Published online Oct 19, 2021. doi: 10.5498/wjp.v11.i10.754
Peer-review started: February 24, 2021
First decision: June 24, 2021
Revised: June 28, 2021
Accepted: August 2, 2021
Article in press: August 2, 2021
Published online: October 19, 2021
Processing time: 232 Days and 16.6 Hours
Yoga is considered a widely-used approach for health conservation and can be adopted as a treatment modality for a plethora of medical conditions, including neurological and psychological disorders. Hence, we reviewed relevant articles entailing various neurological and psychological disorders and gathered data on how yoga exerts positive impacts on patients with a diverse range of disorders, including its modulatory effects on brain bioelectrical activities, neurotransmitters, and synaptic plasticity. The role of yoga practice as an element of the treatment of several neuropsychological diseases was evaluated based on these findings.
Core Tip: A multitude of beneficial effects of yoga practice and the underlying mechanisms of action have been reported and point out its role as an influential element in the integrative therapy of various neuropsychological disorders. In the planning of further investigations, studies should be designed to achieve more accuracy and precision in the heterogeneous field of yoga practices and potential fields of application.
- Citation: Nourollahimoghadam E, Gorji S, Gorji A, Khaleghi Ghadiri M. Therapeutic role of yoga in neuropsychological disorders. World J Psychiatr 2021; 11(10): 754-773
- URL: https://www.wjgnet.com/2220-3206/full/v11/i10/754.htm
- DOI: https://dx.doi.org/10.5498/wjp.v11.i10.754
Several neurological disorders affect mental health and lead to various degrees of impairment in cognitive functions. The use of complementary and alternative medicine, practices that improve the mind’s capacity and body function, amongst patients with neuropsychological disorders is increasing worldwide[1,2]. Biofeedback, homeopathy, acupuncture, meditation, and yoga are among the different categories of these interventions[3]. Yoga is a form of mind-body technique that involves and contributes to both mind and body[4] and has been used as a therapeutic intervention in various neurological and psychological disorders[5]. The word “Yoga” is derived from the Sanskrit origin “yuj” meaning “yoke” or “union,” and it is assumed that yoga describes the union between mind and body[5]. As an ancient Indian non-religious mind-body method[2,6], yoga is considered a philosophical and spiritual discipline that alleviates suffering and promotes human health[4]. Yoga has been practiced in Eastern cultures as a spiritual healing method for over 4000 years. The “Yoga sutra,” a 2000-year-old guidebook, is the earliest known document of yoga that provides the framework of all branches of yoga. This book conceptualized yoga as eight limbs, which were designed to be practiced in sequence[7-9]. There are several styles of yoga, and no one is superior to another (Table 1).
| Type of yoga | Description |
| Ashtanga | Six series of postures during breathing exercises |
| Bikram | Twenty-six poses and a sequence of two breathing exercises that take place in heated rooms with high humidity |
| Hatha | Basic postures and poses with breath regulation and meditation |
| Iyengar | Focuses on the precise structural alignment of the body |
| Jivamukti | Physically intense challenging postures with meditation |
| Kripalu | Breathing exercises at the beginning, gentle stretches, and series of poses before final relaxation |
| Kundalini | Chanting at the beginning and meditation aiming to release energy |
| Sivananda | Based on a 5-point approach, including proper breathing, diet, relaxation, exercise, and positive thinking |
| Vini | Based on in-depth training aiming to be an expert on anatomy and yoga therapy |
| Prenatal | A type of yoga helping mothers with physical training and meditation |
| Yin | Focuses on releasing tension through different joints |
A rapid increase of interest in yoga in Western countries occurred in the first decades of the 19th century, which has continued to this day. The National Health Interview Survey has reported that the number of people in the United States who practice yoga has increased dramatically among all age groups between 2002 to 2012[9,10]. Yoga practice can be a treatment for a variety of disorders as well as physical exercise[9]. This leads to an increase in investigations focusing on the mechanism of action and effect of yoga intervention on various mental and physical conditions[9-11]. Yoga interventions can maintain brain health through various mechanisms, such as the improvement of cerebral oxygenation[12], enhancement of neurotrophic and angiogenic factors (such as angiogenin)[13], balancing the excitatory/inhibitory neurotransmitter equilibrium[14], modulation of immune responses[15], and pre
Yoga is a movement-based embodied contemplative activity that can lead to a variety of neurobiological alterations in different brain regions. Yoga exerts a regulatory effect on brain synaptic plasticity and promotes cognitive tasks, particularly working memory[17,18]. Furthermore, yoga increases inter-hemispheric coherence and symmetry and improves neurocognitive functions[19]. Yoga may also exert pronounced anatomical changes in different brain regions, especially in the limbic system[20].
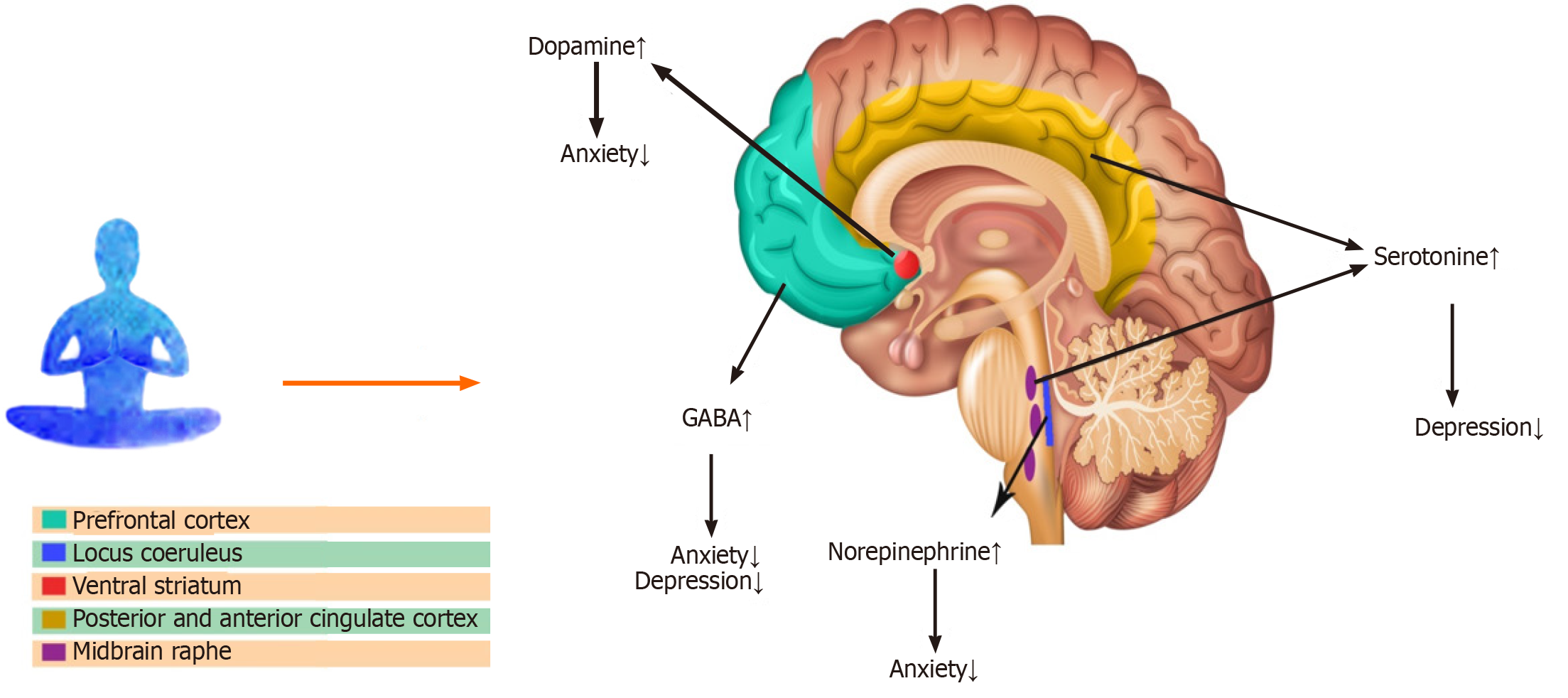
γ-aminobutyric acid (GABA) is considered the main inhibitory neurotransmitter responsible for the regulation of cortical excitability and neural plasticity[21,22]. Multiple lines of evidence suggest that yoga promotes cortical GABAergic inhibitory tone and modulates downstream brain regions[14,23]. A 12 wk yoga practice markedly enhanced the thalamic GABA values, accompanied by improved mood and reduced anxiety[24]. Higher thalamic GABA levels could be the result of enhanced (regional) cerebral blood flow in the prefrontal cortex of yoga practitioners[25], which can lead to the activation of the reticular nucleus of the thalamus and higher GABA production[26,27]. A magnetic resonance spectroscopy study has shown that yoga practitioners exhibited greater brain GABA values after a 60 min session of yoga training compared to controls[28]. In addition to GABA, an enhancement of dopamine has been observed in the ventral striatum of subjects who practice yoga[25,29,30]. It has been suggested that yoga could cause a rise in serotonin. Several investigations performed on participants after their meditation sessions have shown an elevation of the serotonin metabolite levels in urine[25,31]. Moreover, a regular yoga practice may cause a reduction in norepinephrine values. Patients with heart failure who practiced weekly yoga displayed lower levels of norepinephrine in blood samples[30,32] (Figure 1).
Yoga practices regulate electroencephalogram (EEG) signals through switching off non-relevant neural circuits for the preservation of focused attention and blockade of inappropriate signals[33]. Studies on the effects of yoga on brain waves revealed that breathing, meditation, and posture-based yoga practice increase overall brain activity[19], particularly in the amygdala and the frontal cortex. Alpha brain waves pre
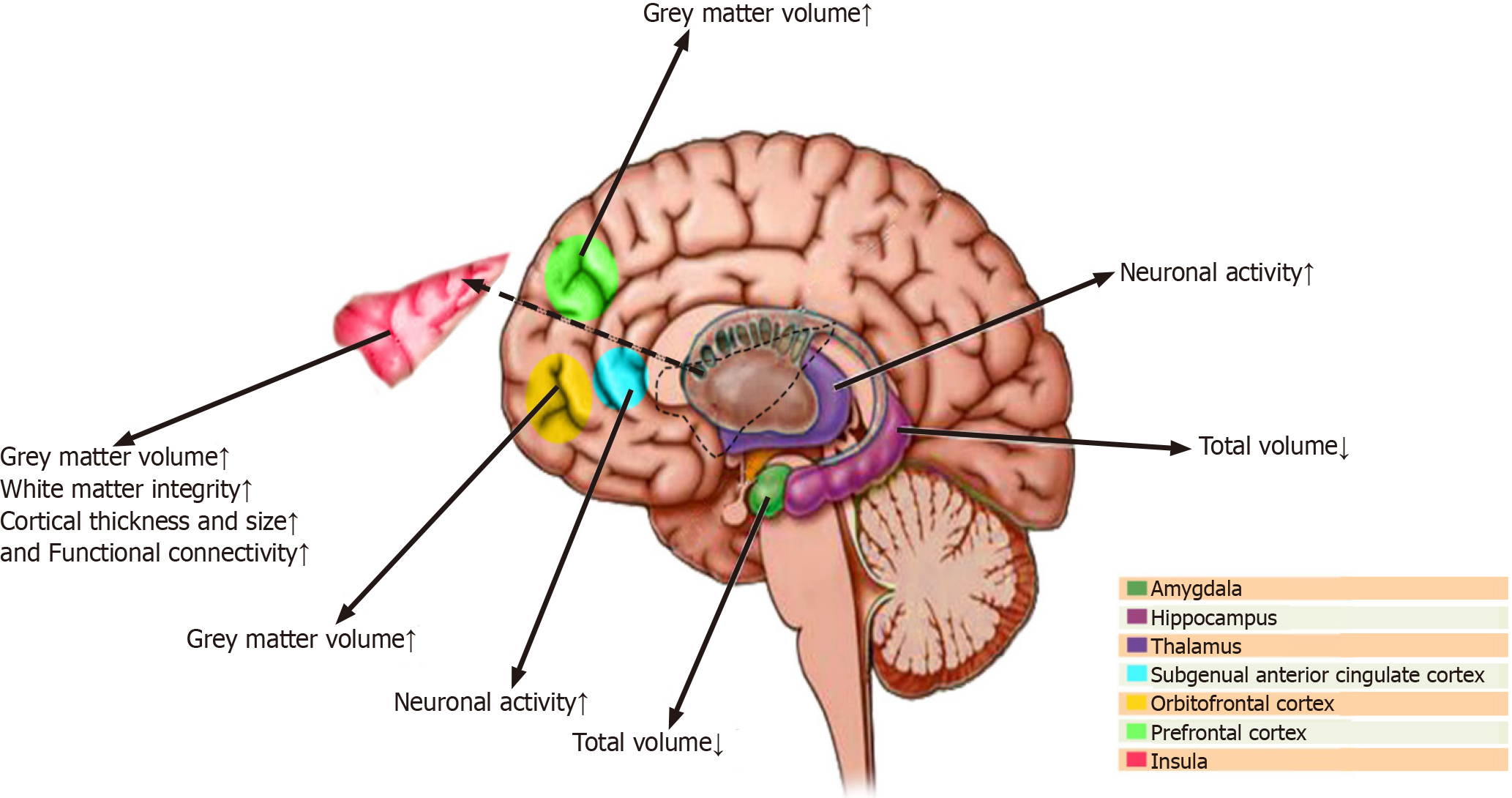
Yoga intervention seems to be associated with brain structural alterations, particularly in the frontal cortex, amygdala, hippocampus, insula, and anterior cingulate cortex[42]. An investigation on regional differences in grey matter volume associated with the practice of yoga has shown a greater grey matter volume in different areas of the dominant hemisphere, including the ventromedial orbitofrontal, ventrolateral prefrontal, and inferior temporal and parietal cortices as well as the left insula in skilled practitioners of yoga[43]. Furthermore, elderly yoga practitioners with several years of yoga experience have shown greater neocortical thickness in the left prefrontal complex cluster, which includes part of the lateral middle frontal gyrus, dorsal superior frontal gyrus, and anterior superior frontal gyrus compared to healthy non-practitioners[44]. A magnetic resonance imaging study revealed the greater volume of gray matter in the left hippocampus in skilled yoga practitioners with at least 3 years of experience compared to the sex- and age-matched control subjects[18]. A population-based study on 3742 subjects revealed a lower right amygdala volume and a lower left hippocampus volume in those who participate in meditation and yoga practices[45] (Figure 2).
Yoga and headaches: Several studies have suggested the beneficial effects of yoga in reducing the frequency and intensity of various forms of headaches, particularly migraine and tension headaches[46]. Yoga has been suggested as a potential complementary therapeutic intervention for headaches[47]. A meta-analysis on yoga for tension-type headaches and migraine has shown preliminary evidence of a short-term beneficial effect of yoga on tension-type headaches. This study revealed a significant improvement in the frequency, duration, and intensity of pain in patients with tension-type headaches[48]. A randomized controlled trial evaluating the beneficial effects of yoga on 114 patients with migraines has shown a significantly greater improvement in various migraine measures, including headache frequency, intensity, and use of rescue medications[49]. Another randomized controlled study with 19 subjects suffering from episodic migraine has shown a reduction in headache intensity, duration, depression, and anxiety as well as an improvement of self-efficacy, migraine-related disability, and quality of life from baseline to initial follow-up[50]. A significant improvement of self-perceived pain frequency, pain intensity and duration, and psychological status as well as a reduction in medication consumption was observed in 31 patients with chronic migraine[51]. Furthermore, a significant decrease in headache frequency, medication intake, and stress perception has been reported in 20 patients with migraine or tension headaches[52]. Yoga has been suggested as a potentially effective approach to reducing headaches associated with menopause[53].
Multiple investigations have explored the mechanisms of action of yoga on headaches. Migraine is a neurovascular disorder with significant upregulation of endothelial adhesion molecules[2,54]. It has been suggested that yoga intervention alleviates pain primarily via modulation of the pain perception system, including the anterior cingulate cortex, insula, sensory cortex, and thalamus[55]. A study on 42 women with migraines evaluated the effect of yoga on endothelial dysfunction in migraine patients. A 12 wk yoga training program increased delivering O2 to the body and reduced peripheral vascular resistance with a significant reduction in plasma values of vascular cell adhesion molecule, which suggests an improvement of vascular function in patients with migraine[8,51,56,57]. The amplitude of the contingent negative variation, an ultra-slow neocortical event-related potential, is significantly greater in patients with migraine compared to healthy controls, which indicates higher cortical excitability[58]. Subjects with migraines, who practice meditation, including yoga, have shown significantly lower amplitude of contingent negative variation[59].
Yoga and Alzheimer’s disease: Alzheimer’s disease (AD) is characterized by neuronal loss, mostly in the neocortex and the hippocampus[2,60], and is associated with memory and cognitive impairments and neuropsychiatric dysfunctions[2,60]. It has been suggested that yoga exerts a beneficial impact on overall brain health in healthy elderly subjects, older people with mild cognitive dysfunction, and subjects with dementia[61]. Yoga practice promotes cognitive function, affective interaction, and physical abilities of the healthy elderly population[62] and exerts a positive impact on total brain volume, neocortical grey matter thickness, and functional connectivity between different brain regions in subjects with mild cognitive dysfunction[63]. Using magnetic resonance imaging volumetric analysis, a trend toward decreased hippocampal volume atrophy has been observed after an 8 wk of yoga practice in patients with mild cognitive dysfunction[64]. A randomized neuroimaging study with 14 subjects has shown that yoga and mindfulness meditation may decrease hippocampal atrophy and promote functional connectivity between different brain regions, including the posterior cingulate cortex, the medial prefrontal cortex, and the hippocampus in adults susceptible to dementia[64]. Furthermore, it has been shown that mind-body interventions, such as yoga, can restore cognition in persons with mild cognitive impairment and delay the onset of AD[65,66]. Elderly subjects suffering from mild to moderate dementia have exhibited an improvement of behavioral impairments after a 12 wk yoga training program[67]. Metabolic enhancement for neurodegeneration, a novel therapeutic approach for AD, has merged yoga and meditation into other treatments of early AD pathology and achieved sustained cognitive improvement in 90% of patients[68]. Yoga may enhance blood flow to areas of the brain that modulate memory functions, reduce neuronal injury, promote the symptoms of early dementia, and delay the onset of AD[69]. Yoga can also improve the physical disability of patients with AD, such as walking, gait speed, and balance[70].
Although the mechanism of yoga action on AD needs to be elucidated, some possible mechanisms have been suggested. The serum values of several neurotrophic factors, such as brain-derived neurotrophic factor, increase after yoga practice in healthy individuals[71]. This may also occur in patients with mild to moderate AD and exerts a neuroprotective effect on the neurodegenerative process of AD[61]. The long-term practice of yoga also increases the serum value of serotonin[72]. The neuroprotective effects of yoga may be due to the enhancement of serotonin. Serotonin significantly destabilizes Aβ fibrils and protects neuron Aβ-induced cell injury and death[73]. The serum levels of melatonin significantly increased after a 3 mo period of yogic practices[74]. Melatonin reduces the Aβ level[75] and promotes microvessel abnormalities in the neocortex and the hippocampus[76] in experimental AD models.
Yoga and epilepsy: The goal of therapeutic approaches for epilepsy, a common neurological disorder characterized by abnormal electrical brain activity[77], is to eliminate or decrease the number and duration of seizures and improve the quality of life[2,78]. Several studies suggest that yogic practices can ameliorate seizures in patients with different types of epilepsy. An investigation on the effects of yoga intervention on seizures and EEG of 32 patients suffering from idiopathic epilepsy has revealed 62% and 83% reduction of seizure frequency 3 and 6 mo after the inter
Yoga and multiple sclerosis: Several clinical trials investigated the potential beneficial effects of yoga therapy in patients with multiple sclerosis (MS), an autoimmune neuroinflammatory demyelinating disorder of the central nervous system[83]. A study tested the effects of a 6 mo yoga intervention on the improvement of different aspects of physical as well as psychosocial conditions in 44 patients with MS and 17 healthy relatives. This investigation has shown significant improvements in the quality of life, walking speed, fatigue, and depression values. However, yoga did not promote the pain, balance, and physical status of these patients[84]. A pilot study on 12 patients suffering from MS has suggested that various yoga trainings for 6 mo may lead to a significant improvement in postural balance and daily physical activities[85].
Another clinical study on 24 participants diagnosed with mild to moderate MS, which underwent an intensive yoga practice for more than 4 mo, has shown marked improvements in the peak expiratory flow rate, physical conditions, mental health, and quality of life of patients with MS[86]. A study conducted on 60 female patients with MS revealed that yoga training significantly improved physical abilities and sexual satisfaction[87]. Yogic training and relaxation have also been suggested for the improvement of neurogenic bladder dysfunction in patients with MS[88].
A qualitative case investigation on a woman with MS suggested that individualized yoga intervention for 6 mo could be beneficial for the improvement of muscle tone and strength as well as self-confidence and stamina[89]. A significant improvement in balance, gait, fatigue, walking speed, and step length has been reported in 18 patients with relapsing-remitting MS after a 12-wk yoga training[90]. Yoga intervention has also exerted a beneficial role on improvements of postural balance and reduction of the influence of postural balance impairment during daily activities in patients diagnosed with MS after yoga practice for 6 mo[85]. A meta-analysis of 10 randomized controlled trials with overall 693 patients with MS who trained with different forms of yoga has revealed a significant improvement of fatigue but no effects on the overall quality of life, sexual function, and psychosocial condition[91].
Yoga and Parkinson’s disease: The potential beneficial therapeutic effects of a yoga intervention for Parkinson’s disease (PD), a chronic and debilitating neurodegenerative disorder, have been investigated. Yoga exerts a range of beneficial effects on different symptoms of PD[92]. A question-based survey on 272 patients with PD has shown that the majority of patients found yoga and meditation helpful for the alleviation of both motor and non-motor (fatigue, sleep difficulties, pain) symptoms[93]. A randomized clinical study on 126 patients with mild to moderate PD who underwent weekly yoga training for 8 consecutive weeks has shown a significant alleviation of psychological symptoms, improvement of the quality of life, and reduction of motor symptoms[94]. Yoga exercises can improve flexibility and balance, decrease muscle rigidity, increase the range of motion, and promote muscle strength in patients with PD[95]. Yoga intervention effectively improves balance and proprioceptive acuity in 33 patients with mild to moderate PD[96]. It has been suggested that incorporating yoga and occupational therapy may promote balance and decrease falls in patients with PD[97]. Yoga training decreases the back pain associated with a lower postural instability, which may reduce falls in patients with PD[98]. Furthermore, yoga as adjunctive therapy in patients with PD has been suggested as an effective treatment for the reduction of psychological complications, particularly anxiety and depression[99-101].
Yoga and neuropathy: Peripheral neuropathy is a common neurological condition due to physical nerve injury, diabetes mellitus, autoimmune disorders, malignancy, kidney failure, nutritional deficiencies, systemic disorders, and idiopathic neuropathies, which can implicate the motor, sensory, and/or autonomous peripheral nerves[102,103]. Several lines of evidence suggest that yoga may alleviate symptoms of various neuropathies[104,105].
Several reports suggest the beneficial effects of yoga practices in patients with neuropathy. Yoga practices were shown to improve numbness and weakness in lower extremities after a stretch or compression injury of the gluteal nerves[106], alleviate chronic pain due to diabetic neuropathy[107], and promote sensory functions and muscle movement in subjects with diabetic peripheral neuropathy[108]. However, it should be noted that some reports indicate yoga-induced nerve injury and neuropathy[109-111], particularly in patients who take sedative medications, people with benign hypermobility of their connective tissue, and the elderly[110,112,113]. Furthermore, yoga may ease compression and decrease nerve compression in carpal tunnel syndrome, which could lead to the improvement of numbness after a few weeks of practice[114,115]. Yoga mediation therapy improved the nerve conduction velocity, which was associated with glycemic control, in patients with diabetic neuropathy[116,117]. A reduction of the impact of chemotherapy-induced peripheral neuropathy symptoms on the lives of patients with breast cancer as well as on the pain intensity after yoga intervention has been reported[118,119].
Yoga, stress, and anxiety: Stress and anxiety are increasing in incidence worldwide. Approximately 34% of the general population is affected by an anxiety disorder during their lifetime[120]. Several investigations were performed on the feasibility and potential efficacy of different forms of yoga on anxiety- and stress-induced symptoms in both children and adults. It has been suggested that yoga may promote mental and physical strength, increase stress resilience, and reduce anxiety[121]. Although some studies do not show any effect[122,123], most investigations indicate that yoga can be effective in the alleviation of anxiety in the form of monotherapy or adjunctive therapy[124-127]. Functional magnetic resonance imaging evaluation revealed that yoga interventions modulate the activity of various brain areas that are crucial to emotion regulation, such as the superior parietal lobule and supramarginal gyrus, and lead to a diminished sympathetic response to stressful emotional stimulations[128]. Training of mindfulness- and yoga-based programs has shown a significant reduction of anxiety symptoms, which was associated with a marked decrease of structural connectivity of the right amygdala[129]. Furthermore, it has been suggested that yoga intervention modulates stress-induced autonomic regulatory reflex and inhibits the production of adrenocorticotropic hormone from the anterior pituitary gland[130], resulting in decreased production of cortisol from the adrenal gland[131].
A meta-analysis revealed that more yoga exercises were accompanied by greater benefits, particularly when subjects were suffering from higher values of anxiety at the early stages[132]. Another meta-analysis of eight trials with 319 adults diagnosed with anxiety disorders who underwent yoga training indicates that yoga could be a safe and effective intervention to reduce the intensity of anxiety[133]. Rhythmic yoga meditative interventions resulted in a reduction of stress associated with a higher plasma dopamine level together in 67 healthy subjects who regularly engaged in mind-body training[134]. Enhancement of dopamine values following yoga practice leads to a suppression of corticostriatal glutamatergic transmission and regulation of conscious states[29]. Yoga interventions have been suggested to enhance vigilance, improve sleep, and reduce anxiety in healthy security personnel[135].
Yoga-based exercises in schools have been suggested to reduce stress and challenging behavioral and cognitive responses to stress, promote physical ability, and strengthen cognitive performance among students[136,137]. Yoga interventions for a period of 8 wk have shown a significant impact on reducing anxiety in school-age children[138]. Using a yoga-based relaxation method (mind-sound resonance technique) alleviated state anxiety and mind wandering and promoted state mindfulness and performance in school children[139]. High-frequency yoga breathing training promotes attention and reduces anxiety in students aged 11-12 years[140]. Furthermore, evaluation of the effect of yoga intervention on stress perception and anxiety levels in college students has shown a significant reduction in anxiety and stress scores associated with a marked enhancement of total mindfulness[141]. Yoga can also help adolescents hospitalized in an acute care psychiatric ward to lessen their emotional distress[142]. Yoga exerts a bifacial effect on the reduction of anxiety and improvement of self-esteem in orphanage residents[143].
Practicing yoga in patients suffering from post-traumatic stress disorder for at least 4 wk resulted in a significant reduction of cortisol values[144]. Yoga practices significantly reduce stress and anxiety in subjects living with human immunodeficiency virus[145], people with cancer[146], such as survivors of lung cancer[147] and patients with breast cancer[148], patients with systemic disease, like rheumatoid arthritis[149,150], and patients with neurologic disorders, such as PD[100]. Yoga exercises have also been suggested as a promising stress-relieving approach in pregnant women[151,152], in women receiving treatment for infertility[153], and in women who are trying to quit smoking[154,155].
Yoga and depression: Depression is the most common psychiatric disorder that affects 25% of women and 12% of men during their lifetime[156-159]. This disorder is commonly treated by antidepressants and psychotherapy[156,160]. Yoga interventions have been suggested as effective adjuvant therapy[161,162] as well as monotherapy[163] for depression.
A narrative review on the efficacy of yoga and mindfulness as an adjuvant treatment in severe mental illnesses including major depressive disorder (MDD) indicated that both yoga and mindfulness have significant and beneficial effects on reducing the severity of depressive symptoms[164]. Yoga practices in combination with the application of conventional antidepressants significantly improved depression symptoms and reduced the remission rate in patients with MDD compared to control patients[165]. A significant decrease in self-reported symptoms of depression after practicing yoga has been observed in individuals aged 18-29 with mild levels of depression[166]. A meta-analysis has shown a more significant reduction in depression compared to psychoeducation[167].
In addition to the improvement of depression, yoga interventions promote mental health and quality of life and interrupt negative thinking in patients with depression[168,169]. A meta-analysis of 10 studies has shown that yoga practices have a statistically significant effect as an adjunct treatment in patients with MDD[162]. In an investigation of hospitalized patients with severe MDD, the effect of yoga intervention was equivalent to treatment with a tricyclic antidepressant[170]. It has been suggested that yoga modulates cortical inhibition via the regulation of the GABAergic system and exerts beneficial effects in MDD[171]. Furthermore, increased GABA-mediated neurotransmitter activity induced by transcranial magnetic stimulation, and multiple yoga therapy sessions was associated with a significant improvement of depression symptoms in patients with MDD[172]. Enhancement of thalamic GABA values has also been suggested as a potential mechanism for the improvement of mood in patients with MDD[173]. Enhancement of serum neurotrophic factors, such as brain-derived neurotrophic factor, in patients with MDD who practiced yoga, pointed to the possible role of increased neuroplasticity in the improvement of depression symptoms[174]. Yoga practices in post-menopausal women resulted in reduced values of follicle-stimulating hormone and luteinizing hormone, which was associated with decreased stress levels and depression symptoms as well as improved quality of life[175]. Yoga practices in association with coherent breathing intervention have been shown to resolve suicidal ideation in patients with MDD[9,176].
Yoga and bipolar affective disorder: Bipolar affective disorder (BD) is a chronic illness with recurrent episodes of manic or depressive symptoms[177,178]. Although most patients with BD are free of symptoms during remission, many of them continue to experience mild symptoms and suffer from functional behavior impairments[177,179]. Studies on the role of yoga in the treatment of BD are scarce. However, some studies have recommended yoga as a specific self-management strategy for BD[5,180]. Patients with BD have shown a significant alleviation of depression and anxiety symptoms, reduction in difficulties with emotion regulation, and improvement of mindfulness skills during the remission phase following several weeks of yoga practices[181]. Yoga interventions have been suggested to decrease negative emotions in patients with BD[182]. Yoga has also been suggested as an adjuvant therapy that improves residual depression symptoms[183] as well as manic symptom severity[184] of patients with BD. An extensive multicenter, randomized controlled study on 160 adults with BD has shown that mindfulness-based cognitive therapy, including yoga practices, improves the severity of manic symptoms and anxiety, promotes mental health and overall functioning, and reduces relapse rates[185].
Yoga and schizophrenia: Schizophrenia (SZ) is a severe mental disorder, which often exhibits itself by positive symptoms, including hallucinatory experiences and delusional beliefs and negative symptoms, such as lack of motivation and social contacts as well as the absence of spontaneous speech and affective flattening[186-188]. A growing body of evidence suggests that yoga training as an add-on therapy could improve both the negative and positive symptoms and promote cognitive functions and emotional recognition of SZ[189-194].
The analysis of yoga intervention effects on the mood of 113 patients with psychosis has revealed significant improvements in tension-anxiety, depression, anger, fatigue, and confusion[195]. Another study on 66 antipsychotic-stabilized patients with SZ has revealed a significant improvement in positive and negative symptoms, socio-occupational functioning, and performance following yoga training[190]. A meta-analysis of 13 investigations with 1159 patients revealed the importance of the frequency of yoga interventions with an improvement of positive symptoms as well as the duration of each session with the alleviation of negative symptoms in patients with SZ[196]. Yoga practices in the patients with SZ who were taking antipsychotic medications and were in a stable condition significantly decreased drug-induced parkinsonian symptoms and improved executive functions and negative symptoms[192]. Long-term yoga intervention in patients with SZ resulted in greater social and occupational functioning and promoted the quality of life[197]. Yoga training in patients with SZ resulted in an improvement of negative and positive symptoms associated with a reduction of paranoid beliefs and promoting quality of life[198]. Yoga as an add-on treatment has shown a greater improvement of the negative symptoms of SZ in comparison to physical exercise therapy[197]. Furthermore, yoga therapy led to a significant reduction in burden scores and an improvement in the quality of life among patients with psychosis[199]. Yoga intervention in patients with SZ significantly improved cognitive dysfunction, presumably through the correction of autonomic dysfunction[200,201].
It has been suggested that yoga may improve SZ symptoms by strengthening the synaptic network of the lateral and medial prefrontal areas and augmentation of the premotor and parietal mirror neuron circuitry[202]. Oxytocin values increased significantly following yoga practice[203]; an effect that has been suggested to play a potential role in the improvement of social cognition after yoga intervention in patients with SZ[204]. Yoga practice in patients with SZ was also associated with a significant decrease in blood cortisol levels, suggesting a beneficial effect of yoga in the reduction of sociophysical stress of patients[204].
Yoga and other psychological disorders: Several other studies indicate the potential beneficial effects of yoga practices on other psychological disorders and syndromes, such as obsessive-compulsive disorder (OCD), burnout, somatoform disorders, and hypochondriasis[205]. The treatment of OCD with yoga together with the pharmacological interventions improved the obsessive thoughts and compulsive behavior of patients with OCD[206,207]. Furthermore, several clinical trials have suggested the promise of yoga intervention as an adjunct therapy for patients with OCD, who were unresponsive to conventional treatments[208,209]. Moreover, yoga training enhanced general satisfaction, improved work exhaustion, and led to greater work engagement and empathy among teachers[210], nurses[211], hospice professionals[212], and physicians[213,214], who were suffering from job burnout. Yoga can promote the psychological and physical well-being of subjects with burnout, particularly when combining it with other activities, such as art and music-therapy[215,216]. Further
While yoga practice may exert various physical and psychological health benefits, there are some reports on its adverse effects. Intensive yoga training may lead to altered perceptions and beliefs in possessing supernatural powers. However, these psychological alterations can be interpreted as a part of spiritual enlightenment in Eastern meditative culture[220]. Furthermore, yoga training may transiently increase the intraocular pressure and lead to progressive optic neuropathy, particularly in patients with glaucoma[109]. The musculoskeletal complications, including back, shoulder, or neck pain, osteoarthritis, joint injuries and dislocations, fractures, disc herniation, and tendon deformities have been reported as a common adverse effects of yoga practice[221-223]. However, the frequency of severe injuries associated with yoga is low (less than 5%), and both acute and chronic injuries recover fully[224,225]. Moreover, there are several reports of peripheral nerve injuries after a yoga practice, particularly in the elderly subjects who take sedative medications and patients with hypermobility of the connective tissue[104-106].
Most scientific publications on yoga deal with the efficacy of said programs to gain an understanding of the subject to counsel patients appropriately. However, the usefulness of meditation specifically for clinicians, as an occupation group that is particularly associated with physical and mental health risks, still needs more accurate evidence. Although most investigations are in favor of the beneficial effects of yoga on neuropsychological disorders, some studies have not found this meditative procedure useful.
Several points in the studies that have shown the beneficial impacts of yoga on neuropsychological disorders have to be taken into consideration. Multiple investigations reporting beneficial effects of yoga on neuropsychological disorders were not precise in design, implementation, and analysis. There was considerable heterogeneity among the description of yoga interventions in different studies. Different yoga types and many disciplines within the practice have been conducted with various duration and frequency of training. Differences in yoga approaches and the use of different outcome measurements may explain why the outcome of yoga interventions often differed in patients with a common pathological circumstance.
Furthermore, many of these studies have several limitations, such as small sample sizes, short-term follow-up, confounding variables, and lack of appropriate controls. Heterogeneity of intervention procedures and poor qualities of the original investigations substantially influence the value of the meta-analyses that evaluated the effects of yoga on various disorders. Several studies evaluated the underlying mechanism of action of yoga on neuropsychological disorders. However, the exact mechanisms remain to be further elucidated.
Although yoga is a complex approach and difficult to standardize, it is crucial to distinctly describe the intervention procedures, both conceptually and operationally, and avoid excessive heterogeneity[226,227] to consider them as an integrative method in treatment plans for neuropsychological disorders[228]. Furthermore, accurate selection of populations and controls is of great importance to evaluate the potential benefit of yoga on patients with neuropsychological diseases.
| 1. | Erwin Wells R, Phillips RS, McCarthy EP. Patterns of mind-body therapies in adults with common neurological conditions. Neuroepidemiology. 2011;36:46-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Mooventhan A, Nivethitha L. Evidence based effects of yoga in neurological disorders. J Clin Neurosci. 2017;43:61-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (1)] |
| 3. | Wells RE, Baute V, Wahbeh H. Complementary and Integrative Medicine for Neurologic Conditions. Med Clin North Am. 2017;101:881-893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Jeter PE, Slutsky J, Singh N, Khalsa SB. Yoga as a Therapeutic Intervention: A Bibliometric Analysis of Published Research Studies from 1967 to 2013. J Altern Complement Med. 2015;21:586-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 116] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 5. | Meyer HB, Katsman A, Sones AC, Auerbach DE, Ames D, Rubin RT. Yoga as an ancillary treatment for neurological and psychiatric disorders: a review. J Neuropsychiatry Clin Neurosci. 2012;24:152-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (1)] |
| 6. | Wahbeh H, Elsas SM, Oken BS. Mind-body interventions: applications in neurology. Neurology. 2008;70:2321-2328. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 202] [Cited by in RCA: 160] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 7. | Bryant EF. The Yoga Sūtras of Patañjali: A New Edition, Translation, and Commentary with Insights From the Traditional Commentators. North Point Press, 2009. |
| 9. | Nyer M, Nauphal M, Roberg R, Streeter C. Applications of Yoga in Psychiatry: What We Know. Focus (Am Psychiatr Publ). 2018;16:12-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 10. | Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: United States, 2002-2012. Natl Health Stat Report. 2015;1-16. [PubMed] |
| 11. | Balasubramaniam M, Telles S, Doraiswamy PM. Yoga on our minds: a systematic review of yoga for neuropsychiatric disorders. Front Psychiatry. 2012;3:117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 110] [Cited by in RCA: 123] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 12. | Bellissimo G, Leslie E, Maestas V, Zuhl M. The Effects of Fast and Slow Yoga Breathing on Cerebral and Central Hemodynamics. Int J Yoga. 2020;13:207-212. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Sharma K, Pannu V, Sayal N, Bhalla A, Anand A. Effects of one month of Common Yoga Protocol practice appear to be mediated by the angiogenic and neurogenic pathway: A pilot study. Explore (NY). 2021;17:451-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Mehta UM, Gangadhar BN. Yoga: Balancing the excitation-inhibition equilibrium in psychiatric disorders. Prog Brain Res. 2019;244:387-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Cahn BR, Goodman MS, Peterson CT, Maturi R, Mills PJ. Yoga, Meditation and Mind-Body Health: Increased BDNF, Cortisol Awakening Response, and Altered Inflammatory Marker Expression after a 3-Month Yoga and Meditation Retreat. Front Hum Neurosci. 2017;11:315. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 110] [Cited by in RCA: 133] [Article Influence: 14.8] [Reference Citation Analysis (2)] |
| 16. | Hassan A, Robinson M, Willerth SM. Modeling the Effects of Yoga on the Progression of Alzheimer's Disease in a Dish. Cells Tissues Organs. 2018;206:263-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Brunner D, Abramovitch A, Etherton J. A yoga program for cognitive enhancement. PLoS One. 2017;12:e0182366. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 18. | Gothe NP, Hayes JM, Temali C, Damoiseaux JS. Differences in Brain Structure and Function Among Yoga Practitioners and Controls. Front Integr Neurosci. 2018;12:26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 19. | Desai R, Tailor A, Bhatt T. Effects of yoga on brain waves and structural activation: A review. Complement Ther Clin Pract. 2015;21:112-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 20. | Pickut BA, Van Hecke W, Kerckhofs E, Mariën P, Vanneste S, Cras P, Parizel PM. Mindfulness based intervention in Parkinson's disease leads to structural brain changes on MRI: a randomized controlled longitudinal trial. Clin Neurol Neurosurg. 2013;115:2419-2425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 99] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 21. | DeFelipe J, Conley M, Jones EG. Long-range focal collateralization of axons arising from corticocortical cells in monkey sensory-motor cortex. J Neurosci. 1986;6:3749-3766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 146] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 22. | Schieber MH, Hibbard LS. How somatotopic is the motor cortex hand area? Science. 1993;261:489-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 288] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 23. | Beart PM. Yoga and GABA: New Insights from the Science. World J Yoga. 2020;2. |
| 24. | Streeter CC, Whitfield TH, Owen L, Rein T, Karri SK, Yakhkind A, Perlmutter R, Prescot A, Renshaw PF, Ciraulo DA, Jensen JE. Effects of yoga versus walking on mood, anxiety, and brain GABA levels: a randomized controlled MRS study. J Altern Complement Med. 2010;16:1145-1152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 257] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 25. | Newberg AB, Iversen J. The neural basis of the complex mental task of meditation: neurotransmitter and neurochemical considerations. Med Hypotheses. 2003;61:282-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 175] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 26. | Cornwall J, Phillipson OT. Mediodorsal and reticular thalamic nuclei receive collateral axons from prefrontal cortex and laterodorsal tegmental nucleus in the rat. Neurosci Lett. 1988;88:121-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 27. | Destexhe A, Contreras D, Steriade M. Mechanisms underlying the synchronizing action of corticothalamic feedback through inhibition of thalamic relay cells. J Neurophysiol. 1998;79:999-1016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 245] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 28. | Streeter CC, Jensen JE, Perlmutter RM, Cabral HJ, Tian H, Terhune DB, Ciraulo DA, Renshaw PF. Yoga Asana sessions increase brain GABA levels: a pilot study. J Altern Complement Med. 2007;13:419-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 147] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 29. | Kjaer TW, Bertelsen C, Piccini P, Brooks D, Alving J, Lou HC. Increased dopamine tone during meditation-induced change of consciousness. Brain Res Cogn Brain Res. 2002;13:255-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 199] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 30. | Krishnakumar D, Hamblin MR, Lakshmanan S. Meditation and Yoga can Modulate Brain Mechanisms that affect Behavior and Anxiety-A Modern Scientific Perspective. Anc Sci. 2015;2:13-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 31. | Walton KG, Pugh ND, Gelderloos P, Macrae P. Stress reduction and preventing hypertension: preliminary support for a psychoneuroendocrine mechanism. J Altern Complement Med. 1995;1:263-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 86] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 32. | Curiati JA, Bocchi E, Freire JO, Arantes AC, Braga M, Garcia Y, Guimarães G, Fo WJ. Meditation reduces sympathetic activation and improves the quality of life in elderly patients with optimally treated heart failure: a prospective randomized study. J Altern Complement Med. 2005;11:465-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 73] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 33. | Aftanas L, Golosheykin S. Impact of regular meditation practice on EEG activity at rest and during evoked negative emotions. Int J Neurosci. 2005;115:893-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 99] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 34. | Klimesch W, Schimke H, Pfurtscheller G. Alpha frequency, cognitive load and memory performance. Brain Topogr. 1993;5:241-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 323] [Cited by in RCA: 307] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 35. | Palva S, Palva JM. New vistas for alpha-frequency band oscillations. Trends Neurosci. 2007;30:150-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 898] [Cited by in RCA: 993] [Article Influence: 52.3] [Reference Citation Analysis (0)] |
| 36. | Cahn BR, Polich J. Meditation states and traits: EEG, ERP, and neuroimaging studies. Psychol Bull. 2006;132:180-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 891] [Cited by in RCA: 773] [Article Influence: 38.7] [Reference Citation Analysis (0)] |
| 37. | Ajjimaporn A, Rachiwong S, Siripornpanich V. Effects of 8 weeks of modified hatha yoga training on resting-state brain activity and the p300 ERP in patients with physical disability-related stress. J Phys Ther Sci. 2018;30:1187-1192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 38. | Teplan M. Fundamentals of EEG measurement. Measure Sci Rev. 2002;2:1-11. |
| 39. | Bhatia M, Kumar A, Kumar N, Pandey RM, Kochupillai V; EEG study; BAER study; P300 study. Electrophysiologic evaluation of Sudarshan Kriya: an EEG, BAER, P300 study. Indian J Physiol Pharmacol. 2003;47:157-163. [PubMed] |
| 40. | Fernández T, Harmony T, Rodríguez M, Bernal J, Silva J, Reyes A, Marosi E. EEG activation patterns during the performance of tasks involving different components of mental calculation. Electroencephalogr Clin Neurophysiol. 1995;94:175-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 113] [Article Influence: 3.6] [Reference Citation Analysis (3)] |
| 41. | Inanaga K. Frontal midline theta rhythm and mental activity. Psychiatry Clin Neurosci. 1998;52:555-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 70] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 42. | Gothe NP, Khan I, Hayes J, Erlenbach E, Damoiseaux JS. Yoga Effects on Brain Health: A Systematic Review of the Current Literature. Brain Plast. 2019;5:105-122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 102] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 43. | Hernández SE, Suero J, Barros A, González-Mora JL, Rubia K. Increased Grey Matter Associated with Long-Term Sahaja Yoga Meditation: A Voxel-Based Morphometry Study. PLoS One. 2016;11:e0150757. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 55] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 44. | Afonso RF, Balardin JB, Lazar S, Sato JR, Igarashi N, Santaella DF, Lacerda SS, Amaro E Jr, Kozasa EH. Greater Cortical Thickness in Elderly Female Yoga Practitioners-A Cross-Sectional Study. Front Aging Neurosci. 2017;9:201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 45. | Gotink RA, Vernooij MW, Ikram MA, Niessen WJ, Krestin GP, Hofman A, Tiemeier H, Hunink MGM. Meditation and yoga practice are associated with smaller right amygdala volume: the Rotterdam study. Brain Imaging Behav. 2018;12:1631-1639. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 46. | Halappa NG. Prevention of Chronic Migraine Attacks with Acupuncture and Vamana Dhauti (Yogic Therapeutic Self-Induced Emesis) Interventions. Int J Yoga. 2019;12:84-88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 47. | Kaushik M, Jain A, Agarwal P, Joshi SD, Parvez S. Role of Yoga and Meditation as Complimentary Therapeutic Regime for Stress-Related Neuropsychiatric Disorders: Utilization of Brain Waves Activity as Novel Tool. J Evid Based Integr Med. 2020;25:2515690X20949451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 48. | Anheyer D, Leach MJ, Klose P, Dobos G, Cramer H. Mindfulness-based stress reduction for treating chronic headache: A systematic review and meta-analysis. Cephalalgia. 2019;39:544-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 49. | Kumar A, Bhatia R, Sharma G, Dhanlika D, Vishnubhatla S, Singh RK, Dash D, Tripathi M, Srivastava MVP. Effect of yoga as add-on therapy in migraine (CONTAIN): A randomized clinical trial. Neurology. 2020;94:e2203-e2212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 50. | Wells RE, Burch R, Paulsen RH, Wayne PM, Houle TT, Loder E. Meditation for migraines: a pilot randomized controlled trial. Headache. 2014;54:1484-1495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 117] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 51. | Sharma N, Singhal S, Singh A, Sharma C. Effectiveness of integrated yoga therapy in treatment of chronic migraine: randomized controlled trial. J Headache Pain. 2013;14:1. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 52. | Latha D, Kaliappan KV. Efficacy of yoga therapy in the management of headaches. J Indian Psychol. 1992;10:1-2. |
| 53. | Lauritsen CG, Chua AL, Nahas SJ. Current Treatment Options: Headache Related to Menopause-Diagnosis and Management. Curr Treat Options Neurol. 2018;20:7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 54. | Naji-Esfahani H, Zamani M, Marandi SM, Shaygannejad V, Javanmard SH. Preventive Effects of a Three-month Yoga Intervention on Endothelial Function in Patients with Migraine. Int J Prev Med. 2014;5:424-429. [PubMed] |
| 55. | Jurisic P, Salm DC, Vieira C, Cidral-Filho FJ, Mazzardo-Martins L, Martins DF. Pain-related encephalic regions influenced by yoga meditation: An integrative review. Complement Ther Clin Pract. 2018;31:320-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 56. | Dabhade AM, Pawar BH, Ghunage MS, Ghunage VM. Effect of pranayama (breathing exercise) on arrhythmias in the human heart. Explore (NY). 2012;8:12-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 57. | Murugesan R, Govindarajulu N, Bera TK. Effect of selected yogic practices on the management of hypertension. Indian J Physiol Pharmacol. 2000;44:207-210. [PubMed] |
| 58. | Kovac S, Speckmann EJ, Gorji A. Uncensored EEG: The role of DC potentials in neurobiology of the brain. Prog Neurobiol. 2018;165-167:51-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 59. | Wells RE, Beuthin J, Granetzke L. Complementary and Integrative Medicine for Episodic Migraine: an Update of Evidence from the Last 3 Years. Curr Pain Headache Rep. 2019;23:10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 60. | MacLeod R, Hillert EK, Cameron RT, Baillie GS. The role and therapeutic targeting of α-, β- and γ-secretase in Alzheimer's disease. Future Sci OA. 2015;1:FSO11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 78] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 61. | Hüttenrauch M, Lopez-Noguerola JS, Castro-Obregón S. Connecting Mind-Body Therapy-Mediated Effects to Pathological Features of Alzheimer's Disease. J Alzheimers Dis. 2021;82:S65-S90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 62. | Hishikawa N, Takahashi Y, Fukui Y, Tokuchi R, Furusawa J, Takemoto M, Sato K, Yamashita T, Ohta Y, Abe K. Yoga-plus exercise mix promotes cognitive, affective, and physical functions in elderly people. Neurol Res. 2019;41:1001-1007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 63. | Luders E, Cherbuin N, Kurth F. Forever Young(er): potential age-defying effects of long-term meditation on gray matter atrophy. Front Psychol. 2014;5:1551. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 64. | Wells RE, Yeh GY, Kerr CE, Wolkin J, Davis RB, Tan Y, Spaeth R, Wall RB, Walsh J, Kaptchuk TJ, Press D, Phillips RS, Kong J. Meditation's impact on default mode network and hippocampus in mild cognitive impairment: a pilot study. Neurosci Lett. 2013;556:15-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 124] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 65. | Larouche E, Hudon C, Goulet S. Potential benefits of mindfulness-based interventions in mild cognitive impairment and Alzheimer's disease: an interdisciplinary perspective. Behav Brain Res. 2015;276:199-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 66. | Farhang M, Miranda-Castillo C, Rubio M, Furtado G. Impact of mind-body interventions in older adults with mild cognitive impairment: a systematic review. Int Psychogeriatr. 2019;31:643-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 67. | Fan JT, Chen KM. Using silver yoga exercises to promote physical and mental health of elders with dementia in long-term care facilities. Int Psychogeriatr. 2011;23:1222-1230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 68. | Hassan A, Robinson M, Willerth SM. Determining the mechanism behind yoga’s effects on preventing the symptoms of Alzheimer’s disease. Neural Regen Res. 2020;15:261-262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 69. | Sha K, Palmer MH, Yeo S. Yoga's Biophysiological Effects on Lower Urinary Tract Symptoms: A Scoping Review. J Altern Complement Med. 2019;25:279-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 70. | McCaffrey R, Park J, Newman D, Hagen D. The effect of chair yoga in older adults with moderate and severe Alzheimer's disease. Res Gerontol Nurs. 2014;7:171-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 71. | Naveen GH, Sinha S, Girish N, Taly AB, Varambally S, Gangadhar BN. Yoga and epilepsy: What do patients perceive? Indian J Psychiatry. 2013;55:S390-S393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 72. | Nirwan M, Halder K, Saha M, Pathak A, Balakrishnan R, Ganju L. Improvement in resilience and stress-related blood markers following ten months yoga practice in Antarctica. J Complement Integr Med. 2020;18:201-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 73. | Metaxas A, Anzalone M, Vaitheeswaran R, Petersen S, Landau AM, Finsen B. Neuroinflammation and amyloid-beta 40 are associated with reduced serotonin transporter (SERT) activity in a transgenic model of familial Alzheimer's disease. Alzheimers Res Ther. 2019;11:38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 74. | Harinath K, Malhotra AS, Pal K, Prasad R, Kumar R, Kain TC, Rai L, Sawhney RC. Effects of Hatha yoga and Omkar meditation on cardiorespiratory performance, psychologic profile, and melatonin secretion. J Altern Complement Med. 2004;10:261-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 148] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 75. | Liu YC, Hsu WL, Ma YL, Lee EHY. Melatonin Induction of APP Intracellular Domain 50 SUMOylation Alleviates AD through Enhanced Transcriptional Activation and Aβ Degradation. Mol Ther. 2021;29:376-395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 76. | Wang P, Sui HJ, Li XJ, Bai LN, Bi J, Lai H. Melatonin ameliorates microvessel abnormalities in the cerebral cortex and hippocampus in a rat model of Alzheimer's disease. Neural Regen Res. 2021;16:757-764. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 77. | Dahl J, Melin L, Lund L. Effects of a contingent relaxation treatment program on adults with refractory epileptic seizures. Epilepsia. 1987;28:125-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 57] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 78. | Santesso N. A Summary of a Cochrane Review: Yoga for epilepsy. Eur J Integr Med. 2015;7:593-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 79. | Panjwani U, Selvamurthy W, Singh SH, Gupta HL, Thakur L, Rai UC. Effect of Sahaja yoga practice on seizure control & EEG changes in patients of epilepsy. Indian J Med Res. 1996;103:165-172. [PubMed] |
| 80. | Kanhere SV, Bagadia DR, Phadke VD, Mukherjee PS. Yoga in Children with Epilepsy: A Randomized Controlled Trial. J Pediatr Neurosci. 2018;13:410-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 81. | Lundgren T, Dahl J, Yardi N, Melin L. Acceptance and Commitment Therapy and yoga for drug-refractory epilepsy: a randomized controlled trial. Epilepsy Behav. 2008;13:102-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 141] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 82. | Panebianco M, Sridharan K, Ramaratnam S. Yoga for epilepsy. Cochrane Database Syst Rev. 2017;10:CD001524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 83. | Thakur P, Mohammad A, Rastogi YR, Saini RV, Saini AK. Yoga as an intervention to manage multiple sclerosis symptoms. J Ayurveda Integr Med. 2020;11:114-117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 84. | Kahraman T, Ozdogar AT, Yigit P, Hosgel I, Mehdiyev Z, Ertekin O, Ozakbas S. Feasibility of a 6-Month Yoga Program to Improve the Physical and Psychosocial Status of Persons with Multiple Sclerosis and their Family Members. Explore (NY). 2018;14:36-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 85. | de Oliveira G, Tavares Mda C, de Faria Oliveira JD, Rodrigues MR, Santaella DF. Yoga Training Has Positive Effects on Postural Balance and Its Influence on Activities of Daily Living in People with Multiple Sclerosis: A Pilot Study. Explore (NY). 2016;12:325-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 86. | Salgado BC, Jones M, Ilgun S, McCord G, Loper-Powers M, van Houten P. Effects of a 4-month Ananda Yoga program on physical and mental health outcomes for persons with multiple sclerosis. Int J Yoga Therap. 2013;27-38. [PubMed] |
| 87. | Najafidoulatabad S, Mohebbi Z, Nooryan K. Yoga effects on physical activity and sexual satisfaction among the Iranian women with multiple sclerosis: a randomized controlled trial. Afr J Tradit Complement Altern Med. 2014;11:78-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 88. | Patil NJ, Nagaratna R, Garner C, Raghuram NV, Crisan R. Effect of integrated Yoga on neurogenic bladder dysfunction in patients with multiple sclerosis-A prospective observational case series. Complement Ther Med. 2012;20:424-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 89. | Powell L, Cheshire A. An Individualized Yoga Programme for Multiple Sclerosis: A Case Study. Int J Yoga Therap. 2015;25:127-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 90. | Guner S, Inanici F. Yoga therapy and ambulatory multiple sclerosis Assessment of gait analysis parameters, fatigue and balance. J Bodyw Mov Ther. 2015;19:72-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 91. | Shohani M, Kazemi F, Rahmati S, Azami M. The effect of yoga on the quality of life and fatigue in patients with multiple sclerosis: A systematic review and meta-analysis of randomized clinical trials. Complement Ther Clin Pract. 2020;39:101087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 92. | Deuel LM, Seeberger LC. Complementary Therapies in Parkinson Disease: a Review of Acupuncture, Tai Chi, Qi Gong, Yoga, and Cannabis. Neurotherapeutics. 2020;17:1434-1455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 72] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 93. | Donley S, McGregor S, Wielinski C, Nance M. Use and perceived effectiveness of complementary therapies in Parkinson's disease. Parkinsonism Relat Disord. 2019;58:46-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 94. | Kwok JYY, Kwan JCY, Auyeung M, Mok VCT, Chan HYL. The effects of yoga versus stretching and resistance training exercises on psychological distress for people with mild-to-moderate Parkinson's disease: study prxotocol for a randomized controlled trial. Trials. 2017;18:509. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 95. | Moriello G, Denio C, Abraham M, DeFrancesco D, Townsley J. Incorporating yoga into an intense physical therapy program in someone with Parkinson's disease: a case report. J Bodyw Mov Ther. 2013;17:408-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 96. | Cherup NP, Strand KL, Lucchi L, Wooten SV, Luca C, Signorile JF. Yoga Meditation Enhances Proprioception and Balance in Individuals Diagnosed With Parkinson's Disease. Percept Mot Skills. 2021;128:304-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 97. | Swink LA, Fling BW, Sharp JL, Fruhauf CA, Atler KE, Schmid AA. Merging Yoga and Occupational Therapy for Parkinson's Disease: A Feasibility and Pilot Program. Occup Ther Health Care. 2020;34:351-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 98. | Myers PS, Harrison EC, Rawson KS, Horin AP, Sutter EN, McNeely ME, Earhart GM. Yoga Improves Balance and Low-Back Pain, but Not Anxiety, in People with Parkinson's Disease. Int J Yoga Therap. 2020;30:41-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 99. | Slomski A. Yoga for Anxiety and Depression Associated With Parkinson Disease. JAMA. 2019;322:296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 100. | Kwok JYY, Kwan JCY, Auyeung M, Mok VCT, Lau CKY, Choi KC, Chan HYL. Effects of Mindfulness Yoga vs Stretching and Resistance Training Exercises on Anxiety and Depression for People With Parkinson Disease: A Randomized Clinical Trial. JAMA Neurol. 2019;76:755-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 244] [Article Influence: 40.7] [Reference Citation Analysis (0)] |
| 101. | Sagarwala R, Nasrallah HA. The effects of yoga on depression and motor function in patients with Parkinson's disease: A review of controlled studies. Ann Clin Psychiatry. 2020;32:209-215. [PubMed] |
| 102. | Streckmann F, Zopf EM, Lehmann HC, May K, Rizza J, Zimmer P, Gollhofer A, Bloch W, Baumann FT. Exercise intervention studies in patients with peripheral neuropathy: a systematic review. Sports Med. 2014;44:1289-1304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 131] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 103. | Martyn CN, Hughes RA. Epidemiology of peripheral neuropathy. J Neurol Neurosurg Psychiatry. 1997;62:310-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 375] [Cited by in RCA: 388] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 104. | Baute V, Zelnik D, Curtis J, Sadeghifar F. Complementary and Alternative Medicine for Painful Peripheral Neuropathy. Curr Treat Options Neurol. 2019;21:44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 105. | Staudt MD, Prabhala T, Sheldon BL, Quaranta N, Zakher M, Bhullar R, Pilitsis JG, Argoff CE. Current Strategies for the Management of Painful Diabetic Neuropathy. J Diabetes Sci Technol. 2020;1932296820951829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 106. | Walker M, Meekins G, Hu SC. Yoga neuropathy. A snoozer. Neurologist. 2005;11:176-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 107. | Hussain N, Said ASA. Mindfulness-Based Meditation Versus Progressive Relaxation Meditation: Impact on Chronic Pain in Older Female Patients With Diabetic Neuropathy. J Evid Based Integr Med. 2019;24:2515690X19876599. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 108. | Van Puymbroeck M, Atler K, Portz JD, Schmid AA. Multidimensional Improvements in Health Following Hatha Yoga for Individuals with Diabetic Peripheral Neuropathy. Int J Yoga Therap. 2018;28:71-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 109. | de Barros DS, Bazzaz S, Gheith ME, Siam GA, Moster MR. Progressive optic neuropathy in congenital glaucoma associated with the Sirsasana yoga posture. Ophthalmic Surg Lasers Imaging. 2008;39:339-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 110. | Dacci P, Amadio S, Gerevini S, Moiola L, Del Carro U, Radaelli M, Figlia G, Martinelli V, Comi G, Fazio R. Practice of yoga may cause damage of both sciatic nerves: a case report. Neurol Sci. 2013;34:393-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 111. | Horner L, Edelsohn L, Gakhal M. Yoga induced acute ulnar nerve compression by a ganglion cyst in Guyon's canal. Del Med J. 2013;85:369-373. [PubMed] |
| 113. | Plewnia C, Wallace C, Zochodne D. Traumatic sciatic neuropathy: a novel cause, local experience, and a review of the literature. J Trauma. 1999;47:986-991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 114. | Garfinkel MS, Singhal A, Katz WA, Allan DA, Reshetar R, Schumacher HR Jr. Yoga-based intervention for carpal tunnel syndrome: a randomized trial. JAMA. 1998;280:1601-1603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 164] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 115. | Moraska A, Chandler C, Edmiston-Schaetzel A, Franklin G, Calenda EL, Enebo B. Comparison of a targeted and general massage protocol on strength, function, and symptoms associated with carpal tunnel syndrome: a randomized pilot study. J Altern Complement Med. 2008;14:259-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 116. | Malhotra V, Singh S, Tandon OP, Madhu SV, Prasad A, Sharma SB. Effect of Yoga asanas on nerve conduction in type 2 diabetes. Indian J Physiol Pharmacol. 2002;46:298-306. [PubMed] |
| 117. | Head KA. Peripheral neuropathy: pathogenic mechanisms and alternative therapies. Altern Med Rev. 2006;11:294-329. [PubMed] |
| 118. | Speck RM, DeMichele A, Farrar JT, Hennessy S, Mao JJ, Stineman MG, Barg FK. Scope of symptoms and self-management strategies for chemotherapy-induced peripheral neuropathy in breast cancer patients. Support Care Cancer. 2012;20:2433-2439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 61] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 119. | Bao T, Zhi I, Baser R, Hooper M, Chen C, Piulson L, Li QS, Galantino ML, Blinder V, Robson M, Seidman A, Panageas KS, Mao JJ. Yoga for Chemotherapy-Induced Peripheral Neuropathy and Fall Risk: A Randomized Controlled Trial. JNCI Cancer Spectr. 2020;4:pkaa048. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 120. | Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. 2015;17:327-335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 743] [Cited by in RCA: 1113] [Article Influence: 111.3] [Reference Citation Analysis (0)] |
| 121. | Worthen M, Cash E. Stress Management. 2020 Aug 29. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. [PubMed] |
| 122. | Davis K, Goodman SH, Leiferman J, Taylor M, Dimidjian S. A randomized controlled trial of yoga for pregnant women with symptoms of depression and anxiety. Complement Ther Clin Pract. 2015;21:166-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 76] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 123. | Tiwari N, Sutton M, Garner M, Baldwin DS. Yogic Breathing Instruction in Patients with Treatment-Resistant Generalized Anxiety Disorder: Pilot Study. Int J Yoga. 2019;12:78-83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 124. | Li AW, Goldsmith CA. The effects of yoga on anxiety and stress. Altern Med Rev. 2012;17:21-35. [PubMed] |
| 125. | Vorkapic CF, Rangé B. Reducing the symptomatology of panic disorder: the effects of a yoga program alone and in combination with cognitive-behavioral therapy. Front Psychiatry. 2014;5:177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 126. | Weaver LL, Darragh AR. Systematic Review of Yoga Interventions for Anxiety Reduction Among Children and Adolescents. Am J Occup Ther. 2015;69:6906180070p1-6906180070p9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 127. | Saeed SA, Cunningham K, Bloch RM. Depression and Anxiety Disorders: Benefits of Exercise, Yoga, and Meditation. Am Fam Physician. 2019;99:620-627. [PubMed] |
| 128. | Wadden KP, Snow NJ, Sande P, Slawson S, Waller T, Boyd LA. Yoga Practitioners Uniquely Activate the Superior Parietal Lobule and Supramarginal Gyrus During Emotion Regulation. Front Integr Neurosci. 2018;12:60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 129. | Tymofiyeva O, Henje E, Yuan JP, Huang CY, Connolly CG, Ho TC, Bhandari S, Parks KC, Sipes BS, Yang TT, Xu D. Reduced anxiety and changes in amygdala network properties in adolescents with training for awareness, resilience, and action (TARA). Neuroimage Clin. 2021;29:102521. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 130. | Bagga OP, Gandhi A. A comparative study of the effect of Transcendental Meditation (T.M.) and Shavasana practice on cardiovascular system. Indian Heart J. 1983;35:39-45. [PubMed] |
| 131. | Katuri KK, Dasari AB, Kurapati S, Vinnakota NR, Bollepalli AC, Dhulipalla R. Association of yoga practice and serum cortisol levels in chronic periodontitis patients with stress-related anxiety and depression. J Int Soc Prev Community Dent. 2016;6:7-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 132. | Hofmann SG, Andreoli G, Carpenter JK, Curtiss J. Effect of Hatha Yoga on Anxiety: A Meta-Analysis. J Evid Based Med. 2016;9:116-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 133. | Cramer H, Lauche R, Anheyer D, Pilkington K, de Manincor M, Dobos G, Ward L. Yoga for anxiety: A systematic review and meta-analysis of randomized controlled trials. Depress Anxiety. 2018;35:830-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 170] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 134. | Jung YH, Kang DH, Jang JH, Park HY, Byun MS, Kwon SJ, Jang GE, Lee US, An SC, Kwon JS. The effects of mind-body training on stress reduction, positive affect, and plasma catecholamines. Neurosci Lett. 2010;479:138-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 135. | Telles S, Kala N, Gupta RK, Verma S, Vishwakarma B, Agnihotri S, Gandharva K, Balkrishna A. Effect of yoga on vigilance, self rated sleep and state anxiety in Border Security Force personnel in India. Work. 2019;63:243-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 136. | Stueck M, Gloeckner N. Yoga for children in the mirror of the science: Working spectrum and practice fields of the training of relaxation with elements of yoga for children. Early Child Dev Care. 2005;175:371-377. [DOI] [Full Text] |
| 137. | Mendelson T, Greenberg MT, Dariotis JK, Gould LF, Rhoades BL, Leaf PJ. Feasibility and preliminary outcomes of a school-based mindfulness intervention for urban youth. J Abnorm Child Psychol. 2010;38:985-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 204] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 138. | Shreve M, Scott A, McNeill C, Washburn L. Using Yoga to Reduce Anxiety in Children: Exploring School-Based Yoga Among Rural Third- and Fourth-Grade Students. J Pediatr Health Care. 2021;35:42-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 139. | Anusuya US, Mohanty S, Saoji AA. Effect of Mind Sound Resonance Technique (MSRT - A yoga-based relaxation technique) on psychological variables and cognition in school children: A randomized controlled trial. Complement Ther Med. 2021;56:102606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 140. | Telles S, Gupta RK, Gandharva K, Vishwakarma B, Kala N, Balkrishna A. Immediate Effect of a Yoga Breathing Practice on Attention and Anxiety in Pre-Teen Children. Children (Basel). 2019;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 141. | Lemay V, Hoolahan J, Buchanan A. Impact of a Yoga and Meditation Intervention on Students' Stress and Anxiety Levels. Am J Pharm Educ. 2019;83:7001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 95] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 142. | Re P, McConnell JW, Reidinger G, Schweit R, Hendron A. Effects of yoga on patients in an adolescent mental health hospital and the relationship between those effects and the patients' sensory-processing patterns. J Child Adolesc Psychiatr Nurs. 2014;27:175-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 143. | Tejvani R, Metri KG, Agrawal J, Nagendra HR. Effect of Yoga on anxiety, depression and self-esteem in orphanage residents: A pilot study. Ayu. 2016;37:22-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 144. | Bergen-Cico D, Possemato K, Pigeon W. Reductions in cortisol associated with primary care brief mindfulness program for veterans with PTSD. Med Care. 2014;52:S25-S31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 145. | Jiang T, Hou J, Sun R, Dai L, Wang W, Wu H, Zhang T, Su B. Immunological and Psychological Efficacy of Meditation/Yoga Intervention Among People Living With HIV (PLWH): A Systematic Review and Meta-analyses of 19 Randomized Controlled Trials. Ann Behav Med. 2021;55:505-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 146. | Danhauer SC, Addington EL, Sohl SJ, Chaoul A, Cohen L. Review of yoga therapy during cancer treatment. Support Care Cancer. 2017;25:1357-1372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 69] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 147. | McDonnell KK, Gallerani DG, Newsome BR, Owens OL, Beer J, Myren-Bennett AR, Regan E, Hardin JW, Webb LA. A Prospective Pilot Study Evaluating Feasibility and Preliminary Effects of Breathe Easier: A Mindfulness-based Intervention for Survivors of Lung Cancer and Their Family Members (Dyads). Integr Cancer Ther. 2020;19:1534735420969829. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 148. | Gosain R, Gage-Bouchard E, Ambrosone C, Repasky E, Gandhi S. Stress reduction strategies in breast cancer: review of pharmacologic and non-pharmacologic based strategies. Semin Immunopathol. 2020;42:719-734. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 57] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 149. | Cartwright T, Cahill M, Sadana V. A mixed methods evaluation of an individualised yoga therapy intervention for rheumatoid arthritis: Pilot study. Complement Ther Med. 2020;50:102339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 150. | Chaurasia N, Singh A, Singh IL, Singh T, Tiwari T. Cognitive dysfunction in patients of rheumatoid arthritis. J Family Med Prim Care. 2020;9:2219-2225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 54] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 151. | Guo P, Zhang X, Liu N, Wang J, Chen D, Sun W, Li P, Zhang W. Mind-body interventions on stress management in pregnant women: A systematic review and meta-analysis of randomized controlled trials. J Adv Nurs. 2021;77:125-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 152. | Traylor CS, Johnson JD, Kimmel MC, Manuck TA. Effects of psychological stress on adverse pregnancy outcomes and nonpharmacologic approaches for reduction: an expert review. Am J Obstet Gynecol MFM. 2020;2:100229. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 136] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 153. | Dumbala S, Bhargav H, Satyanarayana V, Arasappa R, Varambally S, Desai G, Bangalore GN. Effect of Yoga on Psychological Distress among Women Receiving Treatment for Infertility. Int J Yoga. 2020;13:115-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 154. | Bock BC, Fava JL, Gaskins R, Morrow KM, Williams DM, Jennings E, Becker BM, Tremont G, Marcus BH. Yoga as a complementary treatment for smoking cessation in women. J Womens Health (Larchmt). 2012;21:240-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 155. | Uebelacker LA, Broughton MK. Yoga for Depression and Anxiety: A Review of Published Research and Implications for Healthcare Providers. R I Med J (2013). 2016;99:20-22. [PubMed] |
| 156. | Schuver KJ, Lewis BA. Mindfulness-based yoga intervention for women with depression. Complement Ther Med. 2016;26:85-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 157. | Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS; National Comorbidity Survey Replication. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289:3095-3105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5389] [Cited by in RCA: 5447] [Article Influence: 236.8] [Reference Citation Analysis (0)] |
| 158. | Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370:851-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2533] [Cited by in RCA: 2687] [Article Influence: 141.4] [Reference Citation Analysis (0)] |
| 159. | Rubio JM, Markowitz JC, Alegría A, Pérez-Fuentes G, Liu SM, Lin KH, Blanco C. Epidemiology of chronic and nonchronic major depressive disorder: results from the national epidemiologic survey on alcohol and related conditions. Depress Anxiety. 2011;28:622-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 160. | Kupfer DJ. Long-term treatment of depression. J Clin Psychiatry. 1991;52 Suppl:28-34. [PubMed] |
| 161. | Ravindran AV, Lam RW, Filteau MJ, Lespérance F, Kennedy SH, Parikh SV, Patten SB; Canadian Network for Mood and Anxiety Treatments (CANMAT). Canadian Network for Mood and Anxiety Treatments (CANMAT) Clinical guidelines for the management of major depressive disorder in adults. V. Complementary and alternative medicine treatments. J Affect Disord. 2009;117 Suppl 1:S54-S64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 63] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 162. | Haller H, Anheyer D, Cramer H, Dobos G. Complementary therapies for clinical depression: an overview of systematic reviews. BMJ Open. 2019;9:e028527. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 163. | Devi NA, Varambally S, Karmani S, Christopher R, Gangadhar BN. Yoga as monotherapy for the treatment of major depression - A case series. Asian J Psychiatr. 2020;53:102177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 164. | Sathyanarayanan G, Vengadavaradan A, Bharadwaj B. Role of Yoga and Mindfulness in Severe Mental Illnesses: A Narrative Review. Int J Yoga. 2019;12:3-28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 165. | Sharma VK, Das S, Mondal S, Goswampi U, Gandhi A. Effect of Sahaj Yoga on depressive disorders. Indian J Physiol Pharmacol. 2005;49:462-468. [PubMed] |
| 166. | Woolery A, Myers H, Sternlieb B, Zeltzer L. A yoga intervention for young adults with elevated symptoms of depression. Altern Ther Health Med. 2004;10:60-63. [PubMed] |
| 167. | Vollbehr NK, Bartels-Velthuis AA, Nauta MH, Castelein S, Steenhuis LA, Hoenders HJR, Ostafin BD. Hatha yoga for acute, chronic and/or treatment-resistant mood and anxiety disorders: A systematic review and meta-analysis. PLoS One. 2018;13:e0204925. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 168. | Bressington D, Mui J, Yu C, Leung SF, Cheung K, Wu CST, Bollard M, Chien WT. Feasibility of a group-based laughter yoga intervention as an adjunctive treatment for residual symptoms of depression, anxiety and stress in people with depression. J Affect Disord. 2019;248:42-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 169. | La Rocque CL, Mazurka R, Stuckless TJR, Pyke K, Harkness KL. Randomized controlled trial of bikram yoga and aerobic exercise for depression in women: Efficacy and stress-based mechanisms. J Affect Disord. 2021;280:457-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 170. | Janakiramaiah N, Gangadhar BN, Naga Venkatesha Murthy PJ, Harish MG, Subbakrishna DK, Vedamurthachar A. Antidepressant efficacy of Sudarshan Kriya Yoga (SKY) in melancholia: a randomized comparison with electroconvulsive therapy (ECT) and imipramine. J Affect Disord. 2000;57:255-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 182] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 171. | Jakhar J, Mehta UM, Ektare A, Vidyasagar PD, Varambally S, Thirthalli J, Gangadhar BN. Cortical inhibition in major depression: Investigating the acute effect of single-session yoga versus walking. Brain Stimul. 2019;12:1597-1599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 172. | Bhargav PH, Reddy PV, Govindaraj R, Gulati K, Ravindran A, Gayathri D, Karmani SJ, Udupa K, Venkatasubramanian G, Philip M, Debnath M, Bharath RD, Sathyaprabha TN, Gangadhar BN, Muralidharan Pi K. Impact of a Course of Add-on Supervised Yoga on Cortical Inhibition in Major Depressive Disorder: A Randomized Controlled Trial. Can J Psychiatry. 2021;66:179-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 173. | Streeter CC, Gerbarg PL, Brown RP, Scott TM, Nielsen GH, Owen L, Sakai O, Sneider JT, Nyer MB, Silveri MM. Thalamic Gamma Aminobutyric Acid Level Changes in Major Depressive Disorder After a 12-Week Iyengar Yoga and Coherent Breathing Intervention. J Altern Complement Med. 2020;26:190-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 174. | Tolahunase MR, Sagar R, Faiq M, Dada R. Yoga- and meditation-based lifestyle intervention increases neuroplasticity and reduces severity of major depressive disorder: A randomized controlled trial. Restor Neurol Neurosci. 2018;36:423-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 66] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 175. | Jorge MP, Santaella DF, Pontes IM, Shiramizu VK, Nascimento EB, Cabral A, Lemos TM, Silva RH, Ribeiro AM. Hatha Yoga practice decreases menopause symptoms and improves quality of life: A randomized controlled trial. Complement Ther Med. 2016;26:128-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 176. | Serpa JG, Taylor SL, Tillisch K. Mindfulness-based stress reduction (MBSR) reduces anxiety, depression, and suicidal ideation in veterans. Med Care. 2014;52:S19-S24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 87] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 177. | McCormick U, Murray B, McNew B. Diagnosis and treatment of patients with bipolar disorder: A review for advanced practice nurses. J Am Assoc Nurse Pract. 2015;27:530-542. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 178. | Vieta E, Goikolea JM. Atypical antipsychotics: newer options for mania and maintenance therapy. Bipolar Disord. 2005;7 Suppl 4:21-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 49] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 179. | Miller K. Bipolar disorder: etiology, diagnosis, and management. J Am Acad Nurse Pract. 2006;18:368-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 180. | Murray G, Suto M, Hole R, Hale S, Amari E, Michalak EE. Self-management strategies used by 'high functioning' individuals with bipolar disorder: from research to clinical practice. Clin Psychol Psychother. 2011;18:95-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 81] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 181. | Joshi SS, Sharma MP, Varambally S. Effectiveness of Mindfulness-based Cognitive Therapy in Patients with Bipolar Affective Disorder: A Case Series. Int J Yoga. 2018;11:77-82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 182. | Uebelacker L, Dufour SC, Dinerman JG, Walsh SL, Hearing C, Gillette LT, Deckersbach T, Nierenberg AA, Weinstock L, Sylvia LG. Examining the Feasibility and Acceptability of an Online Yoga Class for Mood Disorders: A MoodNetwork Study. J Psychiatr Pract. 2018;24:60-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 183. | Ravindran AV, McKay MS, Silva TD, Tindall C, Garfinkel T, Paric A, Ravindran L. Breathing-focused Yoga as Augmentation for Unipolar and Bipolar Depression: A Randomized Controlled Trial: Le yoga axé sur la respiration comme traitement d'appoint pour la dépression unipolaire et bipolaire: Un essai randomisé contrôlé. Can J Psychiatry. 2021;66:159-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 184. | Weinstock LM, Broughton MK, Tezanos KM, Tremont G, Gillette T, Uebelacker LA. Adjunctive yoga vs bibliotherapy for bipolar depression: a pilot randomized controlled trial. Ment Health Phys Act. 2016;11:67-73. [DOI] [Full Text] |
| 185. | Hanssen I, Huijbers MJ, Lochmann-van Bennekom MWH, Regeer EJ, Stevens AWMM, Evers SMAA, Wensing M, Kupka RW, Speckens AEM. Study protocol of a multicenter randomized controlled trial of mindfulness-based cognitive therapy and treatment as usual in bipolar disorder. BMC Psychiatry. 2019;19:130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 186. | Cramer H, Lauche R, Klose P, Langhorst J, Dobos G. Yoga for schizophrenia: a systematic review and meta-analysis. BMC Psychiatry. 2013;13:32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 80] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 187. | van Os J, Kapur S. Schizophrenia. Lancet. 2009;374:635-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1529] [Cited by in RCA: 1564] [Article Influence: 92.0] [Reference Citation Analysis (0)] |
| 188. | Association AP. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders-DSM-IV-TR. 4th ed. Washington, DC: American Psychiatric Association, 2000: 2000. |
| 189. | Vancampfort D, Probst M, Helvik Skjaerven L, Catalán-Matamoros D, Lundvik-Gyllensten A, Gómez-Conesa A, Ijntema R, De Hert M. Systematic review of the benefits of physical therapy within a multidisciplinary care approach for people with schizophrenia. Phys Ther. 2012;92:11-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 86] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 190. | Bega D, Gonzalez-Latapi P, Zadikoff C, Simuni T. A review of the clinical evidence for complementary and alternative therapies in Parkinson's disease. Curr Treat Options Neurol. 2014;16:314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 191. | Bhatia T, Gujral S, Sharma V, Kumari N, Wood J, Wesesky MA, Jones J, Davis LW, Iyenger S, Haas GL, Nimgaonkar VL, Deshpande SN. Adjunctive yoga training for persons with schizophrenia: who benefits? Acta Neuropsychiatr. 2021;33:113-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 192. | Verma M, Bhargav H, Varambally S, Raghuram N, Bn G. Effect of integrated yoga on anti-psychotic induced side effects and cognitive functions in patients suffering from schizophrenia. J Complement Integr Med. 2018;16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 193. | Govindaraj R, Naik S, Manjunath NK, Mehta UM, Gangadhar BN, Varambally S. Add-on Yoga Therapy for Social Cognition in Schizophrenia: A Pilot Study. Int J Yoga. 2018;11:242-244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 194. | Govindaraj R, Naik SS, Mehta UM, Sharma M, Varambally S, Gangadhar BN. Yoga therapy for social cognition in schizophrenia: An experimental medicine-based randomized controlled trial. Asian J Psychiatr. 2021;62:102731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 195. | Lavey R, Sherman T, Mueser KT, Osborne DD, Currier M, Wolfe R. The effects of yoga on mood in psychiatric inpatients. Psychiatr Rehabil J. 2005;28:399-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 93] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 196. | Wei GX, Yang L, Imm K, Loprinzi PD, Smith L, Zhang X, Yu Q. Effects of Mind-Body Exercises on Schizophrenia: A Systematic Review With Meta-Analysis. Front Psychiatry. 2020;11:819. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 197. | Duraiswamy G, Thirthalli J, Nagendra HR, Gangadhar BN. Yoga therapy as an add-on treatment in the management of patients with schizophrenia--a randomized controlled trial. Acta Psychiatr Scand. 2007;116:226-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 180] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 198. | Visceglia E, Lewis S. Yoga therapy as an adjunctive treatment for schizophrenia: a randomized, controlled pilot study. J Altern Complement Med. 2011;17:601-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 91] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 199. | Varambally S, Vidyendaran S, Sajjanar M, Thirthalli J, Hamza A, Nagendra HR, Gangadhar BN. Yoga-based intervention for caregivers of outpatients with psychosis: a randomized controlled pilot study. Asian J Psychiatr. 2013;6:141-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 200. | Nielsen BM, Mehlsen J, Behnke K. Altered balance in the autonomic nervous system in schizophrenic patients. Clin Physiol. 1988;8:193-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 201. | Bhatia T, Agarwal A, Shah G, Wood J, Richard J, Gur RE, Gur RC, Nimgaonkar VL, Mazumdar S, Deshpande SN. Adjunctive cognitive remediation for schizophrenia using yoga: an open, non-randomized trial. Acta Neuropsychiatr. 2012;24:91-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 202. | Mehta UM, Keshavan MS, Gangadhar BN. Bridging the schism of schizophrenia through yoga-Review of putative mechanisms. Int Rev Psychiatry. 2016;28:254-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 203. | Jayaram N, Varambally S, Behere RV, Venkatasubramanian G, Arasappa R, Christopher R, Gangadhar BN. Effect of yoga therapy on plasma oxytocin and facial emotion recognition deficits in patients of schizophrenia. Indian J Psychiatry. 2013;55:S409-S413. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 204. | Bangalore NG, Varambally S. Yoga therapy for Schizophrenia. Int J Yoga. 2012;5:85-91. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 205. | Grover P, Varma VK, Verma SK, Pershad D. Relationship between the patient's attitude towards yoga and the treatment outcome. Indian J Psychiatry. 1987;29:253-258. [PubMed] |
| 206. | Mehta K, Mehta S, Chalana H, Singh H, Thaman RG. Effectiveness of Rajyoga meditation as an adjunct to first-line treatment in patients with obsessive compulsive disorder. Indian J Psychiatry. 2020;62:684-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 207. | Bhat S, Varambally S, Karmani S, Govindaraj R, Gangadhar BN. Designing and validation of a yoga-based intervention for obsessive compulsive disorder. Int Rev Psychiatry. 2016;28:327-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 208. | Shannahoff-Khalsa D, Fernandes RY, Pereira CAB, March JS, Leckman JF, Golshan S, Vieira MSR, Polanczyk GV, Miguel EC, Shavitt RG. Kundalini Yoga Meditation Versus the Relaxation Response Meditation for Treating Adults With Obsessive-Compulsive Disorder: A Randomized Clinical Trial. Front Psychiatry. 2019;10:793. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 209. | Shannahoff-Khalsa DS, Beckett LR. Clinical case report: efficacy of yogic techniques in the treatment of obsessive compulsive disorders. Int J Neurosci. 1996;85:1-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 210. | Dike IC, Onyishi CN, Adimora DE, Ugodulunwa CA, Adama GN, Ugwu GC, Eze UN, Eze A, Ogba FN, Obiwluozo PE, Onu JC, Onu AO, Omenma ZO, Nwaeze VC, Ani C, Ngwu CN, Uzodinma UE, Iremeka FU. Yoga complemented cognitive behavioral therapy on job burnout among teachers of children with autism spectrum disorders. Medicine (Baltimore). 2021;100:e25801. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 211. | Kavurmaci M, Tan M, Bahcecioglu Turan G. Determining the effect of yoga on job satisfaction and burnout of nurse academicians. Perspect Psychiatr Care. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 212. | Heeter C, Allbritton M, Lehto R, Miller P, McDaniel P, Paletta M. Feasibility, Acceptability, and Outcomes of a Yoga-Based Meditation Intervention for Hospice Professionals to Combat Burnout. Int J Environ Res Public Health. 2021;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 213. | Kirubarajan A, Got T, Park B, Li X, Sobel M. Interventions to Prevent and Treat Burnout in Obstetrics/Gynaecology: A Scoping Review. J Obstet Gynaecol Can. 2021;43:490-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 214. | Silver J, Caleshu C, Casson-Parkin S, Ormond K. Mindfulness Among Genetic Counselors Is Associated with Increased Empathy and Work Engagement and Decreased Burnout and Compassion Fatigue. J Genet Couns. 2018;27:1175-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 215. | Sutar R, Desai G, Varambally S, Gangadhar BN. Yoga-based intervention in patients with somatoform disorders: an open label trial. Int Rev Psychiatry. 2016;28:309-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 216. | Cocchiara RA, Peruzzo M, Mannocci A, Ottolenghi L, Villari P, Polimeni A, Guerra F, La Torre G. The Use of Yoga to Manage Stress and Burnout in Healthcare Workers: A Systematic Review. J Clin Med. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 95] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 217. | Sutar R, Desai G, Varambally S, Gangadhar BN. An exploratory study of factors influencing acceptance of yoga therapy in somatoform disorder. Asian J Psychiatr. 2020;49:101630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 218. | Rani K, Tiwari SC, Singh U, Agrawal GG, Srivastava N. Six-month trial of Yoga Nidra in menstrual disorder patients: Effects on somatoform symptoms. Ind Psychiatry J. 2011;20:97-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 219. | Kulkarni MS, Kakodkar P, Nesari TM, Dubewar AP. Combating the psychological impact of COVID-19 pandemic through yoga: Recommendation from an overview. J Ayurveda Integr Med. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 220. | Lu JS, Pierre JM. Psychotic episode associated with Bikram yoga. Am J Psychiatry. 2007;164:1761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 221. | Matsushita T, Oka T. A large-scale survey of adverse events experienced in yoga classes. Biopsychosoc Med. 2015;9:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 222. | Lauche R, Schumann D, Sibbritt D, Adams J, Cramer H. Associations between yoga practice and joint problems: a cross-sectional survey among 9151 Australian women. Rheumatol Int. 2017;37:1145-1148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 223. | Cramer H, Quinker D, Schumann D, Wardle J, Dobos G, Lauche R. Adverse effects of yoga: a national cross-sectional survey. BMC Complement Altern Med. 2019;19:190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 224. | Penman S, Cohen M, Stevens P, Jackson S. Yoga in Australia: Results of a national survey. Int J Yoga. 2012;5:92-101. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 225. | Russell K, Gushue S, Richmond S, McFaull S. Epidemiology of yoga-related injuries in Canada from 1991 to 2010: a case series study. Int J Inj Contr Saf Promot. 2016;23:284-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 226. | Ospina MB, Bond K, Karkhaneh M, Tjosvold L, Vandermeer B, Liang Y, Bialy L, Hooton N, Buscemi N, Dryden DM, Klassen TP. Meditation practices for health: state of the research. Evid Rep Technol Assess (Full Rep). 2007;1-263. [PubMed] |
| 227. | Büssing A, Michalsen A, Khalsa SB, Telles S, Sherman KJ. Effects of yoga on mental and physical health: a short summary of reviews. Evid Based Complement Alternat Med. 2012;2012:165410. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 227] [Cited by in RCA: 212] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 228. | Tarsha MS, Park S, Tortora S. Body-Centered Interventions for Psychopathological Conditions: A Review. Front Psychol. 2019;10:2907. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Psychiatry
Country/Territory of origin: Germany
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Byeon H, Stoyanov D S-Editor: Fan JR L-Editor: Filipodia P-Editor: Wang LYT