good sleep quality, 11-15 indicating average sleep quality, and > 15 indicating poor sleep quality.
Adverse reactions: According to the Asberg Rating Scale for Side Effects (SERS)[16], the adverse reactions in the coalition and single-agent groups were evaluated before and after treatment (2, 4, 6, and 8 wk later). The SERS contains a total of 14 items and uses a 4-level scoring method (0-3 points). The total score ranges from 0 to 42 and is proportional to the degree of adverse reactions.
Data were analyzed using the IBM SPSS software (version 29.0). Counting variables are expressed as numbers and percentages, and continuous variables are reported as means ± SD. They were tested using χ2 and t tests, respectively. P < 0.05 indicates statistical significance.
The total efficacy rate was 97.50% in the coalition group and 86.25% in the single-agent group (P < 0.05) (Table 2).
| Group | Clinical control | Remarkable | Effective | Invalid | Total effective rate (%) |
| Coalition group (n = 80) | 28 (35.00) | 32 (40.00) | 18 (22.50) | 2 (2.50) | 78 (97.50) |
| Single-agent group (n = 80) | 18 (22.50) | 23 (28.75) | 28 (35.00) | 11 (13.75) | 69 (86.25) |
| χ2 | 6.782 | ||||
| P value | 0.009 |
Pre-treatment, the HAMD-24 and SDS scores of the coalition and single-agent groups were not significantly different (P > 0.05). However, 2, 4, 6, and 8 wk after treatment, the HAMD-24 and SDS scores of the coalition and single-agent groups decreased, with a more significant decrease in the coalition group (P < 0.05) (Figure 1).
Pre-treatment, the 5-HT, DA, and NE levels were not significantly different among the coalition and single-agent groups (P > 0.05). However, 2, 4, 6, and 8 wk after treatment, the levels of 5-HT, DA, and NE increased in the coalition and single-agent groups, with more significant increases in the coalition group (P < 0.05) (Table 3).
| Group | 5-HT (ng/mL) | DA (pg/mL) | NE (pg/mL) | |||
| Pre-treatment | After 8 wk of treatment | Pre-treatment | After 8 wk of treatment | Pre-treatment | After 8 wk of treatment | |
| Coalition group (n = 80) | 95.81 ± 8.35 | 130.56 ± 16.39a | 122.59 ± 13.55 | 148.57 ± 16.34a | 8.83 ± 2.41 | 14.66 ± 2.77a |
| Single-agent group (n = 80) | 96.38 ± 9.05 | 119.25 ± 14.45a | 120.36 ± 12.85 | 133.55 ± 13.44a | 9.11 ± 1.96 | 12.14 ± 2.51a |
| t | -0.421 | 4.628 | 1.068 | 6.354 | -0.808 | 6.017 |
| P value | 0.674 | < 0.001 | 0.287 | < 0.001 | 0.420 | < 0.001 |
Pre-treatment, the MDA and SOD levels were not significantly different between the coalition and single-agent groups (P > 0.05). However, after 8 wk of treatment, SOD levels increased and MDA levels decreased, with more significant increase and decrease ranges in the coalition group (P < 0.05) (Table 4).
| Group | MDA (mmol/L) | SOD (U/mL) | ||
| Pre-treatment | After 8 wk of treatment | Pre-treatment | After 8 wk of treatment | |
| Coalition group (n = 80) | 12.21 ± 1.80 | 7.54 ± 1.02a | 55.55 ± 5.62 | 68.16 ± 6.75a |
| Single-agent group (n = 80) | 12.09 ± 1.77 | 8.80 ± 1.31a | 55.65 ± 5.70 | 61.10 ± 5.95a |
| t | 0.424 | -6.762 | -0.123 | 7.002 |
| P value | 0.672 | < 0.001 | 0.902 | < 0.001 |
Pre-treatment, the PSQI scores were not significantly different between the coalition and single-agent groups (P > 0.05). After 8 wk of treatment, the PSQI scores of the coalition and single-agent groups decreased, with a more significant decrease in the coalition group (P < 0.05) (Table 5).
Pre-treatment, the SERS scores were not significantly different between the coalition and single-agent groups (P > 0.05); however, after 2, 4, 6, and 8 wk of treatment, the SERS scores of the coalition and single-agent groups decreased, with a more significant decrease in the coalition group (P < 0.05) (Table 6).
| Group | Pre-treatment | After treatment | |||
| After 2 wk | After 4 wk | After 6 wk | After 8 wk | ||
| Coalition group (n = 80) | 10.75 ± 2.51 | 8.89 ± 2.39b | 8.16 ± 2.10b | 6.75 ± 2.13b | 5.11 ± 1.69b |
| Single-agent group (n = 80) | 10.86 ± 2.32 | 9.85 ± 2.11a | 9.18 ± 2.03b | 7.75 ± 2.00b | 6.82 ± 1.84b |
| t | -0.294 | -2.702 | -3.136 | -3.062 | -6.116 |
| P value | 0.769 | 0.008 | 0.002 | 0.003 | < 0.001 |
The clinical manifestations of mild-to-moderate depression mainly include inattention, persistently low mood, low self-evaluation, slow thinking activity, poor social adaptability, and listlessness. With disease aggravation, patients may experience mental symptoms, such as delusions and hallucinations[17]. In recent years, the incidence of depression has increased annually, placing a heavy burden on society and families. Paroxetine hydrochloride is a class of selective NE reuptake inhibitors that can be metabolized by the liver without metabolite activity and has a good antidepressant effect with few adverse reactions. It is commonly used to treat depression, but its single-drug effect is poor[18].
The ‘depression syndrome’ category of traditional Chinese medicine occurs because of congenital physical weakness or liver fire flourishing coupled with acquired emotional disorders, resulting in qi blockage, mental disorders, and a class of diseases. Clinical manifestations include depression, chest pain, and hypochondriac fullness. In the theory of traditional Chinese medicine, qi and blood are important components of the human body which maintain the operation of the body’s qi machine. Internal injury of the seven emotions relates to a weak zangqi element, and the stagnation of liver qi and loss of temper lead to the imbalance of Yin and Yang in Zangfu organs, qi, and blood, resulting in mental health disorders and similar diseases of emotional depression[19]. Acupuncture at ghost points clears channels and collaterals, regulates qi, harmonizes Yin and Yang, and improves depressive symptoms[20]. The Shangxing point selected in this study is located in the governor vessel, which can awaken the brain and tranquilize the mind. Shaoshang is the well point of the lung meridian, and Yinbai is the well point of the spleen meridian. Acupuncture can not only drain the lung and transport the spleen but can also awaken the spirit and open the orifices. Shenmai is the Jinmen point of the bladder meridian, which is the same as the lung meridian qi and blood. Therefore, acupuncture can stimulate the meridian qi of the human body and regulate the function of qi and blood. ‘Lingshu·Meridian’ records that changes in the Yangming meridian change the spirit and emotion. Qi and blood are easy to move, and the spirit is not separated from qi and blood. The thirteen ghost acupoints were specially used to wake up the spirit, open the orifices, clear the heart, relieve depression, regulate qi, and tranquilize the mind[21]. Acupuncture at the Guixin and Daling point broadens the chest and regulates qi to promote blood circulation and dredge collaterals. It may be combined with acupuncture at the Laogong point of the heart to purge fire, clear the heart, and calm the mind. Loss of transportation and transformation of the spleen leads to phlegm and dampness. Acupuncture at the Guilei Yinbai point helps the transportation and transformation of the spleen to invigorate it, remove dampness, and reduce turbidity. Acupuncture at the Guigong Shuigou and Guitang Shangxing on the head can dredge the governor vessel and regulate the mind, open the orifices, and relieve depression[22].
In this study, the total efficacy rate was 97.50% in the coalition group and 86.25% in the single-agent group (P < 0.05), suggesting that acupuncture combined with paroxetine hydrochloride tablets had a better effect on mild-to-moderate depression. After treatment, the HAMD, SDS, and PSQI scores in the coalition group were lower than those in the single-agent group (P < 0.05), suggesting that acupuncture at ghost points combined with paroxetine hydrochloride tablets can significantly improve depressive symptoms and sleep disorders in patients. Antidepressants are usually accompanied by adverse reactions, such as drowsiness, dizziness, headache, and gastrointestinal reactions. Studies have shown that acupuncture may not only accelerate the onset time of antidepressants but also improve the overall efficacy and reduce adverse reactions[23,24]. In this study, the total SERS scores of the coalition group after treatment were lower than those of the single-agent group (P < 0.05), suggesting that acupuncture at ghost points can safely reduce the adverse reactions caused by paroxetine hydrochloride tablets.
The 5-HT content in the cerebral cortex and synapses is very high and can promote neuronal differentiation. A lower level of 5-HT correlates with more severe depressive symptoms and worse prognosis[25]. DA is a catecholamine neurotransmitter present in the nerve tissues and body fluids. When people are happy, relaxed, pleasant, comfortable, and enjoyable, DA secretion increases significantly. Poor function of the DA system in patients with depression directly damages the plasticity of the hippocampus-frontal cortex synapses, leading to emotional regulation and cognitive dysfunction[26]. NE is a common neurotransmitter affecting various regions of the brain. It can regulate arousal and stress responses by regulating synaptic afferent activity and reducing afferents of interfering stimuli. It has been reported that depression is closely related to disorders of brain 5-HT and NE activity, and increasing the levels of NE and 5-HT in the brain is a good strategy to treat depression[27]. In a study on depression, Wang et al[28] found that NE and 5-HT activity in the brains of patients was significantly increased after drug intervention. And it showed that similar to the effect of the positive drug (fuoxetine) on the regulation of NE and 5-HT content, Xiaoyao-jieyu-san could effectively increase the NE and 5-HT content in the brain tissue of PSD rats. Studies have shown that acupuncture at ghost points can excite the ascending nerve activation system and promote the production of neurotransmitters, such as 5-HT, DA, and NE. It can further regulate the excitation and inhibition processes of the cerebral cortex through the nerve-endocrine-immune system; thus, various neurotransmitters between synapses can be balanced. Acupuncture at ghost points can simultaneously enhance stress, promote adrenal secretion, and improve mental symptoms[29]. SOD is an enzyme that scavenges free oxygen radicals, and MDA is a product of peroxidation. The expression levels of both reflect the degree of lipid peroxidation in the body and the ability of the body to scavenge free oxygen radicals[30]. After 8 wk of treatment, the levels of NE, 5-HT, DA, and SOD in the coalition and single-agent groups increased, while the level of MDA decreased. The increase and decrease in the coalition group were more significant (P < 0.05), suggesting that paroxetine hydrochloride tablets combined with acupuncture at ghost points can regulate the levels of neurotransmitters in patients with mild-to-moderate depression and reduce the oxidative stress response. This study still has some limitations. For example, this study is a single-center study with a single sample source. Therefore, its generalizability to a wider population, including different ethnic and cultural backgrounds, is not clear. In the future, multi-center studies will be carried out to expand the sample size for further exploration.
In summary, treatment with paroxetine hydrochloride tablets combined with acupuncture at ghost points in patients with mild-to-moderate depression can safely and significantly improve depressive symptoms and sleep disorders, regulate the levels of neurotransmitters, and reduce oxidative stress responses.
| 1. | Ogbo FA, Mathsyaraja S, Koti RK, Perz J, Page A. The burden of depressive disorders in South Asia, 1990-2016: findings from the global burden of disease study. BMC Psychiatry. 2018;18:333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 49] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 2. | Friedrich MJ. Depression Is the Leading Cause of Disability Around the World. JAMA. 2017;317:1517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 279] [Cited by in RCA: 543] [Article Influence: 60.3] [Reference Citation Analysis (0)] |
| 3. | Athira KV, Bandopadhyay S, Samudrala PK, Naidu VGM, Lahkar M, Chakravarty S. An Overview of the Heterogeneity of Major Depressive Disorder: Current Knowledge and Future Prospective. Curr Neuropharmacol. 2020;18:168-187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 69] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 4. | Shen D, Zhao H, Gao S, Li Y, Cheng Q, Bi C, Zhou Z, Yu C. Clinical serum metabolomics study on fluoxetine hydrochloride for depression. Neurosci Lett. 2021;746:135585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Micheli L, Ceccarelli M, D'Andrea G, Tirone F. Depression and adult neurogenesis: Positive effects of the antidepressant fluoxetine and of physical exercise. Brain Res Bull. 2018;143:181-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 202] [Article Influence: 25.3] [Reference Citation Analysis (0)] |
| 6. | Zhang Y, Liu Y, Ning B, Yan L, Wu L, Zhang D, Li C, Ouyang W, Su S, Jiang S, Zhang G, Xu J, Wang Z, Zheng Z, Zheng D, Chen S, Sun L, Fu W. Efficacy of the Integrative Acupuncture and Moxibustion Treatment in Patients With Major Depressive Disorder: The Study Protocol for a Multicenter, Single-Blinded, Randomized Trial in China. Front Med (Lausanne). 2022;9:761419. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Li XH, Li JL, Dong TT, Ma X, Xue XQ, Yang JG. [Governor vessel moxibustion combined with western medication for mild to moderate depression with kidney-yang deficiency: a randomized controlled trial]. Zhongguo Zhen Jiu. 2023;43:14-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Armour M, Smith CA, Wang LQ, Naidoo D, Yang GY, MacPherson H, Lee MS, Hay P. Acupuncture for Depression: A Systematic Review and Meta-Analysis. J Clin Med. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 108] [Article Influence: 15.4] [Reference Citation Analysis (2)] |
| 9. | Wang Y, Huang YW, Ablikim D, Lu Q, Zhang AJ, Dong YQ, Zeng FC, Xu JH, Wang W, Hu ZH. Efficacy of acupuncture at ghost points combined with fluoxetine in treating depression: A randomized study. World J Clin Cases. 2022;10:929-938. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Wang YP, Wen X, Feng XL, He TY. [Yinyang Ruyin acupuncture on refractory insomnia: a randomized controlled trial]. Zhongguo Zhen Jiu. 2019;39:1155-1159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Du K, Yang S, Wang J, Zhu G. Acupuncture Interventions for Alzheimer's Disease and Vascular Cognitive Disorders: A Review of Mechanisms. Oxid Med Cell Longev. 2022;2022:6080282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 12. | First MB. Diagnostic and statistical manual of mental disorders, 5th edition, and clinical utility. J Nerv Ment Dis. 2013;201:727-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 379] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 13. | Kyle PR, Lemming OM, Timmerby N, Søndergaard S, Andreasson K, Bech P. The Validity of the Different Versions of the Hamilton Depression Scale in Separating Remission Rates of Placebo and Antidepressants in Clinical Trials of Major Depression. J Clin Psychopharmacol. 2016;36:453-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 14. | Zung WW. A Self-rating depression scale. Arch Gen Psychiatry. 1965;12:63-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5900] [Cited by in RCA: 6293] [Article Influence: 209.8] [Reference Citation Analysis (0)] |
| 15. | van Strien AM, Keijsers CJ, Derijks HJ, van Marum RJ. Rating scales to measure side effects of antipsychotic medication: A systematic review. J Psychopharmacol. 2015;29:857-866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17520] [Cited by in RCA: 23641] [Article Influence: 638.9] [Reference Citation Analysis (0)] |
| 17. | Ullah H, Di Minno A, Esposito C, El-Seedi HR, Khalifa SAM, Baldi A, Greco A, Santonastaso S, Cioffi V, Sperandeo R, Sacchi R, Daglia M. Efficacy of a food supplement based on S-adenosyl methionine and probiotic strains in subjects with subthreshold depression and mild-to-moderate depression: A monocentric, randomized, cross-over, double-blind, placebo-controlled clinical trial. Biomed Pharmacother. 2022;156:113930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 18. | You Y, Zhang T, Shu S, Qian X, Zhou S, Yao F. Wrist-ankle acupuncture and Fluoxetine in the treatment of post-stroke depression: a randomized controlled clinical trial. J Tradit Chin Med. 2020;40:455-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 19. | Pilkington K. Anxiety, depression and acupuncture: A review of the clinical research. Auton Neurosci. 2010;157:91-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 61] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 20. | Gu T, Wang RH, Wu T, Ke ZH, Yang H, Wang D. [Therapeutic effect on mild perimenopausal depression treated with acupuncture at the "thirteen ghost points" and kaixin powder]. Zhongguo Zhen Jiu. 2020;40:267-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Fu W, Wang MY, Ning BL, Zhou P, Fu WB. [Professor FU Wen-bin's experience in treatment of mental disorder with acupuncture and moxibustion from perspective of "psychosomatic medicine"]. Zhongguo Zhen Jiu. 2021;41:1140-1144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Cheng WJ, Li P, Huang WY, Huang Y, Chen WJ, Chen YP, Shen JL, Chen JK, Long NS, Meng XJ. Acupuncture Relieves Stress-Induced Depressive Behavior by Reducing Oxidative Stress and Neuroapoptosis in Rats. Front Behav Neurosci. 2021;15:783056. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 23. | Yang NN, Lin LL, Li YJ, Li HP, Cao Y, Tan CX, Hao XW, Ma SM, Wang L, Liu CZ. Potential Mechanisms and Clinical Effectiveness of Acupuncture in Depression. Curr Neuropharmacol. 2022;20:738-750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 87] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 24. | Chan YY, Lo WY, Yang SN, Chen YH, Lin JG. The benefit of combined acupuncture and antidepressant medication for depression: A systematic review and meta-analysis. J Affect Disord. 2015;176:106-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 104] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 25. | Zahrai A, Vahid-Ansari F, Daigle M, Albert PR. Fluoxetine-induced recovery of serotonin and norepinephrine projections in a mouse model of post-stroke depression. Transl Psychiatry. 2020;10:334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 26. | Jay TM, Rocher C, Hotte M, Naudon L, Gurden H, Spedding M. Plasticity at hippocampal to prefrontal cortex synapses is impaired by loss of dopamine and stress: importance for psychiatric diseases. Neurotox Res. 2004;6:233-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 102] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 27. | Millan MJ. The role of monoamines in the actions of established and "novel" antidepressant agents: a critical review. Eur J Pharmacol. 2004;500:371-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 198] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 28. | Wang C, Wu C, Yan Z, Cheng X. Ameliorative effect of Xiaoyao-jieyu-san on post-stroke depression and its potential mechanisms. J Nat Med. 2019;73:76-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 29. | Baek JY, Trinh TA, Huh W, Song JH, Kim HY, Lim J, Kim J, Choi HJ, Kim TH, Kang KS. Electro-Acupuncture Alleviates Cisplatin-Induced Anorexia in Rats by Modulating Ghrelin and Monoamine Neurotransmitters. Biomolecules. 2019;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 30. | Liu Z, Niu W, Yang X, Wang Y. Effects of combined acupuncture and eugenol on learning-memory ability and antioxidation system of hippocampus in Alzheimer disease rats via olfactory system stimulation. J Tradit Chin Med. 2013;33:399-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/