Published online Dec 19, 2021. doi: 10.5498/wjp.v11.i12.1346
Peer-review started: June 17, 2021
First decision: July 14, 2021
Revised: August 4, 2021
Accepted: October 20, 2021
Article in press: October 20, 2021
Published online: December 19, 2021
Processing time: 180 Days and 17.7 Hours
Pandemic mitigation policies, such as lockdown, are known to impact on mental health of individuals. Compulsory face covering under relaxed lockdown restrictions gives assurance of less transmission of airborne infection and has the potential to improve mental health of individuals affected by restrictions.
To examine the association of the lockdown relaxation and the implementation of the face covering policy on the mental health of the general population and sub-groups in the United Kingdom using interrupted time series model.
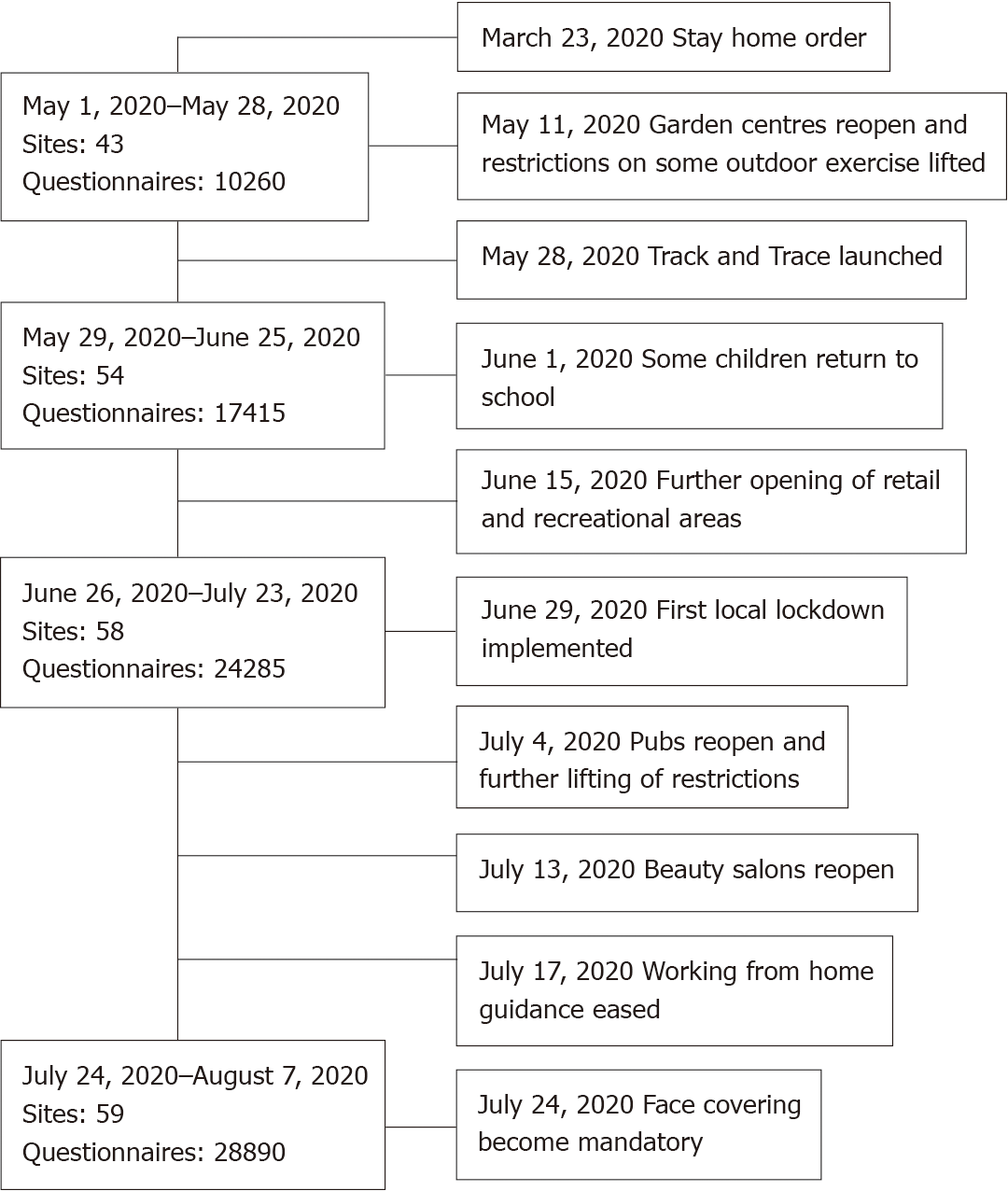
Using a web-based cross-sectional survey of 28890 United Kingdom adults carried out during May 1, 2020 to July 31, 2020, changes in mental health status using generalised anxiety disorder (GAD-7), and impact of events scale-revised (IES-R) scales are examined, at the dates of the first lockdown relaxation (July 4, 2020) and the subsequent introduction of face covering (July 24, 2020) in United Kingdom. A sharp regression discontinuity design is used to check discontinuities in mental health outcomes at policy-change dates.
Average GAD-7 scores of participants were 5.6, 5.6 and 4.3 during the lockdown period, the lockdown relaxation phase and the phase of compulsory face covering, respectively, with lower scores indicating lower anxiety levels. Corresponding scores for IES-R were 17.3, 16.8 and 13.4, with lower scores indicating less distress. Easing lockdown measures and subsequent introduction of face covering, on average, reduced GAD-7 by 0.513 (95%CI: 0.913-0.112) and 1.148 (95%CI: 1.800-0.496), respectively. Corresponding reductions in IES-R were 2.620 (95%CI: 4.279-0.961) and 3.449 (95%CI: 5.725-1.172). These imply that both lockdown relaxation and compulsory face-covering have a positive association with mental health scores (GAD-7 and IES-R).
The differential impact of lockdown and relaxation on the mental health of population sub-groups is evident in this study with future implications for policy. Introduction of face covering in public places had a stronger positive association with mental health than lockdown relaxation.
Core Tip: Positive association of lockdown relaxation and face-covering policies on the mental health (MH) of various population sub-groups is reported. Professional groups and health workers had lower generalised anxiety disorder (GAD-7) scores than other workers. During the compulsory face-covering phase, all professional groups improved on GAD-7 and impact of events scale-revised (IES-R) scores. Significant improvements in MH scores were found among non-key workers. Gender was associated with different MH outcomes during the lockdown, with females scoring higher on the GAD-7 and IES-R scales than males. However, both groups showed a significant improvement in MH status during the period of face-covering, with slightly higher improvements noted in males.
- Citation: Rathod S, Pallikadavath S, Graves E, Rahman MM, Brooks A, Soomro MG, Rathod P, Phiri P. Impact of lockdown relaxation and implementation of the face-covering policy on mental health: A United Kingdom COVID-19 study. World J Psychiatr 2021; 11(12): 1346-1365
- URL: https://www.wjgnet.com/2220-3206/full/v11/i12/1346.htm
- DOI: https://dx.doi.org/10.5498/wjp.v11.i12.1346
Restriction of people’s movements and interactions following wide-spread transmission of coronavirus disease 2019 (COVID-19) has been experienced by the global community. Several countries in the world have implemented lockdown measures to contain the spread of infection and/or delay the spread of infection in order to reduce mortality and morbidity.
The United Kingdom government implemented national lockdown in England on March 23, 2020. The restrictions imposed by the lockdown impacted on the health, economic and social welfare of individuals, households and society[1]. Lockdown reduced educational performance and nutrition of United Kingdom children caused by junk food intake[2]. Although it improved roadside air quality in the United Kingdom because of the reduction of vehicles[3], there was £370 billion loss to the United Kingdom economy[4] in addition to the loss of human lives and health[5].
The lockdown measures were first relaxed on July 4, 2020 and further changes, primarily the compulsory use of face covering in shops, were introduced on July 24, 2020. Table 1 summarises relaxation measures and face covering policy introduced following lockdown on March 23, 2020. Policy makers and mental health care providers need to know the reliable estimates of such effects to target policies and services to mitigate the mental health impact of restrictive measures due to COVID-19.
| Date | Policy changes |
| July 4, 2020 | 2-metre distance rule was dropped |
| Members of two different households have been able to drink or dine together | |
| Households will be able to host visitors, including overnight, and to meet with members of different households, on different occasions – including in a pub, restaurant or hotel, for example | |
| To reopen pubs, campsites, hairdressers, and churches. All these venues will be expected to collect and keep the contact details of visitors, so they can be traced in the event of a local outbreak of the virus | |
| Theatres and concert halls will also be able to reopen but they cannot host live performances because of concerns including the risk that singing can transmit the virus | |
| July 24, 2020 | Face mask has become compulsory in shops |
Globally, there is evidence of mental health decline among the general population during the COVID-19 pandemic. China, Spain, Italy, Iran, the United States, Turkey, Nepal, and Denmark, reported relatively higher rates of symptoms of anxiety (6.33% to 50.9%), depression (14.6% to 48.3%), post-traumatic stress disorder (7% to 53.8%), psychological distress (34.43% to 38%), and stress (8.1% to 81.9%) among the general population[6]. Stay-at-home orders, greater reduction of social contacts and perceived changes in everyday life were the primary pathways to increased mental health problems[7].
In the United Kingdom, there is evidence of minor psychiatric disorders during the first month of lockdown. For example, generalized health questionnaire (GHQ-12) reported an increase of 0.48 (95%CI: 0.07–0.90) from 2018-19 to April, 2020[1]. Daly et al[8] also found a similar increase in GHQ-12 in the United Kingdom. The highest increases of GHQ-12 are seen among 18–24 years old (2.69 points, 95%CI: 1.89–3.48), 25–34 years old (1.57, 95%CI: 0.96–2.18), women (0.92, 95%CI: 0.50–1.35), and people living with young children (1.45, 95%CI: 0.79–2.12). The mental health of United Kingdom adults was slightly better at the early stages of lockdown than at the end of lockdown[9]. Suicidal thoughts increased during lockdown, especially among young United Kingdom adults[10]. However, the mental health effects of COVID-19 on United Kingdom healthcare professionals are ambiguous[11], and some studies found a positive impact of the pandemic on the mental health of this specific group in the United Kingdom[12,13]. A key limitation of these studies is that they did not undertake causal analyses, which is key for policy and programming. Further, there is a need to evaluate the impact of face covering policy on the mental health of different population sub-groups.
Altschul et al[14] captured associations of face-covering with the mental health of United Kingdom adults using the logit model and concluded that wearing face coverings more often does not negatively impact mental health. Mental health impact of face covering may be due to the confidence people felt, particularly those vulnerable, with regard to the protection it might offer from infection. Face covering was promoted with medical narrative[15] and hence its use was primarily seen as a medical intervention. It is important to understand whether such intervention provides mental health improvements. This paper addresses the research gap by trying to capture any associations of COVID-19 restrictions and their easing with key policies on the mental health of United Kingdom adults with special focus on population sub-groups. The authors used sharp regression discontinuity design (RDD) to analyse discontinuities in mental health outcomes at key policy-change dates. We also tested the key identification condition, the local randomization. If the factors affecting mental health outcomes were not found discontinuous at those cut-off dates, discontinuities in mental health outcomes were likely to be causal given other identification conditions (e.g., unconfoundedness) hold[16]. There is no formal way of testing them, but this can be checked informally through falsification tests (e.g., checking discontinuities in mental health outcomes at any false dates, checking false outcomes at lockdown policy changing dates). In this study, we consider the informal test through visual inspection of figures.
A cross-sectional online international survey of adults, 16 years and above, was carried out during May 1, 2020 to July 31, 2020 yielding a sample size of 28890 in England. Further details of the methodology are documented in an earlier publication by the group[13]. Of the total sample, 20174 completed the online questionnaire during lockdown; 4550 during the first phase of relaxation and 4145 during the face covering policy period.
Southern Health National Health Service (NHS) Foundation Trust co-ordinated the online survey with support from 50 NHS Trusts, Universities, and The Centre for Applied Research and Evaluation International Foundation. These organisations advertised the survey to their staff, patients and the general public with a weblink to the survey platform. Overall, more than 100 organizations were involved in sending the survey links to potential participants via professional routes and social media (Figure 1).
To study the impact of easing lockdown and introduction of face covering on mental health, both control and experimental groups are required. However, as the first United Kingdom lockdown was implemented at national level, there was no control group (i.e. areas without lockdown) available naturally within the nation to identify the impact of easing lockdown measures on mental health. In the absence of such control population, the RDD model is the most suitable method to address the objectives. As the United Kingdom lockdown and face covering policy had clear implementation protocols, including exact date and time, it was easier to identify cut-off points for policy change required for the chosen method. As far as we know there was no other policy announcement that might affect the mental health of the population to contaminate the effect. The two cut-off points (date of first lockdown easing and introduction of face covering) were July 4, 2020 and July 24, 2020, respectively. The RDD methodology allows for the creation of control and experimental groups by identifying populations with the same characteristics just before and after each cut-off date (i.e. July 4, 2020 and July 24, 2020). The population before the cut-off date serves as the control group and the after the cut-off date will be the experimental group. This creates two sets of control and experimental groups, one set at each cut-off date generating a quasi-experimental design.
The study received ethics and HRA approval. IRAS project ID: 282858; REC reference: 20/HRA/1934 from London-Westminster Research Ethics Committee on 27 April 2020.
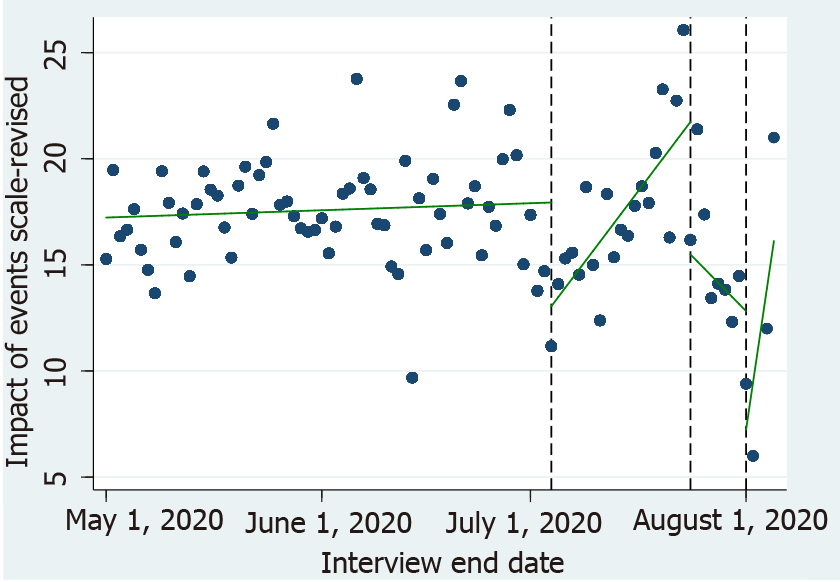
To test whether the data qualifies for RDD, predicted values of generalised anxiety disorder (GAD-7) and impact of events scale-revised (IES-R) are plotted against the interview end date (Figures 2 and 3). Vertical lines indicate cut-off dates. As data are highly scattered, figures without vertical lines (at the cut-off dates) and fitted lines will cause difficulty in understanding discontinuities at the cut-off dates. Predicted values are generated from regressions of these indices on the trend variable allowing discontinuities and changes in slopes. These predicted values pass through scatter points, which are daily averages of these indices. The interview end date is the date of completing the survey questionnaire by an individual. Interview end dates are used to make the trend variable (e.g., 1 for first date, 2 for second date, etc.), and this gives the appropriate assignment variable. The two mental health measures show clear negative discontinuities at the first and second cut-off dates, implying that easing lockdown restrictions and introduction of face covering improved mental health.
Visual inspection of the two figures indicates slope changes after the first cut-off date. In survey data, such slope changes can be difficult to interpret. The analysis captures intercept discontinuities (steps) after also controlling for slope changes, as suggested by Angrist and Pischke[17] in RDD.
The unit of analysis is an adult aged 16 years or over. The outcome of interest, mental health outcome measured using GAD-7 and IES-R, is denoted by Y, which varies across different groups of individuals (e.g., health vs non-health workers, male vs female, etc.) by date. For purposes of regression, date is used as the trend variable, which contains 1 for the first date, 2 for the second date, and so on. Individual and time are indicated by i and t, respectively. As mental health conditions change around the cut-off time, the following RDD type of interrupted time series model was used:
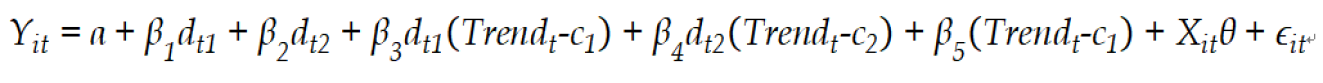
where α is the constant term, dt1 = 1{Interview end date ≥ 4th of July}, and dt2 = 1{Interview end date ≥ 24th of July} are discontinuity dummies, c1 = Value of trend for the date of 4th of July and c1 = Value of trend for the date of 24th of July the two cut-off points, Xit is the row vector of control variables (listed in Tables 2 and 3) and θ is the column vector of their coefficients, and ∈it is the error term. β1 and β2 are parameters of discontinuities at two respective cut-off dates, and β3 and β4, are parameters of kinks (slope changes) at two respective cut-off dates. Parameters of interest in this paper are discontinuity parameters, β1 and β2, which give changes in mental health scores at the two cut-off dates.
| Time by lockdown easing policy | May 1, 2020-July 3, 2020 (Lockdown phase) | July 4-23, 2020 (Lockdown relaxation phase) | July 24-31, 2020 (Face-covering phase) | Total | |||||
| Outcome and control variables | No. | % | No. | % | No. | % | No. | % | P value |
| Total sample | 20173 | 100 | 4550 | 100 | 4145 | 100 | 28890 | 100 | |
| Mental health outcomes/scores | |||||||||
| GAD-7 | |||||||||
| Total | 15634 | 100 | 3379 | 100 | 3153 | 100 | 22166 | 100 | |
| Missing | 4539 | 1171 | 992 | 6711 | |||||
| IES-R | |||||||||
| Total | 14516 | 100 | 3141 | 100 | 2961 | 100 | 20618 | 100 | |
| Missing | 5657 | 1409 | 1184 | 8260 | |||||
| Demographics, lifestyle changes, and pre-existing health conditions | |||||||||
| Key worker | |||||||||
| No | 5400 | 29.7 | 1260 | 31.4 | 1778 | 48.8 | 8438 | 32.6 | |
| Yes (health) | 9205 | 50.6 | 1961 | 48.9 | 1161 | 31.8 | 12327 | 47.7 | |
| Yes (non-health) | 3595 | 19.8 | 793 | 19.8 | 708 | 19.4 | 5096 | 19.7 | |
| Total | 18200 | 100 | 4014 | 100 | 3647 | 100 | 25861 | 100 | < 0.001 |
| Missing | 1973 | 536 | 498 | 3014 | |||||
| Gender | |||||||||
| Female | 15324 | 84.2 | 3331 | 83.4 | 2701 | 75.2 | 21356 | 82.8 | |
| Male | 2872 | 15.8 | 662 | 16.6 | 891 | 24.8 | 4425 | 17.2 | |
| Total | 18196 | 100 | 3993 | 100 | 3592 | 100 | 25781 | 100 | < 0.001 |
| Missing | 1977 | 557 | 553 | 3094 | |||||
| Age category or group | |||||||||
| Under 21 | 332 | 1.8 | 90 | 2.2 | 81 | 2.2 | 503 | 1.9 | |
| 21-24 | 828 | 4.5 | 163 | 4 | 100 | 2.7 | 1091 | 4.2 | |
| 25-34 | 3627 | 19.8 | 709 | 17.5 | 566 | 15.4 | 4902 | 18.8 | |
| 35-44 | 4076 | 22.2 | 794 | 19.5 | 712 | 19.4 | 5582 | 21.4 | |
| 45-54 | 4676 | 25.5 | 1008 | 24.8 | 851 | 23.2 | 6535 | 25.1 | |
| 55-64 | 3462 | 18.9 | 882 | 21.7 | 795 | 21.6 | 5139 | 19.7 | |
| 65 and over | 1319 | 7.2 | 416 | 10.2 | 568 | 15.5 | 2303 | 8.8 | |
| Total | 18320 | 100 | 4062 | 100 | 3673 | 100 | 26055 | 100 | < 0.001 |
| Missing | 1853 | 488 | 472 | 2820 | |||||
| Ethnicity | |||||||||
| Non-white British | 1649 | 9 | 362 | 8.9 | 351 | 9.5 | 2362 | 9.1 | |
| White British | 16703 | 91 | 3698 | 91.1 | 3325 | 90.5 | 23726 | 90.9 | |
| Total | 18352 | 100 | 4060 | 100 | 3676 | 100 | 26088 | 100 | < 0.001 |
| Missing | 1821 | 490 | 469 | 2787 | |||||
| Religion | |||||||||
| Non-Christian | 9794 | 54.1 | 2140 | 54.3 | 1905 | 53.8 | 13839 | 54.1 | |
| Christian | 8306 | 45.9 | 1798 | 45.7 | 1633 | 46.2 | 11737 | 45.9 | |
| Total | 18100 | 100 | 3938 | 100 | 3538 | 100 | 25576 | 100 | 0.911 |
| Missing | 2073 | 612 | 607 | 3300 | |||||
| Age left education | |||||||||
| ≤ 18 (A-level or less) | 5967 | 33 | 1557 | 38.9 | 1249 | 34.4 | 8773 | 34.1 | |
| > 18 (Higher degree) | 12118 | 67 | 2442 | 61.1 | 2381 | 65.6 | 16941 | 65.9 | |
| Total | 18085 | 100 | 3999 | 100 | 3630 | 100 | 25714 | 100 | |
| Missing | 2088 | 551 | 515 | 3161 | |||||
| Accommodation | |||||||||
| Rented home | 5030 | 27.5 | 1163 | 28.7 | 847 | 23 | 7040 | 27 | |
| Own home | 13288 | 72.5 | 2891 | 71.3 | 2834 | 77 | 19013 | 73 | |
| Total | 18318 | 100 | 4054 | 100 | 3681 | 100 | 26053 | 100 | < 0.001 |
| Missing | 1855 | 496 | 464 | 2822 | |||||
| Vulnerable according to government category | |||||||||
| No | 13735 | 80.6 | 2938 | 78.5 | 2610 | 77.7 | 19283 | 79.8 | |
| Yes (do not require shielding) | 2005 | 11.8 | 503 | 13.4 | 494 | 14.7 | 3002 | 12.4 | |
| Yes (require shielding) | 1307 | 7.7 | 303 | 8.1 | 257 | 7.6 | 1867 | 7.7 | |
| Total | 17047 | 100 | 3744 | 100 | 3361 | 100 | 24152 | 100 | < 0.001 |
| Missing | 3126 | 806 | 784 | 4725 | |||||
| Experienced coronavirus | |||||||||
| No | 4354 | 24.9 | 1016 | 26.3 | 971 | 27.8 | 6341 | 25.5 | |
| Yes | 13152 | 75.1 | 2843 | 73.7 | 2518 | 72.2 | 18513 | 74.5 | |
| Total | 17506 | 100 | 3859 | 100 | 3489 | 100 | 24854 | 100 | 0.001 |
| Missing | 2667 | 691 | 656 | 4022 | |||||
| Pre-existing mental health condition | |||||||||
| No | 10685 | 62.6 | 2288 | 60.8 | 2404 | 70.1 | 15377 | 63.3 | |
| Yes | 6395 | 37.4 | 1476 | 39.2 | 1026 | 29.9 | 8897 | 36.7 | |
| Total | 17080 | 100 | 3764 | 100 | 3430 | 100 | 24274 | 100 | < 0.001 |
| Missing | 3093 | 786 | 715 | 4604 | |||||
| Drinking alcohol | |||||||||
| Never | 2611 | 14.6 | 540 | 13.7 | 492 | 13.8 | 3643 | 14.4 | |
| Monthly or less | 3954 | 22.2 | 944 | 24 | 692 | 19.4 | 5590 | 22.1 | |
| 2-4 times a month | 3909 | 21.9 | 930 | 23.6 | 824 | 23 | 5663 | 22.3 | |
| 2-3 times a week | 4873 | 27.3 | 1007 | 25.6 | 999 | 27.9 | 6879 | 27.1 | |
| 4 times or more a week | 2479 | 13.9 | 520 | 13.2 | 569 | 15.9 | 3568 | 14.1 | |
| Total | 17826 | 100 | 3941 | 100 | 3576 | 100 | 25343 | 100 | < 0.001 |
| Missing | 2347 | 609 | 569 | 3532 | |||||
| Taking drug | |||||||||
| No | 17354 | 97.9 | 3810 | 97.3 | 3465 | 97.3 | 24629 | 97.7 | |
| Yes | 369 | 2.1 | 107 | 2.7 | 95 | 2.7 | 571 | 2.3 | |
| Total | 17723 | 100 | 3917 | 100 | 3560 | 100 | 25200 | 100 | < 0.001 |
| Missing | 2450 | 633 | 585 | 3675 | |||||
| Suicidal thoughts | |||||||||
| No | 12015 | 68.3 | 2591 | 66.7 | 2521 | 71.5 | 17127 | 68.5 | |
| Yes | 5572 | 31.7 | 1292 | 33.3 | 1005 | 28.5 | 7869 | 31.5 | |
| Total | 17587 | 100 | 3883 | 100 | 3526 | 100 | 24996 | 100 | < 0.001 |
| Missing | 2586 | 667 | 619 | 3879 | |||||
| Control variables | Means of GAD-7 (n = 18948) (95%CI) | Means of IES-R (n = 17739) (95%CI) | ||||
| May 1, 2020-July 3, 2020 (Lockdown) | July 4-23, 2020 (Lockdown relax) | July 24-31, 2020 (Face-covering) | May 1, 2020-July 3, 2020 (Lockdown) | July 4-23, 2020 (Lockdown relax) | July 24-31, 2020 (Face-covering) | |
| Total study population | 5.6 (5.5-5.7) | 5.6 (5.3-5.8) | 4.4 (4.2-4.6) | 17.3 (16.9-17.6) | 16.8 (16.0-17.6) | 13.4 (12.7-14.2) |
| Key worker | ||||||
| Not a key worker | 5.8 (5.6-6.0) | 6.2 (5.7-6.7) | 4.1 (3.8-4.4) | 18.5 (17.8-19.2) | 19.9 (18.2-21.5) | 13.1 (12.1-14.2) |
| Health | 5.1 (5.0-5.3) | 5 (4.7-5.3) | 4.3 (3.9-4.6) | 15.9 (15.4-16.3) | 14.4 (13.4-15.4) | 12.2 (11.0-13.5) |
| Not in health | 6.3 (6.1-6.6) | 6.1 (5.5-6.6) | 5.3 (4.8-5.9) | 19 (18.2-19.8) | 18.5 (16.8-20.3) | 16.1 (14.4-17.9) |
| Gender | ||||||
| Female | 5.8 (5.7-5.9) | 5.7 (5.5-6.0) | 4.8 (4.5-5.1) | 18 (17.6-18.4) | 17.3 (16.4-18.2) | 14.4 (13.5-15.2) |
| Male | 4.3 (4.0-4.5) | 4.8 (4.1-5.4) | 3.2 (2.8-3.7) | 13.3 (12.4-14.1) | 14.1 (12.2-16.1) | 10.7 (9.4-12.1) |
| Age group | ||||||
| Under 21 | 7.7 (6.8-8.5) | 9.3 (6.7-11.9) | 8.6 (6.4-10.9) | 24 (20.9-27.1) | 30.8 (20.8-40.8) | 28.8 (20.2-37.3) |
| 21-24 | 7.9 (7.4-8.5) | 7.8 (6.3-9.2) | 6.7 (5.0-8.4) | 22.6 (20.8-24.3) | 21.4 (17.0-25.7) | 19.2 (13.9-24.5) |
| 25-34 | 6.8 (6.5-7.0) | 7.5 (7.0-8.1) | 5.7 (5.1-6.4) | 19 (18.2-19.8) | 21.3 (19.4-23.2) | 15.4 (13.3-17.4) |
| 35-44 | 6.1 (5.9-6.3) | 6.1 (5.6-6.6) | 5.2 (4.7-5.7) | 18.3 (17.5-19.0) | 17.8 (16.1-19.5) | 14.4 (12.8-15.9) |
| 45-54 | 4.9 (4.7-5.1) | 4.8 (4.4-5.3) | 4.5 (4.0-5.0) | 16.2 (15.6-16.9) | 14.5 (13.0-16.0) | 13.2 (11.8-14.7) |
| 55-64 | 4.6 (4.4-4.8) | 4.8 (4.3-5.3) | 3.7 (3.3-4.1) | 15.7 (15.0-16.5) | 14.8 (13.2-16.4) | 12.6 (11.2-14.0) |
| 65 and over | 3.1 (2.8-3.4) | 3.1 (2.5-3.7) | 1.9 (1.4-2.3) | 10.8 (9.7-11.8) | 12.2 (9.7-14.6) | 8.1 (6.5-9.7) |
| Ethnicity | ||||||
| Non-white | 4.9 (4.5-5.2) | 5.9 (5.1-6.8) | 4.9 (4.1-5.7) | 15.9 (14.7-17.1) | 19.2 (16.3-22.0) | 14.4 (12.0-16.8) |
| White | 5.6 (5.5-5.7) | 5.5 (5.3-5.8) | 4.4 (4.1-4.6) | 17.4 (17.0-17.7) | 16.6 (15.7-17.4) | 13.3 (12.5-14.1) |
| Religion | ||||||
| Non-Christian | 5.7 (5.6-5.9) | 6.0 (5.6-6.3) | 4.6 (4.3-4.9) | 17.6 (17.2-18.1) | 17.6 (16.5-18.7) | 13.8 (12.8-14.8) |
| Christian | 5.4 (5.2-5.5) | 5.1 (4.8-5.5) | 4.2 (3.9-4.5) | 16.8 (16.3-17.3) | 15.8 (14.6-17.0) | 12.9 (11.9-14.0) |
| Education | ||||||
| A-level or less | 6.2 (6.0-6.4) | 6.1 (5.7-6.6) | 4.5 (4.1-4.9) | 19.1 (18.4-19.8) | 19.1 (17.6-20.5) | 14.3 (12.9-15.7) |
| Higher degree | 5.3 (5.2-5.4) | 5.2 (4.9-5.5) | 4.4 (4.1-4.6) | 16.4 (16.0-16.8) | 15.5 (14.6-16.4) | 13 (12.2-13.9) |
| Type of accommodation | ||||||
| Rented | 7.1 (6.9-7.3) | 7.8 (7.3-8.3) | 6.7 (6.1-7.3) | 21.6 (20.9-22.3) | 23.1 (21.4-24.8) | 19.7 (17.8-21.6) |
| Own | 5 (4.9-5.1) 4 | 4.7 (4.5-5.0) | 3.8 (3.5-4.0) | 15.7 (15.3-16.0) | 14.4 (13.5-15.3) | 11.7 (10.9-12.4) |
| Shielding status (government) | ||||||
| Shielding not required | 5.5 (5.4-5.6) | 5.5 (5.2-5.8) | 4.4 (4.1-4.6) | 16.8 (16.5-17.2) | 16.2 (15.3-17.1) | 12.9 (12.1-13.7) |
| Shielding required (but not Shielding) | 5.5 (5.2-5.9) | 5.1 (4.5-5.8) | 4 (3.4-4.6) | 17.6 (16.5-18.6) | 16.6 (14.5-18.8) | 13 (11.0-14.9) |
| Shielding required (shielding) | 6.6 (6.2-7.0) | 7.4 (6.4-8.5) | 5.5 (4.6-6.5) | 21.2 (19.8-22.6) | 23.9 (20.7-27.2) | 19.3 (16.2-22.3) |
| Experience of COVID-19 | ||||||
| No such experience | 5.1 (4.9-5.3) | 5.1 (4.6-5.6) | 3.9 (3.5-4.4) | 15.5 (14.8-16.2) | 16.3 (14.7-18.0) | 12.1 (10.7-13.5) |
| Yes | 5.7 (5.6-5.8) | 5.7 (5.4-6.0) | 4.6 (4.3-4.9) | 17.8 (17.4-18.2) | 17 (16.1-17.9) 1 | 3.9 (13.1-14.8) |
| Pre-existing mental health | ||||||
| No | 4.1 (4.0-4.2) | 3.7 (3.5-3.9) | 3.2 (2.9-3.4) | 13 (12.6-13.3) | 11.5 (10.7-12.3) | 9.7 (9.0-10.4) |
| Yes | 8.2 (8.0-8.4) | 8.7 (8.3-9.2) | 7.6 (7.1-8.1) | 24.9 (24.3-25.6) | 25.9 (24.5-27.4) | 23 (21.3-24.7) |
| Drinking alcohol | ||||||
| Never | 6.3 (6.0-6.6) | 6.2 (5.5-6.9) | 5.7 (4.9-6.4) | 19.7 (18.6-20.7) | 17.9 (15.6-20.2) | 16.2 (13.8-18.6) |
| Monthly or less | 6.2 (6.0-6.5) | 6.6 (6.0-7.1) | 5 (4.4-5.5) | 18.8 (18.0-19.6) | 19.5 (17.6-21.3) | 15.2 (13.4-17.0) |
| 2-4 times a month | 5.4 (5.2-5.6) | 5.3 (4.8-5.8) | 4.3 (3.8-4.7) | 16.7 (15.9-17.4) | 17 (15.4-18.5) | 13 (11.5-14.5) |
| 2-3 times a week | 5 (4.9-5.2) 5 | 5.2 (4.7-5.6) | 3.9 (3.5-4.4) | 15.5 (14.9-16.1) | 15.2 (13.7-16.7) | 12.2 (10.9-13.5) |
| 4 times or more a week | 5.1 (4.8-5.3) | 4.3 (3.7-5.0) | 3.8 (3.2-4.4) | 16.9 (16.0-17.9) | 13.4 (11.6-15.3) | 12 (10.3-13.7) |
| Drug use | ||||||
| Never | 5.5 (5.4-5.6) | 5.5 (5.2-5.7) | 4.3 (4.1-4.6) | 17.1 (16.8-17.5) | 16.6 (15.8-17.4) | 13.1 (12.4-13.9) |
| Ever | 7.7 (6.8-8.6) | 9.6 (7.9-11.4) | 7.3 (5.5-9.1) | 23.8 (20.9-26.8) | 25.5 (19.9-31.1) | 24.2 (18.3-30.0) |
| Suicidal thoughts ever | ||||||
| No | 4.5 (4.4-4.6) | 4.4 (4.1-4.7) | 3.4 (3.2-3.7) | 13.9 (13.5-14.3) | 13.2 (12.3-14.0) | 10.3 (9.6-11.0) |
| Yes | 7.8 (7.6-8.0) | 8 (7.6-8.5) | 6.9 (6.4-7.4) | 24.3 (23.7-25.0) | 24.4 (22.8-25.9) | 21.6 (19.9-23.3) |
The control variables included in the analysis are socio-demographic characteristics (e.g., profession, age, ethnicity, religion, gender, education, accommodation, etc.), lifestyle characteristics (e.g., experiencing coronavirus, drug use, drinking alcohol, etc.), and pre-existing health conditions (e.g., vulnerability, suicidal thoughts, mental health conditions). The outcome variable of interest is mental health status. Two widely used standardized measures have been used to measure levels of anxiety (GAD-7)[18], and subjective distress (IES–R)[19]. The GAD-7 ranges from 0 to 21, and it categorizes as minimal (0-4), mild (5-9), moderate (10-14), and severe (15-21). The IES-R ranges from 0 to 88, and it categorizes as minimal (0-23), post-traumatic stress disorder (PTSD) may be a concern (24-32), probable PTSD diagnosis (33-38), and high PTSD (39-88). A total of 22,166 respondents completed the GAD-7 questionnaire. Of those 15634 were completed during lockdown, 3379 during the first phase of lockdown relaxation, and 3153 during the face covering phase. A total of 20618 respondents completed the IES-R questionnaire, 14516 respondents completed this during lockdown, 3141 during the first phase and 2961 during the second phase of lockdown relaxation.
Table 2 presents percentage distribution of control variables used in the regressions according to lockdown, lockdown relaxation, and face covering implementation period. It suggests that the proportions of control variables in the three time periods follow a similar pattern. However, there are higher proportions of health workers (31.8%-50.6%) and females (75.2%-84.2%) in the sample. The table shows that (P < 0.001) percentages of control variables vary significantly during each of the time periods. Such discrepancies in demographic characteristics of respondents will not violate identification conditions as discrepancies of those covariates do not exist around the cut-off dates in most cases (e.g., the existence of local randomization available in supplementary material). The table also shows missing values, which are unlikely to make any serious impact on the results of regressions as the individuals are distributed based on comparable characteristics before and after the cut-off dates.
Table 3 provides average scores of the two mental health measures for three time periods: During lockdown; during relaxation and the face covering period. Comparisons of the average scores between these time periods gives us raw estimates of the effects of the lockdown relaxation and the compulsory face covering policies. The average scores of GAD-7 and IES-R at the three time periods suggest that the mental health of the respondents was worse during lockdown but has improved after the lockdown easing and during the period of face covering. For example, the overall mean GAD-7 scores were 5.6 each for the lockdown period and the first phase of lockdown relaxation, compared to 4.4 during the period of face covering. For the IES-R, the average scores were 17.3, 16.8 and 13.4 for the periods of lockdown, lockdown relaxation, and face covering, respectively, suggesting a reduction in anxiety and distress during the first relaxation, but significant reductions were noticed during the period of face-covering.
There were notable differences in the associations of lockdown relaxation and compulsory face covering policies on mental health of various population sub-groups. Among the professional groups, health workers had the lowest GAD-7 score (5.1) compared to other key workers (6.3) and non-key workers (5.8) during the lockdown period. Similar findings were observed for the IES-R, 18.5 for non-key workers, 15.9 for health workers and 19.0 for other key workers. During the compulsory face covering phase, there were improvements (mean reductions) in both mean scores for all three professional groups; the GAD-7 and IES-R scores were 4.1 and 13.1 for non-key workers, 4.3 and 12.2 for health workers, and 5.3 and 16.1 for non-health workers during the period of face covering, respectively. These imply that greater improvements in mental health are found among non-key workers than key workers, meaning that non-key workers were affected more by COVID-19. However, the regression results give a better indication.
In this study, gender was associated with mental health outcomes. During the lockdown, females had higher GAD-7 mean scores (5.8) compared to males (4.3). A similar pattern was observed for the IES-R (18.00 for females and 13.3 males). Both groups have shown significant improvements in anxiety and distress during the period of face covering, but slightly higher improvements are seen among males compared to females.
Table 3 further shows that both GAD-7 and IES-R were higher among younger age groups. For example, during lockdown, GAD-7 score was 7.7 for the under 21 years age group compared to 3.1 for the 65+ age group. The IES-R was 24.00 for the below 21 years age group compared to 10.8 for the 65+ age group. Both the scores of all age groups have declined during the face covering period. Compared to the middle age groups (e.g., 35-44, 45-54), higher reductions (at least in terms of percentage) are seen among the lower and higher age groups.
Ethnic variations in mental health were also noted in this study. White ethnic population had higher GAD-7 (5.6) and IES-R (17.4) scores during the lockdown period compared to non-white (GAD-7, 4.9; IES-R, 15.9) ethnic group. Both ethnic groups showed notable improvements in average GAD-7 and IES-R scores at the face covering period, but not during the lockdown relaxation period. The white group shows greater improvements in mental health than the non-white group. Among non-Christians, both GAD-7 (5.7) and IES-R (17.6) scores were higher compared to Christians (GAD-7, 5.4; IES-R, 16.8). Similar to ethnicity, notable improvements in the average anxiety and distress scores of the two measures were noted in the face covering period, but not for the lockdown relaxation period. Slightly greater improvements in mental health are seen among Christians (who are mainly white ethnic population) than non-Christians.
Educational differences in mental health status by lockdown status and face covering were found in this study. During lockdown, average mental health scores for the two measures were higher for those with A-level or less (GAD-7, 6.2; IES-R, 19.1) compared to those with degree qualification (GAD-7, 5.3; IES-R, 16.4). Although there were some improvements in the mental health scores during the first lockdown relaxation, larger improvements were noted in the face covering period. In the face covering period, larger falls in both scores are seen among lower educated groups, implying that this group of educated people that includes lower-skilled workers was possibly hit more by COVID-19. Those who lived in rental accommodation during lockdown experienced more distress, with higher scores for both GAD-7 (7.1) and IES-R (21.6) compared to those living in their own homes (GAD-7, 5.0; IES-R, 15.7). Notable improvements in both GAD-7 and IES-R scores were found in the face covering period, and greater improvements are seen for those who live in their own houses.
During the lockdown period, those who shielded as per government advice had higher mental health scores for the two measures (GAD-7 = 6.6; IES-R = 21.2) compared to those who did not shield although they were advised to shield (GAD-7 = 5.5; IES-R = 17.6). Again, improvements in mental health of both groups are seen during the face covering period, but greater improvements are seen among those who shielded. Those who have experienced some COVID-19 related unpleasant experiences, had higher anxiety and distress scores (GAD-7 = 5.7; IES-R = 17.8 during the lockdown phase) compared to those who did not experience such situations (GAD-7 = 5.1; IES-R = 15.5 during the lockdown phase). Their mental health status improved significantly when the face covering policy was introduced. Greater improvement is seen among individuals who experienced coronavirus in IES–R scores. Similarly, those who had pre-existing mental health problems had higher mental health scores in both GAD-7 and IES-R in all three phases. Again, they experienced lower mental health problems after the face covering policy was introduced, but individuals without pre-existing mental health conditions experienced greater mental health improvements during the face covering phase.
In all three phases, those who never drank alcohol had higher anxiety and distress scores compared to those who reported alcohol consumption four or more times a week. Implementation of the face covering policy improved mental health scores of all groups of alcohol users. Users of drugs had higher anxiety and distress scores compared to ‘never’ users, but never users of drugs showed higher improvements in mental health scores during the face covering phase. Those who ever experienced suicidal thoughts had higher anxiety and distress scores compared to those who never had such thoughts. As with all other factors, improvements were noted when the face covering policy was introduced, but again, greater improvements are seen among the non-vulnerable group, those who never experienced suicidal thoughts.
Table 4 shows the changes in mental health outcomes measured using GAD-7 and IES-R by two policy changes dates (July 4 and 24, 2020), and demographics, pre-existing health conditions, and lifestyles. For every group of demographics, pre-existing health conditions, and lifestyles, changes in anxiety and distress scores at two dates were estimated by running a simple OLS regression, which followed the specification of the interrupted time series model equation. The coefficients of two discontinuity dummies for two policy changes dates, which are estimates of changes in anxiety and distress scores at two dates, are shown in the Table 4. In each regression, linear function of trend variable (time) was considered, as Figures 2 and 3 did not suggest any non-linearity. To note that, in the regression of a group, all other covariates except one corresponding to that group were used. For example, in the regression of the male group, the only male dummy was dropped, but all other covariates defined by all other groups are used.
| Policy change dates in 2020 | Population sub-groups | GAD-7, changes (95%CI) | P value | IESR, changes (95%CI) | P value |
| July 4, 2020 (Lockdown relaxation date) | Total sample | -0.513 (-0.913, -0.112) | 0.081 | -2.620 (-4.279, -0. 961) | 0.464 |
| July 24, 2020 (Face-covering start date) | Total sample | -1.148 (-1.800, -0.496) | -3.449 (-5.725, -1.172) | ||
| Key worker | |||||
| July 4, 2020 (Lockdown relaxation date) | Not a key worker | -0.910 (-1.810, -0.011) | 0.062 | -3.546 (-6.235, -0.857) | 0.708 |
| Health | 0.017 (-0.602, 0.637) | -1.643 (-3.914, 0.628) | |||
| Non-health | -0.756 (-1.877, 0.365) | -1.704 (-5.115, 1.708) | |||
| July 24, 2020 (Face-covering start date) | Not a key worker | -1.191 (-2.259, -0.123) | 0.064 | -3.877 (-7.410, -0.343) | 0.843 |
| Health | -0.986 (-1.584, -0.387) | -1.693 (-4.376, 0.991) | |||
| Non-health | -1.421 (-3.454, 0.613) | -5.458 (-9.144, -1.772) | |||
| Gender | |||||
| July 4, 2020 (Lockdown relaxation date) | Female | -0.496 (-0.983, -0.010) | 0.817 | -2.606 (-4.445, -0.767) | 0.936 |
| Male | -0.622 (-1.652, 0.409) | -2.461 (-5.929, 1.007) | |||
| July 24, 2020 (Face-covering start date) | Female | -1.013 (-1.778, -0.248) | 0.382 | -3.369 (-5.789, -0.948) | 0.926 |
| Male | -1.739 (-2.993, -0.485) | -3.112 (-6.985, 0.762) | |||
| Age group | |||||
| July 4, 2020 (Lockdown relaxation date) | Under 21 | -5.482 (-9.526, -1.437) | 0.029 | -19.319 (-41.541, 2.902) | 0.260 |
| 21-24 | -0.103 (-1.975, 1.770) | -3.715 (-8.350, 0.920) | |||
| 25-34 | -0.314 (-1.346, 0.717) | -2.653 (-4.900, -0.406) | |||
| 35-44 | -0.640 (-1.646, 0.366) | 0.545 (-2.309, 3.399) | |||
| 45-54 | 0.179 (-0.663, 1.021) | -1.871 (-4.785, 1.043) | |||
| 55-64 | -0.911 (-2.117, 0.294) | -5.390 (-9.419, -1.361) | |||
| 65 and over | -0.923 (-2.330, 0.484) | -2.633 (-8.466, 3.199) | |||
| July 24, 2020 (Face-covering start date) | Under 21 | -0.983 (-5.502, 3.536) | -3.941 (-23.634, 15.753) | ||
| 21-24 | -0.830 (-6.322, 4.661) | -2.354 (-14.469, 9.761) | |||
| 25-34 | -1.928 (-3.272, -0.584) | -7.306 (-11.582, -3.029) | |||
| 35-44 | -0.722 (-2.406, 0.962) | -0.469 (-5.717, 4.780) | |||
| 45-54 | -0.641 (-1.940, 0.658) | -2.386 (-5.752, 0.980) | |||
| 55-64 | -0.997 (-1.971, -0.023) | -1.930 (-5.331, 1.472) | |||
| 65 and over | -1.447 (-2.952, 0.057) | 0.995 | -4.192 (-9.646, 1.261) | 0.795 | |
| Ethnicity | |||||
| July 4, 2020 (Lockdown relaxation date) | Non-white | 1.302 (0.085, 2.518) | 3.185 (-2.139, 8.510) | ||
| White | -0.657 (-1.129, -0.185) | 0.018 | -3.044 (-4.830, -1.259) | 0.035 | |
| July 24, 2020 (Face-covering start date) | Non-white | -0.104 (-1.715, 1.506) | -0.380 (-6.308, 5.548) | ||
| White | -1.243 (-1.957, -0.529) | 0.348 | -3.567 (-5.888, -1.246) | 0.410 | |
| Religion | |||||
| July 4, 2020 (Lockdown relaxation date) | Non-Christian | -0.369 (-0.934, 0.195) | 0.522 | -2.500 (-4.563, -0.437) | 0.904 |
| Christian | -0.652 (-1.298, -0.006) | -2.679 (-4.909, -0.449) | |||
| July 24, 2020 (Face-covering start date) | Non-Christian | -1.298 (-2.290, -0.306) | 0.578 | -3.473 (-6.483, -0.464) | 0.957 |
| Christian | -0.928 (-1.630, -0.226) | -3.354 (-6.289, -0.420) | |||
| Education | |||||
| July 4, 2020 (Lockdown relaxation date) | A-level or less | -1.363 (-1.929, -0.797) | 0.007 | -3.958 (-6.641, -1.275) | 0.221 |
| Higher degree | -0.080 (-0.512, 0.352) | -1.955 (-3.408, -0.502) | |||
| July 24, 2020 (Face-covering start date) | A-level or less | -1.421 (-2.058, -0.783) | 0.460 | -4.109 (-6.780, -1.438) | 0.561 |
| Higher degree | -0.876 (-1.712, -0.041) | -2.667 (-5.356, 0.022) | |||
| Accommodation | |||||
| July 4, 2020 (Lockdown relaxation date) | Rented | -0.369 (-1.449, 0.712) | 0.796 | -1.933 (-5.935, 2.068) | 0.675 |
| Own | -0.517 (-0.919, -0.114) | -2.719 (-4.784, -0.653) | |||
| July 24, 2020 (Face-covering start date) | Rented | -1.837 (-3.056, -0.618) | 0.197 | -4.387 (-9.165, 0.391) | 0.571 |
| Own | -0.782 (-1.419, -0.144) | -2.820 (-4.892, -0.748) | |||
| Require shielding by government | |||||
| July 4, 2020 (Lockdown relaxation date) | Not required | -0.322 (-0.750, 0.107) | 0.241 | -2.212 (-3.717, -0.706) | 0.560 |
| Required shielding, but not shielding | -1.243 (-2.295, -0.191) | -4.136 (-8.303, 0.032) | |||
| Required shielding and shielding | -0.655 (-2.023, 0.713) | -3.447 (-8.512, 1.619) | |||
| July 24, 2020 (Face-covering start date) | Not required | -0.978 (-1.721, -0.234) | 0.393 | -3.175 (-5.683, -0.668) | 0.956 |
| Require shielding, but not shielding | -1.045 (-2.351, 0.261) | -3.730 (-10.106, 2.647) | |||
| Require shielding and shielding | -3.064 (-4.686, -1.442) | -4.742 (-10.111, 0.628) | |||
| Experience of COVID-19 | |||||
| July 4, 2020 (Lockdown relaxation date) | No | -0.559 (-1.279, 0.161) | 0.892 | -1.999 (-4.771, 0.774) | 0.657 |
| Yes | -0.490 (-0.961, -0.018) | -2.795 (-4.666, -0.924) | |||
| July 24, 2020 (Face-covering start date) | No | -1.927 (-2.904, -0.951) | 0.156 | -6.223 (-10.542, -1.905) | 0.131 |
| Yes | -0.875 (-1.621, -0.129) | -2.462 (-4.509, -0.416) | |||
| Pre-existing mental health condition | |||||
| July 4, 2020 (Lockdown relaxation date) | No | -0.343 (-0.729, 0.043) | 0.551 | -2.308 (-3.782, -0.834) | 0.788 |
| Yes | -0.649 (-1.582, 0.284) | -2.772 (-6.246, 0.702) | |||
| July 24, 2020 (Face-covering start date) | No | -0.687 (-1.194, -0.181) | 0.239 | -1.407 (-3.154, 0.340) | 0.056 |
| Yes | -1.576 (-3.163, 0.012) | -6.239 (-10.192, -2.286) | |||
| Drinking alcohol | |||||
| July 4, 2020 (Lockdown relaxation date) | Never | -1.025 (-2.463, 0.412) | -3.091 (-7.778, 1.596) | ||
| Monthly or less | -0.582 (-1.779, 0.615) | -3.020 (-6.621, 0.581) | |||
| 2-4 times a month | -0.243 (-0.901, 0.415) | -2.017 (-4.434, 0.401) | |||
| 2-3 times a week | -0.050 (-0.543, 0.443) | -1.782 (-3.882, 0.319) | |||
| 4 times or more a week | -1.165 (-2.178, -0.151) | 0.401 | -3.784 (-7.229, -0.340) | 0.828 | |
| July 24, 2020 (Face-covering start date) | Never | -1.309 (-3.955, 1.337) | 0.835 | 2.636 (-2.839, 8.111) | 0.607 |
| Monthly or less | -1.240 (-2.787, 0.306) | -2.619 (-5.693, 0.455) | |||
| 2-4 times a month | -1.251 (-2.243, -0.259) | -6.981 (-10.394, -3.568) | |||
| 2-3 times a week | -1.140 (-1.694, -0.587) | -4.444 (-7.173, -1.715) | |||
| 4 times or more a week | -0.601 (-2.269, 1.067) | -1.616 (-6.815, 3.583) | |||
| Taking drugs | |||||
| July 4, 2020 (Lockdown relaxation date) | No | -0.504 (-0.890, -0.118) | 0.542 | -2.522 (-4.160, -0.883) | 0.955 |
| Yes | 0.631 (-3.023, 4.286) | -2.827 (-12.067, 6.412) | |||
| July 24, 2020 (Face-covering start date) | No | -1.114 (-1.669, -0.558) | 0.875 | -3.571 (-5.538, -1.604) | 0.222 |
| Yes | -1.470 (-6.338, 3.398) | 5.805 (-11.429, 23.039) | |||
| Suicidal thoughts ever | |||||
| July 4, 2020 (Lockdown relaxation date) | No | -0.173 (-0.599, 0.252) | 0.039 | -0.941 (-2.482, 0.600) | 0.003 |
| Yes | -1.232 (-1.983, -0.481) | -5.938 (-8.759, -3.118) | |||
| July 24, 2020 (Face-covering start date) | No | -0.831 (-1.343, -0.319) | 0.337 | -2.520 (-4.065, -0.975) | 0.511 |
| Yes | -1.588 (-3.487, 0.310) | -4.256 (-9.486, 0.974) | |||
Compared to discontinuities seen in Figures 2 and 3, the smaller discontinuities in outcomes are due to controlling for the effects of a large set of individual risk factors. This should be obvious as the regressions control for individual risk factors. We have focused on mental health changes at the cut-off dates only, not the differences in the entire time span. Therefore, we do not rely on the results shown in Tables 2 and 3.
Overall, the coefficients suggest a statistically significant fall in both anxiety and distress scores at the two policy changes dates. The fall in GAD-7 score at the first and second cut-off dates was -0.513 (95%CI: -0.913, -0.112) and -1.148 (95%CI: -1.800, -0.496), respectively. The corresponding figures for IES-R were -2.620 (95%CI: -4.279, -0.961) and -3.449 (95%CI: -5.725, -1.172), respectively. These figures suggest that both anxiety and distress reduced when the lockdown relaxation and the face covering measures were introduced. The reductions in mental health scores were higher when the face covering policy was introduced compared to the start of the lockdown relaxation.
There was no statistically significant reduction in the GAD-7 (0.017, 95%CI: -0.602, 0.673) and IES-R scores (-1.643, 95%CI: -3.914, 0.628) for health workers and other key workers (GAD-7: -0.756, 95%CI: -1.877, 0.365; IES-R: -1.704, 95%CI: -5.115, 1.708) at the first cut-off date. However, for health workers, when face covering was introduced the GAD-7 score reduced significantly, although there was no significant change in their IES-R score. At the second cut-off date, other key workers had a significant reduction in IES-R (-5.458, 95%CI: -9.144, -1.772) but no statistically significant change in GAD-7 score (-1.421, 95%CI: -3.454, 0.613).
Anxiety and distress scores significantly reduced for both females (GAD-7: -0.496, 95%CI: -0.983, -0.010; IES-R: -2.606, 95%CI: -4.445, -0.767) and males (GAD-7: -0.622, 95%CI: -1.653, 0.409; IES-R: 2.461, 95%CI: -5.929, 1.007) at the first cut-off date and also at the second cut-off date (females: GAD-7: -1.013, 95%CI: -1.778, -0.248; IES-R: -3.369, 95%CI: -5.789, -0.948) (males: GAD-7: -1739, 95%CI: -2.993, -0.485; IES-R: -3.112, 95%CI: -6.985, -0.762). At both dates, the fall in GAD-7 were higher among males compared to females. IES-R shows the opposite picture. Those below 21 years of age showed a statistically significant decline in GAD-7 (-5.482: 95%CI: -9.526, -1.437) at the first cut-off date compared to all other age groups. However, the reductions in mental health scores were not statistically significant in the below 21 years group when the face covering policy was introduced (GAD-7: -0.983, 95%CI: -5.502, 3.536).
People from white ethnic background had a significant reduction in GAD-7 (-0.657, 95%CI: -1.129, -0.185 at the first cut-off date; and -1.243, 95%CI: -1.957, -0.529 at the second cut-off date) and IES-R (-3.044, 95%CI: -4.830, -1.259 at the first cut-off date; -3.567, 95%CI: -5.888, -1.246 at the second cut-off date). There was no statistically significant change in the mental health status of non-white ethic population in the study.
Christians had a statistically significant fall in GAD-7 (-0.652, 95%CI: -1.298, -0.006 at the first cut-off date; -0.928, 95%CI: -1.630, -0.226 at the second cut-off date) and IES-R (-2.679, 95%CI: -4.909, -0.449 at the first cut-off date; -3.354, 95%CI: -6.289, -0.420 at the second cut-off date). At the first cut-off date, non-Christians had a significant decrease only in IES-R (-3.473, 95%CI: -6.483, -0.464). At the second cut-off date, non-Christians had a significant reduction in GAD-7 (-1.298, 95%CI: -2.290, -0.306) and IES-R: (-3.473, 95%CI: -6.483, -0.464).
There were significant reductions in the anxiety and distress scores of people with A-level or below and higher degree at both cut-off points. However, for higher degree holders, the improvements in mental health were seen only in IES-R (-1.955, 95%CI: -3.408, -0.502) at the first cut-off date and GAD-7 at the second cut-off date (-0.876, 95%CI: -1.712, -0.041). The lower educated group had a greater improvement in mental health at both cut-off dates.
People living in rented accommodation did not report improvements in their mental health at the first cut-off date (GAD-7: -0.369, 95%CI: -1.449, 0.712; IES-R: -1.933, 95%CI: -5.935, 2.068), but did report an improvement at the second cut-off date for GAD-7 only (-1.837, 95%CI: -3.056, -0.618). Those living in their own accommodation had statistically significant improvements in both GAD-7 and IES-R at both cut-off dates.
Those who were shielding did not report any improvements in their mental health at the first cut-off date (GAD-7: -0.655, 95%CI: -2.023, 0.713 and IES-R: -3.447, 95%CI: -8.512, 1.619). There was improvement in GAD-7 at the second cut-off date for this group. Those who were not shielding had no improvement in mental health, except for GAD-7 at the first cut-off date (-1.243, 95%CI: -2.295, -0.191).
Those who experienced COVID-19 illness reported an improvement in their mental health status at the first (GAD-7: -0.490, 95%CI: -0.961, -0.018) and second (GAD-7: -0.875, 95%CI: -1.621, -0.129) cut-off dates. Those who did not experience any such problems reported an improvement in their mental health at the second cut-off date only.
People who had previous mental health conditions did not experience statistically significant improvements in their mental health at the first cut-off date (GAD-7: -0.649 95%CI: -1.582, 0.284; IES-R: -2.772, 95%CI: -6.246, 0.702). At the second cut-off date, there was improvement for this group in IES-R (-6.239, 95%CI: -10.192, -2.286), but not in GAD-7. For those with no mental health issues, improvement in GAD-7 was noted at the second cut-off date.
Statistically significant improvement in mental health was seen at the first cut-off date among respondents who drank alcohol 4 or more times in a week (GAD-7: -1.165, 95%CI: -2.178, -0.151; IES-R: -3.784, 95%CI: -7.229, -0.340). At the second cut-off date, those who drank alcohol moderately had statistically significant improvement in the measured mental health indices. Those who were taking drugs did not experience an improvement in their mental health scores at the first (GAD-7: 0.631, 95%CI: -3.023, 4.286; IES-R: -2.827, 95%CI: -12.067, 6.412) or second cut-off dates (GAD-7: -1.470, 95%CI: -6.338, 3.398; IES-R: 5.805, 95%CI: -11.429, 23.039). However, at both cut-off dates, there were significant improvements in the mental health of those who did not take drugs.
Those who reported suicidal thoughts ever in their life showed improvements in their mental health at the first cut-off date (GAD-7: -1.232, 95%CI: -1.983, -0.481; IES-R: -5.938, 95%CI: -8.759, -3.118), but not at the second cut-off date (GAD-7: -1.588, 95%CI: -3.487, 0.310; IES-R: -4.256, 95%CI: -9.486, 0.974). However, those who had no suicidal thoughts had no improvements in their mental health at the first cut-off date (GAD-7: -0.173, 95%CI: -0.599, 0.252; IES-R: -0.941, 95%CI: -2.482, 0.600), but did improve at the second cut-off date (GAD-7: -0.831, 95%CI: -1.343, -0.319; IES-R: -2.520, 95%CI: -4.065, -0.975).
These results would be robust if the local randomization exists around the cut-off (policy changing) dates, meaning that individuals are randomly distributed around the cut-offs. If it can be shown that all control variables (e.g., demographics, pre-existing health conditions, and lifestyles, which are dummy variables) are insignificantly discontinuous at those cut-off dates, it can be said that the local randomization exists around those cut-offs. In other words, insignificant discontinuities in control variables will guarantee that significant discontinuities in mental health scores (GAD-7 and IES-R) happen due only to policy changes (relaxation of lockdown and face-covering), not due to changes in the control variables, which also affect those mental health scores.
Separate OLS regressions of every control dummy following the same RDD specification in equation were run. The outcome variable was just replaced with the control dummy. Every dummy has a base category, for which the dummy variable is not needed; otherwise, there would be a dummy trap. For that reason, when the male dummy is used, for example, the female dummy is not needed, and Supple
Other biases (caused by unobserved factors’, changes or any other policy changes that affect mental health outcomes) can be captured by checking discontinuities in the density of the assignment/trend variable. We found this was statistically insignificant (not shown). There were no other national policy changes at exactly those cut-off dates. From the visual inspection of Figures 2 and 3, there were no clear discontinuities in mental health outcomes at any other dates. If discontinuities in mental health outcomes at the policy changing cutoff dates were random events, there would have been such discontinuities at other dates. This informal falsification test also implies that our results capture mostly causal effects.
A key limitation of this study is a high number of missing cases and non-random selection of participants. However, the methodology used in this study mitigates against this limitation by comparing matching cases before and after each policy intervention. Identification tests imply that local randomization exists around the cut-off dates, implying that the findings are robust.
Another limitation is the non-probability sample design and time limited survey which means longitudinal changes were not possible to elicit. Similarly, pre pandemic data was not available, although this was not possible for this survey which was not designed pre pandemic. However, the results from phase one will be compared to phase two of the survey that was conducted from November 20, 2020 to February 2021.
This paper examined the association of the lockdown relaxation and the implementation of the face covering policy on the mental health of the general population and sub-groups in the United Kingdom using interrupted time series model. Mental health status was measured using two standardised mental health measures, GAD-7 and IES-R.
This study in the United Kingdom reports a casual association of lockdown on mental health of the participants. The findings compare with similar research carried out in the United Kingdom which showed “minimal” impact of lockdown on the mental health of the general population[1,8,9]. One of the reasons for “mild” anxiety and distress in the United Kingdom during lockdown may be because of several economic and welfare government policies.
This study confirms improvements in anxiety and distress levels following lockdown relaxations. Relaxation of lockdown started on July 4, 2020 in the United Kingdom and showed significant improvements in the population’s mental health conditions. However, much greater improvement in anxiety and distress was observed when face covering in public places was enforced on July 24, 2020. It appears that face covering provided confidence in protection from the virus while visiting friends, public places, clinics, shops and other such places. It may be noted here that when lockdown relaxations were implemented on July 4, 2020, face covering use in the United Kingdom was very limited. Face covering implementation in public places had a significant positive association with mental health on all population sub-groups, suggesting wider benefit of the face covering policy on mental health.
This study identified significantly higher levels of anxiety and distress among people with pre-existing mental health issues, those who were shielding, those who reported suicidal thoughts, drug and alcohol use, and experience of episodes of COVID-19 illness. These population sub-groups benefited by both lockdown relaxation and face covering policy. However, face covering had a greater association with improvement in anxiety and distress than lockdown relaxation.
Higher levels of anxiety and distress among females and younger age groups were noted in this study, which is similar to the emerging global evidence[20]. The findings also compare to other studies that have reported differential impact of COVID-19 Lockdown restrictions on mental health by predisposing health conditions and socio-demographic characteristics. An international study carried out by CARE in 40 countries showed that 27% of women reported an increase in challenges associated with mental illness compared to only 10% of men[20]. A study carried out in Tunisia showed anxiety, depressive symptoms, and stress were found in about 85% of women[21]. Other studies also reported experience of higher mental health problems among females compared to males[6]. A meta-analysis of 206 studies showed minimal differences in the prevalence of mental health issues such as anxiety, depression, and PTSD among healthcare professionals and the public during the pandemic. A new development in this study was that there appears to be higher prevalence of suicidal thoughts/ideation or self-harm (11% vs 5.8%) and lower prevalence of wellbeing (28.2% vs 52.6%) among the public compared to healthcare professionals which had previously not been reported[22]. Globally there is evidence of domestic violence and more workload for women than men during lockdown[23-26]. There is evidence of lower participation of women in COVID-19 related policy committees[27].
Similar to findings from this study, there is evidence from various studies that the younger age groups had higher levels of mental health problems during lockdown restrictions compared to older age groups[6]. However, older adults have shown lower sleeping quality during the pandemic period compared to the pre-pandemic period[28].
Health workers, particularly frontline staff, played an important role during the pandemic. At the beginning of the pandemic, there is evidence of increased mental health impact on health workers. For example, at the time of COVID-19 in China and Japan, depression, anxiety, insomnia and resilience were higher among frontline health workers than the general population[29,30]. The prevalence of depression, anxiety, and stress has been shown to have remained elevated even after the restrictions were lifted in a study in Malaysia[31]. In this study, anxiety and stress levels of health workers were lower than other key workers. The reason for low levels of anxiety and stress among health workers is currently less understood and a probable reason could be their professional attitude and support from the general public for the important work they do for the country. One can also hypothesise that the health workers learned self-help stress-management and mindfulness that they prescribed to their patients[32]. Studies have also reported increased mental health problems in those who had chronic/psychiatric illnesses, unemployment, student status, and frequent exposure to social media/news concerning COVID-19, compared to their counterparts[6,33]. Living alone during the lockdown, a longer duration of illness, and smoking habits had higher associations with COVID-19 related distress[34]. Detachment, pre-existing mental health problems, fewer coping strategies and childlessness were associated with higher levels of depression and stress[35]. Our study shows similar findings, thereby endorsing the evidence base of the impact of the pandemic.
In conclusion, evidence is building on the differential psychological impact of the pandemic, resultant restrictions and policies, based on socio-demographic variables, pre-existing vulnerabilities and health care worker status that will help future planning and policies. Such evidence when used collectively should inform future planning for pandemics and develop collective and individual physical and mental resilience.
The global pandemic caused by coronavirus disease 2019 has led to wide spread changes in people’s day to day lives.
The changes in people’s lives and livelihoods due to the global pandemic, associated lockdowns and government guidance is anticipated to have a great impact on people’s emotional and social wellbeing.
Positive association of lockdown relaxation and face covering policies on the Mental Health of various population sub-groups is reported.
A regression discontinuity design was used to analyse data gathered on people’s health and wellbeing during different time periods and restrictions via online survey platform.
In comparison to other key workers and non-key workers during lock down, professional groups and health workers had lower generalised anxiety disorder (GAD-7) scores indicating lower anxiety levels. Similar findings were noted for the impact of events scale-revised (IES-R) scores with health workers, indicating lower levels of distress. During the compulsory face covering phase, there were improvements in mental health scores for all three professional groups assessed by GAD-7 and IES-R. Greater improvements in mental health scores were found among non-key workers than key workers. Gender was associated with different mental health outcomes during the lockdown, with females scoring higher on the GAD-7 and IES-R scales in comparison to males. However, both groups showed a significant improvement in mental health status during the period of face covering, with slightly higher improvements noted in males.
An impact on people’s wellbeing was found, with anxiety and depression levels improving when relaxations in restrictions happened.
Further investigation into pandemic preparedness for those with pre-existing conditions such as anxiety, depression or obsessive-compulsive disorders and modifying psychological interventions in this population is warranted.
We would like to thank all the participants who gave their time to complete the survey. We also thank our collaborators–NHS and non-NHS organisations that disseminated the survey.
| 1. | Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, Kontopantelis E, Webb R, Wessely S, McManus S, Abel KM. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883-892. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1854] [Cited by in RCA: 1704] [Article Influence: 284.0] [Reference Citation Analysis (0)] |
| 2. | Baraniuk C. Fears grow of nutritional crisis in lockdown UK. BMJ. 2020;370:m3193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Ropkins K, Tate JE. Early observations on the impact of the COVID-19 Lockdown on air quality trends across the UK. Sci Total Environ. 2021;754:142374. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 4. | Jassop J. The UK lockdown and the economic value of human life. Eco Affairs. 2020;40:138-147. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Miles DK, Stedman M, Heald AH. "Stay at Home, Protect the National Health Service, Save Lives": A cost benefit analysis of the lockdown in the United Kingdom. Int J Clin Pract. 2021;75:e13674. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 6. | Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, Chen-Li D, Iacobucci M, Ho R, Majeed A, McIntyre RS. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord. 2020;277:55-64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2424] [Cited by in RCA: 3106] [Article Influence: 517.7] [Reference Citation Analysis (0)] |
| 7. | Benke C, Autenrieth LK, Asselmann E, Pané-Farré CA. Lockdown, quarantine measures, and social distancing: Associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res. 2020;293:113462. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 281] [Cited by in RCA: 362] [Article Influence: 60.3] [Reference Citation Analysis (0)] |
| 8. | Daly M, Sutin AR, Robinson E. Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK Household Longitudinal Study. Psychol Med. 2020;1-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 298] [Cited by in RCA: 414] [Article Influence: 103.5] [Reference Citation Analysis (0)] |
| 9. | Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2021;8:141-149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 504] [Cited by in RCA: 694] [Article Influence: 138.8] [Reference Citation Analysis (0)] |
| 10. | O'Connor RC, Wetherall K, Cleare S, McClelland H, Melson AJ, Niedzwiedz CL, O'Carroll RE, O'Connor DB, Platt S, Scowcroft E, Watson B, Zortea T, Ferguson E, Robb KA. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry. 2020;1-8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 627] [Cited by in RCA: 663] [Article Influence: 132.6] [Reference Citation Analysis (0)] |
| 11. | Lamb D, Greenberg N, Stevelink SAM, Wessely S. Mixed signals about the mental health of the NHS workforce. Lancet Psychiatry. 2020;7:1009-1011. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Jia R, Ayling K, Chalder T, Massey A, Vedhara K. Mental health in the UK during the COVID-19 pandemic: early observations. BMJ Open. 2020;. [DOI] [Full Text] |
| 13. | Rathod S, Pallikadavath S, Young AH, Graves L, Rahman MM, Brooks A, Soomro M, Rathod P, Phiri P. Psychological impact of COVID-19 pandemic: Protocol and results of first three weeks from an international cross-section survey - focus on health professionals. J Affect Disord Rep. 2020;1:100005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 14. | Altschul D, Fawns-Ritchie C, Kwong A, Hartley L, Nangle C, Edwards R, Dawson R, Levein C, Campbell A, Flaig R, McIntosh A, Deary I, Marioni R, Hayward C, Sudlow C, Douglas E, Bell D, Portsou D. Face covering adherence is positively associated with better mental health and wellbeing: a longitudinal analysis of the CovidLife surveys. Wellcome Open Res. 2021;6. [DOI] [Full Text] |
| 15. | van der Westhuizen HM, Kotze K, Tonkin-Crine S, Gobat N, Greenhalgh T. Face coverings for covid-19: from medical intervention to social practice. BMJ. 2020;370:m3021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 16. | Hahn J, Todd P, Van der Klaauw W. Identification and estimation of treatment effects with a regression-discontinuity design. Econometrica. 2001;69:201-209. [DOI] [Full Text] |
| 17. | Angrist JD, Pischke JS. Mostly harmless econometrics: An empiricist's companion. Eur Rev Agr Eco. 2008;. [DOI] [Full Text] |
| 18. | Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11947] [Cited by in RCA: 20762] [Article Influence: 1038.1] [Reference Citation Analysis (0)] |
| 19. | Weiss DS, CR. M. The impact of event scale–revised. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York: Guilford Press, 1997: 399–411. |
| 20. | CARE. Financial Insecurity, Hunger, Mental Health are Top Concerns for Women Worldwide 2020a. [Cited 10 May 2021]. Available from: https://www.care.org/news-and-stories/press-releases/financial-insecurity-hunger-mental-health-are-top-concerns-for-women-worldwide/. |
| 21. | Sediri S, Zgueb Y, Ouanes S, Ouali U, Bourgou S, Jomli R, Nacef F. Women’s mental health: acute impact of COVID-19 pandemic on domestic violence. Arch Womens Ment Health. 2020;1-8. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 162] [Cited by in RCA: 124] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 22. | Phiri P, Ramakrishnan R, Rathod S, Elliot K, Thayanandan T, Sandle N, Haque N, Chau SW, Wong OW, Chan SS, Wong EK, Raymont V, Au-Yeung SK, Kingdon D, Delanerolle G. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: A systematic review and meta-analysis. EClinicalMedicine. 2021;34:100806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 76] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 23. | Vora M, Malathesh BC, Das S, Chatterjee SS. COVID-19 and domestic violence against women. Asian J Psychiatr. 2020;53:102227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 70] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 24. | Kofman YB, Garfin DR. Home is not always a haven: The domestic violence crisis amid the COVID-19 pandemic. Psychol Trauma. 2020;12(S1):S199-S201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 143] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 25. | Boxall H, Morgan, A. and Brown, R. The prevalence of domestic violence among women during the COVID-19 pandemic. Statistical Bulletin no. 28. Canberra: Australian Institute of Criminology, 2020: 38. |
| 26. | Sharma A, Borah SB. Covid-19 and Domestic Violence: an Indirect Path to Social and Economic Crisis. J Fam Violence. 2020;1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 90] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 27. | Wadman M. Where are the women? Science. 2020;368:21-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | Mandelkorn U, Genzer S, Choshen-Hillel S, Reiter J, Meira E Cruz M, Hochner H, Kheirandish-Gozal L, Gozal D, Gileles-Hillel A. Escalation of sleep disturbances amid the COVID-19 pandemic: a cross-sectional international study. J Clin Sleep Med. 2021;17:45-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 99] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 29. | Liang Y, Wu K, Zhou Y, Huang X, Liu Z. Mental Health in Frontline Medical Workers during the 2019 Novel Coronavirus Disease Epidemic in China: A Comparison with the General Population. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 97] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 30. | Sasaki N, Kuroda R, Tsuno K, Kawakami N. The deterioration of mental health among healthcare workers during the COVID-19 outbreak: A population-based cohort study of workers in Japan. Scand J Work Environ Health. 2020;46:639-644. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 71] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 31. | Woon LS, Sidi H, Nik Jaafar NR, Leong Bin Abdullah MFI. Mental Health Status of University Healthcare Workers during the COVID-19 Pandemic: A Post-Movement Lockdown Assessment. Int J Environ Res Public Health. 2020;17:9155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 32. | Bonen A, Hatta H, Holloway GP, Spriet LL, Yoshida Y. Reply from Arend Bonen, Hideo Hatta, Graham P. Holloway, Lawrence L. Spriet and Yuko Yoshida. J Physiol. 2007;584:707-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 33. | Sauer KS, Jungmann SM, Witthöft M. Emotional and Behavioral Consequences of the COVID-19 Pandemic: The Role of Health Anxiety, Intolerance of Uncertainty, and Distress (In)Tolerance. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 56] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 34. | Di Nicola M, Dattoli L, Moccia L, Pepe M, Janiri D, Fiorillo A, Janiri L, Sani G. Serum 25-hydroxyvitamin D levels and psychological distress symptoms in patients with affective disorders during the COVID-19 pandemic. Psychoneuroendocrinology. 2020;122:104869. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 35. | Burhamah W, AlKhayyat A, Oroszlányová M, AlKenane A, Almansouri A, Behbehani M, Karimi N, Jafar H, AlSuwaidan M. The psychological burden of the COVID-19 pandemic and associated lockdown measures: Experience from 4000 participants. J Affect Disord. 2020;277:977-985. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 75] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Member of the Royal College of Psychiatrists Revalidation Committee.
Specialty type: Psychiatry
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shawan DSA, Yu L S-Editor: Fan JR L-Editor: A P-Editor: Fan JR