Published online Feb 19, 2022. doi: 10.5498/wjp.v12.i2.348
Peer-review started: May 30, 2021
First decision: July 14, 2021
Revised: July 27, 2021
Accepted: January 20, 2022
Article in press: January 20, 2022
Published online: February 19, 2022
Processing time: 262 Days and 23.3 Hours
Catatonia is a complex psychomotor syndrome that often goes unrecognized and untreated, even though its classification has evolved in recent years. Prompt and correct identification of catatonia allows for highly effective treatment and prevention of possible complications. The underrecognition of catatonia in older patients is also frequent, and research in this population is scarce.
To conduct a systematic review of the literature on catatonia in older people to ascertain its clinical characteristics across settings.
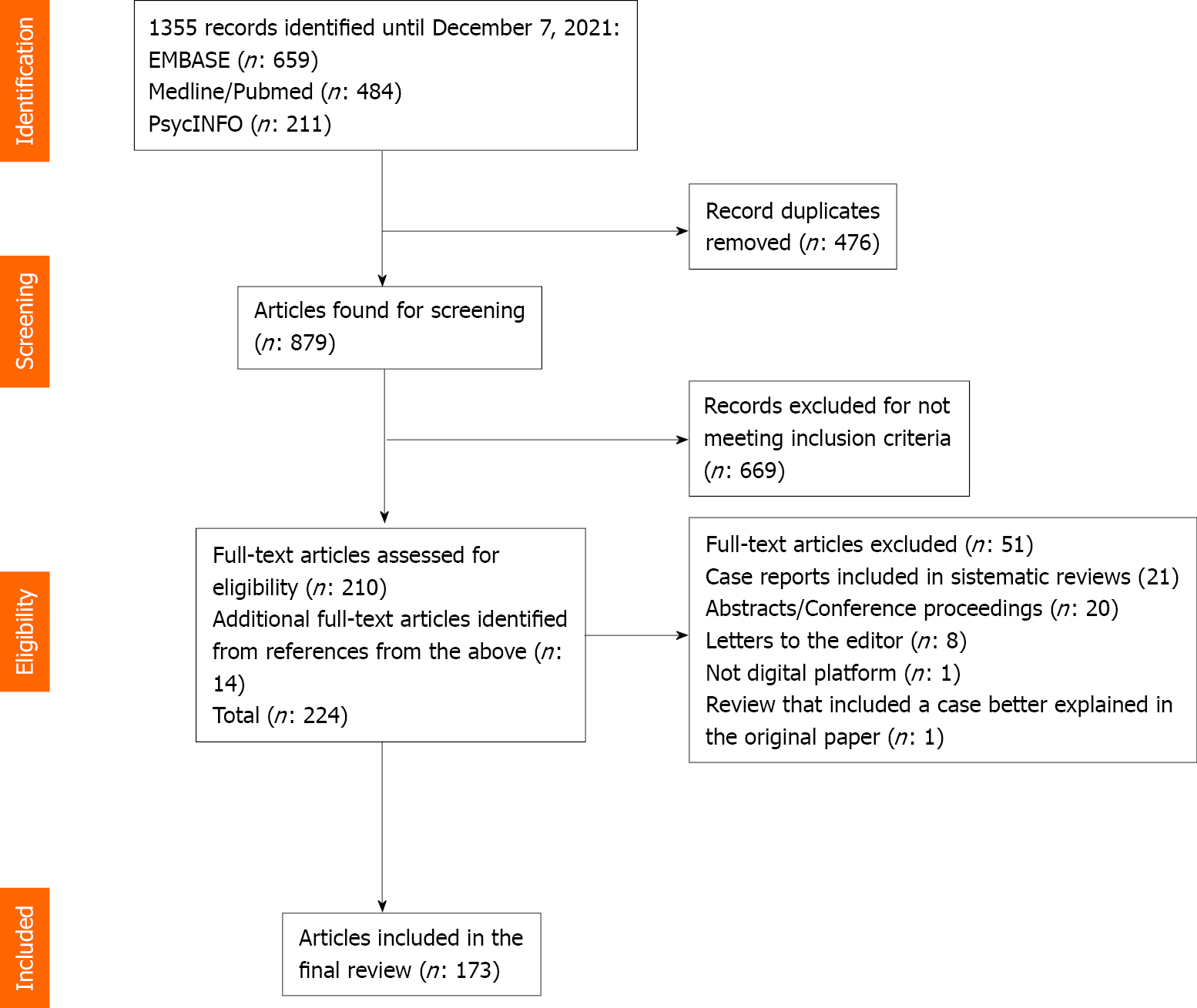
Following the PRISMA guidelines, MEDLINE, EMBASE, and PsycINFO databases were searched from inception to December 2021, with a strategy aimed at identifying all articles published on catatonia in older adults. Titles and abstracts were scanned and selected independently by two authors. Papers investigating issues related to catatonia and/or catatonic symptoms in older people, with English abstracts available, were included. References of selected articles were revised to identify other relevant studies.
In total, 1355 articles were retrieved. After removing duplicates, 879 remained. Of the 879 identified abstracts, 669 were excluded because they did not meet the inclusion criteria. A total of 210 articles underwent full text review, and 51 were eliminated for various reasons. Fourteen more articles were selected from the references. Overall, 173 articles were reviewed: 108 case reports, 35 case series, 11 prospective cohort studies, 6 case-control studies, 3 retrospective cohort studies and 10 reviews. We found several particular aspects of catatonia in this population. Catatonia in older patients is highly prevalent and tends to have a multifactorial etiology. Older patients, compared to younger patients, have a higher risk of developing catatonia with benzodiazepine (BZD) withdrawal, in bipolar disorder, and in the general hospital. Age, together with other risk factors, was significantly associated with the incidence of deep venous thrombosis, neuroleptic malignant syndrome poor outcome, other complications and mortality. Treatment with BZDs and electroconvulsive therapy is safe and effective. Prompt treatment of its cause is essential to ensure a good prognosis.
Catatonia in older patients is highly prevalent and tends to have a multifactorial etiology. The risk of developing catatonia in some settings and conditions, as well as of developing complications, is high in this population. Symptomatic treatment is safe and effective, and timely etiologic treatment is fundamental.
Core Tip: Catatonia in older people is underrecognized and undertreated, as demonstrated by the scarce bibliography published in this age group, in which the prevalence is high and the etiology usually multifactorial. Catatonia can frequently present together with delirium. General medical conditions and neurological disorders have a very important role in its etiology. Older people could have a higher risk of developing catatonia in bipolar disorder, the general hospital and with benzodiazepine (BZD) withdrawal. Also, they have a higher risk of developing complications secondary to this condition. BZDs and electroconvulsive therapy have been proven to be safe and effective symptomatic treatments, but the correct identification and treatment of the etiology are crucial for a full recovery.
- Citation: Jaimes-Albornoz W, Ruiz de Pellon-Santamaria A, Nizama-Vía A, Isetta M, Albajar I, Serra-Mestres J. Catatonia in older adults: A systematic review. World J Psychiatry 2022; 12(2): 348-367
- URL: https://www.wjgnet.com/2220-3206/full/v12/i2/348.htm
- DOI: https://dx.doi.org/10.5498/wjp.v12.i2.348
Catatonia is a psychomotor syndrome caused by physical illnesses, such as infections; endocrine, metabolic, and neurologic disorders; psychiatric conditions, mainly affective and psychotic; and medications and other substances[1]. The contemporary concept of catatonia has evolved significantly. The Diagnostic and Statistical Manual - Fifth Edition (DSM-5) classifies catatonia either as a specifier of all mental disorders, as secondary to a general medical condition (GMC), and as catatonia not otherwise specified for when the syndrome is identified but not yet their etiology[2]. Based on a review of the available evidence published in recent decades and considering their clinical utility and global applicability, the International Classification of Diseases - 11th Edition classifies catatonia as a new diagnostic group at the same hierarchical level as the other included disorders. This edition, approved in May 2019, considers that catatonia can be caused by mental disorders, psychoactive substances (including medications), and medical conditions. In the former, catatonia is valued with the symptom specifier within the category “psychomotor symptoms” and, in the other two cases, as a secondary presentation form[3]. In patients older than 18 years, catatonia is mostly associated with affective disorders[1]. Its early recognition is important, as it is a potentially deadly syndrome. However, it is highly treatable, usually responding to treatment of the cause and to short courses of benzodiazepines (BZDs) or electroconvulsive therapy (ECT)[4-7].
Catatonia is also underrecognized in older adults, something that in this population may lead to delayed treatment, misdiagnosis, adverse events, and even death[8,9]. Despite the increasing amount of research on catatonia, there have been few specific studies on older patients. This review aims to summarize the published literature on catatonia in older adults to provide up-to-date knowledge about this entity for clinicians working with this population.
This systematic review was conducted using the PRISMA method[10]. The MEDLINE, EMBASE, and PsycINFO databases were searched from inception through December 2021. The search strategy was as follows: CATATONIA/or catatoni*.af. and aged/or “aged, 80 and over”/or frail elderly/or (elder* or “old people” or geriatr* or senior* or aged or “over 65” or “over 80” or “65 year*” or “85 year*”).ti,ab. Articles identified were imported into a standard reference manager, EndNote X7, and duplicate manuscripts were removed. Papers that investigated issues related to catatonia and/or catatonic symptoms in older people, with an English abstract available, were included. Titles and abstracts were scanned for relevance. Papers were selected according to the inclusion criteria by two authors independently (Jaimes-Albornoz W and Serra-Mestres J). Full texts were ordered in case of uncertainty to maximize sensitivity. References of selected articles were cross-checked to identify other potentially eligible studies. Case reports, case series, controlled studies, or review articles were eligible for inclusion in this review. The full texts of studies that passed the initial screening were reviewed and potentially excluded based on the same criteria. From this selection we only included Abstracts/Conference proceedings and letters to the editor that describe cases of catatonia whose clinical correlates have not been previously described. The literature search strategy is summarized in the flow chart presented in Figure 1. We also present all the clinical correlates of our catatonic patients in a psychogeriatric unit (Tables 1, 2 and 3). Information on patients diagnosed with dementia in this series has been published previously[11].
| Abstract | |
| Aims | To determine the frequency and characteristics of catatonia in older people in a psychogeriatric ward |
| Methods | All patients admitted were screened for catatonia with the Bush-Francis Catatonia Screening Instrument over a period of 6 mo. Data was collected on sociodemographics, past medical/psychiatric/drug history, clinical findings, treatment, complications/outcome, and investigations. Treatment with lorazepam orally or intramuscularly was initiated in patients who fulfilled diagnostic criteria for catatonia |
| Results | 37 patients were admitted. Prevalence of catatonia was 27%, 10 out of 37 (Bush-Francis criteria) and 24.3%, 9 out of 37 (DSM-5 criteria). The 10 catatonic patients have a mean age of 75.8 years; range: 67-87; and 8 were female. 90% of these patients had a cardiovascular risk factors. The etiology was multifactorial in 50% of the cases. 6 patients had dementia. In 3 of them catatonia was associated with the use of neuroleptics, in 1 with neuroleptics and a urinary infection (she also had delirium), in another with major depression and in only one dementia was a possible etiology. 40% of the cases developed catatonia secondary to affective disorders and 10% to schizophrenia spectrum disorder. In the total sample there were 14 patients with dementia. The catatonia rate in these patients was 42.8% (6 of 14). 9 patients received treatment for catatonia with lorazepam, all of which achieved complete remission, 1 of the these was also treated with clonazepam. 1 patient was treated with sodium valproate and achieved a partial response. 3 patients developed complications secondary to catatonia. One had an elevated creatine kinase of 1083 IU/L, another a deep venous thrombosis, and the last one, hypokalemia |
| Conclusions | Catatonia is a very prevalent entity in the psychogeriatric ward. The etiology is usually multifactorial. This condition occurred frequently in patients admitted with dementia. Treatment with lorazepam is highly effective and safe |
| Age/sex | Medical history | Psychiatric history | Current acute medical diagnosis/antipsychotic exposure | Current acute psychiatric diagnosis |
| 67/F | Bowel obstruction resulting in perforation | Bipolar disorder | None | Bipolar disorder, current episode depressive severe without psychotic symptoms |
| 87/M | Hypertension; Hyperlipidemia; Lip carcinoma | Alzheimer's disease | None/(risperidone, quetiapine) | Late onset Alzheimer's disease |
| 76/F | Hypertension; DM2; Hyperlipidemia | Vascular dementia | None/quetiapine | Vascular dementia |
| 75/F | Ischemic heart disease; Irritable bowel syndrome; Hypothyroidism; Pulmonary fibrosis; Diveticulitis | RDD; Health anxiety; Dementia | None | Late onset Alzheimer's disease; RDD, current episode severe without psychotic symptoms |
| 71/F | Hyperlipidemia; Atrial fibrillation; Repeated urinary tract infections; Diverticulitis | RDD; Alcohol misuse; Alzheimer’s disease | Urinary tract infection/(aripiprazole, olanzapine) | Young onset Alzheimer’s disease; Delirium superimposed on dementia |
| 70/F | Hypertension; Osteoarthritis | RDD | None | RDD, current episode severe with psychotic symptoms |
| 74/F | Parkinson’s disease; Glaucoma; Obesity | Schizoaffective disorder | None | Schizoaffective disorder not otherwise specified |
| 68/F | Hyperlipidemia | Young onset Alzheimer’s disease | None/none | Young onset Alzheimer’s disease |
| 85/M | Hypertension; DM2; Jaw osteomyelitis; Isquemic heart disease; Pacemaker | Mixed dementia | None/risperidone | Mixed dementia |
| 85/F | Hypertension; Atrial fibrillation; Breast cancer | Depression | None | Severe depressive episode without psychotic symptoms |
| Catatonia signs | Country, clinical setting, (n: Patients) | Total (n = 79) | % | ||||
| Spain[5] CLS, (n: 10) | Australia[10] CLS, (n: 6) | United Kingdom[7] PW, (n: 10) | Hungary[11] APW, (n: 11) | Spain[12] PW, (n: 42) | |||
| Inmobility/stupor | 10 | 5 | 7 | 7 | 24 | 53 | 67.1 |
| Staring | 10 | 3 | 7 | 7 | 22 | 49 | 62.0 |
| Mutism | 8 | 2 | 7 | 4 | 18 | 39 | 49.5 |
| Negativism | 7 | 3 | 4 | 0 | 25 | 39 | 49.5 |
| Withdrawal | 8 | 3 | 4 | 3 | 18 | 36 | 45.6 |
| Rigidity | 9 | 4 | 6 | 2 | 15 | 36 | 45.6 |
| Excitement | 0 | 0 | 3 | 3 | 27 | 33 | 41.8 |
| Posturing | 7 | 4 | 5 | 6 | 8 | 30 | 37.9 |
| Verbigeration | 1 | 1 | 2 | 0 | 26 | 30 | 37.9 |
| Perseveration | 1 | 0 | 3 | 2 | 20 | 20 | 33.0 |
| Stereotipies | 4 | 1 | 4 | 2 | 15 | 26 | 33.0 |
| Autonomic abnormalities | 1 | 1 | 3 | 1 | 16 | 16 | 27.8 |
| Impulsivity | 1 | 0 | 2 | 1 | 15 | 19 | 24.0 |
| Automatic obedience | 1 | 1 | 3 | 1 | 16 | 22 | 21.5 |
| Combativeness | 2 | 0 | 4 | 0 | 14 | 20 | 20.4 |
| Ecophenomena | 6 | 1 | 2 | 0 | 5 | 14 | 17.7 |
| Ambitendency | 0 | 1 | 2 | 2 | 8 | 13 | 16.5 |
| Grasp reflex | 0 | 1 | 1 | 2 | 9 | 13 | 16.5 |
| Grimacing | 3 | 1 | 0 | 0 | 8 | 12 | 15.3 |
| Mitgehen | 3 | 0 | 0 | 5 | 1 | 9 | 11.4 |
| Gegenhalten | 3 | 0 | 3 | 2 | 0 | 8 | 10.2 |
| Waxi flexibility | 2 | 0 | 4 | 0 | 0 | 6 | 7.6 |
| Mannerism | 0 | 0 | 0 | 0 | 4 | 4 | 5.1 |
In total, 173 articles were considered: 108 case reports, 35 case series (12 also carried out a systematic review of the literature), 11 prospective cohort studies, 6 case control studies, 3 retrospective cohort studies, and 10 reviews. All articles were reviewed and are summarized below.
The prevalence of catatonia is largely dependent on its recognition, diagnostic criteria used, and setting. Although the general prevalence of catatonia is not fully known, it is considered to be between 5% and 20% among acute psychiatric patients; however, it varies according to the underlying or comorbid conditions[12]. A prevalence of 14%-71% has been described in mood disorders, 4%-67% in schizophrenia spectrum disorders, and between 4%-46% in GMCs[13]. A recent meta-analysis including 74 studies and 107304 individuals showed an overall pooled mean prevalence of catatonia of 9.2% among subjects diagnosed with a variety of psychiatric and medical conditions[13].
In the older population, the prevalence of catatonia also seems to vary depending on the setting and diagnostic criteria used. In liaison psychiatry services using the Bush Francis Catatonia Rating Scale (BFCRS) criteria, the prevalence of catatonia was 5.5%[14] and 8.9%[8]. Another study conducted in older patients in an acute inpatient general psychiatry ward reported a prevalence of 11.2% using the BFCRS and 6.1% using the DSM-5 criteria[15]. The prevalence was noted to be higher in acute psychogeriatric units in the United Kingdom (Table 1) and Spain[16], where the prevalence was 27% and 39.6% and 24.3% and 20.8%, respectively, using the BFCRS and DSM-5 criteria.
The specific brain mechanisms underlying catatonia are still poorly understood. The model developed by Northoff et al[17,18], who hypothesized that catatonic symptoms are mainly associated with orbitofrontal-prefrontal/parietal cortical dysfunction (‘top-down’ model of catatonia), abnormal ‘horizontal’ cortical-cortical modulation, and basal ganglia-cortical dysfunction (a ‘bottom-up’ mechanism), is criticized because the results are inconsistent and have generally been limited to schizophrenic patients with catatonia[19]. Studies with structural and functional brain imaging[20], clinical observations made after lobotomies and frontal lobe lesions, and experiments carried out in animals[21] have described incompatible results with Northoff’s theory[17,18]’s theory. We are still far from having an integrative pathophysiological model of catatonia resulting from clinical, structural, and functional abnormalities of such a different nature. In this regard, only two articles were found about older people with catatonia that used brain imaging. The first was in patients with bipolar disorder (BD) and major depressive disorder (MDD), employing functional near-infrared spectroscopy[22], and the other used SPECT in older patients who developed catatonia as a result of late-onset schizophrenia[23]. Their conclusions were similar to those previously reported in adult patients.
It has also been suggested that catatonia could be a manifestation of intense anxiety and/or fear, resembling tonic immobility in animals, an evolutionary adaptive defense strategy to survive contact with predators attacking moving prey[24]. In humans, fear could also be caused by internal events and psychopathological experiences, such as hallucinations and delusions or anxiety/fear. This freezing would correspond to the immobility, stupor, catalepsy, and mutism observed in catatonia. Alternatively, catatonic excitement would be analogous to the ‘fight-flight’ response mediated by the sympathetic nervous system. A recent study in older patients with MDD found that those with catatonia and with agitation had increased hair cortisol concentrations[25], a hormone associated with stress. Nevertheless, it has also been postulated that it is possible to differentiate between emotive and nonemotive subtypes of catatonia, suggesting that not all catatonia patients experience emotional distress[26]. This theory seems to be supported by the findings that catatonia in older adults is not always related to intense anxiety[27].
The clinical presentation of catatonia in older adults (frequency of catatonic signs and clinical types) is generally similar to that of younger patients. Table 3 shows the frequency of signs of catatonia evaluated with the BFCRS in the 5 prospective observational studies carried out in older people[8,11,14-16]. Two clinical types of catatonia have been consistently reported in both populations[1,28]. A hypokinetic variant (retarded-stuporous) is characterized by reduced movement or immobility, mutism, and withdrawal. This is most frequently observed in depressive disorders and GMCs. A hyperkinetic or excited variant, presenting with increased aimless motor activity (qualitatively different from the overactivity of pure mania, which is purposeful), confusion, and frequent autonomic dysfunction, is mostly observed during manic episodes and in delirious mania. It is noteworthy that both forms of catatonia can coexist in the same patient, occurring in quick succession[1].
A forgotten subtype of catatonia, also described in older people[29], is periodic catatonia. It is characterized by rapid onset, brief and recurrent episodes of catatonia with a longitudinal course. Prognosis is typically better than systematic catatonia, which is insidious and progressive. If it is properly identified can respond extremely well to ECT[29].
The assessment of catatonia requires careful observation during the clinical interview and the elicitation of specific signs during the neurological examination[28]. The routine use of validated rating scales is recommended to facilitate the identification of catatonic signs and the diagnosis of catatonia[30]. In adult patients, seven catatonia rating scales are available. The BFCRS is the most commonly used in research and clinical settings, including older people, because of its validity and reliability and its ease of administration[28,30]. It is also very sensitive, requiring only 2 out of 14 signs of the screening instrument to diagnose this condition[30]. The DMS-5 states that a diagnosis of catatonia can be made if there are at least three symptoms out of 12 presents at the time of assessment: Stupor, catalepsy, waxy flexibility, mutism, negativism, posturing, mannerisms, stereotypy, agitation, grimacing, echolalia and echopraxia[2].
The association of catatonia and delirium has been increasingly described[31,32]. Delirium is considered the most salient factor to predict a medical cause of catatonia[33]. Both share clinical features, lack specific laboratory findings and biomarkers and are diagnosed in similar clinical settings[32]. Delirium is a prominent clinical manifestation of malignant catatonia[34], delirious mania[35] , and neuroleptic malignant syndrome (NMS)[34,36]. Coexisting delirium was found in 30%[8] and 50%[14] of cases of older adults with catatonia in acute medical settings, in which the clinical presentation was generally in the retarded-stuporous form. This high prevalence decreases significantly in acute psychogeriatric wards, where delirium was described in 4.8%[16] and 10%[11] of catatonic cases. The differential diagnosis between catatonia and delirium is challenging, as both cause prominent psychomotor abnormalities. Delirium’s classification predominantly relates to its motor aspects and is thus divided into hyperactive, hypoactive, and mixed forms[31]. There are also hypoactive and hyperactive forms of catatonia. Catatonia can be misdiagnosed as delirium and managed as such, and while delirium appears in the list of differential diagnoses of catatonia, the latter rarely figures into that of delirium[32]. Furthermore, unlike delirium, approximately 80% of catatonia cases of medical etiology are due to neurological disorders[33]. However, there are differences in their pharmacological management. The treatment of choice in catatonia, lorazepam, is rarely the treatment of choice in delirium, except when caused by BZD withdrawal. The most widely used symptomatic treatment of choice in delirium, antipsychotics, is generally to be avoided in the management of catatonia. Therefore, the ability of clinicians to ascertain a catatonic dimension in cases of delirium will facilitate selection of the appropriate treatment[31,32].
Catatonia in older people often presents acutely, but it can also have an insidious presentation. The duration can be transient or chronic, lasting for weeks, months or even years[37,38]. The total duration of illness could be significantly lower if the etiology is a GMC when compared with affective or psychotic disorders[38,39]. Acute catatonia has a good prognosis if it is diagnosed early, its symptoms and etiology are treated in a timely fashion, and the necessary measures are taken to prevent complications. If complications are already present, they are treated aggressively[28]. In organic catatonia, structural brain lesions may have a worse prognosis than metabolic causes[8,40]. Older patients in general hospitals with a longer duration of untreated catatonia may have a worse outcome in terms of rates of complications (40%) and even death (20%)[8].
Catatonia may develop a chronic or continuous course in some patients, mainly with chronic psychoses. In a study in chronically hospitalized older schizophrenic patients, catatonic symptoms were less common and less severe than in acute hospital patients, but the clinical pattern was similar[37]. According to the authors of the study, these findings suggest that catatonic phenomena may persist for years, a course described by Kahlbaum in several cases where catatonia persisted, in some patients, until their death[37].
Neurological disorders: Dementia: Catatonia has been described in all dementia types, with reports in patients with Alzheimer’s disease (AD)[41-43]; frontotemporal dementia (FTD)[44-49]; dementia with Lewy bodies (DLB)[50-55]; and other cases with mixed, vascular, or nonspecified dementia[56,57]. Two prospective studies in psychogeriatric units reported a high prevalence of catatonia in patients with dementia using DSM-5 criteria, at 35.3%[16] and 42.8%[11]. This prevalence was found to be lower in another study in a general psychiatric ward, which report a prevalence of 4.7% using the same criteria[15]. In this last series, almost three-quarters of the patients with catatonia had dementia; 28% of patients had associated depressive disorder, and 36% had a GMC[15], an association also present in most of the published dementia case reports.
Encephalitis: Encephalitis occurs more frequently in younger people; however, a few case reports in older patients have been found[58-62]. Among the patients with anti- N-methyl-D-aspartate (NMDA) receptor encephalitis[59-62], one also tested positive for herpes simplex virus[59]. In this population, in this type of encephalitis, until 17.4% patients could present with catatonia[63]. The remaining case reports of catatonia in older patients involved a patient with paraneoplastic encephalitis[58] and a patient with anti-Hu encephalitis[61]. Prior to catatonia onset, most cases presented with an array of psychopathologies, such as delusions[58-60], auditory hallucinations[60], visuotactile hallucinations[59], and mania[61]. The only exception was a case report of a patient with a history of anxiety who presented with parkinsonism[62].
Epilepsy: In this review, 12 older patients with catatonia in the context of epileptic activity were found. Most had nonconvulsive status epilepticus (NCSE)[61,64,65], one case had complex partial seizures secondary to viral encephalitis in a patient with BD[61], one case of frontal lobe epilepsy in a patient with dementia[66], and a patient with schizophrenia who developed clonic seizures[64]. Among NCSE patients, 4 cases were associated with the use of antidepressants (bupropion 75 mg/d[64], paroxetine 20 mg/d[67], sertraline 50 mg/d[67], mirtazapine 30 mg/d and sertraline 50 mg/d[67]) and 1 with paroxetine 7.5 mg/d and gabapentine 900 mg/d withdrawal[64]. Five had delirium[64,68], 1 had acute kidney injury[65], 4 had acute depressive symptoms[64], 3 had acute psychotic symptoms[64,68], 1 had mania and anti-Hu meningoencephalitis[61].
Cerebrovascular disease: There were articles reporting older patients who developed catatonia secondary to acute strokes[8,69-72] and past or chronic vascular changes[73,74]. No relation was found between lesion location and emergence of catatonia. Some of these cases had longstanding depression as well[71]. As to newer onset psychopathology, there were 1 case with delirium[69], and 2 patients with psychosis[70,71].
Parkinson’s disease: Two papers found that catatonia could be differentiated by parallel ratings of parkinsonian symptoms and catatonia scales in older adult patients with schizophrenia[37] or depression[75]. In the Starkstein's study[75], apomorphine improved Parkinson’s symptoms without affecting catatonic symptoms, thus supporting a biological basis for a distinction between the two conditions. Our review found 6 older patients with catatonia and Parkinson’s disease[76-81]. The cases presented with diverse psychiatric conditions. For instance, one case had depression[81] and another case had depression and posttraumatic stress disorder[76]. All these patients developed symptoms, such as depression[78,79] and psychosis[76-80], prior to catatonia onset.
Other neurological disorders: Other neurological entities found in older patients with catatonia were epidural empyema[7], progressive supranuclear palsy[82], frontotemporal lobes atrophy[83], cerebral Whipple’s disease[84], Creutzfeld-Jakob disease[85] and cerebral anoxia after a cardiac arrest[86].
Metabolic, infectious, endocrine, nutritional and neoplastic disorders: Some metabolic derangements can cause catatonia in older people. These include acute renal failure[15,52,87], heart failure[8,15], liver failure[15], post liver transplantation[88], dehydration[15], hypernatremia[87,89] and hyponatremia[90-93]. Infectious disorders associated with catatonia are acute[94-96] and chronic recurrent urinary tract infection[97]; pneumonia[8,15,98] and coronavirus disease 2019[99-101]. Associated endocrine disorders are hyperparathyroidism[102,103], hypothyroidism[93,95], subclinical Cushing’s syndrome[104], and hyperthyroidism due to Grave's disease[105]. Finally, pertaining to nutritional and neoplastic etiologies, only one case of cyanocobalamin deficiency[106] and another of a colon tumor have been described[15]. Most of these patients had a psychiatric history and developed catatonia secondary to a GMC or in association with drug withdrawal. None of these cases presented with acute psychopathology, with the exception of 4 cases that showed affective and/or psychotic symptoms secondary to the primary metabolic[93] and endocrine disorders[103,105,106].
Antipsychotics: Many cases of catatonia related to antipsychotic use in older patients have been published. Of these, there were patients that developed NMS associated with aripiprazole[107] haloperidol[108-113] and loxapine[114]. In addition, there are reports of catatonia induced by pipothiazine[115], quetiapine[11,116], and droperidol[117] and cases secondary to exposure to more than one antipsychotic: Haloperidol and trifluperazine[109], risperidone and quetiapine[11], aripiprazole and olanzapine[11], and risperidone, haloperidol and tiapride[8].
Other drugs and toxic substances: In total, eleven case reports were found of patients who developed catatonia after exposure to normal doses of a wide variety of drugs, such as phenelzine[118], allopurinol[119], prednisone[95] rivastigmine[41], donepezil[120], azithromycin[121], cefepime[122], amiodarone[123], methotrexate[124], tacro-limus[125] and imiquimod[126]. Eight out of 11 patients were female, one case had a stable BD prior to the index episode[125], another case had DLB[120] and another had AD[41]. None of them had current affective or psychotic psychopathology before exposure to the drug. One case presented with hyponatremia[126] and another with acute interstitial nephritis[122]. The others developed psychotic or depressive symptoms prior to, or simultaneously with, catatonia. There was also a catatonia case secondary to neurotoxicity reported by manganese[96] and another after deep brain stimulation successfully treated with lorazepam and right unilateral ECT[127].
Catatonia secondary to drug withdrawal: Descriptions of catatonia after the rapid tapering or abrupt discontinuation of BZDs after prolonged use have been published. These cases were related to nitrazepam[128], diazepam and alprazolam[128] , oxaze-pam and temazepam[128], clonazepam[128,129], alprazolam[128], temazepam[128], diazepam[128], chlordiazepoxide[128] and lorazepam[130]. The doses of BZDs vary widely, but they are usually in the therapeutic range. The onset of withdrawal catatonia is 3-7 d after discontinuation, and the duration is 3-10 d. Also, it appears to present without electroencephalography abnormalities, such as diffuse slowing[128]. Moreover, there are sporadic reports of withdrawal catatonia secondary to antipsychotics and other psychotropics, such as clozapine[131], olanzapine[94], risperidone and olanzapine and chlorpromazine[56], haloperidol and cyamemazine[132], bromperidol and levomepromazine[133], amantadine[79], gabapentin[64,134], and lithium[94].
Affective disorders: Studies in psychogeriatric units found a prevalence of affective disorders in catatonia of 40% (Table 1) and 42.8%[16]. In a psychiatric general inpatient service, catatonia was most prevalent among older patients with severe depression[75]. These patients had more severe cognitive impairment and more severe deficits in activities of daily living than depressed noncatatonic patients[75]. In a similar setting in Hungary, 28% of catatonic patients suffered from dementia associated with depressive disorder[15]. This relationship between the development of catatonia and organic conditions in patients with affective disorders has been replicated in most of the case reports or case series published[61,64,68,135].
Most case reports of catatonia in affective disorders have been published emphasizing the unusualness of the presentation (patient that can masquerade as Creutzfeld-Jakob disease[136]), the associated psychopathology (cases with nihilistic delusions suggestive of Cotard's syndrome[137,138]), or the comorbid conditions present (the affective cases described in the sections on catatonia secondary to GMCs or drug use/withdrawal).
Schizophrenia spectrum disorders: Reports of older patients with catatonia in psychotic disorders are sporadic. Cases of catatonia have been described in association with schizophrenia[139], psychotic disorder not otherwise specified[16], brief psychotic disorder[135] and schizoaffective disorder[11,15,16]. In a study conducted in older adults with schizophrenia, a catatonia prevalence of 69% using BFCRS criteria was found[37]. In acute inpatient wards, schizophrenia spectrum disorders (SSD) is the third most frequent condition in catatonic older patients following affective disorders and those secondary to GMCs[11,16].
Other disorders: Catatonia has been reported in adjustment disorder[16,140], substance use disorder[16], conversion disorder[140,141], and posttraumatic stress disorder[142]. In one case report, there was a background of melancholia and a recent withdrawal of thioridazine; in another case report, the adjustment disorder was diagnosed with depressed mood. In the remaining reports, psychiatric or organic comorbidities were not detailed. Table 4 shows all the etiologies associated with catatonia described above.
| Psychiatric disorders | General medical conditions | Drugs and toxic substances |
| Schizophrenia spectrum disorders: Schizophrenia; Schizoaffective disorder; Brief psychotic disorder; Psychosis not otherwise specified. Affective disorders: Major depressive disorder; Bipolar disorder. Others psychiatric disorders: Post-traumatic stress disorder; Conversive disorder; Adjustment disorder; Substance use disorder | Neurologic: Dementia: Alzheimer´s dementia; Frontotemporal dementia; Lewy bodies dementia; Mixed dementia; Organic dementia; Dementia not otherwise specified. Epilepsy. Cerebrovascular disease; Parkinson´s disease. Others: Cerebral anoxia; Creutzfeldt-Jakob’s disease; Epidural empyema; Frontotemporal lobes atrophy; Cerebral Whipple’s disease; Progressive supranuclear palsy. Metabolic: Acute renal failure; Heart failure; Liver failure; Post liver transplantation; Dehydration; Hyponatremia; Hypernatremia. Infectious: Urinary tract infection; Pneumonia; COVID-19. Endocrine: Hyperparathyroidism; Hypothyroidism; Hyperthyroidism. Others: Cyanocobalamin deficiency; Colon tumor | Drugs: Regular use: Antipsychotics: Haloperidol; Droperidol; Loxapine; Pipotiazine; Trifluoperazine; Tiapride; Aripiprazole; Risperidone; Quetiapine. Other drugs: Phenelzine; Allopurinol; Prednisone; Rivastigmine; Donepezil; Azithromycin; Cefepime; Amiodarone; Tacrolimus; Methotrexate; Imiquimod. Withdrawal: Benzodiazepines: Nitrazepam, diazepam, alprazolam, oxazepam, temazepam, clonazepam, chlordiazepoxide and lorazepam. Antipsychotics: Clozapine, olanzapine, risperidone, chlorpromazine, levomepromazine, bromperidol, haloperidol and cyamemazine. Others: Amantadine, lithium, gabapentine. Toxic substances: Manganese |
BZDs: BZDs are an effective treatment for catatonia in older adults in whom a full resolution is described within hours/days of treatment initiation[6]. Lorazepam is recommended as the first-line medication, and it is extensively reported to be highly effective, irrespective of the underlying cause[5,6,143,144]. Other BZDs, such as diazepam[128,145], midazolam[146,147], alprazolam[148], oxazepam[128], flunitrazepam[139], temazepam[128] and clorazepate[108], have also been described as useful in older people. This treatment should be maintained until the catatonia etiology is identified and appropriately treated[1,28]. In this review, the initial doses of lorazepam found ranged from 0.25 to 4 mg daily, with most patients receiving 1-2 mg. If catatonic symptoms respond partially to low doses of BZDs, titration to higher doses is recommended to achieve full symptom resolution[5,6]. During catatonic states, in this and in the other age groups, high BZD doses are typically well tolerated[6]. In older people, the associated risks are oversedation, respiratory depression, cognitive impairment, and falls[149]; therefore, monitoring is necessary. In the reviewed cases, doses ranged from 3-20 mg lorazepam/d. Lower response rates to BZDs have been described in patients with structural brain damage or with schizophrenia when compared with mood disorders or acute medical etiologies[5,6].
ECT: ECT should be a first-line treatment in patients with nonresponse or contraindication to BZDs, those who need a rapid response because of life-threatening conditions, or when malignant catatonia features are present[5,6,150]. Better response rates to treatment were found in catatonia related to mood disorders than in catatonia related to nonaffective psychosis[5,6,68]. Even so, ECT is one of the best treatments for catatonic schizophrenia, and this was also described in older patients by Suzuki et al[139], with excellent response rates in this group.
Among the older catatonic patients successfully treated with ECT, the etiology in most of them were mood disorders, followed by those secondary to non-affective psychosis. Less frequently the etiology was related to a GMC.
The number of sessions ranged from 2 to 25, but only 3 patients needed more than 15 sessions to respond. The mean number of sessions among all catatonic episodes was 10.33 sessions/episode. Exceptionally high initial seizure threshold in catatonic older patients treated with ECT has been reported[151].
The most common application frequencies during acute course ECT were 2 or 3 times a week. Most cases were treated with bifrontotemporal electrode placement and also, there has been reports of patients that received right unilateral ECT with a resolution of catatonia[152,153]. Furthermore, there is a report of a patient with catatonic schizophrenia who was treated by successful seizure induction by means of ECT, with electrodes applied bilaterally to the parietotemporal region after bifrontotemporal ECT failed to induce adequate seizures[154]. On the other hand, 3 articles described only a partial response to ECT in 3 older patients during a catatonic state after receiving 7-8 ECT sessions[8,78,155]. All these cases were associated with GMCs (cognitive impairment, Parkinson’s disease, and manganese poisoning).
Two cases of catatonia refractory to ECT treatment have been reported. One on them was associated with encephalitis secondary to ovarian teratoma[58] and another one in a patient with depression and autistic spectrum disorder[151]. Continuation or maintenance ECT is recommended when relapse occurs despite pharmacological treatment and in patients with recurrence of catatonic symptoms when ECT is suspended[139]. Three cases were described with periodic relapses, but each new catatonic episode responded again to a course of ECT. Although there are no absolute contraindications for the use of ECT in older patients and it is considered a safe and well-tolerated treatment, medical risks must be evaluated individually[143,150]. There are case reports of catatonic patients with unstable or potentially unstable clinical conditions, such as a 95-year-old pacemaker user[156], full anticoagulation after pulmonary embolism[157], a 100-year-old patient with severe aortic stenosis[158], deep venous thrombosis[159]; that illustrates how, with the proper precautions, the benefits of ECT in such conditions might outweigh its risks.
ECT requires general anesthesia. Serious adverse effects related to ECT are extremely infrequent but include arrhythmia, seizures, or even death, although these have not been specifically reported in this population. Other mild adverse effects are considered transient, but they can be relevant in the older population, such as cognitive impairment, delirium, hypertension, increased risk of falls, or hypomania[150]. Cognitive impairment related to ECT is reported as transient, even in older patients, but limited cases of prolonged amnesia have also been described[160].
Etiological treatment: Early identification and treatment of etiological causes of catatonia are crucial, especially in this population[8,11,14]. Even in those patients with a previous history of psychiatric disorder, medical etiologies should always be considered because of the frequent simultaneous occurrence of both conditions[8,14,15,143]. Organic, toxic, and pharmacological conditions are common causes of catatonia and are overrepresented in the older population. In most cases of catatonia in this literature search, remission occurred after specific catatonia symptomatic treatment was administered as well as treatment for the underlying medical condition[8,11,64,94]. Some reports noted remission of catatonia only when treating the underlying medical condition, without symptomatic treatment for catatonia[8,69,102,161]. Recent medication changes should be considered relevant because they highly suggest drug-induced catatonia. Suspension of the causal drug should be considered as part of the treatment, as in some patients, resolution of the catatonic state was only achieved with discontinuation of the drug[8,92,95], while others also needed con-comitant symptomatic catatonia treatment[8,95,109,162].
Other treatments: Zolpidem was broadly reported as an effective treatment for catatonia but with transient efficacy. In general, it was used as a diagnostic test because of its very short half-life when catatonia was suspected[108]. Other reports described the successful treatment of catatonic older patients with zolpidem alone or in combination with other treatments; thus, it could be considered an alternative treatment[45,49,58,104]. The NMDA receptor antagonists memantine and amantadine have also been reported as useful symptomatic treatments for catatonia, even in treatment-resistant patients[163]. Memantine doses ranged from 5-10 mg daily[163]. Amantadine was described as effective (doses ranging from 100-200 mg daily)[78,163]; however, nonresponsiveness was also reported[42,45,164,165]. Anticonvulsant drugs have been used as a catatonia treatment option in this population alone or in combination with partial or complete response. There are reports of valproate at doses ranging from 400-1250 mg daily[11,91,135,163], carbamazepine (100 mg/daily)[78], and topiramate[166]. Additionally, there are articles that described no response to valproate[91,163] or carbamazepine 600 mg/daily[167]. Dopaminergic drugs have also been postulated as potential treatments for catatonia due to the hypothesis that the dopaminergic system is involved in its pathophysiology. There are isolated reports of treatment with bromocriptine[112] and dopamine, the latter being used to treat hypotension during a catatonic state with full recovery[168]. The patient received bupropion as continuation treatment without relapse of catatonia. Also, there have been published a NMS cases which were treated satisfactorily with 25 ECT sessions and bupropion 300 mg/d[164] and with 11 ECT sessions and bromocriptine 15 mg/d[112]. Another article reported a case of successful treatment with methylphenidate in an older depressed patient with catatonic stupor who did not respond to lorazepam[169]. There are articles reporting anecdotal evidence of successful treatment of catatonia with propofol[170] , biperiden[171,172], olanzapine[162,173] and lithium[174]. Another article reported the on efficacy of tramadol in several consecutive catatonic episodes in an older patient with a diagnosis of schizoaffective disorder[132]. Finally, neuromodulation treatments, such as repetitive transcranial magnetic stimulation[111] and transcranial direct current stimulation[175], were also described as effective. The catatonia treatments used in older people are summarized in Table 5.
| 1º line | 2º line | 3º line |
| Benzodiazepines: Lorazepam; Diazepam; Midazolam; Alprazolam; Oxazepam; Flunitrazepam; Temazepam | Electroconvulsive therapy: Bifrontotemporal ECT; Right unilateral ECT; Acute ECT; Continuation ECT; Maintenance ECT | Drugs: Amantadine; Biperiden; Bupropion (as continuation treatment); Bromocriptine; Carbamazepine; Dopamine; Lithium; Memantine; Methylphenidate; Olanzapine; Propofol; Topiramate; Tramadol; Valproate; Zolpidem. Neuromodulation treatments: Repetitive Transcranial Magnetic Stimulation; Transcranial Direct Current Stimulation |
Catatonic states can induce complications in relation to immobility, dehydration or inability to have oral intake, which are especially relevant in older patients. Some of these complications include deep vein thrombosis (DVT), pulmonary embolism, pressure ulcers, infections, acute renal injury, rhabdomyolysis, electrolyte distur-bances, pulmonary aspiration and secondary pneumonitis and/or pneumonia, or muscular contractures[143,165,176].
In a retrospective chart review, Ishida et al[176] concluded that age and the presence of risk factors for dynamic vascular patterns were significantly associated with the incidence of DVT. Patients older than 65 years had an odd ratio (OR) of 3.23, and younger patients had an OR of 1[176].
Early identification and treatment of catatonia and its underlying cause are crucial to rapidly improve stupor and prevent all these complications[5,6,144]. Specific preventative measures include frequent vital sign checks, anticoagulation, postural changes, intravenous fluids, nasogastric feeding, and urinary catheterization[165]. Additionally, the progression to malignant catatonia with autonomic instability and hyperthermia is a life-threatening condition that should be watched.
Catatonia in older people is an underrecognized entity and is consequently undertreated, as evidenced by the scarce literature found after a systematic search. The majority of articles are case reports or case series, with few prospective studies. However, a very interesting fact is evident: Most case descriptions show similar medical and psychiatry histories, clinical manifestations, etiologies, comorbidities and responses to treatment; clinical correlates that are very similar to those cases reported by prospective studies.
Catatonia in this population is highly prevalent, and the prevalence increases when the clinical setting studied is more specific (general hospital: 5.5%[14] and 8.9%[8]; general psychiatry unit: 11.2%[15]; psychogeriatric units: 27% (Table 1) and 39.6%[16]. Catatonia prevalence in younger patients in similar settings is lower: 1.6%[177], 1.8%[108] and 2.4%[8] in liaison services and approximately 10% in acute inpatient wards[13]. This suggests that older people may have a higher risk of developing catatonia than those under 65 years of age, as shown in Navarra’s liaison psychiatry study, where their patients over 65 years were 3.95 times more likely to develop catatonia than their younger counterparts[8].
There is some evidence that supports the possibility that somatic and cognitive impairment have a significant role in the development of catatonia[16]. This could be related to the highest prevalence of dementia and medical disorders, such as cardiovascular risk factors (hypertension, type 2 diabetes mellitus, and dyslipidemia), in this population[178], which were present in most case reports described in the United Kingdom psychogeriatric ward (Table 1) and in all patients of the psychiatry liaison consultation studies[8,14] (the other 2 prospective studies did not specify these data). It has been considered whether dementia is a specific risk factor for developing catatonia. Takács et al[15], in a study in a general psychiatry ward, concluded that it was not a risk factor, as the prevalence of catatonia was not very different in their patients with dementia (4.7%) compared to the total study sample (6.1%). However, in studies on psychogeriatric wards, the prevalence was higher in patients with dementia (35.3%[16] and 42.8%[11]) than in the total number of patients [20.8%[16] and 24.3% (Table 1)]. This nonconcordance could be caused by differences in the clinical settings and leaves open the role of dementia as a risk factor for catatonia.
The clinical presentation of catatonia is quite similar to that of adults under 65 years of age. In general, the most frequent signs are the same (immobility, staring, mutism, negativism, withdrawal, rigidity and posturing)[5,12,38]. Unlike what happens in patients under 65 years of age, excitement (41.8%), verbigeration (37.9%), perseveration (33%) and autonomic abnormalities (27.8%) seem to also be very frequent. In older people, the high prevalence of dementia and cardiovascular risk factors could also explain this different profile. In all catatonia prospective studies, the assessment was undertaken in a systematic way using the BFCRS; notably, the low frequency of the catatonic signs considered DSM-5 diagnostic criteria [ecophenomena (17,7%), grimacing (15,3%), waxy flexibility (7,6%) and mannerism (5,1%)] and the high frequency of other catatonic signs included in the BFCRS and not the DSM-5 criteria [staring (62%), withdrawal (45,6%) rigidity (45,6%) and autonomic abnormalities (27,8%)] (Table 3). These results could suggest the need to review the very strict current diagnostic criteria and to take into account what was reported by Stuivenga et al[12], that giving a dimensional approach to catatonic signs could help improve diagnostic sensitivity. In older people, it may be better to use, in an initial assessment, the Bush Francis Catatonia Screening Instrument, which includes the above catatonic signs, to identify more patients susceptible to receiving potentially very effective treatment.
Catatonia and delirium co-occur relatively frequently in older people. Management could be a challenge for clinicians; however, if we follow a therapeutic and care algorithm, the chances of better results are greater[32]. A systematic review on the issue recommended identifying and treating the etiology of both conditions, initially trying a challenge test with lorazepam; avoiding the use of high-potency neuroleptics; taking the necessary measures to prevent and treat complications; and if there is no response with lorazepam, considering the use of amantadine, memantine or topiramate. ECT is indicated in refractory or life-threatening cases[32].
The probability that catatonia in acute medical settings has a medical etiology or is related to drug use/withdrawal is greater than 50%. The prevalence of catatonia was strongly associated with age in the setting of critical illness[179]. This probability increases in critically ill elderly patients by up to 80%-100%[33]. These high rates of catatonia in clinical settings should lead us to consider that the etiology of catatonia is medical until proven otherwise, especially in older adults[33]. It has been frequently reported that the possible organic etiology of patients with catatonia tends to be overlooked, even more so if they have a psychiatric history because of a belief that the psychiatric disorder is the cause of catatonia[143,180].
In almost all dementia cases traced, these disorders were not the cause of catatonia; rather, they emerged as a consequence of the acute onset of psychopathology, GMCs, and/or due to the use of drugs, mainly neuroleptics. This occurred in 29 of 31 (93.5%) patients with dementia reported in observational prospective studies[8,11,14-16]. This does not appear to occur in FTD patients. Catatonia and FTD share a common pathophysiology, frontal lobe dysfunction, and similar symptoms (mutism, stupor, stereotypy, mannerisms, perseveration, negativism, echophenomena, and others[44], which are a central part of their diagnostic criteria[2,181]. This could cause catatonia to be even more underdiagnosed and therefore not adequately treated in this specific type of dementia. In FTD, catatonia should be suspected when the patient has a sudden and sustained increase in previous psychomotor symptoms or when the appearance of new catatonic symptoms is observed. In the rest of the reports of catatonia secondary to neurological disorders, GMCs and the use of drugs, something similar takes place. Catatonia occurs frequently when GMCs cause psychotic or depressive symptoms or when the latter appear as drug adverse effects and/or in patients with a psychiatric history of disorders of both spectra. In future studies, the systematic evaluation of the presence or absence of depressive or psychotic psychopathology in these patients will reveal their roles in the development of catatonia.
In general, in this population, antipsychotics can also increase the risk of NMS and can contribute to the development or worsening of catatonic symptoms[182,183]. Moreover, the NMS risk of poor outcome and mortality is associated with older age[184]. Some authors have recommended antipsychotic discontinuation during the acute phase of catatonia and to reinitiate treatment once catatonia is in remission[5,185]. Due to the risks concerning the safety of antipsychotics, their use in acute catatonia is generally not recommended in this population[185]. Caution should be the rule on prescribing, and the risk assessment should be individualized to each patient[6]. Catatonia can also appear after withdrawal from different types of drugs, mainly BZDs. The predominant subtype was stuporous catatonia with sporadic reports of catatonic excitement. Given that BZD withdrawal is more frequently associated with motor hyperactivity, excited catatonia may not be reported as such[128]. A significant number of these reports described a series of concurrent psychiatric and GMCs that could have played a role in the development of catatonia, mainly depression[128], dementia[57], pneumonia, and infectious exacerbation of chronic obstructive pulmonary disease[128]. Rosebush and Mazurek[186] suggest the possibility that older individuals may be more vulnerable to developing catatonia upon BZD withdrawal, particularly if the drug is rapidly tapered or abruptly discontinued in patients who have taken them for a long time.
In relation to catatonia secondary to psychiatric conditions, this syndrome is more frequently associated with mood disorders than with SSD, as occurs in patients between 18 and 65 years of age. In this population, mood disorders were associated with a 2.7-fold higher risk of developing catatonia compared to psychotic conditions[16]. Again, in patients with affective disorders, age could be a risk factor for developing catatonia. A naturalistic cohort study in BD patients showed that it could present more frequently in older people with catatonic features compared with younger people[187]. As in affective conditions, most of the reports of catatonia in SSD patients have acute psychotic and/or depressive psychopathology and various organic disorders. Although catatonia has been described in practically all the mental conditions of our classification systems, in older adults, cases published outside of affective and SSD disorders are anecdotal and probably due to lack of recognition.
General treatment recommendations on catatonia are derived from case reports or observational studies due to the lack of randomized controlled trials[188]. Despite a possible publication bias, usual treatments, such as BZDs and ECT, show excellent response rates and are considered effective in older adults[5,6,143,144]. Lorazepam is the most extensively used BZD, but other options (Table 5) were tested with good responses. ECT is considered the most successful treatment for catatonia. It is also a safe and effective option for treating catatonia in older patients, regardless of the etiology[5,6]. Some studies have suggested that ECT may be more effective in older patients than in other age groups[139]. It remains controversial whether ECT should be considered a first-line treatment in older patients when catatonia symptoms appear in the context of a MDD[150]. Faster and higher remission rates have been described with ECT in comparison with antidepressant medications. Therefore, it seems reasonable to consider ECT as a priority option if catatonia is present and the underlying condition is also responsive to ECT[150]. There are interesting descriptions of the response to catatonia treatment with other drugs; however, we can consider these options as a third-line treatment because of the limited literature available on the matter (Table 5).
Our review has important limitations, the main one being that all the conclusions are based on the results of mostly case reports and few prospective studies. Publication bias may be present, and the heterogeneity of the prospective studies does not allow for qualitative analysis. The hypotheses presented here will have to be confirmed in prospective studies designed specifically for that purpose. However, the clinical correlates of all these cases significantly coincide with the results of prospective studies, regardless of the year or place of publication or etiology of catatonia. The most important strength is the summarizing of all the bibliographies on catatonia in older adults published since inception in the main medical databases until December 2021, using articles obtained through a systematic search following the PRISMA recommendations.
Catatonia in older people is highly prevalent and is associated with affective disorders, GMCs, and SSDs in that order of frequency, although its etiology is frequently multifactorial. GMCs, mainly dementia and other neurologic disorders, have a significant role in the etiology, and this is sometimes overlooked. Older patients, compared to younger patients, have a higher risk of developing catatonia in BD, in psychiatric liaison services, and they may be more vulnerable to developing catatonia with BZD withdrawal. Age, together with other risk factors, was significantly associated with the incidence of DVT, NMS poor outcome, other complications and mortality. The response to symptomatic treatment with BZDs and ECT is very good and safe, and other effective options are also available. The simultaneous treatment of the etiology of catatonia is also fundamental. Specifically, designed prospective studies are needed to more accurately identify the clinical correlates of catatonia in older people.
Catatonia in older people is an underrecognized and undertreated systemic medical syndrome despite having specific treatment that has shown great effectiveness. These patients are at increased susceptibility of developing potentially life-threatening complications.
Systematic reviews on this topic have not been conducted. Similar previous reviews were not systematic, and since their publication, the number of papers in this regard has practically doubled. We considered that an update was necessary.
This review aimed to synthesize all the published literature related to catatonia in older patients. This summary will provide up-to-date knowledge about this condition.
A comprehensive systematic review was conducted according to PRISMA recom-mendations. An extensive search strategy was developed, and the MEDLINE, EMBASE, and PsycINFO databases were searched. Screening was completed in duplicate. Papers that investigated issues related to catatonia and/or catatonic symptoms in older people with an English abstract available were included. Additionally, we provided all the clinical correlates of our series of catatonia in a psychogeriatric ward.
In total, 173 articles were considered in this systematic review. Most of them were case reports and case series (143), and only 11 were prospective cohort studies. Catatonia in older people is highly prevalent, and in most cases, its etiology is multifactorial. Neurological disorders could play a very important role in catatonia development; in part, cardiovascular risk factors could explain this association. BZDs and ECT are very effective and well tolerated treatments.
This systematic review provides a comprehensive summary of catatonia in older people. These patients have a higher risk of developing catatonia than younger patients with BD in the general hospital and secondary to BZD withdrawal. Age is related, within other risk factors, to poor NMS prognosis and the development of complications.
The current review revealed that the number and quality of studies on this issue are scarce. Given the high morbidity of catatonia in older people, prompt identification and treatment are essential. Thus, further prospective research is warranted to more accurately identify all the clinical aspects of catatonia in older people.
| 1. | Fink M. Rediscovering catatonia: the biography of a treatable syndrome. Acta Psychiatr Scand Suppl. 2013;1-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 146] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 2. | American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders. 5th ed. Washington: American Psychiatric Association, 2013. |
| 3. | Reed GM, First MB, Kogan CS, Hyman SE, Gureje O, Gaebel W, Maj M, Stein DJ, Maercker A, Tyrer P, Claudino A, Garralda E, Salvador-Carulla L, Ray R, Saunders JB, Dua T, Poznyak V, Medina-Mora ME, Pike KM, Ayuso-Mateos JL, Kanba S, Keeley JW, Khoury B, Krasnov VN, Kulygina M, Lovell AM, de Jesus Mari J, Maruta T, Matsumoto C, Rebello TJ, Roberts MC, Robles R, Sharan P, Zhao M, Jablensky A, Udomratn P, Rahimi-Movaghar A, Rydelius PA, Bährer-Kohler S, Watts AD, Saxena S. Innovations and changes in the ICD-11 classification of mental, behavioural and neurodevelopmental disorders. World Psychiatry. 2019;18:3-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 368] [Article Influence: 52.6] [Reference Citation Analysis (0)] |
| 4. | Pelzer AC, van der Heijden FM, den Boer E. Systematic review of catatonia treatment. Neuropsychiatr Dis Treat. 2018;14:317-326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 98] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 5. | Rasmussen SA, Mazurek MF, Rosebush PI. Catatonia: Our current understanding of its diagnosis, treatment and pathophysiology. World J Psychiatry. 2016;6:391-398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 149] [Cited by in RCA: 209] [Article Influence: 20.9] [Reference Citation Analysis (9)] |
| 6. | Sienaert P, Dhossche DM, Vancampfort D, De Hert M, Gazdag G. A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 195] [Cited by in RCA: 193] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 7. | Ramos-Garcia M, González-Salazar C. Electroconvulsive therapy: is there a role for treating older patients? Rev Clin Gerontol. 2013;23:283-294. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Jaimes-Albornoz W, Serra-Mestres J. Prevalence and clinical correlations of catatonia in older adults referred to a liaison psychiatry service in a general hospital. Gen Hosp Psychiatry. 2013;35:512-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Swartz C, Galang RL. Adverse outcome with delay in identification of catatonia in elderly patients. Am J Geriatr Psychiatry. 2001;9:78-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9247] [Cited by in RCA: 9007] [Article Influence: 529.8] [Reference Citation Analysis (0)] |
| 11. | Sharma P, Sawhney I, Jaimes-Albornoz W, Serra-Mestres J. Catatonia in Patients with Dementia Admitted to a Geriatric Psychiatry Ward. J Neurosci Rural Pract. 2017;8:S103-S105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Stuivenga M, Morrens M. Prevalence of the catatonic syndrome in an acute inpatient sample. Front Psychiatry. 2014;5:174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Solmi M, Pigato GG, Roiter B, Guaglianone A, Martini L, Fornaro M, Monaco F, Carvalho AF, Stubbs B, Veronese N, Correll CU. Prevalence of Catatonia and Its Moderators in Clinical Samples: Results from a Meta-analysis and Meta-regression Analysis. Schizophr Bull. 2018;44:1133-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 126] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 14. | Kaelle J, Abujam A, Ediriweera H, Macfarlane MD. Prevalence and symptomatology of catatonia in elderly patients referred to a consultation-liaison psychiatry service. Australas Psychiatry. 2016;24:164-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Takács R, Asztalos M, Ungvari GS, Gazdag G. Catatonia in an inpatient gerontopsychiatric population. Psychiatry Res. 2017;255:215-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 16. | Cuevas-Esteban J, Iglesias-González M, Rubio-Valera M, Serra-Mestres J, Serrano-Blanco A, Baladon L. Prevalence and characteristics of catatonia on admission to an acute geriatric psychiatry ward. Prog Neuropsychopharmacol Biol Psychiatry. 2017;78:27-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Northoff G, Steinke R, Czcervenka C, Krause R, Ulrich S, Danos P, Kropf D, Otto H, Bogerts B. Decreased density of GABA-A receptors in the left sensorimotor cortex in akinetic catatonia: investigation of in vivo benzodiazepine receptor binding. J Neurol Neurosurg Psychiatry. 1999;67:445-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 134] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 18. | Northoff G. What catatonia can tell us about "top-down modulation": a neuropsychiatric hypothesis. Behav Brain Sci. 2002;25:555-77; discussion 578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 217] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 19. | Haroche A, Rogers J, Plaze M, Gaillard R, Williams SC, Thomas P, Amad A. Brain imaging in catatonia: systematic review and directions for future research. Psychol Med. 2020;50:1585-1597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 20. | Walther S, Stegmayer K, Wilson JE, Heckers S. Structure and neural mechanisms of catatonia. Lancet Psychiatry. 2019;6:610-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 213] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
| 21. | Joseph R. Frontal lobe psychopathology: mania, depression, confabulation, catatonia, perseveration, obsessive compulsions, and schizophrenia. Psychiatry. 1999;62:138-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 65] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Nakamura T, Sasayama D, Hagiwara T, Kito H, Washizuka S. Reduced functional connectivity in the prefrontal cortex of elderly catatonia patients: A longitudinal study using functional near-infrared spectroscopy. Neurosci Res. 2021;170:322-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Tsujino N, Nemoto T, Yamaguchi T, Katagiri N, Tohgi N, Ikeda R, Shiraga N, Mizumura S, Mizuno M. Cerebral blood flow changes in very-late-onset schizophrenia-like psychosis with catatonia before and after successful treatment. Psychiatry Clin Neurosci. 2011;65:600-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 24. | Moskowitz AK. "Scared stiff": catatonia as an evolutionary-based fear response. Psychol Rev. 2004;111:984-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 128] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 25. | Baeten RF, Van Rossum EFC, De Rijke YB, Sabbe BGC, Van Der Mast RC, Belge JB, Fransen E, Schrijvers DL, Birkenhäger TK, Van Diermen L. Hair cortisol in patients with a depressive episode treated with electroconvulsive therapy. J Affect Disord. 2020;274:784-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Northoff G, Boeker H, Bogerts B. [Subjective experience and neuronal integration in the brain: do we need a first-person neuroscience? Fortschr Neurol Psychiatr. 2006;74:627-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Cuevas-Esteban J, Iglesias-González M, Serra-Mestres J, Butjosa A, Canal-Rivero M, Serrano-Blanco A, Baladon L. Catatonia in elderly psychiatric inpatients is not always associated with intense anxiety: Factor analysis and correlation with psychopathology. Int J Geriatr Psychiatry. 2020;35:1409-1417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 28. | Serra-Mestres J, Jaimes-Albornoz W. Recognizing Catatonia in Medically Hospitalized Older Adults: Why It Matters. Geriatrics (Basel). 2018;3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 29. | Tang VM, Park H. Brief episodes of non-specific psychosis later diagnosed as periodic catatonia. BMJ Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Sienaert P, Rooseleer J, De Fruyt J. Measuring catatonia: a systematic review of rating scales. J Affect Disord. 2011;135:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 121] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 31. | Grover S, Ghosh A, Ghormode D. Do patients of delirium have catatonic features? Psychiatry Clin Neurosci. 2014;68:644-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 32. | Oldham MA, Lee HB. Catatonia vis-à-vis delirium: the significance of recognizing catatonia in altered mental status. Gen Hosp Psychiatry. 2015;37:554-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 51] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 33. | Oldham MA. The Probability That Catatonia in the Hospital has a Medical Cause and the Relative Proportions of Its Causes: A Systematic Review. Psychosomatics. 2018;59:333-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 67] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 34. | Philbrick KL, Rummans TA. Malignant catatonia. J Neuropsychiatry Clin Neurosci. 1994;6:1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 116] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 35. | Lee BS, Huang SS, Hsu WY, Chiu NY. Clinical features of delirious mania: a series of five cases and a brief literature review. BMC Psychiatry. 2012;12:65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 36. | Caroff SN, Campbell EC, Sullivan KA. Neuroleptic malignant syndrome in elderly patients. Expert Rev Neurother. 2007;7:423-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 37. | Bush G, Petrides G, Francis A. Catatonia and other motor syndromes in a chronically hospitalized psychiatric population. Schizophr Res. 1997;27:83-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 38. | Grover S, Sahoo S, Chakravarty R, Chakrabarti S, Avasthi A. Comparative study of symptom profile of catatonia in patients with psychotic disorders, affective disorders and organic disorders. Asian J Psychiatr. 2019;43:170-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 39. | Ahuja N. Organic catatonia: a review. Indian J Psychiatry. 2000;42:327-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 40. | Levenson JL. Medical aspects of Catatonia. Prim Psychiatry. 2009;16:23-26. |
| 41. | Heinze M, Andreae D, Grohmann R. Rivastigmin and impaired motor function. Pharmacopsychiatry. 2002;35:79-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 42. | Litvan Z, Bauer M, Kasper S, Frey R. Electroconvulsive therapy with S-ketamine anesthesia for catatonia in coexisting depression and dementia. Int Psychogeriatr. 2017;29:1223-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 43. | Kendurkar A. Catatonia in an Alzheimer’s dementia patient. Psychogeriatrics. 2008;8:42-44. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 44. | Lauterbach EC, Kuppuswamy PS, Greenway LL. Differential pharmacological responses of catatonia-like signs in frontotemporal dementia. Neurocase. 2010;16:436-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 45. | Isomura S, Monji A, Sasaki K, Baba S, Onitsuka T, Ohara T, Mizoguchi Y, Kato TA, Horikawa H, Seki Y, Kanba S. FTD with catatonia-like signs that temporarily resolved with zolpidem. Neurol Clin Pract. 2013;3:354-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 46. | Holm AC. Neurodegenerative and psychiatric overlap in frontotemporal lobar degeneration: a case of familial frontotemporal dementia presenting with catatonia. Int Psychogeriatr. 2014;26:345-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 47. | Jaimes-Albornoz W, Ballesteros-Prado A, Serra-Mestres J. Catatonia in Patients with Frontotemporal Dementia. Eur Psychiatry. 2015;30:1436. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 48. | Bretag-Norris R, Gallur L, Flynn P. Heterogeneity in the psychiatric presentation of behavioural variant frontotemporal dementia (bvFTD). Australas Psychiatry. 2019;27:491-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 49. | Sayadnasiri M, Rezvani F. Treatment of Catatonia in Frontotemporal Dementia: A Lesson From Zolpidem Test. Clin Neuropharmacol. 2019;42:186-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 50. | Lakshmana R, Sundram S, Cairns F. Dementia with Lewy Bodies (DLB) presenting with catatonic symptoms. Psychogeriatrics. 2006;6:31-34. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 51. | Maeda K, Ogawa N. Amitriptyline and lorazepam improved catatonia and occipital hypoperfusion in a patient with DLB. Intern Med. 2011;50:363-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 52. | Fekete R. Renal failure in dementia with lewy bodies presenting as catatonia. Case Rep Neurol. 2013;5:10-13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 53. | Dhote J, Kipman A, Gasnier M. [Malignant catatonia in dementia with Lewy Body successfully treated with sismotherapy: A case report]. Encephale. 2020;46:155-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 54. | Beach SR, Praschan NC, Hogan C, Dotson S, Merideth F, Kontos N, Fricchione GL, Smith FA. Delirium in COVID-19: A case series and exploration of potential mechanisms for central nervous system involvement. Gen Hosp Psychiatry. 2020;65:47-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 140] [Cited by in RCA: 128] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 55. | Saito Y, Noto K, Kobayashi R, Suzuki A, Morioka D, Hayashi H, Otani K. Catatonia as the Initial Manifestation of Dementia with Lewy Bodies. Am J Case Rep. 2021;22:e932018. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 56. | Singh D, Forlano R, Athey R. Neuroleptic malignant syndrome and catatonia in a patient with dementia. Aust N Z J Psychiatry. 2008;42:547-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 57. | Valenstein M, Maltbie A, Kaplan P. Catatonia in the emergency department. Ann Emerg Med. 1985;14:359-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 58. | Amorim E, McDade EM. Rapidly-progressive catatonia responsive to zolpidem in a patient with ovarian teratoma-associated paraneoplastic encephalitis. J Clin Neurosci. 2016;30:136-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 59. | Morris NA, Kaplan TB, Linnoila J, Cho T. HSV encephalitis-induced anti-NMDAR encephalitis in a 67-year-old woman: report of a case and review of the literature. J Neurovirol. 2016;22:33-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 60. | Gough J, Coebergh J, Chandra B, Tabet N, Nilforooshan R. 4 A new era in psychiatry: ect and/or plasmapheresis? J Neurol Neurosurg Psychiatry. 2017;88:A29.1-A29. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 61. | Heckel B, Gibson EM, Shah O, McCall J. An atypical presentation of anti-HU receptor meningoencephalitis. Neurology. 2019;92:P2.2-0.25. |
| 62. | Park DG, Kim TJ, Yoon JH. Anti-NMDA receptor encephalitis presenting as catatonia associated with pheochromocytoma. Parkinsonism Relat Disord. 2020;72:62-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 63. | Giné-Servén E, Serra-Mestres J, Martinez-Ramirez M, Boix-Quintana E, Davi-Loscos E, Guanyabens N, Casado V, Muriana D, Torres-Rivas C, Cuevas-Esteban J, Labad J. Anti-NMDA receptor encephalitis in older adults: A systematic review of case reports. Gen Hosp Psychiatry. 2021;74:71-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 64. | Repchak AT, Quinn DK. Epileptic Catatonia: A Case Series and Systematic Review. Psychosomatics. 2016;57:217-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 65. | Hossain S. A case of catatonia-a diagnostic dilemma. Aust New Zeal J Psychiatry. 2021;55:111-112. |
| 66. | George R, Langford A. Intermittent catatonia and complex automatisms caused by frontal lobe epilepsy in dementia. BMJ Case Rep. 2017;2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 67. | Taniguchi G, Miyajima M, Watanabe M, Murata Y, Sone D, Watanabe Y, Okazaki M, Kobayashi-Kimura M, Kato M, Onuma T. Nonconvulsive status epilepticus in the elderly associated with newer antidepressants used at therapeutic doses: A report of three cases. Epilepsy Behav Case Rep. 2015;3:8-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 68. | Gaete G, Velásquez Á. [Ictal catatonia presentation as a non-convulsive status epilepticus: A case report]. Rev Med Chil. 2017;145:126-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 69. | Howard RJ, Low-Beer TS. Catatonia following biparietal infarction with spontaneous recovery. Postgrad Med J. 1989;65:316-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 70. | Saver JL, Greenstein P, Ronthal M, Mesulam MM. Asymmetric catalepsy after right hemisphere stroke. Mov Disord. 1993;8:69-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 71. | Hu HC, Chiu NM. Delayed diagnosis in an elderly schizophrenic patient with catatonic state and pulmonary embolism. Int J Gerontol. 2013;7:183-185. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 72. | AbdelRazek MA, Cheema Z, Yadollahikhales G. A psychiatric pitfall: Akinetic-mutism due to bilateral mesial frontal lobe infarction simulating catatonia. Neurol Psychiatry Brain Res. 2017;24:17-19. [DOI] [Full Text] |
| 73. | Altshuler LL, Cummings JL, Mills MJ. Mutism: review, differential diagnosis, and report of 22 cases. Am J Psychiatry. 1986;143:1409-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 74. | Spear J, Ranger M, Herzberg J. The treatment of stupor associated with MRI evidence of cerebrovascular disease. Int J Geriatr Psychiatry. 1997;12:791-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 75. | Starkstein SE, Petracca G, Tesón A, Chemerinski E, Merello M, Migliorelli R, Leiguarda R. Catatonia in depression: prevalence, clinical correlates, and validation of a scale. J Neurol Neurosurg Psychiatry. 1996;60:326-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 87] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 76. | Alisky JM. Is the immobility of advanced dementia a form of lorazepam-responsive catatonia? Am J Alzheimers Dis Other Demen. 2004;19:213-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 77. | Kamigaichi R, Kubo S, Ishikawa K, Yokoyama K, Ogaki K, Usui C, Hatta K, Arai H, Mochizuki H, Hattori N. Effective control of catatonia in Parkinson's disease by electroconvulsive therapy: a case report. Eur J Neurol. 2009;16:e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 78. | Poyraz BÇ, Aksoy Poyraz C, Yassa A, Arikan MK, Gündüz A, Kiziltan G. Recurrent Catatonia in Parkinson Disease. J Clin Psychopharmacol. 2016;36:104-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 79. | Fryml LD, Williams KR, Pelic CG, Fox J, Sahlem G, Robert S, Revuelta GJ, Short EB. The Role of Amantadine Withdrawal in 3 Cases of Treatment-Refractory Altered Mental Status. J Psychiatr Pract. 2017;23:191-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 80. | Taylor A, González-Montoya V. Unilateral deep brain stimulation masks undiagnosed epilepsy in a Parkinson’s Disease patient: A case report. Neurology. 2018;90:P2.342. |
| 81. | Grandal Leiros B, Roldán Larreta JJ, Moreno Eguinoa L. [Diagnosis and treatment of catatonia in the elderly]. Rev Esp Geriatr Gerontol. 2010;45:360-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 82. | Trzepacz PT, Murcko AC, Gillespie MP. Progressive supranuclear palsy misdiagnosed as schizophrenia. J Nerv Ment Dis. 1985;173:377-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 83. | Utumi Y, Iseki E, Arai H. Three patients with mood disorders showing catatonia and frontotemporal lobes atrophy. Psychogeriatrics. 2013;13:254-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 84. | Stan V, Su F, Weaver L, Schrift M, Gausche E. A case of rapidly progressive cognitive changes: The search for whipple’s disease. J Neuropsychiatry Clin Neurosci. 2016;28:e61-2. |
| 85. | Wang YT, Wu CL. Probable sporadic Creutzfeldt-Jakob disease mimicking a catatonic depression in an elderly adult. Psychogeriatrics. 2017;17:524-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 86. | Saint-Preux F, Nally E, Gurin L. Diagnosis and Treatment of Catatonia in Anoxic Brain. PM&R J. 2019;11:S163. |
| 87. | Mehra A, Grover S. Catatonia Associated with Hypernatremia. Indian J Psychol Med. 2019;41:293-295. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 88. | Tatreau JR, Laughon SL, Kozlowski T. Catatonia After Liver Transplantation. Ann Transplant. 2018;23:608-614. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 89. | Nasti J, Sud R. Catatonia associated with hypernatraemia in an elderly patient. Aust N Z J Psychiatry. 2011;45:88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 90. | McGuire E, Yohanathan M, Lally L, McCarthy G. Hyponatraemia-associated catatonia. BMJ Case Rep. 2017;2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 91. | McDaniel WW, Spiegel DR. Hyponatremia and abnormal ingestion of water in catatonia. Prim Psychiatr. 2010;17:29-33. |
| 92. | Pae CU, Kim TS, Lee C, Paik IH. Effect of aripiprazole for a patient with psychotic symptoms and parkinsonism associated with delayed-sequelae of carbon monoxide intoxication. J Neuropsychiatry Clin Neurosci. 2005;17:558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 93. | Shlykov MA, Rath S, Badger A, Winder GS. 'Myxoedema madness' with Capgras syndrome and catatonic features responsive to combination olanzapine and levothyroxine. BMJ Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 94. | Doran E, Sheehan JD. Acute catatonia on medical wards: a case series. J Med Case Rep. 2018;12:206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 95. | Carroll BT. Catatonia on the consultation-liaison service. Psychosomatics. 1992;33:310-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 96. | Meyen R, Acevedo-Diaz EE, Reddy SS. Challenges of managing delirium and catatonia in a medically ill patient. Schizophr Res. 2018;197:557-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 97. | Su FY, Fitch B, Coates R, Temporini H, Ruxin R. Catatonia as presenting symptoms of chronic recurrent urinary tract infection and its treatment. J Neuropsychiatry Clin Neurosci. 2021;33:256. |
| 98. | Gupta R, Saigal S, Joshi R, Tagore P, Rai N, Prasad K. Unrecognized catatonia as a cause for delayed weaning in Intensive Care Unit. Indian J Crit Care Med. 2015;19:693-694. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 99. | Gouse BM, Spears WE, Nieves Archibald A, Montalvo C. Catatonia in a hospitalized patient with COVID-19 and proposed immune-mediated mechanism. Brain Behav Immun. 2020;89:529-530. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 100. | Amouri J, Andrews PS, Heckers S, Ely EW, Wilson JE. A Case of Concurrent Delirium and Catatonia in a Woman With Coronavirus Disease 2019. J Acad Consult Liaison Psychiatry. 2021;62:109-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 101. | Dotson S, Hartvigsen N, Wesner T, Carbary TJ, Fricchione G, Freudenreich O. Clozapine Toxicity in the Setting of COVID-19. Psychosomatics. 2020;61:577-578. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 102. | Hockaday TD, Keynes WM, McKenzie JK. Catatonic stupor in elderly woman with hyperparathyroidism. Br Med J. 1966;1:85-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 24] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 103. | Parks KA, Parks CG, Onwuameze OE, Shrestha S. Psychiatric Complications of Primary Hyperparathyroidism and Mild Hypercalcemia. Am J Psychiatry. 2017;174:620-622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 104. | Yamaguchi H, Chiba Y, Katsuse O, Tamazawa A, Hirayasu Y. A case of subclinical Cushing's syndrome presenting as catatonia. Psychogeriatrics. 2019;19:402-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 105. | Farah A, McCall WV. ECT administration to a hyperthyroid patient. Convuls Ther. 1995;11:126-128. [PubMed] |
| 106. | Proenca M, Marques F, Cardoso D, Fonseca C. Catatonia as an internal medicine disease: infrequent or still underdiagnosed? BMJ Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 107. | Morcos N, Rosinski A, Maixner DF. Electroconvulsive Therapy for Neuroleptic Malignant Syndrome: A Case Series. J ECT. 2019;35:225-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 108. | Cottencin O, Warembourg F, de Chouly de Lenclave MB, Lucas B, Vaiva G, Goudemand M, Thomas P. Catatonia and consultation-liaison psychiatry study of 12 cases. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:1170-1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 109. | Lee JW. Neuroleptic-induced catatonia: clinical presentation, response to benzodiazepines, and relationship to neuroleptic malignant syndrome. J Clin Psychopharmacol. 2010;30:3-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 110. | Caroff SN, Mann SC, Keck PE Jr, Francis A. Residual catatonic state following neuroleptic malignant syndrome. J Clin Psychopharmacol. 2000;20:257-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 48] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 111. | Di Michele V, Bolino F. A novel treatment option of bipolar depression with psychotic and catatonic features. Gen Hosp Psychiatry. 2006;28:364-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 112. | Maia A, Cotovio G, Barahona-Corrêa B, Oliveira-Maia AJ. Diagnosis and Treatment of Neuroleptic Malignant Syndrome in the Intensive Care Unit: A Case Report. Acta Med Port. 2021;34:464-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 113. | Mashiah T, Mashiah A. Catatonic-like syndrome. Psychosomatics. 1983;24:1016-1019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 114. | Loeb E, Madigand J, Alexandre J, Dollfus S, Coquerel A, Fedrizzi S. Neuroleptic malignant syndrome and catatonia overlapping: 2 case reports. Psychopharmacology (Berl). 2015;232:2643-2644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 115. | Morrison PJ, Stanford CF, McCafferty FG. Catatonia in a 90-year-old patient after depot pipothiazine injection. Br J Psychiatry. 1988;152:865-866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 116. | Lucas GL, Adewumi AD. A case of quetiapine-induced catatonia. J Pharm Pract Res 2018; 48: 167-169. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 117. | Brakman M, de Graaff PJ, Visser EC. [Catatonic syndrome after single low dose of droperidol]. Ned Tijdschr Geneeskd. 2016;160:A9712. [PubMed] |
| 118. | Herrmann N, Lieff SJ. Drug-induced catatonia. Can J Psychiatry. 1988;33:633-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 119. | Collins CE, Thomas DJ, Gumpel JM. Catatonia in the allopurinol hypersensitivity syndrome. BMJ. 1991;302:970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 120. | Morita S, Miwa H, Kondo T. [A patient with probable dementia with Lewy bodies, who showed catatonia induced by donepezil: a case report]. No To Shinkei. 2004;56:881-884. [PubMed] |
| 121. | Plana MT, Blanch J, Romero S, Serra M, Gasto C. Toxic catatonia secondary to azithromycin. J Clin Psychiatry. 2006;67:492-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 122. | Zezoff D, Dinicu A, Nguyen C, Zargarian E, Hanna RM, Nguyen HA. A Case of Neurotoxicity in a Patient with Cefepime-Induced Nephrotoxicity. J Am Soc Nephrol. 2021;32:780. |
| 123. | Rajagopal S. Catatonic depression precipitated by amiodarone prescribed for atrial fibrillation. Indian J Psychiatry. 2015;57:105-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 124. | Karilainen H. Methotrexate induced leucoencephalopathy in a patient with rheumatoid arthritis. Scand J Rheumatol. 2013;42:426-427. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 125. | Aramada H. 43 Resolution of Calcineurin Inhibitor Induced Psychosis in a Kidney Transplant Recipient by Switching to Belatacept. Am J Kidney Dis. 9;73:653. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 126. | Little K, Tseng M. Imiquimod Treatment Associated With Hyponatremia and Catatonia in an Elderly Male: A Case Report. Psychosomatics. 2020;61:200-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 127. | Quinn DK, Rees C, Brodsky A, Deligtisch A, Evans D, Khafaja M, Abbott CC. Catatonia after deep brain stimulation successfully treated with lorazepam and right unilateral electroconvulsive therapy: a case report. J ECT. 2014;30:e13-e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 128. | Oldham MA, Desan PH. Alcohol and Sedative-Hypnotic Withdrawal Catatonia: Two Case Reports, Systematic Literature Review, and Suggestion of a Potential Relationship With Alcohol Withdrawal Delirium. Psychosomatics. 2016;57:246-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 129. | Reeves RR, Kamal A. Complicated Withdrawal Phenomena During Benzodiazepine Cessation in Older Adults. J Am Osteopath Assoc. 2019;119:327-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 130. | Andrade LC, Bosques M, Alamo J, Yepez-Kuri J. Psychotic depression after abrupt discontinuation of long-term use of benzodiazepines. J Am Geriatr Soc. 2019;67 Suppl 1:S179. |
| 131. | Belteczki Z, Ujvari J, Dome P. Clozapine Withdrawal-Induced Malignant Catatonia or Neuroleptic Malignant Syndrome: A Case Report and a Brief Review of the Literature. Clin Neuropharmacol. 2021;44:148-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 132. | Follet M, Lemoine X, Desbordes M, Guillin O, Petit M, Haouzir S. Tramadol improves catatonia: a case report. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32:1996-1997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 133. | Kumagai R, Kitazawa M, Ishibiki Y, Narumi K, Ichimiya Y. A patient with schizophrenia presenting with post-lobotomy catatonia treated with olanzapine: a case report. Psychogeriatrics. 2017;17:202-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 134. | Michael C, Michael A. Catatonia as a rare manifestation of gabapentin withdrawal. J Am Geriatr Soc. 2019;67 Suppl 1:S102. |
| 135. | Onishi H, Okuno S, Yae S, Sairenji M, Onose M, Mizuno Y, Kawanishi C. Brief psychotic disorder mimicking the symptoms of cerebrovascular attack evoked by symptoms that symbolized death in a patient with terminal stage stomach cancer: case report and review of the literature. Palliat Support Care. 2006;4:87-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 136. | Shiner E, Taylor L, Mohan A, Watson S, Sachdev PS. Severe depression masquerading as Creutzfeldt-Jakob disease. BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 137. | Van Haecke B, Titeca K, Lemmens G, Audenaert K. Effectiveness of electroconvulsive therapy for Cotard’s syndrome accompanied by catatonia: A case report. Tijdschr Geneeskd. 2014;70:1422-1428. |
| 138. | Simpson P, Kaul E, Quinn D. Cotard's syndrome with catatonia: a case presentation and discussion. Psychosomatics. 2013;54:196-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 139. | Suzuki K, Awata S, Matsuoka H. One-year outcome after response to ECT in middle-aged and elderly patients with intractable catatonic schizophrenia. J ECT. 2004;20:99-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 140. | Salam SA, Pillai AK, Beresford TP. Lorazepam for psychogenic catatonia. Am J Psychiatry. 1987;144:1082-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 141. | Harris D, Menza MA. Benzodiazepines and catatonia: a case report. Can J Psychiatry. 1989;34:725-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 142. | Shiloh R, Schwartz B, Weizman A, Radwan M. Catatonia as an unusual presentation of posttraumatic stress disorder. Psychopathology. 1995;28:285-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 143. | Takata T, Takaoka K, Fujigaki M. Catatonia in the elderly. Int J Psychiatry Clin Pract. 2005;9:230-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 144. | Lin CC, Hung YY, Tsai MC, Huang TL. The Lorazepam and Diazepam Protocol for Catatonia Due to General Medical Condition and Substance in Liaison Psychiatry. PLoS One. 2017;12:e0170452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 145. | Ungvari G, Leung C, Pang AH, White E. Benzodiazepine Treatment of Catatonia in the Elderly. Hong Kong J Psychiatry. 1994;4:33-38. |
| 146. | Morena G, Sunderland B, Billig N. Midazolam and the treatment of catatonia in major depression in an older adult. Psychosomatics. 1994;35:392-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 147. | Raymond V, Véry E, Jullien A, Eyvrard F, Anguill L, Yrondi A. Case Report: Use of Subcutaneous Midazolam During an Episode of Catatonia. Front Psychiatry. 2021;12:666646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 148. | Challa S, Setters B. Catatonia: Not just another "mental status change”. J Am Geriatr Soc. 2010;58 Suppl 1:S202-S203. |
| 149. | Madhusoodanan S, Bogunovic OJ. Safety of benzodiazepines in the geriatric population. Expert Opin Drug Saf. 2004;3:485-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 130] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 150. | Meyer JP, Swetter SK, Kellner CH. Electroconvulsive Therapy in Geriatric Psychiatry: A Selective Review. Psychiatr Clin North Am. 2018;41:79-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 151. | Bean E, Findlay C, Gee C, Amin J. Refractory catatonia in old age: a case report. J Med Case Rep. 2021;15:406. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 152. | Cristancho P, Jewkes D, Mon T, Conway C. Successful use of right unilateral ECT for catatonia: a case series. J ECT. 2014;30:69-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 153. | Pritchett C, Hermida A, Job G. Ultrabrief Right Unilateral Ect and Catatonia: a Case Series and Literature Review. Am J Geriatr Psychiatry. 2020;28 Suppl 1:S88. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 154. | Suzuki K, Shindo T, Katsura M, Takamatsu K, Ebina Y, Takano T, Awata S, Matsuoka H. Resolution of catatonia by successful seizure induction via electroconvulsive therapy with electrodes applied bilaterally to the parietotemporal region. J ECT. 2007;23:103-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 155. | Jain S, Ferrando SJ. Manganese neurotoxicity presenting with depression, psychosis and catatonia. Psychosomatics. 2011;52:74-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 156. | Gosselink MJ, Schenkeveld KW, Trines SA, van Vliet IM. Successful electroconvulsive therapy in a 95-year-old man with a cardiac pacemaker--a case report. Am J Geriatr Psychiatry. 2011;19:678-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 157. | Lazaro JC, Dantas CDR. Electroconvulsive therapy and anticoagulation after pulmonary embolism: A case report. J Bras Psiquiatr. 2014;63:182-184. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 158. | O'Reardon JP, Cristancho MA, Ryley B, Patel KR, Haber HL. Electroconvulsive therapy for treatment of major depression in a 100-year-old patient with severe aortic stenosis: a 5-year follow-up report. J ECT. 2011;27:227-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 159. | Inagawa Y, Saito S, Okada T, Inoue K, Suda S. Electroconvulsive Therapy for Catatonia With Deep Venous Thrombosis: A Case Series. Prim Care Companion CNS Disord. 2018;20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 160. | Fraser LM, O'Carroll RE, Ebmeier KP. The effect of electroconvulsive therapy on autobiographical memory: a systematic review. J ECT. 2008;24:10-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 142] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 161. | Lim J, Yagnik P, Schraeder P, Wheeler S. Ictal catatonia as a manifestation of nonconvulsive status epilepticus. J Neurol Neurosurg Psychiatry. 1986;49:833-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 43] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 162. | Ueda S, Takeuchi J, Okubo Y. Successful use of olanzapine for catatonia following delirium. Psychiatry Clin Neurosci. 2012;66:465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 163. | Beach SR, Gomez-Bernal F, Huffman JC, Fricchione GL. Alternative treatment strategies for catatonia: A systematic review. Gen Hosp Psychiatry. 2017;48:1-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 99] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 164. | Foguet-Boreu Q, Coll-Negre M, Serra-Millàs M, Cavalleria-Verdaguer M. Neuroleptic malignant syndrome: a case responding to electroconvulsive therapy plus bupropion. Clin Pract. 2018;8:1044. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 165. | Clinebell K, Azzam PN, Gopalan P, Haskett R. Guidelines for preventing common medical complications of catatonia: case report and literature review. J Clin Psychiatry. 2014;75:644-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 166. | McDaniel WW, Spiegel DR, Sahota AK. Topiramate effect in catatonia: a case series. J Neuropsychiatry Clin Neurosci. 2006;18:234-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 167. | Kritzinger PR, Jordaan GP. Catatonia: an open prospective series with carbamazepine. Int J Neuropsychopharmacol. 2001;4:251-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 168. | Liu YW, Chang C, Chen TY, Chang HA, Kao YC, Tzeng NS. Refractory depression with catatonic features was remitted with administration of intravenous dopamine and consequent bupropion as maintenance treatment. Aust N Z J Psychiatry. 2016;50:599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 169. | Prowler ML, Weiss D, Caroff SN. Treatment of catatonia with methylphenidate in an elderly patient with depression. Psychosomatics. 2010;51:74-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 170. | van den Hoven DJ, aan de Stegge BM, Ayodeji ID. Remission of catatonia after intravenous propofol infusion for unrelated reasons. Netherlands J Crit Care. 2021;29:222-225. |
| 171. | Galova A, Berney P, Desmeules J, Sergentanis I, Besson M. A case report of cholinergic rebound syndrome following abrupt low-dose clozapine discontinuation in a patient with type I bipolar affective disorder. BMC Psychiatry. 2019;19:73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 172. | Franz M, Gallhofer B, Kanzow WT. Treatment of catatonia with intravenous biperidene. Br J Psychiatry. 1994;164:847-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 173. | Nicolato R, Romano-Silva MA, Correa H, dos Santos RR, Teixeira AL. Stuporous catatonia in an elderly bipolar patient: response to olanzapine. Aust N Z J Psychiatry. 2006;40:498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 174. | Sugawara H, Takamatsu J, Hashimoto M, Ikeda M. Catatonia associated with late-life psychosis successfully treated with lithium: a case report. Ann Gen Psychiatry. 2021;20:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 175. | Shiozawa P, da Silva ME, Cordeiro Q. Transcranial Direct Current Stimulation for Treating Depression in a Patient With Right Hemispheric Dominance: A Case Study. J ECT. 2015;31:201-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 176. | Ishida T, Sakurai H, Watanabe K, Iwashita S, Mimura M, Uchida H. Incidence of deep vein thrombosis in catatonic patients: A chart review. Psychiatry Res. 2016;241:61-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 177. | Carroll BT, Spetie L. Catatonia on the consultation-liaison service: a replication study. Int J Psychiatry Med. 1994;24:329-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 178. | Karlamangla A, Tinetti M, Guralnik J, Studenski S, Wetle T, Reuben D. Comorbidity in older adults: nosology of impairment, diseases, and conditions. J Gerontol A Biol Sci Med Sci. 2007;62:296-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 89] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 179. | Connell J, Kim A, Brummel NE, Patel MB, Vandekar SN, Pandharipande P, Dittus RS, Heckers S, Ely EW, Wilson JE. Advanced Age Is Associated With Catatonia in Critical Illness: Results From the Delirium and Catatonia Prospective Cohort Investigation. Front Psychiatry. 2021;12:673166. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 180. | Llesuy JR, Coffey MJ, Jacobson KC, Cooper JJ. Suspected Delirium Predicts the Thoroughness of Catatonia Evaluation. J Neuropsychiatry Clin Neurosci. 2017;29:148-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 181. | Neary D, Snowden JS, Gustafson L, Passant U, Stuss D, Black S, Freedman M, Kertesz A, Robert PH, Albert M, Boone K, Miller BL, Cummings J, Benson DF. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998;51:1546-1554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3387] [Cited by in RCA: 3507] [Article Influence: 125.3] [Reference Citation Analysis (0)] |
| 182. | Francis A. Catatonia: diagnosis, classification, and treatment. Curr Psychiatry Rep. 2010;12:180-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 183. | Van Den Eede F, Van Hecke J, Van Dalfsen A, Van den Bossche B, Cosyns P, Sabbe BG. The use of atypical antipsychotics in the treatment of catatonia. Eur Psychiatry. 2005;20:422-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 70] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 184. | Guinart D, Misawa F, Rubio JM, Pereira J, de Filippis R, Gastaldon C, Kane JM, Correll CU. A systematic review and pooled, patient-level analysis of predictors of mortality in neuroleptic malignant syndrome. Acta Psychiatr Scand. 2021;144:329-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 185. | Wang PS, Schneeweiss S, Avorn J, Fischer MA, Mogun H, Solomon DH, Brookhart MA. Risk of death in elderly users of conventional vs. atypical antipsychotic medications. N Engl J Med. 2005;353:2335-2341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 675] [Cited by in RCA: 619] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 186. | Rosebush PI, Mazurek MF. Catatonia after benzodiazepine withdrawal. J Clin Psychopharmacol. 1996;16:315-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 54] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 187. | Nivoli AM, Murru A, Pacchiarotti I, Valenti M, Rosa AR, Hidalgo D, Virdis V, Strejilevich S, Vieta E, Colom F. Bipolar disorder in the elderly: a cohort study comparing older and younger patients. Acta Psychiatr Scand. 2014;130:364-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 188. | Zaman H, Gibson RC, Walcott G. Benzodiazepines for catatonia in people with schizophrenia or other serious mental illnesses. Cochrane Database Syst Rev. 2019;8:CD006570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: Spain
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kaur M S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ