Published online Oct 19, 2023. doi: 10.5498/wjp.v13.i10.772
Peer-review started: December 5, 2022
First decision: January 5, 2023
Revised: January 17, 2023
Accepted: March 22, 2023
Article in press: March 22, 2023
Published online: October 19, 2023
Processing time: 310 Days and 8.3 Hours
Medical school is known for its lengthy process, which is both physically and emotionally draining. Students’ mental balance would shrink as they progress in their medical training. A systematic review and meta-analysis reported that the prevalence of depressive symptoms among medical students remained relatively constant at 27.2%.
To assess the prevalence of depressive symptoms among Tunisian medical students and evaluate its associated factors.
This is a descriptive cross-sectional study that was carried out in the second semester of the academic year 2017/2018, between April 2018 and July 2018 among 1138 medical students. Data were collected using a socio-demographic questionnaire and the Beck Depression Inventory-II (BDI-II).
Sixty-four percent (n = 728) of the participants had depressive symptoms, of which 266 (23.4%) met the criteria for mild, 271 (23.8%) for moderate, and 191 (16.8%) for severe depressive symptoms. Female gender, low socio-economic level, smoking habits and history of mental disorder, performing leisure and physical activities, satisfaction toward a career choice, and happiness perception were the main prognostic factors for depression among medical students. Although academic grades may not be considered a prognostic factor, final-year students appeared to be less depressive than their colleagues.
These findings give insight into mental health issues and comorbidities among Tunisian medical students. It is a hopeful request for decision-makers and academic authorities to set serious measures and draw effective interventions to minimize the currency of psychological distress among this subpopulation.
Core Tip: This study aimed to assess the prevalence of depressive symptoms among Tunisian medical students and evaluate its associated factors. This is a descriptive cross-sectional study that was carried out in the second semester of the academic year 2017/2018, between April 2018 and July 2018 among 1138 medical students. Sixty four percent (n = 728) of the participants had depressive symptoms, of which 266 (23.4%) met the criteria for mild, 271 (23.8%) for moderate, and 191 (16.8%) for severe depressive symptoms. Female gender, low socio-economic level, smoking habits and history of mental disorder, performing leisure and physical activities, satisfaction toward career choice, and happiness perception were the main prognostic factors for depression among medical students. Although academic grade may not be considered as a prognostic factor, final year students appeared to be less depressive than their colleagues.
- Citation: Amamou B, Alouani S, Ben Haouala A, Alouani S, Tlili MA, Mhalla A, Zaafrane F, Gaha L. Depression among medical students in Tunisia: Prevalence and associated factors. World J Psychiatry 2023; 13(10): 772-783
- URL: https://www.wjgnet.com/2220-3206/full/v13/i10/772.htm
- DOI: https://dx.doi.org/10.5498/wjp.v13.i10.772
The Global Burden of Diseases, Injuries, and Risk Factors Study 2017 (GBD 2017), conducted between 1990 and 2017 in 195 countries and territories, concluded that more than 264 million people of all ages were depressed[1].
Depression can be long-lasting or recurrent, and standing still impairs an individual’s ability to function in his daily life[2].
Psychological distress among university students has witnessed a considerable rise, becoming a concern for public health authorities around the globe. And among university students, medical students are particularly more vulnerable to psychological distress and morbidity since medical education is reputed for its long process and it is physically and emotionally consuming[3,4].
Rotenstein et al[5] reported in a systematic review and meta-analysis conducted in 2016 that between 1982 and 2015, depressive symptom prevalence remained relatively constant at 27.2% for medical students with no significant difference between preclinical and clinical students.
Even though it is crucial for an educational institution to assess the mental status of its students, only a few Tunisian studies surveyed the currency of depression among medical students.
Within this framework, this study aimed to assess the prevalence of depressive symptoms among medical students in Tunisia and to evaluate its associated factors.
The present study is a descriptive cross-sectional study that was carried out in the second semester of the academic year 2017/2018, between April 2018 and July 2018 (away from exams). We recruited students from the four medical faculties in Tunisia [Faculty of Medicine of Monastir (FMM), Sousse, Tunis, and Sfax].
The minimal sample size required for the study was 322694. It was calculated using the formula: n = μα2 p (1-p)/δ2, where “μα” is the one-sided magnitude of the confidence level (μα = 1.96) and “p” is the expected proportion of the outcome of interest with an assumption of 30% depression among medical students.
Only enrolled medical students from the first year to the fifth year were invited to complete an online survey as a main tool of the study.
To retrieve an adequate sample for the present study, all candidates were invited to complete an anonymous nationwide web-based questionnaire via their student delegate who published the questionnaire in their Facebook group, mentioning the purpose of the study and assuring the confidentiality and anonymity of each answer. The questionnaire was sent with a description of the study. Every person could only answer the questionnaire once.
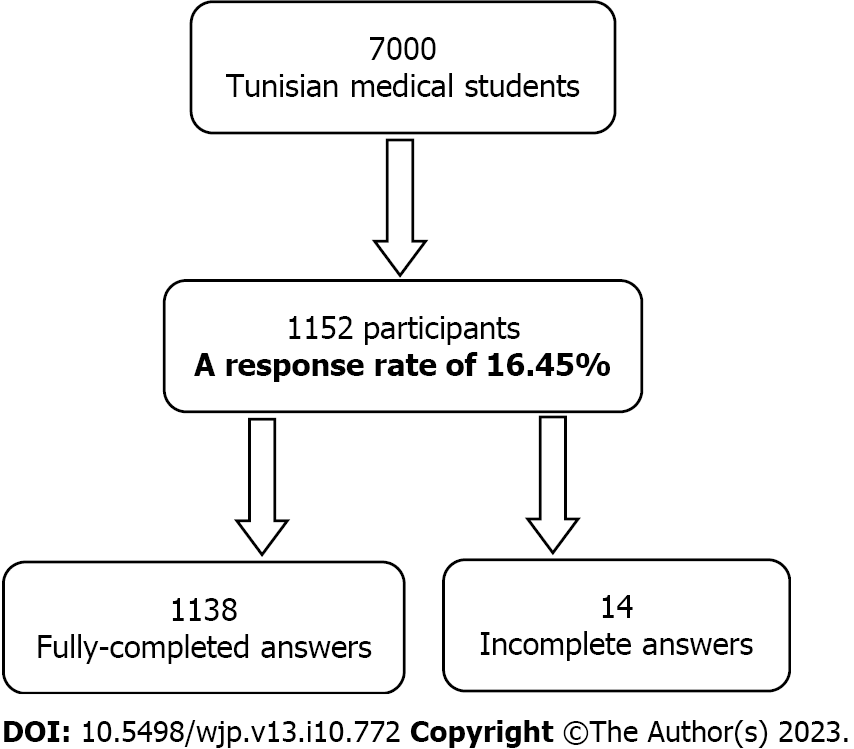
As the response rate is the number of completed and sent survey responses divided by the number of people who viewed the survey, the present study response rate was measured to be 16.45%, considering students who reached the link and viewed the survey content (Figure 1).
The self-report questionnaire employed in the French language (the second language and official language for medical studies in Tunisia) took approximately 15 min to answer and collected data on.
Students’ general characteristics: It consists of personal (age, gender, origin, personal medical history, tobacco use, alcoholism, marital status, self-assessment of their financial status, and current residence) and academic characteristics: Faculty, academic level, satisfaction toward career choice, and dropping out thoughts, leisure and sporting activities, participation in a stress management workshop, and a precedent visit to a psychiatrist/psychologist.
Beck Depression Inventory-II (BDI-II): It is a self-administrated tool, used to screen for the presence of depressive symptoms[6,7]. The BDI-II timeframe extends for 2 wk to correspond with the DSM-IV criteria for diagnosing depressive disorders and includes items measuring cognitive, affective, somatic, and vegetative symptoms of depression. With a sensitivity of 87% and specificity of 79%, the BDI-II was validated using adult and adolescent psychiatric outpatients.
Each participant is asked to answer 21 items rated on a 4-point Linkert scale indicating the degree of severity from 0 (not at all) to 3 (extreme form of each symptom). Cumulative score is calculated. The provisional diagnosis of depression is made if the BDI-II score is greater than 13 and the presence of severe depressive symptoms if the score is greater than or equal to 29. The severity of depression was classified into three categories: Mild, moderate, and severe depression[7,8].
The data collected were keyed into Excel for Windows and statistical analyses were carried out using the software package SPSS version 24 (SPSS Inc.). Descriptive analysis (frequencies, prevalence, mean, and standard deviation) was applied to evaluate the characteristics of the samples. The Chi-square (χ2) test was carried out to compare the prevalence of depression between different groups, while the Student’s t-test was used to analyze quantitative data (age) with the presence of depression. Variables whose P value was < 0.2 were entered as independent variables in regression analysis. The 95% confidence intervals (95%CI) were calculated for prevalence rates. Binary logistic regression models were used to show the predictive model of BDI based on the values of the independent variables (predictors). The level of significance was set at P < 0.05.
We explained the purpose of the study to all participants. The confidentiality and anonymity of each answer were guaranteed. A completed questionnaire was considered as consent to participate in the study. The present study was approved by the ethics committee of the FMM (No. 3067).
The sample consisted of 1138 medical students, including 888 (78%) females and 250 (22%) males, with ages ranging from 18 to 37 years (mean, 22.0 years ± 2.3 years). There were 423 students (37.2%) who were enrolled in the Faculty of Medicine of Tunis (FMT), while 304 (26.7%), 248 (21.8%), and 163 (14.3%) were registered, respectively, in the FMM, Sousse (FMS) and Sfax (FMSF). Of the sample, there were 448 pre-clinical students (Year 1 and Year 2) (39.3%) and 690 clinical students (Year 3, Year 4, and Year 5) (60.6%).
Based on their financial status self-assessment, most of the students (921, 80.9%) were at a moderate socio-economic level while 146 (12.8%) were at a high level and 71 (6.2%) were at a low level. Fourteen percent of the participants were smokers and 16% revealed drinking habits. Almost 70% of the sample did not practice either leisure or physical activities. Only 158 (13.9%) had participated in a stress management workshop and 228 (20%) had sought psychiatric help.
Half of the sample were unsatisfied with their career choice and have thought, at least once, of dropping out of medical studies. Sixty-one percent of participants (699) admitted feeling unhappy. More personal and academically related details are illustrated in Table 1.
| Characteristic | mean ± SD | |
| Age, yr | 22 (2.347) (min 18, max 37) | |
| Gender | Female | 888 (78) |
| Male | 250 (22) | |
| Faculty | Monastir | 304 (26.7) |
| Sousse | 248 (21.8) | |
| Sfax | 163 (14.3) | |
| Tunis | 423 (37.2) | |
| Grade | Year 1 | 252 (22.1) |
| Year 2 | 196 (17.2) | |
| Year 3 | 198 (17.4) | |
| Year 4 | 171 (15) | |
| Year 5 | 321 (28.2) | |
| Marital status | Single | 837 (73.6) |
| Engaged | 269 (23.6) | |
| Married | 29 (2.5) | |
| Divorced | 3 (0.3) | |
| Alone | 193 (17) | |
| With friends/roommates | 220 (19.3) | |
| Academic residency | 127 (11.2) | |
| Family home | 598 (52.5) | |
| Socio-economic level | Low | 71 (6.2) |
| Moderate | 921 (80.9) | |
| High | 146 (12.8) | |
| Children | Yes | 23 (2) |
| No | 1115 (98) | |
| History of medical illness | Yes | 173 (15.2) |
| No | 965 (84.8) | |
| History of mental illness | Yes | 79 (6.9) |
| No | 1059 (93.1) | |
| Leisure activities | Yes | 349 (30.7) |
| No | 789 (69.3) | |
| Physical activities | Yes | 322 (28.3) |
| No | 816 (71.7) | |
| Smoking habits | Yes | 160 (14.1) |
| No | 978 (85.9) | |
| Drinking habits | Yes | 183 (16.1) |
| No | 955 (83.9) | |
| Are you satisfied with your career choice? | Yes | 619 (54.4) |
| No | 519 (45.6) | |
| Have you ever thought of dropping out of medical studies? | Yes | 664 (58.3) |
| No | 474 (41.7) | |
| Stress management training | Yes | 158 (13.9) |
| No | 980 (86.1) | |
| Have you ever visited a psychiatrist? | Yes | 228 (20) |
| No | 910 (80) | |
| Why not? | No answer | 261 (22.9) |
| I feel fine. I don’t need it | 392 (34.4) | |
| I need it, but I am always busy | 366 (23.2) | |
| I need it, but my circle of friends/family discouraged me | 119 (10.5) | |
| Are you happy? | Yes | 439 (38.6) |
| No | 699 (61.4) | |
The BDI-II total scores of participants ranged from 0 to 63 with a mean score of 18.73 ± 10.60 as shown in Table 2. Sixty-four percent (n = 728) of the participants had depressive symptoms, of which 266 (23.4%) met the criteria for mild, 271 (23.8%) for moderate, and 191 (16.8%) for severe depressive symptoms. Among 728 depressive students, only 177 (24.3%) had sought psychiatric help.
| BDI-II total score, mean ± SD | Min 0, max 63, 18.730 (10.654) | |
| Depression level | Absence of depression | 410 (36%) |
| Low | 266 (23.4%) | |
| Moderate | 271 (23.8%) | |
| Severe | 191 (16.8%) | |
Personal characteristics: Female students were more depressed than males. Neither students’ residency nor marital status showed a significant effect on depressive symptoms. Depression was more prevalent among smokers and students with low socio-economic levels.
Depressive symptoms were associated with age (P = 0.048; the age difference was not meaningful), gender (P = 0.038), socio-economic level (P < 10-3), history of medical illness (P = 0.034), history of mental illness (P < 10-3), and smoking habits (P = 0.025).
Academic characteristics: With 70% depressed students, Sousse Faculty of Medicine was ranked as the most depressed faculty. There was no difference between pre-clinical and clinical students. The lack of leisure and physical activities was significantly associated with the presence of depressive symptoms.
The presence of depression was associated with faculty (P = 0.042), leisure activities (P < 10-3), physical activities (P < 10-3), satisfaction toward career choices (P < 10-3), dropping out thoughts (P < 10-3), a precedent visit of a psychiatrist/psychologist (P < 10-3), and happiness perception (P < 10-3). Different correlations are illustrated in Table 3.
| Characteristic | D- | D+ | P value | |
| Age, yr, mean ± SD | 21.820 (2.059) | 22.100 (2.492) | 0.048 | |
| Gender | Female | 306 (34.5) | 582 (65.5) | 0.038 |
| Male | 104 (41.6) | 146 (58.4) | ||
| Faculty | Monastir | 124 (40.8) | 180 (59.2) | 0.042 |
| Sousse | 73 (29.4) | 175 (70.6) | ||
| Sfax | 63 (38.7) | 100 (61.3) | ||
| Tunis | 150 (35.5) | 273 (64.5) | ||
| Grade | Year 1 | 91 (36.1) | 161 (63.9) | 0.57 |
| Year 2 | 72 (36.7) | 124 (63.3) | ||
| Year 3 | 74 (37.4) | 124 (62.6) | ||
| Year 4 | 52 (30.4) | 119 (69.6) | ||
| Year 5 | 121 (37.7) | 200 (62.3) | ||
| Accomodation | Alone | 63 (32.6) | 130 (67.4) | 0.597 |
| With friends/roommates | 79 (35.9) | 141 (64.1) | ||
| Academic residency | 43 (33.9) | 84 (66.1) | ||
| Family home | 225 (37.6) | 373 (62.4) | ||
| Marital status | Single | 301 (36) | 536 (64.0) | 0.786 |
| Engaged | 100 (37.2) | 169 (62.8) | ||
| Married | 8 (27.6) | 21 (72.4) | ||
| Divorced | 1 (33.3) | 2 (66.7) | 0.149 | |
| Children | Yes | 5 (21.7) | 18 (78.3) | |
| No | 405 (36.3) | 710 (63.7) | ||
| Socio-economic level | Low | 9 (12.7) | 62 (87.3) | < 10-3 |
| Moderate | 330 (35.8) | 591 (64.2) | ||
| High | 71 (48.6) | 75 (51.4) | ||
| History of medical illness | Yes | 50 (28.9) | 123 (71.1) | 0.034 |
| No | 360 (37.3) | 605 (62.7) | ||
| History of mental illness | Yes | 14 (17.7) | 65 (82.3) | < 10-3 |
| No | 396 (37.4) | 663 (62.6) | ||
| Leisure activities | Yes | 172 (49.3) | 177 (50.7) | < 10-3 |
| No | 238 (30.2) | 551 (69.8) | ||
| Physical activities | Yes | 145 (45) | 177 (55) | < 10-3 |
| No | 265 (32.5) | 551 (67.5) | ||
| Smoking habits | Yes | 45 (28.1) | 115 (71.9) | 0.025 |
| No | 365 (37.3) | 613 (62.7) | ||
| Drinking habits | Yes | 63 (34.4) | 120 (65.6) | 0.622 |
| No | 347 (36.3) | 608 (63.7) | ||
| Are you satisfied with your career choice? | Yes | 305 (49.3) | 314 (50.7) | < 10-3 |
| No | 105 (20.2) | 414 (79.8) | ||
| Have you ever thought of dropping out of medical studies? | Yes | 167 (25.2) | 497 (74.8) | < 10-3 |
| No | 243 (51.3) | 231 (48.7) | ||
| Stress management training | Yes | 49 (31.0) | 109 (69.0) | 0.157 |
| No | 361 (36.8) | 619 (63.2) | ||
| Have you ever visited a psychiatrist? | Yes | 51 (22.4) | 177 (77.6) | < 10-3 |
| No | 359 (39.5) | 551 (60.5) | ||
| No | ||||
| Are you happy? | Yes | 289 (65.8) | 150 (34.2) | < 10-3 |
| No | 121 (17.3) | 578 (82.7) | ||
Female gender, low socio-economic level, smoking habits, and history of mental disorders were identified to be the main prognostic factors for depression among medical students (Table 4).
| Characteristic | Exp (B) | 95%CI | P value | |
| Gender | 1.544 | 1.135-2.099 | 0.006 | |
| Socio-economic level | High | 1 | ||
| Moderate | 1.83 | 1.276-2.633 | 0.001 | |
| Low | 6.589 | 3.000-14.469 | < 10-3 | |
| History of mental illness | 2.693 | 1.470-4.932 | 0.001 | |
| Smoking habits | 1.669 | 1.123-2.481 | 0.011 | |
| Grade | Year 1 | 1 | ||
| Year 2 | 0.991 | 0.653-1.504 | 0.966 | |
| Year 3 | 0.796 | 0.523-1.213 | 0.288 | |
| Year 4 | 0.918 | 0.584-1.444 | 0.711 | |
| Year 5 | 0.667 | 0.456-0.974 | 0.036 | |
| Leisure activities | 0.459 | 0.344-0.613 | < 10-3 | |
| Physical activities | 0.679 | 0.505-0.914 | 0.011 | |
| Satisfaction toward career choice | 0.238 | 0.179-0.316 | < 10-3 | |
| Stress management training | 1.609 | 1.085-2.385 | 0.018 | |
| Happiness perception | 0.143 | 0.107-0.193 | < 10-3 | |
Although academic grade and participation in a stress management workshop did not show a significant correlation in the univariate analysis, we added these two variables in the regression analysis as they were mentioned in the literature. Academic grade may not be considered a prognostic factor. However, as detailed in Table 4, final-year students seemed to be less depressed than their colleagues.
Performing leisure and physical activities, satisfaction toward a career choice, happiness perception, and participation in a stress management workshop were considered prognostic factors for depression among participants.
Sixty-four percent (n = 728) of the participants had depressive symptoms. These results seem to be higher than the aggregate prevalence of 27.2% (range, 9.3%-55.9%) reported by Rotenstein et al[5] in their systematic review and meta-analysis that covered 195 studies in 47 different countries, involving 129123 medical students. In a medical education journal, a meta-analysis that concerned a total of 62728 medical students pooled across 77 studies was published in March 2016[9], which reported similar results (28%).
The magnitude of depression found in our study closely resembled the findings from some neighboring countries: Egypt 60.2%[10], Bahrain 65.6%[11], etc. Lower prevalence were found in India[12] (18%), Thailand[13] (12.6%), Germany[14] (10.3%), etc.
Nationally, the proportion of depressed medical students was higher than what was reported in a previous Tunisian study[15] that was conducted at the University of Sfax and showed that out of 80 medical students, 31% were depressed. Similar results were found in another study that included Tunisian medical residents (30.5%)[16]. Both studies used the same screening tool (Hospital Anxiety and Depression scale)[15,16].
This variation worldwide can be explained to be due to sample size and data collection tools. Besides, diversity in cultural, religious, and spiritual peculiarities[17] in addition to dissimilarity in the healthcare system might also elucidate the disparity of findings between countries.
Female gender: Globally, there were controverted issues given the impact of gender on depression symptoms. The significant correlation of poor mental health with female students found in the current study is supported by previous studies in Sweden[18], Nepal[19], Australia[20], etc. In contrast, no difference in depression between genders was disclosed in previous studies in Tunisia[16], Greece[21], Ethiopia[22], etc. Furthermore, regression analysis yielded mixed findings with some considering female gender as a risk factor for depression: South Africa[23], Turkey[24], South Korea[25], etc. Studies took a multitude of tracks to elucidate why female students were more prone to depression than their male peers, and they suggested social stigma, gender inequity, and cultural constraints as the main reasons[9,26,27].
Financial status: Based on their financial status self-assessment, students at a low socioeconomic level were more likely to get depressed than their peers. These outcomes are in harmony with those run in neighboring and foreign countries[3,10,14,25,28]. The impact of financial status on the occurrence of depression was documented in numerous studies among general populations[29-32]. A large four-year study (The PATH Through Life Survey) was conducted by Butterworth and colleagues in the city of Canberra and the surrounding regions in south-east Australia, and it included 6715 participants from different cohorts (1975-1979; 1956-1960; and 1937-1941). The study proclaimed that the lack of financial resources was strongly associated with depression[33,34].
Mental problems: Out of 1138 participants, 79 (6.9%) reported having a history of mental illness. These results seem to be akin to those found in other studies[26,35]. Nineteen Saudi Arabian medical students (out of 398) reported having a psychological illness. Eighty-four percent of them met the BDI criteria for depression. The chi-square test detected a significant correlation (P < 0.001) and multiple linear regression inferred that the presence of psychological problems makes students 1.435 times more likely to get depressed [P = 0.03, exp(B) 4.200, 95%CI: 1.150-15.338][35]. These findings are congruous with those reported earlier by Asal et al[36], Pagnin et al[37], and Pillay et al[38], who found that depressive and anxiety features were related to students’ history of poor mental health[36-38].
Smoking, drinking, and substance use: Out of 1138 participants, 160 (14.1%) had smoking habits while 183 (16.1%) had drinking habits. Smokers (115, 71.9%) and drinkers (120, 65.6%) met the BDI-II criteria for depression. The regression analysis considered smoking as a risk factor for depression. Many studies have looked for the link between substance use and the occurrence of depression[39]. On the other hand, Palestinian and Saudi Arabian studies that explored the impact of smoking only (but not drinking for cultural limitations) found no significant correlation with depression (P = 0.08)[26,35]. Moreover, O. Coskun and colleagues[24] perceived no significant relationship between alcohol and the magnitude of depression. Correspondingly, studies among Ethiopian, Nepali, and Australian medical students found, also, no significant link between substance use and the development of depression[19,20,22]. Strikingly, a similar study was performed in the Netherlands. Authors noticed that first-year students who had drinking habits tended to be more balanced in their mental wellness than non-drinking students. Hence, drinking seems to be a coping tool wielded to ease the pressure but also to inflate social interactions and activities[40,41]. Even though drinking can be regarded as a relief from stress or a coping strategy, immoderate drinking may ruin liver and pancreas functioning, alter the cardiovascular system, and lead to tumoral issues as well as numerous psychiatric disorders[41-44].
Physical activities: Almost 70% of the sample did not practice any physical activity. Among them, 551 (67.5%) met the BDI-II criteria for depression. The regression analysis considered physical activity as a protective factor against depression[45].
A tiny number of studies had explored physical behavior among medical students. Abdelwahed and colleagues, for instance, observed that 210 out of 442 were performing physical activity at least three times a week. Yet, statistical analysis did not show any significant correlation between physical activity and depression (P = 0.647), anxiety (P = 0.78), or stress (P = 0.76)[10].
Worldwide, the impact of physical exercises was exemplified in numerous studies. A systematic review on the effects of physical activity on brain structure and function in youth related that physical activity can redesign white matter integrity and arousal of regions key to cognitive tasks[46]. Identically, Rebar and colleagues performed a meta-analysis of the impact of physical activity on depression and anxiety among the non-clinical population[47]. Authors concluded that physical activity was shown to decrease depression by a medium effect [standardized mean difference (SMD) = -0.50; 95%CI: -0.93 to -0.06] and anxiety by a small effect (SMD = -0.38; 95%CI: -0.66 to -0.11)[47].
Leisure activities and extracurricular involvement: More than half of the participants (69.3%) were not performing any leisure activity. Fifty hundred and fifty-one (69.8%) among them were found depressed. Statistical analysis proved a significant association between spare time ventures and the occurrence of depression: The odds of developing depression was reduced to half among socially active participants. These findings seem in line with a Nepalian study where 34% of students (221/651) were involved in extracurricular activities. While those who answered “Always” and “Often” as the frequency of their extra activities were 28.6% and 21.7% depressed, respectively, those who answered “Rarely” and “Never” were 42.4% and 41.7% depressed, respectively. Even though a strong correlation (P < 10-3) was found in the chi-square test, having a spare schedule tends to be a protective factor against anxiety (P = 0.012, OR = 0.367, 95%CI: 0.165-0.799) but not depression[19]. The part taken by social life and social relationships turns out to be a key strand in the fight against depression and lessen stressful life pressures[22,40,48,49]. Dyrbye et al[28], who drove a longitudinal study among 3743 United States medical students from 2010 to 2014, noticed that students who avowed having low social support were more likely to manifest depressive features (P < 10-3). Similarly, Turkish and Palestinian studies substantiated the strong correlation (P < 10-3) that relates social interaction and social stand with the contingency of depression[24,35].
Satisfaction and dropping out ideas: Statistical analysis showed a strong correlation between students’ dissatisfaction and depression (P < 10-3). Unsatisfaction is, then, considered a risk factor for developing depression. These data closely resemble findings from other studies. Pokhrel et al[19] demonstrated that satisfied students in Nepal were less prone to depression (OR = 0.51, 95%CI: 0.33-0.80). Similarly, discontented KSA medical students tend to be more depressed than their peers (P = 0.03)[35]. Studies conducted in New Zealand[50] and Palestine[26] reported results in line with our study. The influence that satisfaction toward career choice has on students’ mental health did not come out of anywhere. It arises from the reluctance to study medicine: Whether to please parents’ desire to become a doctor or to go along with friends aiming to get higher social status. All of it ends by being hushed, knowing the reality of medicine[51].
As disclosed above, medical students are without a doubt prone to several mental afflictions. Therefore, preventing such distress among students should be a priority and a must.
Primary prevention is possible by supplying learners with seminars on time management, relaxation exercises, and mindfulness activities through counseling services such as the listening unit that has been established in our faculty. Finally, prioritizing students’ welfare starts by providing space and needed materials to enhance students’ physical exercises and group activities, delivering variable and healthy meals in university restaurants, and revising students’ schedules to suit their academic, physical, and psychological needs.
Overall, the authors acknowledge some limitations to this study. Being a descriptive cross-sectional study, causal links between the correlations could not be inaugurated. Preferably, further studies should be surveyed in longitudinal, prospective, and multicenter designs aiming to yield a greater overview of the circumstances. Even though the number of students who participated in this survey is much higher than those carried out in Tunisian and neighboring studies, a larger sample size would have risen the diligence and exactness of our study.
As our study was based on self-administrated questionnaires and all data employed were self-reported, it is possible that students could have understated or overstated their depressive symptoms. The choice, itself, of participating in the online survey may mirror some level of bias related to the personal traits and characteristics of the students. We have estimated the occurrence of depression among medical students using a self-reported inventory (BDI-II), there were no clinical assessments supervised by psychiatrists. Consequently, the diagnostic value may be restricted, and further psychiatric interviews are required to validate our results. Other students’ characteristics that were correlated to the development of depressive symptoms were not explored among participants, such as emotional intelligence, coping skills, social support, religious beliefs, personality characteristics, and substance use disorders.
These findings give insight into Tunisian medical students’ mental health issues and comorbidities. It is a hopeful request for decision-makers and academic authorities to take serious measures and offer effective interventions to minimize the currency of psychological distress among this subpopulation. To date, this is the largest study on depression among Tunisian and Maghrebian medical students. Yet, further research is recommended to explore other correlated factors and to evaluate the effectiveness of these measures on depression levels among medical students.
Most medical schools in the world (including Tunisia) still recruit their students based solely on the university entrance exam score. Students’ motivation, though being a crucial conjecture in their academic performance and well-being, has never been conventionally and structurally assessed in Tunisia. As a result, many students simply choose the medical field due to social codes, family influences, and cultural norms.
It is crucial for an educational institution to assess the mental status of students and its associated factors.
To assess the prevalence of depressive symptoms among Tunisian medical students and to evaluate its associated factors.
This is an online survey of students from the four Tunisian medical faculties using Beck’s depression questionnaire.
Sixty-four percent (n = 728) of the participants had depressive symptoms. Female gender, low socioeconomic level, smoking habits and history of mental disorder, performing leisure and physical activities, satisfaction toward a career choice, and happiness perception were the main prognostic factors for depression among medical students.
These findings give insight into mental health issues and comorbidity among Tunisian medical students. It is a hopeful request for decision-makers and academic authorities to take serious measures and offer effective interventions to minimize the currency of psychological distress among this subpopulation.
Further studies are needed to explore other correlated factors (such as emotional intelligence, coping skills, social support, religious beliefs, and personality characteristics) and to evaluate the effectiveness of these measures on depression levels among Tunisian medical students.
| 1. | Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4675] [Cited by in RCA: 4634] [Article Influence: 421.3] [Reference Citation Analysis (0)] |
| 2. | Vilagut G, Forero CG, Barbaglia G, Alonso J. Screening for Depression in the General Population with the Center for Epidemiologic Studies Depression (CES-D): A Systematic Review with Meta-Analysis. PLoS One. 2016;11:e0155431. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 735] [Cited by in RCA: 704] [Article Influence: 70.4] [Reference Citation Analysis (0)] |
| 3. | January J, Madhombiro M, Chipamaunga S, Ray S, Chingono A, Abas M. Prevalence of depression and anxiety among undergraduate university students in low-and middle-income countries: a systematic review protocol. Syst Rev. 2018;7:57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 4. | Mahroon ZA, Borgan SM, Kamel C, Maddison W, Royston M, Donnellan C. Factors Associated with Depression and Anxiety Symptoms Among Medical Students in Bahrain. Acad Psychiatry. 2018;42:31-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 5. | Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, Sen S, Mata DA. Prevalence of Depression, Depressive Symptoms, and Suicidal Ideation Among Medical Students: A Systematic Review and Meta-Analysis. JAMA. 2016;316:2214-2236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1620] [Cited by in RCA: 1467] [Article Influence: 146.7] [Reference Citation Analysis (0)] |
| 6. | Survey Monkey. Free online survey software and questionnaire tool. [cited 3 January 2021]. Available from: https://www.surveymonkey.com/welcome/sem/. |
| 7. | Smarr KL, Keefer AL. Measures of depression and depressive symptoms: Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9). Arthritis Care Res (Hoboken). 2011;63 Suppl 11:S454-S466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 512] [Cited by in RCA: 706] [Article Influence: 47.1] [Reference Citation Analysis (0)] |
| 8. | Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996;67:588-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3738] [Cited by in RCA: 4205] [Article Influence: 140.2] [Reference Citation Analysis (0)] |
| 9. | Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. 2016;50:456-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 316] [Cited by in RCA: 404] [Article Influence: 40.4] [Reference Citation Analysis (1)] |
| 10. | Abdel Wahed WY, Hassan SK. Prevalence and associated factors of stress, anxiety and depression among medical Fayoum University students. Alex J Med. 2017;53:77-84. [RCA] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 129] [Article Influence: 18.4] [Reference Citation Analysis (1)] |
| 11. | Abdelaziz AMY, Alotaibi KT, Alhurayyis JH, Alqahtani TA, Alghamlas AM, Algahtani HM, Jahrami HA. The association between physical symptoms and depression among medical students in Bahrain. Int J Med Educ. 2017;8:423-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Vijayalakshmi P, Thimmaiah R, Gandhi S, BadaMath S. Eating Attitudes, Weight Control Behaviors, Body Image Satisfaction and Depression Level Among Indian Medical and Nursing Undergraduate Students. Community Ment Health J. 2018;54:1266-1273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Angkurawaranon C, Jiraporncharoen W, Sachdev A, Wisetborisut A, Jangiam W, Uaphanthasath R. Predictors of quality of life of medical students and a comparison with quality of life of adult health care workers in Thailand. Springerplus. 2016;5:584. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Wege N, Muth T, Li J, Angerer P. Mental health among currently enrolled medical students in Germany. Public Health. 2016;132:92-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 62] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 15. | Vaysse B, Gignon M, Zerkly S, Ganry O. [Alcohol, tobacco, cannabis, anxiety and depression among second-year medical students. Identify in order to act]. Sante Publique. 2014;26:613-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Marzouk M, Ouanes-Besbes L, Ouanes I, Hammouda Z, Dachraoui F, Abroug F. Prevalence of anxiety and depressive symptoms among medical residents in Tunisia: a cross-sectional survey. BMJ Open. 2018;8:e020655. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Koenig HG. Research on religion, spirituality, and mental health: a review. Can J Psychiatry. 2009;54:283-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 686] [Cited by in RCA: 566] [Article Influence: 33.3] [Reference Citation Analysis (1)] |
| 18. | Dahlin M, Joneborg N, Runeson B. Stress and depression among medical students: a cross-sectional study. Med Educ. 2005;39:594-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 501] [Cited by in RCA: 544] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 19. | Pokhrel NB, Khadayat R, Tulachan P. Depression, anxiety, and burnout among medical students and residents of a medical school in Nepal: a cross-sectional study. BMC Psychiatry. 2020;20:298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 88] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 20. | Bore M, Kelly B, Nair B. Potential predictors of psychological distress and well-being in medical students: a cross-sectional pilot study. Adv Med Educ Pract. 2016;7:125-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 71] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 21. | Nasioudis D, Palaiodimos L, Dagiasis M, Katsarou A, Ntouros E. Depression in military medicine cadets: a cross-sectional study. Mil Med Res. 2015;2:28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Kebede MA, Anbessie B, Ayano G. Prevalence and predictors of depression and anxiety among medical students in Addis Ababa, Ethiopia. Int J Ment Health Syst. 2019;13:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 62] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 23. | Van der Walt S, Mabaso WS, Davids EL, De Vries PJ. The burden of depression and anxiety among medical students in South Africa: A cross-sectional survey at the University of Cape Town. S Afr Med J. 2019;110:69-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 24. | Coskun O, Ocalan AO, Ocbe CB, Semiz HO, Budakoglu I. Depression and hopelessness in pre-clinical medical students. Clin Teach. 2019;16:345-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 25. | Roh MS, Jeon HJ, Kim H, Han SK, Hahm BJ. The prevalence and impact of depression among medical students: a nationwide cross-sectional study in South Korea. Acad Med. 2010;85:1384-1390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 69] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 26. | Shawahna R, Hattab S, Al-Shafei R, Tab’ouni M. Prevalence and factors associated with depressive and anxiety symptoms among Palestinian medical students. BMC Psychiatry. 2020;20:244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 27. | Azad N, Shahid A, Abbas N, Shaheen A, Munir N. Anxiety And Depression In Medical Students Of A Private Medical College. J Ayub Med Coll Abbottabad. 2017;29:123-127. [PubMed] |
| 28. | Dyrbye LN, Wittlin NM, Hardeman RR, Yeazel M, Herrin J, Dovidio JF, Burke SE, Cunningham B, Phelan SM, Shanafelt TD, van Ryn M. A Prognostic Index to Identify the Risk of Developing Depression Symptoms Among U.S. Medical Students Derived From a National, Four-Year Longitudinal Study. Acad Med. 2019;94:217-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 29. | Fryers T, Melzer D, Jenkins R. Social inequalities and the common mental disorders: a systematic review of the evidence. Soc Psychiatry Psychiatr Epidemiol. 2003;38:229-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 372] [Cited by in RCA: 363] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 30. | Kessler RC, Cleary PD. Social class and psychological distress. Am Sociol Rev. 1980;45:463-478. [PubMed] |
| 31. | Muntaner C, Eaton WW, Miech R, O’Campo P. Socioeconomic position and major mental disorders. Epidemiol Rev. 2004;26:53-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 354] [Cited by in RCA: 377] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 32. | Skapinakis P, Weich S, Lewis G, Singleton N, Araya R. Socio-economic position and common mental disorders. Longitudinal study in the general population in the UK. Br J Psychiatry. 2006;189:109-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 88] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 33. | Butterworth P, Rodgers B, Windsor TD. Financial hardship, socio-economic position and depression: results from the PATH Through Life Survey. Soc Sci Med. 2009;69:229-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 183] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 34. | Butterworth P, Cherbuin N, Sachdev P, Anstey KJ. The association between financial hardship and amygdala and hippocampal volumes: results from the PATH through life project. Soc Cogn Affect Neurosci. 2012;7:548-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 75] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 35. | Hamasha AA, Kareem YM, Alghamdi MS, Algarni MS, Alahedib KS, Alharbi FA. Risk indicators of depression among medical, dental, nursing, pharmacology, and other medical science students in Saudi Arabia. Int Rev Psychiatry. 2019;31:646-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (7)] |
| 36. | Asal AR, Abdel-Fattah MM. Prevalence, symptomatology, and risk factors for depression among high school students in Saudi Arabia. Neurosciences (Riyadh). 2007;12:8-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 37. | Pagnin D, de Queiroz V. Influence of burnout and sleep difficulties on the quality of life among medical students. Springerplus. 2015;4:676. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 38. | Pillay N, Ramlall S, Burns JK. Spirituality, depression and quality of life in medical students in KwaZulu-Natal. S Afr J Psychiatr. 2016;22:731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 39. | Masri R, Kadhum M, Farrell SM, Khamees A, Al-Taiar H, Molodynski A. Wellbeing and mental health amongst medical students in Jordan: a descriptive study. Int Rev Psychiatry. 2019;31:619-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 40. | Borst JM, Frings-Dresen MH, Sluiter JK. Prevalence and incidence of mental health problems among Dutch medical students and the study-related and personal risk factors: a longitudinal study. Int J Adolesc Med Health. 2016;28:349-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 41. | Geisner IM, Mallett K, Kilmer JR. An examination of depressive symptoms and drinking patterns in first year college students. Issues Ment Health Nurs. 2012;33:280-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 42. | Archie S, Zangeneh Kazemi A, Akhtar-Danesh N. Concurrent binge drinking and depression among Canadian youth: prevalence, patterns, and suicidality. Alcohol. 2012;46:165-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 43. | Mason WA, Kosterman R, Haggerty KP, Hawkins JD, Redmond C, Spoth RL, Shin C. Dimensions of adolescent alcohol involvement as predictors of young-adult major depression. J Stud Alcohol Drugs. 2008;69:275-285. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 55] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 44. | O’Hara RE, Cooper ML. Bidirectional associations between alcohol use and sexual risk-taking behavior from adolescence into young adulthood. Arch Sex Behav. 2015;44:857-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 45. | Keating XD, Guan J, Piñero JC, Bridges DM. A meta-analysis of college students’ physical activity behaviors. J Am Coll Health. 2005;54:116-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 334] [Cited by in RCA: 313] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 46. | Valkenborghs SR, Noetel M, Hillman CH, Nilsson M, Smith JJ, Ortega FB, Lubans DR. The Impact of Physical Activity on Brain Structure and Function in Youth: A Systematic Review. Pediatrics. 2019;144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 120] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 47. | Rebar AL, Stanton R, Geard D, Short C, Duncan MJ, Vandelanotte C. A meta-meta-analysis of the effect of physical activity on depression and anxiety in non-clinical adult populations. Health Psychol Rev. 2015;9:366-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 466] [Cited by in RCA: 669] [Article Influence: 60.8] [Reference Citation Analysis (0)] |
| 48. | Conijn M, Boersma HJ, van Rhenen W. [Burnout in Dutch medical students: prevalence and causes]. Ned Tijdschr Geneeskd. 2015;159:A8255. [PubMed] |
| 49. | Moak ZB, Agrawal A. The association between perceived interpersonal social support and physical and mental health: results from the National Epidemiological Survey on Alcohol and Related Conditions. J Public Health (Oxf). 2010;32:191-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 137] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 50. | Samaranayake CB, Fernando AT. Satisfaction with life and depression among medical students in Auckland, New Zealand. N Z Med J. 2011;124:12-17. [PubMed] |
| 51. | Karaoglu N, Seker M. Anxiety and depression in medical students related to desire for and expectations from a medical career. West Indian Med J. 2010;59:196-202. [PubMed] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychology
Country/Territory of origin: Tunisia
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Laranjeira C, Portugal; Wang QX, China; Zhang YF, China S-Editor: Chen YL L-Editor: Wang TQ P-Editor: Chen YL