Published online Mar 19, 2022. doi: 10.5498/wjp.v12.i3.536
Peer-review started: November 12, 2021
First decision: December 12, 2021
Revised: January 3, 2022
Accepted: February 23, 2022
Article in press: February 23, 2022
Published online: March 19, 2022
Processing time: 125 Days and 22.1 Hours
Observational studies based on electronic health records (EHR) report an increased risk of neurological/neuropsychiatric sequelae for patients who have had coronavirus disease 2019 (COVID-19). However, these studies may suffer from biases such as unmeasured confounding, residual reverse causality, or lack of precision in EHR-based diagnoses. To rule out these biases, we tested causal links between COVID-19 and different potential neurological/neuropsychiatric sequelae through a two-sample Mendelian randomization analysis of summary statistics from large Genome-Wide Association Scans of susceptibility to COVID-19 and different neurological and neuropsychiatric disorders, including major depression, anxiety, schizophrenia, stroke, Parkinson’s and Alzheimer’s diseases. We found robust evidence suggesting that COVID-19 – notably the hospitalized and most severe forms – carries an increased risk of neuropsychiatric sequelae, particularly Alzheimer’s disease, and to a lesser extent anxiety disorder. In line with a large longitudinal EHR-based study, this evidence was stronger for more severe COVID-19 forms. These results call for a targeted screening strategy to tackle the post-COVID neuropsychiatric pandemic.
Core Tip: Inspired by suggestive findings of an increased incident risk of neurological and neuropsychiatric sequelae in people who have had coronavirus disease 2019 (COVID-19), we carried out a two-sample Mendelian randomization analysis to further investigate causality links and build evidence free of biases such as unmeasured confounding, residual reverse causality or lack of precision in electronic health record-based diagnoses. This analysis – typically applied to genetic associations from large genomic studies on the diseases of interest – indicated that the most severe forms of COVID-19 increased the risk of Alzheimer’s disease and anxiety, further supporting the findings of large observational studies.
- Citation: Tirozzi A, Santonastaso F, de Gaetano G, Iacoviello L, Gialluisi A. Does COVID-19 increase the risk of neuropsychiatric sequelae? Evidence from a mendelian randomization approach. World J Psychiatry 2022; 12(3): 536-540
- URL: https://www.wjgnet.com/2220-3206/full/v12/i3/536.htm
- DOI: https://dx.doi.org/10.5498/wjp.v12.i3.536
During the ongoing coronavirus disease 2019 (COVID-19) pandemic, increasing attention is being paid to the long-term sequelae of the acute disease, particularly neurological and neuropsychiatric[1,2]. A recent retrospective analysis in more than 236000 COVID-19 survivors reported a significant increase of neurological/psychiatric outcomes in the six months after diagnosis, particularly for those treated in hospital, in an intensive care unit, and those who suffered encephalopathy[3]. The risk of first diagnosis of such sequelae, which included dementia, cerebrovascular, psychotic, mood and anxiety disorders, was almost double in those with COVID-19 compared to patients who suffered other types of viral influenza or respiratory infections, suggesting a specific contribution of Sars-CoV-2 infection to these sequelae[3]. This observational study was based on electronic health records, which unavoidably lack the precision of neurological/neuropsychiatric diagnoses, and may be subject to unmeasured confounding or residual reverse causality biases; in fact, most of the reported disorders are themselves risk factors for COVID-19 infection, and their milder forms may go undetected.
To overcome these limitations and provide independent evidence of the observations, we carried out a two-sample Mendelian randomization (MR) analysis to test whether susceptibility to COVID-19 could predispose to an increase in the risk of different psychiatric/neurodegenerative disorders, including major depression, anxiety, schizophrenia, stroke, Parkinson’s and Alzheimer’s diseases, as already suggested in the literature[2,3].
We employed summary statistics from large Genome-Wide Association Studies (GWAS) on COVID-19 susceptibility and all the disorders tested, through the MR-Base web app, or the equivalent R package TwoSampleMR v 0.5.6[4] when up-to-date summary statistics were not available in the MR-Base[5]. Since we detected no violation of the balanced horizontal pleiotropy assumption, we used Inverse variance weighted regression to model the relation between effects on exposure and outcome for each of the genetic instrumental variants (IVs). We selected the variants showing genome-wide significant associations with (COVID-19) exposure[6] (P < 5 × 10-8), removed palindromic variants, applied Linkage Disequilibrium (LD) clumping (r2 cutoff 0.1 and clumping window 1000 kb), and retained only the variants that were also tested in the “outcome” study, resulting in 17-23 variants for each analysis.
MR analyses were repeated, testing variants associated with three different COVID-19 exposures, namely all (112612), hospitalized (24274) and severe cases (8779; namely, patients who required respiratory support, or whose death was related to COVID-19)[6], compared to population controls (> 1 million, see https://www.covid19hg.org/results/r6/).
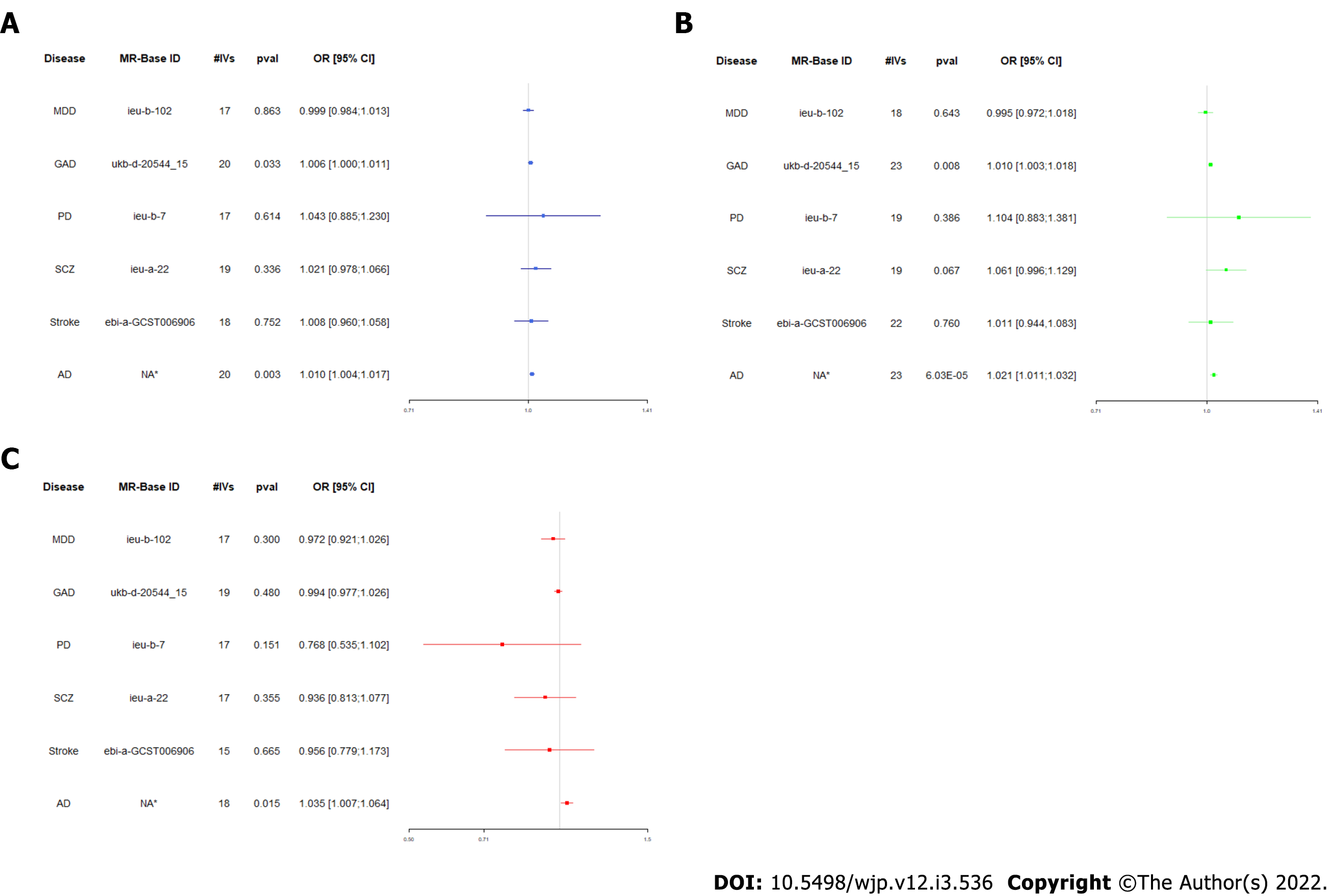
This analysis indicated a significant causal link between severe and hospitalized COVID-19 and the risk of Alzheimer’s disease and anxiety disorder (AD) (Figure 1), which survived Bonferroni correction for six different outcome conditions (α = 8.3 × 10-3).
This evidence is closely aligned with that from a large observational study[3], where patients who were hospitalized and required intensive care had a steeper increase in incident neuropsychiatric sequelae in the six months after infection. However, the increases observed here in Alzheimer (1%-3%) and anxiety risk (0.5%-1%) were considerably smaller than those reported by Taquet et al[3], although measures of incident and prevalent risk and the different design and setting of the studies mean they are not directly comparable. This might be explained by the typically low effect size of the common variants detected in GWAS and used in MR analysis, and by the type of comparison in the original study on COVID-19[6], where population controls can include a number of undetected cases, reducing the power of the comparison.
Our analysis presents some limitations. First, the use of summary statistics from a meta-analysis of diverse ancestries may introduce a population stratification bias. Although no data based only on European samples are available for the COVID-19 GWAS round 6 meta-analysis, we carried out a sensitivity analysis with the round 5 (European) meta-analysis results. This provided significant evidence of causality between hospitalized COVID-19 forms and increased AD risk (by 1.8%, P < 0.05), while only a trend of association was observed for increased AD risk vs the other COVID-19 exposures (Table 1). No significant evidence of causality was found for anxiety, although severe COVID-19 slightly increased the risk of GAD by 0.6% (P = 0.09). Overall, effect sizes between MR analysis using round 6 and round 5 (only EUR) data were very similar, corroborating the bounty of our main analysis. The lack of significance in most of the sensitivity MR analyses may be due to the notably smaller number of IVs used (from 3 to 10), implied by the smaller sample size and lower power of the round 5 meta-analysis. Therefore, caution is suggested in interpreting these data and further analyses are needed based on larger datasets, of European ancestry.
Second, partial sample overlap between the studies analyzed may introduce a type I error inflation bias which, however, does not apply to case-control outcomes when risk factor IVs are tested only in control participants[7]. While we do know the exact prevalence of Alzheimer and anxiety cases in the COVID-19 GWAS, the relatively low prevalence of these disorders in the general population (especially AD) suggests the real bias introduced by sample overlap may be very close to zero.
Last, although converging epidemiological and genetic evidence supports a causal effect of COVID-19 infection on neuropsychiatric/neurodegenerative disorders, the exact molecular mechanisms of this relationship remain to be clarified. The most convincing hypotheses so far involve the neurotropic action of the virus, dysregulation of the inflammatory response and of the vascular system, which in turn promote mechanisms that can affect mental health, like alteration of the blood-brain barrier and neuro-inflammation[2,8,9]. While deeper functional analyses will help clarify these aspects, the evidence presented here underlines the need for a targeted screening strategy to tackle the neuropsychiatric effects.
| 1. | Gialluisi A, de Gaetano G, Iacoviello L. New challenges from Covid-19 pandemic: an unexpected opportunity to enlighten the link between viral infections and brain disorders? Neurol Sci. 2020;41:1349-1350. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | de Erausquin GA, Snyder H, Carrillo M, Hosseini AA, Brugha TS, Seshadri S; CNS SARS-CoV-2 Consortium. The chronic neuropsychiatric sequelae of COVID-19: The need for a prospective study of viral impact on brain functioning. Alzheimers Dement. 2021;17:1056-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 134] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 3. | Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. The Lancet Psychiatry [Internet]. 2021;8:416-427. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 901] [Cited by in RCA: 1372] [Article Influence: 274.4] [Reference Citation Analysis (0)] |
| 4. | Hemani G, Zheng J, Elsworth B, Wade KH, Haberland V, Baird D, Laurin C, Burgess S, Bowden J, Langdon R, Tan VY, Yarmolinsky J, Shihab HA, Timpson NJ, Evans DM, Relton C, Martin RM, Davey Smith G, Gaunt TR, Haycock PC. The MR-Base platform supports systematic causal inference across the human phenome. Elife. 2018;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4747] [Cited by in RCA: 5624] [Article Influence: 703.0] [Reference Citation Analysis (0)] |
| 5. | Jansen IE, Savage JE, Watanabe K, Bryois J, Williams DM, Steinberg S, Sealock J, Karlsson IK, Hägg S, Athanasiu L, Voyle N, Proitsi P, Witoelar A, Stringer S, Aarsland D, Almdahl IS, Andersen F, Bergh S, Bettella F, Bjornsson S, Brækhus A, Bråthen G, de Leeuw C, Desikan RS, Djurovic S, Dumitrescu L, Fladby T, Hohman TJ, Jonsson PV. , Kiddle SJ, Rongve A, Saltvedt I, Sando SB, Selbæk G, Shoai M, Skene NG, Snaedal J, Stordal E, Ulstein ID, Wang Y, White LR, Hardy J, Hjerling-Leffler J, Sullivan PF, van der Flier WM, Dobson R, Davis LK, Stefansson H, Stefansson K, Pedersen NL, Ripke S, Andreassen OA, Posthuma D. Genome-wide meta-analysis identifies new loci and functional pathways influencing Alzheimer’s disease risk. Nat Genet. 2019;51:404-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1688] [Cited by in RCA: 1678] [Article Influence: 239.7] [Reference Citation Analysis (0)] |
| 6. | COVID-19 Host Genetics Initiative. Mapping the human genetic architecture of COVID-19. Nature. 2021;600:472-477. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 386] [Cited by in RCA: 390] [Article Influence: 78.0] [Reference Citation Analysis (0)] |
| 7. | Burgess S, Davies NM, Thompson SG. Bias due to participant overlap in two-sample Mendelian randomization. Genet Epidemiol. 2016;40:597-608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 525] [Cited by in RCA: 1221] [Article Influence: 122.1] [Reference Citation Analysis (0)] |
| 8. | Iadecola C, Anrather J, Kamel H. Effects of COVID-19 on the Nervous System. Cell. 2020;183:16-27.e1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 488] [Cited by in RCA: 457] [Article Influence: 76.2] [Reference Citation Analysis (0)] |
| 9. | Boldrini M, Canoll PD, Klein RS. How COVID-19 Affects the Brain. JAMA Psychiatry. 2021;78:682-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 292] [Article Influence: 58.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non-Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Genetics and heredity
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Coelho AC, Yoshikawa M S-Editor: Wu YXJ L-Editor: A P-Editor: Wu YXJ