Published online Nov 19, 2023. doi: 10.5498/wjp.v13.i11.903
Peer-review started: August 18, 2023
First decision: September 14, 2023
Revised: September 28, 2023
Accepted: October 16, 2023
Article in press: October 16, 2023
Published online: November 19, 2023
Processing time: 91 Days and 5.9 Hours
The degree of psychological stress and the difficulty and efficacy of laparoscopic surgery differ in patients with pelvic abscesses after different durations of anti-infection treatment.
To compare and analyse the effects of different durations of anti-infective therapy on patients’ preoperative psychological stress level and the clinical efficacy of laparoscopic surgery in patients with pelvic abscesses to offer a reference for the selection of therapy plans.
A total of 100 patients with pelvic abscesses who were admitted to the Department of Gynecology of Suzhou Ninth Hospital affiliated to Soochow University (Suzhou Ninth People's Hospital) from January 2018 to December 2022 were retrospectively enrolled. According to the different durations of anti-infective therapy, they were divided into Group S (50 patients, received anti-infective therapy for 24-48 h) and Group L (50 patients, received anti-infective therapy for 48-96 h). Baseline data, state-trait anxiety score at admission and before surgery, self-rating anxiety scale (SAS) + self-rating depression scale (SDS) score, surgery time, adhesion grading score, intraoperative blood loss, presence or absence of intraoperative intestinal injury, ureteral injury or bladder injury, postoperative body temperature, length of hospital stay, and presence or absence of recurrence within 3 mo after surgery, chronic pelvic pain, incision infection, dysmenorrhea, menstrual disorder or intestinal obstruction were compared between the S group and the L group.
There was no significant difference in the background data between the S group and the L group (P < 0.05). There was no significant difference in the state-trait anxiety score or SAS + SDS score between the S group and the L group on admission (P < 0.05). The state-trait anxiety score and SAS + SDS score of the S group were lower than those of Group L after receiving different durations of anti-infective therapy (P < 0.05). There was no significant difference in the incidence of intestinal, ureteral or bladder injury between the S group and the L group (P < 0.05). The surgery time of Group S was shorter than that of Group L, and the adhesion score and intraoperative blood loss volume were lower than those of Group L (P < 0.05). There was no significant difference in the incidence of incision infection, dysmenorrhea, menstrual disorder or intestinal obstruction between the S group and the L group (P < 0.05). The postoperative body temperature of Group S was lower than that of Group L (P < 0.05), and the hospital stay was shorter than that of Group L (P < 0.05). The incidences of recurrence and chronic pelvic pain within 3 mo after surgery were lower than that of Group L (P < 0.05).
Twenty-four to forty-eight hours of anti-infective therapy is better than 48-96 h of anti-infective therapy for patients with pelvic abscesses because the degree of psychological stress is lower, which is more conducive to achieving better outcomes after laparoscopic surgery.
Core Tip: A pelvic abscess is a typical manifestation of pelvic inflammatory disease that can endanger the patient's life in severe cases. Here, we analysed the data of 100 patients with pelvic abscesses and divided them into Group S (anti-infective treatment for 24-48 h) and Group L (anti-infective treatment for 48-96 h) according to different durations of anti-infection. Through statistical analysis of the data of the two groups of patients, the authors researched the effects of different durations of preoperative anti-infective therapy on the psychological stress of patients and the postoperative effects of laparoscopic surgery in China to select the optimal duration of anti-infective therapy.
- Citation: Zhang RR, Zhang L, Zhao RH. Anti-infective therapy durations predict psychological stress and laparoscopic surgery quality in pelvic abscess patients. World J Psychiatry 2023; 13(11): 903-911
- URL: https://www.wjgnet.com/2220-3206/full/v13/i11/903.htm
- DOI: https://dx.doi.org/10.5498/wjp.v13.i11.903
One of the most common serious infections in nonpregnant women of childbearing age is pelvic inflammatory disease (PID)[1]. PID is caused by mixed microbial infections of the upper reproductive tract, predominantly affects sexually active young women, and may be asymptomatic or present with tubuloovarian abscesses, which may be life threatening[2]. One of the most prevalent types of pelvic abscesses in women of childbearing age is tubo-ovarian abscesses. The best therapy for pelvic abscesses should be safe, effective, economical, minimally invasive, and have minimal effect on female fertility. Salpingo-ovarian abscesses have traditionally been treated with broad-spectrum antibiotics[3]. Long-term conservative therapy with drugs and long-term repeated use of antibiotics often lead to chronic pelvic abscesses or secondary adhesion, which decreases the patient's fertility, causes chronic pelvic pain, and seriously affects quality of life. Surgical intervention is required for patients who fail to receive conservative therapy. Except for a few patients with low-lying abscesses and a palpable posterior fornical incision and drainage tube, surgery has replaced conservative drug therapy and has become the first choice for the treatment of pelvic abscesses. Laparoscopic surgery has less biological impact on the body but a stronger protective effect on the immunity of the body, thereby reducing the incidence of infectious complications[4,5]. Preoperative anti-infective therapy can limit lesion development, prevent the spread of inflammation, and improve the efficacy of surgery. However, clinical observation shows that different durations of anti-infective therapy have different effects on surgery and postoperative outcomes. In our study, the data of 100 patients with pelvic abscesses who were admitted to our hospital in recent years were collected, and the differences in the outcomes of anti-infective therapy administered preoperatively, intraoperatively or postoperatively for different durations in patients with pelvic abscesses were analysed to find a more appropriate duration of anti-infective therapy.
Data from a total of 100 patients with pelvic abscesses who were admitted to our hospital from January 2018 to December 2022 were retrospectively collected. According to different durations of anti-infective therapy, they were divided into Group S and Group L. Group S was treated with anti-infective therapy for 24-48 h, and Group L was treated with anti-infective therapy for 48-96 h. There were 50 patients in Group S and 50 patients in Group L.
Inclusion criteria: (1) Patients with pelvic abscesses that were diagnosed by symptoms, physical examination, ultrasound, routine blood examination and vaginal fornix puncture; (2) Patients undergoing elective laparoscopic surgery who were treated with sulperazon plus ornidazole for anti-infection treatment before surgery; (3) Patients who received anti-infective therapy and were evaluated with the state-trait anxiety[6], self-rating anxiety scale (SAS) and self-rating depression scale (SDS) scales[7]; and (4) Patients with complete data.
The exclusion criteria were as follows: (1) Patients with blood diseases or infectious diseases, who were pregnant or lactating, or with mental disorders or severe organ failure; (2) Patients with ruptured pelvic abscesses or who received other antibiotics before antibiotic therapy; and (3) Patients who refused to participate or had family members who were not supportive.
Patients and their relatives understood the content of our study and signed informed consent forms.
After the patients were diagnosed with pelvic effusion by examination, the Group S and the Group L were treated with sulperazon combined with ornidazole for anti-infective therapy; that is, according to the results of germ culture and drug sensitivity tests of puncture fluid, the patients were given 3.0 g sulperazon (H20020597; Pfizer Pharmaceuticals Co., LTD) and 0.25 g ornidazole (Hunan Jiudian Pharmaceutical Co., LTD). Both drugs were administered by intravenous drip twice every 24 h. Group S received 24-48 h of anti-infective therapy, while Group L received 48-96 h of anti-infective therapy. State-trait anxiety and SAS + SDS scores were obtained from both groups before and after admission.
After anti-infective therapy, laparoscopic surgery was performed in both groups. After general anaesthesia, the patient was intubated and mechanically ventilated to assist respiration, and the patient was placed in the head-down and bladder lithotomy position. After routine skin disinfection and skin draping, a 1 cm curved incision was made below the umbilical margin of the patient, and CO2 pneumothorax was established with a pressure range of 10-12 mmHg. The laparoscope was placed in the abdomen, and surgery holes of 1 cm and 0.5 cm in size were cut at the left and right McHolley points of the lower abdomen, respectively. The exposed abscesses were incised, and pus and fragments were aspirated with an aspirator and sent to the laboratory. The surgical scope should be determined according to the patient's fertility requirements and the extent of the lesion and adjusted according to the patient's situation and needs. Patients with fertility requirements should undergo salpingostomy. After the surgery, normal saline and metronidazole solution were used to wash the pelvic cavity repeatedly, the patient's position was adjusted to head up and foot down, and the pelvic cavity was washed again. If the abscesses involved the fallopian tube, they were removed by bipolar coagulation, and haemostasis was performed. After abscess removal, the pelvis was flushed with 250 mL of 0.5% metronidazole solution, and a pelvic drainage tube was placed. According to the results of the germ culture and drug sensitivity test of abscess secretion, the corresponding antibiotics were given after the surgery. The body temperature was maintained at the normal level for 24 h. Then, oral antibiotics were administered for 1 to 2 wk.
(1) The psychological stress of the patients in Group S and Group L was investigated by the scale at admission and before surgery. The state-trait anxiety score includes two parts: State anxiety (S-AI) and trait anxiety (T-AI). Each item is scored from 1 to 4 points, with positive emotions scored in reverse order. The total score of the S-AI and T-AI is 20 to 80 points. The higher the score, the higher the anxiety level. The SAS and SDS compiled by Zung[8,9] (the SAS/SDS self-rating scale includes 20 items, and each item is scored from 1 to 4; the higher the score, the greater the degree of psychological stress) were used to evaluate the patients; (2) Surgery time, adhesion score (the modified classification standard of adhesion of the American Society for Reproductive Medicine in 1996[10] was used to evaluate the extent, degree and nature of the adhesion during surgery), intraoperative blood loss, the presence or absence of intraoperative intestinal, ureteral and bladder injuries; and (3) Postoperative body temperature, length of hospital stay, and the presence or absence of recurrence within 3 mo after the surgery, chronic pelvic pain, incision infection, dysmenorrhea, menstrual disorder, or intestinal obstruction.
SPSS 26.0 was used for statistical analysis. Measurement data are expressed as the mean ± SD, and a t test was used. Count data are expressed as a percentage (%), the χ2 test was used, and P < 0.05 was regarded as statistically significant.
There was no significant difference in age, sex, body temperature, mass diameter or reproductive history between Group S and Group L (P > 0.05). As shown in Table 1.
| Baseline data | Group S (n = 50) | Group L (n = 50) | t/χ2 | P value |
| Age (mean ± SD) | 32.2 ± 4.1 | 33.9 ± 5.3 | 1.794 | 0.076 |
| Duration disease (mo, mean ± SD) | 14.7 ± 3.2 | 15.4 ± 2.9 | 1.146 | 0.255 |
| Body temperature (°C, mean ± SD) | 37.5 ± 1.5 | 37.7 ± 1.3 | 0.713 | 0.478 |
| Diameter of mass (cm, mean ± SD) | 5.9 ± 1.9 | 6.3 ± 1.6 | 1.139 | 0.258 |
| Reproductive history [n (%)] | 46 (82) | 43 (86) | 0.919 | 0.338 |
There was no significant difference in the state-trait anxiety score or SAS + SDS score between the Group S and the Group L at admission (P > 0.05). The state-trait anxiety score and SAS + SDS score of Group S were significantly lower than those of Group L after 24-48 h and 48-96 h of anti-infective therapy (P < 0.05) (Figure 1).
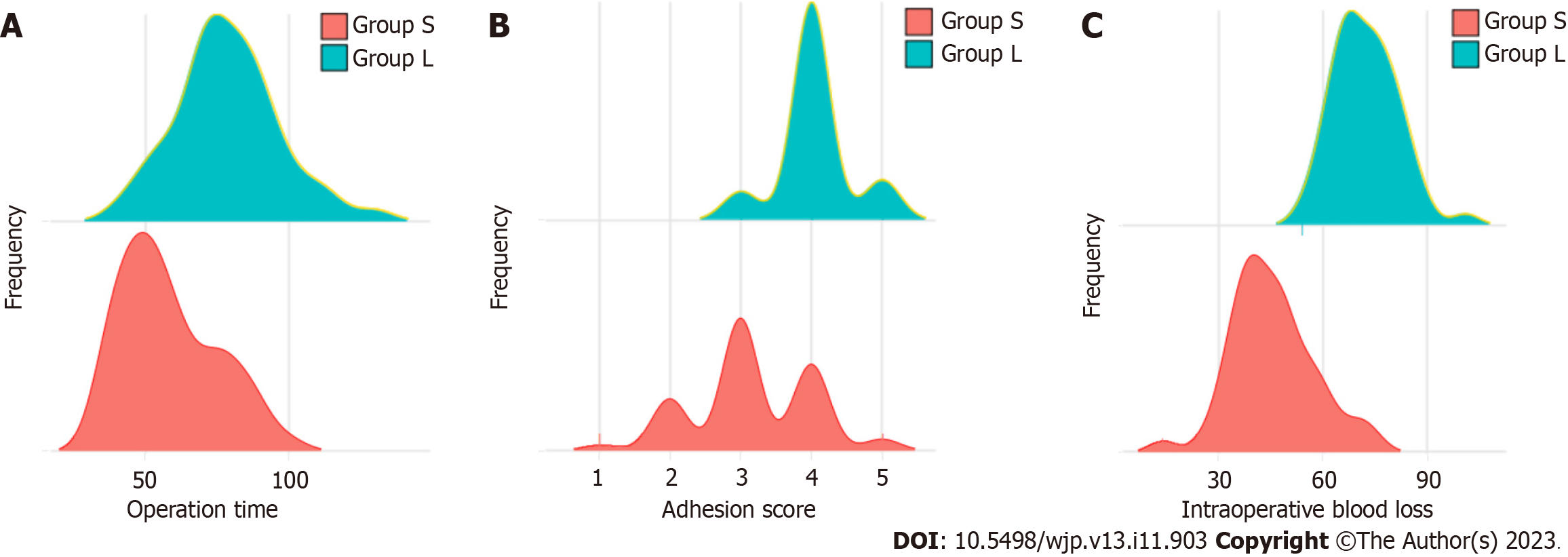
There was no significant difference in the incidence of intestinal, ureteral and bladder injuries between the Group S and the Group L (P > 0.05). The surgery time of Group S was shorter than that of Group L, and the adhesion score and intraoperative blood loss were lower than those of Group L (P < 0.05). As shown in Table 2 and Figure 2.
| Clinical indicators | Group S (n = 50) | Group L (n = 50) | t/χ2 | P value |
| Surgery time (min) | 55.45 ± 16.48 | 78.78 ± 17.87 | 2.714 | < 0.01 |
| Adhesion score | 3.17 ± 0.84 | 4.04 ± 0.49 | 6.326 | < 0.001 |
| Intraoperative blood loss (mL) | 45.54 ± 11.94 | 72.15 ± 9.21 | 12.48 | < 0.001 |
| Intraoperative intestinal injury | 1 (2.00) | 3 (6.00) | 1.042 | 0.307 |
| Intraoperative ureteral injury | 2 (4.00) | 6 (8.00) | 2.174 | 0.140 |
| Intraoperative bladder injury | 0 (0.00) | 2 (4.00) | 2.041 | 0.153 |
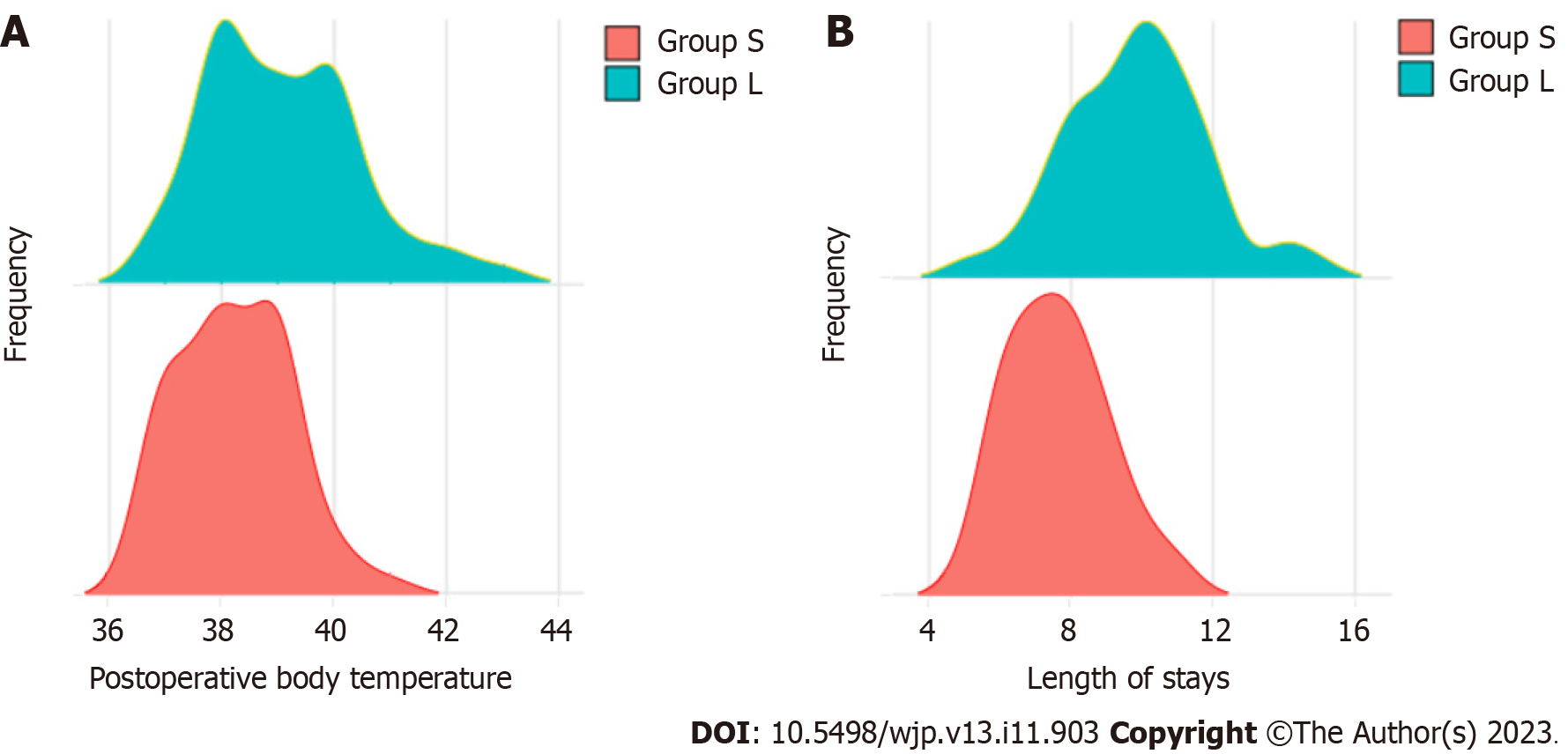
There was no significant difference in the incidence of postoperative incision infection, dysmenorrhea, menstrual disorder, or intestinal obstruction between the Group S and the Group L after different durations of anti-infective therapy (P > 0.05). Postoperative body temperature was lower in Group S after 24-48 h of anti-infective therapy than in Group L after 48-96 h of anti-infective therapy (P < 0.05), and the hospital stay was shorter than that of Group L (P < 0.05) (Figure 3). The incidences of recurrence and chronic pelvic pain within 3 mo after surgery in Group S were lower (P < 0.05) than that in Group L (Table 3).
| Indicators | Group S (n = 50) | Group L (n = 50) | t/χ2 | P value |
| Postoperative body temperature | 38.02 ± 0.98 | 38.94 ± 1.37 | 3.862 | < 0.001 |
| Length of stay (d) | 7.68 ± 1.41 | 9.94 ± 2.01 | 6.509 | < 0.001 |
| Tumour recurrence within 3 mo after surgery | 1 (2.00) | 8 (6.00) | 5.983 | 0.014 |
| Chronic pelvic pain | 2 (12.00) | 12 (20.00) | 8.306 | 0.004 |
| Incision infection | 0 (0.00) | 3 (6.00) | 3.093 | 0.079 |
| Dysmenorrhea | 5 (10.00) | 11 (22.00) | 2.679 | 0.102 |
| Menstrual disorders | 2 (4.00) | 4 (8.00) | 0.709 | 0.4 |
| Intestinal obstruction | 0 (0.00) | 1 (2.00) | 1.01 | 0.315 |
In the past, pelvic abscesses were often treated with conservative drug therapy[11], that is, long-term repeated use of antibiotics, because antibiotic therapy alone was not only ineffective in achieving a complete cure but could also cause the disease to develop into chronic PID or chronic pelvic abscesses, leading to secondary pelvic adhesion[12]. Therefore, surgery gradually replaced conservative therapy to become the main therapy method. In laparoscopic surgery, the advantages are the small incision, sufficient surgical field, no unnecessary interference, no exposure of abdominal organs to the air, less interference with the pelvic environment, less intraoperative blood loss, and fewer complications[13]. However, a pelvic abscess is an inflammatory reaction caused by a pathogenic bacterial infection. If surgical therapy is carried out directly after diagnosis, it is easy for inflammation to spread and affect the surgical outcome. Preoperative anti-infective therapy can control the spread of systemic inflammation, relieve pelvic abscesses, and facilitate a smooth course of surgery. However, there is no consensus on the optimal duration of preoperative anti-infective therapy.
In our study, the incidences of intraoperative injury and postoperative complications in Group S were lower than that in Group L, but the difference was not statistically significant, which may be related to the small sample size and individual differences between patients. However, the state-trait anxiety score and SAS + SDS score of Group S were statistically lower than those of Group L (P < 0.05), indicating that patients who received 24-48 h of anti-infective therapy had less preoperative psychological stress than those who received 48-96 h of anti-infective therapy. This may be because a long duration of preoperative anti-infective therapy diminishes patients' expectations for surgery or because patients have a misunderstanding of their illness. Stevens et al[14] showed that the higher the patients' preoperative expectations for surgery, the higher their depression and anxiety scores. Therefore, we speculated that with a prolonged anti-infection treatment time, patients' expectations of the operation effect increased, and they were more likely to have anxiety, depression and other psychological conditions. The study by Kılıç et al[15] showed that the longer the treatment time, the heavier the patients’ psychological burden. According to this, we believe that a longer period of anti-infection treatment may make patients with pelvic abscesses think that preoperative preparation is not sufficient, their physical weakness cannot withstand the surgical trauma, or their disease will be suddenly worsened, thus causing them to experience worry, anxiety, depression and other adverse emotions. Therefore, we suggest that surgeons pay attention to patients who have undergone anti-infection treatment for an extended period before surgery or have anxiety and depression to be able to provide certain preoperative psychological education if necessary. However, after reviewing a large number of studies, we did not find any correlation between preoperative anti-infective treatment time and preoperative psychological state in patients with pelvic abscesses. Therefore, the specific relationship between preoperative anti-infective treatment time, psychological stress effect and surgical effect in patients with pelvic abscesses needs to be further investigated.
After 24-48 h of anti-infective therapy, the surgery time, adhesion score, intraoperative blood loss volume, postoperative body temperature was significantly lower and the hospital stay was significantly shorter in Group S than those in Group L (P < 0.05), indicating that compared with 24-48 h of anti-infective therapy, long-term anti-infective therapy is more likely to produce abdominopelvic adhesion[16]. Adhesions occur in 60% to 90% of gynaecological patients after abdominal pelvic surgery[17], and fibrous connections connecting tissue surfaces at abnormal locations can lead to chronic pelvic pain, infertility, intestinal obstruction, and the need for a complex reoperation[18-20]. In addition, it was found that in patients with long-term anti-infective therapy who underwent laparoscopic surgery, the abdominopelvic adhesion was more serious, the adhesion range was large, and the adhesion was dense, making it difficult to separate and a hindrance to surgery. The reason may be that 24-48 h after anti-infective therapy, the pelvic lesions are mainly composed of inflammatory exudate, and the membranoid adhesion is loose and easy to separate, which is more conducive to the surgery and thus to the postoperative effect. After 48-96 h of anti-infective therapy, inflammatory exudate on the surface of various organs of the patient's body can organize to form fibrin-like adhesion bands. Inflammatory exudates and tissue adhesions with increased density are hindrances to surgery and increase the incidence of postoperative complications. In addition, according to the above findings, we speculate that a smooth course of laparoscopic surgery and its increased efficacy after 24-48 h of anti-infective treatment may be related to the lower degree of psychological stress of patients before surgery. Ki et al[21] showed that compared with patients without anxiety before surgery, patients with anxiety before surgery had worse postoperative recovery quality. The researchers noted that anxiety before surgery can affect the quality of physical and mental recovery after surgery. In addition, Park et al[22] confirmed that anxiety and depression had a negative impact on the clinical outcome of rotator cuff repair. For the results of this study, we believe that a short period of anti-infection treatment before surgery can reduce the degree of psychological stress of patients before surgery and relieve anxiety and depression to promote a smooth operation and improve its curative effect. However, our views are limited to the research centre and the study population, thus it is necessary to expand the research scope to enhance the reliability of the results of this study.
The data showed that in addition to pelvic pain and incision infection, there were complications such as injury to the surrounding organs in the Group S and the Group L after the surgery, and the incidence of dysmenorrhea was higher, which was mainly related to the difficulty of separation of a thick-walled abscess or the difficulty of removing inflammatory exudates on the surface of organs[23,24]. In addition, surgery may also be one of the reasons for a high incidence of complications. Laparoscopic operators should be aware of potential complications and how to prevent them, strictly adhere to the surgical indications during therapy and learn how to identify complications early to deal with them safely and effectively. In cases of difficult surgery, experienced surgeons are better suited to operate[25,26].
However, our study still has some limitations: (1) The patient data were collected from a single centre, making extrapolation difficult; (2) it is a retrospective study, and the results of our study can only offer recommendations, thus future prospective studies are needed to verify the research findings; and (3) The sample size was small, and there was considerable bias, so a large sample study is still needed to verify the conclusion.
Compared with 48-92 h, 24-48 h of anti-infective therapy followed by laparoscopic surgery for pelvic abscesses is associated with less psychological stress in patients, is more conducive to surgery, and increases surgical efficacy.
Pelvic abscess is a serious pelvic inflammatory disease (PID). It can be caused by a variety of factors, including surgery (e.g., low anterior resection), pelvic visceral perforation, diverticulitis, appendicitis, ischaemic colitis, inflammatory bowel disease, or PID.
Different durations of anti-infective therapy have different effects on patients' psychological state, the difficulty of laparoscopic surgery and surgical efficacy.
The aim of this study was to determine the optimal duration of preoperative anti-infective therapy in patients with pelvic abscesses.
This study retrospectively analysed the differences in preoperative psychological stress, intraoperative operation difficulty and postoperative recovery of patients with pelvic abscesses after different durations of anti-infection treatment.
Among the 100 patients with pelvic abscesses, the patients who received 24-48 h of anti-infection treatment had less preoperative psychological stress, less intraoperative operation difficulty and better postoperative recovery than those who received 48-96 h of anti-infection treatment.
Through observation, we put forward the theory that 24-48 h of anti-infection treatment is better than 48-96 h of anti-infection treatment for patients with pelvic abscesses undergoing laparoscopic surgery.
The different effects of anti-infection treatment on patients’ preoperative psychological stress and the difficulty and efficacy of laparoscopic surgery in patients with pelvic abscesses were observed.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hammam N, Canada; Mahdavi-Roshan M, Iran S-Editor: Lin C L-Editor: A P-Editor: Guo X
| 1. | Jaiyeoba O, Lazenby G, Soper DE. Recommendations and rationale for the treatment of pelvic inflammatory disease. Expert Rev Anti Infect Ther. 2011;9:61-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Gradison M. Pelvic inflammatory disease. Am Fam Physician. 2012;85:791-796. [PubMed] |
| 3. | Granberg S, Gjelland K, Ekerhovd E. The management of pelvic abscess. Best Pract Res Clin Obstet Gynaecol. 2009;23:667-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 103] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 4. | Kwon SY, Brown S, Hibbeln J, Freed JS. Conservative management of pelvic abscess following sacrocolpopexy: a report of three cases and review of the literature. Int Urogynecol J. 2017;28:875-879. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Targarona EM, Balagué C, Knook MM, Trías M. Laparoscopic surgery and surgical infection. Br J Surg. 2000;87:536-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 74] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res (Hoboken). 2011;63 Suppl 11:S467-S472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 846] [Cited by in RCA: 1142] [Article Influence: 81.6] [Reference Citation Analysis (0)] |
| 7. | Shafer AB. Meta-analysis of the factor structures of four depression questionnaires: Beck, CES-D, Hamilton, and Zung. J Clin Psychol. 2006;62:123-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 502] [Cited by in RCA: 565] [Article Influence: 26.9] [Reference Citation Analysis (0)] |
| 8. | Zung WW. A SELF-RATING DEPRESSION SCALE. Arch Gen Psychiatry. 12:63-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5900] [Cited by in RCA: 6261] [Article Influence: 208.7] [Reference Citation Analysis (0)] |
| 9. | Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2251] [Cited by in RCA: 2929] [Article Influence: 53.3] [Reference Citation Analysis (1)] |
| 10. | Johnson NP, Hummelshoj L, Adamson GD, Keckstein J, Taylor HS, Abrao MS, Bush D, Kiesel L, Tamimi R, Sharpe-Timms KL, Rombauts L, Giudice LC; World Endometriosis Society Sao Paulo Consortium. World Endometriosis Society consensus on the classification of endometriosis. Hum Reprod. 2017;32:315-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 522] [Cited by in RCA: 418] [Article Influence: 46.4] [Reference Citation Analysis (0)] |
| 11. | Holt B, Varadarajulu S. Endoscopic ultrasound-guided pelvic abscess drainage (with video). J Hepatobiliary Pancreat Sci. 2015;22:12-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Poincloux L, Caillol F, Allimant C, Bories E, Pesenti C, Mulliez A, Faure F, Rouquette O, Dapoigny M, Abergel A, Giovannini M. Long-term outcome of endoscopic ultrasound-guided pelvic abscess drainage: a two-center series. Endoscopy. 2017;49:484-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 13. | Shigemi D, Matsui H, Fushimi K, Yasunaga H. Laparoscopic Compared With Open Surgery for Severe Pelvic Inflammatory Disease and Tubo-Ovarian Abscess. Obstet Gynecol. 2019;133:1224-1230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Stevens KN, Nadarajah V, Jauregui JJ, Song X, Medina SH, Smuda MP, Packer JD, Henn RF 3rd. Preoperative Expectations of Patients Undergoing Knee Surgery. J Knee Surg. 2021;34:612-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 15. | Kılıç G, Kılıç E, Tekeoğlu İ, Sargın B, Cengiz G, Balta NC, Alkan H, Kasman SA, Şahin N, Orhan K, Gezer İA, Keskin D, Mülkoğlu C, Reşorlu H, Ataman Ş, Bal A, Duruöz MT, Küçükakkaş O, Şen N, Toprak M, Yurdakul OV, Melikoğlu MA, Ayhan FF, Baykul M, Bodur H, Çalış M, Çapkın E, Devrimsel G, Hizmetli S, Kamanlı A, Keskin Y, Ecesoy H, Kutluk Ö, Şendur ÖF, Tolu S, Tuncer T, Nas K. Beyond expectations: disease duration and psychological burden in psoriatic arthritis. Rheumatol Int. 2023;43:1695-1704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Chappell CA, Wiesenfeld HC. Pathogenesis, diagnosis, and management of severe pelvic inflammatory disease and tuboovarian abscess. Clin Obstet Gynecol. 2012;55:893-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 17. | Lang J, Ma D, Xiang Y, Hua K, Liu K, Pan L, Wang P, Yao S, Zhao F, Cheng W, Cui M, Guo H, Guo R, Hong L, Li P, Liu M, Meng Y, Wang H, Wang J, Wang W, Wu M, Yang X, Zhang J. Chinese expert consensus on the prevention of abdominal pelvic adhesions after gynecological tumor surgeries. Ann Transl Med. 2020;8:79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Al-Jabri S, Tulandi T. Management and prevention of pelvic adhesions. Semin Reprod Med. 2011;29:130-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Tulandi T, Al-Shahrani A. Adhesion prevention in gynecologic surgery. Curr Opin Obstet Gynecol. 2005;17:395-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Al-Took S, Platt R, Tulandi T. Adhesion-related small-bowel obstruction after gynecologic operations. Am J Obstet Gynecol. 1999;180:313-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 106] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 21. | Ki M, Kim DC, You SW, Oh J, Jang J, Yoo HH. Appropriateness of the anxiety subscale of the Hospital Anxiety and Depression Scale for Koreans to measure preoperative anxiety and the effect of preoperative anxiety on postoperative quality of recovery. Anesth Pain Med (Seoul). 2023;18:260-269. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Park JH, Rhee SM, Kim HS, Oh JH. Effects of Anxiety and Depression Measured via the Hospital Anxiety and Depression Scale on Early Pain and Range of Motion After Rotator Cuff Repair. Am J Sports Med. 2021;49:314-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 23. | Li TC, Saravelos H, Richmond M, Cooke ID. Complications of laparoscopic pelvic surgery: recognition, management and prevention. Hum Reprod Update. 1997;3:505-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Dumitrașcu MC, Nenciu CG, Nenciu AE, Călinoiu A, Neacșu A, Cîrstoiu M, Șandru F. Laparoscopic myomectomy - The importance of surgical techniques. Front Med (Lausanne). 2023;10:1158264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 25. | Dawod E, Nieto JM. Endoscopic ultrasound guided gastrojejunostomy. Transl Gastroenterol Hepatol. 2018;3:93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 26. | Mahadev S, Lee DS. Endoscopic Ultrasound-Guided Drainage of Pelvic Fluid Collections. Gastrointest Endosc Clin N Am. 2017;27:727-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |