Published online Mar 9, 2024. doi: 10.5409/wjcp.v13.i1.88864
Peer-review started: October 13, 2023
First decision: December 11, 2023
Revised: December 17, 2023
Accepted: January 4, 2024
Article in press: January 4, 2024
Published online: March 9, 2024
Processing time: 145 Days and 8.7 Hours
Fever is a common cause of medical consultation and hospital admission, particularly among children. Recently, the United Kingdom’s National Institute for Health and Care Excellence (NICE) updated its guidelines for assessing fever in children under five years of age. The efficient assessment and management of children with fever are crucial for improving patient outcomes.
To evaluate fever assessment in hospitalized children and to assess its adherence with the NICE Fever in under 5s guideline.
We conducted a retrospective cohort review of the electronic medical records of children under five years of age at the Department of Pediatrics, Salmaniya Medical Complex, Bahrain, between June and July 2023. Demographic data, vital signs during the first 48 h of admission, route of temperature measurement, and indications for admission were gathered. Fever was defined according to the NICE guideline. The children were divided into five groups according to their age (0-3 months, > 3-6 months, > 6-12 months, > 12-36 months, and > 36-60 months). Patients with and without fever were compared in terms of demography, indica
Of the 136 patients reviewed, 80 (58.8%) were boys. The median age at admission was 14.2 [interquartile range (IQR): 1.7-44.4] months, with the most common age group being 36-60 months. Thirty-six (26.4%) patients had fever, and 100 (73.6%) were afebrile. The commonest age group for febrile patients (> 12-36 months) was older than the commonest age group for afebrile patients (0-3 months) (P = 0.027). The median weight was 8.3 (IQR: 4.0-13.3) kg. Patients with fever had higher weight than those without fever [10.2 (IQR: 7.3-13.0) vs 7.1 (IQR: 3.8-13.3) kg, respectively] (P = 0.034). Gastrointestinal disease was the leading indication for hospital admission (n = 47, 34.6%). Patients with central nervous system diseases and fever of unknown etiology were more likely to be febrile (P = 0.030 and P = 0.011, respectively). The mean heart rate was higher in the febrile group than the afebrile group (140 ± 24 vs 126 ± 20 beats per minute, respectively) [P = 0.001 (confidence interval: 5.8-21.9)] with a positive correlation between body temperature and heart rate, r = 0.242, n = 136, P = 0.004. A higher proportion of febrile patients received paracetamol (n = 35, 81.3%) compared to the afebrile patients (n = 8, 18.6%) (P < 0.001). The axillary route was the most commonly used for temperature measurements (n = 40/42, 95.2%), followed by the rectal route (n = 2/42, 4.8%). The department demonstrated full compliance with the NICE guideline for five criteria: the type of thermometer used, route and frequency of temperature measurement, frequency of heart rate measurement, and use of antipyretics as needed. Partial compliance was noted for two criteria, the threshold of fever at 38 °C or more, and the respiratory rate assessment in febrile patients. Minimal compliance or no record was observed for the remaining three criteria; routine assessment of capillary refill, temperature reassessment 1-2 h after each antipyretic intake, and refraining from the use of tepid sponging.
This study showed that fever assessment in hospitalized children under five years of age was appropriate, but certain areas of adherence to the NICE guideline still need to be improved.
Core Tip: Fever assessment in children is vital in clinical practice. This study examined the compliance with fever assessment in our hospital according to the National Institute for Health and Care Excellence guideline. We found that while certain aspects were adequate, namely the thermometer type, route, frequency of temperature and heart rate measurement, and appropriate antipyretic use, there were areas that needed improvement, including capillary refill routine assessment, temperature reassessment 1-2 h after antipyretic administration, and refraining from tepid sponging. These findings emphasize the importance of continuous quality improvements in pediatric care to enhance adherence to evidence-based guidelines and improve patient outcomes.
- Citation: Isa HM, Isa AJ, Alnasheet MA, Mansoor MM. Fever assessment in children under five: Are we following the guidelines? World J Clin Pediatr 2024; 13(1): 88864
- URL: https://www.wjgnet.com/2219-2808/full/v13/i1/88864.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v13.i1.88864
Fever is one of the most common reasons for medical consultations in children[1,2]. Fever is the physiological elevation in body temperature in response to various conditions[1]. Infections are the most common causes of fever. Fever due to an infection will most likely result in administration of an antipyretic, performance of investigations, and potentially prescription of an antibiotic. Accordingly, ensuring that we are dealing with fever in the first place is crucial.
Fever is defined by the National Institute for Health and Care Excellence (NICE) as an elevation in body temperature above the normal daily variations[1]. Despite being ambiguous, this definition takes into account that the core body temperature is subject to variations, as many factors can influence the body temperature, such as age, time of the day, level of activity, and meals[3]. In the pediatric age group, a temperature of 38 °C or higher is generally considered fever[1]. There is considerable controversy regarding the best anatomical site for temperature measurement and the best thermometer to use[4].
Although not convenient for repeated use, the rectal thermometer is generally considered an accurate reflection of the body’s core temperature[5-11]. Choosing the instrument for accurate measurement can be difficult. Tympanic thermo
The NICE Fever in under 5s guideline recommends the use of axillary electronic thermometers for temperature measurement in infants under the age of 4 wk[2]. For children aged 4 wk to 5 years, it is recommended to use axillary electronic thermometers, axillary chemical dot thermometers, or infra-red tympanic thermometers[2]. The guideline does not emphasize routine use of oral or rectal routes to measure body temperature in children aged 0-5 years[2]. The gui
Although many studies on the methods of measuring and managing fever in children have been reported worldwide, no studies on this topic have been reported in Bahrain. This study aimed to assess the current practice of fever measurement in the main hospital in Bahrain and compare it with the NICE guideline.
This was a retrospective cohort study based on the electronic medical records of patients admitted to the Department of Pediatrics, Salmaniya Medical Complex (SMC), Bahrain between June 1, 2023 and July 11, 2023. SMC is the main tertiary care hospital in Bahrain to which most pediatric cases are referred for admission. It has 30 wards and a total capacity of 1200 beds.
The Department of Pediatrics has four general wards for 75 patients. In each ward, three nurses per shift were responsible for the daily measurement of temperature and other vital signs, including blood pressure, heart and respiratory rates, and pulse oximetry. All measurements were performed by pediatric ward nurses and immediately entered into the electronic medical records. Temperature recordings were performed every 4 h for each patient regardless of the condition. In febrile patients, the temperature was also recorded 30-60 min after each antipyretic intake. For children less than one year of age, temperature measurements are usually performed using the axillary or rectal routes. For children above one year of age, temperature measurements are usually performed via oral or axillary routes.
Temperature measurements were performed using a Food and Drug Administration-approved electronic thermometer (Welch-Allyn SureTemp Plus Model 692, New York, United States). The thermometer contained a liquid-crystal display screen and several buttons: a button to toggle between Celsius and Fahrenheit scales, a pulse timer, a mode selection button to choose the site for measurement, and a recall button to display the last measured temperature. Two probes can be used to obtain measurements using this thermometer: a red probe for rectal measurements and a blue probe for oral or axillary measurements. The different routes and types of thermometers used to assess the temperature in children are shown in Figure 1.
The study population comprised all children with ages ranging from birth to five years, who were admitted for 48 h or more to the pediatric ward during the study period. Premature babies, children with bleeding disorders, immunocompromised or neutropenic patients, children with burns or extensive skin diseases, children with anorectal pathologies, and patients in the neonatal intensive care unit were excluded from the study.
Demographic data including sex, age, reason for admission, and weight (kg) on admission were collected. The anatomical site used for temperature measurement was noted. The first recorded temperature in the ward, along with heart and respiratory rates, were collected. These parameters were recorded for each patient during the first 48 h of admission. The threshold of fever was set to ≥ 38 ˚C, according to the recommendations set by NICE[1]. For each patient, the first and second indications for admission as well as the presence of an underlying disease were noted when applicable, and these indications were categorized based on the main system involved in the patient’s disease.
Data were entered into an Excel worksheet and then analyzed using the Statistical Package for Social Sciences program version 28 (IBM Corp., Armonk, NY, United States). The children were divided into five groups according to their age in months (0-3, > 3-6, > 6-12, > 12-36, and > 36-60). Categorical variables were presented as frequency and percentage while continuous variables were presented mean ± SD or median and interquartile range (IQR), according to normality of distribution. Patients were divided into two groups (febrile and afebrile). Febrile group included any patient who had a spike in temperature ≥ 38 °C during the first 48 h of admission. Patients with and without fever were compared in terms of demography, indication for admission, route of temperature measurement, and other vital signs. Compliance with the NICE Fever in under 5s guideline was assessed. Full compliance was defined as > 95%, partial compliance as 70%-95%, and minimal compliance as ≤ 69%. Group data were compared using Pearson’s χ2 test for categorical variables, and Student’s t test or Mann-Whitney U test for continuous variables. Body temperature measurements were correlated with heart and respiratory rates using Spearman’s correlation coefficient (rs). The coefficient of determination (r2) and a simple regression equation were calculated. The confidence interval (CI) was set to 95%. P value < 0.05 was considered statistically significant.
This study was conducted in accordance with the principles of Helsinki Declaration, and it was ethically approved by the Research and Research Ethics Committee, Salmaniya Medical Complex, Government Hospitals, Kingdom of Bahrain (IRB number: 38020523, May 02, 2023).
The records of 136 patients were reviewed during the study period. The patient demographic data are shown in Table 1. Eighty (58.8%) patients were boys, and 56 (41.2%) were girls. Ninety-seven (71.3%) patients were Bahraini nationals, while 39 (28.7%) were non-Bahraini (11 patients were from Pakistan, nine from India, seven from Yemen, three from Egypt, two from the Philippines and Tunisia each, one patient from Nepal, Oman, Sri Lanka, Sudan, and Syria). The median age at the time of admission was 14.2 (IQR: 1.7-44.4) months. The most common age group was > 36-60 months (n = 43, 31.6%). Thirty-six (26.4%) patients had fever, and 100 (73.6%) were afebrile. Febrile patients were older in age [15.6 (IQR: 6.8-44.2) months] than afebrile patients [11.1 (IQR: 0.7-45.1) months], but this difference was not statistically significant (P = 0.097). The most frequent age group among patients with fever was >12-36 months, whereas that among patients without fever was 0-3 months (P = 0.027). The median weight on admission was 8.3 (IQR: 4.0-13.3) kg. Patients with fever had higher median weight [10.2 (IQR: 7.3-13.0) kg] than those without fever [7.1 (IQR: 3.7-13.3) kg] (P = 0.034).
| Demographic data | Total, n = 136 (100) | Febrile1, n = 36 (26.5) | Afebrile, n = 100 (73.5) | P value |
| Sex | 0.3252 | |||
| Male | 80 (58.8) | 24 (66.7) | 56 (56) | |
| Female | 56 (41.1) | 12 (33.3) | 44 (44) | |
| Nationality | 0.2852 | |||
| Bahraini | 97 (71.3) | 23 (63.9) | 74 (74) | |
| Non-Bahraini | 39 (28.6) | 13 (36.1) | 26 (26) | |
| Age at presentation (mo) | 0.0273 | |||
| 0-3 | 39 (28.7) | 4 (11.1) | 35 (35) | |
| > 3-6 | 8 (5.9) | 4 (11.1) | 4 (4) | |
| > 6-12 | 17 (12.5) | 5 (13.9) | 12 (12) | |
| > 12-36 | 29 (21.3) | 12 (33.3) | 17 (17) | |
| > 36-60 | 43 (31.6) | 11 (30.6) | 32 (32) | |
| Weight on admission (kg), (n = 124) | 8.3 (4.0-13.3) | 10.2 (7.3-13.0) | 7.1 (3.7-13.3) | 0.0344 |
| Anatomical site of temperature measurement, (n = 42) | 1.0002 | |||
| Axillary | 40 (95.2) | 16 (40) | 24 (60) | |
| Rectal | 2 (4.8) | 1 (50) | 1 (50) |
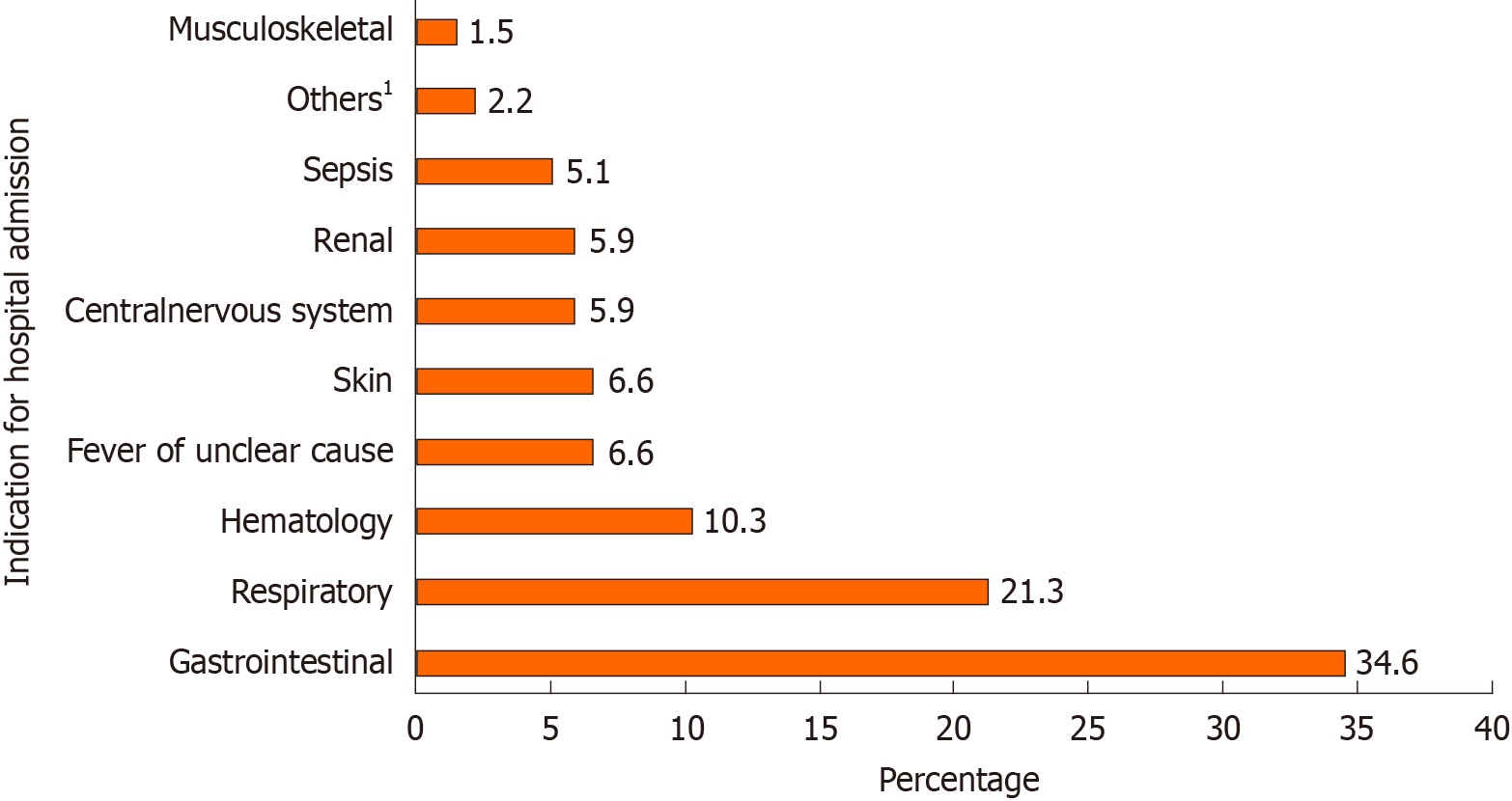
The indications for hospital admission are shown in Figure 2. The most frequent cause of admission was gas
| Diagnosis | Total, n = 136 (100) | Febrile, n = 36 (26.5) | Afebrile, n = 100 (73.5) | P value1 |
| Gastrointestinal disease | 47 (34.6) | 8 (22.2) | 39 (39.0) | 0.101 |
| Respiratory disease | 29 (21.3) | 11 (30.6) | 18 (18.0) | 0.154 |
| Hematological disease | 14 (10.3) | 2 (5.6) | 12 (12.0) | 0.353 |
| Fever of unknown etiology | 9 (6.6) | 6 (16.7) | 3 (3.0) | 0.011 |
| Skin disease | 9 (6.6) | 1 (2.8) | 8 (8.0) | 0.444 |
| Central nervous system disease | 8 (5.9) | 5 (13.9) | 3 (3.0) | 0.030 |
| Renal disease | 8 (5.9) | 1 (2.8) | 7 (7.0) | 0.681 |
| Sepsis | 7 (5.1) | 0 (0.0) | 7 (7.0) | 0.189 |
| Musculoskeletal disease | 2 (1.5) | 1 (2.8) | 1 (1.0) | 0.461 |
| Others2 | 3 (2.2) | 1 (2.8) | 2 (2.0) | 1.000 |
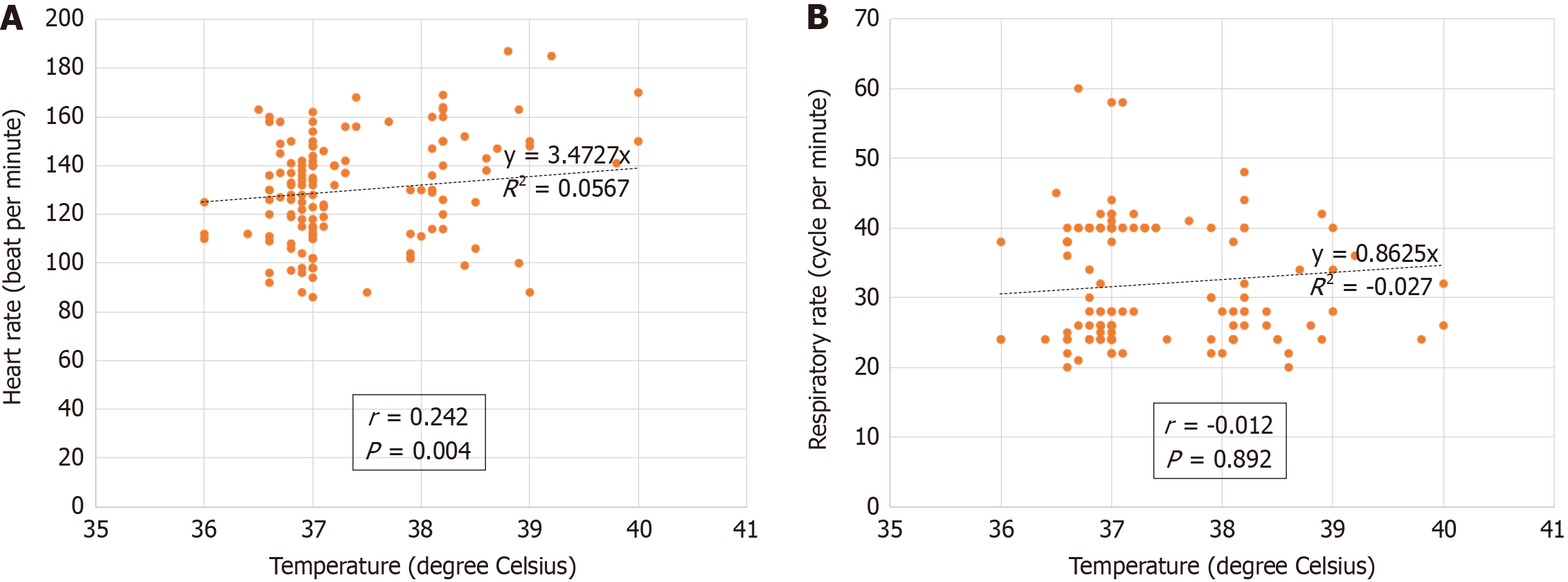
The recorded body temperature and its relationship with the heart and respiratory rates are shown in Table 3. Most of the patients were afebrile (n = 100, 73.5%) while the remaining 36 (26.5%) patients had a temperature of 38 °C or above [10 (7.4%) were febrile on admission and 26 (19.1%) developed fever later during their hospital stay]. Patients in the febrile group had a higher mean heart rate than the afebrile group, 140 ± 24 vs 126 ± 20 beats per minute, respectively [P = 0.001 (CI: 5.8-21.9)]. There was a positive correlation between body temperature and heart rate, r = 0.242, n = 136, P = 0.004 while no significant correlation was detected between temperature and respiratory rate, r = -0.012, n = 135, P = 0.892 (Figure 3). None of the patients had capillary refill recorded while in the hospital ward. Paracetamol was administered to 43 (31.6%) patients. A greater proportion of febrile patients (n = 35, 81.3%) received paracetamol than afebrile patients (n = 8, 18.6%); (P < 0.001).
The current practice of fever assessment in the pediatric department was compared with the NICE Fever in the under 5s guideline (Table 4). Full compliance (> 95%) was achieved for five key criteria: the type of thermometer used, route of temperature measurement, frequency of temperature and heart rate measurements, and use of antipyretics in children with fever who appear distressed. In contrast, partial compliance (70%-95%) was observed for two criteria; the threshold of fever at 38 °C or more (93%), and the respiratory rate assessment in febrile patients. Minimal compliance (< 65%) or no record was observed for the remaining three criteria (routine assessment of capillary refill, temperature reassessment 1-2 h after each antipyretic intake, and refraining from the use of tepid sponging).
| Criterion1 | Compliance | ||
| Minimal | Partial | Full | |
| 1: Fever is considered if temperature is 38 degrees Celsius or more | - | Yes | - |
| 2: Do not routinely use oral or rectal routes to measure the body temperature of children 0-5 yr | - | - | Yes |
| 3: In infants under the age of 4 wk, measure the body temperature with an electronic thermometer under the axilla | - | - | Yes |
| 4: In children aged 4 wk to 5 yr, measure the body temperature by one of the following: Electrical thermometer to the axilla, chemical dot thermometer to the axilla, or infra-red tympanic thermometer | - | - | Yes |
| 5: As part of routine assessment of children with fever: Record the heart rate | - | - | Yes |
| 6: As part of routine assessment of children with fever: Record the respiratory rate | - | Yes | - |
| 7: As part of routine assessment of children with fever: Record the capillary refill time | NR | NR | NR |
| 8: Use of antipyretics in children with fever who appear distressed | - | - | Yes |
| 9: In case of febrile patient, the temperature is reassessed 1-2 h after each anti-pyretic intake | Yes | - | - |
| 10: The use of tepid sponging is not recommended for the treatment of fever | NR | NR | NR |
This study found a male predominance (58.8%) among the children who required hospital admission. This trend is consistent with the results of other studies conducted in different countries. This percentage is similar to that reported by Mehdi et al[12] in Pakistan and Ambaye et al[13] in Ethiopia (58% each) and comparable with that observed by Alam et al[14] and George et al[15] in Bangladesh and Nepal (51% and 71%, respectively). However, the reason for this male predominance has not been extensively studied. A reasonable explanation for this may be the higher male birth rate in this population. With regard to live birth statistics from Bahrain’s national registry, although there is a consistently higher birth rate of boys than of girls, the difference is relatively modest. According to the latest available records from 2016 to 2020, the difference in birth rates was between 50.5% and 51.7%[16]. While these percentages reflect a male predominance in the birth rate, they are unlikely to be the major contributing factor to the higher male predominance reported in our study. This male predominance may also be attributed to a sex bias in the health-seeking behavior of parents[14,17]. Other potential reasons include sociocultural variations and biological/genetic differences in disease susceptibility across the sexes. However, the sex distribution requires further investigation.
We observed a significant association between patient weight at admission and the presence of fever (P = 0.034). Patients with fever had a higher median weight than the afebrile patients. This finding raises questions about the potential relationship between a child’s weight and their susceptibility to developing fever, and whether body weight itself could be a contributing factor leading to hospital admission.
The top three reasons for hospital admission in the current study were gastrointestinal (34.6%), respiratory (21.3%), and hematological (10.3%) diseases. Gastrointestinal disease predominance was similar to the findings of other studies published in Pakistan and Bangladesh, as reported by Mehdi et al[12] and Alam et al[14], respectively. In contrast, studies conducted in other countries have shown respiratory diseases to be the predominant cause of admission in this age group, including those conducted by Ambaye et al[13] in Ethiopia, George et al[15] in Nigeria, Bhurtel et al[18] in Nepal, and Merrill et al[19] in the United States of America. These differences might be the result of variations in healthcare availability, environmental factors, societal hygiene practices, vaccination rates, antibiotic use, dietary habits, population density, and migration patterns[20].
Temperature is a vital sign that is routinely measured in patients admitted for fever[1]. Assessing the accuracy and consistency of the routes used for temperature measurement is important because the presence of fever can significantly influence diagnostic and treatment decisions[1,3]. This study showed a preference for the axillary route (n = 40/42, 95.2%), followed by the rectal route (n = 2/42, 4.8%); the tympanic thermometer route was not utilized. This aligns with the existing literature regarding the ongoing debate regarding the optimal thermometer route for accurate temperature assessment[4-11]. While rectal thermometry is generally regarded as a reliable indicator of core body temperature, recent studies have suggested the limitations of this method, especially for repetitive use[4]. The limitations include the discomfort it causes to patients, time consumption, the slow rise and drop in its readings in relation to core temperature, the effect of local blood flow and stool on its accuracy, the risk of perforation and a general need for privacy. Research is exploring alternative routes[5-11]. Tympanic thermometry has been recognized by different studies for its accuracy and convenience compared with the rectal and axillary routes[10,11]. It measures the thermal radiation of the tympanic membrane using infrared radiation emission detectors, either through thermopile or pyroelectric sensors[4]. Due to the close proximity of the tympanic membrane’s blood supply and the body’s thermoregulatory sensor, the hypothalamus, tympanic temperature measurements were found to provide the closest measurement to the core body temperature[5-11]. Adding to that, tympanic thermometers are fast and easy to use, and are therefore cost-effective in terms of nursing time[4]. Axillary thermometry relies on the placement of thermometers over the axillary artery for more than four minutes for mercury-based and 40-80 s for electronic-based thermometers, which has an impact on nursing time[4]. Although simple to use, it has shown limitations in accuracy mainly because it requires proper placement and supervision, and local factors such as blood flow and sweat can affect precision[4,5,21,22]. Despite this, NICE still recommends its use in children under five years of age[2]. Valuable information for optimizing temperature assessment in the pediatric population can be obtained from further evaluation of these routes.
A variable level of compliance was found in the current practice compared to the NICE Fever in under 5s guideline. Ten key criteria were used for evaluation. Our department demonstrated full compliance (> 95%) to certain guidelines, including routine assessment of heart rate, using antipyretics as necessary for temperatures ≥ 38 °C, and measuring temperatures using specific routes and types of thermometry. Conversely, partial compliance (70%-95%) was noted when considering fever exclusively for temperatures above a threshold of 38 °C (93%), as well as routine assessment of the respiratory rate. Additionally, our data point to minimal compliance (< 65%) with regard to the reassessment of tem
The study’s strengths are its approach to investigating current practices in a specific age group within a specific setting. Moreover, it provides a comprehensive analysis of a diversity of factors, including age, sex, reason for admission, and weight. Comparing the effects of these factors with those of other international studies has provided valuable information regarding the similarities and differences in pediatric admissions and fever assessment. The evaluation of compliance with the NICE guideline is a practical implementation of evidence-based recommendations and emphasizes the importance of quality improvement in healthcare. Furthermore, this study identified potential areas of investigation such as sex distribution, reasons for admission, and weight differences between febrile and afebrile patients, which opens the door for future research.
This study was limited by its retrospective nature and reliance on electronic medical records for data collection, which led to a lack of some relevant data. Additionally, despite SMC being the main hospital in Bahrain, this was a single-center study, which may limit the generalizability of its results. The study could not include records of capillary refill time, or use of non-pharmacological interventions, because they were incomplete due to customary record-keeping practices. Another limitation was that most patients were usually seen in the pediatric emergency department before admission; thus, records of the first true temperature and initial management were absent, as the data were inclusive only of pediatric inpatient records. Moreover, tympanic thermometers were not used in our patients, which might have limited the comparison between different types of temperature measurement routes. Despite these limitations, the present study is the first to evaluate fever in the Department of Pediatrics in Bahrain and can form a foundation for future studies.
This study provides valuable information regarding the patterns of pediatric admissions, temperature measurement routes, and compliance with the NICE guideline for Fever in under 5s, in the Department of Pediatrics at the Salmaniya Medical Complex in Bahrain. This revealed a male predominance in hospital admissions, with gastrointestinal diseases being the most common reason for admission in children below five years of age. The axillary route of temperature measurement was predominantly used, whereas tympanic thermometry was never utilized despite its recognized accuracy and convenience. The assessment of compliance with the NICE guideline revealed both areas of adherence and areas that needed improvement. Further studies that focus on exploring sex disparities in pediatric admissions, weight differences between febrile and afebrile patients, the use of tympanic thermometry for temperature assessment, and the impact of conducting regular audits to help track improvements in adherence to guidelines and their impact on patient care are needed.
Fever is a common cause of medical consultations and hospital admissions in children. It is a physiological elevation in body temperature in response to various conditions. Recently, the United Kingdom’s National Institute for Health and Care Excellence (NICE) updated its guidelines for assessing fever in children under five years of age. The presence of fever and proper fever assessment can have a significant impact on investigations, management plans, and the overall prognosis of patients.
Many studies on fever assessment in children have been reported worldwide; however, no such studies have been conducted in Bahrain. This gap motivated us to evaluate the current practices of fever assessment.
To evaluate the current practice of fever assessment in hospitalized children under five years in the main hospital in Bahrain and to assess its adherence to the NICE Fever in under 5s guideline.
We retrospectively reviewed the electronic medical records of children under five years of age admitted to the Department of Pediatrics, Salmaniya Medical Complex, Bahrain, between June and July 2023. Demographic data, vital signs during the first 48 h of admission, route of temperature measurement, and indications for admission were collected. The children were divided into five groups according to their age in months. The NICE Fever in under 5s guideline was used to define fever. Febrile and afebrile patients were compared in terms of demography, indication of admission, route of temperature measurement, and other vital signs. Compliance with the NICE guideline was assessed.
Of the 136 patients reviewed, 80 (58.8%) were boys. The median age at admission was 14.2 [interquartile range (IQR): 1.7-44.4] months. Thirty-six (26.4%) patients had fever, and 100 (73.6%) were afebrile. The commonest age group of febrile patients was higher (> 12-36 months) than for the group without fever (0-3 months) (P = 0.027). The median weight was 8.3 (IQR: 4.0-13.3) kg. Patients with fever had higher weight than those without [10.2 (IQR: 7.3-13.0) vs 7.1 (IQR: 3.8-13.3) kg, respectively] (P = 0.034). Gastrointestinal disease was the leading indication for hospital admission (n = 47, 34.6%). Patients with central nervous system diseases and fever of unknown etiology were more likely to be febrile (P = 0.030 and P = 0.011, respectively). The mean heart rate was higher in the febrile group than the afebrile group (140 ± 24 vs 126 ± 20 beats per minute, respectively) [P = 0.001 (confidence interval: 5.8-21.9)] with a positive correlation between body temperature and heart rate, r = 0.242, n = 136, P = 0.004. A higher proportion of febrile patients received paracetamol (n = 35, 81.3%) than the afebrile patients (n = 8, 18.6%) (P < 0.001). The axillary route was most commonly used for temperature measurements (n = 40/42, 95.2%), followed by the rectal route (n = 2/42, 4.8%). The department demonstrated full compliance with the NICE guideline for five criteria: type of thermometer, route and frequency of temperature measurement, frequency of heart rate measurement, and use of antipyretics as needed. Partial compliance was noted for two criteria, the threshold of fever at 38 °C or more, and the respiratory rate assessment in febrile patients. Minimal compliance or no record was observed for the remaining three criteria (routine assessment of capillary refill, temperature reassessment 1-2 h after each antipyretic intake, and refraining from the use of tepid sponging).
The evaluation of fever in children under five years of age revealed areas of adherence to the guideline and areas that require enhancement. Specific noteworthy findings have emerged, such as a higher number of boys being admitted to the hospital, a common occurrence of gastrointestinal diseases, a significant difference in weight between febrile and afebrile patients, and an underuse of tympanic thermometry despite its established accuracy and convenience.
Specific improvements in fever assessment in children under the age of five years should be implemented in accordance with international guidelines. Further studies exploring the sex disparities, indications for admission, and weight differences between febrile and afebrile patients are warranted. Furthermore, the use of tympanic thermometry for temperature assessment in children should be explored.
The authors gratefully acknowledge all those who provide care for children in the Department of Pediatrics, Salmaniya Medical Complex, Kingdom of Bahrain.
| 1. | Ischimine P. Assessment of fever in children. BMJ Best Practice 2023. Cited 26 Aug 2023. Availabe from: https://bestpractice.bmj.com/topics/en-gb/692#. |
| 2. | Fever in under 5s: assessment and initial management. London: National Institute for Health and Care Excellence (NICE); 2021-Nov-26 . [PubMed] |
| 3. | Barbi E, Marzuillo P, Neri E, Naviglio S, Krauss BS. Fever in Children: Pearls and Pitfalls. Children (Basel). 2017;4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | El-Radhi AS, Barry W. Thermometry in paediatric practice. Arch Dis Child. 2006;91:351-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 95] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Temperature measurement in paediatrics. Paediatr Child Health. 2000;5:273-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Mogensen CB, Wittenhoff L, Fruerhøj G, Hansen S. Forehead or ear temperature measurement cannot replace rectal measurements, except for screening purposes. BMC Pediatr. 2018;18:15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Romanovsky AA, Quint PA, Benikova Y, Kiesow LA. A difference of 5 degrees C between ear and rectal temperatures in a febrile patient. Am J Emerg Med. 1997;15:383-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Pecoraro V, Petri D, Costantino G, Squizzato A, Moja L, Virgili G, Lucenteforte E. The diagnostic accuracy of digital, infrared and mercury-in-glass thermometers in measuring body temperature: a systematic review and network meta-analysis. Intern Emerg Med. 2021;16:1071-1083. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 9. | Mah AJ, Ghazi Zadeh L, Khoshnam Tehrani M, Askari S, Gandjbakhche AH, Shadgan B. Studying the Accuracy and Function of Different Thermometry Techniques for Measuring Body Temperature. Biology (Basel). 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Erdem N, Demirdağ TB, Tezer H, Cura-Yayla BC, Baran-Aksakal FN, Tapısız A, Derinöz O, Okur A, Pınarlı FG, Koçak Ü, Bideci A. The comparison and diagnostic accuracy of different types of thermometers. Turk J Pediatr. 2021;63:434-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 11. | Shi D, Zhang LY, Li HX. Diagnostic test accuracy of new generation tympanic thermometry in children under different cutoffs: a systematic review and meta-analysis. BMC Pediatr. 2020;20:210. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Mehdi Ah, Riaz K, Ghazal N, Kamran NS, Saboohi E, Malick AHH, Tariq AB. Disparities among pediatric hospital admissions according to gender. Int J SciRep. 2020;6:269-273. [DOI] [Full Text] |
| 13. | Ambaye M, Tefera M. Pattern of admissions to the pediatric emergency unit of Tikur Anbessa Hospital in Addis Ababa, Ethiopia (2012-2013 G.C). Ethiop J Health Dev. 2016;30:86-91. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Alam D, Islam S, Roy B, Md Shahid, Roy TK, Rahman SM. Disease Profile Among Children Admitted in a Tertiary Care Hospital. Chatt Maa Shi Hosp Med Coll J. 2019;31-35. [DOI] [Full Text] |
| 15. | George IO, Alex-Hart BA, Frank-Briggs AI. Mortality pattern in children: a hospital based study in Nigeria. Int J Biomed Sci. 2009;5:369-372. [PubMed] [DOI] [Full Text] |
| 16. | Ministry of Health. Health Statistics 2020. 31 May 2022. Cited 11 Dec 2023. Available from: https://www.moh.gov.bh/Content/Files/Publications/statistics/HS2020/PDF/CH-03-vital%20stat_2020%20(2).pdf. |
| 17. | Ismail SA, McCullough A, Guo S, Sharkey A, Harma S, Rutter P. Gender-related differences in care-seeking behaviour for newborns: a systematic review of the evidence in South Asia. BMJ Glob Health. 2019;4:e001309. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 18. | Bhurtel R, Pokhrel RP, Kalakheti B. Acute Respiratory Infections among Under-five Children Admitted in a Tertiary Hospital of Nepal: A Descriptive Cross-sectional Study. JNMA J Nepal Med Assoc. 2022;60:17-21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 19. | Merrill C, Owens PL. Reasons for Being Admitted to the Hospital through the Emergency Department for Children and Adolescents, 2004. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006. [PubMed] |
| 20. | Keating EM, Haq H, Rees CA, Dearden KA, Luboga SA, Schutze GE, Kazembe PN. Global Disparities Between Pediatric Publications and Disease Burden From 2006 to 2015. Glob Pediatr Health. 2019;6:2333794X19831298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Paramita T, Karyanti M, Soedjatmiko S, Hendarto A, Suyoko D, Latief A. A comparison of axillary and tympanic membrane to rectal temperatures in children. Paediatr Indones. 2017;57:47-51. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Edelu BO, Ojinnaka NC, Ikefuna AN. A comparison of axillary with rectal thermometry in under 5 children. Niger Med J. 2011;52:207-210. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Bahrain Medical Society, 20000547; National Health Regulation Authority, 11002084; Al-Kawther Society for Social Care, 133.
Specialty type: Pediatrics
Country/Territory of origin: Bahrain
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shahriari M, Iran S-Editor: Liu JH L-Editor: A P-Editor: Zheng XM