Published online Dec 20, 2025. doi: 10.5493/wjem.v15.i4.110936
Revised: July 27, 2025
Accepted: October 24, 2025
Published online: December 20, 2025
Processing time: 183 Days and 22.7 Hours
Hematidrosis is an extremely rare and enigmatic condition characterized by spontaneous bleeding through intact skin or mucosa, typically occurring in res
To evaluate the efficacy and safety of beta-blockers, particularly propranolol, in the management of hematidrosis.
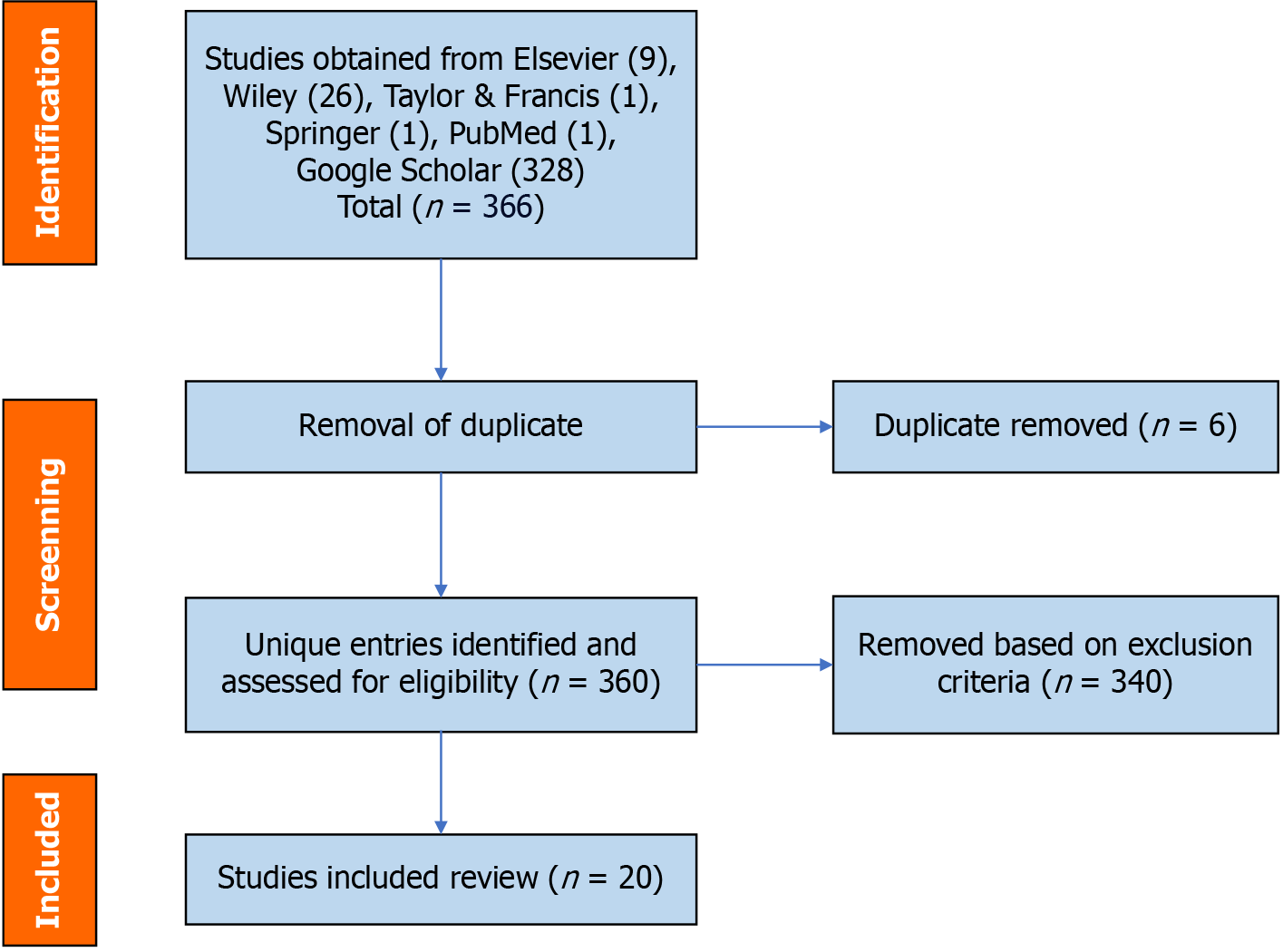
A systematic literature search was conducted in January 2024 across six major databases to identify studies published between 2014 and 2024 that reported the use of beta-blockers in patients with hematidrosis. Eligible studies included clinical case reports or case series that described beta-blocker treatment outcomes. Data were synthesized narratively in accordance with the PRISMA 2020 guide
Twenty studies met the inclusion criteria. Among them, propranolol was the most frequently prescribed beta-blocker and was associated with symptomatic impro
Beta-blockers, especially propranolol, appear to be an effective and well-tolerated treatment option for hematidrosis, particularly in stress-induced presentations. Despite promising findings, the evidence base is constrained by the lack of high-quality studies. Future research should focus on prospective, controlled trials to establish standardized diagnostic and treatment protocols for this rare condition.
Core Tip: Hematidrosis is an extremely rare condition characterized by spontaneous bleeding through intact skin, often triggered by emotional stress. This systematic review evaluates the efficacy and safety of beta-blockers, particularly propranolol, in managing hematidrosis. The findings indicate that propranolol can significantly reduce symptom frequency and severity, especially when combined with psychotherapy. By focusing solely on clinical studies involving beta-blocker use, this review bridges a critical gap in the literature and highlights the need for standardized treatment protocols and controlled clinical trials. The results support a multidisciplinary approach targeting both physiological and psychological triggers.
- Citation: Palabiyik AA. Efficacy of beta-blockers in the treatment of hematidrosis: A systematic review. World J Exp Med 2025; 15(4): 110936
- URL: https://www.wjgnet.com/2220-315x/full/v15/i4/110936.htm
- DOI: https://dx.doi.org/10.5493/wjem.v15.i4.110936
Hematidrosis, a rare medical phenomenon characterized by the excretion of blood-stained fluid through sweat glands, has intrigued clinicians and researchers for centuries[1]. Its occurrence is often linked to extreme physical or psychological stress, with reported cases spanning diverse demographic groups and geographies[2]. Although not life-threatening, the condition poses significant emotional and physical distress to affected individuals[3].
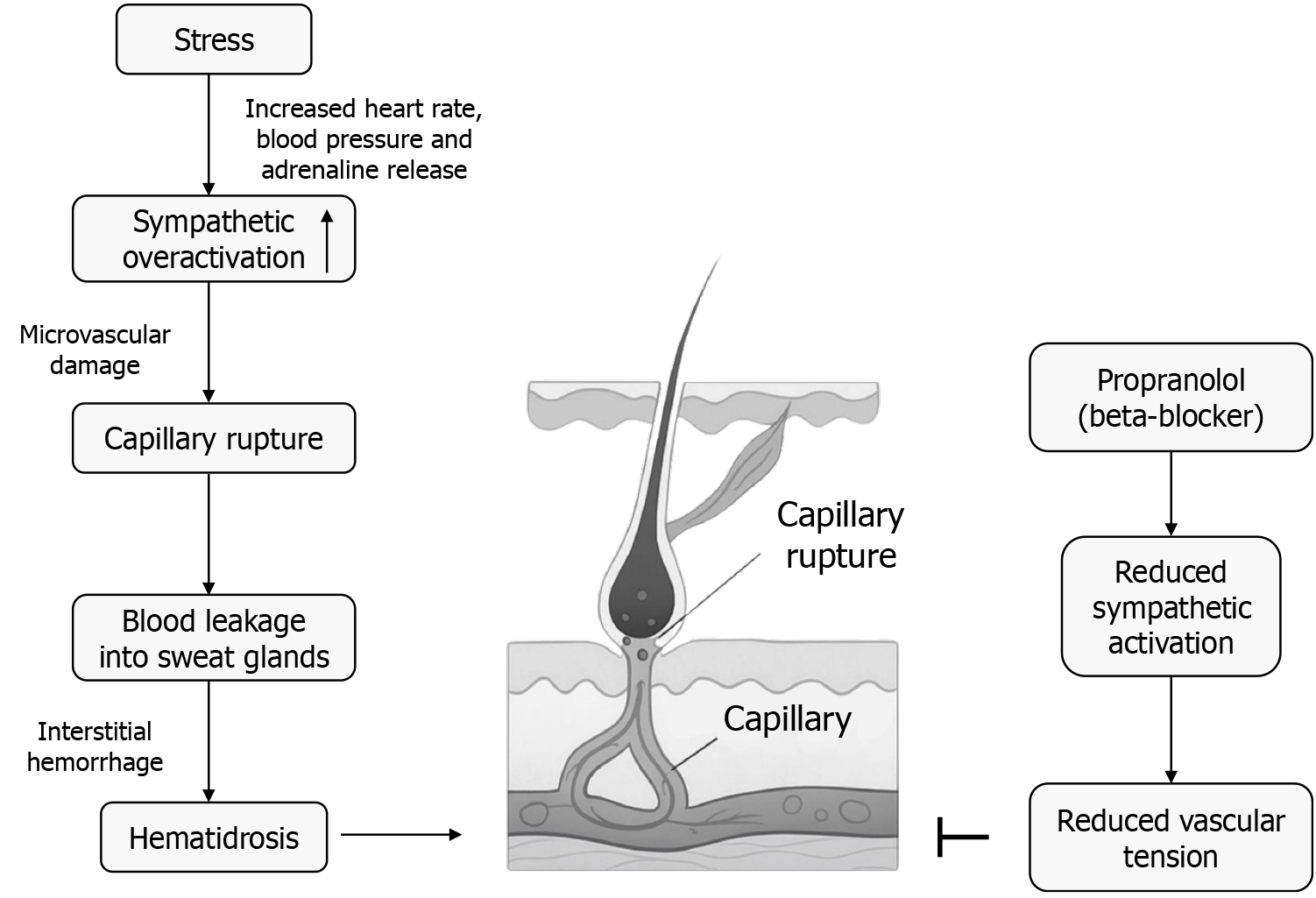
The pathophysiology of hematidrosis remains incompletely understood. The most widely accepted hypothesis suggests that capillary vessels surrounding sweat glands rupture under extreme stress, allowing blood to seep into the glands and mix with sweat[4]. Recent studies also propose a link between autonomic dysregulation and the condition, emphasizing the role of the sympathetic nervous system. This phenomenon is often transient and resolves spontaneously, but severe cases may necessitate medical intervention[1].
Historically, treatment options for hematidrosis have been limited and largely anecdotal. Emerging evidence suggests that beta-blockers, particularly propranolol, may offer therapeutic benefits[5]. These medications work by mitigating the physiological effects of stress through adrenergic inhibition, potentially addressing the underlying pathophysiology of the condition[6]. Combination therapies, including beta-blockers and psychotherapy, have also shown promise in some cases[7].
Rare sweat-related conditions such as chromhidrosis and pseudochromhidrosis have been described in the literature, often mimicking hematidrosis in their clinical presentation. While pseudochromhidrosis involves the excretion of colored sweat caused by chromogenic bacteria or chemical agents rather than blood, its differentiation from true hematidrosis underscores the diagnostic complexity of sweat gland disorders[8].
The bleeding could only be explained as hematohidrosis associated with primary headache of epilepsy/migraine type, infection and stress. The bleeding resolved spontaneously with anti-epileptic agents (Epilim 600 mg, Propranolol 10 mg, Tramacet) and supportive psychotherapy[9].
Our case together with findings from the review indicates that treatment with Beta blockers may be effective for treatment of haematohidrosis in children[10]. Hematidrosis (bloody sweat) remains a controversial but fascinating phenomenon, likely representing a true dermatologic and vascular event associated with extreme stress and sympathetic overactivation rather than a pigmentary or psychogenic artifact[11].
Discrete exceptional clinical entities, not fully understood in their pathogenesis, could possibly constitute the underlying condition to some of these cases, for example, autoerythrocyte sensitization syndrome (Gardner–Diamond syndrome), vicarious menstruation, hematidrosis, and hemolacria[12].
Although the etiology of hematohydrosis is still not fully understood, it is thought that over-activation of the sympathetic nervous system or psychological stress may be involved by increasing local vascular permeability[13].
Hematohidrosis, also known as hematidrosis, is a rare disorder of unknown etiology characterized by recurrent episodes of self-limited exudation of bloody secretion from intact skin and mucosa. Some factors like somatoform and psychosomatic disorders are believed to induce bleeding, particularly acute physical or emotional stress, acute fear, anxiety, and intense mental contemplation[14]. Hematidrosis is an extremely rare condition in which the patient spontaneously starts sweating blood. It often occurs in patients suffering from stress and anxiety, and despite existing for centuries, its pathogenesis remains poorly understood[15].
Hematidrosis, also known as hematohydrosis or hemidrosis, is an episodic and rare skin disease in which blood oozes from the sweat glands, usually occurring during periods of emotional or physical stress[16].
Hematohidrosis is a rare idiopathic condition that manifests as self-limited episodes of spontaneous bloody discharge through intact skin or sweat gland orifices. Some theories have been proposed, including increased vascular pressure leading to the passage of blood cells through the ducts of the sweat glands, vasculitis of dermal vessels and exacerbated sympathetic activation leading to periglandular vessel constriction and subsequent expansion, allowing the passage of blood content into the ducts. There is no specific management of this condition. Wang et al. used propranolol based on the hypothesis of sympathetic overactivity and found it effective[17]. The proposed physiological mechanism through which propranolol acts in hematidrosis is summarized in Figure 1.
Hematohidrosis is a rare clinical condition in which human beings sweat blood under conditions of extreme physical or emotional stress. The capillary blood vessels that feed the sweat glands rupture, causing them to exude blood as sweat, a condition where spontaneous painless bleeding occurs through unbroken skin with a good prognosis[18].
Hematidrosis is an eccrine sweat disorder presenting as one or several episodes of spontaneous, bloody sweating from non-traumatized skin. It remains an elimination diagnosis made after ruling out other conditions such as bleeding disorders, chromhidrosis, or self-inflicted skin lesions[19].
Hematidrosis is a fascinating disorder characterized by blood oozing from the intact skin and mucous membranes in the absence of a bleeding problem. It frequently affects young girls under stressful situations and probably suffering from an underlying anxiety disorder[20].
Despite sporadic reports of successful treatment using beta-blockers, there remains a significant gap between these isolated clinical observations and the establishment of evidence-based management strategies. Therefore, this systematic review aims to bridge this gap by synthesizing existing literature on the use of beta-blockers in hematidrosis, evaluating their therapeutic potential, and highlighting areas that require further clinical research.
A systematic literature review was conducted in accordance with the PRISMA guidelines. The databases searched included Elsevier, Wiley, Taylor and Francis, Springer, PubMed, and Google Scholar to ensure comprehensive coverage of biomedical and clinical research related to hematidrosis. The search spanned from January 2014 to January 2024, reflecting the need to capture recent advancements and case studies on this rare condition.
The literature search included keywords and Medical Subject Headings (MeSH) terms such as “Hematidrosis”, “Hematohidrosis”, and Boolean combinations like “Hematidrosis AND treatment”, “Hematidrosis AND beta-blockers”, “Hematidrosis AND etiology”, and “Hematidrosis AND clinical manifestations”. In PubMed, specific MeSH terms were applied, including “Hematidrosis” (MeSH), “Sweating” (MeSH Terms), and “Skin Manifestations” (MeSH Terms). Boolean logic operators such as AND, OR, and parentheses were utilized to structure nested queries, including more complex combinations like (“Hematidrosis” OR “Hematohidrosis”) AND (“treatment” OR “beta-blockers” OR “etiology” OR “clinical manifestations”).
Peer-reviewed case reports, observational studies. Interventional clinical studies, and systematic/narrative reviews addressing hematidrosis. Studies published in English. Articles providing relevant clinical, genetic, or surgical data.
Non-English language publications. Studies without accessible full texts. Conference abstracts, editorials, letters to the editor, and other non-peer-reviewed formats. Duplicate publications.
Articles lacking relevant clinical, genetic, surgical, or diagnostic data were excluded. An initial total of 366 articles were retrieved from Elsevier (9), Wiley (26), Taylor and Francis (1), Springer (1), PubMed (1), and Google Scholar (328). After deduplication, 360 unique articles remained. Following full-text screening and the application of inclusion/exclusion criteria, 340 articles were excluded at the full-text stage. As a result, 20 articles were included in this systematic review. The full selection process is shown in Figure 2. To assess inter-rater reliability during the study selection phase, Cohen’s Kappa coefficient (κ) was calculated by the author. Of the total 366 records evaluated, both reviewers agreed on the inclusion of 20 articles and the exclusion of another 340. Only a small number of discrepancies were observed, which were resolved through consensus discussions. The observed agreement (Po) was approximately 98.4%, and the expected agreement by chance (Pe) was 50.0%. Based on these values, the Cohen’s Kappa coefficient was calculated as κ = 0.96, indicating almost perfect agreement according to Landis and Koch’s benchmark scale. This high level of inter-rater reliability strengthens the methodological rigor of the review and affirms the clarity and consistency of the inclusion/exclusion criteria applied during the screening process.
In addition to studies involving the administration of beta-blockers, we also included reports that provided comparative therapeutic insights or theoretical discussions relevant to hematidrosis. These studies were considered valuable in framing the broader clinical context and supporting mechanistic interpretations of beta-blocker efficacy.
The findings suggest that beta-blockers, particularly propranolol, play a critical role in the effective management of hematidrosis. In the analyzed studies, beta-blockers were consistently associated with significant reductions in the frequency and severity of bleeding episodes.
A total of 8 clinical studies were included in this systematic review, each reporting the use of beta-blockers in patients with hematidrosis. All involved propranolol, either as monotherapy or in combination with psychotherapy. The reported age range of patients was 9 to 25 years, with a predominance of female patients.
In most studies, propranolol was administered at doses ranging from 10 to 40 mg/day, and symptom improvement rates were typically above 75%. Several reports noted complete remission, particularly in stress-induced cases treated with both pharmacologic and psychological approaches. No adverse effects related to beta-blocker use were observed.
The included studies were primarily case reports and small case series published between 2014 and 2024, originating from diverse geographic regions. None of the studies employed randomized controlled trials or direct comparisons of treatment modalities. These limitations underscore the need for prospective, controlled investigations to optimize treatment protocols. A structured summary of the included studies is presented in Table 1.
| Ref. | Treatment | Main findings | Age (mean/range) | Sex (M/F) | Beta-blocker dosage | Follow-up duration | Outcome measures |
| Anyfantakis et al[1], 2024 | Propranolol, psychotherapy | Symptoms linked to stress; propranolol effective | 10-17 | F: 5/M: 1 | 10-20 mg/day | 4-12 weeks | Symptom cessation, no recurrence |
| Biswas et al[3], 2022 | Propranolol, psychotherapy | Effective control with low-dose propranolol | 13-18 | F: 3 | 10 mg/day | 2-4 weeks | Resolution of symptoms |
| Shafique et al[4], 2021 | Propranolol, psychotherapy | 94% success with propranolol | 9-18 | F: 33/M: 3 | 10-40 mg/day | 1-6 months | Disappearance of hematidrosis episodes |
| Tshifularo[9], 2022 | Propranolol, psychotherapy | Pediatric cases managed successfully | 9-14 | F: 5/M: 2 | 10-20 mg/day | 2-3 weeks | No recurrence reported |
| Prabha et al[17], 2017 | Propranolol | Positive response to propranolol | 12-15 | F: 2/M: 1 | 20-40 mg/day | 3-8 weeks | Cessation of symptoms |
| Tshifularo[18], 2014 | Propranolol, psychotherapy | Improvement under treatment | 13-18 | F: 4 | 10-20 mg/day | 1 month | Episodes resolved |
| Kluger[19], 2018 | Propranolol, relaxation | Stress-related cases improved | 10-25 | F | 10-40 mg/day | Varied | Symptom resolution in most cases |
| Alsermani et al[20], 2018 | Propranolol | Complete resolution of symptoms | 14 | F: 1 | 10 mg twice/day | 3 weeks | Symptom-free |
This systematic review analyzed 20 studies examining the role of beta-blockers, particularly propranolol, in the treatment of hematidrosis a rare and often stress-induced condition characterized by spontaneous bleeding through intact skin. The results suggest that beta-blockers are not only effective but also well-tolerated in the majority of cases, with propranolol demonstrating clinical benefits in over 75% of reported patients.
Consistent with previous findings in the literature, the therapeutic efficacy of beta-blockers appears to stem from their ability to suppress the sympathetic nervous system’s hyperactivation, which is believed to contribute to capillary rupture in response to intense emotional or physical stress. Studies such as those by Shafique et al[4] and Anyfantakis et al[1] reinforce the hypothesis that reducing adrenergic arousal mitigates the hallmark symptom of hematidrosis—bloody sweating.
While beta-blocker monotherapy proved beneficial in several cases, combination strategies that included psychotherapy—particularly cognitive behavioral therapy (CBT)-were associated with enhanced outcomes. This aligns with the multifactorial pathogenesis of hematidrosis, which includes psychological, neurological, and vascular components. As such, a multidisciplinary approach that integrates pharmacologic and psychosocial interventions may offer the most robust and durable treatment response.
A major challenge in synthesizing the data was the considerable heterogeneity among studies. This heterogeneity arose from variations in study design (case reports vs. case series), patient demographics (age and sex distribution), dosing regimens (ranging from 10 mg/day to 40 mg/day of propranolol), and treatment duration (from 1 week to 6 months). Additionally, some studies combined pharmacological treatment with psychotherapy, while others applied propranolol as a monotherapy.
These differences made direct comparisons difficult and precluded meta-analysis. The variability in outcome measures (e.g., subjective symptom relief vs. recurrence monitoring) also limited the ability to draw generalized conclusions.
Furthermore, while propranolol was the most frequently reported beta-blocker, none of the studies offered head-to-head comparisons between different pharmacologic agents or standardized dosing regimens. Long-term outcomes were also sparsely documented, making it difficult to assess relapse rates or sustained efficacy over time.
Despite these limitations, the current evidence suggests a promising therapeutic role for beta-blockers in the management of hematidrosis, particularly in cases triggered by psychological stress. Future research should focus on designing multicenter, controlled trials that evaluate not only the clinical efficacy and safety of beta-blockers but also their long-term effects, optimal dosing strategies, and potential synergy with psychotherapeutic modalities.
This systematic review provides evidence that propranolol, a non-selective beta-blocker, demonstrates promising efficacy and tolerability in managing hematidrosis, particularly in stress-induced cases. Across the analyzed cases, propranolol was consistently associated with reduction or complete cessation of bleeding episodes. Its therapeutic effect appears to stem from modulation of adrenergic overactivation, which is hypothesized to play a key role in the pathophysiology of this rare condition. Integration of beta-blockers with psychotherapeutic interventions, especially CBT, may offer enhanced outcomes in select cases. These findings underscore the clinical relevance of beta-blockers as a first-line option in hematidrosis treatment protocols.
| 1. | Anyfantakis D, Tsoucalas G, Karelis A, Papazoglou N, Spandidos DA, Krasagakis K, Symvoulakis E. Diapedesis leading to hematidrosis due to abrupt emotional suffering (Review). Exp Ther Med. 2024;28:453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Elbadry M, Badry M, Ragab A, Ahmed M. Hematohidrosis: Reports and update of clinically mysterious phenomenon. Indian J Otol. 2020;26:99. [DOI] [Full Text] |
| 3. | Biswas D, Mondal DK, Biswas R, Halder A. Hematidrosis: A rare entity - case series and review of literature. Indian J Psychiatry. 2022;64:423-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 4. | Shafique DA, Hickman AW, Thorne A, Elwood HR, Zlotoff BJ. Pediatric hematidrosis - A case report and review of the literature and pathogenesis. Pediatr Dermatol. 2021;38:994-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (33)] |
| 5. | Ikramuddin S, Liu S, Ryan D, Hassani S, Hasan D, Feng W. Propranolol or Beta-Blockers for Cerebral Cavernous Malformation: a Systematic Review and Meta-analysis of Literature in Both Preclinical and Clinical Studies. Transl Stroke Res. 2024;15:1088-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Mohseni S, Joseph B, Peden CJ. Mitigating the stress response to improve outcomes for older patients undergoing emergency surgery with the addition of beta-adrenergic blockade. Eur J Trauma Emerg Surg. 2022;48:799-810. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Hassan W, Nila SA, Ahmed M, Okello DO, Maqbool M, Dabas MM, Nour M, Khan SM, Ansari F, Anum N, Pervaiz S. Comparative Efficacy and Long-Term Outcomes of Beta-Blockers Alone or in Combination With Angiotensin-Converting Enzyme (ACE) Inhibitors in Chronic Heart Failure: A Systematic Review. Cureus. 2024;16:e74329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Tempark T, Wittayakornrerk S, Jirasukprasert L, Chatproedprai S, Wananukul S. Pseudochromhidrosis: report and review of literature. Int J Dermatol. 2017;56:496-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Tshifularo M. Migraine induced recurrent bloody otorrhea: A spontaneous extra-cranial hemorrhagic phenomena: Case series. Am J Otolaryngol. 2022;43:103218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Hansson K, Johansson EK, Albåge M, Ballardini N. Paediatric haematohidrosis: an overview of a rare but clinically distinct condition. Acta Paediatr. 2019;108:1023-1027. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Favaloro EJ, Lippi G. Commentary: Controversies in Thrombosis and Hemostasis Part 1-Hematidrosis: "Blood, Sweat and Fears" or A "Pigment of Fertile Imaginations?". Semin Thromb Hemost. 2018;44:296-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 12. | Bonamonte D, Vestita M, Filoni A, Giudice G, Angelini G. Religious stigmata as malingering artifact: Report of a case and review of the literature. Medicine (Baltimore). 2016;95:e5354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Aygün B, Gülcü Üstün NS. Hematohydrosis and OCD in a Male Pediatric Patient. Psychiatr Danub. 2023;35:136. [PubMed] |
| 14. | Mutanabbi M, Ali MA, Akhter S, Mosleh T, Morshed J. Haematohidrosis: A Rare Case Report of A 12 year Old Girl with Unexplained and Puzzling Spontaneous Multiple Site Bleeding. Bangladesh J Child Health. 2021;45:45-47. [DOI] [Full Text] |
| 15. | Pandya R. A case report of hematidrosis: blood, sweat, and fear. Eur J Med Case Rep. 2022;6:156-159. [DOI] [Full Text] |
| 16. | Yeşilova Y, Turan E, Aksoy M. Hematidrosis on the forehead following trauma: a case report. Int J Dermatol. 2017;56:212-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Prabha N, Chhabra N, Arora R. Beta-blockers in dermatology. Indian J Dermatol Venereol Leprol. 2017;83:399-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Tshifularo M. Blood otorrhea: blood stained sweaty ear discharges: hematohidrosis; four case series (2001-2013). Am J Otolaryngol. 2014;35:271-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Kluger N. Hematidrosis (bloody sweat): a review of the recent literature (1996–2016). Acta Dermatovenerol APA. 2018;27. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Alsermani M, Alzahrani H, El Fakih R. Hematidrosis: A Fascinating Phenomenon-Case Study and Overview of the Literature. Semin Thromb Hemost. 2018;44:293-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/