Published online May 19, 2021. doi: 10.5498/wjp.v11.i5.189
Peer-review started: February 16, 2021
First decision: March 16, 2021
Revised: March 28, 2021
Accepted: April 21, 2021
Article in press: April 21, 2021
Published online: May 19, 2021
Processing time: 85 Days and 17.6 Hours
An inconclusive result from BRCA1/2 genetic testing indicates that a genetic variant of uncertain significance is detected. This case constitutes the majority of genetic test results, but studies specifically addressing the psychological adjustment of people with inconclusive results are scarce.
To examine psychological outcomes of receiving an uninformative BRCA1/2 test result.
PubMed, PsychInfo, and Cochrane Central Register of Controlled Trials were screened for studies focusing on distress, anxiety, and depression levels in individuals with inconclusive genetic test results. This review is based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses method.
Studies on psychological outcomes of inconclusive BRCA1/2 focused on general and specific distress, anxiety, and depression. Overall, they produced mixed results. These inconsistent findings are probably due to the uncertainty caused by this type of result, that may also influence the decisions of individuals about surveillance and prophylactic options, reducing their compliance. In addition, this review highlights specific risk and protective factors that affect psychological adjustment in individuals with an inconclusive genetic testing result.
Individuals with inconclusive genetic test results need specific educational programs and support to better understand the meaning of their results in order to be able to make decisions about surveillance and prophylactic options.
Core Tip: Undergoing BRCA1/2 genetic testing can produce a significant psycho-social impact. The possible test results are positive (increased risk of developing cancer), negative (the same probability of developing cancer as the general population), or inconclusive. This last outcome produces a more complex situation, as it means that a deleterious mutation is neither identified nor definitively excluded. Though the inconclusive case constitutes most genetic test results, studies specifically addressing psychological adjustment of people with such a result are scarce. The current review aims to address this gap, highlighting psychological outcomes following this kind of result and highlighting specific risk and protective factors.
- Citation: Bramanti SM, Trumello C, Lombardi L, Cavallo A, Stuppia L, Antonucci I, Babore A. Uncertainty following an inconclusive result from the BRCA1/2 genetic test: A review about psychological outcomes. World J Psychiatr 2021; 11(5): 189-200
- URL: https://www.wjgnet.com/2220-3206/full/v11/i5/189.htm
- DOI: https://dx.doi.org/10.5498/wjp.v11.i5.189
In the context of breast and ovarian cancer surveillance, genetic screening for the detection of mutations in BRCA1 (chromosome 13) and BRCA2 (chromosome 17) genes is a significant advance in cancer care. Each individual carries these two genes, which are responsible for the control and repair of DNA alterations; however, in their mutated form, they are linked to an increased risk of tumor development[1]. These genes are characterized by autosomal dominant inheritance, so one parent has a 50% chance of transmitting them to their children[1,2]. The lifetime risk of developing breast cancer in the general population ranges from 10%-14%, and this risk rises to 85% in women who carry a mutation in the BRCA1 and BRCA2 genes[2,3].
For individuals with high cancer history, genetic counselling is proposed. Medical and family histories are collected, and if there is at least 10% likelihood, a buccal smear or a blood sample is taken. The possible test results are positive, negative, or inconclusive[4]. The first one implies that the individual is a carrier of a mutation with an increased risk of developing cancer during his life. A negative result means that the individual is not a carrier of mutation, so he has the same probability of developing cancer as the general population. An inconclusive result produces a more complex situation, as it means that a deleterious mutation is neither identified nor definitively excluded. This may be due to two main reasons: (1) No known BRCA1/2 mutations were found, but a genetic variant of uncertain significance is detected; and (2) Not detecting a mutation in a cancer-affected person who is the first member tested (proband) in a high-risk family[5,6]. In the current review we indistinctly use the terms “inconclusive” and “uninformative” to refer to both the aforementioned situations. Though the inconclusive case constitutes the majority of genetic test results[1,7], research and clinical attention is lacking in this topic, as stated by several authors[5,8].
Undergoing genetic testing and its results can produce a significant psycho-social impact[2,9]. Generally, individual who receives a positive test result reports higher levels of distress, anxiety, and depression[10] while who receives a negative test result reports a decrease in distress levels following the discovery of test results[11]. A recent review of existing literature[12] highlighted that a positive genetic testing results can be traumatic, although not all individuals with such a result experience increased distress. The high distress levels experienced by individuals who receive a positive test results may depend by an increased risk of future diseases and the implications for their whole family[12]. A study highlighted that a possible factor that influences affective states is the perceived risk of developing cancer, regardless of test result[13]. Overall, higher levels of distress, anxiety and depression could depend by some risk factors as having a cancer diagnosis, having a greater history of breast/ovarian cancer, being younger than 40 years old, being unmarried and having high pre-test levels of anxiety and depression[12].
As for those who receive an inconclusive result, the literature is conflictual; some studies identify higher levels of distress in those with an inconclusive result[14] while other studies found that individuals who receive an inconclusive result seem reassured[15]. However, as stated by several authors[12,16], studies specifically addressing psychological adjustment of people with inconclusive genetic test results are scarce. According to Vadaparampil et al[8], this gap should be filled, as the topic of inconclusive test results is a key topic deserving clinical and research attention.
Starting from these premises, the main purpose of the current review was to investigate short-, intermediate-, and long-term consequences of receiving uninformative BRCA1/2 test results. To pursue this aim, we analyzed cross-sectional and longitudinal studies which examined anxiety, depression and distress in individuals who receive inconclusive results compared to positive and negative results. In addition, we aimed to highlight risk and protective factors that affect psychological adjustment in individuals with an inconclusive genetic testing result, also considering differences associated with being or not affected by a cancer diagnosis.
This systematic review followed the guidelines of Preferred Reporting Items for Systematic Review and Meta-Analyses[17].
We conducted a comprehensive literature search in PubMed, PsychInfo, and Cochrane Central Register of Controlled Trials. All search results were limited to the last 21 years (1999-2020).
We combined search terms related to genetic counselling and its result [(Genetic*, Familial*, OR Mutation*) and (Inconclusive OR Uncertain) and (Breast* OR BRCA*)] with terms relating to psychological outcomes (Psycho*, Distress, Emot*, Anxiety, OR Depression). The reference sections of previous reviews were also checked to ensure that all relevant studies for this review were included.
Studies were included if they: Analyzed psychological outcomes of receiving an uncertain result; included adult, human subjects; and were written in the English language.
Exclusion criteria were: Articles not specific to BRCA mutation; articles not reporting psychological outcomes; articles that assessed the impacts of genetic counselling before subjects received genetic test results; and literature reviews, qualitative studies, commentaries, letters to the editor, unpublished articles and doctoral theses, abstracts of conferences, congresses, books, and case-reports.
Following the review by Hamilton et al[18], we defined short-term as within 1 mo of genetic testing results, intermediate term between 1 and 6 mo, and long-term over 6 mo.
The eligibility criteria were evaluated according to the following aspects: Participants, intervention, comparison, outcome, and study design. (1) Participants: Human adult participants receiving an uncertain result from genetic testing about the presence of BRCA mutation; (2) Intervention: The focus was not limited on a specific intervention; (3) Comparison: Studies comparing people with inconclusive genetic test results to positive and negative results; (4) Outcomes: We analyzed studies that considered short- (1 mo), intermediate- (1-6 mo), and long- (6+ mo) term psychological outcomes (i.e., general and specific distress, anxiety, and depression); and (5) Study design: We included observational and/or quantitative studies.
Anxiety, depression, and distress (both general and specific) have been the focus of the review as they were the outcome measures most frequently evaluated.
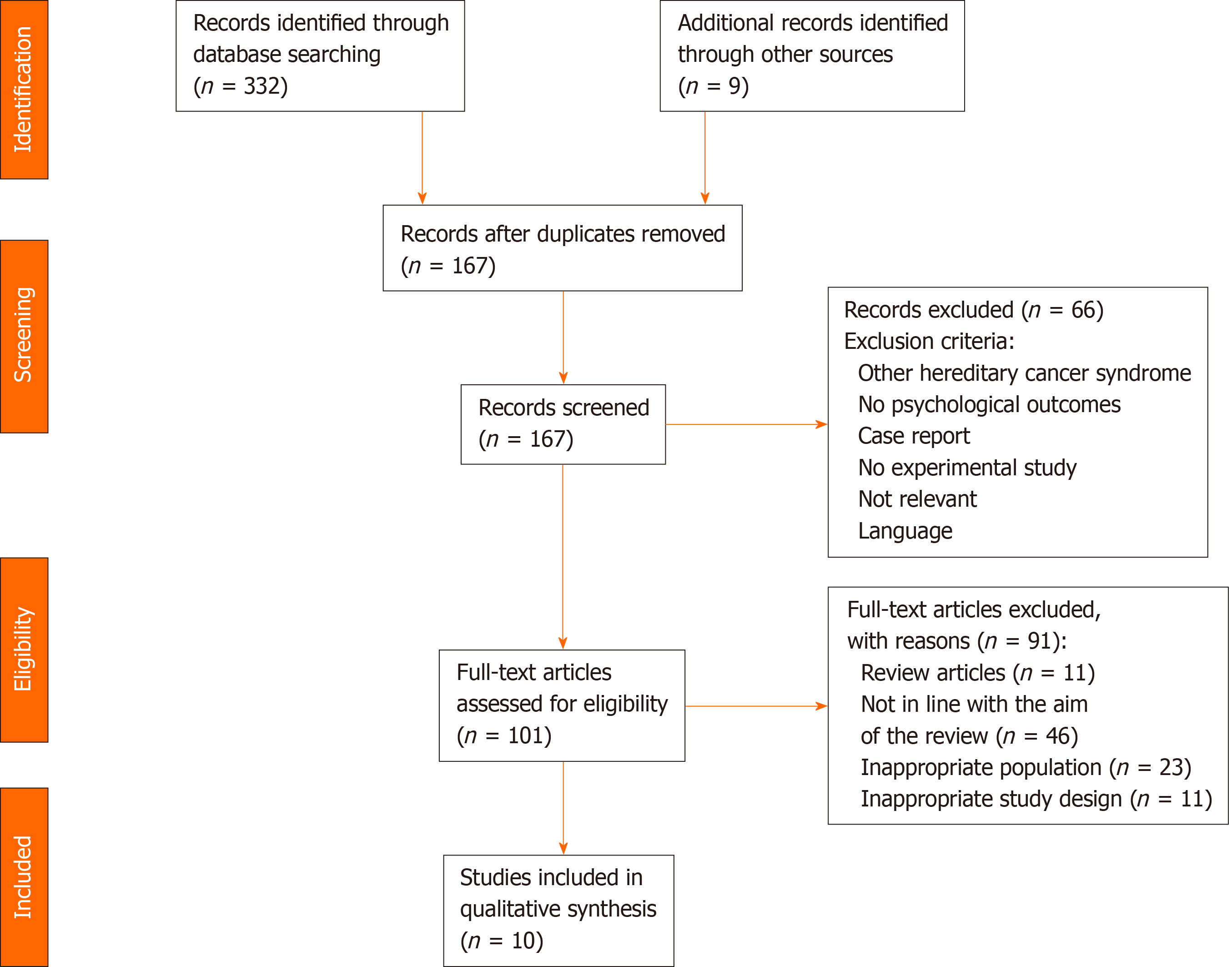
A total of 341 studies were identified; of those, 174 were removed as duplicates. The titles of the selected studies were double screened by two authors independently, 66 studies were excluded because they were not consistent with the eligibility criteria. The abstract of 101 selected studies and the full text of all potentially relevant articles were double screened and evaluated by two authors independently; discrepancies were resolved by discussion; the following were excluded: 11 were reviews, 46 did not focus on psychological variables, 23 studies involved a sample with a different genetic mutation from BRCA or did not focus on inconclusive results, and 11 had an inadequate study design (qualitative studies, unpublished articles, case-reports, books or abstracts of congresses). A total of 10 articles met our inclusion criteria and were, therefore, considered in this systematic review (Figure 1). Included studies were published between 2002-2017 and were most commonly conducted in the United States, followed by Canada and the United Kingdom. Eight studies were longitudinal (80%) and two were cross-sectional (20%). All the included studies were classified on the basis of the timing of questionnaire administration; most studies (n = 7) assessed also baseline levels of psychological measures before the blood test or buccal smear test.
Only one study considered exclusively short-term psychological outcomes, four studies only intermediate-term, and three studies long-term (Table 1). Sample sizes from the reviewed studies ranged from 48 to 465 (mean = 193.30, standard deviation = 135.14), resulting in a total of 1933 participants. Of these, 38% (n = 730) received inconclusive test results, 32% (n = 620) received negative results, 21% (n = 408) received positive results, 7% (n = 126) decided not to undergo genetic testing, and 2% (n = 49) were still waiting for their test results. Only two studies included male participants; the sample was predominantly female (98%).
| Ref. | Average months after genetic test disclosure | ||
| ≤ 1 m | Between 1 and 6 mo | More than 6 mo | |
| Bish et al[29], 20021 | Y | Y | |
| Claes et al[24], 20041 | Y | ||
| Graves et al[36], 20121 | Y | ||
| Lumish et al[27], 2017 | Y | ||
| Manne et al[22], 20041 | Y | ||
| O’Neill et al[20], 20061 | Y | ||
| O’Neill et al[6], 2009 | Y | Y | |
| Power et al[21], 2011 | Y | ||
| Schwartz et al[31], 20021 | Y | ||
| Smith et al[25], 20081 | Y | Y | |
Of the reviewed articles, six studies compared people with and without a cancer history. The majority of the sample (73%) had a cancer diagnosis. Only four studies reported the type of cancer diagnosis; of these, 94% had breast cancer, 4% had ovarian cancer, and 2% had both.
The findings were divided into four categories: (1) General distress; (2) Anxiety; (3) Depression; and (4) Genetic testing-specific distress. The tools used for the evaluation of each construct are synthesised in Table 2.
| Ref. | C country | AAim | Study design | Psychological measurements | Sample size and gene mutation status | Personal cancer history |
| Bish et al[29], 2002 | United Kingdom | Examine the effects of an uncertain test results affects mood and behavior | Longitudinal | HADS; IES; GHQ-28; Cancer Worry Scale | Total sample = 48. Positive = 0. Negative = 0. Inconclusive = 48 | History = 48. No history = 0 |
| Claes et al[24], 2004 | United States | Evaluate the impact of a genetic test result | Retrospective | IES; STAI; SCL-90; UCL; Semi structured-interview | Total sample = 48. Positive = 18. Negative = 6. Inconclusive = 24 | History = 48. No history = 0 |
| Graves et al[36], 2012 | United States | Evaluate the long-term psychosocial impact of the genetic test result | Longitudinal | IES; STAI; BSI; PSS; MICRA | Total sample = 465. Positive = 144. Negative = 60. Inconclusive = 261 | History = 390. No history = 75 |
| Lumish et al[27], 2017 | United States | Investigate the psychological outcomes of people who undergoing genetic test | Cross-sectional | IES; MICRA; SWD; AT-20 | Total sample = 232. Positive = 25. Negative = 173. Inconclusive = 34 | History = 129. No history = 103 |
| Manne et al[22], 2004 | United States | Evaluate the distress related to undergoing the genetic test | Longitudinal | IES; BSI; Discussion about testing; Sharing of concerns; Comfort sharing concerns; Protective Buffering; Relationship strain; Support/encouragement for testing; Perceived negative partner behaviors. | Total sample = 144. Positive = 38. Negative = 15. Inconclusive = 91 | History = 115. No history = 29 |
| O’Neill et al[20], 2006 | United States | Explore psychological consequence and the tolerance of uncertain in women who receive an inconclusive test result | Longitudinal | IES; BSI; MICRA; IUS | Total sample = 64. Positive = 0. Negative = 0. Inconclusive = 64 | History = 64. No history = 0 |
| O’Neill et al[6], 2009 | United States | Assess differences in distress levels over time | Longitudinal | IES; BSI; MICRA | Total sample = 209. Positive = 0. Negative = 190. Inconclusive = 19 | History = 209. No history = 0 |
| Power et al[21], 2011 | Canada | Examine levels of distress in people undergoing genetic test | Cross-sectional | History Questionnaire; Feelings about Test Results Measure; Psychosocial Needs Questions; BSI-18 | Total sample = 318. Positive = 85. Negative = 51. Inconclusive = 33. Attending result = 49. Not undergo genetic test = 100 | History =160. No history = 158 |
| Schwartz et al[31], 2002 | United States | Examine the long-term psychological impact of receiving BRCA 1/2 test result | Longitudinal | IES; HSCL-25 | Total sample = 279. Positive = 78. Negative = 58. Inconclusive = 143 | History = 186. No history = 93 |
| Smith et al[25], 2008 | United States | Evaluate psychological consequences of genetic test results | Longitudinal | GSI; IES; PSS; STAI; CES-D; QoLS | Total sample = 126. Positive = 20. Negative = 67. Inconclusive = 13. Not undergo genetic test = 26 | History = 58. No history = 68 |
The Brief Symptoms Inventory (BSI)[19-22], the Symptom Checklist 90 Revised (SCL-90)[23-25], the Impact of Event Scale[26,27], the General Health Questionnaire[28,29], and the Hopkins Symptom Checklist[30,31] were used to assess general distress symptoms. Depressive symptoms were assessed using the BSI[6,19,20], the SCL-90[23,24], the Hospital Anxiety and Depression Scale (HADS)[29,32], and the Center for Epidemiologic Studies Depression Scale[25,33].
The BSI[6,19,20], the SCL-90[23,24], the HADS[29,32], and the State Trait Anxiety Invento
Finally, genetic testing-specific distress was evaluated by means of the Multidimen
The majority of the reviewed studies did not find significant differences in psychological adjustment among individuals who received inconclusive, positive and negative results[22,24,25,29,31]. One study observed higher levels of distress, especially on the somatization scale, in those who received inconclusive results compared with positive and negative results, and people deciding not to undergo genetic testing[21]. Instead, a recent study of Lumish et al[27] highlighted that individuals receiving an inconclusive result reported intermediate levels of general distress, higher than negative but lower than positive result.
Schwartz et al[31] did not find increased levels of distress in people with inconclusive results compared to positive and negative results, but they did not identify a decrease in distress levels in the intermediate-term (i.e., 1-6 mo) in individuals with inconclusive results, which occurs in those who receive negative results. Two studies found that general distress decreased slightly over time, from pre-test to 6 mo post-test[20,25]. Other studies reported that there were no differences in distress levels from pre-test levels up to 6 mo after genetic test disclosure[22,29].
Regarding differences between cancer affected patients and unaffected patients, overall, unaffected patients with positive or inconclusive results reported higher levels of distress compared to both affected patients and unaffected patients with negative results[27]. Other studies highlighted that having had a cancer diagnosis did not influence distress levels; in fact, they did not detect differences between affected and unaffected patients[21,22,25].
In addition to genetic test results, other factors which could increase distress levels in those who receive an inconclusive result may be a cancer diagnosis[27], higher distress levels before genetic testing[25], the intolerance of uncertainty[20], and cancer-related distress[20].
However, there are also some protective factors that could mitigate or decrease distress levels such as marital status[20], partner support, and protective buffering[21].
None of the reviewed studies found differences in anxiety levels among individuals with inconclusive, positive and negative results[24,25,29] except for one study that found that patients with inconclusive results reported higher levels of anxious symptoms after test result disclosure than negative ones[6].
Some studies observed anxious symptoms in the intermediate-term[25] and long-term[6,29]. Two studies of these did not find changes in anxiety levels in the intermediate-term[25,29], while O’Neill et al[6] detected a decrease in anxiety over time for individuals who received negative test result and stable levels of anxiety in those who received inconclusive results from the discovery of the test result up to 6 mo later, with a subsequent decrease.
Only one of the reviewed articles that focused on anxiety investigated whether there were differences among affected and unaffected patients and found that there were no differences between them[25].
Overall, some factors that could influence anxiety levels in individuals who receive an inconclusive test results, might be: Higher distress levels before genetic testing[25], higher pre-testing anxiety[6], correctly interpreting the meaning of the genetic test result[24,29], primary appraisal, namely the way people evaluate the importance of a stressful situation[6], and ethnicity[6].
Four of the included studies focused on depression[6,24,25,29]. The majority of the reviewed studies did not identify differences between those receiving inconclusive, positive and negative results[24,25,29].
Two studies did not identify effects of time on depression in the intermediate-term[25,29]. Only one study analyzed long-term outcomes (6 mo), highlighting that depressive levels were significantly higher in individuals receiving inconclusive results compared to negative[6].
Having received a cancer diagnosis did not influence depressive levels, regardless of the test results[25]. Other factors could influence depressive levels among individuals who receive an inconclusive test result: Misinterpretation of test results[24,29], pre-test depressive levels[6,25], primary appraisal[6], and ethnicity[6].
Four of the included studies focused on genetic testing-specific distress[6,20,27,36], which was assessed only after genetic test disclosure. All the reviewed studies measured specific distress in the long-term[6,27,36] except for one study that assessed it in the intermediate-term[20].
Two studies found that inconclusive results were associated with lower levels of genetic testing-specific distress than positive test results[27,36] but higher than negative results[27,36].
Higher levels of genetic testing-specific distress were observed from 1-6 mo and 1 year after genetic test disclosure[6,20,36]; specifically, individuals with inconclusive results reported higher levels of specific distress persisting even 1 year after test disclosure[6]. O’Neill et al[6] detected that distress levels among inconclusive results stayed stable over time and decreased among negative results.
Individuals affected by cancer who receive inconclusive results showed higher levels of distress related to genetic testing than unaffected individuals with inconclusive results, affected carriers, and both affected and unaffected non-carriers[27]. On the contrary, Graves et al[36] identified that mutation carriers with a cancer diagnosis had higher levels of distress than affected individuals with uncertain results.
In general, some potential risk factors that could influence genetic testing-specific distress in individuals who receive an inconclusive result are higher pre-test perceived risk[6,20], lower education level[27,36], younger age[27,36], ethnicity[6,36], lower genetic knowledge[27], coping with uncertainty[20], confusion regarding the interpretation of test results[27], pre-test distress[6,36], pre-test anxiety[36], and stronger levels of primary appraisal[6]. Some protective factors, such as being married[36] and stronger secondary appraisal[6], can reduce distress related to genetic testing.
The main purpose of the current review was to investigate the consequences of receiving inconclusive results from BRCA1/2 genetic testing on psychological outcomes such as general distress, anxiety, depression, and genetic testing-specific distress. To our knowledge, our review is the first to explore the short-, intermediate-, and long-term psychological effects of receiving inconclusive results in both affected and unaffected patients, as previous reviews were mainly based on individuals who receive a positive or a negative result[12,13,37]. From the analysis of the selected articles, overall different results were found.
Most studies (five of the ten considered) did not report differences in levels of general distress, anxiety, and depression among individuals with inconclusive results, as compared with both positive and negative results[22,24,25,29,31]. Other studies have found that those who receive inconclusive results experience higher levels of general and specific distress, anxiety, and depression than who have a negative result[6,27,36], but lower than positive ones[27,36]; and finally, a study identified that the inconclusive results caused greater levels of general distress when compared with both positive and negative results[21].
The differences detected from the reviewed studies might depend on the different tools used to assess distress, anxiety, and depression, which might not be sufficiently sensitive in this field[12]. As evidenced by a study by Power et al[21], individuals with an uninformative BRCA1/2 test result reported higher levels of distress, specifically in the somatization scale, so it could be that this subgroup of patients experienced distress through the body. Hence, it could be useful to develop more sensible tools, specifically addressing this field.
Although no differences were found between negative and inconclusive results, there was no decrease over time in the levels of distress, anxiety, or depression, which instead occurred in individuals with a negative result[6,31]. A possible explanation for these results might be the lack of relief from this type of test result[16] and having to copy with the uncertainty[21,24,29,38,39]. Indeed, individuals who have difficulty in coping with uncertainty have higher levels of ongoing distress[20]. The uncertainty related to this type of result also influences the decisions of individuals about surveillance and prophylactic options; only a fraction of patients who receive this type of result decides to increase cancer screening[27]. Moreover, some patients determine not to carry out preventive surgery, as they need a more certain result before deciding on this irreversible option[24], from which psychological benefits might be derived due to the cancer risk decrease[40], or it can also lead to adverse psychological impacts and dissatisfaction[41-43]. Graves et al[36] identified that having prophylactic surgery does not reduce distress levels but only the perceived risk of developing cancer.
Two studies showed that individuals with a cancer diagnosis have greater levels of distress, anxiety, and depression than those without a previous cancer diagnosis[27,36]; in the group of affected people, being mutation carriers[36] or having received an inconclusive result[27] were associated with a worse psychological adjustment. Patients with a recent cancer diagnosis could represent a population more vulnerable to higher levels of distress, anxiety, and depression due to the impact of the diagnosis and its treatment[44,45]. Other studies did not find differences between affected and unaffected patients[20,25,31]. A possible explanation for these inconsistent results could be the psychological benefit that affected patients derived from genetic testing[12,37], because medical surveillance protocols make the process predictable and understandable[37]. Due to this, affected patients and individuals who receive a positive test result might be better able to cope with this situation than individuals who have to cope with the uncertainty[20,46,47].
Apart from having had a cancer diagnosis[27,36], other factors that influence the psychological outcomes related to genetic test disclosure also emerged from the current review. Among the major risk factors are: Higher pre-test levels of distress and anxiety[6,24,25,31], younger age[6,22,27,36], correctly interpreting the meaning of the test result[24,29], intolerance of uncertainty[20], use of the primary appraisal[6], higher perceived risk before genetic testing[6,20], having a family history of cancer[25,36], lower education level[27,36], lower genetic knowledge[27], having children[36], lower income[36], and belonging to a minority ethnicity[6]. Regarding appraisal, it consists in the evaluation of the relevance of a stressful event such as genetic testing and/or cancer diagnosis[48,49]. Some studies have shown that different coping and evaluation strategies influence distress and stress levels; using a higher primary appraisal and emotional suppression are associated with higher levels[50,51], while increased use of secondary appraisal and cognitive reappraisal are associated with better psychological outcomes[50,52].
In addition to secondary appraisal and cognitive reappraisal, other factors could decrease distress levels such as being married[20,36], having partner support[22], having a bilateral salpingo-oophorectomy[36], and protective buffering[22].
This review revealed that those who receive inconclusive results are a subgroup of patients who need educational programs and more pre-test information to better understand the meaning of their test so they can make decisions about surveillance and prophylactic options.
This literature review has some limitations. First, only a few studies were included in this review because the majority of studies focus on the psychological outcomes of those who receive positive or negative results, although inconclusive results are the most common[1,7]. Another limitation is that the studies we analyzed included different standardized measures concerning distress, anxiety, and depression. It could be that these standardized tools are not sufficiently sensitive in this field and that those who receive positive, negative, and inconclusive results experience emotional distress differently. Moreover, the sample is unbalanced, as some studies exclusively include patients affected by a cancer diagnosis, a factor that contributes to experiencing higher levels of distress, anxiety, and depression. Finally, there was high variability between the time elapsed from the genetic test to the administration of the psychological questionnaires among the reviewed articles, and not all the reviewed studies administered the questionnaires at the same time to all patients. These limitations lead us not to generalize our results.
The results of this systematic review give a fuller picture of the psychological impact of receiving inconclusive results and can help genetic counsellors, health professionals, and researchers to provide more support to this subgroup of patients, by providing adequate information about the meaning of inconclusive genetic test result and its implications in terms of risk to develop cancer. The present review could also be able to improve the knowledge of experiences related to coping with uncertainty, suggesting which are the psychological aspects to consider when working with this type of patients. There is still much to understand in this difficult context, and it is necessary to take into greater consideration those who receive inconclusive results in the research and pre-test and post-test educational program to fully explain to people that inconclusive results do not exclude the possibility that they still might face a higher risk of developing ovarian or breast cancer. These considerations are required in health care contexts to provide adequate psychosocial support for people undergoing genetic testing.
The majority of BRCA1/2 genetic test consists of an inconclusive result, which produces a complex situation, as it means that a deleterious mutation is neither identified nor definitively excluded.
Studies specifically focusing on the psychological adjustment of people with inconclusive results are scarce and a systematic review on this topic is missing.
The principal purpose of this review was to examine short-, intermediate-, and long-term psychological outcomes of receiving an uninformative BRCA1/2 test result, with regard to distress (both general and genetic testing-specific), anxiety, and depressive levels. A further purpose was to highlight risk and protective factors affecting psychological adjustment in individuals with an inconclusive genetic testing result, also considering differences associated with being or not affected by a cancer diagnosis.
The guidelines of Preferred Reporting Items for Systematic Review and Meta-Analyses were followed in the current review. A comprehensive literature search in PubMed, PsychInfo, and Cochrane Central Register of Controlled Trials was carried out. Search results referred to the last 21 years (1999-2020).
Studies on psychological outcomes of inconclusive BRCA1/2 focused on general and specific distress, anxiety, and depression. Overall, they produced mixed results. These inconsistent findings are probably due to the uncertainty caused by this type of result, that may also influence the decisions of individuals about surveillance and prophylactic options, reducing their compliance. In addition, this review highlights specific risk and protective factors that affect psychological adjustment in individuals with an inconclusive genetic testing result.
This review highlights that individuals who receive an inconclusive result are a subgroup of patients who need educational programs and more pre-test information to better understand the meaning of their test in order to make adequate decisions about surveillance and prophylactic options.
Overall, the current review highlights the importance to address two main issues in this field: From a research perspective, it is recommended the development of tools more sensible to detect the psychological outcomes of inconclusive BRCA1/2 genetic test results; from a clinical perspective, health professionals and genetic counsellors should provide more psychoeducational support to this subgroup of patients about the meaning and the management of the uncertainty associated with their condition.
| 1. | Leblond D, Brédart A, Dolbeault S, De Pauw A, Stoppa Lyonnet D, Flahault C, Sultan S. [Cognitive, emotional and behavioral impact of an uncertain outcome after study of BRCA1/2: review of the literature]. Bull Cancer. 2011;98:184-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Stuppia L. BRCA1 and BRCA2 Molecular Testing in Women with Different Risk of Hereditary Breast Cancer: ost/Effectiveness and Psychological Implications. Curr Womens Health Rev. 2012;8:12-16. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Roukos DH, Briasoulis E. Individualized preventive and therapeutic management of hereditary breast ovarian cancer syndrome. Nat Clin Pract Oncol. 2007;4:578-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 90] [Article Influence: 4.7] [Reference Citation Analysis (1)] |
| 4. | Lerman C, Shields AE. Genetic testing for cancer susceptibility: the promise and the pitfalls. Nat Rev Cancer. 2004;4:235-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 51] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Ardern-Jones A, Kenen R, Lynch E, Doherty R, Eeles R. Is no news good news? Hered Cancer Clin Pract. 2010;8:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | O'Neill SC, Rini C, Goldsmith RE, Valdimarsdottir H, Cohen LH, Schwartz MD. Distress among women receiving uninformative BRCA1/2 results: 12-month outcomes. Psychooncology. 2009;18:1088-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 90] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 7. | Mannis GN, Fehniger JE, Creasman JS, Jacoby VL, Beattie MS. Risk-reducing salpingo-oophorectomy and ovarian cancer screening in 1077 women after BRCA testing. JAMA Intern Med. 2013;173:96-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Vadaparampil ST, Wey JP, Kinney AY. Psychosocial aspects of genetic counseling and testing. Semin Oncol Nurs. 2004;20:186-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Sommaggio P. La consulenza genetica: un ponte tra autopoiesi ed autotrascendimento. EUT Edizioni Università di Trieste. 2010;2:155-180. |
| 10. | Metcalfe KA, Mian N, Enmore M, Poll A, Llacuachaqui M, Nanda S, Sun P, Hughes KS, Narod SA. Long-term follow-up of Jewish women with a BRCA1 and BRCA2 mutation who underwent population genetic screening. Breast Cancer Res Treat. 2012;133:735-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 64] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 11. | Beran TM, Stanton AL, Kwan L, Seldon J, Bower JE, Vodermaier A, Ganz PA. The trajectory of psychological impact in BRCA1/2 genetic testing: does time heal? Ann Behav Med. 2008;36:107-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 60] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Lombardi L, Bramanti SM, Babore A, Stuppia L, Trumello C, Antonucci I, Cavallo A. Psychological aspects, risk and protective factors related to BRCA genetic testing: a review of the literature. Support Care Cancer. 2019;27:3647-3656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 13. | Heshka JT, Palleschi C, Howley H, Wilson B, Wells PS. A systematic review of perceived risks, psychological and behavioral impacts of genetic testing. Genet Med. 2008;10:19-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 247] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 14. | van Dijk S, van Asperen CJ, Jacobi CE, Vink GR, Tibben A, Breuning MH, Otten W. Variants of uncertain clinical significance as a result of BRCA1/2 testing: impact of an ambiguous breast cancer risk message. Genet Test. 2004;8:235-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | van Dijk S, Timmermans DR, Meijers-Heijboer H, Tibben A, van Asperen CJ, Otten W. Clinical characteristics affect the impact of an uninformative DNA test result: the course of worry and distress experienced by women who apply for genetic testing for breast cancer. J Clin Oncol. 2006;24:3672-3677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 71] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Dorval M, Gauthier G, Maunsell E, Dugas MJ, Rouleau I, Chiquette J, Plante M, Laframboise R, Gaudet M, Bridge PJ, Simard J. No evidence of false reassurance among women with an inconclusive BRCA1/2 genetic test result. Cancer Epidemiol Biomarkers Prev. 2005;14:2862-2867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13930] [Cited by in RCA: 13818] [Article Influence: 812.8] [Reference Citation Analysis (3)] |
| 18. | Hamilton JG, Lobel M, Moyer A. Emotional distress following genetic testing for hereditary breast and ovarian cancer: a meta-analytic review. Health Psychol. 2009;28:510-518. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 183] [Cited by in RCA: 181] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 19. | Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13:595-605. [PubMed] |
| 20. | O'Neill SC, DeMarco T, Peshkin BN, Rogers S, Rispoli J, Brown K, Valdimarsdottir H, Schwartz MD. Tolerance for uncertainty and perceived risk among women receiving uninformative BRCA1/2 test results. Am J Med Genet C Semin Med Genet. 2006;142C:251-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 58] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 21. | Power TE, Robinson JW, Bridge P, Bernier FP, Gilchrist DM. Distress and psychosocial needs of a heterogeneous high risk familial cancer population. J Genet Couns. 2011;20:249-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Manne S, Audrain J, Schwartz M, Main D, Finch C, Lerman C. Associations between relationship support and psychological reactions of participants and partners to BRCA1 and BRCA2 testing in a clinic-based sample. Ann Behav Med. 2004;28:211-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Ettema JHM, Arrindell WA. SCL-90. Handleiding bij een multidimensionele psychopathologie-indicator. Swets Zeitlinger. 1986;. |
| 24. | Claes E, Evers-Kiebooms G, Boogaerts A, Decruyenaere M, Denayer L, Legius E. Diagnostic genetic testing for hereditary breast and ovarian cancer in cancer patients: women's looking back on the pre-test period and a psychological evaluation. Genet Test. 2004;8:13-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 34] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Smith AW, Dougall AL, Posluszny DM, Somers TJ, Rubinstein WS, Baum A. Psychological distress and quality of life associated with genetic testing for breast cancer risk. Psychooncology. 2008;17:767-773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 67] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 26. | Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41:209-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5271] [Cited by in RCA: 4878] [Article Influence: 103.8] [Reference Citation Analysis (0)] |
| 27. | Lumish HS, Steinfeld H, Koval C, Russo D, Levinson E, Wynn J, Duong J, Chung WK. Impact of Panel Gene Testing for Hereditary Breast and Ovarian Cancer on Patients. J Genet Couns. 2017;26:1116-1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 99] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 28. | Goldberg D, Williams P. Manual of the General Health Questionnaire. England: NFER Publishing, 1978. |
| 29. | Bish A, Sutton S, Jacobs C, Levene S, Ramirez A, Hodgson S. No news is (not necessarily) good news: impact of preliminary results for BRCA1 mutation searches. Genet Med. 2002;4:353-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 30. | Parloff MB, Kelman HC, Frank JD. Comfort, effectiveness, and self-awareness as criteria of improvement in psychotherapy. Am J Psychiatry. 1954;111:343-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 240] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 31. | Schwartz MD, Peshkin BN, Hughes C, Main D, Isaacs C, Lerman C. Impact of BRCA1/BRCA2 mutation testing on psychologic distress in a clinic-based sample. J Clin Oncol. 2002;20:514-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 138] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 32. | Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28548] [Cited by in RCA: 32902] [Article Influence: 765.2] [Reference Citation Analysis (0)] |
| 33. | Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Appl Psychol Meas. 1977;1:385-401. [DOI] [Full Text] |
| 34. | Spielberger C, Gorsuch F, Lushene R. STAI manual for the state-trait anxiety inventory. Palo Alto, CA: Consulting Psychologists Press, 1971. |
| 35. | Cella D, Hughes C, Peterman A, Chang CH, Peshkin BN, Schwartz MD, Wenzel L, Lemke A, Marcus AC, Lerman C. A brief assessment of concerns associated with genetic testing for cancer: the Multidimensional Impact of Cancer Risk Assessment (MICRA) questionnaire. Health Psychol. 2002;21:564-572. [PubMed] |
| 36. | Graves KD, Vegella P, Poggi EA, Peshkin BN, Tong A, Isaacs C, Finch C, Kelly S, Taylor KL, Luta G, Schwartz MD. Long-term psychosocial outcomes of BRCA1/BRCA2 testing: differences across affected status and risk-reducing surgery choice. Cancer Epidemiol Biomarkers Prev. 2012;21:445-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 64] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 37. | Ringwald J, Wochnowski C, Bosse K, Giel KE, Schäffeler N, Zipfel S, Teufel M. Psychological Distress, Anxiety, and Depression of Cancer-Affected BRCA1/2 Mutation Carriers: a Systematic Review. J Genet Couns. 2016;25:880-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 81] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 38. | Hallowell N, Foster C, Ardern-Jones A, Eeles R, Murday V, Watson M. Genetic testing for women previously diagnosed with breast/ovarian cancer: examining the impact of BRCA1 and BRCA2 mutation searching. Genet Test. 2002;6:79-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 61] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 39. | Broadstock M, Michie S, Marteau T. Psychological consequences of predictive genetic testing: a systematic review. Eur J Hum Genet. 2000;8:731-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 241] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 40. | Hatcher JP, Jones DN, Rogers DC, Hatcher PD, Reavill C, Hagan JJ, Hunter AJ. Development of SHIRPA to characterise the phenotype of gene-targeted mice. Behav Brain Res. 2001;125:43-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 75] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 41. | Frost MH, Schaid DJ, Sellers TA, Slezak JM, Arnold PG, Woods JE, Petty PM, Johnson JL, Sitta DL, McDonnell SK, Rummans TA, Jenkins RB, Sloan JA, Hartmann LC. Long-term satisfaction and psychological and social function following bilateral prophylactic mastectomy. JAMA. 2000;284:319-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 217] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 42. | Payne SR, Newman B, King MC. Complex germline rearrangement of BRCA1 associated with breast and ovarian cancer. Genes Chromosomes Cancer. 2000;29:58-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 43. | Borreani C, Manoukian S, Bianchi E, Brunelli C, Peissel B, Caruso A, Morasso G, Pierotti MA. The psychological impact of breast and ovarian cancer preventive options in BRCA1 and BRCA2 mutation carriers. Clin Genet. 2014;85:7-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 44. | Cicero G, De Luca R, Dorangricchia P, Lo Coco G, Guarnaccia C, Fanale D, Calò V, Russo A. Risk Perception and Psychological Distress in Genetic Counselling for Hereditary Breast and/or Ovarian Cancer. J Genet Couns. 2017;26:999-1007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 45. | Schlich-Bakker KJ, ten Kroode HF, Ausems MG. A literature review of the psychological impact of genetic testing on breast cancer patients. Patient Educ Couns. 2006;62:13-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 67] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 46. | Brunstrom K, Murray A, McAllister M. Experiences of Women Who Underwent Predictive BRCA 1/2 Mutation Testing Before the Age of 30. J Genet Couns. 2016;25:90-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 47. | Low CA, Bower JE, Kwan L, Seldon J. Benefit finding in response to BRCA1/2 testing. Ann Behav Med. 2008;35:61-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 49. | Halbert CH, Schwartz MD, Wenzel L, Narod S, Peshkin BN, Cella D, Lerman C. Predictors of cognitive appraisals following genetic testing for BRCA1 and BRCA2 mutations. J Behav Med. 2004;27:373-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 50. | Peh CX, Liu J, Bishop GD, Chan HY, Chua SM, Kua EH, Mahendran R. Emotion regulation and emotional distress: The mediating role of hope on reappraisal and anxiety/depression in newly diagnosed cancer patients. Psychooncology. 2017;26:1191-1197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 63] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 51. | Lodder LN, Frets PG, Trijsburg RW, Meijers-Heijboer EJ, Klijn JG, Duivenvoorden HJ, Tibben A, Wagner A, van der Meer CA, Devilee P, Cornelisse CJ, Niermeijer MF. Presymptomatic testing for BRCA1 and BRCA2: how distressing are the pre-test weeks? J Med Genet. 1999;36:906-913. [PubMed] |
| 52. | Babore A, Bramanti SM, Lombardi L, Stuppia L, Trumello C, Antonucci I, Cavallo A. The role of depression and emotion regulation on parenting stress in a sample of mothers with cancer. Support Care Cancer. 2019;27:1271-1277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Psychiatry
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Stoyanov D S-Editor: Fan JR L-Editor: A P-Editor: Li JH